Key Points
Question
Are the ocular changes that develop in a ground-based analogue of weightlessness similar to the ocular changes experienced by astronauts during weightlessness?
Findings
Peripapillary total retinal thickness increased to a greater degree among individuals exposed to bed rest than among astronauts during spaceflight, while choroidal thickening developed only among astronauts during spaceflight.
Meaning
Differences in peripapillary total retinal thickness and choroidal thickness observed in astronauts vs individuals exposed to bed rest suggest that the mechanism(s) underlying optic disc edema may differ between those groups.
Abstract
Importance
Optic disc edema develops in astronauts during long-duration spaceflight and is a risk for all future astronauts during spaceflight. Having a ground-based analogue of weightlessness that reproduces critical features of spaceflight-associated neuro-ocular syndrome will facilitate understanding, preventing, and/or treating this syndrome.
Objective
To determine whether the ocular changes in individuals exposed to an analogue of weightlessness are similar to the ocular changes in astronauts exposed to a duration of spaceflight comparable to this analogue of weightlessness.
Design, Setting, and Participants
This cohort study, conducted from 2012 to 2018, investigated 11 healthy test participants before, during, and after 30 days of strict 6° head-down tilt bed rest as well as 20 astronauts before and during approximately 30 days of spaceflight. Data were collected at NASA Johnson Space Center, the German Aerospace Center, and on board the International Space Station. Statistical analysis was performed from February 13 to April 24, 2019.
Main Outcomes and Measures
Peripapillary total retinal thickness and peripapillary choroid thickness quantified from optical coherence tomography images.
Results
Peripapillary total retinal thickness increased to a greater degree among 11 individuals (6 men and 5 women; mean [SD] age, 33.4 [8.0 years]) exposed to bed rest than among 20 astronauts (17 men and 3 women; mean [SD] age, 46.0 [6.0] years), with a mean difference between groups of 37 μm (95% CI, 13-61 μm; P = .005). Conversely, choroid thickness did not increase among the individuals exposed to bed rest but increased among the astronauts, resulting in a mean difference between groups of 27 μm (95% CI, 14-41 μm; P < .001).
Conclusions and Relevance
These findings suggest that strict head-down tilt bed rest produces a different magnitude of edema than occurs after a similar duration of spaceflight, and no change in choroid thickness. It is possible that a mild, long-term elevation in intracranial pressure experienced by individuals exposed to bed rest is greater than the intracranial pressure experienced by astronauts during spaceflight, which may explain the different severity of optic disc edema between the cohorts. Gravitational gradients that remain present during bed rest may explain the lack of increase in choroid thickness during bed rest, which differs from the lack of gravitational gradients during spaceflight. Despite the possibility that different mechanisms may underlie optic disc edema development in modeled and real spaceflight, use of this terrestrial model of spaceflight-associated neuro-ocular syndrome will be assistive in the development of effective countermeasures that will protect the eyes of astronauts during future space missions.
This cohort study examines whether the ocular changes in individuals exposed to an analogue of weightlessness are similar to the ocular changes in astronauts exposed to a duration of spaceflight comparable to this analogue of weightlessness.
Introduction
Optic disc edema, the primary finding leading to the diagnosis of spaceflight-associated neuro-ocular syndrome (SANS), occurs in approximately 15% of astronauts flying long-duration missions to the International Space Station (ISS)1,2,3 but, to our knowledge, has not been observed in individuals participating in the traditional spaceflight analogue of 6° head-down tilt bed rest (BR).4,5 The traditional analogue allowed participants to use a pillow and to raise onto an elbow during meals, which may have limited the headward fluid shift and lowered intracranial pressure (ICP), as previously suggested.6 Therefore, NASA recently modified the traditional BR model by requiring individuals to maintain a strict head-down tilt position to sustain the hydrostatic pressure gradient toward the head and by including a mild hypercapnic environment similar to levels of carbon dioxide (CO2) that occur on the ISS.7 These modifications have been associated with the development of optic disc edema in 45% of individuals after 30 days of BR.8
The purpose of this study was to compare 2 structural changes of the eye during BR and spaceflight. Given that ICP is higher during head-down tilt than in the supine posture,9,10 yet ICP during weightlessness is less than supine posture,6 we hypothesized that there would be a greater magnitude of optic disc edema and choroidal thickening in individuals during BR than in astronauts during spaceflight.
Methods
In this cohort study, conducted from October 4 to December 4, 2017, 11 healthy test participants (6 men and 5 women) volunteered to participate in a 30-day strict 6° head-down tilt BR study conducted at the German Aerospace Center: envihab facility.8 Data from 20 astronauts (17 men and 3 women) collected from 2012 to 2018 were analyzed from before spaceflight and during approximately 30 days of spaceflight. Data from 7 novice astronauts (3 men and 4 women) who have not flown in space were collected and analyzed from 2 occasions approximately 4 months apart (range, 112-147 days). The Institutional review boards at NASA Johnson Space Center and the German Aerospace Center and the Human Research Multilateral Review Board that governs human participant research on the ISS approved all protocols, and all participants provided written informed consent.
