Abstract
Background:
With the rapid rise in opioid overdose-related deaths, state policymakers have expanded policies to increase the use of naloxone by emergency medical services (EMS). However, little is known about changes in EMS naloxone administration in the context of continued worsening of the opioid crisis and efforts to increase use of naloxone. This study examines trends in patient demographic and EMS response characteristics over time and by county urbanicity.
Methods:
We used data from the 2013–2016 National EMS Information System to examine trends in patient demographics and EMS response characteristics for 911-initiated incidents that resulted in EMS naloxone administration. We also assessed temporal, regional, and urban-rural variation in per capita rates of EMS naloxone administrations compared with per capita rates of opioid-related overdose deaths.
Results:
From 2013 to 2016, naloxone administrations increasingly involved young adults and occurred in public settings. Particularly in urban counties, there were modest but significant increases in the percentage of individuals who refused subsequent treatment, were treated and released, and received multiple administrations of naloxone before and after arrival of EMS personnel. Over the four year period, EMS naloxone administrations per capita increased at a faster rate than opioid-related overdose deaths across urban, suburban, and rural counties. Although national rates of naloxone administration were consistently higher in suburban counties, these trends varied across U.S. Census Regions, with the highest rates of suburban administration occurring in the South.
Conclusions:
Naloxone administration rates increased more quickly than opioid deaths across all levels of county urbanicity, but increases in the percentage of individuals requiring multiple doses and refusing subsequent care require further attention.
Keywords: naloxone, emergency medical services, opioids, drug overdose
INTRODUCTION
In 2017, an estimated 49,068 deaths were attributable to opioid overdoses, up from 8,050 in 1999.1 Although the rate of increase in deaths due to opioid analgesics has slowed, deaths due to heroin and synthetic opioids such as fentanyl have surged in recent years,1 with a corresponding increase in the prevalence of illicit opioids seen in hospital encounters data,2 in law enforcement seizure data,3 and among opioid treatment program entrants.4 This increase in non-prescription opioid overdoses has largely been concentrated among young adults2, 5 and in urban areas, where overdose deaths from synthetic opioids have surpassed those from opioid analgesics.6, 7 The evolution of the opioid crisis influences not only the populations and communities most affected but has important implications for strategies implemented to mitigate opioid-related harms.8–11
Expanding access to naloxone, an opioid antagonist effective in reversing the life-threatening effects of opioids,12 is one strategy increasingly used by state and local policymakers to reduce opioid-related overdoses. Historically used only by paramedics and clinicians in organized health care settings,13 recent state and local policy changes have increasingly authorized all emergency medical services (EMS) licensure levels to administer naloxone. As of September 2017, all but one U.S. state had expanded EMS scope of practice to allow basic life support (BLS) personnel, including emergency medical technicians (EMTs), to administer naloxone,14 up from only thirteen states just four years prior.15 These efforts may have particular benefits for residents of rural areas, who have faced disparities in access to prehospital naloxone, a more limited supply of paramedics, and increasingly greater rates of drug overdose deaths compared with residents of urban and suburban areas.16, 17
While prior studies have found notable disparities in access to prehospital naloxone in rural communities,16, 18, 19 these national studies have largely examined cross-sectional data on EMS events prior to the increase in prevalence of synthetic opioids and expansion of EMS scope of practice. Other recent work has documented an upward trend in EMS naloxone administrations nationwide20 but has not examined differential changes in pre-hospital naloxone administration across geographic regions nor across different levels of urbanicity. Nor have studies examined how the characteristics of EMS calls in which naloxone is administered might differ between urban, suburban, and rural areas in the context of the continued evolution of the opioid crisis and associated policy changes, despite clear differences by county urbanicity in access to treatment for opioid use disorder,21 availability of community-based naloxone distribution programs,22 and general EMS workforce demands.23 Yet, such information can inform policies and resource allocation decisions in a dynamically evolving opioid risk environment.
To address this gap in the literature and better understand trends in EMS administration of naloxone, this study uses 2013 to 2016 data from a national dataset containing information on the administration of naloxone by EMS personnel to examine trends in EMS naloxone administration, including location, patient demographics, and EMS response characteristics. It is hypothesized that trends in EMS naloxone administration will reflect the shift in opioid overdoses toward younger individuals, particularly in areas with more potent synthetic opioids. In addition, we expect trends in EMS response characteristics to differ by urbanicity due to the changing scope of practice laws in this period increasing access to naloxone in rural counties.
