Abstract
Purpose:
Little is known about racial variations in the financial impact of cancer care. Using data from a national survey of racially diverse patients with metastatic breast cancer, we examined racial/ethnic patterns in employment and cost-management (i.e., financial coping) behaviors.
Methods:
We conducted an online survey of patients with metastatic breast cancer. Participants reported on socio-demographic characteristics, employment, and financial coping behaviors. We employed adjusted modified Poisson regressions to evaluate racial/ethnic differences in changes in work for pay and financial coping.
Results:
Our analysis included 1,052 respondents from 41 states, including Non-Hispanic Blacks (NHB, 9%), Hispanics (7%), Asians/Pacific Islanders/Native Hawaiians (API/NH, 10%), American Indians/Alaskan Natives (AI/AN, 8%), and Non-Hispanic Whites (NHW, 66%). In adjusted analyses comparing NHWs with patients of color, patients of color were more likely to take unpaid leave (NHB Adjusted Risk Ratio [ARR]=2.27; 95%CI=1.54, 3.34), take paid leave (Hispanic ARR=2.27; 95%CI=1.54, 1.29), stop work (AI/AN ARR=1.22; 95%CI=1.05, 1.41), and reduce work hours (AI/AN ARR=1.33; 95%CI=1.14, 1.57). Patients of color were more likely than NHWs to stop treatment (NHB ARR=1.22; 95%CI=1.08, 1.39), borrow money from friends/family (Hispanic ARR=1.75; 95%CI=1.25, 2.44), skip other medical bills (API/NH ARR=2.02; 95%CI=1.54, 2.63), and skip non-medical bills (AI/AN ARR=1.67 95%CI=1.06, 2.63). Non-Hispanic Whites more commonly reported using savings or skipping a vacation to help manage costs.
Conclusions:
Racial/ethnic differences exist in employment changes and financial coping among metastatic breast cancer patients, with patients of color experiencing worse consequences. Equity must be a guiding principle in strategies addressing financial burden during cancer care.
Keywords: breast neoplasms, employment, health equity, health care disparities, cost of cancer care, quality of life
Introduction
Breast cancer is the second leading cause of cancer-related death among women, with notable differences by race/ethnicity in breast cancer burden[1, 2]. For example, compared with White women, women of color are more likely to be diagnosed with metastatic breast cancer and die from the disease[3]. Such inequities in the distribution of metastatic disease are concerning, as they have negative financial implications for women whose treatment regimens may be more complex and costly due to indefinite treatment duration.
Financial toxicity, or the financial burden and distress that cancer patients experience, is now considered a significant adverse effect of cancer care[4], affecting more than 30% of cancer patients[5]. Financial toxicity has been linked to lower health-related quality of life and higher mortality among cancer patients [6, 7]. Moreover, patients reporting cancer-related financial burden are more likely to engage in cost-management (i.e., financial coping) behaviors, such as delaying/discontinuing treatment, forgoing medical care, and filing for bankruptcy[5, 8–10].
Although racial/ethnic disparities in financial barriers to care are well-documented[11], research on racial/ethnic differences in financial burden has been limited. One recent prospective cohort study of Black and White women with breast cancer found that compared with Whites, Black women were more likely to report income loss, health care-related financial barriers, health care-related transportation barriers, job loss, and loss of health insurance[12]. However, no study, to our knowledge has examined racial/ethnic differences in employment status and financial coping among women with incurable metastatic disease. Moreover, little is known regarding the extent of financial coping in less studied racially/ethnically diverse populations, including Hispanics/Latinas, Asians/Pacific Islanders, and American Indians/Alaskan Natives. Such understanding can help inform the development of future interventions aimed at addressing financial toxicity, with a bend towards equity.
Using data from a national survey of diverse patients with metastatic breast cancer, we examined racial/ethnic patterns in employment changes and financial coping due to cancer. Specifically, we assessed racial/ethnic differences in cancer-related changes in work for pay (e.g., work discontinuation, taking unpaid leave) and cost-management behaviors (e.g., treatment discontinuation, borrowing money, applying for financial assistance) among non-Hispanic Whites, non-Hispanic Blacks, Hispanics/Latinas, Asian/Pacific Islanders, and American Indians/Alaskan Natives.
Methods
Participants
Study participants were contacted through the Metastatic Breast Cancer Network via email and asked to complete a 20-minute online survey assessing their financial experiences with cancer care. Study participants provided written online, informed consent prior to initiating the survey. Participants who completed the survey were sent a $10 gift card. Over a two-week period, 1,691 responses were received. Individuals were removed if responses were duplicates (n=622; identified through the re-use of an email address or through exact matching responses across thirteen demographic variables- including both free-text and multiple-choice responses) or if a participant completed fewer than half of all survey items (n=17). A total of 1,052 unique individuals were included in analysis. This study was approved by the University of North Carolina at Chapel Hill Institutional Review Board.
