Introduction:
Despite outspending other high-income nations in medical care, the United States consistently underperforms on many indicators of health.1 This is true for maternal and newborn outcomes and of particular concern are wide racial/ethnic inequities in obstetric outcomes. Black and Latina mothers suffer excess rates of severe maternal morbidity.2–5 Further, black women are three to four times more likely to die from pregnancy-related causes than white women.4 Moreover, Native Americans and some Asians and Latinas experience maternal deaths more often than white women.4,6
Shortfalls in hospital quality and safety contribute to poor obstetric outcomes. The Institute of Medicine has defined healthcare quality as “the degree to which health services for individuals and populations increase the likelihood of desired health outcomes and care consistent with current professional knowledge.”7 Ideally, quality of care should provide health services consistent with standard of care and consistently bend the arc of a patient’s treatment course towards a healthy outcome.8 In obstetrics, processes of care and outcomes vary greatly across hospitals after risk adjustment, suggesting that this standard is not achieved for all women. For instance, cesarean delivery rates vary 10 fold.9 Administration of oxytocin and use of episiotomies differ greatly among labor and delivery units.10 Similarly, rates of postpartum hemorrhage, peripartum infection and severe perineal laceration also vary.11 Though measures of key interventions and many outcomes in obstetrics show significant variability, so too do the most severe outcomes, like maternal mortality and severe maternal morbidity.
Poor quality and safety generate health inequities in the form of racial and ethnic disparities in obstetric outcomes. As defined by Dr. Paula Braveman, health equity refers to a broader concept of “social justice in health (i.e. no one is denied the possibility to be healthy for belonging to a group that has historically been economically/socially disadvantaged),” whereas “ health disparities are the metric we use to measure progress toward achieving health equity.” In this paper, we refer to maternal health disparities in this context.12 While these disparities are linked with economic, social and environmental disadvantage, quality of care is an underlying cause that is potentially modifiable.13,14 Thus, targeting efforts towards improving quality of care, grounded in health equity, is a key to addressing racial and ethnic disparities.
To understand our failures in achieving the highest quality of care in obstetrics, there are two methodologies at our disposal - qualitative and quantitative. Quantitative research “counts” – whether it be “prevalence, frequency, magnitude, incidence” and qualitative describes “the complexity, breadth, or range of occurrences or phenomena.”15 While quantitative studies are designed to obtain accurate, generalizable data and to limit confounding variables, qualitative research depends on collecting data in the natural environment and producing non-quantified information that reflects variation in individual and institutional responses, experiences and perspectives, through open-ended discussions and observations.16 Mixed-methods synergize features of both qualitative and quantitative methods to generate a richer and ideally, complementary data set. To date, most studies looking at quality and safety and racial/ethnic disparities in obstetrics have relied on quantitative approaches; thus, our understanding of the context surrounding variation remains elusive and questions on the drivers of these disparities are often left unanswered.
In this paper, we ask how research in obstetrical quality can go beyond a purely quantitative approach to tackle the challenge of health inequity in quality and safety. The current framework relies on quantitative approaches to measure the magnitude of disparities in processes and outcomes in obstetrics. However, combining quantitative with qualitative methods can provide an opportunity to delve deeper and to understand their drivers and causes. We also consider how to incorporate women’s voices and experiences, often neglected, into our research methods.
We start by exploring mixed methods approaches, specifically positive deviance, which has been used in many areas of medicine, but not in obstetrics. We then describe the use of quantitative methods in obstetrics and highlight the limitations of only using this approach, especially when tackling disparities. Next, we present some qualitative studies carried out in obstetrics and the insights provided by this method. We end by showing the potential of positive deviance, as a mixed methods approach, to generate new knowledge for addressing racial and ethnic disparities in maternal outcomes.
Positive Deviance within a Mixed Methods Approach
An area of interest in mixed methods is positive deviance (PD). Although it was first thought of as an ethnographic qualitative approach, there has been a push to use PD in a mixed methods framework, as a means to bridge the qualitative and quantitative.16,17 The core of the PD approach is that solutions to problems that face a community often exist within that community and that certain members possess a specific set of knowledge and skills that can be applied across the board to improve performance of others.18 The PD approach examines variation in performance in a particular measure, among a cohort of people or institutions, pools together high performers and conducts interviews to understand practices that cause “positive deviance” from average or below-average performers. PD was first applied in the setting of malnutrition. In Bangladesh, an observational study to distinguish what made some children thrive and others become malnourished, revealed different practices in hand-washing, contact with cattle and dryness of the earth surface that babies were left to play on.19 These lessons provided answers for a problem not otherwise captured by traditional methods of data collection and ultimately, were disseminated to reduce malnutrition and diarrheal illness for other community members. A key feature of PD includes dissemination of lessons learned to improve low performers; in that way, PD is an active form of research, dedicated to providing real time solutions for real time problems.20 The PD approach has been employed in other fields like education, business, government and most importantly, extended to understand medical care and health systems.20
When examining health care organizations, Bradley et al. note that steps to execute a PD approach include 1) identifying “positive deviants,” typically using quantitative data; 2) analyzing organizations using qualitative methods to generate hypotheses about practices that allow organizations to achieve top performances; 3) testing hypotheses in larger samples and 4) mobilizing various key stakeholders to implement and test the newly characterized “best practices.”21 This last step highlights how positive deviance is intended to engage its studied community. Participants have a stake in the research because their information is used to craft the best practices for everyday clinical care. It is important to note that in PD, quantitative performance measures are used to identify the extent of variation and through qualitative interviews among high performers, hypotheses are generated.
