Abstract
Peripherally inserted central catheters (PICCs), a form of central venous catheter (CVC) inserted into the cephalic or basilic veins, are most commonly used for administration of long-term antibiotics or for total parenteral nutrition. PICCs are associated with fewer complications than traditional CVCs; however, they have been implicated in accidental malpositioning, leading to both atrial and ventricular arrhythmias. We present a case of atrial fibrillation possibly triggered by migration of the tip of the PICC deep into the right atrium. Retraction of the tip resulted in resolution of the arrhythmia.
Keywords: Atrial fibrillation, central venous catheter, iatrogenic arrhythmias, peripherally inserted central catheters
Peripherally inserted central catheters (PICCs) are traditionally inserted into the cephalic or basilic veins, with the terminal end draining ideally at the junction between the superior vena cava and right atrium.1 Central venous catheters (CVCs) are associated with several complications, such as malpositioning, thrombophlebitis, and catheter-associated bloodstream infections.1 Cardiac arrhythmias secondary to CVC placement are relatively common2; however, they have seldom been described after PICC placement. We present a case of atrial fibrillation (AF) related to malpositioning of the tip of the PICC.
CASE STUDY
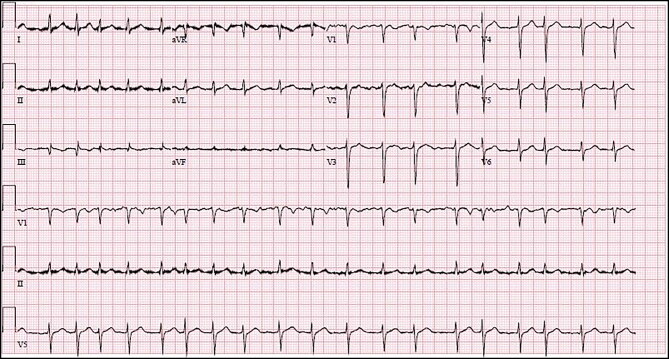
A 45-year-old black man with hypertension diagnosed during the hospital stay was admitted for community-acquired pneumonia complicated by loculated empyema thoracis. He underwent video-assisted thoracoscopic surgery for drainage of empyema and thoracic decortication. This was complicated by respiratory failure requiring ventilator support. During the course of the hospitalization, the patient’s condition necessitated PICC placement. The port of entry was the right basilic vein, and the distal end terminated at the junction between the superior vena cava and right atrium, as confirmed by chest radiography. The PICC was stabilized at the port of entry by a StatLock stabilization device. The patient then developed new-onset rapid AF right after placement (Figure 1). His vital signs during the onset of AF were a heart rate of 147 beats/min and blood pressure of 137/71 mm Hg; he had 99% oxygen saturation on 60% fraction of inspired oxygen on the ventilator. His heart rate ranged in the 130s to 150s thereafter. Examination revealed normal breath sounds, irregular rhythm, and tachycardia. His laboratory parameters including thyroid-stimulating hormone levels were within normal limits.
Figure 1.
Electrocardiogram demonstrating atrial fibrillation.
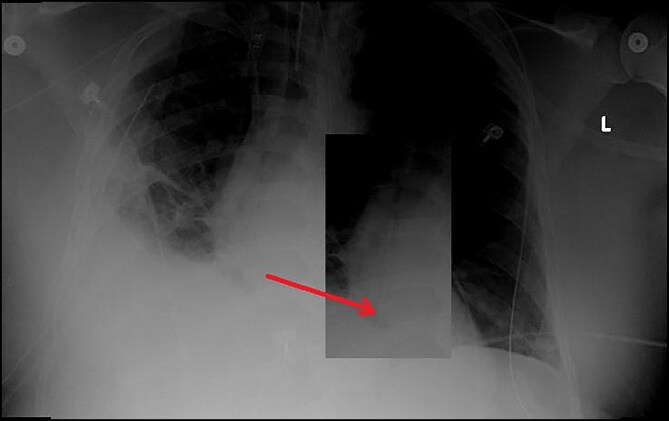
He was started on a diltiazem infusion to achieve ventricular rate control. Echocardiography revealed a normal ejection fraction with normal right atrial and left atrial sizes. His CHA2DS2-VASc score was 1. Cardiology advised against any anticoagulation. The patient was continued on a diltiazem infusion to achieve ventricular rate control. A repeat chest radiograph showed the displacement of the PICC deep into the right atrium (Figure 2). The PICC was initially retracted by 5 cm, but manipulating the PICC resulted in a repeat episode of rapid AF, necessitating an increase in the rate of the diltiazem infusion. The tip of the catheter was withdrawn by another 3 cm and the AF resolved within 2 hours. The diltiazem infusion was stopped. During the subsequent year of follow-up, there was no recurrence of AF.
Figure 2.
Chest radiograph demonstrating the migration of the tip of the peripherally inserted central catheter deep into the right atrium.
