Abstract
Objectives:
Sense of community (SOC) is a comprehensive psychological assessment of the relationship between person and place and relates to positive psychological outcomes in community-living adults, but has not been tested in assisted living (AL). This study describes SOC, identifies associated factors, and explores the relationship between SOC and psychological well-being with a sample of AL residents.
Method:
Participants included 202 residents of 21 ALs. The Brief Sense of Community Scale, a multidimensional theory-based measure, assessed total SOC (Cronbach’s α = .87; M = 25.89, SD = 6.08) and dimensions of SOC (i.e. need fulfillment, group membership, influence, and emotional connection).
Results:
A second-order confirmatory factor analysis supported the multidimensional theoretical framework of SOC with the current sample. While bivariate correlations and multiple regressions varied by dimension, social relationships, physical health, and decisional control in the move to AL consistently yielded positive relationships with SOC factors. In the final step of a hierarchical multiple regression, total SOC significantly related to psychological well-being (F(1, 192) = 7.92, p = .005); although, its contribution was small (3%) when accounting for relevant covariates.
Conclusion:
Key findings suggest that the most accepted framework of SOC with community-living adults can be applied to the AL setting, but requires additional theoretical and empirical work. Findings also provide preliminary support for the relationship between SOC and psychological well-being. The authors discuss implications for future research and clinical practice, including strategies to promote SOC for AL residents.
Keywords: Assisted living, sense of community, person and place, psychological well-being, psychosocial wellness
Assisted living (AL) continues to grow as a popular residential care option for adults with health limitations (Wilson, 2007). Recent estimates suggest that, in the United States alone, over 733,000 residents live in 31,100 ALs (Khatutsky et al., 2016). The AL industry aims to deliver a psychosocial person-centered model of care that emphasizes psychological and social well-being (Kane, Chan, & Kane, 2007; Mollica, Houser, & Ujvari, 2012). Researchers and policymakers believe that a strong sense of community (SOC), built through frequent opportunities for social interactions and engagement, can promote a high quality of life for residents after relocation to AL (CEAL, 2010; Yee, Capitman, Leutz, & Sceigaj, 1999).
SOC is most often defined as, ‘a feeling that members have of belonging, a feeling that members matter to one another and to the group, and a shared faith that members’ needs will be met through their commitment to be together’ (McMillan & Chavis, 1986, p. 9). This theoretical construct is regarded as one of the most comprehensive psychological assessments of the relationship between person and place because it captures both socio-emotional and spatial components of a shared environment (Francis, Giles-Corti, Wood, & Knuiman, 2012; Peterson, Speer, & McMillan, 2008). The scope of SOC, coupled with the AL industry’s emphasis on community building and psychosocial well-being, make this construct particularly important to investigate in the AL setting. Despite its importance, SOC continues to receive little attention in the AL literature, and the relationship between SOC and psychological well-being has not yet been tested in a sample of AL residents. To address these limitations, this study aims to: (1) evaluate the application of an accepted theoretical model of SOC to AL residents; (2) identify environmental, individual, health, social, and relocation factors that relate with SOC; and (3) provide evidence for the preliminary impact of SOC on residents’ psychological well-being.
Definition and theoretical framework of SOC
Sarason (1974) introduced SOC as a foundational component of the psychological study of the connection between individuals and their socio-physical environment. In this seminal work, Sarason described SOC as a feeling associated with individual membership of a supportive and dependable social environment, and an integral aspect of personal and collective identity, bonding, and well-being. McMillan and Chavis (1986) proposed the most widely accepted definition and theoretical framework of SOC, which includes four dimensions capturing socio-emotional and spatial components of a shared environment:
need fulfillment (i.e. faith that the community will meet its members’ needs and values);
group membership (i.e. members experience sense of belonging, relatedness to others, and shared identity);
influence (i.e. individuals have power within the community and members are influenced through shared investment in supporting the community); and
emotional connection (i.e. members have strong inter-personal bonds, shared experiences, and attachment to place).
Based on this definition and framework, an AL resident with a strong SOC may experience person-environment fit and value-congruent care (i.e. need fulfillment), choice and control (i.e. influence), as well as positive regard for and meaningful connections with staff and other residents (i.e. emotional connection and group membership). Alternatively, a resident with poor SOC may experience poor care, loss of independence, and social isolation. Taken together, SOC is a psychological construct that assesses the connection between person and socio-physical environment, and encompasses many components of a positive resident experience in AL (CEAL, 2010; Cutler, 2007).
Factors associated with SOC
Previous studies identified multiple factors that relate to SOC with community-living adults, including the built environment (e.g. proximity to amenities and presence of public spaces), individual characteristics (e.g. demographics), and social factors (e.g. network size, social support, and social participation) (Francis et al., 2012; Long & Perkins, 2007; Prezza, Amici, Roberti, & Tedeschi, 2001). Social factors evidence consistently strong effects on SOC, whereas the effects of individual characteristics and the built environment on SOC depend more on the participant population and social environment. Given the higher likelihood of health limitations in older adulthood, previous research supports health as a population-specific factor that relates to SOC with older adults (Cramm & Nieboer, 2013; Tang, Chi, Xu, & Dong, 2018). However, the strength of relationships amongst these variables and SOC in AL has yet to be explored empirically.
Although SOC has not been measured directly in AL, previous research supports two distinct factors (i.e. organizational and relocation factors) that may relate to SOC in this setting, as evidenced by their relationships with other relevant constructs. Organizational factors (e.g. community type, payment structure, and size) related with social cohesion, homelikeness, and psychological well-being in AL (Mitchell & Kemp, 2000; Street, Burge, Quadagno, & Barrett, 2007; Street & Burge, 2012). Relocation factors (e.g. choice and control in the move and time in AL) related with homelikeness, place attachment, and psychological well-being in AL (Burge & Street, 2009; Cutchin, Owen, & Chang, 2003; Street & Burge, 2012). Overall, organizational and relocation factors may represent setting-specific factors that add to the built environment, individual characteristics, social factors, and health that are known to relate to SOC in community-living older adults, to help explain this construct in the AL setting.
