Abstract
Objective: To provide family physicians with a practical, evidence-based approach to managing patients with cerumen impaction. Methods: MEDLINE, The Cochrane Library, and the Turning Research Into Practice (TRIP) database were searched for English-language cerumen impaction guidelines and reviews. All such articles published between 1992 and 2018 were reviewed, with most providing level II and III evidence. Results: Cerumen impaction is a common presentation seen in primary care and cerumen removal is one of the most common otolaryngologic procedures performed in general practice. Cerumen impaction is often harmless but can be accompanied by more serious symptoms. Cerumenolytics and irrigation of the ear canal are reasonable first-line therapies and can be used in conjunction or isolation. If irrigation and cerumenolytics are contraindicated, manual removal is appropriate, but the tools necessary are not commonplace in primary care clinics and specialized training may be required to prevent adverse outcomes. Conclusion: Family physicians play a key role in the assessment and management of cerumen impaction and are well equipped to do so. Knowledge of the available techniques for cerumen removal as well as their contraindications ensures that cerumen is removed safely and effectively. When cerumen removal cannot be removed safely in a primary care setting, referral to Otolaryngology-Head and Neck Surgery is appropriate.
Keywords: cerumen, cerumen impaction, earwax, primary care
Introduction
Cerumen impaction is commonly seen in primary care, and family physicians play a key role in the assessment and management of this condition. However, there is little evidence to guide management of this common presentation.1 While cerumen impaction is often harmless, management can be complicated by patient comorbidities. Knowledge of available cerumen removal techniques as well as their contraindications ensures that safe and effective treatment is provided. With this in mind, the majority of cases of cerumen impaction can be safely and effectively managed in a primary care setting. In cases where impacted cerumen cannot be removed safely in primary care, referral to otolaryngology–head and neck surgery is appropriate. Herein, we provide an updated clinical review of cerumen management along with an evidence-based, practical management approach for primary care physicians.
Cerumen, commonly known as earwax, is a hydrophobic, waxy substance that provides mechanical and microbial protection to the epithelial lining of the external auditory canal.2 Typically, cerumen is carried out of the ear canal via migration of the canal’s epithelial lining, aided by jaw movement.3 Cerumen accumulates when this clearing process becomes compromised. This can occur through regular use of cotton tipped swabs, digital manipulation of the ear canal, or use of hearing aids, all of which can pack cerumen deep into the ear canal. Cerumen impaction is defined as the symptomatic accumulation of cerumen, or cerumen accumulation that prevents diagnostic assessment.1 Cerumen impaction is common, affecting approximately 10% of children and one-third of geriatric and intellectually disabled individuals.2 Cerumen removal is one of the most common otolaryngologic procedures performed by family physicians.2
Cerumen impaction is often harmless but can be accompanied by more serious symptoms. Removal of impacted cerumen is generally considered safe but does have associated risks, including eardrum perforation, canal laceration, and failed removal of cerumen.4 These risks can be mitigated by identifying high-risk patients and tailoring management strategies. Commonly used cerumen removal techniques include cerumenolytics (cerumen softening agents), irrigation, and manual removal. It is also appropriate to not intervene if patients are asymptomatic and visualization of the tympanic membrane is not vital.1 The available literature suggests that cerumenolytics and irrigation used alone or in combination are effective and low cost.5-9 In patients with contraindications for cerumenolytics or irrigation, or in those that do not respond to first line treatment, manual removal of cerumen is recommended.1,10 However, manual removal requires tools that are not always available in primary care clinics, and more technical skill is required compared to other techniques.10
Symptoms and Causes
