Abstract
The Bernese periacetabular osteotomy (PAO) is a well-established procedure for the management of symptomatic hip dysplasia. The associated Smith–Petersen exposure offers excellent visualization of the acetabulum and control of acetabular osteotomy and mobilization. The traditional exposure of the true pelvis involves osteotomy of the iliac wing in order to mobilize the sartorial and inguinal ligament insertion. However, full osteotomy of the iliac spine may necessitate screw fixation if a relatively large segment of bone is included. A known complication with screw fixation of the iliac wing osteotomy involves failure of fixation and screw back out. Moreover, the screw may irritate the patient even in the setting of adequate fixation. A larger osteotomy may also injure the lateral femoral cutaneous nerve (LFCN) as it travels near the anterior–superior spine. To minimize the risk of these potential complications, a wafer osteotomy may be used to develop a sleeve of tissue involving the sartorial insertion. This sleeve also mobilizes the entirety of the LFCN medially and affords protection throughout the procedure. Furthermore, the wafer osteotomy may be re-fixed to the stable pelvis during closure with simple heavy suture fixation alone, avoiding screw insertion or associated removal. Because only a wafer or bone is taken during the spine osteotomy, more bone is available at the anterior–superior iliac spine for fixation of the mobile fragment after repositioning. In this technical note, we describe the wafer osteotomy technique in further detail.
INTRODUCTION
Acetabular dysplasia is a frequent cause of early-onset hip degeneration, progressing to end-stage osteoarthritis in up to 50% of cases by 50 years of age. Poor coverage of the femoral head and altered biomechanics exposes younger patients in particular to a high rate of early osteoarthritis [1]. The Bernese periacetabular osteotomy (PAO) was initially presented in the 1980s [2] and has since shown to provide substantial pain relief and improved function in over 90% of patients after several decades [3, 4].
The goal of PAO is to correct the 3D orientation of the acetabulum to provide more adequate coverage of the femoral head. The Bernese PAO utilizes the Smith–Petersen approach. Some studies have criticized the operation for its technical complexities and steep learning curve. One of the most frequent complications discussed is nerve injury, as the osteotomies are conducted in close vicinity to the lateral femoral cutaneous nerve (LFCN), femoral, obturator and sciatic nerves. There is evidence to support that the prevalence of major nerve injuries is associated with the learning curve and ranges from 0 to 30% [5]. Injury to the LFCN, reportedly occurring in up to one-third of patients, is likely due to stretch/compression causing neural ischemia or direct irritation during the procedure [6]. In addition, another disadvantage with this approach is the need for extensive exposure and soft tissue release, which might affect recovery [7].
The associated Smith–Petersen exposure offers excellent visualization of the acetabulum and control of acetabular osteotomy and mobilization. The traditional exposure of the true pelvis involves osteotomy of the iliac wing in order to mobilize the sartorial and inguinal ligament insertion. However, full osteotomy of the iliac spine may necessitate screw fixation if a relatively large segment of bone is included. A known complication with screw fixation of the iliac wing osteotomy involves failure of fixation and screw back out. Moreover, the screw may irritate the patient even in the setting of adequate fixation. A larger osteotomy may also injure the LFCN as it travels near the anterior–superior spine. To minimize the risk of these potential complications, a wafer osteotomy may be used to develop a sleeve of tissue involving the sartorial insertion. This sleeve also mobilizes the entirety of the LFCN medially and affords protection throughout the procedure. Furthermore, the wafer osteotomy may be re-fixed to the stable pelvis during closure with simple heavy suture fixation alone, avoiding screw insertion or associated removal. Because only a wafer or bone is taken during the spine osteotomy, more bone is available at the anterior–superior iliac spine (ASIS) for fixation of the mobile fragment after repositioning. In this technical note, we describe the wafer osteotomy technique in further detail.