SOC and psychological well-being
Among community-living older adults, a significant body of literature suggests that SOC significantly relates to psychological well-being, even after controlling for environmental, individual, social, and health variables (Pozzi, Marta, Marzana, Gozzoli, & Ruggieri, 2014; Sum, Mathews, Pourghasem, & Hughes, 2009; Tang et al., 2018; Zhang, Zhang, Zhou, & Yu, 2018). Possible mechanisms for the strong relationship between SOC and psychological well-being include positive outlook, valued roles, and emotional safety, as well as buffering stress (Boyd & Bright, 2007; Kobau et al., 2011; Pretty, Bishop, Fisher, & Sonn, 2006). In AL, a few studies found that constructs relevant to SOC also related to positive psychological outcomes. For example, sense of belonging negatively related with depression and loneliness (McLaren et al., 2013; Prieto-Flores et al., 2011), and resident influence positively related with facility satisfaction (Mitchell & Kemp, 2000). Taken together, a large body of literature suggests that SOC positively relates with psychological well-being, and there is some evidence to support the existence of this relationship in the AL setting.
Purpose
The purpose of this study is to investigate residentreported SOC in AL. Our first aim is to explore the application of the theoretical framework of SOC, as proposed by McMillan and Chavis (1986), to AL residents. Next, we will investigate associations between SOC and variables relevant to the AL setting, including: built environment, individual, social, health, organizational, and relocation factors. Lastly, we will test the relationship between SOC and psychological well-being. Even though cross-sectional data limits our ability to test directional models, results from this study will provide preliminary evidence for the strength of relationships between the targeted constructs, which can be explored further in future research.
Method
Participants
The current sample included 202 AL residents, aged 51 to 100 (M = 83.03, SD = 10.27). The majority were female (n = 144), White (n = 182), widowed (n = 119), and moved from a local residence (n = 123; i.e. a private home in the same county or independent living unit on the same campus). Participant demographics and health characteristics were consistent with national averages, except the current sample was more educated (67% with more than high school education) and included more residents that financed with Medicaid (30%) than national averages (Caffrey et al., 2012; Khatutsky et al., 2016). The 21 ALs from which the sample was recruited ranged in size from 16 to 104 residents (M = 54.19, SD = 25.07). Most ALs were chain operated (n = 11) and cost more than $3,000 per month (n = 16).
Measures
SOC
The Brief Sense of Community Scale (BSCS) measured SOC (Peterson et al., 2008). The BSCS includes two items for each dimension of SOC (8 total items): need fulfillment (e.g. ‘I can get what I need from [my current assisted living]’); group membership (e.g. ‘I feel like a member of the community at [my current assisted living]’); influence (e.g. ‘I have a say about what goes on at [my current assisted living]’); and emotional connection (e.g. ‘I have a good bond with others at [my current assisted living]’). Participants responded to items on a 5-point scale, 1 = Strongly Disagree, 5 = Strongly Agree. The BSCS evidenced reliability and convergent validity as a uni or multi-dimensional scale (Peterson et al., 2008). In the current sample, one item on the influence subscale (i.e. ‘People in [my current AL] are good at influencing each another’) was omitted for poor consistency with other items. Scores were summed to create a revised 7-item total scale (i.e. scores range from 5 to 35), as well as four subscales (i.e. scores range from 2 to 10, and 1 to 5 for influence); higher scores indicate greater SOC. Internal consistency with the sample was acceptable for total SOC (Cronbach’s α = .87), need fulfillment (Cronbach’s α = .90), group membership (Cronbach’s α = .72), and emotional connection subscales (Cronbach’s α = .77); internal consistency was not calculated for the one-item influence subscale. Confirmatory factor analysis (CFA) found that the four-factor structure was a good fit for the data (χ2(9) = 23.11, p = .006; χ2/df = 2.57; CFI = .98, TLI = .96, RMSEA = .09); factor loadings ranged from .70 to .91. Total SOC (p = .919) and subscales (p > .103) did not relate with social desirability, as measured by the Five-item Socially Desirable Response Set (Hays, Hayashi, & Stewart, 1989).
Environmental characteristics
Staff described the built environment, including the presence of: other levels of care, amenities within walking distance of the campus (i.e. that residents are allowed to go to without supervision), and common spaces; and reported organizational characteristics, including: ownership type, size, cost, and resident financing strategies (e.g. percent of private-pay beds).
Resident characteristics
Participants self-reported gender, age, education, relationship status, ethnicity, and Medicaid status.
Relocation factors
Residents responded to a single item assessing the degree of control in the decision to move to AL on a five-point scale, 1 = Little or None, 5 = A Lot (Davidson & O’Connor, 1990), and self-reported time in current AL and previous residence.
Health factors
The Physical Health subscale of the PROMIS Short-Form Global Health Scale measured physical health. This subscale contains four items assessing global physical health, functional ability, pain, and fatigue (Hays, Bjorner, Revicki, Spritzer, & Cella, 2009). Scores range from 4 to 20, higher scores indicate greater physical health. Internal consistency with the sample was acceptable (Cronbach’s α = .71).
The clock drawing test (CDT) assessed cognitive ability. The current study used the Cahn quantitative scoring method. Scores range from 0 to 10, higher scores indicate greater cognitive ability; scores below seven are consistent with impairment (Cahn et al., 1996). Using a subsample of 28 participants, inter-rater reliability was acceptable in the current study (ICC = .71, 95% CI = .48–.86, p < .001).