For the quantitative phase, performance measures must be easily accessible, valid and proven indicators of “success.”20 Examples in obstetrics include reducing or eliminating elective deliveries before 39 weeks gestation, reducing cesarean rates for low-risk first births and increasing the use of antenatal steroids in preterm births.22,23 To generate hypotheses in the qualitative phase, data collection often relies on open-ended interviews to understand organizational context, including group dynamics and norms of hospital culture. Data collection can also take the form of observations, focus groups or review of organizational documents.15 Interview and focus group data are usually tape-recorded and transcribed, so they can then be coded to produce specific responses. Responses are then reviewed to identify similarities and differences and compared to reveal how context influences variation. In PD and mixed-methods, the ultimate data “output” can take the form of patterns and themes, or emergent taxonomies, concepts and theories, in hopes of classifying the information into different bundles or domains to form a framework for the lessons learned.15 Moreover, sampling in positive deviance also requires a diverse set of subjects. Whereas quantitative studies generally rely on representative samples, qualitative work uses “purposive” samples. Positive deviance studies require conscious sampling of settings at the extremes, i. e., high performers and low performers, as greater contrast between high and low outliers will reveal more about what creates variation among a group of people or institutions.16
In mixed-methods, the qualitative work can precede the quantitative component, especially in formative phases of research identifying gaps of understanding and where there is a need for research. For example, in studying quality improvement, the qualitative component would be used to discover potential sources of errors and the quantitative component would seek to look at the frequency of errors.24 While qualitative research tends to be less generalizable, given its focus on a specific set of experiences and subjects, quantitative data can extend findings to a broader population. However, the dynamic between qualitative and quantitative does not need to be sequential and can consist of “embedding, integrating, connecting” the two methods within the study.25
Use of Positive Deviance in Other Fields of Medicine
Positive deviance has been used in numerous settings in medicine to improve quality and safety. Work by Krumholz and colleagues used a positive deviance approach to identify innovative strategies from “positive deviants” in health care, those organizations that were consistently high performers with regard to a specific outcome.17 Their work on improving care for patients with acute myocardial infarction ultimately sought to lessen the time interval from symptom onset to hospital arrival to primary percutaneous coronary intervention (PCI), known as “door-to-balloon time.” At the time, less than 50% of patients met the national target of a door-to-balloon time within 90 minutes.17 In their study, step one involved picking out positive deviants from the National Registry of Myocardial Infarction, those that had door-to-balloon time less than or equal to 90 minutes. Step two consisted of conducting in-depth interviews at these sites, with physicians, staff, different clinical departments and administrators. From these interviews, they recognized that senior management support, shared goals, physician leaders, interdisciplinary teams and data feedback were crucial in quick post-MI PCI time.17 They then tested their hypotheses quantitatively through web-based hospital surveys and were able to identify more specific hospital strategies that were linked to lower door-to-balloon times. For example, lower times were associated with activation of the catheterization laboratory by emergency medicine physicians instead of cardiologists and having real-time feedback on door-to-balloon times for catheterization laboratory and emergency department staff.16 These lessons were then disseminated to other hospitals, through a public campaign mobilized by a partnership between the research team and the American College of Cardiology. The results were promising: patients treated in hospitals participating in the campaign for at least three months were significantly more likely to have shorter PCI time intervals than patients treated in non-participating hospitals.17
Other applications of the PD approach include increasing post-MI beta blocker use, appropriate anticoagulation use within the VHA system, diabetes management in medical homes and improved vaccination, hand hygiene and clozapine use.26–31 These studies distill elements of organizational culture and hospital best practices that contribute to high performance, and, importantly, that might not have been considered before. For increasing beta-blocker uptake, goal agreement, administrative support, data feedback and leadership were features of the institutions that distinguished high from low performers.26 Increased clozapine use for treatment resistant schizophrenics was attributed to interdisciplinary teams and inclusion of non-physician staff as well as physician comfort with clozapine use.31 High flu vaccination rates in the Veterans Health Care System were attributed to leadership and collaboration.29 One particular theme that emerges from this review is the importance of less concrete, and thus less frequently quantified, attributes like data feedback and teamwork in guaranteeing quality care and patient safety. The positive deviance approach highlights the ways in which qualitative data can provide alternative answers to healthcare performance and patient satisfaction.