Surgical technique
The senior author is dual-fellowship trained in adult lower extremity reconstruction and hip preservation. The author’s overall technique for the Bernese PAO is consistent with prior publications [2, 8]. This particular iliac spine wafer technique represents a modification of the Smith–Petersen approach. The wafer osteotomy modification has been used consistently for the last 5 years for all PAO procedures, during which 194 procedures were performed.
Anatomy and positioning of exposure
The patient is positioned supine on a radiolucent table. Markings are made so that the curvilinear incision is centered about the ASIS (Fig. 1a). An alternate more transverse skin incision (‘bikini’ incision) may be employed (Fig. 1b). Dissection of subcutaneous tissue is followed by separation of the fascia overlying the tensor fascia lata (TFL) in the tensor-sartorius interval (Fig. 2). Subsequently, the ASIS is osteotomized (Fig. 3a) as a several-millimeter thick mobile fragment and reflected (Fig. 3b) with preservation of the sartorius attachment to the mobile fragment of the wafer osteotomy (Fig. 3c). During these steps, care should be taken to protect the LFCN as it emerges medial to the ASIS—running and branching to varying degrees in a fatty tissue layer in the tensor-sartorius interval directly beneath the subcutaneous layer (Fig. 4) [8]. To minimize inadvertent injury with this approach, it is recommended to make the C-shaped skin incision and deeper dissection slightly laterally to the ASIS, to hold the tensor muscle laterally, and to contain all dissections within the TFL fascia. It has also been shown that flexing the leg to 45° may also reduce soft tissue tension and ease dissection [9]. After the superior pubic ramus is visualized (Fig. 5a and b), further dissection of the ilium can be extended to the quadrilateral plate.
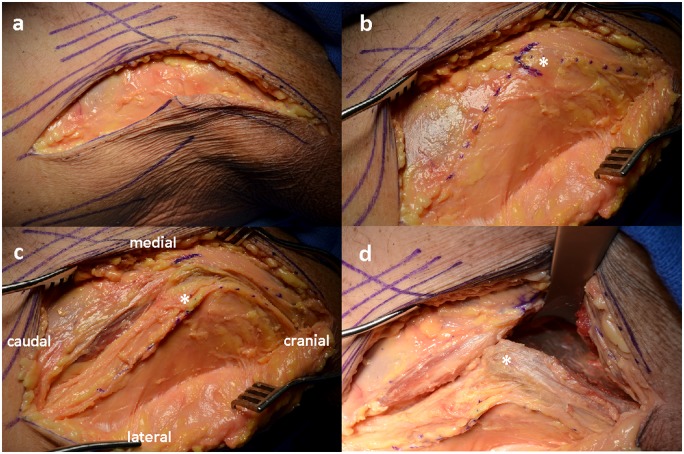
Fig. 1.
Surface markings of the planned curvilinear incision (a). An alternate, more transverse ‘bikini’ incision (b) may be employed for the Smith–Petersen approach, but this skin incision variation is not extensile. ASIS, anterior–superior iliac spine; GT, greater trochanter.
Fig. 2.
Cadaveric model showing superficial dissection (a, b) down to the anterior–superior iliac spine (*), followed by a fascial incision exposing the tensor facia lata (c). Exposure of the iliac wing down to the true pelvis is made after wafer osteotomy (d) of the anterior–superior iliac spine.
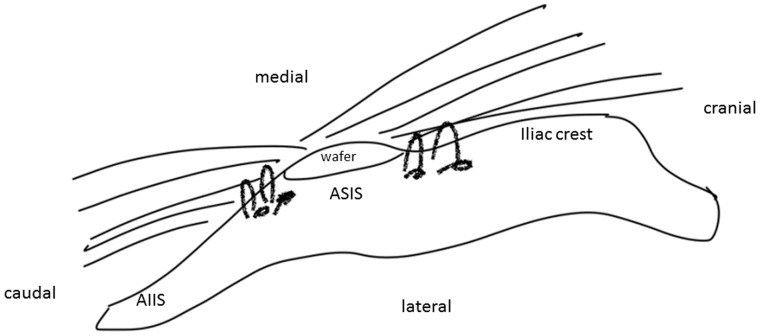
Fig. 3.
