Abstract
Background:
Despite being one of the most common sports injuries, there are no criteria-based rehabilitation programs published for acute adductor injuries.
Purpose:
To evaluate return-to-sport (RTS) outcomes and reinjuries after criteria-based rehabilitation for athletes with acute adductor injuries.
Study Design:
Cohort study; Level of evidence, 2.
Methods:
Male adult athletes with an acute adductor injury underwent a supervised, standardized criteria-based exercise rehabilitation program. Magnetic resonance imaging (MRI) was used to grade the injury extent from 0 (negative finding) to 3 (complete tear/avulsion). There were 3 milestones used to evaluate the RTS continuum: (1) clinically pain-free, (2) completion of controlled sports training, and (3) return to full team training. Subsequent injuries were registered within the first year.
Results:
We included 81 athletes with an acute adductor injury (MRI grade 0: n = 14; grade 1: n = 20; grade 2: n = 30; grade 3: n = 17). Of these, 61 (75%) athletes achieved RTS milestone 1, 50 (62%) achieved RTS milestone 2, and 75 (93%) achieved RTS milestone 3. There were no statistical differences in the RTS duration between MRI grade 0, 1, and 2 at any RTS milestone; thus, these were grouped together as grade 0-2. The median time (interquartile range [IQR]) for athletes with grade 0-2 injuries to become clinically pain-free was 13 days (IQR, 11-21 days), to complete controlled sports training was 17 days (IQR, 15-27 days), and to return to full team training was 18 days (IQR, 14-27 days). For athletes with a grade 3 injury, median times were 55 days (IQR, 31-75 days), 68 days (IQR, 51-84 days), and 78 days (IQR, 68-98 days), respectively. The overall 1-year reinjury rate was 8%. Athletes who achieved RTS milestone 1 had a statistically significantly lower reinjury rate than athletes who did not (5% vs 21%, respectively; ϕ = –0.233; P = .048). Athletes who achieved RTS milestone 2 had a nonstatistically significantly lower reinjury rate than athletes who did not (6% vs 13%, respectively; ϕ = –0.107; P = .366).
Conclusion:
We analyzed the results of a criteria-based rehabilitation protocol for athletes with acute adductor injuries. Athletes with an MRI grade 0-2 adductor injury were clinically pain-free after approximately 2 weeks and returned to full team training after approximately 3 weeks. Most athletes with an MRI grade 3 adductor injury were pain-free and returned to full team training within 3 months. Meeting the clinically pain-free criteria resulted in fewer reinjuries compared with not meeting the criteria.
Keywords: groin, hip, muscle injury, muscle strain, avulsion, RTP, RTS
Acute adductor injuries are common in sports. In elite soccer, the season prevalence of acute adductor time-loss injuries is 14%, resulting in a mean (±SD) absence of 14 ± 24 days and an injury burden of 8 days per 1000 hours of exposure.7 To date, no criteria-based rehabilitation protocols for acute adductor injuries have been published, and specified criteria for when players are allowed to return to sport (RTS) have not been described. Variations in rehabilitation protocols, such as exercise selection or decisions on progression, may affect the duration and outcome of the rehabilitation and should be standardized if prognostic information is to be generalized.
RTS is a continuum, which is reported to comprise 3 levels: return to participation (participation in sports but at a lower level than the RTS goal), return to the previous level of sport, and return to performance (RTS at a previous or higher level of performance).1 In sports medicine research, specifically soccer, RTS is defined as a “return to full participation in team training and availability for match selection.”9 This does not include the specification of any criteria; thus, the decision on readiness for full participation may vary considerably between different medical teams. It is also well-known that RTS decisions are influenced by many contextual factors.4,25 RTS duration is therefore likely often influenced by various decision modifiers related to risk tolerance, such as timing of the season and athlete importance. This limits the generalizability of the commonly used RTS definition as well as the applicability to individual cases. A standardized description of specific RTS criteria is therefore essential to assist clinicians in gaining more specific and reliable information on RTS duration.
We elected to undertake an exploratory study with the primary aim of evaluating the RTS duration for athletes with an acute adductor injury; we thus developed a standardized criteria- and exercise-based rehabilitation protocol including specific milestones within the RTS continuum. Our secondary aims were to assess self-reported disability and the clinical measures of strength and range of motion upon completion of the rehabilitation protocol as well as any subsequent groin pain within 1 year after RTS.
Methods
Participants
Athletes with acute groin injuries were consecutively included in a single-center prospective cohort study over 4 sports seasons (August 2013 to June 2017) at an orthopaedic and sports medicine hospital in Qatar. Ethical approval was obtained for this study, and written informed consent was acquired from all athletes before inclusion.
Eligibility criteria were male athletes aged 18 to 40 years who participated in competitive sports. Athletes had to present to the hospital within 7 days of an acute onset of groin pain that occurred during sports, and a clinical diagnosis of an acute adductor injury by a sports medicine physician using a standardized clinical examination was a requirement for this study.21 A clinical examination has been shown to be accurate in diagnosing acute adductor injuries.23 To be considered an athlete, patients had to be officially registered through a sports association or federation corresponding to the 2 highest national leagues in soccer or highest national competition level in any other sport. Exclusion criteria were a gradual onset or exacerbation of ongoing groin pain, acute groin pain not involving the adductors on clinical examination, clinical signs or symptoms of prostatitis or urinary tract infection, or other known coexisting chronic diseases such as a clinical suspicion of significant hip osteoarthritis.
Sample Size
We utilized a convenience sample based on consecutive inclusion over 4 years (2013-2017). The inclusion of participants for this study was discontinued because of a change in practice in which the majority of athletes with acute adductor injuries were being assessed and treated in the clubs and federations rather than at our hospital.