METHODS
Data Sources and Sample
Using the 2013 to 2016 National Emergency Medical Services Information System (NEMSIS), a uniform database representative of the U.S. population of EMS patients,24 we identified 698,260 incidents in which EMS personnel administered naloxone using the text-based field for medications administered. In 2013, 43 states participated in NEMSIS, with three additional states (Rhode Island, Vermont, and Louisiana) and the District of Columbia submitting data by 2016. Consistent with previous research,16, 20 we restricted our sample to 911-initiated EMS incidents and excluded calls reported as cancelled, no patient found, or no treatment required. While the NEMSIS provides a standardized national registry of EMS responses, it is important to note that it relies on the completeness and accuracy of reporting by EMS field personnel, and the public use version of the data does not contain codes to identify overdose incidents in which naloxone was not administered. Our analyses of the NEMSIS are thus restricted to overdose incidents in which EMS responded and administered naloxone, which allows examination of a broader class of opioid overdose outcomes than mortality data but likely captures a relatively small proportion of total opioid overdose events.25 In addition, because the data do not contain codes for whether an incident involved an opioid overdose, our sample of EMS naloxone administrations may also capture non-opioid-overdose incidents in which naloxone treatment was administered as part of standard resuscitative procedures in emergent situations with undetermined underlying clinical cause.
To explore the relationship between EMS naloxone administration and opioid overdose mortality, we obtained information on opioid-related overdose death rates from the Center for Disease Control’s National Center for Health Statistics multiple cause of death mortality files, restricting the mortality sample to those states included in the NEMSIS in each year. Consistent with previous research,26 we identified opioid-related overdose deaths using International Classification of Diseases, 10th (ICD-10) edition codes for a drug overdose (X40-X44, X60-X64, X85, and Y10-Y14) as well as an ICD-10 code for opium (T40.0), heroin (T40.1), other opioids (T40.2), methadone (T40.3), other synthetic narcotics (T40.4), and other or unspecified narcotics (T40.6). Given research showing geographic and temporal variation in the specificity with which specific drugs are reported in the death certificate data,27, 28 we also assessed EMS naloxone administration trends compared with all drug overdose mortality. The corresponding author’s Institutional Review Board determined the study to be exempt.
Variables
Annual rates of EMS naloxone administrations and opioid-related overdose deaths per capita were calculated overall and by county urbanicity and U.S. Census Region. Within the NEMSIS, county urbanicity is defined based on the county in which the reporting EMS agency is located and is categorized based on the county’s Urban Influence Code29 as urban (large or small metropolitan counties), suburban (micropolitan counties adjacent to metropolitan county), rural/frontier (non-urban core counties adjacent to metropolitan county or non-core counties adjacent to micropolitan county). To convert counts to per capita rates, population counts for the states included in NEMSIS in each year were obtained from the U.S. Census Bureau and summarized by county urbanicity (urban, suburban, or rural/frontier) using the 2013 Urban Influence Codes,29 consistent with the county-based urbanicity classification used in NEMSIS.
The NEMSIS dataset includes information on patient age (categorized as 0–19, 20–29, 30–39, 40–49, 50–59, and ≥ 60 years) and gender, as well as information about EMS response characteristics, including incident location (categorized as “home/residence,” “street or highway,” “trade or service,” or “other location”). Information on whether the patient had received naloxone prior to EMS personnel arrival or whether the individual received naloxone multiple times from the reporting EMS agency came from text-based fields. Finally, we examined the disposition of individuals administered naloxone using the categorical variable in the NEMSIS, which includes the following classification: died at scene, treated and released, treated and transferred care, treated and transported by EMS, treated and transported by law enforcement, treated and transported by private vehicle, or a “refused care” category for individuals who withdrew consent for care at some point during the EMS response or refused to give consent (such as might occur after an individual was revived with naloxone).
Analysis
We examined variation in incident characteristics involving EMS naloxone administration over time from 2013 to 2016 and stratified by urbanicity. We also assessed trends in per capita naloxone administration and opioid-related and all-drug overdose death rates over time by county urbanicity and by U.S. Census Region. Significance of changes over time was assessed using the chi-squared test of independence, and comparisons were considered statistically significant based on a two-sided p-value of 0.05. A sensitivity analysis including NEMSIS data from 2012, which did not include California, Montana, and Indiana, was conducted to assess changes in observed trends. As there was no meaningful difference in findings using the 2012 data, we chose to present the 2013 to 2016 data to allow more complete and consistent state coverage. Analyses were conducted using SAS 9.4 (SAS Institute, Cary, NC).
