Abstract
This study uses Surveillance, Epidemiology, and End Results (SEER) registry data to describe trends in thyroid cancer incidence overall and by tumor size in the United States from 1992 to 2016.
The incidence of thyroid cancer in the United States tripled between 1974 and 2013, increasing from 4.5 to 14.4 per 100 000 population.1,2 This increase has primarily been attributed to increasing detection of a subclinical reservoir of small thyroid cancers, although a concurrent increase in the true incidence of disease has not been ruled out. Autopsy studies reveal that many persons without known thyroid disease (4%-11%) harbor clinically occult thyroid cancers, suggesting that increasing health care utilization and imaging technologies have led to the detection of increasing numbers of cancers, without a change in the actual occurrence of thyroid cancer.1,3
In parallel, the incidence of thyroid cancer in South Korea increased to a level 15 times greater in 2011 than in 1993, attributed to a widespread practice of screening healthy persons with thyroid ultrasound.4 As awareness of this phenomenon emerged among physicians and the public, and screening practices were curtailed, the incidence of thyroid cancer in South Korea reversed, first declining in 2014.4
Our objective was to determine whether trends in US thyroid cancer incidence have changed in recent years.
Methods
Trends in the age-adjusted incidence of thyroid cancer from 1992 to 2016 (all histologies, stratified by size, with reporting delay adjustment) were analyzed in the Surveillance, Epidemiology, and End Results (SEER) 13 registry, a population-based cancer surveillance registry from 13 geographic regions representing 14% of the US population, using SEER*Stat version 8.3.6 (National Cancer Institute). Segmented log-linear regression was used to determine break points and annual percentage change (APC). Changes in time series trends were assessed by examining differences in slope between segments with a 1-tailed t test (Joinpoint 4.7; https://surveillance.cancer.gov/joinpoint/). The threshold for significance was P < .05. The Weill Cornell Medicine institutional review board deemed this study exempt from review and patient consent. A data use agreement was signed with the SEER program.
Results
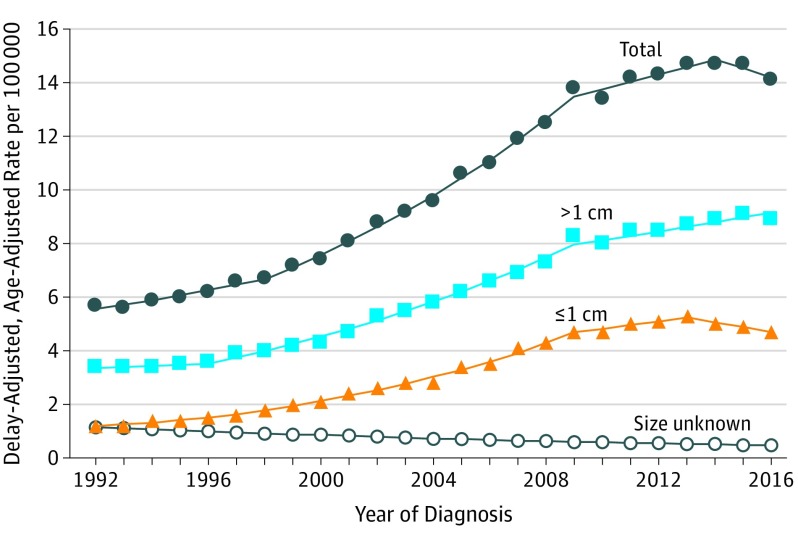
Age-adjusted thyroid cancer incidence in the United States increased from 5.7 to 13.8 per 100 000 between 1992 and 2009, with the greatest APC (6.6% [95% CI, 6.2%-7.0%]) from 1998 to 2009. The rate of increase significantly slowed from 2009 to 2014 (incidence, 13.8 to 14.7 per 100 000; APC, 2.0% [95% CI, 0.3%-3.7%]; change in slope, t = −5.4; P < .001). Since 2014, the incidence of thyroid cancer has been stable (from 14.7 to 14.1 per 100 000; APC, −2.4% [95% CI, −7.5% to 3.1%]; change in slope, t = −1.7; P = .06) (Figure and Table).
Figure. Trends in Thyroid Cancer Incidence Rates, Stratified by Tumor Size, 1992-2016.
Age-adjusted incidence per 100 000, adjusted for reporting delay, of thyroid cancer in the US Surveillance, Epidemiology, and End Results 13 registry from 1992 to 2016. The data markers indicate the observed incidence at each year. The lines represent trends based on segmented regression (Table). In the most recent periods, the annual percentage change in incidence rates for all thyroid cancers was −2.4%; for cancers greater than 1 cm, +2.0%; for subcentimeter cancers, −3.7%.
