This cohort study compares income-specific trends in the incidence rates of first psychiatric hospital admissions and evaluates whether an income gradient exists in the incidence rates at all levels of household income among adults in Finland.
Key Points
Question
Is household income associated with the incidence rates of first hospital admissions for mental disorders?
Findings
In this nationwide open cohort study of more than 6.2 million persons, a clear income gradient was observed at all levels of income among adults, with adjusted incidence rate ratios varying from 2.94 to 4.46 in the lowest compared with the highest income deciles. This association varied over time, and a continuous decrease in the annual incidence rates emerged only in the high-income groups.
Meaning
Household income appears to be an important risk factor for first hospital-treated mental disorders at all levels of income, and mechanisms linking income and mental health may be located partly within the health care system itself.
Abstract
Importance
The association between income and mental health has long been a question of interest. Nationwide register data provide means to examine trends and patterns of these associations.
Objectives
To compare income-specific trends in the incidence rates of first psychiatric hospital admissions and to evaluate whether an income gradient exists in the incidence rates at all levels of household income.
Design, Setting, and Participants
This population-based open cohort study used linked registry data from nationwide Finnish Hospital Discharge and Statistics Finland population registers to determine annual incidence rates of first psychiatric hospital admissions. All Finnish citizens (N = 6 258 033) living in the country at any time from January 1, 1996, through December 31, 2014, contributed to 96 184 614 person-years at risk of first inpatient treatment for mental disorders. The analyses were conducted from August 1, 2018, through September 30, 2019.
Exposures
Equivalized disposable income, sex, age group, reduction in income decile in the previous 3 years, urbanicity, educational level, and living alone status.
Main Outcomes and Measures
Annual percentage changes in the age-standardized incidence rates and incidence rate ratios (IRRs).
Results
Altogether, 186 082 first psychiatric inpatient treatment episodes occurred (93 431 [50.2%] men), with overall age-standardized incidence rates per 1000 person-years varying from 1.59 (95% CI, 1.56-1.63) in 2014 to 2.11 (95% CI, 2.07-2.15) in 2008. In the highest income deciles, a continuous mean decrease per year of 3.71% (95% CI, 2.82%-4.59%) in men and 0.91% (95% CI, 0.01%-1.80%) in women occurred throughout the study period, in contrast to the lowest deciles, where the trends first increased (1.31% [95% CI, 0.62%-2.01%] increase in men from 1996 to 2007 and 5.61% [95% CI, 2.36%-8.96%] increase in women from 1996 to 2001). In the adult population, an income gradient was observed at all levels of household income: the lower the income decile, the higher the adjusted IRRs compared with the highest decile. The IRRs in the lowest decile varied from 2.94 (95% CI, 2.78-3.11) to 4.46 (95% CI, 4.17-4.76). In other age groups, the gradient did not persist at the highest income deciles. Diagnosis-specific income gradient was steepest in schizophrenia and related psychotic disorders, with estimated IRRs of the lowest income decile of 5.89 (95% CI, 5.77-6.02).
Conclusions and Relevance
In this cohort study, clear negative income gradient in the incidence rates of first hospital-treated mental disorders was observed in the adult population of Finland. These findings suggest that reduction in the use of inpatient care has not taken place equally between different income groups.
Introduction
The negative association between household income and different mental health outcomes has been observed repeatedly,1,2,3,4,5,6,7,8 but not always.9,10,11,12 Significant differences in health and mortality are found between all socioeconomic levels of society, which is often referred to as the social gradient in health.13,14 This pattern has its roots in childhood15,16 and has been observed in some studies of common mental disorders.8,17 However, some studies18,19,20 argue that, after basic needs are met, additional income is not associated with increases in well-being. At present, whether there is an income gradient in the incidence rates of first hospital-treated mental disorders is unknown.