RESULTS
We found a substantial increase in the number of EMS incidents in which naloxone was administered, rising from 107,666 in 2013 to 206,354 in 2016. Across all four years, EMS-administered naloxone occurred predominantly in response to incidents occurring in private residences and among individuals who were male, over age 40, and residing in the South (Table 1). We also found an increase in the percentage of EMS-administered naloxone in urban settings with a corresponding decrease in suburban and rural counties (p-values all <0.001). However, we noted a significant shift in location over time, with the percentage of EMS incidents in which naloxone was administered in streets/highways and public settings such as bars, restaurants, and other businesses increasing significantly from 2013 to 2016, as well as a trend toward naloxone receipt among young adults aged 20 to 39. Over the same time period, there were decreases in the percentage of EMS naloxone administrations in private residences and to individuals over age 40 (with the most pronounced decline among individuals age 60 and older). Despite the shift in the age distribution toward younger adults, across each year more than 40% of naloxone administrations by EMS were for adults aged 50 and older.
TABLE 1.
Characteristics of Emergency Medical Services (EMS) Naloxone Administrations, by Year of Incident
| 2013 (n=107,666) | 2014 (N=122,506) | 2015 (N=166,002) | 2016 (N=206,354) | ||
|---|---|---|---|---|---|
| % | % | % | % | p-value | |
| Patient gender | <0.001 | ||||
| Male | 54.6 | 56.4 | 58.4 | 61.0 | |
| Female | 44.9 | 43.1 | 41.3 | 38.6 | |
| Patient age | <0.001 | ||||
| <20 | 4.2 | 3.8 | 3.5 | 3.0 | |
| 20–29 | 17.4 | 18.0 | 19.7 | 20.6 | |
| 30–39 | 15.4 | 16.2 | 18.2 | 19.9 | |
| 40–49 | 16.5 | 15.9 | 15.4 | 15.6 | |
| 50–59 | 19.7 | 19.3 | 18.6 | 18.2 | |
| 60+ | 26.5 | 26.3 | 24.1 | 22.5 | |
| Unknown | 0.3 | 0.4 | 0.4 | 0.4 | |
| Incident location | <0.001 | ||||
| Private residence | 65.3 | 63.9 | 62.0 | 55.6 | |
| Industrial place | 0.3 | 0.3 | 0.3 | 0.2 | |
| Street or highway | 8.4 | 9.4 | 11.7 | 12.1 | |
| Trade or service | 5.3 | 5.4 | 6.2 | 6.6 | |
| Residential institution | 2.9 | 3.2 | 2.9 | 2.8 | |
| Other location | 12.0 | 13.0 | 11.9 | 15.3 | |
| Unknown | 5.9 | 4.9 | 5.0 | 7.4 | |
| Patient disposition | <0.001 | ||||
| Died at scene | 2.7 | 2.9 | 3.0 | 3.1 | |
| Patient refused/withdrew permission | 0.4 | 0.5 | 0.8 | 1.8 | |
| Treated and released | 1.0 | 1.2 | 1.4 | 1.9 | |
| Treated and transferred | 2.2 | 3.1 | 3.6 | 4.7 | |
| Treated, transport by EMS | 93.6 | 92.2 | 91.2 | 88.4 | |
| Treated, transport by law enforcement | 0.0 | 0.0 | 0.0 | 0.0 | |
| Treated, transport by private vehicle | 0.1 | 0.1 | 0.0 | 0.0 | |
| EMS-administered naloxone doses | <0.001 | ||||
| 1 | 85.0 | 83.5 | 81.6 | 78.6 | |
| ≥ 2 | 15.0 | 16.5 | 18.4 | 21.4 | |
| Naloxone prior to EMS arrival | <0.001 | ||||
| Yes | 0.3 | 0.8 | 0.7 | 1.4 | |
| No | 99.7 | 99.2 | 99.3 | 98.6 | |
| Census region | <0.001 | ||||
| Midwest | 19.6 | 20.0 | 20.2 | 20.1 | |
| Northeast | 14.0 | 16.1 | 19.0 | 19.4 | |
| South | 48.0 | 45.1 | 44.4 | 47.0 | |
| West | 18.3 | 18.7 | 16.3 | 13.6 | |
| County urbanicity | <0.001 | ||||
| Urban | 81.5 | 80.7 | 81.1 | 83.9 | |
| Suburban | 7.7 | 7.2 | 6.9 | 6.0 | |
| Rural or frontier | 9.4 | 8.9 | 8.6 | 7.4 | |
| Not recorded | 1.5 | 3.2 | 3.4 | 2.6 | |
From 2013 to 2016, there were statistically significant increases (all p<0.001) in the percentage of individuals receiving multiple doses of naloxone from EMS personnel (15.0% in 2013 to 21.4% in 2016), as well as smaller but notable increases in the percentage of individuals who had received naloxone prior to EMS arrival (0.3% to 1.4%) and who refused or withdrew consent to receive subsequent treatment from EMS following the administration of naloxone (0.4% to 1.8%). Across all years, there were comparably few cases and more modest increases in the number of individuals who were treated and released without receiving transport or subsequent care (1.0% to 1.9%) or who had died at the scene (2.7% to 3.1%).
