Abstract
Objective:
To examine the effect of long-term violent victimization from late adolescence to the mid-thirties, on posttraumatic stress disorder (PTSD) and comorbid psychiatric disorders in later adulthood among urban African Americans and Puerto Ricans.
Methods:
Data were collected from a large urban community sample (N=674) at four time points associated with mean ages of 19, 24, 29, and 36 years. Trajectories of violent victimization were extracted using growth mixture modeling and used to predict psychiatric disorders and comorbidities in adulthood.
Results:
The sample was 52.8% African American and 47.2% Puerto Rican with 60% females. Three trajectory groups of violent victimization were identified: high, intermediate, and low. Over half of the sample reported relatively high and intermediate level violent victimization experiences from adolescence to adulthood. Group comparisons showed that participants belonging to the relatively high victimization group had greater odds of having PTSD, major depressive episode (MDE), and substance use disorder (SUD) separately, as well as comorbid PTSD-SUD and PTSD-MDE, as compared to those classified as having relatively low levels of victimization. Having intermediate level victimization experiences, compared to low level victimization experiences over time was associated with higher odds of PTSD and MDE separately, and comorbid PTSD-MDE.
Conclusions:
Long-term exposure to relatively high levels of violent victimization during emerging and young adulthood is associated with PTSD and comorbid psychiatric disorders in the thirties. Social, structural and interpersonal factors underlying the differential patterns of violent victimization in urban African American and LatinX youth need to be identified to adequately inform prevention efforts.
Keywords: violent victimization, PTSD, psychological comorbidity, longitudinal studies
Introduction
Exposure to traumatic events is not random. Neighborhood characteristics can contribute to increased exposure to and experiences of violence (Breslau et al., 1998a; Spikes, Willis, & Koenig, 2010). In fact, adolescents and young adults of color who live in structurally and economically disadvantaged urban neighborhoods are at higher risk of experiencing traumatic events, including violent victimization, compared to their White counterparts (Breslau et al., 1998b; Madero-Hernandez & Fisher, 2017; E. L. Smith, Cooper, States., & Bureau of Justice Statistics, 2013; Spikes et al., 2010; Truman, Langton, & Planty, 2013; Wilson, 1987). Violent victimization can refer to experiences of assault such as being badly beaten up, or violent and aggravated offenses, such as homicide (Breslau et al., 1998b; Morgan & Truman, 2018). According to the U.S. Bureau of Justice Statistics, in 2015, the homicide rate for African Americans was 8 times greater than the rate for Whites (Centers for Disease Control, 2017). Furthermore, among the three largest racial and ethnic groups in the United States, Blacks1 and Hispanics2 report higher rates of serious violent victimization than Whites; on average 22% and 32% higher, respectively, between 2015 and 2017 (Morgan & Truman, 2018). With regard to gender, men typically experience higher rates of violent victimization than women for all types of violent crime, except rape and sexual assault (Truman et al., 2013).
Experiences of violent victimization can contribute to psychiatric problems, including posttraumatic stress (Boney-McCoy & Finkelhor, 1995; Elklit, 2002; Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995; Kilpatrick et al., 2003a). Posttraumatic stress is often triggered by experiencing or witnessing traumatic event(s) that overwhelm a person’s capacity to cope with the trauma (American Psychiatric Association, 2013). This can include events related to natural disasters, serious accidents, terrorist acts, rape, or other violent assaults. Typically, these traumatic events are unanticipated, uncontrollable, and are characterized by a sense of horror, helplessness, and threat of injury or death (American Psychiatric Association, 2013). Previous research has found that traumatic events related to violent victimization are more likely to be associated with posttraumatic stress, including posttraumatic stress disorder (PTSD), than other traumatic events, especially non-interpersonal traumas such as natural disasters (Amstadter, McCart, & Ruggiero, 2007; Kessler et al., 1995; McCutcheon et al., 2010; Resnick, Kilpatrick, Dansky, Saunders, & Best, 1993). Violent victimization thus increases the risk of PTSD, compared to other types of trauma (Resnick et al., 1993). Since African Americans and LatinX populations have a higher likelihood of experiencing violence due to social and structural factors (e.g. poor neighborhood conditions), they are at high risk for PTSD associated with violent victimization (Crouch, Hanson, Saunders, Kilpatrick, & Resnick, 2000; Schwartz, Bradley, Sexton, Sherry, & Ressler, 2005; Xie, Heimer, Lynch, & Planty, 2018).
Most research examining victimization in conjunction with PTSD focuses on a single exposure to trauma or victimization (Elklit, 2002; Kilpatrick et al., 2003; Resnick et al., 1993). However, many adults maintain healthy and relatively stable levels of psychosocial functioning following a single exposure to crime or other stressful life event (Bonanno, 2004). Repeat victimization, or experiencing multiple traumatic events, heighten the likelihood of developing PTSD (Amstadter et al., 2007; Hedtke et al., 2008). Many urban, young adults of color - particularly those living in poor, disorganized neighborhoods - are victimized on more than one occasion and over the course of many years, and thus are at a higher risk for PTSD (Spikes et al., 2010; Weist, Acosta, & Youngstrom, 2001; Wilson, 1987). Few studies have explored the risk of PTSD among urban, young adults who repeatedly experience violent victimization in the U.S. For instance, one study that examined repeated exposure to victimization and its association with PTSD, as well as substance use and depression comorbidities, only included women (Hedtke et al., 2008). Other studies have examined similar psychopathologies, but are limited to childhood and adolescence and/or did not focus on urban populations (Barker, Arseneault, Brendgen, Fontaine, & Maughan, 2008; Biggs et al., 2010; Jennings, Higgins, Tewksbury, Gover, & Piquero, 2010; D. Smith & Ecob, 2007).
Violent victimization heightens not only the odds of suffering from PTSD, but also of PTSD comorbid with other trauma-related psychiatric disorders, such as substance use (Bremner, Southwick, Darnell, & al, 1997; Conway, Hu, Kim, & Bullon, 1994; Kilpatrick et al., 2003; Salzinger, Feldman, Stockhammer, & Hood, 2002) and depressive disorders (Bargai, Ben-Shakhar, & Shalev, 2007; Blanchard, Buckley, Hickling, & Taylor, 1998; Dixon, Howie, & Starling, 2005; Haden & Scarpa, 2008; Kilpatrick et al., 2003; Momartin, Silove, Manicavasagar, & Steel, 2004; Rytwinski, Scur, Feeny, & Youngstrom, 2013; Spikes et al., 2010; Vaughn et al., 2010). As Amstadter and colleagues state: “[…] chronicity of exposure leads to greater severity of symptoms and a more complex clinical picture” (2007). Indeed, Helzer and colleagues (1987) found that those meeting criteria for PTSD were more than twice as likely to have depressive disorders and drug use disorders than those without PTSD. Similarly, Cottler, Compton, Mager, Spitznagel, & Janca (1992) found that PTSD was more common among substance users than non-substance users in the general population. However, research on this topic among racial/ethnic minority groups is scarce, and there are no studies examining the link between repeated experiences of victimization and PTSD comorbid with substance use disorder (SUD) and major depressive episode (MDE). There is an apparent gap in the literature with regard to examining repeated exposure to violent victimization and its association with PTSD, comorbid with other psychiatric disorders, among urban communities of color living in poor neighborhood conditions. Examining these associations is particularly important, as this population is at significant risk for violent victimization and, consequently, PTSD and its comorbidities. Understanding and quantifying these associations is necessary to develop meaningful prevention policies and practices.