Table. Trends in Thyroid Cancer Incidence in the United States, 1992-2016.
| Tumor Size by Year | APC (95% CI)a | Change in APC | P Value for Change in APCb |
|---|---|---|---|
| All Sizes | |||
| 1992-1998 | 3.1 (2.2 to 4.1) | ||
| 1998-2009 | 6.6 (6.2 to 7.0) | +3.5 | <.001 |
| 2009-2014 | 2.0 (0.3 to 3.7) | −4.6 | <.001 |
| 2014-2016 | −2.4 (−7.5 to 3.1) | −4.4 | .06 |
| ≤1 cm | |||
| 1992-1996 | 6.2 (2.6 to 9.8) | ||
| 1996-2009 | 9.1 (8.4 to 9.8) | +2.9 | .06 |
| 2009-2013 | 2.9 (−2.5 to 8.6) | −6.2 | .02 |
| 2013-2016 | −3.7 (−8.7 to 1.7) | −6.6 | .04 |
| >1 cm | |||
| 1992-1996 | 1.1 (−1.0 to 3.3) | ||
| 1996-2009 | 6.5 (6.1 to 6.9) | +5.4 | <.001 |
| 2009-2016 | 2.0 (1.1 to 2.9) | −4.5 | <.001 |
| Unknown Size | |||
| 1992-2016 | −3.6 (−4.1 to −3.2) | ||
Abbreviation: APC, annual percentage change.
Time intervals are bounded by break points in the trend line, as determined by multiple permutation testing.
The P value for change in APC reflects testing of the change in slope of APC via 1-tailed t test for each period compared with the preceding period.
The incidence of subcentimeter thyroid cancers steadily increased from 1992 to 2009, from 1.2 to 4.7 per 100 000, with the greatest APC (9.1% [95% CI, 8.4%-9.8%]) from 1996 to 2009. The trend stabilized from 2009 to 2013 (incidence, 4.7 to 5.3 per 100 000; APC, 2.9% [95% CI, −2.5% to 8.6%]; change in slope, t = −2.3; P = .02), and then declined from 2013 to 2016 (incidence, 5.3 to 4.7 per 100 000; APC, −3.7% [95% CI, −8.7% to 1.7%]; change in slope, t = −1.9; P = .04) (Figure and Table).
Discussion
Between 2009 and 2016, after 3 decades of rapid increase,1 the incidence of thyroid cancer incidence in the United States reached a plateau and possibly started to decline. Increasing trends in the incidence of subcentimeter thyroid cancers, most prone to increasing detection, began to reverse direction between 2013 and 2016. Limitations of this study include the nature of observational analyses, which cannot prove causality, and that the trends may not generalize to other areas of the United States beyond the SEER 13 geographic regions.
Although a true decline in the occurrence of thyroid cancer is a possible explanation for these changing trends, less intensive workup of thyroid nodules is more likely. These changes have occurred during a time of evolving understanding of overdiagnosis and the indolent nature of many small thyroid cancers, reflected in changing clinical practice guidelines, including recommendations against screening for thyroid cancer by the US Preventive Services Task Force in 2017.5 Recently, several US professional societies have developed radiographic classification systems for thyroid nodules and introduced risk-stratified recommendations against routine biopsy of nodules more likely to be benign or represent indolent cancers. For example, in 2009 and 2015, American Thyroid Association guidelines introduced size and appearance-based criteria, recommending observation rather than immediate biopsy for many smaller, lower-risk nodules.6
Section Editor: Jody W. Zylke, MD, Deputy Editor.
References
- 1.Lim H, Devesa SS, Sosa JA, Check D, Kitahara CM. Trends in thyroid cancer incidence and mortality in the United States, 1974-2013. JAMA. 2017;317(13):1338-1348. doi: 10.1001/jama.2017.2719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Davies L, Welch HG. Increasing incidence of thyroid cancer in the United States, 1973-2002. JAMA. 2006;295(18):2164-2167. doi: 10.1001/jama.295.18.2164 [DOI] [PubMed] [Google Scholar]
- 3.Furuya-Kanamori L, Bell KJL, Clark J, Glasziou P, Doi SAR. Prevalence of differentiated thyroid cancer in autopsy studies over six decades: a meta-analysis. J Clin Oncol. 2016;34(30):3672-3679. doi: 10.1200/JCO.2016.67.7419 [DOI] [PubMed] [Google Scholar]
- 4.Ahn HS, Welch HG. South Korea’s thyroid-cancer “epidemic”—turning the tide. N Engl J Med. 2015;373(24):2389-2390. doi: 10.1056/NEJMc1507622 [DOI] [PubMed] [Google Scholar]
- 5.Bibbins-Domingo K, Grossman DC, Curry SJ, et al. ; US Preventive Services Task Force . Screening for thyroid cancer: US Preventive Services Task Force recommendation statement. JAMA. 2017;317(18):1882-1887. doi: 10.1001/jama.2017.4011 [DOI] [PubMed] [Google Scholar]
- 6.Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016;26(1):1-133. doi: 10.1089/thy.2015.0020 [DOI] [PMC free article] [PubMed] [Google Scholar]