Explanations for the association between income and mental health fall into 2 categories.21,22,23,24 According to social causation, income influences mental health through psychosocial pathways. The selection hypothesis, on the other hand, posits that mental disorders may cause downward social mobility within and across generations. These mechanisms are not mutually exclusive, but they vary between disorders and contexts and during the life course.22,25,26,27 In addition to academic and ethical interest, these associations have practical implications for social policy in general and for the design of accessible health services.28,29,30
Psychiatric hospital treatment has been reduced in the era of deinstitutionalization.31,32 In Finland, the annual population rates of psychiatric hospital care have decreased from 6.2 to 4.7 per 1000 inhabitants, and mean length of stay in inpatient care has reduced from 67 to 31 days from 1996 to 2014.33 First psychiatric hospital admission rates are rarely reported34,35 but present an overall perspective on the annual emergence of severe mental health conditions and can thus facilitate comparisons between income groups. Hence, whether the incidence of first-time hospital-treated mental disorders has been reduced in the era of outpatient-centered services and, if so, whether the reduction has occurred equally within population are unknown to date.
Using national individual-level register data, we investigated the associations between household income and the incidence rates of first hospital admissions for mental disorders in Finland from January 1, 1996, through December 31, 2014. We hypothesized that an income gradient exists in the incidence rate of first inpatient treatments for mental disorders on the national level and examined (1) how equally the income-specific trends in the incidence rates of first psychiatric hospital admissions have changed during the era of decreasing inpatient care and (2) whether the possible income-specific differences persist after adjusting for potential well-known confounding factors, including urbanicity of the living municipality,36 educational attainment,10 living alone,37 and income reduction during the previous 3 years before the first admission.5,38
Methods
Data Sources and Study Population
Individual-level register data on hospital care and population registers were combined for this population-based open cohort study. We identified all first psychiatric hospital admissions and the dynamic population at risk of first admissions in Finland from 1996 through 2014. The ethical review board of the National Institute for Health and Welfare approved the study protocol. Informed consent is not required for register-based studies in Finland. We followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
The population register of Statistics Finland included data on the total population on the last day of each study year, with socioeconomic variables and time of birth and death. We collected the following individual-level data: sex (man or woman), nationality (Finnish citizen or not), urbanicity of residence municipality (urban, semiurban, or rural),39 household net income, size of the household dwelling unit, and for persons 20 years or older, the level of educational attainment (less than upper secondary, upper secondary, or tertiary, a national classification based on the United Nations Educational, Scientific and Cultural Organization’s International Standard Classification of Education 2011),40 and living alone status (living alone or not).
The Finnish Hospital Discharge register (1969-1993), followed by the Care Register for Health Care, maintained by the National Institute for Health and Welfare, covers all inpatient hospital treatments in Finland, and displays good accuracy of mental health diagnoses.41 We collected all admission and discharge dates and discharge diagnoses.
Assessment of the First Psychiatric Hospital Admissions and Diagnoses
We identified all persons with first-time psychiatric hospital inpatient admissions. Outpatient visits, day-hospital treatment in psychiatric hospitals, or treatments in other general hospital wards with psychiatric diagnoses were not included. Treatments in psychiatric facilities were reliably recognized starting from the year 1976. Hence, the shortest definitive clearance period to define a first admission (ie, the time with no previous inpatient treatments before the first admission) was 20 years (January 1, 1976, through December 31, 1995). To cover the whole study period and facilitate the evaluation of temporal trends, we used a 20-year clearance period for every study year. The International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) has been used in Finland since 1996. For details, see the eMethods in the Supplement.
Assessment of Equivalized Disposable Income Deciles
We calculated the equivalized disposable income by adjusting the net income of a household dwelling unit for the size of the unit, using the Organisation for Economic Co-operation and Development–modified equivalence scale.42 Net income is obtained after subtracting taxes from income subject to state taxation.43 We calculated 10th percentiles (deciles) of the annual Finnish income distribution to categorize the population into 10 income groups. The income deciles 1, 3, and 5 years before the first psychiatric hospital admission were also calculated, and possible decrease in income decile in the previous 3 years was recorded.