Optical Coherence Tomography
Optical coherence tomography (OCT) images were acquired from a radial pattern of B-scans centered over the optic disc (BR: 24 B-scans, 20°, automatic real-time tracking [ART] = 50, enhanced depth imaging, high-resolution mode; spaceflight: 12 or 24 B-scans, 20°, ART = 16, high-resolution mode [OCT1]) using the Spectralis (Heidelberg Engineering) with active eye tracking. Optical coherence tomography images were collected before BR and after the first 24 hours, 15 days, and 30 days of head-down tilt BR, and 6 and 13 days after BR. A separate set of OCT images (12 B-scans in a radial pattern centered over the optic nerve head, ART = 50, high-resolution mode [OCT2]) were acquired from 5 individuals in the seated position before BR, on the first day after BR, and 6 months after BR who received a diagnosis of Frisén grade optic disc edema after 30 days of head-down tilt BR8 to track recovery. Astronauts underwent imaging before spaceflight and during a median of 37 days (range, 22-47 days) of spaceflight. Optical coherence tomography images were linked within individuals using the follow-up feature to ensure that repeated tests were performed in the same anatomical location. Segmentation of the internal limiting membrane, the Bruch membrane, and the Bruch membrane opening were verified manually by 2 independent readers. Using custom-written Matlab code, the mean peripapillary total retinal thickness (TRT) in an ellipse from the Bruch membrane opening to 250 μm was quantified as previously described.11 The retinal nerve fiber layer circle scan was used to quantify choroid thickness by manually segmenting the choroid scleral border, which could be reliably delineated in only 14 of the 20 astronauts from images collected during spaceflight. For all images, thickness measures from 2 readers needed to be less than 10% apart to pass quality control, and the mean of both measures was used for analysis.
Precision Testing
To quantify our precision to detect subtle changes in peripapillary TRT and choroid thickness that are greater than our day-to-day measurement variability, we measured TRT and choroid thickness on 2 occasions in novice astronauts in the seated, supine, and 15° head-down tilt postures. The statistical distribution of these measures was modeled with a Bayesian hierarchical model incorporating random effects for each source of variation (individual, session, position, analyzer, and residual error). Peripapillary TRT was modeled according to the following equations. For observation i, TRTi ~ norm (μi, τe), where μ = θanalyzer + θposition + θsession + θparticipant. The random-effects θ distributions were assumed independent normal with means of 0 and precisions (1/variance) of τanalyzer, τposition, τsession, and τparticipant. The hyperpriors on the all the precision parameters τ were modeled as independent diffuse (uninformative) gamma distributions, and the population mean, α0, was modeled as a diffuse normal distribution. Total variation was estimated as the sum of all the different components other than between individuals. WinBugs (MRC Biostatistics Unit, University of Cambridge) was used to generate posterior distributions, and after 10 000 burn-in, 50 000 Gibbs samples resulted in a median estimate of 9.7 μm for 1 SD of the variability in peripapillary TRT owing to analyzer, position, day, and residual. Assuming a normal test-retest distribution, values within 2 SDs capture 95% of the expected changes owing to all sources of error and physiological variability not associated with optic disc edema. Therefore, under that distributional assumption, a change in peripapillary TRT of more than 19.4 μm would have a less than 5% chance of being observed owing to sampling error or normal physiological variability. We interpret this threshold to represent a conservative estimate of the change in peripapillary TRT between 2 time points that represents the earliest signs of optic disc edema. The same approach was applied to the choroid thickness data and resulted in an estimate of 22.2 μm for 2 SDs of the day-to-day variability in choroid thickness.
Statistical Analysis
Statistical analyses of the changes associated with BR and spaceflight were conducted from February 13 to April 24, 2019, using linear mixed-effects models. These models used change in retinal or choroid thickness (from baseline) as the dependent variable and a fixed effect for time (BR days) to analyze the BR-associated time course. This fixed effect was replaced with group for the comparisons between individuals participating in BR and astronauts in spaceflight. Individual-specific random effects were included to adjust for the repeated measures within individuals, including right and left eye measures. Robust SEs calculated through classic sandwich adjustment were used to address the different measurement variance across time points. When significant effects were found via the F test for time, Bonferroni adjustments were made to adjust P values for the multiple testing time points during and after BR. P < .05 was considered significant. All analyses were conducted in SAS, version 9.4 (SAS Institute Inc) using the GLIMMIX procedure, including an LSMEANS statement for the pairwise comparisons across time within BR and between groups for the comparison between spaceflight and BR.