Outcomes
Changes in Work for Pay.
To assess changes in work, we combined survey items from several prior studies that assessed changes in work status among cancer patients and survivors[9, 12–14]. Specifically, participants were asked, “Since being told you have metastatic or stage IV breast cancer, which changes, if any, have you made in your work for pay? (Select all that apply).” Participants could select multiple responses in eight dimensions including stopping work completely, reducing hours, taking paid leave, taking unpaid leave, retiring early, or changing jobs as a result of their cancer.
Financial Coping/Cost-Management Behaviors.
We define our financial coping measures according to the framework developed by Altice and colleagues, where cancer financial coping behaviors are defined as those behaviors that “patients adopt to manage their medical care while experiencing increased household expenses during/following cancer care”[15]. Consistent with the Altice and colleagues definition, we use the terms “financial coping” and “cost-management behaviors” interchangeably throughout this paper. To assess cost-management behaviors, we combined survey items from several prior studies that assessed financial coping behaviors among cancer patients and survivors[5, 13, 16, 17]. Specifically, we asked, “Which of the following have you done to manage the cost of your cancer? (Select all that apply).” Cost-management behaviors included discontinuing care due to cost, skipping vacations or other activities, withdrawing money from savings, filing for disability, avoiding treatment for other medical problems, skipping payment of non-medical bills, and applying for or receiving financial assistance.
Covariates
The primary variable of interest was race/ethnicity, as defined by self-report. Individuals could select more than one racial category but nearly all individuals identified as only one race. All those who identified as more than one race (n=3) identified as White and another race and were categorized into the non-White group. Individuals who identified as having Hispanic ethnicity are classified as “Hispanic” regardless of race- the majority of these individuals are White Hispanics (67%). The sample size was sufficient to report on non-Hispanic White, non-Hispanic Black, Hispanic, Asian/Pacific Islander/Native Hawaiian, and American Indian/Alaskan Native participants.
Control variables were divided into clinical characteristics and socioeconomic characteristics. Clinical variables included age at the time of the survey and years living with metastatic disease. Socioeconomic variables included insurance coverage (uninsured, private insurance, or public insurance), marital status, whether any dependents are present in the household, total household income, educational attainment (binary indicator of a two or four-year college degree vs. high school education or less), and whether women were employed at the time of the survey.
Statistical Analysis
First, we evaluated racial/ethnic differences in participant sociodemographic and clinical characteristics using chi-squared tests comparing each racial/ethnic group to non-Hispanic Whites. Next, we calculated unadjusted prevalence rates of each outcome by race, using chi-squared tests to report statistically significant differences between each racial/ethnic group and non-Hispanic Whites. Lastly, we estimated modified Poisson regressions predicting each outcome as a function of race/ethnicity (non-Hispanic Whites as reference group), adjusting for patient clinical and sociodemographic characteristics. Differences are presented as risk ratios and each group is compared to non-Hispanic Whites using a Wald test. Statistical tests were two-sided with significance assessed using an alpha value of .05. All analyses were performed using Stata 15 (College Station, Tx).
Results
Participant Characteristics
Survey participant characteristics are displayed in Table 1. The study sample included 66.0% non-Hispanic Whites, 9.0% non-Hispanic Blacks, 6.6% Hispanics, 10.1% Asians/Pacific Islanders/Native Hawaiians, and 8.3% American Indians/Alaskan Natives. Mean age for the sample was 42.3 years. Compared with all other racial/ethnic groups, non-Hispanic Whites were more likely to report living with metastatic breast cancer for less than a year, possessing insurance, and being married or living with a partner. Most participants reported having dependents (ranging from 87.5% of non-Hispanic Whites to 100.0% of American Indians/Alaskan Natives. Hispanics exhibited the lowest levels of income (68.1% reporting household incomes below $30,000) and education (79.7% reporting high school education or less). Non-Hispanic Blacks were most likely to be currently employed (93.7%).