Persons who are registered as institutionalized or who are homeless, abroad, registered as unknown, or living in quarters that do not meet the definition of dwelling do not constitute household-dwelling units and are categorized as nondwelling. Therefore, no income data are available for this nondwelling population. However, instead of leaving these persons out of the analyses, we analyzed them as a separate income group.
Statistical Analysis
We computed stratum-specific incidence rates of the first psychiatric hospital admissions for every calendar year by dividing the number of first admissions by the person-years at risk in the following strata: sex, 5-year age groups, nationality, income decile, decrease in income decile, urbanicity of the residential municipality, educational level, and living alone status. Age-standardized incidence rates with 95% CIs were calculated by applying direct age standardization to the 2013 Revision of the European Standard Population.44 Analyses were conducted separately for the main ICD-10 categories of psychiatric diagnoses.
Every person in the population register with no previous hospital admissions within the clearance period of 20 years contributed to the person-time at risk. Exact dates of immigration to and from the country, moves between municipalities, or changes in household composition were not available, and therefore changes were assumed to occur on average in midyear. Non-Finnish citizens had a high rate of missing data, for example, 13.2% of the person-years at risk had missing income data compared with 0.9% in the case of Finnish citizens. Hence, all analyses included Finnish citizens only.
We used a joinpoint regression model to analyze changes in trends in age-standardized incidence rates.45 Sex-, income decile–, and diagnosis-specific trends were analyzed separately. We used a model with a maximum of 3 joinpoints requiring at least 2 observations between joinpoints, a log-linear regression model, and the bayesian information criterion method to assess significant changes in time trends. Annual percentage changes (APCs), the estimated annual changes in rates from one joinpoint to the next in percentage, and weighted means of combined APCs were calculated. The 2-sided α level was set at .05.
To account for potential confounders, we used multivariable Poisson regression models to examine income decile-specific incidence rate ratios (IRRs) and corresponding 95% CIs. We used the incidence rates in the highest income decile as a reference. Analysis was conducted separately in 5 periods (1996-1999, 2000-2003, 2004-2007, 2008-2011, and 2012-2014) and in 3 age groups (5-19, 20-64, and ≥65 years). The division into 5 periods was used to summarize data and to make it easier to compare indicators. We adjusted the models for sex, age group, urbanicity of residential municipality, decrease in income decile, and, in the groups aged 20 to 64 years and 65 years or older, educational attainment and living alone status. We conducted separate analyses for all first admissions and for the main ICD-10 categories of psychiatric diagnoses. We replicated the analysis using the income decile 1, 3, and 5 years before the first admission, instead of the current income decile. This procedure accounted more strongly for the temporal order of having a certain level of income and the first hospital admission.
For data management and analyses, we used the following: Python, version 2.7 (Python Software Foundation); R, version 3.5.1 (R Project for Statistical Computing); Stata, version 15.1 (StataCorp LLC); and Joinpoint Regression Program, version 4.6.0.0 (Statistical Methodology and Applications Branch, Surveillance Research Program, National Cancer Institute). The analyses were conducted from August 1, 2018, through September 30, 2019.
Results
First Admissions and the First Admission Rates
A total of 6 258 033 Finnish citizens contributed 96 184 614 person-years at risk of first inpatient treatment for mental disorders during the study period. Of those at risk, 186 082 persons (93 431 men [50.2%] and 92 651 women [49.8%]) had their first admission to psychiatric inpatient care. The most commonly presented diagnostic main group consisted of mood disorders (ICD-10 codes F30-F39) in 80 548 cases (43.3%) (eTable 1 in the Supplement).