The current study provides a unique opportunity to explore violent victimization in a longitudinal sample of African Americans and mainland Puerto Ricans from urban communities. Study participants were followed from late adolescence (~19 years old) to adulthood (~36 years old) with four follow-up visits within this timeframe. Investigators were able to observe longitudinal trends of violent victimization over time and examine their associations with PTSD and comorbidities with other psychiatric disorders. Our questions were as follows:
-
(1)
What are the differential longitudinal trajectories of violent victimization among urban African Americans and Puerto Ricans?
-
(2)
Are there gender differences in trajectory group membership?
-
(3)
What are the associations between membership in trajectories of victimization and PTSD, SUD, and MDE, and PTSD co-morbid with SUD and MDE?
We hypothesized that men would be overrepresented in trajectories characterized by higher levels of victimization, while women would be overrepresented in trajectories with lower levels of victimization. We further hypothesized that individuals in trajectories characterized by higher rates of victimization over time would be at greater risk for PTSD, SUD, and MDE than those characterized by lower violent victimization rates. We also hypothesized that those in trajectories with higher rates of victimization would be at greater risk for PTSD comorbid with SUD and PTSD comorbid with MDE than those at lower rates of victimization.
Methods
The Institutional Review Board of the New York University School of Medicine approved the study’s procedures. A Certificate of Confidentiality was obtained from the National Institute on Drug Abuse. At T1 and T2, passive consent procedures were followed with the parents of minors, while adolescents provided assent. Informed consent was obtained from all participants who were 18 years or older.
Data source
The data for this research were drawn from the Harlem Longitudinal Development Study. The study follows a cohort of African American and Puerto Rican young adults who were first recruited from 11 high schools in the East Harlem neighborhood of New York City in 1990. Detailed descriptions of recruitment, consent, and study procedures, as well as retention strategies and attrition rates at baseline or time 1 (T1) can be found in Brook, Hamburg, Balka, & Wynn (1992) and Brook, Whiteman, Balka, & Hamburg (1992). To summarize, at T1, after passive consent (from parents) and assent (from adolescents) were obtained, surveys were administered in classrooms with no teachers present (T1; 1990; N=1332). Approximately 80% of students recruited at baseline completed the T1 survey (Brook, Whiteman, Balka, Win, & Gursen, 1997). At time 2 (T2; 1994 – 1996; N=1190), the participants were interviewed in person or by phone. At time 3 (T3; 2000 – 2001; N=662), participants were interviewed in person. At Time 4 (T4; 2004 – 2006) and Time 5 (T5; 2011 – 2013), data were collected via self-administered questionnaires that were mailed to participants’ home. Mean ages (years) and standard deviations (SD) at each timepoint are the following: T1 – 14.2 (1.3), T2 – 19.2 (1.5), T3 – 24.4 (1.3), T4 – 29.2 (1.3), and T5 – 35.9 (1.4). For this study, data from T2 through T5 were included in the analyses, as our measure of violent victimization was added to the research at T2. There were 674 participants in this study who participated at T5.
Measures
Violent victimization was assessed by four items asking about the participants’ experiences of victimization in the past five years, including (1) being threatened with a weapon, (2) being hit with a weapon or shot, (3) being cut/stabbed with a knife, and (4) being beaten up (Chavez & Oetting, 1994). The response options were (0) never; (1) once; (2) twice; (3) three or four times; and (4) five or more times. Cronbach’s α was 0.71, 0.73, 0.76, and 0.75, respectively, at T2, T3, T4, and T5.
PTSD at T5 was assessed using the Posttraumatic Stress Disorder Checklist – Specific version (PCL-S). The PCL is a 17-item self-report measure of PTSD symptoms that closely matches DSM-IV (Weathers, Frank; Litz, Brett; Herman, Debra S.; Keane, 1993). The PCL-S is a version of the scale that measures trauma symptoms in response to a specific incident. Respondents rate each item from (1) “not at all” to (5) “extremely” to indicate the degree to which they have been bothered by that particular symptom over the past month. Participants received a diagnosis of PTSD if (1) they answered ‘yes’ to the question “Have you ever experienced or witnessed or had to deal with an extremely stressful or traumatic event, that included actual or threatened death or serious injury (e.g., rape) to you or someone else,” (2) the summed score on questions 1–17 was greater than or equal to 44, and (3) they met the DSM-IVTR criteria as defined by endorsing at least one item from cluster B, three items from cluster C, and two items from cluster D (American Psychiatric Association, 2000; Kilpatrick et al., 2003).
In addition, the minimum score on the endorsed items fulfilling DSM-IV-TR criteria had to be four on items 1, 2, 9, 10, 12, and 15 and three on the remaining 11 items (Blanchard, Jones-Alexander, Buckley, & Forneris, 1996). The internal reliability of this measure was high (Cronbach’s α = 0.96).
SUD at T5 was assessed using the University of Michigan Composite International Diagnostic Interview (Wittchen & Kessler, 1994) which we adapted for consistency with the criteria used in DSM-IV-TR (American Psychiatric Association, 2000). Participants were classified as having a SUD if they met either the criteria of substance dependence or substance abuse; otherwise, they received a score of zero. The internal reliability of this measure was high (α = 0.90).
MDE at T5 was assessed using an adaptation of the Mini International Neuropsychiatric Interview (MINI) (Sheehan et al., 1998). The participants were asked ten yes/no-questions. A diagnosis of MDE was given if the participant fulfilled the criteria specified by DSM-IV-TR. Otherwise, the participant received a score of zero on this measure. The internal reliability of this measure was good (Cronbach’s α=0.81).
Information on participants’ gender (female=1, male=2) and race/ethnicity (African American=1, Puerto Rican=2) was obtained by self-report.
Data Analysis
Growth mixture modeling (GMM) was used to identify and extract the trajectories of victimization between age 19 and age 36. We applied the maximum likelihood estimation with robust standard errors (MLR) in Mplus for the GMM and apply the full information maximum likelihood (FIML) approach for missing data (Muthén & Muthén, 1998). The Bayesian information criterion (BIC), entropy, and Lo-Mendell-Rubin Likelihood Ratio Test (LRT) were used to determine the number of trajectory groups (Muthén & Muthén, 2010). Each trajectory group was required to have a prevalence of at least 5%. After the trajectory groups were identified based on the above criteria, participants were assigned to a group for which they had the largest Bayesian posterior probability (BPP). We then used violent victimization trajectory group membership as a predictor in our models.