Table 1:
Sample characteristics by race and ethnicity
| NH White | NH Black | p value | Hispanic | p value | Asian/PI | p value | American Indian/AN | p value | Overall | |
|---|---|---|---|---|---|---|---|---|---|---|
| N | 694 | 95 | 70 | 106 | 87 | 1052 | ||||
| Age, mean (SD) | 42.87 (9.68) | 44.38 (5.59) | 39.61 (7.66) | 43.41 (5.44) | 36.40 (7.58) | 42.31 (8.95) | ||||
| Years with metastatic disease | <.001 | <.001 | <.001 | <.001 | ||||||
| <1 year | 219 (31.6%) | 11 (11.6%) | 7 (10.1%) | 10 (9.4%) | 1 (1.1%) | 248 (23.6%) | ||||
| 1–2 years | 311 (44.8%) | 44 (46.3%) | 45 (65.2%) | 50 (47.2%) | 48 (55.2%) | 498 (47.4%) | ||||
| 2+ years | 164 (23.6%) | 40 (42.1%) | 17 (24.6%) | 46 (43.4%) | 38 (43.7%) | 305 (29.0%) | ||||
| Insurance Type | <.001 | <.001 | <.001 | <.001 | ||||||
| Uninsured | 121 (17.4%) | 72 (75.8%) | 27 (38.6%) | 77 (72.6%) | 19 (21.8%) | 316 (30.0%) | ||||
| Private | 363 (52.3%) | 17 (17.9%) | 37 (52.9%) | 8 (7.5%) | 1 (1.1%) | 426 (40.5%) | ||||
| Public | 210 (30.3%) | 6 (6.3%) | 6 (8.6%) | 21 (19.8%) | 67 (77.0%) | 310 (29.5%) | ||||
| Marital Status | <.001 | <.001 | <.001 | <.001 | ||||||
| Divorced/ Widowed/ Separated | 38 (5.5%) | 16 (16.8%) | 4 (5.8%) | 16 (15.1%) | 4 (4.6%) | 78 (7.4%) | ||||
| Married, living with a partner | 585 (84.5%) | 72 (75.8%) | 31 (44.9%) | 71 (67.0%) | 35 (40.2%) | 794 (75.7%) | ||||
| Never married | 69 (10.0%) | 7 (7.4%) | 34 (49.3%) | 19 (17.9%) | 48 (55.2%) | 177 (16.9%) | ||||
| Dependents | 0.04 | 0.20 | .001 | <.001 | 99 (9.4%) | |||||
| Yes | 607 (87.5%) | 90 (94.7%) | 64 (92.8%) | 104 (98.1%) | 87 (100.0%) | 952 (90.6%) | ||||
| Income Category | <.001 | <.001 | <.001 | <.001 | ||||||
| <15,000 | 27 (3.9%) | 6 (6.4%) | 8 (11.6%) | 7 (6.6%) | 3 (3.4%) | 51 (4.9%) | ||||
| 15,000–29,999 | 74 (10.8%) | 28 (29.8%) | 39 (56.5%) | 27 (25.5%) | 6 (6.9%) | 174 (16.7%) | ||||
| 30,000–49,999 | 429 (62.4%) | 42 (44.7%) | 17 (24.6%) | 39 (36.8%) | 25 (28.7%) | 552 (52.9%) | ||||
| 50,000 or more | 158 (23.0%) | 18 (19.1%) | 5 (7.2%) | 33 (31.1%) | 53 (60.9%) | 267 (25.6%) | ||||
| Education | <.001 | <.001 | <.001 | <.001 | ||||||
| High School or less | 429 (61.8%) | 58 (61.1%) | 55 (79.7%) | 33 (31.1%) | 33 (37.9%) | 608 (57.8%) | ||||
| College degree (2y or 4y) | 265 (38.2%) | 37 (38.9%) | 14 (20.3%) | 73 (68.9%) | 54 (62.1%) | 443 (42.2%) | ||||
| Working Currently | <.001 | 0.3 | <.001 | <.001 | ||||||
| Yes | 372 (53.8%) | 89 (93.7%) | 33 (47.1%) | 80 (75.5%) | 20 (23.0%) | 456 (43.4%) |
NH- Non-Hispanic; PI- Pacific Islander or Native Hawaiian; AN- Alaskan Native Differences from non-Hispanic White assessed using t-test or X2 test.
Unadjusted Comparisons
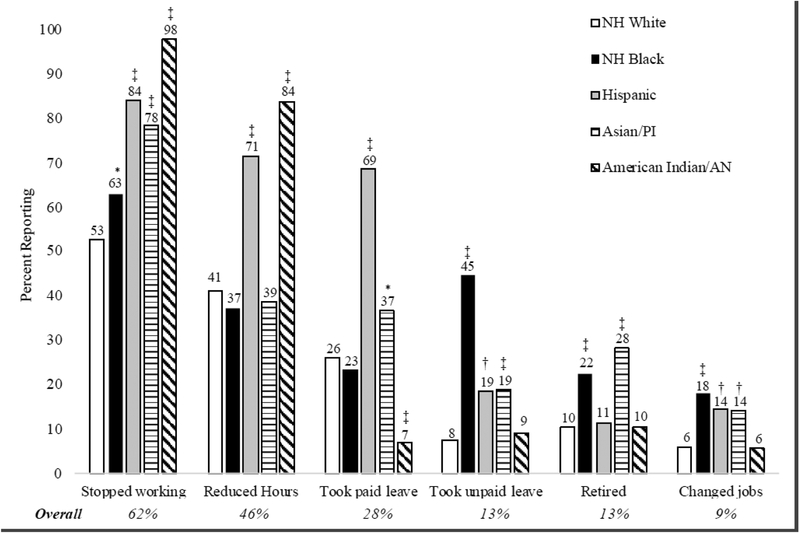
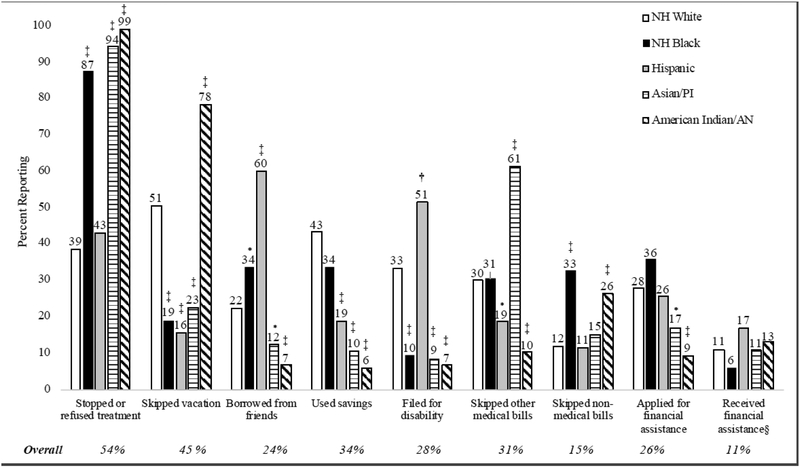