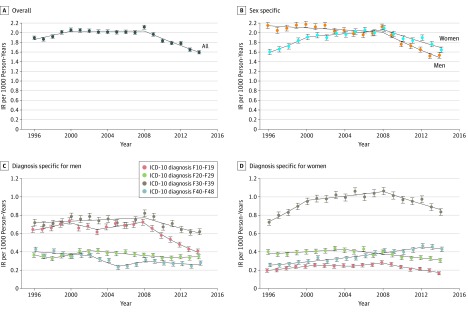
Table 1 contains annual incidence rates of first psychiatric hospital admissions in the first and last year of the study period. All years are presented in eTable 2 in the Supplement. The incidence rate per 1000 person-years varied from 1.59 (95% CI, 1.56-1.63) in 2014 to 2.11 (95% CI, 2.07-2.15) in 2008 (Figure 1A). Men had higher incidence rates in the beginning of the study period (2.15 [95% CI, 2.09-2.22]) compared with women (1.61 [95% CI, 1.56-1.66]), whereas women had higher rates in at the end (1.65 [95% CI, 1.60-1.70] vs 1.54 [95% CI, 1.49-1.59]) (Figure 1B and Table 1). Much of the variation in the overall trends occurred in the incidence rates of substance use and mood disorders, with largest percentage increase of 4.53% (95% CI, 2.27%-6.84%) in mood disorders from 1996 through 1999 and largest percentage decrease of 8.8% (95% CI, 9.69%-7.91%) in substance use disorders from 2008 through 2014 (Figure 1C and D and eFigures 1-3 and eTables 3-6 in the Supplement).
Table 1. Age-Standardized Incidence Rates of First Psychiatric Hospital Admissions in the First and Last Year of the Study Perioda.
| Variable | 1996 | 2014 | ||||
|---|---|---|---|---|---|---|
| Admissions, No. (%) | Person-Years at Risk, Millions (%) | Incidence Rate (95% CI) per 1000 Person-Years | Admissions, No. (%) | Person-Years at Risk, Millions (%) | Incidence Rate (95% CI) per 1000 Person-Years | |
| All populationb | 9713 | 5.12 | 1.9 (1.86-1.94) | 8387 | 5.31 | 1.59 (1.56-1.62) |
| Finnish citizens | 9547 (100) | 5.05 | 1.89 (1.85-1.93) | 8056 (100) | 5.10 | 1.59 (1.56-1.63) |
| Sex | ||||||
| Men | 5423 (56.8) | 2.46 (48.7) | 2.15 (2.09-2.22) | 3832 (47.6) | 2.50 (49.0) | 1.54 (1.49-1.59) |
| Women | 4124 (43.2) | 2.59 (51.3) | 1.61 (1.56-1.66) | 4224 (52.4) | 2.60 (51.0) | 1.65 (1.60-1.70) |
| Income decile and nondwelling population | ||||||
| 1 (lowest) | 1870 (19.6) | 0.47 (9.3) | 3.92 (3.72-4.14) | 1804 (22.4) | 0.43 (8.5) | 4.02 (3.79-4.26) |
| 2 | 1206 (12.6) | 0.49 (9.7) | 2.71 (2.55-2.89) | 1116 (13.9) | 0.48 (9.4) | 2.62 (2.45-2.79) |
| 3 | 1047 (11.0) | 0.49 (9.8) | 2.31 (2.16-2.47) | 909 (11.3) | 0.49 (9.7) | 1.95 (1.82-2.10) |
| 4 | 933 (9.8) | 0.49 (9.8) | 2.06 (1.92-2.21) | 776 (9.6) | 0.50 (9.8) | 1.63 (1.51-1.75) |