Multivariable logistic regression models were used to examine whether membership in a particular victimization experience trajectory group was associated with PTSD, MDE, SUD, separately; as well as PTSD comorbid with SUD, and PTSD comorbid with MDE at T5. To adjust for the uncertainty of class membership, we used the BPP values associated with the assigned victimization trajectory group as weights in each model (Brook, Pahl, & Ning, 2006; Nagin, 2005; Nagin, 1999). These analyses controlled for gender and race/ethnicity and were conducted using SAS software, version 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
Descriptive Statistics
Among the 674 participants, 52.8% (n=356) self-identified as African American and 47.2% (n=318) as Puerto Rican. Further, 60% (n=405) were female and most reported having a college degree or higher education (n=411, 61%) and being in a relationship (n=494, 73.3%). The sample’s median annual household income was $40,888. Of the 674 T5 participants, 66% participated in all five data collection waves, 32% participated in four waves, and 2% participated in three waves. Chi-squared (χ2) and t tests were used to determine significant differences in attrition rates within the sample. The male attrition rate was significantly higher than the female rate (male: 49.8%, female: 38.1%, χ2 = 16.5, p<0.001). However, there were no differences in the attrition rates of African American (AA) and Puerto Rican (PR) participants (AA=43.7%, PR=43.0%, χ2 = 0.05, p > 0.05). The mean score of victimization at T2 among individuals who participated both at T2 and T5 (mean = 0.40) was not statistically different from the mean score of victimization at T2 among individuals who participated at T2, but not at T5, mean = 0.47 (t=1.85, p= 0.06). The correlations of violent victimization across time points were r (T2, T3) = 0.56, p<0.001, r (T3, T4) = 0.59, p<0.001, and r (T4, T5) = 0.23, p<0.001. The distribution of violent victimization at each data collection time point and psychiatric outcomes of interest at T5 in the sample and stratified by gender and race/ethnicity are provided in Table 1.
Table 1.
Distribution of sample characteristics overall and by gender and race/ethnicity, Harlem Longitudinal Development Study, n=647.
| Measuresa | mean (SD) / n (%) |
||||||
|---|---|---|---|---|---|---|---|
| All (n=647) |
Male (n=269) |
Female (n=405) |
t or χ2 | AAb
(n=356) |
PRc
(n=318) |
t or χ2 | |
| Violent Victimization score | |||||||
| Mean age 19 y (T2) | 0.39 (0.59) | 0.64 (0.76) | 0.24 (0.38) | t = −8.19* | 0.37 (0.56) | 0.43 (0.63) | t = −1.43 |
| Mean age 24 y (T3) | 0.50 (0.68) | 0.78 (0.80) | 0.28 (0.44) | t = −8.33* | 0.51 (0.69) | 0.51 (0.67 | t = −0.11 |
| Mean age 29 y (T4) | 0.47 (0.66) | 0.79 (0.84) | 0.25 (0.39) | t = −9.59* | 0.46 (0.65) | 0.47 (0.68) | t = −0.09 |
| Mean age 36 y (T5) | 0.11 (0.35) | 0.18 (0.44) | 0.07 (0.28) | t = −3.63* | 0.12 (0.37) | 0.12 (0.34) | t = −0.06 |
| Have PTSD (T5) | 53 (7.9%) | 19 (7.1%) | 34 (8.4%) | χ2= 0.40 | 30 (8.4%) | 23 (7.2%) | χ2= 0.33 |
| Have SUD (T5) | 61 (9.1%) | 42 (15.6%) | 19 (4.7%) | χ2= 23.43* | 29 (8.2%) | 32 (10.1%) | χ2= 0.75 |
| Have MDE (T5) | 108 (16.0%) | 34 (12.6%) | 74 (18.3%) | χ2= 3.90* | 54 (15.2%) | 54 (17.0%) | χ2= 0.41 |
| Have co-morbid PTSD-SUD (T5) | 11 (1.6%) | 7 (2.6%) | 4 (1.0%) | χ2= 2.63 | 7 (2.0%) | 4 (1.3%) | χ2= 0.53 |
| Have co-morbid PTSD-MDE (T5) | 32 (4.8%) | 9 (3.4%) | 23 (5.7%) | χ2= 1.95 | 19 (5.3%) | 13 (4.1%) | χ2= 0.58 |
Notes.
T2 – T5: survey follow-up time 2 – time 5; PTSD: Posttraumatic stress disorder; SUD: substance use disorder; MDE: major depressive episode
AA: African American
PR: Puerto Rican
p<.05
Gender and Racial/Ethnic Differences
We conducted χ2 and t tests to examine racial/ethnic and gender differences in violent victimization and psychiatric disorders (Table 1). The results indicated that males reported higher scores on victimization from T2 to T5 (male 0.61 vs. female 0.23, t= −8.19, p<0.001 at T2; male 0.76 vs. female 0.26, t= −8.33, p<0.001 at T3; male 0.75 vs. female 0.24, t= −9.59, p<0.001 at T4; male 0.17 vs. female 0.06, t= −3.63, p<0.001 at T5). Moreover, the prevalence of SUDs in the mid-thirties was higher among males than females (χ2= 23.43, p<0.001). Incidence of MDE in the mid-thirties, on the other hand, was higher among women than men (χ2= 3.90, p<0.05). There were no gender differences in PTSD, PTSD comorbid with SUD, or PTSD comorbid with MDE. In addition, there were no racial/ethnic differences in victimization from T2 to T5, or any of the psychiatric disorders and their comorbidities.
Identifying Trajectory Groups
We computed solutions for two through four trajectory groups (Table 2). We chose the 3-group model, which had the smallest BIC and a significant Lo-Mendell-Rubin LRT indicating better model fit than the 2-group model. Further, the mean BPP for each of three trajectory groups ranged from 0.78 to 0.86, which indicates adequate classification (Nagin, 2005). Although the 4-group model had entropy closest to 1, the BIC was larger than that of the 3-group model, and the Lo-Mendell-Rubin LRT was not significant. Each participant was assigned to the trajectory group for which they had the largest BPP.
Table 2.
Violent victimization trajectory group model goodness-of-fit statistics
| No. of Trajectory Groups | Model Statisticsa | ||
|---|---|---|---|
| BIC | Entropy | Lo-Mendell-Rubin χ2 | |
| 2 | 2986.61 | 0.633 | 201.18* |
| 3 | 2945.75 | 0.663 | 63.05* |
| 4 | 2951.21 | 0.722 | 18.53 |
Notes.