Participants also responded to items assessing vision (i.e. ‘How would you rate your eyesight, even when wearing glasses?’) and hearing (i.e. ‘How would you rate your hearing, even when wearing hearing aids?’) on five-point scales, 1 = Poor, 5 = Excellent. Items were summed (scores range from 2 to 10), higher scores indicate greater sensory ability.
Social factors
A modified version of the Lubben Social Network Scale (Lubben et al., 2006) measured social relationships with other residents, staff, and outside visitors (i.e. family and friends). Items assessed social network size, tangible support, and emotional support; the tangible support item was omitted from the staff subscale to avoid bias. Scores range from 0 to 15, and 0 to 10 for the staff subscale, higher scores indicate better relationships. Internal consistency for the sample was acceptable for the co-resident (Cronbach’s α = .83), staff-resident (Cronbach’s α = .74), and outside visitors (Cronbach’s α = .87) subscales. Participants also self-reported social activity attendance by indicating the percentage of programmed activity offerings they attended in the seven days prior to data collection.
Psychological well-being
The Mental Health subscale of the PROMIS measured psychological well-being. The scale contains four items assessing social function, satisfaction with social network, cognition, and mood (Hays et al., 2009). Scores range from 4 to 20, higher scores indicate greater psychological well-being. Internal consistency with the sample was acceptable (Cronbach’s α = .73).
Procedures
Multiple strategies were used to recruit a convenience sample of residents at the targeted ALs in Colorado, including: staff referrals, in-person announcements at activities, and snowball sampling. All resident interviews began with informed consent and a cognitive screen to determine eligibility. The current study used the following inclusion criteria: (a) age 50 or older; (b) able to speak and understand English; (c) functioned as own decision maker; and (d) score a five or above on the Memory Impairment Scale (Buschke et al., 1999). Of the 235 residents who volunteered, 33 were excluded based on criteria (i.e. three did not meet criterion a and 30 did not meet criterion d), yielding a sample of 202 participants.
Participants who met eligibility completed questionnaires containing study variables. The majority of questionnaires were administered one-to-one (n = 185; i.e. researcher read questions aloud and participants indicated responses on large-print laminate sheets); interviews typically lasted between 30 and 50 minutes. A small subsample (n = 17, 8%) completed questionnaires using alternative methods (i.e. group interviews or take-home copies of the survey). A series of one-way analysis of variance revealed no differences across administration method for study variables or social desirability.
Data preparation and statistical analyses
Missing data was only observed for the CDT (n = 17); a mean replacement was used in regression analyses. All other statistical assumptions were met. We computed descriptive statistics and psychometrics for each study variable. All statistical analyses were conducted using SPSS v.24 and AMOS v.24.
For the first aim, we conducted a second-order CFA to test the consistency of factor structures with the guiding theoretical framework of SOC. The following evaluated factor loadings (≥ .40) and model fit: relative chi-square (χ2/ DF) ≤ 3; comparative fit index (CFI) ≥ .90; Tucker-Lewis index (TLI) ≥ .90; and root mean square error of approximation (RMSEA) ≤ .10 (Garson, 2015; Matsunaga, 2010). For the second aim, we tested correlations amongst study variables; categorical variables were dummy-coded and tested with a point-biserial correlation. We then conducted a series of multiple linear regressions with SOC factors as dependent variables and factors that yielded significant bivariate correlations as independent variables. For the third aim, we conducted a hierarchical multiple regression with variables that yielded significant bivariate correlations with psychological well-being in the first step and SOC in the second step; psychological well-being was the dependent variable.
Results
Application of SOC in AL
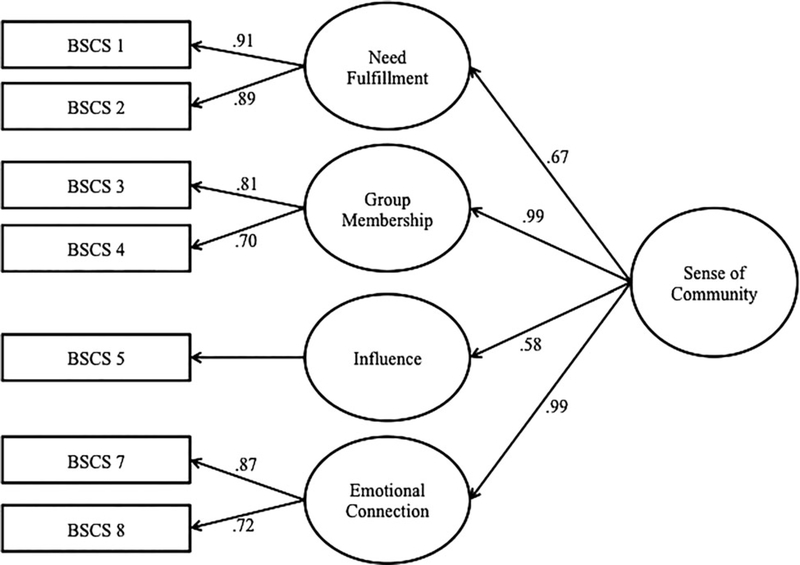
Participants’ total SOC ranged from 7 to 35 (M = 25.89, SD = 6.08). A second-order CFA tested if need fulfillment, membership, influence, and emotional connection represented a single underlying factor of SOC with the current sample; this theoretical model was a good fit for the data (χ2 (11) = 27.61, p = .004; χ2 /df = 2.51; CFI = .98, TLI = .96, RMSEA = .09), factors loadings ranged from .58 to .99, see Figure 1.
Figure 1.