| 5 | 816 (8.5) | 0.50 (9.8) | 1.75 (1.62-1.90) | 662 (8.2) | 0.50 (9.9) | 1.32 (1.22-1.43) |
| 6 | 747 (7.8) | 0.50 (9.8) | 1.63 (1.49-1.81) | 579 (7.2) | 0.51 (9.9) | 1.15 (1.05-1.25) |
| 7 | 674 (7.1) | 0.50 (9.9) | 1.38 (1.25-1.57) | 564 (7.0) | 0.51 (10.0) | 1.11 (1.02-1.22) |
| 8 | 668 (7.0) | 0.50 (9.9) | 1.36 (1.21-1.58) | 482 (6.0) | 0.51 (10.0) | 0.97 (0.88-1.09) |
| 9 | 639 (6.7) | 0.50 (9.9) | 1.32 (1.18-1.53) | 382 (4.7) | 0.52 (10.1) | 0.79 (0.70-0.91) |
| 10 (highest) | 597 (6.3) | 0.50 (9.9) | 1.22 (1.09-1.41) | 338 (4.2) | 0.52 (10.1) | 0.73 (0.64-0.84) |
| Nondwelling | 256 (2.7) | 0.07 (1.3) | 4.37 (3.81-5.03) | 323 (4.0) | 0.09 (1.7) | 4.59 (4.08-5.17) |
| Data missing | 94 (1.0) | 0.05 (1.0) | 5.26 (4.05-7.36) | 121 (1.5) | 0.04 (0.8) | 6.22 (4.96-9.58) |
| Income decreased in previous 3 y | ||||||
| No | 6034 (63.2) | 3.26 (64.5) | 1.78 (1.74-1.83) | 5313 (66.0) | 3.46 (67.7) | 1.51 (1.47-1.56) |
| Yes | 3309 (34.7) | 1.54 (30.4) | 2.07 (1.99-2.16) | 2534 (31.5) | 1.41 (27.7) | 1.72 (1.65-1.79) |
| Data missing | 204 (2.1) | 0.26 (5.1) | 5.21 (4.36-6.65) | 209 (2.6) | 0.24 (4.6) | 4.93 (4.20-5.95) |
| Urbanicity of residence municipality | ||||||
| Urban | 6687 (70.0) | 3.26 (64.6) | 2.05 (1.99-2.10) | 5727 (71.1) | 3.48 (68.3) | 1.63 (1.59-1.67) |
| Semiurban | 1460 (15.3) | 0.87 (17.3) | 1.70 (1.61-1.79) | 1249 (15.5) | 0.85 (16.6) | 1.55 (1.46-1.64) |
| Rural | 1400 (14.7) | 0.91 (18.1) | 1.56 (1.48-1.64) | 1080 (13.4) | 0.77 (15.1) | 1.49 (1.40-1.59) |
| Educational levelc | ||||||
| Lower | 3795 (46.5) | 1.54 (40.8) | 3.06 (2.95-3.17) | 1974 (32.1) | 0.95 (24.1) | 3.10 (2.94-3.27) |
| Secondary | 3048 (37.4) | 1.35 (35.8) | 2.10 (2.00-2.21) | 2913 (47.4) | 1.70 (43.0) | 1.62 (1.56-1.69) |
| Tertiary | 1316 (16.1) | 0.88 (23.4) | 1.53 (1.42-1.65) | 1259 (20.5) | 1.30 (32.9) | 0.98 (0.92-1.05) |
| Living alonec | ||||||
| No | 5105 (62.6) | 2.88 (76.2) | 1.73 (1.68-1.78) | 3424 (55.7) | 2.86 (72.2) | 1.22 (1.18-1.26) |
| Yes | 3054 (37.4) | 0.90 (23.8) | 3.59 (3.46-3.73) | 2722 (44.3) | 1.10 (27.8) | 2.62 (2.51-2.73) |
Standardized to the 2013 European Standard Population by 5-year age groups.
Contains data for all Finland; all other rows contain Finnish citizens only.
Includes those 20 years or older.
Figure 1. Trends in Age-Standardized Incidence Rates of First Psychiatric Hospital Admissions.