Figures 1 and 2 display unadjusted comparisons of outcomes (i.e., changes in work pay, Figure 1; and cost-management behaviors, Figure 2) by race/ethnicity, with non-Hispanic Whites as the reference group for chi-squared comparison tests. Regarding changes in work for pay (Figure 1: Changes in work for pay by race and ethnicity), stopping work completely was the most commonly reported change in work for pay across all racial/ethnic groups (62.3%), with participants of color reporting higher rates of work discontinuation relative to non-Hispanic Whites. Retiring early and changing jobs were least commonly reported across the entire sample (13.3%, 8.5% respectively), but relatively more common among participants of color than non-Hispanic Whites. With respect to cost-management behaviors (Figure 2: Cost-management behaviors by race and ethnicity), stopping or refusing treatment was the most commonly reported cost-management behavior for non-Hispanic Blacks (87.4%, statistically significantly higher than non-Hispanic Whites, 38.6%), Asians/Pacific Islanders/Native Hawaiians (94.3%, statistically significantly higher than non-Hispanic Whites), and American Indians/Alaskan Natives (98.9%, statistically significantly higher than non-Hispanic Whites), while borrowing money from friends was most commonly reported for Hispanics (60.0%, statistically significantly higher than non-Hispanic Whites, 22.2%), and skipping a vacation was the most commonly reported cost-management behavior for non-Hispanic Whites (50.6%, statistically significantly higher than non-Hispanic Blacks, 18.9%; Hispanics, 15.7%; Asians/Pacific Islanders/Native Hawaiians, 22.6%). Of note, very few participants applied for and received financial assistance for their cancer care (25.7% applied, of those 11.1% received assistance), with no statistically significant differences by race/ethnicity.
Figure 1: Changes in work for pay by race and ethnicity.
* p value <.05, † p value <.01, ‡ p value <.001
Differences from non-Hispanic White assessed using X2 test.
Figure 2: Cost-management behaviors by race and ethnicity.
* p value <.05, † p value <.01, ‡ p value <.001; încludes only those who applied for financial assistance (n=270)
Differences from non-Hispanic White assessed using X2 test
Adjusted Comparisons
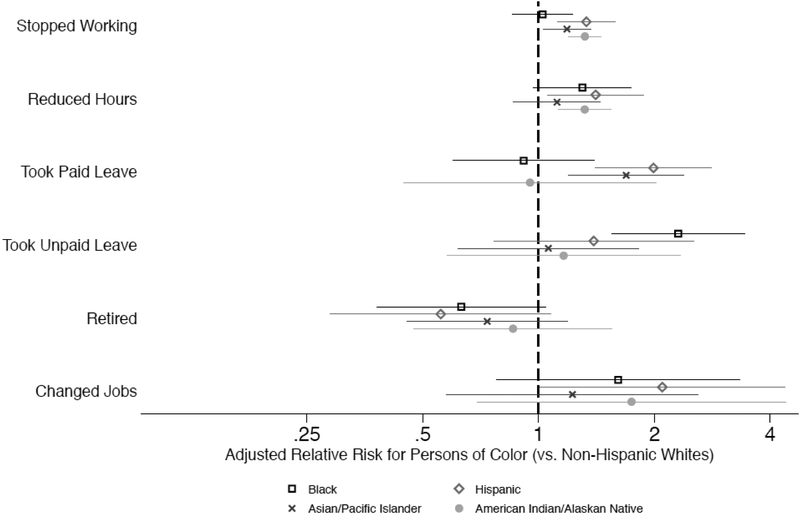
Results from the adjusted modified Poisson regression analyses are reported in Figures 3 and 4. In adjusted analyses comparing non-Hispanic Whites with non-Hispanic Blacks on changes in work for pay (Figure 3: Relative risk of changes in work for pay by race and ethnicity, adjusted; Supplemental Table 1), Blacks were more likely to report taking unpaid leave (ARR=2.31; 95%CI=1.55, 3.43). Of note, non-Hispanic Blacks exhibited the highest prevalence of unpaid leave in the entire sample (highest prevalence group, 44.7%; see Figure 1). Hispanics were more likely than Whites to report reducing work hours (ARR=1.41; 95%CI=1.05, 1.88), taking paid leave (ARR=1.99; 95%CI=1.40, 1.88); highest prevalence group, 68.6%), and changing jobs (ARR=2.10; 95%CI=1.01, 4.37). Asians/Pacific Islanders/Native Hawaiians were also more likely than non-Hispanic Whites to report stopping work (ARR=1.19; 95%CI=1.12, 1.58) and taking paid leave (ARR=1.69; 95%CI=1.19, 2.39). Moreover, compared with non-Hispanic Whites, American Indians/Alaskan Natives were more likely to report stopping work completely (ARR=1.32 95%CI=1.20, 1.46; highest prevalence group, 97.7%) and reducing work hours (ARR=1.32; 95%CI=1.13, 1.54; highest prevalence group, 83.9%).