Urban/Suburban/Rural and Regional Variation
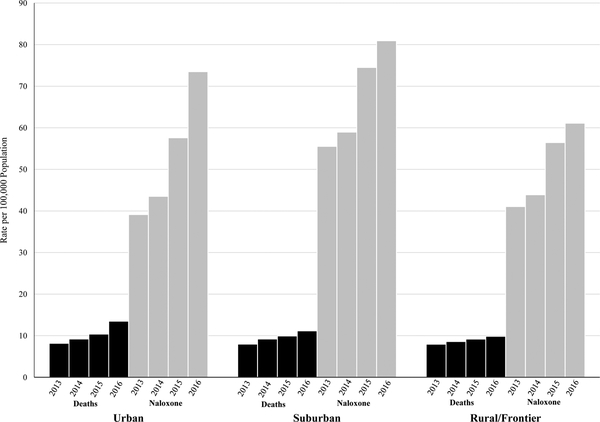
Given differences in the nature of the opioid problem and available treatment by urbanicity and region,7 we assessed whether national trends in EMS-administered naloxone mask important geographic variation. Figure 1 illustrates the increase in per capita rates of both EMS naloxone administrations and opioid-related overdose deaths from 2013 through 2016, stratified by county urbanicity. Over the four-year period, there was an 88% increase in EMS naloxone administrations per capita in urban counties, a rate of increase exceeding that seen in suburban (46%) and rural counties (49%), paralleling increases in opioid-related overdose deaths in urban (65%), suburban (40%), and rural counties (24%). Per capita EMS naloxone administrations were consistently higher in suburban counties, but there were substantial increases in EMS naloxone administration rates in 2015 and 2016 across all levels of county urbanicity that do not correspond to comparable increases in opioid overdose mortality. Results were consistent when examining all drug overdose mortality (see Supplemental Material), showing that the increases in all drug overdose death rates were also greatest in urban areas (42%), followed by suburban (27%) and rural areas (18%).
FIGURE 1.
Per Capita Rates of Opioid-Related Overdose Deaths and Naloxone Administrations by Emergency Medical Services (EMS) Responding to 911 Calls, by County Urbanicity
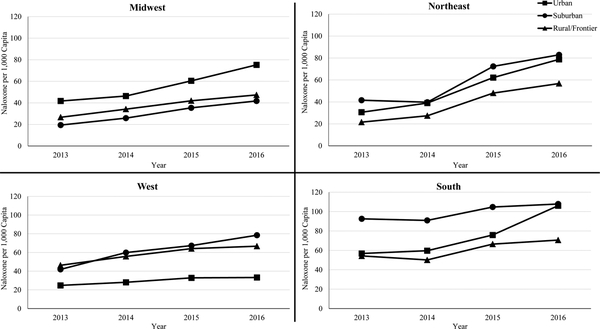
While suburban areas nationally had the highest EMS naloxone administration rates relative to other urbanicity levels, there was substantial variation in naloxone administration by urbanicity in different regions (Figure 2). The highest level of naloxone administration in suburban counties was in the South, primarily the South Atlantic division which includes West Virginia and North Carolina (see Supplemental Material for figures stratified by Census Division). In contrast, EMS naloxone administration rates in the Midwest were highest in urban counties, with suburban counties having the lowest rates of naloxone administration. The Northeast had the most the rapid growth in naloxone administration rates at all urbanicity levels since 2013, with rates of naloxone administration persistently highest in suburban and urban counties. The West, however, has seen relatively little growth in naloxone administration rates, with relatively low levels of EMS naloxone administration in urban areas compared with other regions.
FIGURE 2.