Demographics and Self-reported Disability
Athlete demographics, such as age, height, weight, and type of sport, were recorded. The athletes were also asked to complete the modified Copenhagen Hip and Groin Outcome Score (HAGOS) questionnaire28 at the initial examination and on the day of completing the rehabilitation protocol (controlled sports training). This questionnaire has both English and Arabic versions, which was translated and cross-culturally adapted before the study (www.koos.nu). The modification was that we requested answers related to the time period “since injury,” instead of the “past week” at the initial examination, and how the athlete feels “today,” instead of the “past week” after the completion of controlled sports training. A total of 5 subscales were included, each with a score from 0 to 100. The subscale “participation in physical activities” was not included, as all athletes had discontinued training at the time of the examination.
Clinical Examination
Standardized clinical examinations (Appendix 1) were performed by a physical therapist (A.S.) on the day of presentation (blinded to imaging findings) and on the day of completing the rehabilitation protocol (completion of controlled sports training). The clinical pain provocation tests have previously been published in detail.23 The physical therapist also examined passive range of motion in a side-lying hip abduction position and performed the bent knee fall out test as well as assessed eccentric strength in side-lying hip adduction and side-lying hip abduction positions. Furthermore, eccentric adduction strength in the outer range was tested on the day the athlete completed the rehabilitation protocol. The limb symmetry index and side-lying eccentric adduction/abduction strength ratio were calculated. Intratester and intertester reproducibility of these tests were good (intraclass correlation coefficient, 0.66-0.92; SEM, 7%-14%) (Appendix 1).
Magnetic Resonance Imaging Assessment
Magnetic resonance imaging (MRI) was performed on a 1.5-T system (Magnetom Espree; Siemens) using a body matrix coil and 8 standardized sequences, as previously published in detail.20,21 Anonymized MRI scans were scored by 2 radiologists blinded to the clinical information. For this study, injury grades from 0 to 3 were used: grade 0 indicated no acute injury findings (negative finding); grade 1, diffuse intramuscular hyperintensity, representing edema only; grade 2, fluid-equivalent intramuscular collection, indicating structural disruption; and grade 3, avulsion or complete musculotendinous disruption.20,24 In athletes with multiple adductor injuries on imaging, we reported the primary adductor injury according to (1) highest injury grade, (2) highest intramuscular edema extent (with multiple grade 1 or 2 injuries), or amount of retraction (with multiple grade 3 injuries). Both intrarater and interrater reproducibility for MRI injury grading were almost perfect; for the presence versus absence of an acute injury, the intrarater and interrater kappa values were 1.00 (95% CI, 1.00-1.00) and 0.89 (95% CI, 0.76-1.00), respectively, and for acute injury grading from 1 to 3, the intrarater and interrater kappa values were 0.92 (95% CI, 0.74-1.00) and 0.97 (95% CI, 0.79-1.00), respectively.20
Rehabilitation Protocol
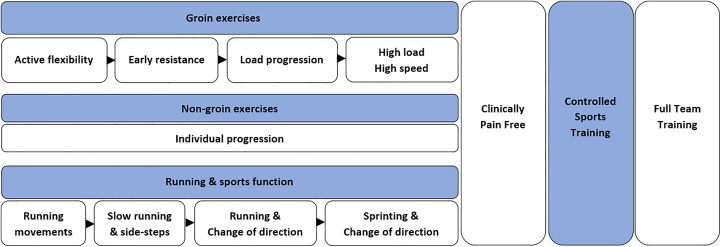
All athletes followed a standardized criteria-based rehabilitation program based on active exercises, with an independent progression of basic exercises and progressive running and change-of-direction drills as well as a controlled sports training phase (Figure 1). The rehabilitation program used in this study was based mainly on our clinical experience in managing athletes with acute groin injuries while also considering the available literature on specific elements, such as muscle activation and strength increases in different exercises5,11,12,15,19,27 and treatment of long-standing groin pain.10,14,22 Additionally, pilot testing of 40 patients was performed during the development of the protocol.
Figure 1.
Overview of the phases and focus of the standardized criteria-based rehabilitation protocol. Progression of the phases in the basic exercise part (groin and non-groin exercises) and in the running and sports function part could be performed independently. Criteria for both parts of the protocol had to be met before initiating on-pitch/on-court controlled sports training. Blue shading indicates the general exercise focus, and white shading indicates the phases and return-to-sport milestones. See Appendix 2 for further details.
The rehabilitation program was supervised by a sports physical therapist with individual face-to-face sessions offered 5 times per week at our facility. The protocol included 9 “groin exercises” (Figure 2). These exercises were chosen because of their limited equipment requirements, so as to optimize the possibility for usage in other settings. Athletes were instructed to perform the included exercises with as many repetitions as possible (volitional failure) within a pain score of 2 on a numerical rating scale from 0 to 10, where 0 is no pain and 10 is the worst possible pain. Athletes were encouraged to increase loading to perform exercises with minor pain corresponding to 2 of 10; that is, if pain was ≤1 of 10, they were encouraged to increase the load, and if pain was ≥3 of 10, the load was reduced. We called this “pain-controlled repetition maximum.”
Figure 2.
Nine groin exercises included in the protocol: (1 and 2) leg swings in hip abduction/adduction and hip extension/flexion with support, (3) standing hip circles, (4) standing hip adduction, (5) hip flexion, (6) trunk rotation, and (7) tension arc performed with elastic bands, (8) one-leg coordination exercise, and (9) the Copenhagen adduction exercise (see Appendix 2 for further description of the protocol).
Detailed information is provided in Appendix 2, including description on sets, repetitions, loads, velocity, and progression criteria. Groin exercises were performed on alternate days 3 times a week. The athletes also followed a separate criteria-based progression of running and sports function, including sprinting and change of direction with and without a ball, where relevant, which could be progressed daily according to the individual athlete (Appendix 2). For both these parts, the treating physical therapist assessed whether the athlete was able to progress in phases in the beginning of each session according to the protocol criteria, regardless of the initial clinical diagnosis and MRI findings. The physical therapist was not blinded to the diagnosis, as provided by the treating sports physician. Athletes were not allowed to progress between phases if they were taking pain medication. In total, sessions lasted between 30 and 120 minutes depending on the phase.