Benefits of Mixed-Methods such as Positive Deviance for Health Disparities Research
The use of mixed methods, such as PD, to address concerns of quality and safety in obstetrics may be beneficial and especially important in the setting of health disparities. The addition of qualitative methods to quantitative methods has the potential to center on the voice and experience of patients and provide context to quantitative findings that reveal disparities.32 Qualitative research, when carried out by culturally knowledgeable researchers who can communicate in plain language, is well suited to study underserved populations. The format of qualitative research, its interviews and text-based data, is an opportunity to reach and provide a platform to those that might otherwise be overlooked.17 While this is certainly true of individual interviews, focus groups are a particularly powerful resource in qualitative studies. In these settings, patients are given space, time and weight, in a way that might not otherwise be possible within the standard hierarchy of medical care. Informal details provided by patients on their daily lives and their challenges can inform the formal protocols and procedures that make up the healthcare system. Patients are especially useful for confirming whether what professionals believe are “patient-centered” approaches are being implemented and being experienced as desired. Moreover, qualitative research gives power to the experiences specific to the intersections of healthcare and race. In attempting to limit variation in a community and disseminate lessons learned from top performers, PD is a natural fit, to narrow the racial/ethnic disparities gap in maternal outcomes.
Qualitative and Quantitative Methods to Reduce Disparities and Narrow Variation in Obstetrics
Few studies in obstetrics have used mixed methods to address racial and ethnic disparities. However, both quantitative and qualitative research methods have been employed separately to assess disparities and to improve quality. Quantitative research methods have revealed the magnitude of racial/ethnic disparities in obstetrics. In an analysis of 25 hospitals over a 3-year period, Grobman et al, reported that performance measures in obstetric care varied greatly according to both race and ethnicity.33 Black and Hispanic women were almost twice as likely to experience severe postpartum hemorrhage and peripartum infection. Asian women were most likely to receive an episiotomy. These differences persisted despite controlling for hospital site of delivery and other patient characteristics.33 Reasons for these disparities were unclear; based on their quantitative data alone, Grobman et al. could not explain why Asian women had more episiotomies or why postpartum hemorrhage was less likely to occur in white women. Similarly, Creanga et al., in examining inter-hospital differences in 15 indicators of delivery quality, found that hospitals predominantly serving black women had poorer performance on 12 of the 15.34 While the study showed that patient populations differed, for example white-serving hospitals generally cared for older and wealthier women, the authors were unable to offer specific drivers for poorer outcomes in primarily black-serving hospitals.
Our team was able to use quantitative methods to measure the magnitude of disparities as well as to identify hospitals with high and low performance. Ultimately, our data suggests a need for improved care at hospitals that disproportionately serve black women. Using data from the Nationwide Inpatient Sample, we found that black women delivered in certain hospitals and that these hospitals had worse outcomes for both white and black women, regardless of patient risk factors.35 We ranked hospitals by the proportion of black women who delivered at each hospital and analyzed the risks of severe maternal morbidity for black and white women after adjusting for patient characteristics, comorbidities, hospital characteristics and within-hospital clustering.
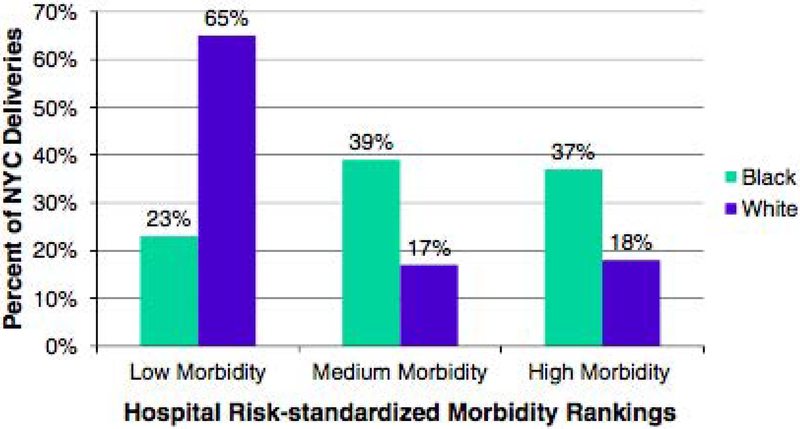
In New York City, after adjustment for patient case mix, we found seven-fold variation in severe maternal morbidity rates and that white women were more likely to be delivered in the low-morbidity hospitals: 65% of white versus 23% of black deliveries occurred in hospitals in the lowest tertile for morbidity (Figure 1).36 We estimated that black-white differences in delivery location may contribute as much as 47.7% of the racial disparity in severe maternal morbidity rates in New York City.36 In pediatrics, research by our team and others have also found that black very low-birth weight babies are more likely to be delivered in hospitals with higher risk-adjusted mortality37–39 and studies in other areas of medicine have demonstrated similar findings.40–42 Despite these glaring variations in outcomes, it is unclear what contributes to these disparities.