Second-order confirmatory factor analysis of the BSCS with the current sample.
Factors associated with SOC
Correlations amongst SOC factors and environmental (i.e. built environment and organizational characteristics), individual, social, health, and relocation factors tested convergent validity, and provided insight into setting- and population-specific relationships with SOC in AL, see Table 1.
Table 1.
Study variables and relationships with SOC and psychological well-being.
| M or n | SD or % | Total SOC | NF | MB | IN | EC | PWB | |
|---|---|---|---|---|---|---|---|---|
| Built environment | ||||||||
| AL structure (stand-alone) | 100 | 50% | −.05 | −.10 | .01 | −.03 | −.04 | .01 |
| Close proximity to amenities (yes) | 157 | 78% | .13 | .13 | .12 | .05 | .11 | −.01 |
| Exercise facility (yes) | 92 | 48% | .02 | −.02 | −.01 | .18* | −.01 | .07 |
| Outdoor walking path (yes) | 147 | 73% | .09 | −.01 | .12 | .12 | .09 | .02 |
| Resident characteristics | ||||||||
| Age | 83.03 | 10.27 | .03 | .09 | .01 | .01 | −.02 | .07 |
| Gender (female) | 144 | 71% | −.01 | −.07 | .02 | −.05 | .05 | .04 |
| Education (more than high school) | 135 | 67% | −.13 | −.17* | −.06 | −.04 | −.14 | −.01 |
| Relationship status (married) | 28 | 14% | .07 | .03 | .06 | .05 | .10 | −.04 |
| Medicaid status (yes) | 61 | 30% | −.01 | −.07 | .01 | .06 | .03 | .02 |
| Social factors | ||||||||
| Co-resident relationships | 6.41 | 4.21 | .44*** | .22** | .37*** | .24** | .55*** | .28*** |
| Staff-resident relationships | 4.56 | 2.93 | .46*** | .28*** | .40*** | .28*** | .50*** | .25*** |
| Outside relationships | 8.48 | 3.72 | .28** | .21** | .25*** | .18* | .26*** | .30*** |
| Social activity attendance | 20.64% | 19.58 | .24** | .20** | .20** | .14 | .22** | .20** |
| Health factors | ||||||||
| Physical health | 12.83 | 2.92 | .23** | .21** | .17* | .12 | .21** | .47*** |
| Cognitive ability | 7.69 | 1.93 | .12 | .07 | .14 | .07 | .10 | .20** |
| Sensory ability | 5.75 | 1.84 | .11 | .08 | .07 | .02 | .15* | .33*** |
| Relocation factors | ||||||||
| Decisional control in the move | 3.12 | 1.53 | .28*** | .20** | .32*** | .20** | .19** | .17* |
| Months in AL | 21.17 | 20.44 | .03 | .03 | .04 | .01 | .02 | .07 |
| Previous residence (local) | 123 | 70% | −.01 | .01 | −.02 | .04 | −.03 | −.09 |
| Organizational characteristics | ||||||||
| Size | 57.37 | 24.06 | −.13 | −.17* | −.10 | −.09 | −.06 | .04 |
| Cost ($3,000+ per month) | 159 | 79% | .08 | .20** | −.02 | .07 | .01 | .02 |
| Ownership (chain operator) | 109 | 54% | −.04 | .08 | −.09 | −.07 | −.07 | .02 |
| Finance strategy (75%+ private-pay) | 140 | 69% | .03 | .11 | .01 | −.01 | −.02 | −.03 |
| Sense of community | 29.20 | 6.39 | ||||||
| Need fulfillment | 7.75 | 2.11 | .79*** | |||||
| Group membership | 7.57 | 2.10 | .88*** | .57*** | ||||
| Influence | 3.19 | 1.20 | .65*** | .35*** | .46*** | |||
| Emotional connection | 7.37 | 2.05 | .87*** | .53*** | .72*** | .53*** | ||
| Psychological well-being | 13.41 | 3.12 | .40*** | .30*** | .36*** | .23** | .36*** | |
Note. NF, need fulfillment; GM, group membership; IN, influence; EC, emotional connection; PWB, psychological well-being. Sample size is 202, except for correlation with cognitive ability (n = 185). Relationships were calculated with a Pearson r coefficient for continuous variables and a point-biserial correlation coefficient for continuous variables. Dummy-coded level is indicated in parentheses for continuous variables.
p < .05,
p < .01.
p < .001.
Environmental and individual characteristics yielded small and targeted relationships with specific dimensions of SOC. For example, only need fulfillment related with organizational characteristics, like size (r = −.17, p = .018) and cost (r = .20, p = .005).
Decisional control in the move related with total SOC (r = .28, p < .001), need fulfillment (r = .20, p = .006), group membership (r = .32, p < .001), influence (r = .20, p = .005), and emotional connection (r = .19, p = .006), all with small to moderate effect sizes. No other relocation factor yielded a significant relationship with SOC.
Physical health significantly related with total SOC (r = , p = .001), need fulfillment (r = .21, p = .002), group membership (r = .17, p = .014), and emotional connection (r = .21, p = .003) with small effect sizes. Sensory ability was the only other health factor to yield a significant relationship with an SOC factor (i.e. emotional connection).
Social factors yielded strong relationships with SOC factors. Total SOC related with co-resident (r = .44, p < .001), staff-resident (r = .46, p < .001), and outside (r = .28, p < .001) relationships, with moderate effect sizes. Co-resident (r = .22 to .55), staff-resident (r = .28 to .50), and outside relationships (r = .18 to .26) significantly related with all SOC subscale with small to large effect sizes. Social activity participation yielded small relationships with total SOC (r = , p = .001), need fulfillment (r = .20, p = .002), group membership (r = .20, p = .005), and emotional connection (r = .22, p = .002), but not influence.