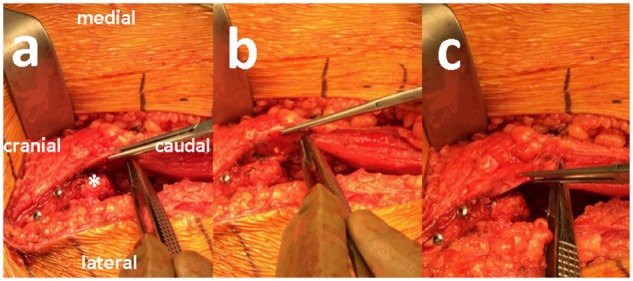
Wafer osteotomy mobile fragment of the anterior–superior iliac spine (*) (a) with sartorial/inguinal ligament attachment. This fragment can be reduced back to the stable pelvis (b, c) and affixed with heavy suture fixation at closure.
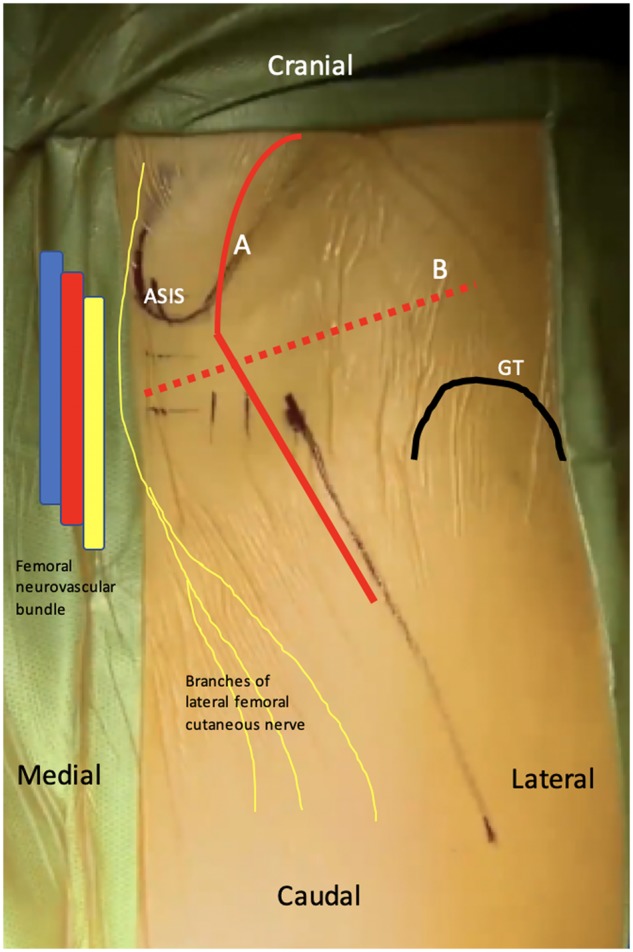
Fig. 4.