Figure 1.
Distribution of Black and White Deliveries at Black-serving Hospitals in US
Qualitative studies have been utilized to help us understand disparities and to elucidate the most important factors that lead to worse maternal outcomes. For example, one major qualitative study, which derived themes from text-based data from clinicians, built a descriptive model of provider and system related preventability of severe maternal outcomes. The study examined a tertiary care center in Chicago, one that predominantly served black and Hispanic mothers.43 Thematic categories for preventability included assessment and point of entry to care; diagnosis/recognition of high-risk conditions; and policies and procedures (lab results, oversight of others, scheduling and assessment, emergency preparedness, patient education). In the end, inadequate diagnosis/recognition of high-risk cases and inappropriate treatment were the most commonly reported reasons for preventable deaths.43 These findings were echoed in a larger current national study conducted by the CDC of maternal deaths across nine states in the United States that asked clinicians to describe contributing factors in open-ended responses. The CDC found that these deaths were related to clinician, facility and system factors, such as inadequate training, missed or delayed diagnosis of complications, poor communication and lack of coordination between clinicians.44
Qualitative studies have been broadly used in the quality and safety literature. For example, lack of coordination between clinicians, staff and patients is well documented. In an attempt to understand specific barriers to communication, one study used focus groups with obstetricians, anesthesiologists, nurses and pharmacists.45 Findings were concrete and actionable. For example, focus groups highlighted technical difficulties in communicating with services not located in or near labor and delivery, like the pharmacy and lab, as well as a lack of specific clinician “ownership” of a given patient, due to the large and diverse care team. From this qualitative data, improvement projects were developed. Shorter-term projects on increasing inter-departmental coordination like standardizing hand-off processes within the ED were completed and long-term initiatives to develop team-training courses on teamwork and culture were developed. Another study examined factors that contributed to failures in intrapartum safety by conducting qualitative surveys among members of ACOG, American College of Nurse-Midwives and other professional organizations.46 Free-text responses from physicians, midwives and nurses were collected and coded. Identified subthemes during moments of conflict included “perceived imperviousness” and “inaction” and “resignation.”46 Clinicians felt that their concerns were overlooked or that they were unable to speak up to individuals at the center of the conflict, despite the fact that it might undermine patient safety. Thus, qualitative studies can point to why disparities exist, including challenges in effective communication and teamwork on labor and delivery floors.
While clinician perspectives can provide new perspectives on safety gaps, patient experiences, as expressed in focus groups or interviews, can reveal different kinds of barriers to quality care that lead to variations in maternal outcomes. There is a growing recognition that the postpartum period is a critical interval to address the medical and emotional needs of mothers. However, rates of postpartum visits are low - 16–36 % of women do not attend the 6-week follow-up visit.47A retrospective study attempting to understand factors in postpartum attendance identified having Medicaid and being Hispanic as predictors of non-attendance.47 Treatment for postpartum depression is also low among low-income women of color. White women were twice as likely to start treatment and therapy after a diagnosis of depression than Black and Latina women, even though severity and onset were similar across the various racial groups.48 While quantitative studies can track postpartum uptake of mental health services, they are unable to tell us why there is an underutilization of services. Patient and clinician focus groups on postpartum care disclosed three themes about the postpartum period: women felt unprepared for the postpartum period, there was no coordinated care for mothers during the postpartum period and there was a “disconnect” between clinicians and mothers about what was most important to know and do during this period.49 Other research investigating postpartum depression suggests that clinicians should consider patients’ cultural and social context when negotiating treatment decisions for depression.51 Low-income mothers belonging to a racial/ethnic minority tended to normalize their depressive symptoms and were further discouraged from seeking help because they perceived mental health services as cold and apathetic.51
Qualitative studies have also been able to clarify why postpartum care is inadequate in managing comorbid conditions identified during pregnancy, like hypertension and obesity, which are of particular concern for women of color.13,52 In one study, Hispanic women cited financial barriers to care, emphasizing that the cost of an uninsured checkup outweighs concerns about their health or glycemic control.53 Another study revealed the tenuous connection in the minds of many mothers between gestational diabetes and development of type 2 Diabetes. Thus, they often minimized the severity of their diagnosis, even though 70% of women with gestational diabetes will develop Type 2 diabetes.54,55 Given the host of factors that might influence postpartum care, initiatives to increase participation must center around patients’ experiences, beliefs and knowledge, which are far more likely to emerge in qualitative research.