Multiple regressions provided insight into the amount of shared variance variables that yielded significant relationships accounted for in SOC factors. Collinearity diagnostics were calculated with a Variance Inflation Factor (VIF); across all regressions, VIF for independent variables ranged from 1.01 to 1.88 (no multicollinearity). Independent variables explained 35% of variance in total SOC (F(6, 195) = 17.51, p < .001); 25% of variance in need fulfillment (F(9, 192) = 7.13, p < .001); 29% of variance in group membership (F(6, 195) = 13.38, p < .001); 15% of variance in influence (F(5, 196) = 6.71, p < .001), and 39% of variance in emotional connection (F(7, 194) = 17.45, p < .001), see Table 2.
Table 2.
Multivariate regression on total SOC and subscales.
| Independent variable | Total SOC | NF | GM | IN | EC |
|---|---|---|---|---|---|
| Exercise facility | .15* | ||||
| More than HS education | −.14* | ||||
| Co-resident relationships | .17* | .03 | .12 | .36*** | |
| Staff-resident relationships | .28*** | .21* | .25** | .20* | .23** |
| Outside relationships | .12* | .09 | .11 | .09 | .08 |
| Activity attendance | .09 | .08 | .08 | .02 | |
| Physical health | .14* | .11* | .10 | .07 | .14* |
| Sensory ability | −.06 | ||||
| AL size | −.13* | ||||
| AL cost ($3,000+) | .21** | ||||
| Decisional control in the move | .23*** | .22** | .28*** | .15* | .14* |
Note. NF, need fulfillment; GM, group membership; IN, influence; EC, emotional connection. Statistics are standardized regression weights (β).
p < .05.
p < .01.
p < .001.
SOC and psychological well-being
A hierarchical multiple regression tested the relationship between SOC and psychological well-being after accounting for relevant covariates. To test if SOC accounted for unique variance in psychological well-being, we entered social, health, and relocation factors that yielded significant relationships with psychological well-being in the first step, and SOC in the second step. Due to concerns with Collinearity amongst SOC subscales, we entered total SOC, rather than subscales, in the second step. VIF for independent variables were less than 1.88 at each block (no multicollinearity). In step 1, relocation, health, and social factors accounted for 37% of variance in psychological well-being (F(8, 193) = 14.06, p < .001). In the second step, SOC accounted for an additional 3% of variance (F(1, 192) = 7.92, p = .005). Overall, the model explained 40% of variance in psychological well-being (F(9, 192) = 13.81, p < .001); physical health (β = .35, p < .001), sensory ability (β = .17, p = .006), cognitive ability (β = .12, p = .045), outside relationships (β = .14, p = .024), and SOC (β = .20, p = .005) significantly related to psychological well-being, see Table 3.
Table 3.
Hierarchical regression on psychological well-being.
| Variable | Step 1 | Step 2 |
|---|---|---|
| Decisional control in the move | .09 | .05 |
| Physical health | .38*** | .35*** |
| Sensory ability | .16* | .17** |
| Cognitive ability | .12* | .12* |
| Co-resident relationships | .11 | .07 |
| Staff-resident relationships | .04 | −.01 |
| Outside relationships | .16** | .14* |
| Social activity attendance | .05 | .03 |
| SOC | .20** | |
Note. Statistics are standardized regression weights (β).
p < .05.
p < .01.
p < .001.
Discussion
This study presents several important findings that contribute to the understanding of SOC in AL, and the relationship between SOC and psychological well-being after relocation. Factor structures supported the application of McMillan and Chavis’s theoretical framework of SOC to AL residents in the current sample. In general, SOC related with previously established (i.e. social factors and physical health) and AL-specific (i.e. decisional control in the move) factors, but not fixed factors like environmental or individual characteristics. Social relationships related selectively across dimensions of SOC, providing insight into the various components of the AL social environment that relate to structural and socio-emotional aspects of SOC. After accounting for relocation, health, and social factors, SOC only contributed a modest amount to explaining psychological well-being. Collectively, these findings highlight the importance of social, health, and relocation factors for SOC amongst AL residents, and provide preliminary support for the role of SOC in explaining resident psychological well-being. Yet, there is a need for future theoretical and empirical development of SOC specific to AL.
SOC in AL and associated factors
The multidimensional theory-based measure used in the current study evidenced acceptable reliability, and factor structures were consistent with the targeted theoretical framework of SOC for the current sample of AL residents. In addition, significant relationships amongst SOC factors and social relationships, social activity, and physical health provided evidence of construct validity with the current sample. Collectively, these finding suggest the measure and theoretical model used in this study are applicable to the AL setting. It should be noted that one item on the BSCS was omitted from the current study due to poor psychometric properties (i.e. ‘People at [my current AL] are good at influencing each another’). This finding likely relates to low rates of conformity in older adulthood (Pasupathi, 1999), and suggests the need for future research to consider the role of conformity in SOC with older adults. Alternatively, residents in this study may have rated this item inconsistently due to wording that did not identify the source of influence. In AL, there are multiple social ecologies (e.g. residents, family, staff, and administration) with varying degrees of power to influence the community. In the current study, we kept wording consistent with the original BSCS scale, but future research on SOC in AL may choose to consider capturing social ecologies separately (e.g. ‘Staff at my AL are good at influencing residents’). Overall, additional theoretical development is needed on SOC in AL that addresses issues specific to the population (e.g. low conformity in older adulthood) and social environment (e.g. multiple social ecologies in AL).