Patients with cerumen impaction can present with symptoms, including aural fullness, hearing loss, ear pain, itching, tinnitus, and otitis externa.11 Symptomatic accumulation of cerumen occurs when the natural elimination mechanism is disrupted or is inadequate. There are four main factors that lead to cerumen impaction; often, cerumen impaction results from a combination of these factors.12
Overproduction
If the rate of cerumen production exceeds the rate of cerumen migration out of the ear, cerumen impaction will occur. Some individuals with recurrent cerumen impaction may suffer from idiopathic cerumen overproduction.13
Obstruction
Variations in the anatomy of the ear canal can lead to cerumen accumulation. Benign bony growths in the ear canal (exostoses or osteomas) can obstruct cerumen migration. Soft tissue malformations can cause obstructions, as in the case of patients with a history of otitis externa or ear canal trauma. Finally, some individuals may have particularly narrow or tortuous ear canals, whereas others may have hair that impedes cerumen expulsion.12
Cerumen impaction can also occur when objects are inserted into the ear canal. The use of hearing aids and ear plugs can obstruct cerumen elimination, and cotton swabs (Q-tips) commonly cause cerumen to be forced deeper into the ear canal.12
Inadequate Epithelial Migration
Cerumen glands progressively atrophy and become less numerous with age, resulting in drier cerumen.14 The drier cerumen is less readily transported by the epithelial conveyor mechanism.15 This is compounded by hair in the auditory canal becoming coarser with age, obstructing cerumen movement.16 These factors are thought to contribute to the high rates of cerumen impaction in elderly patients.10,16 Finally, the natural process of epithelial migration may be insufficient for some cerumen subtypes.17
Cerumen Phenotype
Cerumen can be divided into 2 genetically determined phenotypes: “dry” and “wet.” The “dry” cerumen subtype is predominant in people of Asian and Native American descent, whereas the “wet” subtype is predominant in people of African and European descent.18,19 As the name suggests, dry cerumen is brittle and dry and can vary in color from a light to brownish-gray. Wet cerumen conversely is often dark in color, wet, and sticky.18 Cerumen subtype is inherited as a simple Mendelian trait with the “dry” allele being recessive.20 It has been asserted that having a wet or dry cerumen phenotype may promote or protect against cerumen impaction, and that phenotype may also affect the efficacy of different cerumen removal techniques.21-24 However, strong evidence to support cerumen impaction management tailored to cerumen phenotypes does not exist.23 Further research is needed before cerumen impaction management based on phenotype can be recommended, and to convincingly link cerumen phenotype with impaction rates.
Diagnosis
Cerumen impaction is diagnosed by direct visualization (otoscopy). If cerumen accumulation has become symptomatic or prevents needed assessment of the ear canal or tympanic membrane, it is considered to be impacted.1
Management
Prior to cerumen removal, potential contraindications must be identified. These include a nonintact tympanic membrane, exostoses, ear canal stenosis, diabetes mellitus, an anticoagulated or immunocompromised state, and prior radiation therapy affecting the ear canal.1 These are factors that increase the risk of trauma, infection, or hemorrhage when combined with certain cerumen extraction techniques.14
Observation
If cerumen impaction is asymptomatic and visualization of the tympanic membrane or ear canal is not necessary, watchful waiting is reasonable. Studies have shown that in many cases impacted cerumen clears without intervention or remains asymptomatic.1,25 The American Academy of Otolaryngology–Head and Neck Surgery recommends that asymptomatic cerumen that does not impede needed assessment can safely be left alone, as it may not progress to impaction or may resolve spontaneously. If it progresses, it can be safely managed at that time.1
Active Management
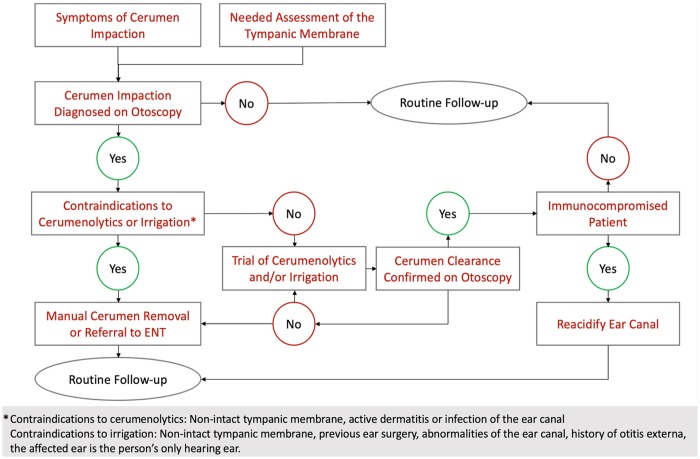
There are three methods of cerumen removal commonly employed in clinical practice: cerumenolytic agents, irrigation, and manual removal.4 These removal methods are often used concurrently.4 To date, a randomized controlled clinical trial comparing the effectiveness of these strategies has not been conducted.26 A schema outlining an approach to cerumen management is shown in Figure 1.