More qualitative research is also needed to understand what prevents many women from racial/ethnic groups from seeking prenatal care. Quantitative data estimates later or no care to be more than twice as frequent among Black and Native American women versus white women.56 Studies have identified quantifiable risk factors for inadequate prenatal care, citing insurance status, social support, age, education and marital status.56 However, little is known about what prevents women from racial/ethnic minority groups from seeking the care they need. The importance of considering the patient experience became apparent in one study on the determinants of prenatal care among a group of 24 mothers. Interviews revealed mothers did not have reliable information about the importance of well-timed prenatal care and thus delayed seeking prenatal care.57 In trying to identify the barriers to antenatal care in another study, three themes distilled from focus groups with black women were structural barriers, psychological stress, attitudes and perceptions. Specific structural barriers cited by these women included lack of insurance, transportation difficulties, inflexible clinic hours and psychosocial stress growing out of lack of social support.58 While quantitative research often collects data about insurance status, in interviews with mothers on Medicaid more specifics emerge, such as the technical challenges of obtaining insurance cards and long queues at the medical assistance office. Women also reported difficulties with obtaining Medicaid coverage, finding a physician that accepted their care plan and using Medicaid covered transportation to and from prenatal care visits.58 These contextual details provide starting points for quality improvement activities and re-frame our understanding of what makes or breaks participation in maternal health care. Attitudes and perceptions revealed that discrimination and poor quality of prenatal care swayed women to limit their visits.58 Discrimination was rarely overt, but body language and demeanor often clued in patients about clinician bias. Poor quality of care often involved shorter visits and predominantly yes and no questions for these mothers during their visits. On the other hand, positive experiences around prenatal care included personable follow-up calls and increased time with providers.58
Next Steps: The Use of Positive Deviance/Mixed Methods in Disparities Research
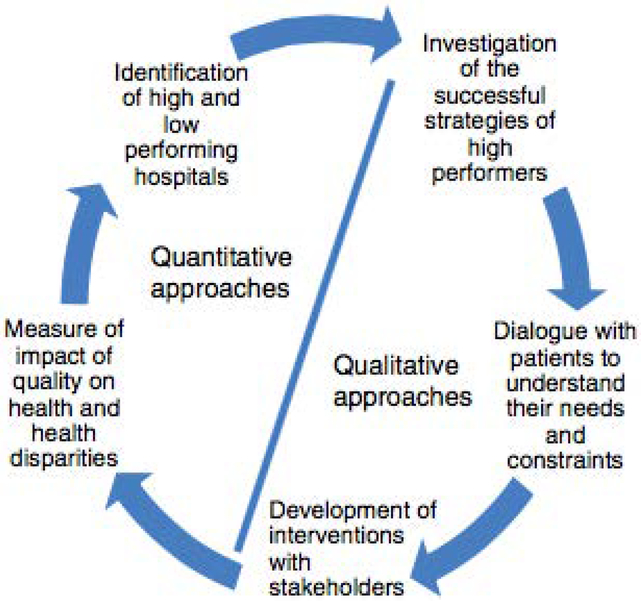
While quantitative and qualitative methods have been used separately in obstetrics to point to disparities in quality and safety, there has been little use of positive deviance or mixed-methods to understand disparities and the contribution of quality of care to creating disparities. We believe integrating these two methods has the potential to provide new perspectives to address maternal morbidity and to narrow racial/ethnic disparity gaps, as shown in research from other areas using the PD framework. As illustrated schematically in Figure 2, the first step is to identify the “positive deviants,” i.e., organizations that consistently demonstrate exceptionally high performance in an area of interest.21 In the setting of disparities, it can be helpful to identify hospitals or healthcare organizations that demonstrate high performance on a particular quality metric and that do not demonstrate poorer performance for women from racial and ethnic backgrounds. Reviewing quality metrics stratified by race and ethnicity is an important step in identifying top performers. If the target is to reduce racial and ethnic disparities then we have to identify high performers across racial and ethnic groups. The second step is to study high performing organizations in-depth, using qualitative methods to generate hypotheses about practices that allow organizations to achieve top performance for all racial and ethnic groups. Qualitative interviews are crucial. Performing interviews with different hospital staff, clinicians and patients will help identify root causes of variation and refine best practices. Open-ended questions about disparities in care, bias and the strategies and policies utilized to ensure high quality for all patients will also be important to discuss. Conducting focus groups and interviews with patients will be invaluable to gain an understanding of their needs, especially listening to mothers, families and larger communities as they speak about their experiences.
Figure 2.