Additional nongroin exercises were included on alternate days if athletes attended more than 3 sessions per week. The choice of additional exercises was not standardized but focused primarily on the posterior kinetic chain muscle groups (hip abductors, extensors, hamstrings, and calves). Additional exercises also depended on the individual athlete’s needs, such as the type of sport or injury history, and could for example also involve shoulder exercises if they were considered appropriate for the specific athlete. No groin pain was allowed during these exercises. Athletes were advised to attend 5 rehabilitation sessions per week at the hospital. Compliance was calculated as the number of sessions completed/number of possible sessions × 100 (%).
Therapeutic ultrasound, lasers, dry needling, and other similar complementary and alternative treatments were prohibited during the rehabilitation period. Manual soft tissue treatment was prohibited on the painful area but allowed elsewhere on the injured muscle for up to 5 minutes if an athlete perceived adductor tightness to be limiting exercise performance. Nonsteroidal anti-inflammatory drugs were not prescribed, and their use was discouraged.
After meeting the clinically pain-free criteria (Table 1), athletes progressed to a supervised, sport-specific on-field/on-court training phase (controlled sports training). Because of the number of drills and tests, athletes from indoor sports would have a minimum of 2 sessions (2 days) and outdoor sports a minimum of 3 sessions (3 days) before returning to the club. Thus, this can be considered an addition of time-based criteria within the rehabilitation protocol.
TABLE 1.
Criteria for Completion of Rehabilitation Protocola
| Clinically Pain-Free | Completion of Controlled Sports Training |
|---|---|
|
|
aDetailed description of the criteria can be found in Appendices 1 and 2.
RTS Continuum
There were 3 different milestones used to evaluate the RTS continuum, and the number of days from injury was calculated until (1) clinically pain-free, (2) controlled sports training was completed, and (3) full team training resumed, regardless of meeting all protocol criteria.
Athletes were encouraged to enter team training progressively after the completion of controlled sports training. The decision on when to return to full team training was at the discretion of the athlete and the club medical and coaching staff without further criteria, as this involves a risk assessment and risk tolerance decision including more than solely medical factors.25 Return to full team training could therefore occur immediately after completing the rehabilitation protocol, after a prolonged period of training with the club, or even during the rehabilitation period without meeting any criteria. If athletes discontinued rehabilitation before meeting the specific criteria, they were excluded from the respective analyses (considered as missing data). The date of return to full team training was obtained through weekly telephone calls to the athlete after the last supervised rehabilitation session.
Subsequent Injuries
We recorded subsequent injuries through telephone calls at 2, 6, and 12 months after the last rehabilitation session using the subsequent injury classification (SIC) model.25 Athletes were also instructed to inform the coordinating researchers if they suspected a reinjury. Additionally, medical records at the hospital were checked to reduce the risk of missing any subsequent injuries and to confirm the injury diagnosis where possible. Subsequent injuries were grouped into reinjuries (exact same injury in terms of body site and nature) (SIC code 2: acute onset of pain that occurs after full recovery of the index injury [related to index injury]; SIC code 3: acute-onset exacerbation or reinjury before full recovery [related to index injury]) and other groin pain (SIC code 4: continual or sporadic experiences of groin pain or other physical discomfort [related to index injury]; SIC code 5: continual or sporadic experiences of groin pain or other physical discomfort [not related to index injury]; SIC code 7: injury to same body site ([groin]) but of a different nature [related to index injury]; SIC code 8: injury to same body site ([groin]) but of a different nature [not related to index injury]). Other injuries were not reported (SIC codes 9 and 10: injury to different body part [irrespective of nature]).8
Statistical Analysis
Descriptive statistics were used to provide an overview of the RTS duration and clinical measures. Missing RTS data from athletes not achieving specific milestones or being lost to follow-up were excluded. Similarly, missing data for the clinical measures (eg, because of device malfunction or unreturned questionnaires) were excluded from the descriptive overview. The Kruskal-Wallis test with pairwise comparisons was used to compare RTS duration between athletes with different MRI injury grades. We calculated the standardized effect size (r) as , with 0.1 considered small, 0.3 medium, and 0.5 large.25 We compared the distribution of reinjuries between athletes who completed the rehabilitation protocol and those who did not using the Pearson chi-square test. Standardized effect sizes are reported as phi (ϕ) with similar effect size cutoff values as described above.13 Statistical significance was considered at P ≤ .05. All statistical analyses were performed using SPSS software (v 21; IBM).
Results
Participants
A flowchart of athlete inclusion is provided in Figure 3. Overall, 6 athletes (7%) were lost to follow-up, 20 athletes (25%) did not meet the clinically pain-free criteria, and 31 athletes (38%) did not meet the controlled sports training criteria. Demographic data of all included athletes can be found in Table 2, and demographic data for athletes achieving the specific RTS milestones, as well as athletes lost to follow-up, can be found in Appendix 3, Table A1.
Figure 3.
Flowchart of athlete inclusion for the 3 return-to-sport milestones.
TABLE 2.