Figure 1.
Schema illustrating an approach to the management of cerumen impaction.
Cerumenolytics
Cerumenolytic agents are compounds used to break down impacted cerumen to lessen the need for irrigation or manual removal. Cerumenolytics can also be used in combination with these methods.1 As no cerumenolytic agents have been shown to be more effective than water or saline, we recommend water and saline as first line agents.5-7,9 The duration of treatment has also been shown to have little impact.6 When the use of cerumenolytics is limited to patients with intact tympanic membranes, without active dermatitis or infection of the ear canal, adverse effects of cerumenolytics are minor and rare.1,9
Based on our clinical experience, we recommend mineral oil or docusate sodium be used as second line cerumenolytics in cases were water or saline are ineffective. In clinic, we have been observed them to clear cerumen more effectively than water-based alternatives. Additionally, patients often prefer hydrogen peroxide for its bubbling activity, although we have observed reduced efficacy compared with other cerumenolytics.
Irrigation
Gentle irrigation with a syringe or electric irrigator is commonly performed in clinical practice.4 Irrigation is an effective method of cerumen removal and it is the most commonly employed method in family practice.1 Adverse effects are rare when contraindications to the procedure (see below) are considered and the water used for irrigation is brought to body temperature to prevent stimulating the vestibular system.4,5 Alternatively, aural irrigation conducted by patients at home may represent a cost-effective alternative to irrigation in the clinic and provide comparable benefits.27
Aural irrigation should be avoided in patients with perforated tympanic membranes or myringotomy tubes to avoid introducing water and potentially infectious agents into the middle ear.1,10,14,23 Irrigation should also be avoided in those who have previously undergone ear surgery. The pressure applied to the tympanic membrane during aural irrigation is safe in normal ears, but risks perforating tissue that has become thinned or atrophic following surgery or trauma.1,28 This does not apply to patients who have had myringotomy tubes extruded more than 18 months prior and who are no longer followed by otolaryngology.29 Additionally, irrigation should be avoided in patients with abnormalities of the ear canal with the potential to trap water and promote infection.1 Irrigation should be avoided in a person’s only hearing ear, and if they have a history of otitis externa.4
Care should be taken when treating immunocompromised patients, as invasive otitis externa has been reported in diabetic patients following aural irrigation.30,31 Cerumen is acidic and normally coats the walls of the ear canal, inhibiting the growth of bacteria and fungi.32 The elimination of cerumen raises the pH and along with the introduction of water can predispose vulnerable patients to develop otitis externa following irrigation.33 Reacidification of the canal with 2% acetic acid can help prevent colonization by the bacteria that can cause otitis externa and malignant otitis externa.1,33 This, along with a list of other clinical recommendations is included in Figure 2.
Figure 2.
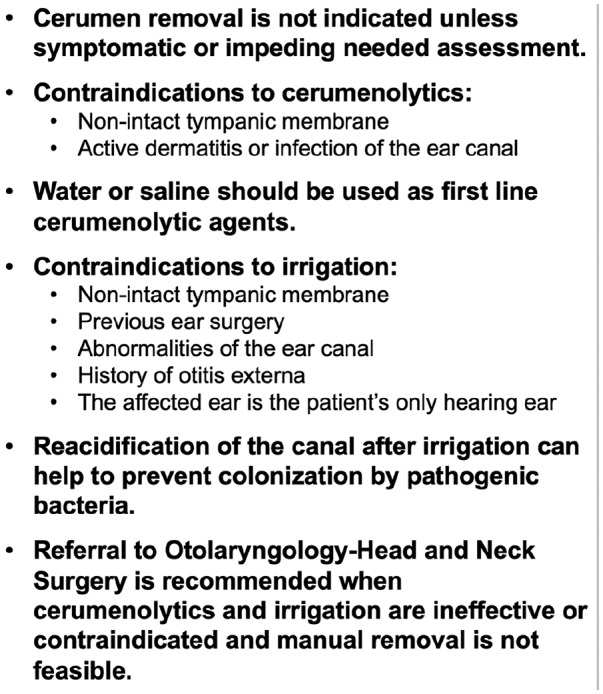
Clinical recommendations for the management of cerumen impaction.