Proposed Research Cycle for Integrating Quantitative and Qualitative Investigations of Obstetrical Quality
Once the research team identifies the best practices (e.g. strong leadership, communication and coordination, unconscious bias training) that appear to be associated with high quality care for all patients, they can work in partnership with key stakeholders to develop interventions based on evidence about the newly characterized best practices. Rallying key stakeholders allows for large implementation of multidisciplinary initiatives to tackle racial disparities. Next, the team can measure the impact on health and health disparities of the newly designed interventions. A novel example of mobilizing key stakeholders is an effort to improve maternal outcomes in California. The California Department of Health and the California Maternal Quality Care Collaborative, created a strong public-private partnership whose actions led to reducing maternal deaths by one-half (from 13.1 to 7.2 for every 100,000 live births).59
Narrowing the racial/ethnic disparities gap in maternal health requires quality improvement measures grounded in health equity. From research, we know that the burden of death and disease falls disproportionately on women belonging to racial/ethnic minorities and that a majority of maternal mortality and severe maternal morbidity cases are preventable. We also know that regular use of protocols and procedures can ensure better outcomes for mothers and that checklists and toolkits can improve care provided by clinicians and staff. Nevertheless, there can often be a disconnect between theory and practice, between the message of research conclusions and actual implementation of those conclusions. Indeed, variations across hospitals persist but drivers of racial and ethnic disparities remain unknown. Positive deviance offers an alternative framework to address and understand our failings, ultimately to improve quality of care and patient safety in obstetrics. This approach has been used successfully in other disciplines and it can be a useful tool in obstetrics to reduce disparities and ensure healthy outcomes for all mothers and children.
Funding:
Supported by the National Institute on Minority Health and Health Disparities (R01MD007651), the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health (R01HD078565) and the Blavatnik Family Foundation. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References:
- 1.Papanicolas I, Woskie LR, Jha AK. Health Care Spending in the United States and Other High-Income Countries. JAMA. 2018;319(10):1024–1039. [DOI] [PubMed] [Google Scholar]
- 2.Howell EA, Egorova N, Balbierz A, et al. Black-white differences in severe maternal morbidity and site of care. American Journal of Obstetrics and Gynecology. 2016; 214(1): 122.e1–122.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Howell EA, Egorova NN, Janevic T, Balbierz A, Zeitlin J, Hebert PL. Severe Maternal Morbidity Among Hispanic Women in New York City: Investigation of Health Disparities. Obstet Gynecol. 2017;129(2):285–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Creanga AA, Berg CJ, Syverson C, Seed K, Bruce FC, Callaghan WM. Race, ethnicity, and nativity differentials in pregnancy-related mortality in the United States: 1993–2006. Obstet Gynecol. 2012. August;120(2 Pt 1):261–8. [DOI] [PubMed] [Google Scholar]
- 5.Howell EA, Zeitlin J. Quality of Care and Disparities in Obstetrics. Obstet Gynecol Clin North Am. 2017;44(1):13–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.New York City Department of Health and Mental Hygiene. Pregnancy-Associated Mortality: New York City, 2006–2010; 2015. [Google Scholar]
- 7.Institute of Medicine (IOM). 2001. Crossing the Quality Chasm Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, D.C: National Academy Press. [Google Scholar]
- 8.Lohr K Committee to Design a Strategy for Quality Review and Assurance in Medicare, editor Medicare: a strategy for quality assurance. Vol. 1 Washington, DC: IOM, National Academy Press; 1990. [Google Scholar]
- 9.Kozhimannil KB, Law MR, Virnig BA. Cesarean delivery rates vary tenfold among US hospitals; reducing variation may address quality and cost issues. Health Aff (Millwood) 2013; 32(3): 527–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Balit JL, Grobman WA, Rice MM, et al. Risk adjusted models for adverse obstetric outcomes and variation in risk-adjusted outcomes across hospitals. Am J Obstet Gynecol 2013; 209(5): 446. e1–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grobman WA, Balit JL, Rice MM, et al. Can differences in obstetrics outcomes be explained by differences in the care provided? The MFMU Network APEX Study. Am J Obstet Gynecol 2014; 211(2); 147. e1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Braveman P What are health disparities and health equity? We need to be clear. Public Health Rep. Jan-Feb 2014;129 Suppl 2:5–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Howell EA. Reducing Disparities in Severe Maternal Morbidity and Mortality. Symposium on Maternal Mortality and Severe Maternal Morbidity. Clin Obstet Gynecol. 2018. January 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.U.S. Department of Health and Human Services. The Secretary’s Advisory Committee on National Health Promotion and Disease Prevention Objectives for 2020. Phase I report: Recommendations for the framework and format of Healthy People 2020. Available at: https://www.healthypeople.gov/sites/default/files/PhaseI_0.pdf (Accessed Dec 25 2018).