Model Statistics:
BIC: Lower values indicate better fit
Entropy: Range (0,1) with values closer to 1 indicating better fit
Lo-Mendell-Rubin: p<.05 indicates that K-group model is improvement over K-1-group model
p<.05
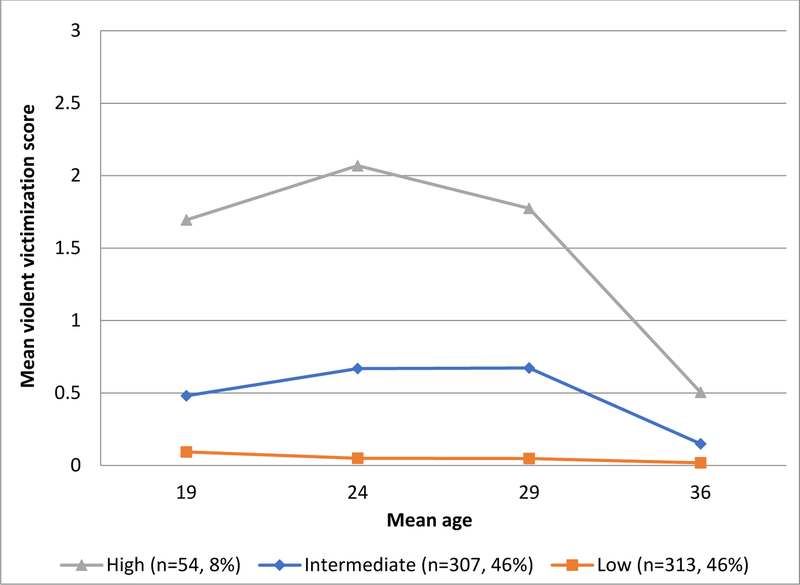
Figure 1 illustrates the observed trajectories for each group based on the average victimization score in that group at each time point. As shown in Figure 1, we labeled the three victimization trajectory groups: low, intermediate, and high violent victimization experience (LV, IV, and HV, respectively) to describe the relative levels of victimization experience observed in the data. The LV trajectory group had an estimated prevalence of 46% (n=313) and included participants who reported no or low experiences of being victimized at each wave. In the LV group, the mean victimization scores at T2-T5 were 0.06, 0.07, 0.05, and 0.01, respectively. The IV trajectory group had an estimated prevalence of 46% (n=307). In the IV group, the mean victimization scores at T2-T5 were 0.44, 0.56, 0.53, and 0.11, respectively. Across time, individuals in the IV group had 7 to over 10 times higher mean victimization scores than individuals in the LV group. The HV group had an estimated prevalence of 8% (n=54). In the HV group, the mean victimization scores at T2-T5 were 1.57, 1.88, 1.77, and 0.54, respectively. Individuals in the HV group had almost 3 to 5 times greater mean victimization scores than individuals in the IV group. As hypothesized, there were gender differences in group membership with males more likely to fall into the HV trajectory group and females more likely to fall into the LV group (χ2= 105.80, p<0.001). The HV, IV, and LV groups included 83.3%, 51.5%, and 21.1% men, respectively.
Figure 1.
Trajectories of violent victimization from late adolescence to the mid-thirties, Harlem Longitudinal Development Study, n=647. Mean violent victimization score is computed as the average of four items assessing frequency of violent victimization experiences including (1) being threatened with a weapon, (2) being hit with a weapon or shot, (3) being cut/stabbed with a knife, and (4) being beaten up (Chavez & Oetting, 1994). Response options ranged from (0) never to (4) five or more times.
Table 3 displays the percentages of individuals meeting criteria for PTSD, SUD, MDE, PTSD comorbid with SUD, and PTSD comorbid with MDE by trajectory group membership. Table 4 shows the adjusted odds ratios (AORs) for the regression of psychiatric outcomes (PTSD, SUD, MDE, and PTSD comorbid with SUD and PTSD comorbid with MDE) on trajectory group membership. Specifically, we compare relatively high and intermediate violent victimization experience trajectory groups to the low experience, and the relatively high violent victimization experience group to the intermediate experience trajectory group.
Table 3.
Prevalence of psychiatric disorders (PTSD, SUD, MDE as well as comorbid PTSD-SUD and PTSD-MDE)a in the mid-thirties by violent victimization experience trajectory group, Harlem Longitudinal Development Sudy, n=647
| Violent Victimization Experience | Prevalence | ||||
|---|---|---|---|---|---|
| Trajectory Group | PTSD | SUD | MDE | Comorbid PTSD-SUD | Comorbid PTSD-MDE |
| High | 16.7 % | 22.2 % | 24.1 % | 7.4 % | 11.1 % |
| Intermediate | 10.1 % | 10.8 % | 18.6 % | 2.0 % | 6.8 % |
| Low | 4.2 % | 5.1 % | 12.1 % | 0.3 % | 1.6 % |
Note.
PTSD: Posttraumatic stress disorder; SUD: substance use disorder; MDE: major depressive episode
Table 4.
Adjusted odds ratios (AORs) and confidence intervals (CIs) for regression of psychiatric disorders (PTSD, SUD, MDE as well as comorbid PTSD-SUD and PTSD-MDE)a in the mid-thirties on violent victimization trajectory group, Harlem Longitudinal Development Study, n=647
| Violent Victimization Trajectory | AOR (CI)b | ||||
|---|---|---|---|---|---|
| Group | PTSD | SUD | MDE | Comorbid PTSD-SUD | Comorbid PTSD-MDE |
| High | 8.7*** (3.0,25.7) | 3.0* (1.2,7.8) | 4.1** (1.8, 9.4) | 23.2* (2.1,255.2) | 18.4*** (4.5,76.3) |
| Intermediate | 3.7** (1.7,7.8) | 1.6 (0.8,3.3) | 2.1** (1.3, 3.5) | 5.7 (0.6,51.3) | 6.3** (2.2, 18.4) |
| Low (referent group) | -- | -- | -- | -- | -- |
| High | 2.4 (0.9,5.8) | 1.9 (0.8,4.1) | 1.9 (0.9,4.2) | 4.1 (1.0,16.4) | 2.9 (0.9,8.7) |
| Intermediate (referent group) | -- | -- | -- | -- | -- |
Notes.
PTSD: Posttraumatic stress disorder; SUD: substance use disorder; MDE: major depressive episode
Gender and race-ethnicity were statistically controlled in all models
p<.05,
p<.01,
p<.001
Associations between Trajectory Groups and Psychiatric Disorders
Multivariable logistic regressions were conducted to assess the associations of trajectory group membership with PTSD and comorbidities, adjusting for gender and race/ethnicity. Membership in the HV trajectory group was associated with an over eight-fold increase in the likelihood of meeting criteria for PTSD (AOR=8.7, p<0.001), a three-fold increase in meeting criteria for SUD (AOR=3.0, p=0.02), and a four-fold increase in meeting criteria for MDE (AOR=4.1, p=0.009) at age 36, compared to being classified as being in the LV group. Membership in the IV trajectory group, compared with the LV trajectory group, was associated with an almost four-fold increase in the likelihood of meeting criteria for PTSD (AOR=3.7, p=0.007) and doubled the risk for MDE (AOR=2.1, p=0.004) at age 36.