Figure 3: Relative risk of changes in work for pay by race and ethnicity, adjusted.
Bars represent 95% confidence intervals; Analysis: Adjusted relative risk of each behavior relative to non-Hispanic Whites after adjusting for clinical characteristics (age, years with metastatic disease) and socioeconomic characteristics (insurance, marital status, dependents, household income, and education). Significance assessed using a Wald test.
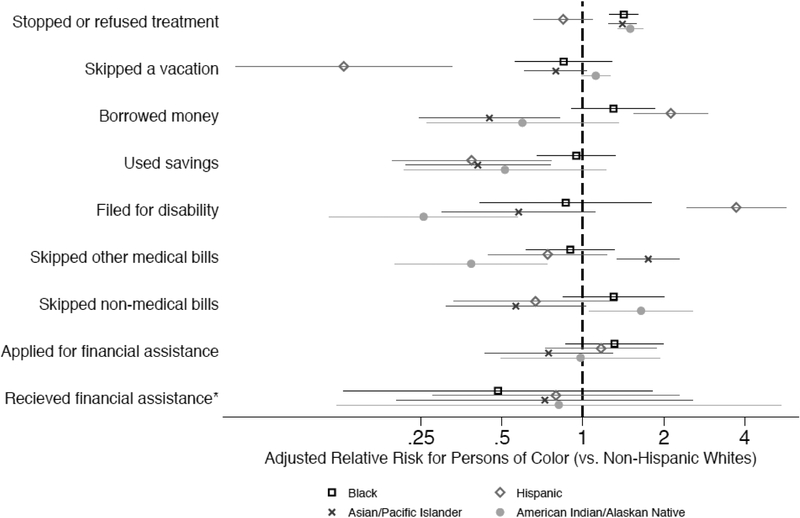
Figure 4: Relative risk of cost-management behaviors by race and ethnicity, adjusted.
*includes only those who applied for financial assistance (n=270)
Analysis: Adjusted relative risk of each behavior relative to non-Hispanic Whites after adjusting for clinical characteristics (age, years with metastatic disease) and socioeconomic characteristics (insurance, marital status, dependents, household income, education, and current work status). Significance assessed using a Wald test.
Racial/ethnic differences in cost-management behaviors were also observed in adjusted analyses (Figure 4: Relative risk of coping behaviors by race and ethnicity, adjusted; Supplemental Table 2). Specifically, non-Hispanic Blacks were more likely than non-Hispanic Whites to report stopping or refusing treatment (ARR=1.42; 95%CI=1.26, 1.61). Hispanics were more likely than Whites to report borrowing money from friends (ARR=2.12; 95%CI=1.55, 2.91; highest prevalence group, 60.0) and filing for disability (ARR=3.72; 95%CI=2.43, 5.69; highest prevalence group, 51.4%), but were less likely to report skipping a vacation (ARR=0.13; 95%CI=0.05, 0.33), and using savings (ARR=0.39; 95%CI=0.19, 0.76). Asians/Pacific Islanders/Native Hawaiians were more likely than non-Hispanic Whites to report stopping or refusing treatment (ARR=1.40; 95%CI=1.25, 1.58) and skipping other medical bills (ARR=1.75; 95%CI=1.34, 2.28; highest prevalence group, 61.3%), but less likely than non-Hispanic Whites to report borrowing money from friends (ARR=0.45; 95%CI=0.25, 0.82) and using savings (ARR=0.41; 95%CI=0.22, 0.76).