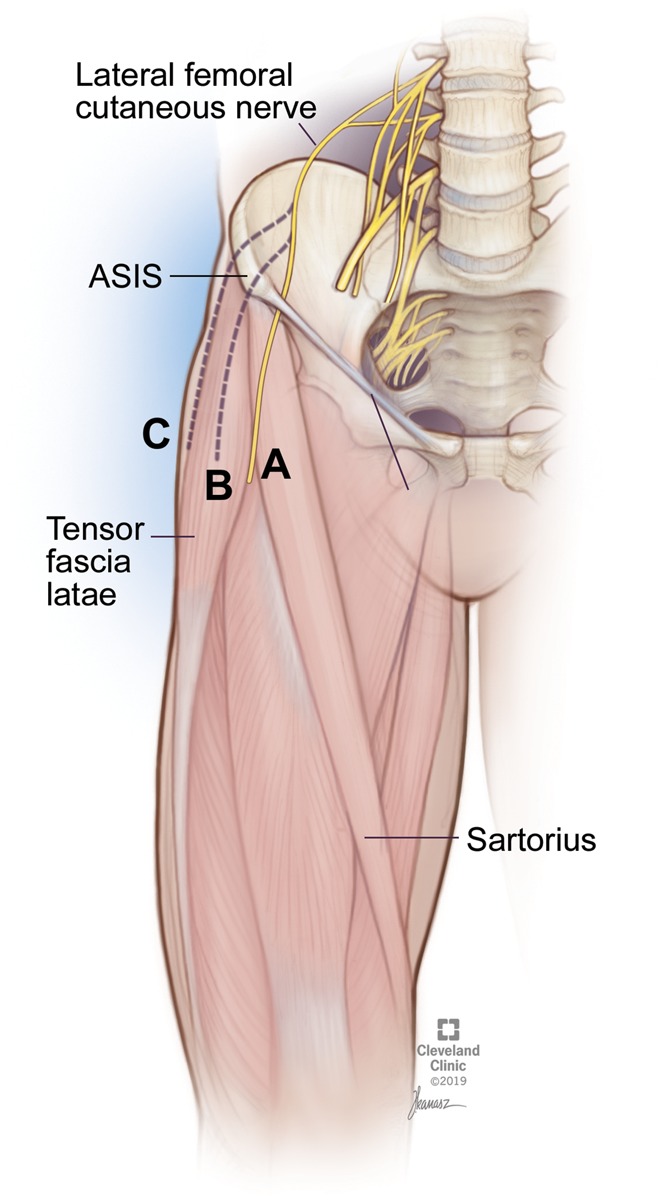
Branching pattern of the lateral femoral cutaneous nerve in relation to the anterior–superior iliac spine (ASIS). While pattern A is the most common branching orientation, patterns B and C are anatomic variants.
Fig. 5.
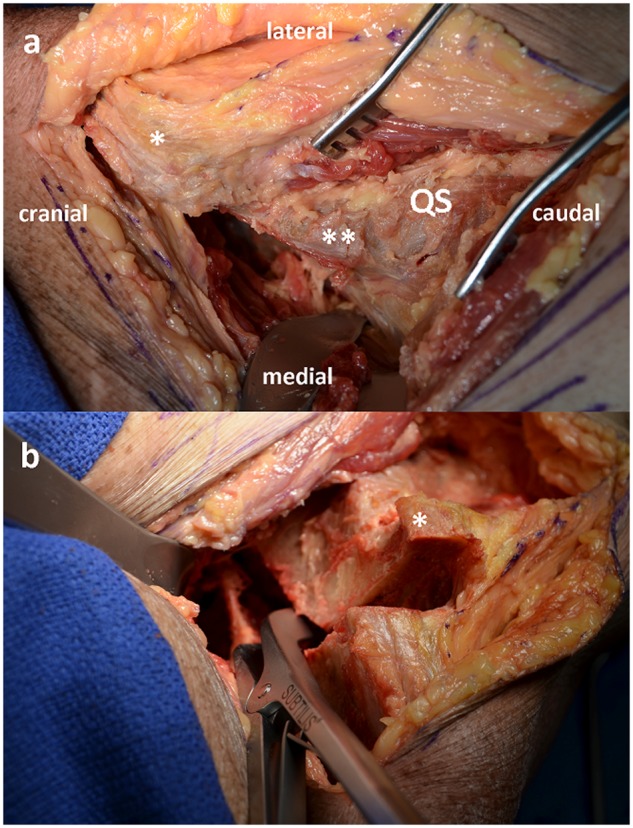
Cadaveric dissection down to the hip joint and quadrilateral surface prior to osteotomy of the acetabulum (a). After completion of periacetabular osteotomies, the acetabular fragment can be mobilized and placed in the proper acetabular orientation (b). *Anterior–superior iliac spine; **anterior–inferior iliac spine; QS, quadrilateral surface.