- 15.Curry LA, Nembhard IM, Bradley EH. Qualitative and Mixed Methods Provide Unique Contributions to Outcomes Research. Circulation 2009;119:1442–1452. [DOI] [PubMed] [Google Scholar]
- 16.Rose AJ, McCullough MB. A Practical Guide to Using the Positive Deviance Method in Health Services Research. 2017. (52):3 1207–1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Krumholz HM, Curry LA, Bradley EH. Survival after acute myocardial infarction (SAMI) study: the design and implementation of a positive deviance study. Am Heart J. 2011;162(6):981–987.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Positive Deviance Initiative: Projects [http://www.positivedeviance.org/projects/]
- 19.Guldan GS, Zeitlin MF, Beiser AS, Super CM, Gershoff SN, Datta S. Maternal education and child feeding practices in rural Bangladesh. Soc Sci Med. 1993;36(7):925–935. [DOI] [PubMed] [Google Scholar]
- 20.Marsh DR, Schroeder DG, Dearden KA, Sternin J, Sternin M. The power of positive deviance. BMJ. 2004;329(7475):1177–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bradley et al. Research in action: using positive deviance to improve quality of health care. Implementation Science. 2009. (4):25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.National Quality Forum. [Accessed Jan 16, 2019];NQF Endorses Perinatal Measures. 2012. http://www.qualityforum.org/News_And_Resources/Press_Releases/2012/NQF_Endorses_Perinatal_Measures.aspx.
- 23.The Joint Commission. [Accessed Jan 16, 2019]; Specifications Manual for Joint Commission National Quality Measures (v2016A) 2016. https://manual.jointcommission.org/releases/TJC2016A/.
- 24.Curry et al. Mixed Methods in Biomedical and Health Services Research. Circulation: Cardiovascular Quality and Outcomes. 2013;6:119–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fetters MD, Curry LA, Creswell JW. Achieving integration in mixed methods designs-principles and practices. Health Serv Res. 2013;48(6 Pt 2):2134–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bradley EH, Holmboe ES, Mattera JA, Roumanis SA, Radford MJ, Krumholz HM. A qualitative study of increasing beta-blocker use after myocardial infarction: Why do some hospitals succeed? JAMA. May 23–30 2001;285(20):2604–2611. [DOI] [PubMed] [Google Scholar]
- 27.Rose AJ, Petrakis BA et al. “Organizational Characteristics of High- and Low-Performing Anticoagulation Clinics in the Veterans Health Administration.” Health Services Research. 2012. 47 (4): 1541–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gabbay RA, Friedberg MW, Miller-Day M, Cronholm PF, Adelman A, Schneider EC. A positive deviance approach to understanding key features to improving diabetes care in the medical home. Ann Fam Med. 2013;11 Suppl 1(Suppl 1):S99–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Razouki Z, Knighton T, Martinello RA, et al. Organizational factors associated with Health Care Provider (HCP) influenza campaigns in the Veterans health care system: a qualitative study. BMC Health Serv Res. 2016;16:211 Published 2016 Jul 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Marra AR, Guastelli LR, de Araújo CM, dos Santos JL, Lamblet LC, Silva M Jr, de Lima G, Cal RG, Paes AT, Cendoroglo Neto M, Barbosa L, Edmond MB, dos Santos OF. Positive deviance: a new strategy for improving hand hygiene compliance. Infect Control Hosp Epidemiol. 2010. January; 31(1):12–20. [DOI] [PubMed] [Google Scholar]
- 31.Gören JL et al. Organizational Characteristics of Veterans Affairs Clinics With High and Low Utilization of Clozapine. Psychiatr Serv. 2016. November 1;67(11):1189–1196. Epub 2016 Jun 15. [DOI] [PubMed] [Google Scholar]
- 32.O’Hara JK, Grasic K, Gutacker N, et al. Identifying positive deviants in healthcare quality and safety: a mixed methods study. J R Soc Med. 2018;111(8):276–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Grobman WA, Bailit JL, Rice MM, et al. Racial and ethnic disparities in maternal morbidity and obstetric care. Obstet Gynecol. 2015;125(6):1460–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Creanga AA, Bateman BT, Mhyre JM, Kuklina E, Shilkrut A, Callaghan WM. Within hospital differences: Performance of racial and ethnic minority- serving hospitals on delivery-related indicators. Am J Obstet Gynecol. 2014. December; 211(6): 647.e1–16. [DOI] [PubMed] [Google Scholar]
- 35.Howell EA, Egorova N, Balbierz A, Zeitlin J, Hebert PL. Black-white differences in severe maternal morbidity and site of care. Am J Obstet Gynecol. 2015;214(1):122.e1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Howell EA, Egorova NN, Balbierz A, Zeitlin J, Hebert PL. Site of delivery contribution to black-white severe maternal morbidity disparity. Am J Obstet Gynecol. 2016;215(2):143–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Howell EA, Hebert P, Chatterjee S, Kleinman LC, Chassin MR. Black/white differences in very low birth weight neonatal mortality rates among New York City hospitals. Pediatrics. 2008. March;121(3):e407–415. [DOI] [PubMed] [Google Scholar]
- 38.Howell EA, Janevic T, Hebert PL, Egorova NN, Balbierz A, Zeitlin J. Differences in Morbidity and Mortality Rates in Black, White, and Hispanic Very Preterm Infants Among New York City Hospitals. JAMA Pediatr. March 1 2018;172(3):269–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Profit J, Gould JB, Bennett M, et al. Racial/Ethnic Disparity in NICU Quality of Care Delivery. Pediatrics. September 2017;140(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cheng EM, Keyhani S, Ofner S, et al. Lower use of carotid artery imaging at minority-serving hospitals. Neurology. 2012. July 10;79(2):138–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Barnato AE, Lucas FL, Staiger D, Wennberg DE, Chandra A. Hospital-level racial disparities in acute myocardial infarction treatment and outcomes. Med Care. 2005. April;43(4):308–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bach PB, Pham HH, Schrag D, Tate RC, Hargraves JL. Primary care physicians who treat blacks and whites. N Engl J Med. 2004. August 5;351(6):575–584 [DOI] [PubMed] [Google Scholar]
- 43.System Geller S, Cox S, and Kilpatrick S A descriptive model of preventability in maternal morbidity and mortality. Journal of Perinatology, 2006. 26 (2): p. 79. [DOI] [PubMed] [Google Scholar]
- 44.Building U.S. Capacity to Review and Prevent Maternal Deaths. (2018). Report from nine maternal mortality review committees. Retrieved from http://reviewtoaction.org/Report_from_Nine_MMRCs.