Trends in Per Capita Rates of Emergency Medical Services Naloxone Administrations, by Census Region
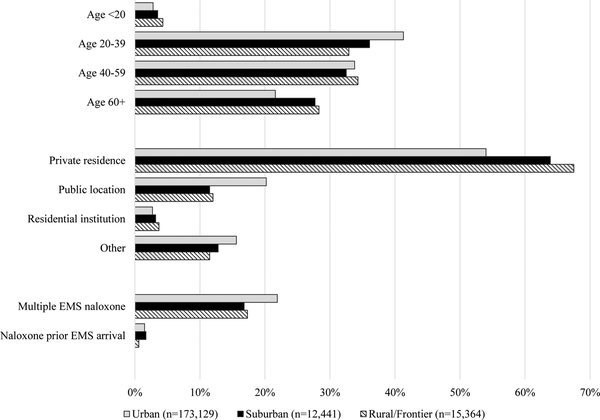
Finally, we examined if individual or incident characteristics involving naloxone administration differed by the urbanicity of EMS agency locations (Figure 3). Compared with suburban and rural counties, a greater percentage of individuals administered naloxone by EMS in urban counties were between ages 20 and 39. In contrast, recipients of EMS-administered naloxone in suburban and rural counties were skewed toward persons over age 60. Naloxone administration in urban counties more commonly occurred in public settings, while naloxone administration in rural counties occurred more frequently in private residences. Individuals in urban areas were also more likely to have received a dose of naloxone prior to EMS administration and were more likely to receive multiple doses of naloxone from EMS personnel (p-values all <0.001).
FIGURE 3.
Characteristics of Emergency Medical Services Naloxone Administrations in 2016, by County Urbanicity
DISCUSSION
The substantial increase in 911 calls resulting in naloxone administration by EMS personnel from 2013 to 2016 corresponds with the worsening opioid crisis, including a dramatic increase in deaths involving fentanyl.30 Prior studies have found substantially elevated risk of mortality after nonfatal opioid overdose,31–33 but these risks are heterogeneous across populations. For instance, one study in Marion County, Indiana showed nearly 10% of individuals who received EMS-administered naloxone died during an average two years of follow-up, with younger adults more likely to die from drug-related causes and older adults from causes related to chronic health conditions.32 In light of public concerns that individuals administered naloxone who refuse subsequent interventions or transport may miss a critical opportunity to receive treatment,34–38 it is important to emphasize that effective interventions may include treatment with buprenorphine or methadone maintenance therapy, which have been shown to significantly reduce mortality risk,31, 39 as well as efforts to address high-risk opioid prescribing, a significant risk for opioid-related mortality in older individuals.40 Furthermore, while we found that the percentage of individuals administered naloxone by EMS who refused care or were treated and released without subsequent medical attention had increased since 2014, we note that over 93% of patients received transport after naloxone administration by EMS in 2016. Further research on the context of those EMS naloxone administration incidents that involve refusal of subsequent care, as well as longitudinal follow-up study of patients who receive treatment for overdose from EMS can offer insights on opportunities to engage and support individuals who receive prehospital naloxone through EMS channels.41
As stronger opioids such as fentanyl and carfentanil become more widely available, opioid overdose victims may require more than a single dose of naloxone, and thus a longer observation window may be required for individuals administered naloxone by EMS.30 In 2016, over one in five individuals receiving naloxone from EMS received multiple doses, a 42% increase from 2013; furthermore, a small but increasing share of individuals received naloxone before the arrival of EMS. Given increasing availability of more potent opioids, attention to additional harm reduction approaches, such as test strips and supervised injection facilities, will become increasingly important as a complement to naloxone in public health efforts to decrease fatal opioid overdoses.
Regional and urban-rural differences in EMS naloxone administration trends mirror differential trends in rates of opioid overdose mortality.7 The shifting composition of EMS naloxone administrations toward younger, male patients also aligns with evidence on the demographic characteristics of overdose deaths involving illicit opioids relative to those involving prescription opioids.11 Across all levels of county urbanicity, naloxone administration rates increased more quickly than opioid deaths, with the most notable increases in naloxone administrations observed in 2015 and 2016. This is encouraging as more widespread naloxone use is a key component of public health efforts to reduce opioid-related overdose deaths. Our findings coincide with the timing of policies passed after 2014 in many states to allow non-paramedic EMS professionals to administer naloxone,14 raising important questions for future research regarding the extent to which recent policies are contributing to the increase in naloxone administrations.