Results
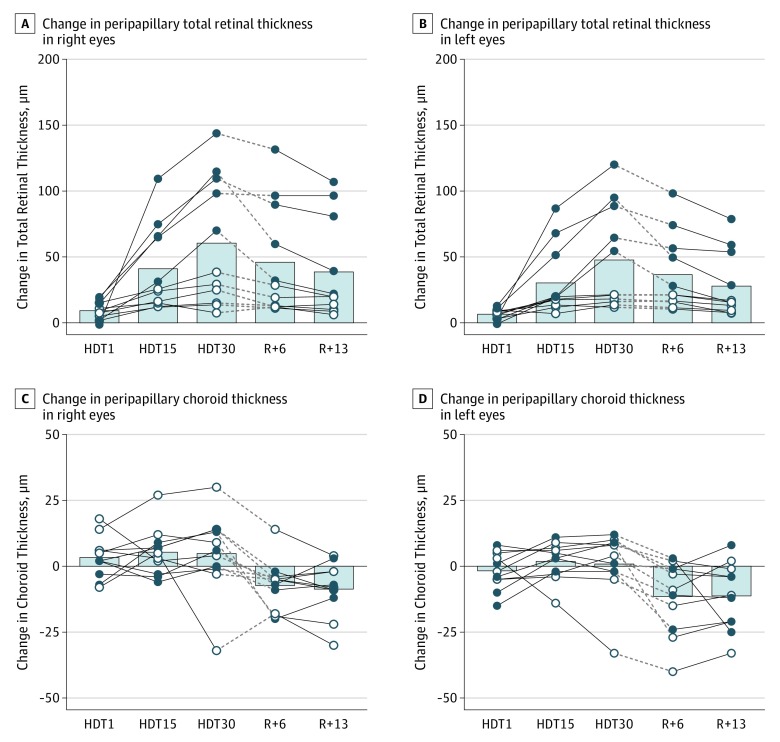
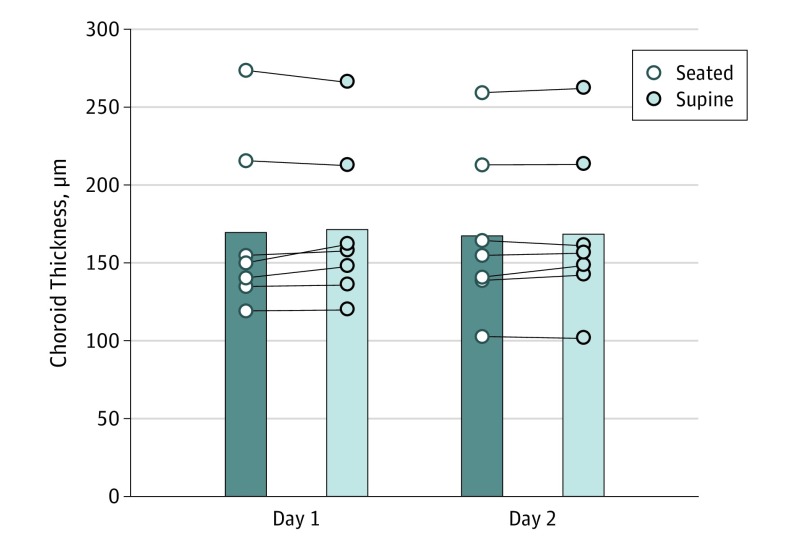
Anthropometric characteristics of the individuals participating in BR and the astronauts are presented in the Table. There was a greater proportion of women in the BR group than in the astronaut group (5 of 11 [45%] vs 3 of 20 [15%]), and those in the BR group were younger (mean [SD] age, 33.4 [8.0] vs 46.0 [6.0] years) and weighed less (mean [SD], 70.8 [8.6] vs 79.9 [8.9] kg) than those in the astronaut group. During BR, the change in peripapillary TRT increased significantly at all time points (head-down tilt day 1, 8.1 μm [95% CI, 4.6-11.6 μm]; P < .001; head-down tilt day 15, 36.1 μm [95% CI, 16.0-56.2 μm]; P < . 001; head-down tilt day 30, 53.9 μm [95% CI, 24.1-83.7 μm]; P < .001; day 6 after BR, 41.2 μm [95% CI, 16.5-65.9 μm]; P = .001; day 13 after BR, 33.4 μm [95% CI, 11.7-55.0 μm]; P = .003), although the mean for the group did not exceed our measurement precision until 15 days of head-down tilt BR, and it remained elevated through recovery on day 13 after BR (Figure 1). Compared with the pre-BR period, the mean change in choroid thickness was not significantly different during BR, yet the choroid was significantly thinner than baseline during post-BR testing (day 6 after BR, −9.5 μm [95% CI, −17.8 to −1.2 μm]; P = .02; day 13 after BR, −9.9 μm [95% CI, −18.2 to −1.6 μm]; P = .01) (Figure 1). These statistically significant changes were not greater than our day-to-day measurement precision. Furthermore, choroid thickness data acquired during the precision study did not reveal differences in thickness between seated and supine postures at either of the 2 visits (Figure 2).12 In the 5 individuals with a diagnosis of Frisén grade optic disc edema, the increase in peripapillary TRT was also observed in the set of seated OCT images collected on the first day after BR and returned to values within our measurement precision in all but a single eye at 6 months after BR despite no medical intervention (Figure 3). There was no evidence of choroidal or retinal folds by OCT.