- 45.Grobman et al. Perspectives on communication in labor and delivery: a focus group analysis. Journal of Perinatalogy, 2011. April;31(4):240–5. [DOI] [PubMed] [Google Scholar]
- 46.Lyndon A, Zlatnik MG, Maxfield DG, Lewis A, McMillan C, Kennedy HP. Contributions of clinical disconnections and unresolved conflict to failures in intrapartum safety. J Obstet Gynecol Neonatal Nurs. 2013;43(1):2–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wilcox A, Levi EE & Garrett JM Predictors of Non-Attendance to the Postpartum Follow-up Visit. Maternal Child Health Journal, 2016. 20(Suppl 1): 22. [DOI] [PubMed] [Google Scholar]
- 48.Kozhimannil KB, Trinacty CM, Busch AB, Huskamp HA, Adams AS. Racial and ethnic disparities in postpartum depression care among low-income women. Psychiatr Serv. 2011;62(6):619–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Martin A, Horowitz C, Balbierz A, Howell EA. Views of women and clinicians on postpartum preparation and recovery. Matern Child Health J. 2014;18(3):707–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Negron R, Martin A, Almog M, Balbierz A, Howell EA. Social support during the postpartum period: mothers’ views on needs, expectations, and mobilization of support. Matern Child Health J. 2013;17(4):616–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Abrams LS, Dornig K, Curran L. Barriers to Service Use for Postpartum Depression Symptoms Among Low-Income Ethnic Minority Mothers in the United States. Qualitative Health Research.2009. April;19(4):535–51. [DOI] [PubMed] [Google Scholar]
- 52.Cheng C, Fowles E, Walker L. Postpartum Maternal Health Care in the United States: A Critical Review. J Perinat Educ. 2006. Summer; 15(3): 34–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Collier SA. A qualitative study of perceived barriers to management of diabetes among women with a history of diabetes during pregnancy. J Womens Health (Larchmt). 2011. September;20(9):1333–9. [DOI] [PubMed] [Google Scholar]
- 54.Tang JW et al. Perspectives on prevention of type 2 diabetes after gestational diabetes: a qualitative study of Hispanic, African-American and White women. Matern Child Health J. 2015. July;19(7):1526–34. [DOI] [PubMed] [Google Scholar]
- 55.Yee LM et al. “Using a Patient Navigator to Improve Postpartum Care in an Urban Women’s Health Clinic.” Obstet Gynecol. 2017. May;129(5):925–933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gadson A Exploring the social determinants of racial/ethnic disparities in prenatal care utilization and maternal outcome. Seminars in perinatology. 2017; 41(5). 308–317. [DOI] [PubMed] [Google Scholar]
- 57.Meyer E Working Towards Safe Motherhood: Delays and Barriers to Prenatal Care for Women in Rural and Peri-Urban Areas of Georgia. Matern Child Health J. 2016. July;20(7):1358–65. [DOI] [PubMed] [Google Scholar]
- 58.Mazul MC, Salm Ward TC & Ngui EMJ Anatomy of Good Prenatal Care: Perspectives of Low Income African-American Women on Barriers and Facilitators to Prenatal Care. Racial and Ethnic Health Disparities (2017) 4: 79. [DOI] [PubMed] [Google Scholar]
- 59.Main EK, Markhow C, Gould J, Addressing Maternal Mortality And Morbidity In California Through Public-Private Partnerships. Health Affairs 2018. (37):9, 1484–1493. [DOI] [PubMed] [Google Scholar]