Demographic Data of All Athletes (N = 81)a
| Age, y | 25.7 ± 4.3 (18-37) |
| Height, cm | 179.6 ± 8.9 (162-210) |
| Weight, kg | 77.6 ± 13.7 (47-115) |
| Body mass index, kg/m2 | 23.9 ± 7.6 (18-37) |
| Sport | |
| Soccer | 47 (58) |
| Futsal | 18 (22) |
| Handball | 5 (6) |
| Volleyball | 5 (6) |
| Basketball | 4 (5) |
| Shot put | 1 (1) |
| Table tennis | 1 (1) |
| Primary injury location by MRI grade | |
| Grade 0 | 14 (17) |
| Grade 1 | 20 (25) |
| Adductor longus | 14 (17) |
| Adductor brevis | 3 (4) |
| Adductor magnus | 1 (1) |
| Pectineus | 1 (1) |
| Obturator externus | 1 (1) |
| Grade 2 | 30 (37) |
| Adductor longus | 27 (33) |
| Pectineus | 1 (1) |
| Obturator externus | 2 (2) |
| Grade 3 | 17 (21) |
| Adductor longus | 17 (21) |
aData are reported as mean ± SD (range) or n (%). MRI, magnetic resonance imaging.
Compliance
Rehabilitation attendance for the 50 athletes who met the controlled sports training criteria was 89% (interquartile range [IQR], 76%-100%; range, 48%-100%). This was equivalent to 11.5 (IQR, 8-20; range, 4-72) supervised sessions, with 10 (IQR, 7-14; range, 4-23) sessions for athletes with grade 0-2 injuries and 40 (IQR, 26-47; range, 17-72) sessions for athletes with grade 3 injuries. Overall rehabilitation attendance for the 61 athletes who met the clinically pain-free criteria was 88% (IQR, 75%-100%; range, 31%-100%). This was equivalent to 10 (IQR, 7-18; range, 3-72) supervised sessions.
RTS Continuum
The duration until the 3 milestones within the RTS continuum is provided in Table 3 and Figure 4. There were no statistically significant differences in duration until any RTS milestone between athletes with MRI grade 0 and 1 (milestone 1: r = 0.06, P = .658; milestone 2: r = 0.08, P = .578; milestone 3: r = 0.13, P = .258), grade 0 and 2 (milestone 1: r = 0.14, P = .281; milestone 2: r = 0.20, P = .156; milestone 3: r = 0.13, P = .252), and grade 1 and 2 (milestone 1: r = 0.09, P = .504; milestone 2: r = 0.13, P = .348; milestone 3: r = 0.01, P = .902) injuries. There were statistically significant differences between athletes with grade 3 injuries versus those with grade 0-2 injuries (P < .001), for all RTS milestones. Athletes with grade 3 injuries had a considerably longer RTS duration than athletes with grade 0-2 injuries; standardized effect sizes were 0.674 (P < .001), 0.715 (P < .001), and 0.698 (P < .001) for each RTS milestone, respectively.
TABLE 3.
Duration From Injury to 3 RTS Milestonesa
| Clinically Pain-Free | Completion of Controlled Sports Training | Return to Full Team Training | ||||
|---|---|---|---|---|---|---|
| n | Duration, d | n | Duration, d | n | Duration, d | |
| All adductor injuries | 61 | 15 (12-29) [6-166] | 50 | 24 (16-34) [9-212] | 75 | 22 (15-33) [5-224] |
| MRI grade 0 | 12 | 13 (11-14) [6-23] | 9 | 16 (15-17) [10-27] | 13 | 17 (13-18) [5-27] |
| MRI grade 1 | 16 | 13 (11-17) [7-33] | 13 | 17 (16-21) [9-37] | 18 | 21 (16-26) [7-41] |
| MRI grade 2 | 20 | 17 (11-24) [7-44] | 16 | 25 (15-30) [10-64] | 28 | 21 (14-28) [7-57] |
| MRI grade 0-2 (grouped) | 48 | 13 (11-21) [6-44] | 38 | 17 (15-27) [9-64] | 59 | 18 (14-27) [5-57] |
| MRI grade 3 | 13 | 55 (31-75) [27-166] | 12 | 68 (51-84) [32-212] | 16 | 78 (68-98) [35-224] |
aData are reported as median (interquartile range) [range]. MRI, magnetic resonance imaging; RTS, return to sport.
Figure 4.
Duration in days from injury to each of the 3 different return-to-sport milestones visualized according to magnetic resonance imaging injury grading: (A) clinically pain-free (purple), (B) completion of controlled sports training (green), and (C) return to full team training (orange). Black lines represent median values, and dots represent individual athletes.
Clinical Measures
The athletes generally had high scores on all 5 included HAGOS subscales upon completion of the rehabilitation protocol (median, 96-100) (Table 4). Athletes generally had symmetric range of motion on the bent knee fall out and hip abduction tests (mean, 99% and 101%, respectively) (Table 4). Similarly, side-lying and supine eccentric adduction strength as well as side-lying eccentric abduction strength were generally also symmetric (mean, 97%, 99%, and 101%, respectively) (Table 4). An overview of the clinical results grouped according to MRI injury grading can be found in Appendix 3, Table A2.
TABLE 4.