Associations between Trajectory Groups and Comorbid Psychiatric Disorders
Membership in the HV trajectory group, as compared with the LV trajectory group, was associated with an over 20-fold increase in the likelihood of meeting criteria for PTSD comorbid with SUD (AOR=23.2, p=0.01) and PTSD comorbid with MDE (AOR=18.4, p<0.001) at age 36. Those in the IV group had over six times increased odds of suffering from PTSD comorbid with MDE than those in the LV group (AOR=6.3, p=0.007).
Discussion
Our results showed that over half of African American and Puerto Rican urban young adults in the study experienced intermediate or relatively high rates of violent victimization at more than one point during young adulthood. Almost one in 12 African American and Puerto Rican urban young adults (8% of the sample) experienced relatively high levels of repeated exposure to violent victimization (HV) between late adolescence and the mid-thirties. This finding that a relatively small subgroup of individuals was repeatedly exposed to victimization concurs with literature that reports that the risk for victimization is increased by previous incidents of victimization (Lauritsen & Quinet, 1995; Menard & Huizinga, 2001; Sullivan, Wilcox, & Ousey, 2011). While absolute levels of victimization in this group may not seem dramatically high (e.g., two incidents in the past five years at age 24), the types of violent victimization measured in this study were of a severe nature (e.g., being hit with a weapon or shot) and are likely to be traumagenic. Hence, other, less severe, incidents of victimization were not captured by our measure, but may have occurred between assessments.
Victimization in the group characterized by relatively high levels of victimization peaked at age 24 and, subsequently, declined to a mean of less than one incident in the past five years at age 36. A similar pattern was observed in the intermediate group that experienced, on average, less than one incident of violent victimization between ages 19 and 29 (IV). These findings are in accord with previous research that reports decreasing exposure to violent victimization past the mid-twenties (Averdijk, 2014; Daigle, Beaver, & Hartman, 2008; DeCamp & Zaykowski, 2015; Skott, 2019). However, other studies have not examined longitudinal trajectories of victimization into the mid-thirties and, therefore, did not capture the continuous steep downward trend in exposure to violence that our data showed. One possibility for these declining trends is that normative developmental and social transitions in the early thirties (e.g., marriage, parenthood, increased responsibilities, improved economic stability) limit opportunities for violence exposure (Laub & Sampson, 2003; Pahl, Brook, & Lee, 2013). For example, data from the National Crime Victimization Survey show that victimization rates are much lower among unmarried individuals than among married ones (Truman et al., 2013). However, further research is needed to identify the social and/or structural mechanisms that may lead to decreased levels of violent victimization over the course of young adulthood.
Confirming our hypothesis, men were more likely than women to experience higher rates of violent victimization over time. Nearly 80% of the males in this study reported victimization experiences that were relatively intermediate or high over the course of young adulthood, confirming the results of studies showing elevated levels of exposure to violent victimization among urban young men of color (Richardson, St. Vil, Sharpe, Wagner, & Cooper, 2016; Truman et al., 2013). Women, on the other hand, were overrepresented in the low victimization group, with about 60% reporting relatively low levels of violent victimization over the course of young adulthood. These gender differences may in part have been due to the measure of violent victimization employed in this study. It did not include the forms of victimization most typically experienced by women, namely rape and sexual assault (Iverson et al., 2013). Indeed, our measure included items reflective of violent crime, to which men are exposed at higher levels than women (Truman et al., 2013).
Our findings evidenced a greater likelihood of meeting criteria for PTSD, SUD, and MDE, as well as PTSD comorbid with SUD and PTSD comorbid with MDE among those in the trajectory group experiencing relatively high rates of violent victimization over time, compared to those in the low victimization group. The traumatic nature of experiences of victimization, such as being assaulted, likely overwhelms an individual’s coping resources and may increase the risk of developing symptoms characteristic of PTSD (e.g. hypervigilance), particularly if traumatic events occur repeatedly (Amstadter et al., 2007). Similarly, depression may arise from feelings of helplessness and the inability to cope with repeated traumatic experiences (Bargai et al., 2007), thus contributing to MDE. Finally, substance abuse can be interpreted as an attempt to cope with the traumatic stress and depression associated with repeated exposure to violence (Khantzian & Albanese, 2008). In our study, individuals in the intermediate victimization group were also more likely to meet criteria for PTSD and MDE, as well as PTSD comorbid with MDE, than those in the low victimization group, suggesting that relatively lower levels of violence exposure, if repeated, may predispose individuals to traumatic stress and depression.
On the other hand, it is also likely that individuals with existing psychiatric vulnerabilities are at heightened risk of being victimized (Cascardi & O’Leary, 1992; Egan & Perry, 1998; Finkelhor & Asdigian, 1996). Experiencing psychological distress caused by trauma or depression increases target vulnerability by making individuals more susceptible to victimization(Finkelhor & Asdigian, 1996). In addition, traumatic stress and depression can interfere with the ability to detect risky situations, as they may compromise cognitive and affective capacities. Similarly, individuals under the influence of drugs or alcohol are often less vigilant in dangerous situations and may thus increase their chances of victimization (DeCamp & Zaykowski, 2015). Furthermore, being intoxicated can have a disinhibiting effect on aggressive behaviors and promote engagement in violent situations (Bushman & Cooper, 1990; Lorenz & Ullman, 2016; Testa & Parks, 1996).
This study is among the first to examine the longitudinal trajectories of violent victimization in urban African American and Puerto Rican young adults into the mid-thirties. Repeated exposure to victimization during young adulthood was experienced by over half of the sample and was found to be associated with trauma-related responses. Among this majority, a smaller group of mostly male participants not only experienced violence repeatedly, but at relatively high levels. These individuals exhibited the highest risk for PTSD, MDE, SUDs and PTSD comorbid with these conditions. Our findings thus suggest that repeat victimization at relatively high levels is related to a range of psychiatric morbidity and comorbidity in adulthood.
Limitations
A limitation of this study concerns our use of self-report measures. Participants may have underreported the incidence of violent victimization (Conway et al., 1994) and violent victimization experiences may be more prevalent among urban African American and Puerto Rican adults than our findings indicated. Individuals may hesitate to provide personal information in a research setting, particularly related to potentially traumatic experiences. A further limitation concerns our measure of violent victimization which did not discriminate between interpersonal and other types of victimization and did not assess sexual assault experience. However, the measure did capture the types of victimization that can be experienced in the context of intimate partner violence (e.g., being beaten up), a type of victimization to which a sizeable minority of women are exposed (Campbell, 2002; Iverson et al., 2013).
In addition, the demographic characteristics of this sample restrict our ability to generalize findings to other racial/ethnic groups, or to non-urban populations. However, urban adolescents and young adults of color experience the highest incidence of violent victimization in the U.S. (Spikes et al., 2010), justifying a focus on these populations.