Finally, American Indians/Alaskan Natives were more likely than non-Hispanic Whites to report stopping or refusing treatment (ARR=1.50; 95%CI=1.34, 1.67; highest prevalence group, 98.9%), skipping a vacation (ARR=1.15; 95%CI=1.01, 1.31; highest prevalence group, 78.2%), and skipping non-medical bills (ARR=1.65 95%CI=1.05, 2.57. Yet, they were less likely than non-Hispanic Whites to report filing for disability (ARR=0.26; 95%CI=0.11, 0.57) and skipping other medical bills (ARR=0.38; 95%CI=0.20, 0.74) to cope with cancer care costs.
Discussion
Women with metastatic breast cancer experience a range of changes in work for pay and engage in a wide variety of cost-management strategies to cope with the costs of their cancer care. We observed racial/ethnic differences in the prevalence and types of work changes and cost-related coping behaviors reported by participants in our study. Specifically, women of color were more likely than their non-Hispanic White counterparts to report adverse changes in their employment status due to the burden of their cancer care (e.g., stopping work completely, reducing hours, taking unpaid leave). Furthermore, stopping/refusing treatment was the most commonly reported cost-management behavior among patients of color, while using savings and skipping a vacation were the most common financial coping practices reported among non-Hispanic Whites. These findings highlight the need for an equity prioritization lens in efforts aimed at addressing financial burden among cancer patients.
Higher prevalence of adverse changes in work for pay among women of color likely reflects racial/ethnic differences in the types of jobs held by persons of color relative to their White counterparts. National data indicate that, on average, Blacks and Hispanics are more likely than Whites to be employed in service, transportation, and manual labor positions, but less likely to hold management, professional, and related positions [18]. As such, racial/ethnic differences in employment categories have implications for racial variations in changes in work for pay, as individuals in service, transportation, and manual labor positions generally have less flexibility and autonomy in determining their work roles and schedules, as well as less job security, relative to persons employed in management/professional positions [19, 20]. Furthermore, given the persistent physical side effects of metastatic cancer treatment and the physical demands of many service, transportation, and manual labor positions, individuals in these positions may face additional barriers in performing their job duties that can affect job retention. More research is needed to further elucidate associations between race/ethnicity, job type, and changes in work for pay among cancer patients, as well as identify strategies for addressing the disproportionate burden of work discontinuation and other adverse effects of cancer treatment on employment among persons of color. Indeed, past research suggests that increasing employer support for employees with cancer, including accommodating alternative work schedules and responsibilities, is critical to work continuation and return[21]. Such practices are also consistent with employment-related non-discrimination policies, such as the American Disabilities Act, which requires employers to provide reasonable accommodations to employees or job applicants with a disability (e.g., cancer, mental impairment) [22]. Additionally, ensuring equitable access to physical and occupational therapy may help mitigate the abovementioned barriers to job performance and retention in patients of color. Similarly, early identification of individuals at high-risk of adverse work changes and creating systems of support for these individuals (e.g., early referrals to physical/occupational therapy, broad and equitable enforcement of employment-related non-discrimination policies for persons with disabilities), can help off-set the negative impact of cancer care on work status.
Racial/ethnic disparities in cancer patient survival are well-documented and partly attributable to racial/ethnic differences in treatment completion [23, 24]. In this study, treatment refusal/discontinuation was the most commonly reported cost-management behavior among patients of color, suggesting that financial burden, over and above socioeconomic status, is a potential key driver of racial/ethnic inequities in survival among metastatic breast cancer patients. As such, supportive cancer care services that address financial burden, particularly among patients of color, hold much promise for helping to mitigate racial/ethnic inequities in cancer care outcomes. Interestingly, very few patients in our study reported that they applied for and received financial assistance for their cancer treatment costs. In a recent study of oncology navigators’ perceptions of financial burden and financial assistance resources, our team identified several barriers to patients obtaining financial assistance, including lack of financial assistance resources at hospitals, limited knowledge about available resources, and complex/duplicative application processes [25]. Thus, to improve equitable access to financial assistance services, it will be important to establish systems within cancer hospitals that enhance transparency regarding available financial resources and coordination for patients seeking these resources.
It is also worth noting that the cost-management strategies most commonly reported among non-Hispanic Whites included using savings and skipping a vacation. Yet, most of the patients of color in this study were more likely to report other cost-management behaviors such as stopping/refusing treatment, borrowing money from friends, and skipping payments on non-medical bills. These racial/ethnic differences in the types of coping behaviors employed likely reflects broader national trends in wealth and access to economic reserves. For example, prior research has shown that for every dollar of wealth that Whites possess, Blacks have 6 cents and Latinos have 7 cents [26, 27]. These longstanding wealth inequalities need to be taken into account in broader discussions related to addressing financial toxicity, particularly among patients with metastatic disease who are more likely to face prolonged financial strain due to their ongoing need for cancer treatment.