Osteotomies
Osteotomies may proceed once the above exposures are completed, starting with the ischium and pubic ramus. Next, attention is directed to the supra-acetabular and retro-acetabular osteotomies. The final osteotomy is performed with an angled osteotome and aligns the retroacetabular cut with the incomplete ischial cut, which helps with fragment mobilization and acetabular reorientation [9]. With successful osteotomies completed, the mobile fragment can then be fully mobilized and repositioned into the ideal spatial orientation for adequate coverage.
Suture closure
During closure, sutures are passed through the lateral cuff of tissue along the iliac crest. They should not be trans-osseous, and do not require bone tunnels. The knots are kept on the lateral (outer) part of the iliac crest to avoid soft tissue irritation, and the bite of the suture is not passed medial to the medial border of the wafer/ASIS, to avoid iatrogenic injury to the LFCN (Fig. 6).
Fig. 6.
Depiction of suture repair following osteotomy.
DISCUSSION
Khan et al. recently described a similar technique for a minimally invasive PAO [10]. The authors demonstrated excellent post-surgical results, with a significant improvement in University of California, Los Angeles (UCLA), Tegner activity and Non-Arthritic Hip Score (NAHS) values (all P-values <0.001). Similarly, no major complications were reported in their cohort of 166 hips. The technique proposed in the current paper is unique in its use of the wafer osteotomy, which allows for mobilization of the ASIS fragment. This technique, therefore, can be particularly useful for patients who previously underwent surgery of the pelvis. Specifically, if the iliac apophysis had been previous split, the resultant deformed anatomy of the pelvis may necessitate the use of a supra-acetabular iliac osteotomy above the level of the ASIS.
The sleeve created in the proposed approach allows for medial translation, and subsequent protection, of the LCFN regardless of potential anatomical variation in the path of the nerve. The importance of protecting this structure is notable given the high rates of damage that have been reported in the literature. Specifically, in a 2009 systematic review by Clohisy et al., rates of LFCN dysesthesias were reported in up to 14% of cases, with nearly one-third of such cases requiring neurolysis [11]. A more recent review by Swarup et al. similarly demonstrated high rates of this complication, with more contemporary data demonstrating rates of LFCN damage reaching up to 14.8% [12].
An additional benefit associated with the proposed technique relates to the ability to re-fix the proposed wafer osteotomy back to the pelvis without the need for screw fixation. Screw complications, such as joint penetration, broken/migrated screw leading to fixation failure and prominent screw rub against local tissue leading to pain, have been heavily reported in literature. Consequently, the need for hardware removal has been reported to be ranging anywhere from 6.5 to 17% [13, 14]. Specifically, the analysis by Clohisy et al. reported that symptomatic hardware removal was shown to be as high as 35% in a 12-year follow-up study [11]. Therefore, the fact that our technique does not require screw fixation for this aspect of the procedure suggests that rates of these complications and subsequent reoperations may be decreased following its implementation.
CONCLUSIONS
Since its introduction in the 1980s, the Bernese PAO has evolved to be a powerful tool for the treatment of hip dysplasia in young adults. Despite its technical complexities and significant learning curve, the PAO is continually being refined with promising long-term results in the setting of hip preservation. The purpose of this study was to explore a modified approach during PAO that enables safe surgical exposure.
To minimize the risk of various complications associated with PAO procedures, the proposed wafer osteotomy may be used to develop a sleeve of tissue involving the sartorial insertion. This sleeve also mobilizes the entirety of the LFCN medially and affords protection throughout the procedure. Furthermore, the wafer osteotomy may be re-fixed to the stable pelvis during closure with simple heavy suture fixation alone, avoiding screw insertion or associated removal. Because only a wafer or bone is taken during the spine osteotomy, more bone is available at the ASIS for fixation of the mobile fragment after repositioning.