Table. Characteristics of Study Participants.
| Characteristic | Bed Rest Cohort | Spaceflight Cohort |
|---|---|---|
| Sex, No. | ||
| Male | 6 | 17 |
| Female | 5 | 3 |
| Age, mean (SD), y | 33.4 (8.0) | 46.0 (6.0) |
| Height, mean (SD), cm | 173.5 (9.8) | 176.7 (5.8) |
| Weight, mean (SD), kg | 70.8 (8.6) | 79.9 (8.9) |
| BMI, mean (SD) | 23.4 (2.2) | 25.6 (2.7) |
Abbreviation: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared).
Figure 1. Change in Peripapillary Total Retinal Thickness and Peripapillary Choroid Thickness During and After 30 Days of Bed Rest in a Mildly Hypercapnic Environment.
A, Change in peripapillary total retinal thickness in the right eyes. B, Change in peripapillary total retinal thickness in the left eyes. C, Change in peripapillary choroid thickness in the right eyes. D, Change in peripapillary choroid thickness in the left eyes. All data from images collected in participants in the head-down tilt (HDT) (HDT day 1 [HDT1], HDT day 15 [HDT15], and HDT day 30 [HDT 30]) or horizontal (baseline, day 6 after bed rest [R+6], and day 13 after bed rest [R+13]) positions. The change in total retinal thickness associated with bed rest was significant at all days (marginal means: HDT1, 8.1 μm [95% CI, 4.4-11.8 μm]; P < .001; HDT15, 36.1 μm [95% CI, 14.2-58.0 μm], P < .001; HDT30, 53.9 μm [95% CI, 21.4-86.4 μm], P < .001; R+6, 41.2 μm [95% CI, 14.2-68.1 μm]; P < .001; R+13, 33.4 μm [95% CI, 9.8-56.9 μm]; P = .002). The association of bed rest with change in choroid thickness was not significant at any bed rest day (marginal means: HDT1, 0.7 μm [95% CI, −4.1 to 5.5 μm]; P > .99; HDT15, 3.6 μm [95% CI, −1.1 to 8.2 μm]; P = .22; HDT30, 2.7 μm [95% CI, −7.3 to 12.8 μm]; P > .99), but was significant during recovery after bed rest (marginal means: R+6, −9.5 μm [95% CI, −17.8 to −1.2 μm]; P = .02; R+13, −9.9 μm [95% CI, −18.2 to −1.6 μm]; P = .01). Columns represent the mean of all participants. Filled symbols represent individuals with diagnosis of optic disc edema from ophthalmoscopy images collected on HDT30. The dashed line indicates the break between bed rest when individuals were exposed to carbon dioxide, and post–bed rest recovery when they were not.
Figure 2. Choroid Thickness in Seated and Supine Posture in 7 Novice Astronauts Assessed on 2 Days Separated by Approximately 4 Months (Range, 112-147 Days).
The mean (SD) change on day 1 (1.9 [8.5] μm) was not statistically different from day 2 (3.0 [11.4] μm). The mean (SD) thickness measured in the seated posture from both days (169.2 [51.6] μm; n = 7) was similar to that in a previous report in healthy individuals using the same analysis method (169.3 [43.0] μm; n = 40).12 The columns indicate the mean.
Figure 3. Change in Peripapillary Total Retinal Thickness Immediately After and 6 Months After 30 Days of Bed Rest in a Mildly Hypercapnic Environment in Individuals With a Diagnosis of Optic Disc Edema.
A, Change in peripapillary total retinal thickness in the right eyes immediately after (R+0) and 6 months after (R+6 month) 30 days of bed rest. B, Change in peripapillary total retinal thickness in the left eyes at R+0 and R+6 month. All data from images collected in individuals in the seated position. Columns represent the mean of all 5 individuals.