Dimensions of SOC evidenced varying strengths of correlations with built environment, individual, social, health, organizational, and relocation factors. These findings provide insight into the roles of each dimension in contributing to overall SOC in AL. For example, only need fulfillment related with organizational variables. Specifically, residents in our study that lived in smaller or more expensive ALs reported greater faith that their community would meet individual needs and support personal values. These findings suggest that select organizational factors may relate with the perception of provision of care in AL, which was captured by spatial dimensions of SOC (i.e. need fulfillment). Findings also suggest that socioemotional-focused dimensions of SOC (i.e. group membership and emotional connection) may capture individual and inter-personal components of the AL setting.
While co-resident and staff-resident relationships yielded significant correlations with all dimensions of SOC, these relationships varied in multivariate models. Specifically, staff-resident relationships was a significant predictor of all dimensions of SOC, but co-resident relationships only significantly related to emotional connection in a multivariate regression. It is possible that because residents are mostly of the same age and social ecological level, co-resident relationships are a source of emotional intimacy primarily through shared experiences of life stage and being an AL resident. For the most part, staff and residents differ in age, role, and social ecological level in AL; therefore, because residents and staff are connected mostly through place, these relationships may be particularly important for building components of SOC in AL (e.g. promoting needs and values, feeling a part of the whole community, and intimacy with a range of individuals). Interesting areas of future research might include testing the impact of peer versus intergenerational relationships on SOC, and exploring the meaning of shared experiences of aging and relocation to AL for peer bonding in this setting.
Decisional control in the move to AL significantly related with each dimension of SOC in the current study. Relocation factors may be particularly salient to the resident experience in AL, as the move to AL is often precipitated by cumulative losses and-or a major life event (e.g. hospitalization) and the move itself involves various losses (e.g. previous residence, relationships, and roles) (Chen et al., 2008; Seipke, 2008; Soöderberg, Ståhl, & Emilsson, 2012). Therefore, future research targeting constructs that attempt to capture the psychosocial experience of AL residents, like SOC, should consider the context of the move to AL, as this may shape the psychosocial experience of residents after relocation.
SOC and psychological well-being
Total SOC along with social, health, and relocation factors explained 40% of variance in psychological well-being, yet SOC only accounted for 3% of unique variance. The strong effect of the combination of these factors on psychological well-being is consistent with previous research and high-lights the importance of social and health factors for the psychological well-being of AL residents (Jang, Park, Dominguez, & Molinari 2014). The significance of SOC in the second step of the regression model suggests that SOC is associated with slightly better psychological well-being of AL residents after controlling for health (i.e. physical, cognitive, or sensory health) and relationships. Therefore, our findings provide preliminary empirical support for the positive relationship between SOC and psychological well-being with AL residents. Future longitudinal research is needed to confirm the impact of SOC on psychological well-being in AL, as cross-sectional data does not allow us to comment on direction.
Theoretical and research implications
Results suggest that SOC, as defined in the current study, warrants additional theoretical and empirical work in AL. While our findings support the merit of using McMillan and Chavis’s framework in future AL research, future scholars should address measurement issues related to the concept of conformity within the influence dimension of this framework. In addition, the multiple social ecological levels (i.e. residents, family, staff, and administration) that exist in AL need to be investigated separately in order to determine whether there exists invariance in conceptual understanding and measurement of SOC, especially as each of these ecologies likely have varying levels of power within the community. It is also likely that most AL community members have multiple community affiliations, which may influence SOC and its relationship to psychological well-being. For example, a resident that regularly attends religious gatherings in their previous neighborhood may report lower SOC in AL, but derive psychosocial benefits from other community affiliations. Taken together, future research is needed to develop more sophisticated models and measurements of SOC in AL that consider social ecological levels within AL (e.g. resident, family, staff, or administration), personal contexts of AL (e.g. workplace, home, or home of a loved one), and multiple community affiliations.
Clinical implications
Results from the current study may inform future interventions and clinical practices in AL aimed at promoting resident SOC. Empowering community members is a core component of building community (Minkler, Wallerstein, & Wilson, 2008). Future research is needed to investigate mechanisms to empower residents in AL (e.g. increased roles within the community), and the impact of these mechanisms on SOC and psychosocial well-being. Community building interventions may also choose to focus on promoting relationships amongst residents, staff, and outside family members and friends, with a particular emphasis on staff-resident relationships. Potential strategies for cultivating these relationships might include community events (e.g. barbeques with residents, families and friends, and staff and their families), initiatives with shared goals amongst residents and staff (e.g. reduce total waste in the AL), or highlighting appropriate personal information about community members (e.g. staff spotlights). Our findings suggest that the aforementioned interventions may be particularly important to consider for residents with health limitations.
Decisional control in the move was a setting-specific factor that significantly related with total SOC and each dimension of SOC in the current sample. Future research is needed to investigate best practices for involving potential residents in the relocation process including: incorporating personal preferences, offering choices, and delegating tasks. In other fields, decisional control is enhanced by motivational interviewing skills (Rollnick & Miller, 1995), which might be a useful intervention strategy with potential residents of AL. The goals of these strategies are to increase the likelihood that residents will incorporate choice, control, and rationale in their relocation process and narrative. Strategies are also needed for reducing the impact of perceived lack of control after relocation (see Morgan & Brazda, 2013).
Limitations
Limitations of the current study include convenience sampling, which may have biased our sample toward residents with higher SOC. This study also sampled ALs in the same geographic region, which may limit generalizability. In addition, as mentioned, we omitted an item from the influence subscale of the BSCS due to poor contributions to internal consistency, and, thus, assessed influence with a single item targeting members’ power within the community. Therefore, we did not capture the full construct of influence and results with this subscale should be interpreted with caution.