While most EMS naloxone administration still occurs in private residences, there is a trend for EMS-administered naloxone, particularly in urban communities, to be provided in public settings such as businesses and on streets and highways. Policies that make naloxone available to casual bystanders, such as placing naloxone kits in public venues and areas with frequent overdoses, may be important complements to existing efforts such as third-party prescribing and naloxone distribution programs that are more likely to enhance naloxone use by an individual’s friends or family. The finding that characteristics of EMS naloxone administration incidents vary by urban-rural status, combined with the growing burden of illicit opioids in overdoses in more urban areas,10 suggest the potential need for targeted approaches to naloxone delivery and other public health interventions that account for the local environment.
Limitations
Our study had several limitations. The NEMSIS is a convenience sample, relying on information submitted by EMS agencies in participating states. While generalizable to the U.S. population of EMS patients,24 we do not know if our findings are generalizable to the four non-participating jurisdictions as of 2016 (Rhode Island, Vermont, Louisiana, and the District of Columbia); however, the population of those jurisdictions represents only 2.2% of the US population,42 and results were consistent in census divisions unaffected by sample changes, so we believe it is unlikely that sample composition changes drive our results. Findings from the NEMSIS should also not be considered generalizable to all overdoses, as the dataset contains information only for individuals who were administered naloxone from EMS, a population likely to skew older and hence involve pharmaceutical opioid overdose events rather than those related to heroin or other illicit opioids.8, 40, 43 In addition, the public NEMSIS does not capture variables that would permit us to identify opioid overdose events in which naloxone was not administered, or to confirm whether a naloxone recipient did in fact overdose on opioids; given patient privacy protections, the NEMSIS also does not provide state identifiers, and thus we cannot determine whether the changes in EMS naloxone administration are driven by changes in state policies aimed at increasing naloxone access. Finally, while our findings are statistically significant, we note that many changes in trends over time are small, and the clinical impact of these changes should be explored in future research.
Conclusions
In light of the ongoing opioid crisis and the role of naloxone in reversing potentially fatal overdoses, it is encouraging that we observed that rates of increase in naloxone administration by EMS personnel exceeded increases in opioid-related overdose deaths. However, EMS administration of naloxone is complemented in many communities by naloxone available from pharmacies under standing orders and from community-based naloxone distribution programs, and understanding how to maximize the benefits from all three approaches is critical to effective harm reduction efforts. Furthermore, as the opioid crisis evolves and opioid-related overdoses continue to climb, policy approaches need to evolve to address shifts in the populations most affected, and continued efforts are needed to enhance the availability and use of naloxone to reverse potentially fatal overdoses, ensure that individuals receive treatment to decrease the likelihood of future overdoses, and potentially decrease high-risk prescribing of opioid analgesics to such individuals.
Supplementary Material
ACKNOWLEDGEMENTS
The authors would like to thank Dr. N Clay Mann for providing guidance and assistance with the primary data set. We also thank Ray Barrishansky for his valuable feedback on early versions of the article, and Lynn Polite for assistance in manuscript preparation.
FUNDING
This work was supported by the following grants from the National Institutes of Health: R21 DA045950–01, (Smart, PI) and P50 DA046351 (Stein, PI), both from the National Institute on Drug Abuse (NIDA). The content is solely the responsibility of the authors and does not necessarily represent the official views of NIDA or the National Institutes of Health. The funding organization had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. The authors declare they have no conflicts of interest.
REFERENCES
- 1.National Institute on Drug Abuse. Overdose Death Rates. 2018;Available at: https://www.drugabuse.gov/related-topics/trends-statistics/overdose-death-rates. Accessed October 8, 2018.