There are limitations to this study that are worth noting. First, this study cohort is a convenience sample of patients with metastatic breast cancer who were members of a metastatic breast cancer support network and willing to complete an online survey. Thus, participants in this study may be a more engaged patient population and may differ from the broader population of patients with metastatic breast cancer in ways that are meaningful to our study outcomes. Consistent with this notion, we found that participants in this study were relatively younger (mean age = 43.2 years; median age = 44 years) than the general population of women living with metastatic breast cancer in the US [28]. Prior research suggests that younger and working-age cancer survivors are at great risk for financial burden [10, 29]. Thus, additional research is needed to assess racial/ethnic variations in financial coping across age subgroups of patients with metastatic breast cancer. Moreover, given our focus on metastatic breast cancer, findings from this study may not generalize to other cancer types or disease stages. Despite these limitations, this study has several strengths that make it a novel and important contribution to the literature, such as our large and racially/ethnically diverse sample that included understudied groups of patients of color (i.e., Asians/Pacific Islanders/Native Hawaiians, and American Indians/Alaskan Natives). Additionally, our intentional focus on patients with metastatic disease provides insight into the distinct financial challenges faced by a group of patients with indefinite treatment trajectories.
Conclusion
Women with metastatic breast cancer experience substantial financial burden as a result of their cancer treatment. Importantly, our study suggests that patients of color experience more adverse changes in work for pay and financial coping than their White counterparts. Given the negative impact of financial strain on patient well-being and treatment decision-making, as well as longstanding disparities in cancer outcomes, equity must be a guiding principle in strategies aimed at addressing financial toxicity in cancer patients.
Supplementary Material
Funding Sources
This work was supported by the National Comprehensive Cancer Network and Pfizer Independent Grants for Learning & Change (no grant number); and the National Cancer Institute (1 K01CA218473-01A1 to C.A.S).
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may differ from this version.
Conflicts of Interest
Ms. Sellers reports payment as a consultant with Pfizer which was unrelated to the submitted work. None of the other study authors have any conflicts of interest to disclose, beyond receiving independent grant funding from Pfizer.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Ethical Standards & Compliance
The experiments conducted in this study comply with the current laws of the country in which they were performed.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Contributor Information
Cleo A Samuel, Department of Health Policy and Management, Gillings School of Global Public Health and Lineberger Comprehensive Cancer Center, University of North Carolina, Chapel Hill, NC.
Jennifer C Spencer, Department of Health Policy and Management, Gillings School of Global Public Health, University of North Carolina, Chapel Hill, NC.
Donald L Rosenstein, Lineberger Comprehensive Cancer Center, University of North Carolina, Chapel Hill, NC.
Katherine E Reeder-Hayes, Lineberger Comprehensive Cancer Center, University of North Carolina, Chapel Hill, NC.
Michelle L Manning, Lineberger Comprehensive Cancer Center, University of North Carolina, Chapel Hill, NC.
Jean B Sellers, Lineberger Comprehensive Cancer Center, University of North Carolina, Chapel Hill, NC.
Stephanie B Wheeler, Department of Health Policy and Management, Gillings School of Global Public Health and Lineberger Comprehensive Cancer Center, University of North Carolina, Chapel Hill, NC.
References
- 1.Miller JW, Smith JL, Ryerson AB, et al. (2017) Disparities in breast cancer survival in the United States (2001–2009): Findings from the CONCORD-2 study. Cancer 123:5100–5118. 10.1002/cncr.30988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.DeSantis CE, Fedewa SA, Goding Sauer A, et al. (2016) Breast cancer statistics, 2015: Convergence of incidence rates between black and white women. CA Cancer J Clin 66:31–42. 10.3322/caac.21320 [DOI] [PubMed] [Google Scholar]
- 3.Iqbal J, Ginsburg O, Rochon PA, et al. (2015) Differences in Breast Cancer Stage at Diagnosis and Cancer-Specific Survival by Race and Ethnicity in the United States. JAMA 313:165 10.1001/jama.2014.17322 [DOI] [PubMed] [Google Scholar]
- 4.Zafar SY (2016) Financial Toxicity of Cancer Care: It’s Time to Intervene. J. Natl. Cancer Inst 108 [DOI] [PubMed] [Google Scholar]