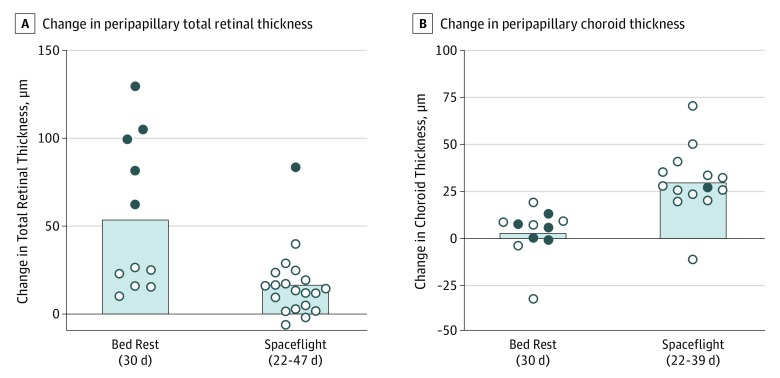
After similar durations of exposure to either BR or spaceflight, peripapillary TRT increased to a greater degree in individuals participating in BR than in astronauts, with a mean difference between groups of 37 μm (95% CI, 13-61 μm; P = .005), while choroid thickness did not increase in individuals participating in BR but increased in astronauts, resulting in a mean difference between groups of 27 μm (95% CI, 14-41 μm; P < .001) (Figure 4). After BR, 5 of 11 individuals (45%) developed Frisén grade edema (grade 1 or 2), while only 1 of 20 astronauts (5%) developed Frisén grade edema (grade 1) after a similar duration of actual spaceflight. Linear regression analysis between the change in choroid thickness and the change in peripapillary TRT did not reveal a significant association for either individuals participating in BR (r2 = 0.015; P = .68) or astronauts (r2 = 0.002; P = .91).
Figure 4. Change in Peripapillary Total Retinal Thickness and Peripapillary Choroid Thickness After 30 Days of Bed Rest or 22 to 47 Days of Weightlessness on the International Space Station.
A, Change in peripapillary total retinal thickness. B, Change in peripapillary choroid thickness. Symbols represent the mean from both eyes for each individual or astronaut, when available. Columns represent mean of all individuals. Filled symbols are individuals with diagnosis of optic disc edema from ophthalmoscopy images.
Discussion
We report that the development of optic disc edema is greater in individuals participating in the spaceflight analog strict 6° head-down tilt BR than in astronauts experiencing a similar duration of actual spaceflight. Conversely, peripapillary choroid thickness increased during spaceflight, but not in individuals participating in BR. Together, these data indicate that mechanistic causes or modifying factors associated with ocular changes in BR may differ from spaceflight. Identifying factors associated with this variability will provide new insight into the mechanisms of optic disc edema in astronauts and help focus efforts on developing countermeasures to prevent it or treatments to reverse it.
Elevated ICP was originally hypothesized to be a major factor associated with the development of optic disc edema during spaceflight; however, SANS does not appear to mimic terrestrial idiopathic intracranial hypertension because data collected during parabolic flight,6 mathematical modeling experiments,13 and empirical observations of the lack of observed idiopathic intracranial hypertension symptoms in SANS indicate distinct disease mechanisms.3,14,15 We hypothesize that the strict head-down tilt during BR and the long-term headward fluid shift during spaceflight both result in a long-term, mild elevation in ICP rather than a pathologically elevated ICP, as previously suggested.6 During the BR period, none of the 5 individuals who developed peripapillary edema reported symptoms associated with idiopathic intracranial hypertension such as severe headache, pulsatile tinnitus, or blurred vision. Similarly, astronauts during spaceflight do not report these symptoms.
During acute periods of weightlessness, ICP measured in the supine posture decreases despite an increase in jugular venous area, which should theoretically increase ICP.6 This finding suggests that a nonvascular factor may be responsible for lowering ICP during weightlessness. The spinal dural sac acts as a reservoir to accommodate shifting cerebrospinal fluid volume during posture changes,16 and cerebrospinal fluid volume shifting into and out of the dural sac blunts ICP changes in response to various ICP provocations.17 We hypothesize that the weightlessness-induced decrease in intrathoracic pressure18 and/or unloading of abdominal tissue weight reduces pressure surrounding the spinal dural sac, thereby drawing cerebrospinal fluid out of the cranium, and reduces ICP. This hypothesis could explain the paradoxical decrease in ICP measured during weightlessness in parabolic flight.6 Because this decrease would not occur during BR, and thereby result in a higher ICP, it may partially explain the difference in time course for the development of optic disc edema. Although no model perfectly replicates a given pathologic mechanism, more work is needed to better understand the mechanisms underpinning the similarities and differences between optic disc edema induced by spaceflight or optic disc edema induced by BR.