- 2.Unick GJ and Ciccarone D. US regional and demographic differences in prescription opioid and heroin-related overdose hospitalizations. Int J Drug Policy. 2017;46:112–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gladden RM. Fentanyl law enforcement submissions and increases in synthetic opioid–involved overdose deaths—27 states, 2013–2014. MMWR Morb Mortal Wkly Rep. 2016;65. [DOI] [PubMed] [Google Scholar]
- 4.Pouget ER, Fong C and Rosenblum A. Racial/Ethnic Differences in Prevalence Trends for Heroin use and Non-Medical use of Prescription Opioids Among Entrants to Opioid Treatment Programs, 2005–2016. Subst Use Misuse. 2018;53(2):290–300. [DOI] [PubMed] [Google Scholar]
- 5.Rudd RA, Seth P, David F and Scholl L. Increases in Drug and Opioid-Involved Overdose Deaths - United States, 2010–2015. MMWR Morb Mortal Wkly Rep. 2016;65(5051):1445–1452. [DOI] [PubMed] [Google Scholar]
- 6.Monnat SM and Rigg KK. The Opioid Crisis in Rural and Small Town America. Durham, NH: Carsey School of Public Policy;2018. [Google Scholar]
- 7.Rigg KK, Monnat SM and Chavez MN. Opioid-related mortality in rural America: Geographic heterogeneity and intervention strategies. Int J Drug Policy. 2018;57:119–129. [DOI] [PubMed] [Google Scholar]
- 8.McBain RK, Rose AJ and LaRochelle MR. The US Opioid Epidemic. Prev Med. 2018;112:176–178. [DOI] [PubMed] [Google Scholar]
- 9.Dasgupta N, Beletsky L and Ciccarone D. Opioid crisis: No easy fix to its social and economic determinants. Am J Public Health. 2018;108(2):182–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vivolo-Kantor AM, Seth P, Gladden RM, et al. Vital signs: trends in emergency department visits for suspected opioid overdoses—United States, July 2016–September 2017. MMWR Morb Mortal Wkly Rep. 2018;67(9):279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mattson CL, O’Donnell J, Kariisa M, Seth P, Scholl L and Gladden RM. Opportunities to Prevent Overdose Deaths Involving Prescription and Illicit Opioids, 11 States, July 2016–June 2017. MMWR Morb Mortal Wkly Rep. 2018;67(34):945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Boyer EW. Management of opioid analgesic overdose. N Engl J Med. 2012;367(2):146–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wermeling DP. Review of naloxone safety for opioid overdose: practical considerations for new technology and expanded public access. Therapeutic Advances in Drug Safety. 2015;6(1):20–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kinsman JM and Robinson K. National Systematic Legal Review of State Policies on Emergency Medical Services Licensure Levels’ Authority to Administer Opioid Antagonists. Prehosp Emerg Care. 2018:1–5. [DOI] [PubMed] [Google Scholar]
- 15.Davis CS, Southwell JK, Niehaus VR, Walley AY and Dailey MW. Emergency medical services naloxone access: a national systematic legal review. Acad Emerg Med. 2014;21(10):1173–1177. [DOI] [PubMed] [Google Scholar]
- 16.Faul M, Dailey MW, Sugerman DE, Sasser SM, Levy B and Paulozzi LJ. Disparity in naloxone administration by emergency medical service providers and the burden of drug overdose in US rural communities. Am J Public Health. 2015;105(S3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mack KA, Jones CM and Ballesteros MF. Illicit drug use, illicit drug use disorders, and drug overdose deaths in metropolitan and nonmetropolitan areas—United States. Am J Transplant. 2017;17(12):3241–3252. [DOI] [PubMed] [Google Scholar]
- 18.Hatten BW. Factors associated with prehospital naloxone use. Clin Toxicol. 2014;52(4):316–317. [Google Scholar]
- 19.Faul M, Lurie P, Kinsman JM, Dailey MW, Crabaugh C and Sasser SM. Multiple Naloxone Administrations Among Emergency Medical Service Providers is Increasing. Prehosp Emerg Care. 2017:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cash RE, Kinsman J, Crowe RP, Rivard MK, Faul M and Panchal AR. Naloxone Administration Frequency During Emergency Medical Service Events—United States, 2012–2016. MMWR Morb Mortal Wkly Rep. 2018;67:850––853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stein BD, Dick AW, Sorbero M, et al. A population-based examination of trends and disparities in medication treatment for opioid use disorders among Medicaid enrollees. Subst Abus. 2018:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lambdin BH, Davis CS, Wheeler E, Tueller S and Kral AH. Naloxone laws facilitate the establishment of overdose education and naloxone distribution programs in the United States. Drug Alcohol Depend. 2018;188:370–376. [DOI] [PubMed] [Google Scholar]
- 23.Chapman SA, Crowe RP and Bentley MA. Recruitment and Retention of New Emergency Medical Technician (EMT)-Basics and Paramedics. Prehosp Disaster Med. 2016;31(S1):S70–S86. [DOI] [PubMed] [Google Scholar]
- 24.Mann NC, Kane L, Dai M and Jacobson K. Description of the 2012 NEMSIS public-release research dataset. Prehosp Emerg Care. 2015;19(2):232–240. [DOI] [PubMed] [Google Scholar]
- 25.Darke S, Mattick RP and Degenhardt L. The ratio of non‐fatal to fatal heroin overdose. Addiction. 2003;98(8):1169–1171. [DOI] [PubMed] [Google Scholar]
- 26.Hedegaard H, Warner M and Miniño A. Drug Overdose Deaths in the United States, 1999–2016. Hyattsville, MD: National Center for Health Statistics;2017. [Google Scholar]
- 27.Ruhm CJ. Geographic Variation in Opioid and Heroin Involved Drug Poisoning Mortality Rates. Am J Prev Med. 2017;53(6):745–753. [DOI] [PubMed] [Google Scholar]
- 28.Ruhm CJ. Corrected US opioid-involved drug poisoning deaths and mortality rates, 1999–2015. Addiction. 2018;113(7):1339–1344. [DOI] [PubMed] [Google Scholar]
- 29.U.S. Department of Agriculture. 2013. Urban Influence Codes. [Dataset]. 2013;Available at: https://www.ers.usda.gov/data-products/urban-influence-codes/. Accessed October 8, 2018.