Clinical Results of Self-reported Disability, Strength, and ROMa
| Initial Examination | Completion of Controlled Sports Training | |||
|---|---|---|---|---|
| n | Value | n | Value | |
| HAGOS Pain (0-100) | 48 | 75 (55-86) [20-100] | 47 | 100 (98-100) [78-100] |
| HAGOS Symptoms (0-100) | 48 | 57 (41-79) [0-93] | 47 | 96 (93-100) [68-100] |
| HAGOS ADL (0-100) | 48 | 75 (55-88) [10-100] | 47 | 100 (100-100) [80-100] |
| HAGOS Sport (0-100) | 48 | 31 (47-67) [6-100] | 47 | 100 (97-100) [63-100] |
| HAGOS QOL (0-100) | 48 | 65 (40-85) [10-100] | 47 | 100 (85-100) [25-100] |
| Pain on adductor palpation | 50 | 50 (100) | 50 | 3 (6) |
| Pain on adductor resistance | 50 | 46 (92) | 50 | 4 (8) |
| Pain on adductor stretch | 50 | 34 (68) | 50 | 0 (0) |
| Bent knee fall out test | 49 | 49 | ||
| LSI, % | 89 (63-107) [10-140] | 99 ± 18 (73-146) | ||
| Injured leg, cm | 18 (13-26) [5-40] | 14 ± 4 (4-27) | ||
| Uninjured leg, cm | 14 (12-18) [4-32] | 14 ± 5 (4-27) | ||
| Hip abduction ROM | 48 | 49 | ||
| LSI, % | 82 ± 25 (8-133) | 101 ± 7 (82-117) | ||
| Injured leg, deg | 35 ± 11 (4-58) | 47 ± 8 (30-67) | ||
| Uninjured leg, deg | 44 ± 9 (20-68) | 47 ± 8 (30-69) | ||
| Eccentric strength test ability | 47 | 28 (60) | 49 | 49 (100) |
| Eccentric adduction strength in side-lying position | 28 | 49 | ||
| LSI, % | 71 ± 23 (23-111) | 97 ± 13 (56-129) | ||
| Injured leg, N·m/kg | 2.1 ± 0.9 (0.5-3.8) | 3.3 ± 0.6 (2.0-4.8) | ||
| Uninjured leg, N·m/kg | 3.0 ± 0.5 (2.1-4.2) | 3.4 ± 0.6 (2.0-4.8) | ||
| Eccentric abduction strength in side-lying position | 28 | 49 | ||
| LSI, % | 94 ± 16 (64-128) | 101 ± 14 (67-134) | ||
| Injured leg, N·m/kg | 2.5 ± 0.6 (1.0-3.7) | 2.9 ± 0.5 (1.7-3.8) | ||
| Uninjured leg, N·m/kg | 2.7 ± 0.6 (1.6-4.0) | 2.8 ± 0.6 (1.8-4.0) | ||
| Adduction/abduction ratio | 28 | 49 | ||
| Injured leg | 0.85 ± 0.29 (0.19-1.28) | 1.18 ± 0.23 (0.69-1.81) | ||
| Uninjured leg | 1.13 ± 0.26 (0.63-1.54) | 1.24 ± 0.29 (0.77-2.19) | ||
| Eccentric adduction strength in supine position | N/A | 49 | ||
| LSI, % | N/A | 99 ± 17 (47-135) | ||
| Injured leg, N·m/kg | N/A | 3.0 ± 0.7 (1.6-4.7) | ||
| Uninjured leg, N·m/kg | N/A | 3.0 ± 0.6 (1.8-4.4) | ||
aData are reported as median (interquartile range) [range], n (%), or mean ± SD (range). Missing data: 2 athletes did not complete the HAGOS questionnaire at both time points, and 1 did not complete the questionnaire at discharge; 2 athletes did not perform the hip abduction ROM and 1 athlete did not perform the bent knee fall out test because of pain during the initial examination; and 3 athletes were not able to perform the strength tests during the initial examination, and 1 athlete did not perform ROM and strength tests at the completion of rehabilitation because of device malfunction. Eccentric strength results are only reported for athletes who were able to perform the eccentric adduction test. ADL, Activities of Daily Living; HAGOS, Copenhagen Hip and Groin Outcome Score; LSI, limb symmetry index; N/A, not applicable; QOL, Quality of Life; ROM, range of motion.
Subsequent Injuries
There were 6 athletes (8%) who had a reinjury within the first year, and the majority of these (5/6) occurred within the first 2 months after returning to full team training (Table 5). An overview of reinjuries grouped according to MRI injury grading can be found in Appendix 3, Table A3.
TABLE 5.
Subsequent Groin Pain According to RTS Milestones and Time After RTSa
| Return to Full Team Training | Completion of Controlled Sports Training | No Completion of Controlled Sports Training | Clinically Pain-Free | Not Clinically Pain-Free | |
|---|---|---|---|---|---|
| All adductor injuries, n | 75 | 50 | 25 | 61 | 14 |
| Reinjury | |||||
| 0-2 mo | 5/74 (7) | 2/50 (4) | 3/24 (13) | 2/60 (3) | 3/14 (21) |
| 0-6 mo | 6/73 (8) | 3/49 (6) | 3/24 (13) | 3/59 (5) | 3/14 (21) |
| 0-12 mo | 6/72 (8) | 3/48 (6) | 3/24 (13) | 3/58 (5) | 3/14 (21) |
| Other groin pain | |||||
| 0-2 mo | 10/74 (14) | 7/50 (14) | 3/24 (13) | 8/60 (13) | 2/14 (14) |
| 0-6 mo | 13/73 (18) | 9/49 (18) | 4/24 (17) | 11/59 (19) | 2/14 (14) |
| 0-12 mo | 15/72 (21) | 9/48 (19) | 6/24 (25) | 12/58 (21) | 3/14 (21) |
aData are reported as No. of subsequent injuries/No. of athletes contacted at the respective time point (%) unless otherwise indicated. Missing data: 3 athletes could not be contacted for follow-up at ≥1 time points within 12 months after RTS because they moved to different countries. RTS, return to sport.
Athletes who achieved RTS milestone 1 (clinically pain-free) had a lower proportion of reinjuries than athletes who did not (Table 5). This difference was statistically significant at all time points with small to moderate effect sizes (0-2 months: 3% vs 21%, respectively, ϕ = –0.282, P = .015; 0-6 months: 5% vs 21%, respectively, ϕ = –0.234, P = .045; 0-12 months: 5% vs 21%, respectively, ϕ = –0.233, P = .048). There was a similar proportion of athletes who reported other groin pain at any time point, regardless of achieving RTS milestone 1 (0-2 months: 13% vs 14%, respectively, ϕ = –0.011, P = .925; 0-6 months: 19% vs 14%, respectively, ϕ = –0.045, P = .702; 0-12 months: 21% vs 21%, respectively, ϕ = –0.007, P = .951) (Table 5).