DISCUSSION
Peripherally inserted central catheters are placed by specialized nursing staff or interventional radiology; they are long and flexible, commonly made of nonthrombogenic material like silicone or polyurethane,3 and inserted into the cephalic vein, basilic veins, or brachial vein using an ultrasound-guided antecubital insertion technique, with the patient’s arm abducted to 90° from the body and the head turned toward the ipsilateral side. This positioning is particularly useful to straighten the curve in the subclavian vein and decrease the angle between the subclavian and internal jugular veins.4 The PICC courses along the subclavian vein to terminate at the junction of the superior vena cava and right atrium, with the optimal position being the distal third of the superior vena cava. The right tracheobronchial angle is the best landmark to identify the cavoatrial junction.4 A postprocedural chest radiograph is often obtained to confirm the placement. Fluoroscopy and transesophageal echocardiogram are other methods to confirm the placement.5
PICCs are associated with complications such as deep venous thrombosis and catheter-associated bloodstream infections.6 Malpositioning is also common, but malpositioning leading to arrhythmias is seldom reported. Improper placement to begin with and postpositional migration7 are some of the ways in which a PICC can cause arrhythmias. Mechanical stimulation of the heart musculature is the main reason for the induction of arrhythmias.
Because of their long and flexible nature, PICCs are more prone to be malpositioned. These catheters are placed with the arm in the abducted position, and hand movements like flexion and adduction can cause displacement of the tip about 2 to 3.3 cm.8 Malpositioning can also lead to advancement of the PICC to a maximum of 9.5 cm.9 Changing from a supine to erect position can cause cephalad migration of the catheter tip, dislodging it into the right atrium. Sometimes, PICCs may even advance deep into the right ventricle, leading to ventricular tachycardias.9 Traditionally, Tegaderm and GripLock tape are used to secure the PICC in position. Some centers use a tracking and tip confirmation system, which minimizes complications,10 and others use StatLock stabilization devices to keep the PICC in position.8
The resolution of arrhythmia after repositioning the device, the absence of structural heart disease, and the absence of any cardiovascular risk factors in our patient suggest that AF was induced by PICC migration. The tip of the PICC was initially at the junction of the superior vena cava and right atrium, and a StatLock device was used to hold it in position. We hypothesize that the tip migrated deep into the right atrium—almost into the right ventricle—due to positional change when the patient was rolled to his side by nursing staff. This probably led to the onset of rapid AF. Once the tip was retracted by 8 cm, the AF resolved.
References
- 1.Pikwer A, Åkeson J, Lindgren S. Complications associated with peripheral or central routes for central venous cannulation. Anaesthesia. 2012;67:65–71. doi: 10.1111/j.1365-2044.2011.06911.x. [DOI] [PubMed] [Google Scholar]
- 2.Stuart RK, Shikora SA, Akerman P, et al. Incidence of arrhythmia with central venous catheter insertion and exchange. JPEN J Parenter Enteral Nutr. 1990;14:152–155. doi: 10.1177/0148607190014002152. [DOI] [PubMed] [Google Scholar]
- 3.Seckold T, Walker S, Dwyer T. A comparison of silicone and polyurethane PICC lines and postinsertion complication rates: a systematic review. J Vasc Access. 2015;16:167–177. doi: 10.5301/jva.5000330. [DOI] [PubMed] [Google Scholar]
- 4.Vesely TM. Central venous catheter tip position: a continuing controversy. J Vasc Interv Radiol. 2003;14:527–534. doi: 10.1097/01.RVI.0000071097.76348.72. [DOI] [PubMed] [Google Scholar]
- 5.Gapp J, Krishnan M, Ratnaraj F, et al. Cardiac arrhythmias resulting from a peripherally inserted central catheter: two cases and a review of the literature. Cureus. 2017;9:e1308. doi: 10.7759/cureus.1308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Johansson E, Hammarskjöld F, Lundberg D, et al. Advantages and disadvantages of peripherally inserted central venous catheters (PICC) compared to other central venous lines: a systematic review of the literature. Acta Oncol. 2013;52:886–892. doi: 10.3109/0284186X.2013.773072. [DOI] [PubMed] [Google Scholar]
- 7.Haygood TM, Malhotra K, Ng C, et al. Migration of central lines from the superior vena cava to the azygous vein. Clin Radiol. 2012;67:49–54. doi: 10.1016/j.crad.2011.05.011. [DOI] [PubMed] [Google Scholar]
- 8.Waterhouse J, Bandisode V, Brandon D, et al. Evaluation of the use of a stabilization device to improve the quality of care in patients with peripherally inserted central catheters. AACN Adv Crit Care. 2014;25:213–220. doi: 10.1097/NCI.0000000000000026. [DOI] [PubMed] [Google Scholar]
- 9.Kalso E, Rosenberg PH, Vuorialho M, et al. How much do arm movements displace cubital central venous catheters? Acta Anaesthesiol Scand. 1982;26:354–356. doi: 10.1111/j.1399-6576.1982.tb01781.x. [DOI] [PubMed] [Google Scholar]
- 10.Bidgood C. Improving the patient experience with real-time PICC placement confirmation. Br J Nurs. 2016;25:539–543. doi: 10.12968/bjon.2016.25.10.539. [DOI] [PubMed] [Google Scholar]