Previous speculation implicated choroidal engorgement as an additional factor that may be associated with the development of optic disc edema,19 yet our data do not support this association. Mathematical modeling suggests that even small changes in choroidal volume will produce significant tissue strain at the optic nerve head,20 which would imply that greater strains developed at the optic nerve head in astronauts than in individuals participating in BR. Given the fact that there was a greater incidence of optic disc edema in those participating in BR than in astronauts, yet individuals in the BR group did not experience a change in choroid thickness, suggests that choroidal engorgement was not associated with the development of optic disc edema. However, choroidal thickening during spaceflight likely results from the weightlessness-induced headward fluid shift, and understanding why choroidal thickening does not develop in individuals participating in BR despite greater optic disc edema formation will provide insight into the underlying mechanisms. We do not believe that differences in the posture of individuals participating in BR (supine) and astronauts (seated) during baseline choroid thickness measurements were associated with the different choroid thickness responses in each group because choroid thickness does not change owing to an acute posture change (Figure 2).12 Varying reports of the association of posture with choroid thickness support21 and refute19,22 our observations, perhaps because of the different analysis approaches or retinal regions being evaluated.
Increased choroid thickness in astronauts may have been associated with the lack of gravitational gradient experienced during weightlessness, which differed from participants’ experience during BR. During weightlessness, the unloading of tissue may allow the choroid to expand to a greater degree for a given headward fluid shift–mediated increase in venous pressure.23 While lying on their backs, individuals participating in BR were positioned in a strict head-down tilt and therefore were continuously exposed to a posterior gravitational vector. That vector may have supported drainage through the vortex veins to potentially minimize changes in choroid thickness. However, our thickness measures do not differentiate between intravascular vs extravascular fluid within the total thickness of the choroid. Use of OCT angiography may be a useful technique to better characterize the choroidal vasculature response to both BR and weightlessness during prolonged spaceflight.
Mildly elevated ambient CO2 on the ISS has been hypothesized to be associated with the development of optic disc edema, so for this reason, elevated ambient CO2 (0.5%; approximately 4 mm Hg Pco2) was incorporated into the current BR study design. Because the individuals participating in BR and the astronauts were exposed to similar mild elevations in ambient Pco2, it is unlikely that this factor was associated with the differences in retinal thickness or choroid thickness changes between and within these groups. This conclusion is supported by evidence that exposure to a mildly hypercapnic environment does not induce physiologically significant changes in end-tidal Pco2, a surrogate for arterial Pco2, during acute head-down tilt,24 BR,8 or in astronauts during spaceflight,25 which would be necessary for a physiological response.
At the molecular level, SANS has been associated with variability in the status of B vitamins resulting from genetic differences in single-nucleotide polymorphisms within the 1-carbon metabolism pathway26,27 and more recently during BR.28 Differences in folic acid fortification between the European diet provided to individuals participating in BR and the food consumed by astronauts on the ISS, as well as variability in the distribution of single-nucleotide polymorphisms between the European and Western populations, may be associated with alterations in the 1-carbon metabolic pathway of the 2 groups presented here. Additional work is warranted to test this hypothesis and determine whether a precision medicine approach would help attenuate the development of optic disc edema.
An additional factor implicated in the development of optic disc edema during spaceflight is the use of the Advanced Resistive Exercise Device, which was speculated to generate spikes in ICP during resistive exercise by astronauts on the ISS.29 However, the limited evidence outlined here does not support this hypothesis. First, the individuals participating in BR were completely sedentary for the 30 days of strict head-down tilt BR, and 45% developed Frisén grade edema. Conversely, individuals who participated in a previous 70-day head-down tilt study (but without strict head-down tilt) did not show differences in ocular outcomes between the control or exercising groups.5 Second, after obtaining consent, we reviewed exercise logs and results from ocular tests from 34 astronauts who flew to the ISS between 2002 and 2014. Eight of the 34 astronauts received a diagnosis of optic disc edema, and there was no difference in the mean time per day spent performing aerobic exercise or in the mean volume of resistance exercise completed between astronauts who did and astronauts who did not receive a diagnosis of optic disc edema. Prospective investigations should be conducted to verify these retrospective analyses and determine whether exercise may provide a protective effect to minimize the development of optic disc edema, given that individuals participating in BR who did not exercise demonstrated larger changes in peripapillary TRT than did astronauts who did exercise.
Although no female astronauts have received a diagnosis of Frisén grade edema, the women in our BR and astronaut cohorts demonstrated increased retinal thickness, suggesting that sex may not be a factor associated with variability in SANS. In addition, while individuals participating in BR showed slightly greater retinal thickening in their right vs left eyes, similar to asymmetric findings reported in an astronaut case report,3 additional studies are needed to clarify whether this represents asymmetric pathologic characteristics or physiological variability within the mild manifestation of edema in SANS.
Limitations
This study has some limitations. Both cohorts were small and demonstrated large variability in change in TRT and choroid thickness. This study did not control for all possible differences between these cohorts, such as diet, exercise, sleep duration and quality, sex, B vitamin status, or genetic single-nucleotide polymorphism prevalence. The determining factors associated with the differences between these cohorts provide us with opportunities to better understand mechanisms leading to optic disc edema, and thus improve our ability to treat it. Lumbar puncture opening pressure was not obtained, preventing us from commenting directly on the role ICP played in the development of optic disc edema.