Conclusions
The identification of risk factors that make individuals vulnerable to the development of PTSD comorbid with other psychiatric disorders is of crucial importance. PTSD comorbid with other psychiatric disorders is a particularly serious condition, as it has proven to persist longer than PTSD alone and can be more difficult to treat than PTSD with no comorbidities (Brady, Killeen, Brewerton, & Lucerini, 2000; Green et al., 2006). Findings here reinforce that repeat victimization may be an important contributor to psychiatric morbidity and comorbidity among urban young men and women of color. It is therefore imperative to identify social, structural, and interpersonal factors underlying the differential patterns of repeat violent victimization in urban African American and LatinX young adults. Research into these areas can contribute to the development of policies aimed at reducing the incidence of violent victimization, as well as inform interventions for victims of violent crime.
Public Health Significance Statement:
This study highlights the effect of long-term exposure to violent victimization during late adolescence and adulthood on the diagnosis of PTSD and psychological comorbidities in later adulthood.
Acknowledgments
This work was supported by the National Institute on Drug Abuse [R01 DA005702].
Footnotes
We use the terms “Black” and “African American” interchangeably in this paper. The sample included both African and Caribbean Americans from New York City.
In this research, we refer to Hispanics when citing research based on Census categories and LatinX in other instances where we generalize beyond a specific ethnic or national subgroup. The term “LatinX” encompasses persons of Cuban, Mexican, Puerto Rican, Dominican South, or Central American or other Spanish descent. We use the specific term “Puerto Rican” when referring to participants in our study.
Contributor Information
Kerstin Pahl, Nathan S. Kline Institute for Psychiatric Research 140 Old Orangeburg Rd., Bldg. 35 Orangeburg, NY 10962, New York University School of Medicine 215 Lexington Avenue, 15th floor New York, NY 10016
Sharifa Z. Williams, Nathan S. Kline Institute for Psychiatric Research 140 Old Orangeburg Rd., Bldg. 35 Orangeburg, NY 10962.
Jung Yeon Lee, Nathan S. Kline Institute for Psychiatric Research 140 Old Orangeburg Rd., Bldg. 35 Orangeburg, NY 10962, New York University School of Medicine 215 Lexington Avenue, 15th floor New York, NY 10016
Adriana Joseph, Nathan S. Kline Institute for Psychiatric Research 140 Old Orangeburg Rd., Bldg. 35 Orangeburg, NY 10962
Chloe Blau, Nathan S. Kline Institute for Psychiatric Research 140 Old Orangeburg Rd., Bldg. 35 Orangeburg, NY 10962
References
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders: DSM-IV-TR. Washington, DC: American Psychiatric Association. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-V-TR. Washington, DC: American Psychiatric Association. [Google Scholar]
- Amstadter AB, McCart MR, & Ruggiero KJ (2007). Psychosocial interventions for adults with crime-related PTSD. Professional Psychology: Research and Practice, 38(6), 640–651. 10.1037/0735-7028.38.6.640 [DOI] [Google Scholar]
- Averdijk M. (2014). Methodological challenges in the study of age- victimization patterns. Can we use the accelerated design of the NCVS to reconstruct victim careers? International Review of Victimology, 20(3), 265–288. [Google Scholar]
- Bargai N, Ben-Shakhar G, & Shalev AY (2007). Posttraumatic Stress Disorder and Depression in Battered Women: The Mediating Role of Learned Helplessness. Journal of Family Violence, 22(5), 267–275. 10.1007/s10896-007-9078-y [DOI] [Google Scholar]
- Barker ED, Arseneault L, Brendgen M, Fontaine N, & Maughan B. (2008). Joint Development of Bullying and Victimization in Adolescence: Relations to Delinquency and Self-Harm. Journal of the American Academy of Child & Adolescent Psychiatry, 47(9), 1030–1038. 10.1097/CHI.OBO13E31817EEC98 [DOI] [PubMed] [Google Scholar]
- Biggs BK, Vernberg E, Little TD, Dill EJ, Fonagy P, & Twemlow SW (2010). Peer victimization trajectories and their association with children’s affect in late elementary school. International Journal of Behavioral Development, 34(2), 136–146. [Google Scholar]
- Blanchard EB, Buckley TC, Hickling EJ, & Taylor AE (1998). Posttraumatic stress disorder and comorbid major depression: is the correlation an illusion? Journal of Anxiety Disorders, 21(1), 21–37. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, & Forneris CA (1996). Psychometric Properties of the PTSD Checklist (PCL). Behaviour Research and Therapy, 34, 669–673. 10.1016/0005-7967(96)00033-2 [DOI] [PubMed] [Google Scholar]
- Bonanno GA (2004). Loss, trauma, and human resilience: Have we underestimated the human capacity to thrive after extremely aversive events? American Psychologist, 59(1), 20. [DOI] [PubMed] [Google Scholar]
- Boney-McCoy S, & Finkelhor D. (1995). Psychosocial sequelae of violent victimization in a national youth sample. Journal of Consulting and Clinical Psychology, 63, 726–736. 10.1037/0022-006X.63.5.726 [DOI] [PubMed] [Google Scholar]
- Brady KT, Killeen TK, Brewerton T, & Lucerini S. (2000). Comorbidity of psychiatric disorders and posttraumatic stress disorder. The Journal of Clinical Psychiatry, 61(Suppl7), 22–32. [PubMed] [Google Scholar]
- Bremner Southwick, Darnell A, & al, et. (1997). Chronic Ptsd in Vietnam Combat Veterans: Course of Illness and Substance Abuse. Year Book of Psychiatry and Applied Mental Health, 1997(7), 307–308. Retrieved from https://insights.ovid.com/year-book-psychiatryapplied-mental-health/ybps/1997/00/070/chronic-ptsd-vietnam-combat-veteranscourse/71/00062674 [DOI] [PubMed] [Google Scholar]
- Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, & Andreski P. (1998a). Trauma and Posttraumatic Stress Disorder in the Community. Archives of General Psychiatry, 55(7), 626 10.1001/archpsyc.55.7.626 [DOI] [PubMed] [Google Scholar]
- Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, & Andreski P. (1998b). Trauma and Posttraumatic Stress Disorder in the Community. Archives of General Psychiatry, 55(7), 626 10.1001/archpsyc.55.7.626 [DOI] [PubMed] [Google Scholar]