Cross-sectional methods limit causal inferences about the relationships identified in this study. There are also additional variables that relate with SOC in AL that were not included in the current study, including, but not limited to, the use of public spaces, attitudes toward administration, and attachment to previous residences. Lastly, there may be overlap between constructs like SOC, psychological well-being, and adaptation. While these constructs differ theoretically, lay definitions amongst AL residents may not differ. Most factors that related with SOC in the current study also related with psychological well-being, and are consistent with correlates of adaptation to AL identified in previous research (Brownie, Horstmanshof, & Garbutt, 2014). Future research is needed to investigate the overlap between these constructs in AL to ensure they are capturing different components of the AL experience and different variance in statistical analyses.
Conclusion
Despite the aforementioned limitations, to the knowledge of the authors, this study is the first to apply McMillan and Chavis’s theoretical framework of SOC to a sample of AL residents. Key findings suggest that the factor structure of the targeted framework is applicable to the AL setting, but requires additional theoretical and empirical work to improve measurement and setting-specific models. Future research is also needed to test directional models of SOC and psychological well-being. Results from this study also have implications for care and operations in AL, as administrators and staff may consider ways to promote SOC after relocation, particularly for residents with health limitations.
Funding
This work was supported in part by a training grant from the National Institute on Aging, award number T32AG044296.
References
- Boyd NM, & Bright DS (2007). Appreciative inquiry as a mode of action research for community psychology. Journal of Community Psychology, 35(8), 1019–1036. [Google Scholar]
- Brownie S, Horstmanshof L, & Garbutt R. (2014). Factors that impact residents’ transition and psychological adjustment to long-term aged care: A systematic literature review. International Journal of Nursing Studies, 51(12), 1654–1666. [DOI] [PubMed] [Google Scholar]
- Burge S, & Street D. (2009). Advantage and choice: Social relationships and staff assistance in assisted living. Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 65, 358–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buschke H, Kuslansky G, Katz M, Stewart WF, Sliwinski MJ, Eckholdt HM, & Lipton RB (1999). Screening for dementia with the memory impairment screen. Neurology, 52, 231–231. [DOI] [PubMed] [Google Scholar]
- Caffrey C, Sengupta M, Park-Lee E, Moss A, Rosenoff E, & Harris-Kojetin L. (2012). Residents living in residential care facilities: United States, 2010 (NCHS Data Brief No. 91). Hyattsville, MD: National Center for Health Statistics. [PubMed] [Google Scholar]
- Cahn DA, Salmon DP, Monsch AU, Butters N, Wiederholt WC, Corey-Bloom J, & Barrett-Connor E. (1996). Screening for dementia of the Alzheimer type in the community: The utility of the Clock Drawing Test. Archives of Clinical Neuropsychology, 11(6), 529–539. [PubMed] [Google Scholar]
- Center for Excellence in Assisted Living (CEAL). (2010). Person-centered care in assisted living: An informational guide. Retrieved from www.theceal.org/…/k2/…/197_9dbab55605eb0a9d547b29d1fd84fb5e
- Chen SL, Brown JW, Mefford LC, de La Roche A, McLain AM, Haun MW, & Persell DJ (2008). Elders’ decisions to enter assisted living facilities: A grounded theory study. Journal of Housing for the Elderly, 22(1–2), 86–103. [Google Scholar]
- Cramm JM, & Nieboer AP (2013). Relationships between frailty, neighborhood security, social cohesion and sense of belonging among community-dwelling older people. Geriatrics & Gerontology International, 13, 759–763. [DOI] [PubMed] [Google Scholar]
- Cutchin MP, Owen SV, & Chang PFJ (2003). Becoming “at home” in assisted living residences: Exploring place integration processes. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 58(4), S234–S243. [DOI] [PubMed] [Google Scholar]
- Cutler LJ (2007). Physical environments of assisted living: Research needs and challenges. The Gerontologist, 47(suppl 1), 68–82. [DOI] [PubMed] [Google Scholar]
- Davidson HA, & O’Connor BP (1990). Perceived control and acceptance of the decision to enter a nursing home as predictors of adjustment. The International Journal of Aging and Human Development, 31(4), 307–318. [DOI] [PubMed] [Google Scholar]
- Francis J, Giles-Corti B, Wood L, & Knuiman M. (2012). Creating sense of community: The role of public space. Journal of Environmental Psychology, 32(4), 401–409. [Google Scholar]
- Garson GD (2015). Structural equation modeling. Asheboro, NC: Statistical Associates Publishing; Retrieved from http://www.statisticalassociates.com/sem_p.pdf [Google Scholar]
- Hays RD, Bjorner JB, Revicki DA, Spritzer KL, & Cella D. (2009).Development of physical and mental health summary scores from the patient-reported outcomes measurement information system (PROMIS) global items. Quality of Life Research, 18(7), 873–880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hays RD, Hayashi T, & Stewart AL (1989). A five-item measure of socially desirable response set. Educational and Psychological Measurement, 49(3), 629–636. [Google Scholar]
- Jang Y, Park NS, Dominguez DD, & Molinari V. (2014). Social engagement in older residents of assisted living facilities. Aging & Mental Health, 18, 642–647. [DOI] [PubMed] [Google Scholar]
- Kane RA, Chan J, & Kane RL (2007). Assisted living literature through May 2004: Taking stock. The Gerontologist, 47(suppl 1), 125–140. [DOI] [PubMed] [Google Scholar]