Conclusions
These findings suggest that the spaceflight analogue of strict head-down tilt BR induced optic disc edema to a greater degree, and choroidal thickening to a lesser degree, than actual spaceflight of similar duration. Replication of these findings is needed, but identifying the factors underlying these differences will provide new insight into mechanisms that underlie optic disc edema in astronauts. We speculate that both groups experience a long-term mild elevation in ICP, yet small differences in the magnitude of ICP experienced in BR vs weightlessness in spaceflight may dictate the severity of optic disc edema. Direct measures of ICP should be performed in both environments to confirm this hypothesis. Use of this terrestrial model of optic disc edema will be valuable for investigating countermeasures to protect astronauts and for studying the early onset of this pathologic condition, which is limited in symptomatic patients presenting with more advanced disease.
References
- 1.Stenger MB, Tarver WJ, Brunstetter T, et al. Risk of spaceflight associated neuro-ocular syndrome (SANS). https://humanresearchroadmap.nasa.gov/evidence/reports/SANS.pdf?rnd=0.434276635495143. Published November 30, 2017. Accessed February 15, 2018.
- 2.Lee AG, Mader TH, Gibson CR, Tarver W. Space flight–associated neuro-ocular syndrome. JAMA Ophthalmol. 2017;135(9):992-994. doi: 10.1001/jamaophthalmol.2017.2396 [DOI] [PubMed] [Google Scholar]
- 3.Mader TH, Gibson CR, Otto CA, et al. Persistent asymmetric optic disc swelling after long-duration space flight: implications for pathogenesis. J Neuroophthalmol. 2017;37(2):133-139. doi: 10.1097/WNO.0000000000000467 [DOI] [PubMed] [Google Scholar]
- 4.Taibbi G, Cromwell RL, Zanello SB, et al. Ocular outcomes comparison between 14- and 70-day head-down–tilt bed rest. Invest Ophthalmol Vis Sci. 2016;57(2):495-501. doi: 10.1167/iovs.15-18530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Taibbi G, Cromwell RL, Zanello SB, et al. Ophthalmological evaluation of integrated resistance and aerobic training during 70-day bed rest. Aerosp Med Hum Perform. 2017;88(7):633-640. doi: 10.3357/AMHP.4768.2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lawley JS, Petersen LG, Howden EJ, et al. Effect of gravity and microgravity on intracranial pressure. J Physiol. 2017;595(6):2115-2127. doi: 10.1113/JP273557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Law J, Van Baalen M, Foy M, et al. Relationship between carbon dioxide levels and reported headaches on the International Space Station. J Occup Environ Med. 2014;56(5):477-483. doi: 10.1097/JOM.0000000000000158 [DOI] [PubMed] [Google Scholar]
- 8.Laurie SS, Macias BR, Dunn JT, et al. Optic disc edema after 30 days of strict head-down tilt bed rest. Ophthalmology. 2019;126(3):467-468. doi: 10.1016/j.ophtha.2018.09.042 [DOI] [PubMed] [Google Scholar]
- 9.Petersen LG, Petersen JCG, Andresen M, Secher NH, Juhler M. Postural influence on intracranial and cerebral perfusion pressure in ambulatory neurosurgical patients. Am J Physiol Regul Integr Comp Physiol. 2016;310(1):R100-R104. doi: 10.1152/ajpregu.00302.2015 [DOI] [PubMed] [Google Scholar]
- 10.Petersen LG, Lawley JS, Lilja-Cyron A, et al. Lower body negative pressure to safely reduce intracranial pressure. J Physiol. 2019;597(1):237-248. doi: 10.1113/JP276557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Patel N, Pass A, Mason S, Gibson CR, Otto C. Optical coherence tomography analysis of the optic nerve head and surrounding structures in long-duration International Space Station astronauts. JAMA Ophthalmol. 2018;136(2):193-200. doi: 10.1001/jamaophthalmol.2017.6226 [DOI] [PubMed] [Google Scholar]
- 12.Jiang L, Chen L, Qiu X, et al. Choroidal thickness in Chinese patients with non-arteritic anterior ischemic optic neuropathy. BMC Ophthalmol. 2016;16(1):153. doi: 10.1186/s12886-016-0313-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lakin WD, Stevens SA. Modelling the response of intracranial pressure to microgravity environments In: Hosking RJ, Venturino E, eds. Aspects of Mathematical Modelling: Applications in Science, Medicine, Economics and Management: Mathematics and Biosciences in Interaction. Basel, Switzerland: Birkhäuser; 2008:211-227. doi: 10.1007/978-3-7643-8591-0_11 [DOI] [Google Scholar]