- Brook JS, Hamburg BA, Balka EB, & Wynn PS (1992). Sequences of drug involvement in African American and Puerto Rican adolescents. Psychological Reports, 71, 179–182. [DOI] [PubMed] [Google Scholar]
- Brook JS, Pahl K, & Ning Y. (2006). Peer and parental influences on longitudinal trajectories of smoking among African Americans and Puerto Ricans. Nicotine & Tobacco Research, 8(5), 639–651. [DOI] [PubMed] [Google Scholar]
- Brook JS, Whiteman M, Balka EB, & Hamburg BA (1992). African American and Puerto Rican drug use: Personality, familial, and other environmental risk factors. Genetic, Social, and General Psychology Monographs, 118(4), 417–438. [PubMed] [Google Scholar]
- Brook JS, Whiteman M, Balka EB, Win PT, & Gursen MD (1997). African American and Puerto Rican drug use: A longitudinal study. Journal of the American Academy of Child and Adolescent Psychiatry, 36(9), 1260–1268. PMID: [PubMed] [Google Scholar]
- Bushman BJ, & Cooper HM (1990). Effects of Alcohol on Human Aggression: An Integrative Research Review. Psychological Bulletin, 107(3), 341–354. 10.1037/0033-2909.107.3.341 [DOI] [PubMed] [Google Scholar]
- Campbell JC (2002). Health consequences of intimate partner violence. The Lancet, 359(9314), 1331–1336. 10.1016/S0140-6736(02)08336-8 [DOI] [PubMed] [Google Scholar]
- Cascardi M, & O’Leary KD (1992). Depressive symptomatology, self-esteem, and selfblame in battered women. Journal of Family Violence, 7(4), 249–259. [Google Scholar]
- Chavez EL, & Oetting ER (1994). Dropout and delinquency: Mexican-American and Caucasian non-Hispanic youth. Journal of Clinical Child Psychology, 23(1), 47–55. 10.1207/s15374424jccp2301_7 [DOI] [Google Scholar]
- Conway T, Hu T-C, Kim P, & Bullon A. (1994). Prevalence of violence victimization among patients seen in an urban public hospital walk-in clinic. Journal of General Internal Medicine, 9(8), 430–435. 10.1007/BF02599057 [DOI] [PubMed] [Google Scholar]
- Cottler LB, Compton WM, Mager D, Spitznagel EL, & Janca A. (1992). Posttraumatic stress disorder among substance users from the general population. American Journal of Psychiatry, 149, 664–670. [DOI] [PubMed] [Google Scholar]
- Crouch JL, Hanson RF, Saunders BE, Kilpatrick DG, & Resnick HS (2000). Income, race/ethnicity, and exposure to violence in youth: Results from the national survey of adolescents. Journal of Community Psychology, 28(6), 625–641. [Google Scholar]
- Daigle LE, Beaver KM, & Hartman JL (2008). A Life-Course Approach to the Study of Victimization and Offending Behaviors. Victims and Offenders, 3, 365–390. [Google Scholar]
- DeCamp W, & Zaykowski H. (2015). Developmental victimology: Estimating group victimization trajectories in the age–victimization curve. International Review of Victimology, 21(3), 255–272. [Google Scholar]
- Dixon A, Howie P, & Starling J. (2005). Trauma Exposure, Posttraumatic Stress, and Psychiatric Comorbidity in Female Juvenile Offenders. Journal of the American Academy of Child & Adolescent Psychiatry, 44(8), 798–806. 10.1097/01.CHI.0000164590.48318.9C [DOI] [PubMed] [Google Scholar]
- Egan SK, & Perry DG (1998). Does low self-regard invite victimization? Developmental Psychology, 34(2), 299. [DOI] [PubMed] [Google Scholar]
- Elklit A. (2002). Victimization and PTSD in a Danish national youth probability sample. Journal of the American Academy of Child & Adolescent Psychiatry, 41(2), 174–181. 10.1097/00004583-200202000-00011 [DOI] [PubMed] [Google Scholar]
- Finkelhor D, & Asdigian NL (1996). Risk factors for youth victimization: Beyond a lifestyles/routine activities theory approach. Violence and Victims, 11(1), 3–19. [PubMed] [Google Scholar]
- Green BL, Krupnick JL, Chung J, Siddique J, Krause ED, Revicki D, … Miranda J. (2006). Impact of PTSD comorbidity on one-year outcomes in a depression trial. Journal of Clinical Psychology, 62(7), 815–835. 10.1002/jclp.20279 [DOI] [PubMed] [Google Scholar]
- Haden SC, & Scarpa A. (2008). Community violence victimization and depressed mood: The moderating effects of coping and social support. Journal of Interpersonal Violence, 23(9), 1213–1234. [DOI] [PubMed] [Google Scholar]
- Hedtke KA, Ruggiero KJ, Fitzgerald MM, Zinzow HM, Saunders BE, Resnick HS, & Kilpatrick DG (2008). A longitudinal investigation of interpersonal violence in relation to mental health and substance use. Journal of Consulting and Clinical Psychology, 76(4), 633–647. 10.1037/0022-006X.76.4.633 [DOI] [PubMed] [Google Scholar]
- Helzer JE, Robins LN, & McEvoy L. (1987). Post-Traumatic Stress Disorder in the General Population. New England Journal of Medicine, 317(26), 1630–1634. 10.1056/NEJM198712243172604 [DOI] [PubMed] [Google Scholar]
- Iverson KM, King MW, Resick PA, Gerber MR, Kimerling R, & Vogt D. (2013). Clinical Utility of an Intimate Partner Violence Screening Tool for Female VHA Patients. Journal of General Internal Medicine, 28(10), 1288–1293. 10.1007/s11606013-2534-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jennings WG, Higgins GE, Tewksbury R, Gover AR, & Piquero AR (2010). A Longitudinal Assessment of the Victim-Offender Overlap. Journal of Interpersonal Violence, 25(12), 2147–2174. 10.1177/0886260509354888 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, & Nelson CB (1995). Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry, 52(12), 1048–1060. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/7492257 [DOI] [PubMed] [Google Scholar]
- Khantzian EJ, & Albanese MJ (2008). Understanding Addiciton as Self Medication: Finding Hope Behind the Pain. Lanham, MD: Rowman & Littlefield. [Google Scholar]
- Kilpatrick DG, Ruggiero KJ, Acierno R, Saunders BE, Resnick HS, & Best CL (2003). Violence and risk of PTSD, major depression, substance abuse/dependence, and comorbidity: Results from the National Survey of Adolescents. Journal of Consulting and Clinical Psychology, 71(4), 692–700. 10.1037/0022-006X.71.4.692 [DOI] [PubMed] [Google Scholar]
- Laub J, & Sampson R. (2003). Shared Beginnings, Divergent Lives: Delinquent Boys to Age 70. Cambridge, MA: Belknap Press. [Google Scholar]
- Lauritsen JL, & Quinet KFD (1995). Repeat victimization among adolescents and young adults. Journal of Quantitative Criminology, 11(2), 143–166. [Google Scholar]
- Lorenz K, & Ullman SE (2016). Alcohol and sexual assault victimization: Research findings and future directions. Aggression and Violent Behavior, 31, 82–94. 10.1016/j.avb.2016.08.001 [DOI] [Google Scholar]