Manual Removal
Manual cerumen removal uses instruments to remove cerumen under direct visualization. This method of cerumen removal is considered to be safe and effective in the hands of a well-trained practitioner but can lead to trauma in less experienced hands. Although there is little supportive evidence, The American Academy of Otolaryngology–Head and Neck Surgery supports manual removal of cerumen as effective based on case series and expert opinion.1
An advantage of manual removal is that it can be done quickly and avoids exposing the ear canal to moisture, reducing the risk of infection.10 Manual cerumen removal is often preferred in patients with congenital or acquired abnormalities of the ear, those who have recently had ear surgery, and immunocompromised patients.1 Manual removal with a binocular microscope or endoscope provides better visualization in more complex cases where cerumenolytics or irrigation risk causing otitis media or where irrigation could perforate a weakened tympanic membrane.1 However, manual cerumen removal is not without risks. Perforation of the tympanic membrane, ear canal trauma, vertigo, and pain have been reported following manual removal of cerumen.4
In practice, family physicians often do not have ready access to the equipment used for manual cerumen removal such as microsuction equipment or binocular microscopes that improve procedure comfort and safety.10 However, lack of these tools does not preclude primary care providers from performing manual cerumen removal and doing so may be essential in areas without ready access to otolaryngology services. Practitioner experience is the main consideration in the implementation of manual cerumen removal.
Conclusion
Family physicians play a key role in the assessment and management of patients with cerumen impaction. Knowledge of the available techniques for cerumen removal as well as their contraindications ensures that cerumen is removed safely and effectively when necessary. In cases where cerumenolytics and irrigation are ineffective or contraindicated and practitioners are uncomfortable performing manual removal (or lack the necessary equipment), referral to otolaryngology–head and neck surgery is recommended.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Garret A. Horton  https://orcid.org/0000-0003-4071-2136
https://orcid.org/0000-0003-4071-2136
References
- 1. Schwartz SR, Magit AE, Rosenfeld RM, et al. Clinical practice guideline (update): earwax (cerumen impaction). Otolaryngol Head Neck Surg. 2017;156(1 suppl):S1-S29. [DOI] [PubMed] [Google Scholar]
- 2. Roeser RJ, Ballachanda BB. Physiology, pathophysiology, and anthropology/epidemiology of human earcanal secretions. J Am Acad Audiol. 1997;8:391-400. [PubMed] [Google Scholar]
- 3. Alberti P. Epithelial migration on the tympanic membrane. J Laryngol Otol. 1964;78:808-830. [DOI] [PubMed] [Google Scholar]
- 4. Sharp JF, Wilson JA, Ross L, Barr-Hamilton RM. Ear wax removal: a survey of current practice. BMJ. 1990;301:1251-1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Clegg A, Loveman E, Gospodarevskaya E, et al. The safety and effectiveness of different methods of earwax removal: a systematic review and economic evaluation. Health Technol Assess. 2010;14:1-192. [DOI] [PubMed] [Google Scholar]
- 6. Hand C, Harvey I. The effectiveness of topical preparations for the treatment of earwax: a systematic review. Br J Gen Pract. 2004;54:862-867. [PMC free article] [PubMed] [Google Scholar]
- 7. Loveman E, Gospodarevskaya E, Clegg A, et al. Ear wax removal interventions: a systematic review and economic evaluation. Br J Gen Pract. 2011;61:e680-e683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Eekhof JA, de Bock GH, Le Cessie S, Springer MP. A quasi-randomised controlled trial of water as a quick softening agent of persistent earwax in general practice. Br J Gen Pract. 2001;51:635-637. [PMC free article] [PubMed] [Google Scholar]