- 14.Mader TH, Gibson CR, Pass AF, et al. Optic disc edema, globe flattening, choroidal folds, and hyperopic shifts observed in astronauts after long-duration space flight. Ophthalmology. 2011;118(10):2058-2069. doi: 10.1016/j.ophtha.2011.06.021 [DOI] [PubMed] [Google Scholar]
- 15.Lee AG, Mader TH, Gibson CR, Brunstetter TJ, Tarver WJ. Space flight-associated neuro-ocular syndrome (SANS). Eye (Lond). 2018;32(7):1164-1167. doi: 10.1038/s41433-018-0070-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hirasawa Y, Bashir WA, Smith FW, Magnusson ML, Pope MH, Takahashi K. Postural changes of the dural sac in the lumbar spines of asymptomatic individuals using positional stand-up magnetic resonance imaging. Spine (Phila Pa 1976). 2007;32(4):E136-E140. doi: 10.1097/01.brs.0000255202.94153.ca [DOI] [PubMed] [Google Scholar]
- 17.Martins AN, Wiley JK, Myers PW. Dynamics of the cerebrospinal fluid and the spinal dura mater. J Neurol Neurosurg Psychiatry. 1972;35(4):468-473. doi: 10.1136/jnnp.35.4.468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Videbaek R, Norsk P. Atrial distension in humans during microgravity induced by parabolic flights. J Appl Physiol (1985). 1997;83(6):1862-1866. doi: 10.1152/jappl.1997.83.6.1862 [DOI] [PubMed] [Google Scholar]
- 19.Shinojima A, Iwasaki K, Aoki K, Ogawa Y, Yanagida R, Yuzawa M. Subfoveal choroidal thickness and foveal retinal thickness during head-down tilt. Aviat Space Environ Med. 2012;83(4):388-393. doi: 10.3357/ASEM.3191.2012 [DOI] [PubMed] [Google Scholar]
- 20.Feola AJ, Nelson ES, Myers J, Ethier CR, Samuels BC. The impact of choroidal swelling on optic nerve head deformation. Invest Ophthalmol Vis Sci. 2018;59(10):4172-4181. doi: 10.1167/iovs.18-24463 [DOI] [PubMed] [Google Scholar]
- 21.Almeida DRP, Zhang L, Chin EK, et al. Comparison of retinal and choriocapillaris thicknesses following sitting to supine transition in healthy individuals and patients with age-related macular degeneration. JAMA Ophthalmol. 2015;133(3):297-303. doi: 10.1001/jamaophthalmol.2014.5168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Balasubramanian S, Tepelus T, Stenger MB, et al. Thigh cuffs as a countermeasure for ocular changes in simulated weightlessness. Ophthalmology. 2018;125(3):459-460. doi: 10.1016/j.ophtha.2017.10.023 [DOI] [PubMed] [Google Scholar]
- 23.Anderson AP, Swan JG, Phillips SD, et al. Acute effects of changes to the gravitational vector on the eye. J Appl Physiol (1985). 2016;120(8):939-946. doi: 10.1152/japplphysiol.00730.2015 [DOI] [PubMed] [Google Scholar]
- 24.Laurie SS, Vizzeri G, Taibbi G, et al. Effects of short-term mild hypercapnia during head-down tilt on intracranial pressure and ocular structures in healthy human subjects. Physiol Rep. 2017;5(11):e13302. doi: 10.14814/phy2.13302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Prisk GK, Fine JM, Cooper TK, West JB. Vital capacity, respiratory muscle strength, and pulmonary gas exchange during long-duration exposure to microgravity. J Appl Physiol (1985). 2006;101(2):439-447. doi: 10.1152/japplphysiol.01419.2005 [DOI] [PubMed] [Google Scholar]
- 26.Zwart SR, Gregory JF, Zeisel SH, et al. Genotype, B-vitamin status, and androgens affect spaceflight-induced ophthalmic changes. FASEB J. 2016;30(1):141-148. doi: 10.1096/fj.15-278457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zwart SR, Gibson CR, Mader TH, et al. Vision changes after spaceflight are related to alterations in folate- and vitamin B-12–dependent one-carbon metabolism. J Nutr. 2012;142(3):427-431. doi: 10.3945/jn.111.154245 [DOI] [PubMed] [Google Scholar]
- 28.Zwart SR, Laurie SS, Chen JJ, et al. Association of genetics and B vitamin status with the magnitude of optic disc edema during 30-day strict head-down tilt bed rest [published online August 15, 2019]. JAMA Ophthalmol. 2019. doi: 10.1001/jamaophthalmol.2019.3124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Marshall-Bowman K, Barratt MR, Gibson CR. Ophthalmic changes and increased intracranial pressure associated with long duration spaceflight: an emerging understanding. Acta Astronaut. 2013;87:77-87. doi: 10.1016/j.actaastro.2013.01.014 [DOI] [Google Scholar]