- Madero-Hernandez A, & Fisher BS (2017). Race, Ethnicity, Risky Lifestyles, and Violent Victimization. Race and Justice, 7(4), 325–349. 10.1177/2153368716651476 [DOI] [Google Scholar]
- McCutcheon VV, Sartor CE, Pommer NE, Bucholz KK, Nelson EC, Madden PAF, & Heath AC (2010). Age at trauma exposure and PTSD risk in young adult women. Journal of Traumatic Stress, 23(6), 811–814. 10.1002/jts.20577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menard S, & Huizinga D. (2001). Repeat victimization in a high-risk neighborhood sample of adolescents. Youth and Society, 32(4), 447–472. [Google Scholar]
- Momartin S, Silove D, Manicavasagar V, & Steel Z. (2004). Comorbidity of PTSD and depression: associations with trauma exposure, symptom severity and functional impairment in Bosnian refugees resettled in Australia. Journal of Affective Disorders, 80(2–3), 231–238. [DOI] [PubMed] [Google Scholar]
- Morgan R, & Truman J. (2018). Criminal Victimization, 2017. Bureau of Justice Statistics, (December). Retrieved from https://www.bjs.gov/content/pub/pdf/cv17.pdf [Google Scholar]
- Muthén L, & Muthén B. (1998). Mplus user’s guide: Statistical analysis with latent variables. Los Angeles, CA: Authors; Retrieved from https://scholar.google.com/scholar?hl=en&as_sdt=0%2C22&q=Mplus+user%27s’+guide+%286th+ed.%29+Los+Angeles%2C+CA%3A+Muthén+%26+Muthén.&btnG= [Google Scholar]
- Muthén L, & Muthén B. (2010). Mplus User’s Guide: Statistical Analysis with Latent Variables: User’s Guide. 10.1111/j.1600-0447.2011.01711.x [DOI] [Google Scholar]
- Nagin D. (2005). Group-based modeling of development. Harvard University Press. [Google Scholar]
- Nagin DS (1999). Analyzing developmental trajectories: A semiparametric, group-based approach. Psychological Methods, 4(2), 139–157. 10.1037/1082989X.4.2.139 [DOI] [PubMed] [Google Scholar]
- Pahl K, Brook JS, & Lee JY (2013). Joint trajectories of victimization and marijuana use and their health consequences among urban African American and Puerto Rican young men. Journal of Behavioral Medicine, 36(3), 305–314. 10.1007/s10865-0129425-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2017). QuickStats: Age-Adjusted Rates for Homicides,* by Race/Ethnicity†— United States, 1999–2015. [Google Scholar]
- Resnick HS, Kilpatrick DG, Dansky BS, Saunders BE, & Best CL (1993). Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. Journal of Consulting and Clinical Psychology, 61(6), 984–991. 10.1037/0022-006X.61.6.984 [DOI] [PubMed] [Google Scholar]
- Richardson JB, Vil C St., Sharpe T, Wagner M, & Cooper C. (2016). Risk factors for recurrent violent injury among black men. Journal of Surgical Research, 204(1), 261–266. [DOI] [PubMed] [Google Scholar]
- Rytwinski NK, Scur MD, Feeny NC, & Youngstrom EA (2013). The Co-Occurrence of Major Depressive Disorder Among Individuals With Posttraumatic Stress Disorder: A Meta-Analysis. Journal of Traumatic Stress, 26(3), 299–309. 10.1002/jts.21814 [DOI] [PubMed] [Google Scholar]
- Salzinger S, Feldman RS, Stockhammer T, & Hood J. (2002). An ecological framework for understanding risk for exposure to community violence and the effects of exposure on children and adolescents. Aggression and Violent Behavior, 7(5), 423–451. 10.1016/S1359-1789(01)00078-7 [DOI] [Google Scholar]
- Schwartz AC, Bradley RL, Sexton M, Sherry A, & Ressler KJ (2005). Posttraumatic Stress Disorder Among African Americans in an Inner City Mental Health Clinic. Psychiatric Services, 56(2), 212–215. 10.1176/appi.ps.56.2.212 [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan H, Amorim P, Janavs J, Weiller E, … Dunbar GC (1998). The MINI-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry, Vol. 59, pp. 22–33. [PubMed] [Google Scholar]
- Skott S. (2019). Disaggregating Violence: Understanding the Decline. Journal of Interpersonal Violence, 1–25. [DOI] [PubMed] [Google Scholar]
- Smith D, & Ecob R. (2007). An investigation into causal links between victimization and offending in adolescents. British Journal of Sociology, 58(4), 633–659. [DOI] [PubMed] [Google Scholar]
- Smith EL, Cooper AD, States., U., & Bureau of Justice Statistics. (2013). Homicide in the U.S. known to law enforcement, 2011. Retrieved from http://purl.fdlp.gov/GPO/gpo45503
- Spikes PS, Willis LA, & Koenig LJ (2010). Violence, Trauma, and Mental Health Disorders: Are They Related to Higher HIV Risk for African Americans? In African Americans and HIV/AIDS (pp. 85–112). 10.1007/978-0-387-78321-5_6 [DOI] [Google Scholar]
- Sullivan CJ, Wilcox P, & Ousey GC (2011). Trajectories of victimization from early to mid-adolescence. Criminal Justice and Behavior, 38(1), 85–104. [Google Scholar]
- Testa M, & Parks KA (1996). The role of women’s alcohol consumption in sexual victimization. Aggression and Violent Behavior, 1(3), 217–234. 10.1016/1359-1789(95)00017-8 [DOI] [Google Scholar]
- Truman J, Langton L, & Planty M. (2013). Criminal Victimization, 2012. Retrieved from https://www.bjs.gov/content/pub/pdf/cv12.pdf
- Vaughn MG, Fu Q, Delisi M, Beaver KM, Perron BE, & Howard MO (2010). Criminal victimization and comorbid substance use and psychiatric disorders in the United States: Results from the NESARC. Annals of Epidemiology, 20, 281–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers Frank; Litz Brett; Herman Debra S.; Keane TM (1993). The PTSD checklist (PCL): Reliability, validity, and diagnostic utility. San Antonio, TX. [Google Scholar]
- Weist MD, Acosta OM, & Youngstrom EA (2001). Predictors of violence exposure among inner-city youth. Journal of Clinical Child Psychology, 30, 187–198. 10.1207/S15374424JCCP3002_6 [DOI] [PubMed] [Google Scholar]
- Wilson WJ (1987). The truly disadvantaged: The inner city, the underclass, and public policy. Chicago, IL: The University of Chicago Press. [Google Scholar]
- Wittchen HU, & Kessler RC (1994). Modifications of the CIDI in the National Comorbidity Survey: The Development of the UM-CIDI (No. 2). Retrieved from http://www.hcp.med.harvard.edu/ncs/ftpdir/um-cidi.pdf
- Xie M, Heimer K, Lynch JP, & Planty M. (2018). Why is the Victimization of Young Latino Adults Higher in New Areas of Settlement? Journal of Quantitative Criminology, 34(3), 657–690. 10.1007/s10940-017-9350-0 [DOI] [Google Scholar]