- Khatutsky G, Ormond C, Wiener JM, Greene AM, Johnson R,Jessup EA, & Harris-Kojetin L. (2016). Residential care communities and their residents in 2010: A national portrait (DHHS Publication No. 2016–1041). Hyattsville, MD: National Center for Health Statistics. [Google Scholar]
- Kobau R, Seligman ME, Peterson C, Diener E, Zack MM, Chapman D, & Thompson W. (2011). Mental health promotion in public health: Perspectives and strategies from positive psychology. American Journal of Public Health, 101(8), e1–e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long DA, & Perkins DD (2007). Community social and place predictors of sense of community: A multilevel and longitudinal analysis. Journal of Community Psychology, 35(5), 563–581. [Google Scholar]
- Lubben J, Blozik E, Gillmann G, Iliffe S, von Renteln Kruse W, Beck JC, & Stuck AE (2006). Performance of an abbreviated version of the Lubben Social Network Scale among three European community-dwelling older adult populations. The Gerontologist, 46(4), 503–513. [DOI] [PubMed] [Google Scholar]
- Matsunaga M. (2010). How to factor-analyze your data right: Do’s, don’ts, and how-to’s. International Journal of Psychological Research, 3(1), 97–110. [Google Scholar]
- McLaren S, Turner J, Gomez R, McLachlan AJ, & Gibbs PM (2013). Housing type and depressive symptoms among older adults: A test of sense of belonging as a mediating and moderating variable. Aging & Mental Health, 17, 1023–1029. [DOI] [PubMed] [Google Scholar]
- McMillan DW, & Chavis DM (1986). Sense of community: A definition and theory. Journal of Community Psychology, 14(1), 6–23. [Google Scholar]
- Minkler M, Wallerstein N, & Wilson N. (2008). Improving health through community organization and community building In Glanz K, Rimer BK, & Viswanath K. (Eds.) Health behavior and health education: Theory, research and practice (4th ed., pp. 287–312). San Francisco, CA: Jossey-Bass, Inc. [Google Scholar]
- Mitchell JM, & Kemp BJ (2000). QoL in assisted living homes: A multidimensional analysis. The Journals of Gerontology Series B: Psychological Sciences & Social Sciences, 55, P117–P127. [DOI] [PubMed] [Google Scholar]
- Mollica RL, Houser AN, & Ujvari K. (2012). Assisted living and residential care in the states in 2010. Washington, DC: AARP Public Policy Institute. [Google Scholar]
- Morgan LA, & Brazda MA (2013). Transferring control to others: Process and meaning for older adults in assisted living. Journal of Applied Gerontology, 32(6), 651–668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasupathi M. (1999). Age differences in response to conformity pressure for emotional and nonemotional material. Psychology and Aging, 14(1), 170–174. [DOI] [PubMed] [Google Scholar]
- Peterson NA, Speer PW, & McMillan DW (2008). Validation of a brief sense of community scale: Confirmation of the principal theory of sense of community. Journal of Community Psychology, 36(1), 61–73. [Google Scholar]
- Pozzi M, Marta E, Marzana D, Gozzoli C, & Ruggieri RA (2014). The effect of the psychological sense of community on the psychological well-being in older volunteers. Europe’s Journal of Psychology, 10(4), 598–612. [Google Scholar]
- Prieto-Flores ME, Fernandez-Mayoralas G, Forjaz MJ, Rojo-Perez F, & Martinez-Martin P. (2011). Residential satisfaction, sense of belonging and loneliness among older adults living in the community and in care facilities. Health & Place, 17, 1183–1190. [DOI] [PubMed] [Google Scholar]
- Prezza M, Amici M, Roberti T, & Tedeschi G. (2001). Sense of community referred to the whole town: Its relations with neighboring, loneliness, life satisfaction, and area of residence. Journal of Community Psychology, 29(1), 29–52. [Google Scholar]
- Rollnick S, & Miller WR (1995). What is motivational interviewing? Behavioural and Cognitive Psychotherapy, 23(4), 325–334. [DOI] [PubMed] [Google Scholar]
- Sarason SB (1974). The psychological sense of community: Prospects for a community psychology. San Francisco, CA: Jossey-Bass, Inc. [Google Scholar]
- Seipke HL (2008). Assisted living, elderly women and sense of self: Communicating the impact of reduction of long-standing activities. Journal of Women & Aging, 20, 131–148. [DOI] [PubMed] [Google Scholar]
- Söoderberg M, Ståhl A, & Emilsson UM (2012). Family members’ strategies when their elderly relatives consider relocation to a residential home—Adapting, representing and avoiding. Journal of Aging Studies, 26(4), 495–503. [DOI] [PubMed] [Google Scholar]
- Street D, & Burge SW (2012). Residential context, social relationships, and subjective well-being in assisted living. Research on Aging, 34(3), 365–394. [Google Scholar]
- Street D, Burge S, Quadagno J, & Barrett A. (2007). The salience of social relationships for resident well-being in assisted living. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 62(2), S129–S134. [DOI] [PubMed] [Google Scholar]
- Sum S, Mathews RM, Pourghasem M, & Hughes I. (2009). Internet use as a predictor of sense of community in older people. Cyberpsychology & Behavior, 12, 235–239. [DOI] [PubMed] [Google Scholar]
- Tang F, Chi I, Xu L, & Dong X. (2018). Exploring relationships of psychological sense of community with self-rated health and depressive symptoms among older Chinese Americans. Gerontology and Geriatric Medicine, 4, 2333721418778183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson KB (2007). Historical evolution of assisted living in the United States, 1979 to the present. The Gerontologist, 47, 8–22. [DOI] [PubMed] [Google Scholar]
- Yee DL, Capitman JA, Leutz WN, & Sceigaj M. (1999). Resident-centered care in assisted living. Journal of Aging & Social Policy, 10, 7–26. [DOI] [PubMed] [Google Scholar]
- Zhang J, Zhang J, Zhou M, & Yu NX (2018). Neighborhood characteristics and older adults’ well-being: The roles of sense of community and personal resilience. Social Indicators Research, 137(3), 949–963. [Google Scholar]