There was no statistically significant difference at any time point in the rate of reinjuries between those who achieved RTS milestone 2 (controlled sports training) and those who did not (0-2 months: 4% vs 13%, respectively, ϕ = −0.159, P = .173; 0-6 months: 6% vs 13%, respectively, ϕ = −0.109, P = .351; 0-12 months: 6% vs 13%, respectively, ϕ = −0.107, P = .366) (Table 5). There was a similar proportion of athletes reporting other types of groin pain at any time point, regardless of achieving RTS milestone 2 (0-2 months: 14% vs 13%, respectively, ϕ = 0.021, P = .860; 0-6 months: 18% vs 17%, respectively, ϕ = 0.021, P = .858; 0-12 months: 19% vs 25%, respectively, ϕ = −0.073, P = .538) (Table 5).
Discussion
Our study describes a group of 75 athletes with acute adductor injuries who underwent a standardized criteria-based rehabilitation program. The athletes had a relatively large range in RTS duration, with most returning to full team training within 1 month. The majority of athletes with an MRI grade 0-2 injury completed our standardized criteria-based rehabilitation protocol in 2 to 4 weeks, whereas athletes with an MRI grade 3 injury completed the protocol in 2 to 3 months.
The RTS duration for athletes with a grade 3 injury in our study is similar to those reported in 2 small case series of nonoperative treatment of adductor longus avulsions. In a study of 14 American football players with complete adductor longus avulsions, all athletes returned to sport with a mean missed playing time of 6.1 ± 3.1 weeks (range, 3-12 weeks) using a variety of rehabilitation protocols.18 Similarly, 6 elite athletes (soccer and ice hockey) all returned to sport without functional deficiencies using a structured nonoperative approach in 89 ± 13 days (range, 75-110 days).29 In comparison, case series on operative treatment have reported mean RTS durations of around 12 to 21 weeks.3,18,26
The RTS duration for athletes with grade 0-2 adductor injuries in our study is comparable with a large epidemiological study of elite male European soccer players in which an average of 14 ± 6.2 days (range, 0-361 days) of absence from sport was reported.7 In that study, 49% of injuries resulted in less than 7 days of absence. In our study, no athletes completed controlled sports training within 7 days. This may partially be because of the required progression criteria but more likely because of a selection bias, as athletes with minor injuries may not have presented at our hospital and thus were not included. This is indicated by a median duration from injury to the first rehabilitation session of 4 days (IQR, 3-6 days) in our study. Another study used a retrospective review of MRI scans in 20 male elite soccer players with acute adductor longus injuries in which 15 players had noncomplete injuries.17 These 15 players also had an RTS duration of 2 to 4 weeks. Neither the treatment nor RTS criteria were reported in that study. Most elite athletes likely receive a high quality of treatment. In contrast, recreational athletes with acute muscle injuries can have a considerably longer duration of RTS, with reported medians of 2 and 3 months depending on the time of treatment initiation.2
For elite athletes, a standardized criteria-based rehabilitation program and specific RTS criteria may be more important for the risk of reinjuries rather than for the mean RTS duration, as the RTS duration was similar to other studies. In our study, we had a low reinjury rate of 4% within 2 months and 6% within 1 year in athletes who met the RTS criteria. In epidemiological studies on elite European soccer, the early reinjury rate (0-2 months) was reported to be 18% after acute adductor injuries.7 In elite soccer in Qatar, a 27% reinjury rate within 2 seasons was reported after acute groin injuries.16 This could indicate that following a criteria-based rehabilitation protocol may reduce the reinjury risk, and we encourage further studies on this.
The RTS criteria in our study were all related to pain during tests and sports function, whereas other elements, such as range of motion and strength asymmetry, are often suggested as key decision variables. In acute hamstring injuries, localized discomfort during muscle palpation and discomfort during muscle resistance tests just after RTS were associated with a higher risk of reinjuries, whereas range of motion and strength deficits did not differentiate those at an increased risk.6 It is unknown if adding any range of motion and strength criteria could have further reduced the number of adductor reinjuries in our study. It is notable that the mean limb symmetry indices for both strength and range of motion measures were all around 100% at the completion of controlled sports training, except for supine eccentric adduction strength in athletes with a grade 3 adductor injury (limb symmetry index, 80% ± 17%, Appendix 3).
Strengths and Limitations
Using a standardized criteria-based rehabilitation program is one strength of our study, as this minimized variation in the treatment received that could potentially have influenced the RTS duration. The exercise program was performed with minimal equipment requirements, improving the generalizability and implementation potential.
Because of the lack of a control group, it is uncertain whether the exercise program had any influence on the RTS duration. The content of the exercise protocol used in this study was based on available literature on both healthy and injured participants as well as on clinical experience in managing athletes with acute groin injuries. Additionally, pilot testing of 40 patients was performed during the development of the protocol. There are many elements that we believe are important in our protocol, such as early activation, structured progression of intensity and volume, exercising with minor pain, a split program ensuring muscle-specific recovery, and early initiation of running and change of direction. We recognize that a different exercise program may also give similar results; however, few comparisons are possible, as larger epidemiological studies do not specify included rehabilitation protocols.7,30 In comparison, a time-based progression was used in a study on recreational athletes with muscle injuries, in which dynamic resistance exercises were not included until 4 weeks after the injury.2 At this time point, the majority of athletes in our study had already resumed full team training, suggesting that the structure of an exercise-based rehabilitation program can influence the RTS duration. We did not standardize the exercise selection of the nongroin exercises to allow some flexibility in the treatment, as usually required for elite athletes from different sports. The effect of these exercises on RTS duration and reinjuries is uncertain.