- 9. Aaron K, Cooper TE, Warner L, Burton MJ. Ear drops for the removal of ear wax. Cochrane Database Syst Rev. 2018;(7):CD012171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. McCarter DF, Courtney AU, Pollart SM. Cerumen impaction. Am Fam Physician. 2007;75:1523-1528. [PubMed] [Google Scholar]
- 11. DeWeese DD, Saunders WH. Textbook of Otolaryngology. 4th ed. St Louis, MO: Mosby; 1973. [Google Scholar]
- 12. Jabor MA, Amedee RG. Cerumen impaction. J La State Med Soc. 1997;149:358-362. [PubMed] [Google Scholar]
- 13. Mandour MA, El-Ghazzawi EF, Toppozada HH, Malaty HA. Histological and histochemical study of the activity of ceruminous glands in normal and excessive wax accumulation. J Laryngol Otol. 1974;88:1075-1085. [DOI] [PubMed] [Google Scholar]
- 14. Zivic RC, King S. Cerumen-impaction management for clients of all ages. Nurse Pract. 1993;18:29-36,39. [DOI] [PubMed] [Google Scholar]
- 15. Meador JA. Cerumen impaction in the elderly. J Gerontol Nurs. 1995;21:43-45. [DOI] [PubMed] [Google Scholar]
- 16. Ruby RR. Conductive hearing loss in the elderly. J Otolaryngol. 1986;15:245-247. [PubMed] [Google Scholar]
- 17. Robinson AC, Hawke M, Naiberg J. Impacted cerumen: a disorder of keratinocyte separation in the superficial external ear canal? J Otolaryngol. 1990;19:86-90. [PubMed] [Google Scholar]
- 18. Matsunaga E. The dimorphism in human normal cerumen. Ann Hum Genet. 1962;25:273-286. [DOI] [PubMed] [Google Scholar]
- 19. Petrakis NL. Dry cerumen—a prevalent genetic trait among American Indians. Nature. 1969;222:1080-1081. [DOI] [PubMed] [Google Scholar]
- 20. Bass EJ, Jackson JF. Cerumen types in Eskimos. Am J Phys Anthropol. 1977;47:209-210. [DOI] [PubMed] [Google Scholar]
- 21. Ping C, Yanling H, Youhua W, Shufen W, Zhinan W, Zhongfang X. Epidemiology of cerumen impaction among municipal kindergartens children in Wuhan, China. Int J Pediatr Otorhinolaryngol. 2017;100:154-156. [DOI] [PubMed] [Google Scholar]
- 22. Ballachanda B, Miyamoto RT, Miyamoto C, Taylor B. The Human Ear Canal. San Diego, CA: Plural; 2013. [Google Scholar]
- 23. Guest JF, Greener MJ, Robinson AC, Smith AF. Impacted cerumen: composition, production, epidemiology and management. QJM. 2004;97:477-488. [DOI] [PubMed] [Google Scholar]
- 24. Carr MM, Smith RL. Ceruminolytic efficacy in adults versus children. J Otolaryngol. 2001;30:154-156. [DOI] [PubMed] [Google Scholar]
- 25. Crandell CC, Roeser RJ. Incidence of excessive/impacted cerumen in individuals with mental retardation: a longitudinal investigation. Am J Ment Retard. 1993;97:568-574. [PubMed] [Google Scholar]
- 26. Wilson SA, Lopez R. Clinical inquiries. What is the best treatment for impacted cerumen? J Fam Pract. 2002;51:117. [PubMed] [Google Scholar]
- 27. Coppin R, Wicke D, Little P. Randomized trial of bulb syringes for earwax: impact on health service utilization. Ann Fam Med. 2011;9:110-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Sørensen VZ, Bonding P. Can ear irrigation cause rupture of the normal tympanic membrane?: an experimental study in man. J Laryngol Otol. 1995;109:1036-1040. [DOI] [PubMed] [Google Scholar]
- 29. Harkin H. Ear irrigation. In: Lucas J, ed. New Practice Nurse. London, England: Churchill Livingstone; 2007:154-158. [Google Scholar]
- 30. Rubin J, Yu VL, Kamerer DB, Yu VL, Wagener M. Aural irrigation with water: a potential pathogenic mechanism for inducing malignant external otitis? Ann Otol Rhinol Laryngol. 1990;99(2 pt 1):117-119. [DOI] [PubMed] [Google Scholar]
- 31. Zikk D, Rapoport Y, Himelfarb MZ. Invasive external otitis after removal of impacted cerumen by irrigation. N Engl J Med. 1991;325:969-970. [DOI] [PubMed] [Google Scholar]
- 32. Martinez Devesa P, Willis CM, Capper JW. External auditory canal pH in chronic otitis externa. Clin Otolaryngol Allied Sci. 2003;28:320-324. [DOI] [PubMed] [Google Scholar]
- 33. Sander R. Otitis externa: a practical guide to treatment and prevention. Am Fam Physician. 2001;63:927-936, 941-942. [PubMed] [Google Scholar]