FUNDING
No funding was obtained for our analysis.
CONFLICT OF INTEREST STATEMENT
A.F.K. reports the following disclosures: research support (Zimmer Biomet, DePuy Synthes), paid presenter or speaker (Corin, DePuy Synthes, Heraeus Medical and Zimmer Biomet), paid consultant (Pacira Pharmaceuticals, Heraeus Medical, DePuy Synthes and Zimmer Biomet), stock or stock options (Zimmer Biomet, Johnson & Johnson and Procter & Gamble), IP royalties (Innomed), board or committee member (AAOS and AAHKS), and editorial or governing board (BMC Musculoskeletal Disorders). M.M., A.J.A., A.A.S. and L.T.S. have nothing to disclose.
REFERENCES
- 1. Leunig M, Ganz R.. Evolution of technique and indications for the Bernese periacetabular osteotomy. Bull NYU Hosp Jt Dis 2011; 69(Suppl. 1): S42–6. [PubMed] [Google Scholar]
- 2. Ganz R, Klaue K, Vinh TS. et al. A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin Orthop Relat Res 1988; 232: 26–36. [PubMed] [Google Scholar]
- 3. Pascual-Garrido C, Harris MD, Clohisy JC.. Innovations in joint preservation procedures for the dysplastic hip “the periacetabular osteotomy”. J Arthroplasty 2017; 32: S32–7. [DOI] [PubMed] [Google Scholar]
- 4. Kamath AF. Bernese periacetabular osteotomy for hip dysplasia: surgical technique and indications. World J Orthop 2016; 7: 280–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sierra RJ, Beaule P, Zaltz I. et al. Prevention of nerve injury after periacetabular osteotomy. Clin Orthop Relat Res 2012; 470: 2209–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Biedermann R, Donnan L, Gabriel A. et al. Complications and patient satisfaction after periacetabular pelvic osteotomy. Int Orthop 2008; 32: 611–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hussell JG, Mast JW, Mayo KA. et al. A comparison of different surgical approaches for the periacetabular osteotomy. Clin Orthop Relat Res 1999; 363: 64–72. [PubMed] [Google Scholar]
- 8. Rudin D, Manestar M, Ullrich O. et al. The anatomical course of the lateral femoral cutaneous nerve with special attention to the anterior approach to the hip joint. J Bone Joint Surg Am 2016; 98: 561–7. [DOI] [PubMed] [Google Scholar]
- 9. Tibor L, Sink E.. Periacetabular osteotomy for hip preservation: authors’ preferred technique. Orthop Clin North Am 2012; 43: 343–57. [DOI] [PubMed] [Google Scholar]
- 10. Khan OH, Malviya A, Subramanian P. et al. Minimally invasive periacetabular osteotomy using a modified Smith-Petersen approach: technique and early outcomes. Bone Joint J 2017; 99-B: 22–8. [DOI] [PubMed] [Google Scholar]
- 11. Clohisy JC, Schutz AL, St John LB. et al. Periacetabular osteotomy a systematic literature review. Clin Orthop Relat Res 2009; 467: 2041–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Swarup I, Ricciardi BF, Sink EL.. Avoiding complications in periacetabular osteotomy. JBJS Rev 2015; 3: 1–9. [DOI] [PubMed] [Google Scholar]
- 13. Thawrani D, Sucato DJ, Podeszwa DA. et al. Complications associated with the Bernese periacetabular osteotomy for hip dysplasia in adolescents. J Bone Jt Surg Am 2010; 92: 1707–14. [DOI] [PubMed] [Google Scholar]
- 14. Ganz R, Klaue K, Mast J. [ Peri-acetabular reorientation osteotomy]. Acta Orthop Belg 1990; 56: 357–69. [PubMed] [Google Scholar]