A key strength of the protocol is the specific criteria for RTS milestones 1 and 2, which improve uniformity and generalizability. It is common that, even with a defined RTS (eg, full team training), there can be many nonmedical factors that influence the decision on when RTS occurs.25 Specific RTS criteria are often not reported in studies on acute muscle injuries.7,30 Thus, athletes may not be pain-free at RTS or may have been exposed to maximal sport-specific training before RTS, which blurs direct comparisons. The criteria that we included in this study make future objective comparisons possible. Our RTS milestone 3 (return to full team training) is, however, still influenced by the same RTS decision-making limitations as the larger epidemiological studies, in that nonmedical factors may influence the RTS time point.
Another limitation of this study is the small number of athletes included, especially for the evaluation of reinjuries. Furthermore, there was no standardized clinical or imaging examination of all subsequent injuries, which were registered based on telephone calls to the athletes. This is the largest detailed study on acute adductor injuries in athletes to date, but the results may only be considered an initial step toward a more detailed focus on the treatment of acute adductor injuries. All athletes were male, and the majority of athletes (80%) were participating in football-codes (soccer and futsal); thus, extrapolation to other types and levels of sport and to female athletes should be done cautiously.
Conclusion
Our exploratory study describes the content and results of a standardized criteria-based rehabilitation protocol for acute adductor injuries in male athletes. There was a relatively large range in time needed to reach the 3 RTS milestones, with most athletes returning to full team training within 1 month. Athletes with an MRI grade 0-2 adductor injury were clinically pain-free in around 2 weeks and returned to full team training in around 3 weeks. Athletes with grade 3 adductor injury were clinically pain-free and returned to full team training within 3 months. The overall reinjury rate was 8%. Completing a criteria-based protocol, especially meeting clinically pain-free criteria, may result in fewer reinjuries.
Supplemental Material
Supplemental Material, DS_10.1177_2325967119897247 for Return to Sport After Criteria-Based Rehabilitation of Acute Adductor Injuries in Male Athletes: A Prospective Cohort Study by Andreas Serner, Adam Weir, Johannes L. Tol, Kristian Thorborg, Sean Lanzinger, Roald Otten and Per Hölmich in Orthopaedic Journal of Sports Medicine
Acknowledgment
The authors acknowledge all the physical therapists who were involved in the rehabilitation of the athletes (Damien Delahunty, Philipp Jacobsen, Abdallah Itani, Kostas Epameinontidis, Einar Einarsson, Grani Gardarsson, and Dermot Simpson), the sports rehabilitators (Polyvios Kyritsis and Theodosia Palli), the radiologists involved in this project (Frank Roemer, Ali Guermazi, and Eduardo Yamashiro), the Aspetar sports medicine physicians, and the doctors and physical therapists from the National Sports Medicine Program, all of whom have contributed to making this project possible.
Footnotes
Final revision submitted November 15, 2019; accepted November 24, 2019.
One or more of the authors has declared the following potential conflict of interest or source of funding: The publication fee for this article was funded by Aspetar Orthopaedic and Sports Medicine Hospital. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Shafallah Medical Genetics Center (project No. 2012-013) and the Anti-Doping Lab Qatar institutional review board (EXT2014000004).
Supplemental Material: Appendices 1-3 for this article are available at http://journals.sagepub.com/doi/suppl/10.1177/2325967119897247
References
- 1. Ardern CL, Glasgow P, Schneiders A, et al. 2016 consensus statement on return to sport from the First World Congress in Sports Physical Therapy, Bern. Br J Sports Med. 2016;50(14):853–864. [DOI] [PubMed] [Google Scholar]
- 2. Bayer ML, Magnusson SP, Kjaer M; Tendon Research Group Bispebjerg. Early versus delayed rehabilitation after acute muscle injury. N Engl J Med. 2017;377(13):1300–1301. [DOI] [PubMed] [Google Scholar]
- 3. Bharam S, Feghhi DP, Porter DA, Bhagat PV. Proximal adductor avulsion injuries: outcomes of surgical reattachment in athletes. Orthop J Sports Med. 2018;6(7):2325967118784898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Creighton DW, Shrier I, Shultz R, Meeuwisse WH, Matheson GO. Return-to-play in sport: a decision-based model. Clin J Sport Med. 2010;20(5):379–385. [DOI] [PubMed] [Google Scholar]
- 5. Delmore RJ, Laudner KG, Torry MR. Adductor longus activation during common hip exercises. J Sport Rehabil. 2014;23(2):79–87. [DOI] [PubMed] [Google Scholar]
- 6. De Vos R-J, Reurink G, Goudswaard G-J, Moen MH, Weir A, Tol JL. Clinical findings just after return to play predict hamstring re-injury, but baseline MRI findings do not. Br J Sports Med. 2014;48(18):1377–1384. [DOI] [PubMed] [Google Scholar]
- 7. Ekstrand J, Hägglund M, Waldén M. Epidemiology of muscle injuries in professional football (soccer). Am J Sports Med. 2011;39(6):1226–1232. [DOI] [PubMed] [Google Scholar]
- 8. Finch CF, Cook J. Categorising sports injuries in epidemiological studies: the subsequent injury categorisation (SIC) model to address multiple, recurrent and exacerbation of injuries. Br J Sports Med. 2014;48(17):1276–1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fuller CW, Ekstrand J, Junge A, et al. Consensus statement on injury definitions and data collection procedures in studies of football (soccer) injuries. Scand J Med Sci Sports. 2006;16(2):83–92. [DOI] [PubMed] [Google Scholar]