- 5.Kent EE, Forsythe LP, Yabroff KR, et al. (2013) Are survivors who report cancer-related financial problems more likely to forgo or delay medical care? Cancer 119:. 10.1002/cncr.28262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lathan CS, Cronin A, Tucker-Seeley R, et al. (2016) Association of financial strain with symptom burden and quality of life for patients with lung or colorectal cancer. J Clin Oncol 34:1732–1740. 10.1200/JCO.2015.63.2232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zafar SY, McNeil RB, Thomas CM, et al. (2015) Population-based assessment of cancer survivors’ financial burden and quality of life: a prospective cohort study. J Oncol Pr 11:145–150. 10.1200/JOP.2014.001542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zafar SY, Peppercorn JM, Schrag D, et al. (2013) The Financial Toxicity of Cancer Treatment: A Pilot Study Assessing Out-of-Pocket Expenses and the Insured Cancer Patient’s Experience. Oncologist 18:381–390. 10.1634/theoncologist.2012-0279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yabroff KR, Dowling EC, Guy GP, et al. (2016) Financial hardship associated with cancer in the United States: Findings from a population-based sample of adult cancer survivors. J Clin Oncol. 10.1200/JCO.2015.62.0468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ramsey S, Blough D, Kirchhoff A, et al. (2013) Washington State cancer patients found to be at greater risk for bankruptcy than people without a cancer diagnosis. Heal Aff 32:1143–1152. 10.1377/hlthaff.2012.1263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clark CR, Ommerborn MJ, A. Coull B, et al. (2016) Income Inequities and Medicaid Expansion are Related to Racial and Ethnic Disparities in Delayed or Forgone Care Due to Cost. Med Care 54:555–561. 10.1097/MLR.0000000000000525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wheeler SB, Spencer JC, Pinheiro LC, et al. (2018) Financial impact of breast cancer in black versus white women. J Clin Oncol 36:1695–1701. 10.1200/JCO.2017.77.6310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jagsi R, Pottow JAE, Griffith KA, et al. (2014) Long-term financial burden of breast cancer: Experiences of a diverse cohort of survivors identified through population-based registries. J Clin Oncol. 10.1200/JCO.2013.53.0956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yousuf Zafar S, Peppercorn JM, Schrag D, et al. The Financial Toxicity of Cancer Treatment: A Pilot Study Assessing Out-of-Pocket Expenses and the Insured Cancer Patient’s Experience. 10.1634/theoncologist.2012-0279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Altice CK, Banegas MP, Tucker-Seeley RD, Yabroff KR (2017) Financial hardships experienced by cancer survivors: A systematic review. J. Natl. Cancer Inst 109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Irwin B, Kimmick G, Altomare I, et al. (2014) Patient experience and attitudes toward addressing the cost of breast cancer care. Oncologist 19:1135–1140. 10.1634/theoncologist.2014-0117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zafar SY, Peppercorn JM, Schrag D, et al. (2013) The financial toxicity of cancer treatment: a pilot study assessing out-of-pocket expenses and the insured cancer patient’s experience. Oncologist 18:381–390. 10.1634/theoncologist.2012-0279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.(2015) Labor force characteristics by race and ethnicity, 2014. US Bur Labor Stat [Google Scholar]
- 19.Swanberg JE, Pitt-Catsouphes M, Drescher-Burke K (2005) A question of justice : Disparities in employees’ access to flexible schedule arrangements. J Fam Issues 26:866–895. 10.1177/0192513X05277554 [DOI] [Google Scholar]
- 20.Jeszeck C (2015) Contingent Workforce: Size, Characteristics, Earnings, and Benefits (GAO-15–168R). Washington, DC [Google Scholar]
- 21.Spelten ER, Sprangers MAG, Verbeek JHA. (2002) Factors reported to influence the return to work of cancer survivors: a literature review. Psychooncology 11:124–131. 10.1002/pon.585 [DOI] [PubMed] [Google Scholar]
- 22.Disability Discrimination. In: US Equal Employ. Oppor. Commision https://www.eeoc.gov/laws/types/disability.cfm. Accessed 15 May 2019
- 23.Bickell NA, LePar F, Wang JJ, Leventhal H (2007) Lost opportunities: physicians’ reasons and disparities in breast cancer treatment. J Clin Oncol 25:2516–2521 [DOI] [PubMed] [Google Scholar]
- 24.Bickell NA (2002) Race, ethnicity, and disparities in breast cancer: victories and challenges. Women’s Heal Issues 12:238–251 [DOI] [PubMed] [Google Scholar]
- 25.Spencer JC, Samuel CA, Rosenstein DL, et al. (2018) Oncology navigators’ perceptions of cancer-related financial burden and financial assistance resources. Support Care Cancer 26:1315–1321. 10.1007/s00520-017-3958-3 [DOI] [PubMed] [Google Scholar]
- 26.(2014) Net Worth and Asset Ownership of Households: 2011 [Google Scholar]
- 27.Williams DR, Priest N, Anderson NB (2016) Understanding associations among race, socioeconomic status, and health: Patterns and prospects. Heal Psychol 35:407–411. 10.1037/hea0000242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen M-T, Sun H-F, Zhao Y, et al. (2017) Comparison of patterns and prognosis among distant metastatic breast cancer patients by age groups: a SEER population-based analysis. Sci Rep 7:9254 10.1038/s41598-017-10166-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Banegas MP, Guy GP, de Moor JS, et al. (2016) For Working-Age Cancer Survivors, Medical Debt And Bankruptcy Create Financial Hardships. Health Aff 35:54–61. 10.1377/hlthaff.2015.0830 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.