- 30.Fairbairn N, Coffin PO and Walley AY. Naloxone for heroin, prescription opioid, and illicitly made fentanyl overdoses: Challenges and innovations responding to a dynamic epidemic. Int J Drug Policy. 2017;46:172–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Larochelle MR, Bernson D, Land T, et al. Medication for Opioid Use Disorder After Nonfatal Opioid Overdose and Association With Mortality: A Cohort Study. Ann Intern Med. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ray BR, Lowder EM, Kivisto AJ, Phalen P and Gil H. EMS naloxone administration as non‐fatal opioid overdose surveillance: 6‐year outcomes in Marion County, Indiana. Addiction. 2018;113(12):2271–2279. [DOI] [PubMed] [Google Scholar]
- 33.Olfson M, Wall M, Wang S, Crystal S and Blanco C. Risks of fatal opioid overdose during the first year following nonfatal overdose. Drug Alcohol Depend. 2018;190:112–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wolfram J More Philly overdose patients turning down ambulance ride after naloxone. 2017;Available at: https://whyy.org/segments/philly-overdose-patients-turning-ambulance-ride-naloxone/. Accessed November 29, 2018, 2018.
- 35.Gokavi M Dayton police have revived one overdose patient 20 times. 2017;Available at: https://www.daytondailynews.com/news/crime--law/dayton-police-have-revived-one-overdose-patient-times/ZS7LRrdXlZ6K60sxlD61AO/. Accessed May 17, 2019. [Google Scholar]
- 36.Stoffers C Narcan: It Saves Lives. Does It Enable Addicts? 2015;Available at: https://www.themarshallproject.org/2015/08/14/narcan-it-saves-lives-does-it-enable-addicts. Accessed May 17, 2019.
- 37.Doleac J and Mukherjee A. The Moral Hazard of Lifesaving Innovations: Naloxone Access, Opioid Abuse, and Crime. Institute for the Study of Labor (IZA);2018. [Google Scholar]
- 38.Russell A and Anderson K. Narcan Saves Lives, But With Some Unintended Consequences. 2016;Available at: https://www.vpr.org/post/narcan-saves-lives-some-unintended-consequences#stream/0. Accessed May 17, 2019.
- 39.Morgan JR, Schackman BR, Weinstein ZM, Walley AY and Linas BP. Overdose following initiation of naltrexone and buprenorphine medication treatment for opioid use disorder in a United States commercially insured cohort. Drug Alcohol Depend. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rose AJ, McBain R, Schuler MS, et al. Effect of Age on Opioid Prescribing, Overdose, and Mortality in Massachusetts, 2011 to 2015. J Am Geriatr Soc. 2019;67(1):128–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.D’onofrio G, O’connor PG, Pantalon MV, et al. Emergency department–initiated buprenorphine/naloxone treatment for opioid dependence: a randomized clinical trial. JAMA. 2015;313(16):1636–1644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.U.S. Census Bureau. State Population Totals and Components of Change: 2010–2016. [Dataset]. 2017;Available at: https://www.census.gov/data/tables/2016/demo/popest/state-total.html. Accessed July 23, 2018, 2018.
- 43.Banta-Green CJ, Coffin PO, Schoeppe JA, Merrill JO, Whiteside LK and Ebersol AK. Heroin and pharmaceutical opioid overdose events: Emergency medical response characteristics. Drug Alcohol Depend. 2017;178:1–6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.