- 10. Hölmich P, Uhrskou P, Ulnits L, et al. Effectiveness of active physical training as treatment for long-standing adductor-related groin pain in athletes: randomised trial. Lancet. 1999;353(9151):439–443. [DOI] [PubMed] [Google Scholar]
- 11. Ishøi L, Sørensen CN, Kaae NM, Jørgensen LB, Hölmich P, Serner A. Large eccentric strength increase using the Copenhagen adduction exercise in football: a randomized controlled trial. Scand J Med Sci Sports. 2016;26(11):1334–1342. [DOI] [PubMed] [Google Scholar]
- 12. Jensen J, Hölmich P, Bandholm T, Zebis MK, Andersen LL, Thorborg K. Eccentric strengthening effect of hip-adductor training with elastic bands in soccer players: a randomised controlled trial. Br J Sports Med. 2014;48(4):332–338. [DOI] [PubMed] [Google Scholar]
- 13. Kim H-Y. Statistical notes for clinical researchers: chi-squared test and Fisher’s exact test. Restor Dent Endod. 2017;42(2):152–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. King E, Franklyn-Miller A, Richter C, et al. Clinical and biomechanical outcomes of rehabilitation targeting intersegmental control in athletic groin pain: prospective cohort of 205 patients. Br J Sports Med. 2018;52(16):1054–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Krommes K, Bandholm T, Jakobsen MD, et al. Dynamic hip adduction, abduction and abdominal exercises from the Hölmich groin-injury prevention program are intense enough to be considered strengthening exercises: a cross-sectional study. Int J Sports Phys Ther. 2017;12(3):371–380. [PMC free article] [PubMed] [Google Scholar]
- 16. Mosler AB, Weir A, Eirale C, et al. Epidemiology of time loss groin injuries in a men’s professional football league: a 2-year prospective study of 17 clubs and 606 players. Br J Sports Med. 2018;52(5):292–297. [DOI] [PubMed] [Google Scholar]
- 17. Pezzotta G, Pecorelli A, Querques G, Biancardi S, Morzenti C, Sironi S. MRI characteristics of adductor longus lesions in professional football players and prognostic factors for return to play. Eur J Radiol. 2018;108:52–58. [DOI] [PubMed] [Google Scholar]
- 18. Schlegel TF, Bushnell BD, Godfrey J, Boublik M. Success of nonoperative management of adductor longus tendon ruptures in National Football League athletes. Am J Sports Med. 2009;37(7):1394–1399. [DOI] [PubMed] [Google Scholar]
- 19. Serner A, Jakobsen MD, Andersen LL, Hölmich P, Sundstrup E, Thorborg K. EMG evaluation of hip adduction exercises for soccer players: implications for exercise selection in prevention and treatment of groin injuries. Br J Sports Med. 2014;48(14):1108–1114. [DOI] [PubMed] [Google Scholar]
- 20. Serner A, Roemer FW, Hölmich P, et al. Reliability of MRI assessment of acute musculotendinous groin injuries in athletes. Eur Radiol. 2017;27(4):1486–1495. [DOI] [PubMed] [Google Scholar]
- 21. Serner A, Tol JL, Jomaah N, et al. Diagnosis of acute groin injuries: a prospective study of 110 athletes. Am J Sports Med. 2015;43(8):1857–1864. [DOI] [PubMed] [Google Scholar]
- 22. Serner A, van Eijck CH, Beumer BR, Hölmich P, Weir A, de Vos R-J. Study quality on groin injury management remains low: a systematic review on treatment of groin pain in athletes. Br J Sports Med. 2015;49(12):813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Serner A, Weir A, Tol JL, et al. Can standardised clinical examination of athletes with acute groin injuries predict the presence and location of MRI findings? Br J Sports Med. 2016;50(24):1541–1547. [DOI] [PubMed] [Google Scholar]
- 24. Serner A, Weir A, Tol JL, et al. Characteristics of acute groin injuries in the adductor muscles: a detailed MRI study in athletes. Scand J Med Sci Sports. 2018;28(2):667–676. [DOI] [PubMed] [Google Scholar]
- 25. Shrier I. Strategic Assessment of Risk and Risk Tolerance (StARRT) framework for return-to-play decision-making. Br J Sports Med. 2015;49(20):1311–1315. [DOI] [PubMed] [Google Scholar]
- 26. Tansey RJ, Benjamin-Laing H, Jassim S, Liekens K, Shankar A, Haddad FS. Successful return to high-level sports following early surgical repair of combined adductor complex and rectus abdominis avulsion. Bone Joint J. 2015;97(11):1488–1492. [DOI] [PubMed] [Google Scholar]
- 27. Thorborg K, Bandholm T, Zebis M, Andersen LL, Jensen J, Hölmich P. Large strengthening effect of a hip-flexor training programme: a randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. 2016;24(7):2346–2352. [DOI] [PubMed] [Google Scholar]
- 28. Thorborg K, Holmich P, Christensen R, Petersen J, Roos EM. The Copenhagen Hip and Groin Outcome Score (HAGOS): development and validation according to the COSMIN checklist. Br J Sports Med. 2011;45(6):478–491. [DOI] [PubMed] [Google Scholar]
- 29. Ueblacker P, English B, Mueller-Wohlfahrt H-W. Nonoperative treatment and return to play after complete proximal adductor avulsion in high-performance athletes. Knee Surg Sports Traumatol Arthrosc. 2016;24(12):3927–3933. [DOI] [PubMed] [Google Scholar]
- 30. Werner J, Hägglund M, Ekstrand J, Waldén M. Hip and groin time-loss injuries decreased slightly but injury burden remained constant in men’s professional football: the 15-year prospective UEFA Elite Club Injury Study. Br J Sports Med. 2019;53(9):539–546. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, DS_10.1177_2325967119897247 for Return to Sport After Criteria-Based Rehabilitation of Acute Adductor Injuries in Male Athletes: A Prospective Cohort Study by Andreas Serner, Adam Weir, Johannes L. Tol, Kristian Thorborg, Sean Lanzinger, Roald Otten and Per Hölmich in Orthopaedic Journal of Sports Medicine