Data markers denote the annual age-standardized incidence rates per 1000 person-years; error bars, 95% CIs. Lines represent results of the joinpoint regression model. Rates have been age standardized to the 2013 European Standard Population by 5-year age groups. ICD-10 indicates International Statistical Classification of Diseases and Related Health Problems, Tenth Revision; IR, incident rate. Codes F10 to F19 indicate mental and behavioral disorders due to psychoactive substance use; F20 to F29, schizophrenia, schizotypal, and delusional disorders; F30 to F39, mood disorders; and F40 to F48, neurotic, stress-related, and somatoform disorders.
Income-Specific Temporal Trends
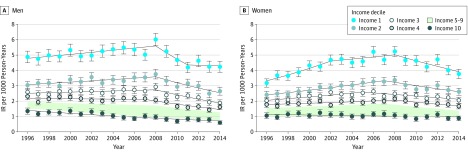
In the income-specific joinpoint regression analysis, opposite trends in the age-standardized rates between different income deciles were observed in the beginning of the study period (Figure 2, Table 2, and eFigure 4 in the Supplement for the nondwelling population). Increasing trends (ie, positive APC with 95% CIs not including 0) occurred in the 7 lowest income deciles in women and in the 3 lowest deciles in men. In the highest income deciles, a continuous mean decrease of 3.71% (95% CI, 2.82%-4.59%) per year in men and 0.91% (95% CI, 0.01%-1.80%) per year in women occurred throughout the study period (Table 2). Statistically significant increasing trends did not occur in any of the 4 most common main ICD-10 categories of psychiatric diagnoses in the highest income decile in men or women, but occurred in all diagnostic categories in the lowest income decile, except in men with neurotic, stress-related and somatoform disorders (eFigures 5-8 in the Supplement). Age-specific annual incidence rates per 1000 person-years changed during the study period in girls and women aged 15 to 19 from 3.32 (95% CI, 2.62-4.15) to 7.83 (95% CI, 6.67-9.14) in the lowest income decile and 1.98 (95% CI, 1.22-3.02) to 2.74 (95% CI, 1.80-3.98) in the highest income deciles, whereas in in boys and men aged 15 to 19 years, they changed from 6.48 (95% CI, 5.39-7.71) to 5.81 (95% CI, 4.74-7.04) in the lowest income decile and 3.04 (95% CI, 2.13-4.21) to 1.42 (95% CI, 0.80-2.35) in the highest income decile (eFigures 9 and 10 in the Supplement).
Figure 2. Trends in Income Decile and Sex-Specific Age-Standardized Incidence Rates of First Psychiatric Hospital Admissions.
Data markers denote the annual age-standardized incidence rates per 1000 person-years; error bars, 95% CIs. Lines represent the results of the joinpoint regression model. Rates have been age standardized to the 2013 European Standard Population by 5-year age groups. Income is equivalized disposable income deciles, with 1 indicating the lowest income decile and 10, the highest.
Table 2. Joinpoint Analysis of Sex- and Income-Specific Age-Standardized Incidence Rates of First Psychiatric Hospital Admissionsa.
| Variable | Segment 1 | Segment 2 | Segment 3 | Segment 4 | Total Follow-up, MAAPC (95% CI) | ||||
|---|---|---|---|---|---|---|---|---|---|
| Segment Start | AAPC (95% CI) | Segment Start | AAPC (95% CI) | Segment Start | AAPC (95% CI) | Segment Start | AAPC (95% CI) | ||
| Overall Trends | |||||||||
| Total | 1996 | 2.26 (0.71 to 3.83) | 2000 | 0.01 (−0.61 to 0.64) | 2008 | −3.96 (−4.78 to −3.15) | NA | NA | −0.84 (−1.03 to −0.38) |
| Men | 1996 | −0.52 (−1.00 to −0.04) | 2008 | −4.93 (−6.33 to −3.52) | NA | NA | NA | NA | −2.01 (−2.54 to −1.49) |
| Women | 1996 | 4.69 (2.18 to 7.25) | 2000 | 0.95 (−0.00 to 1.91) | 2008 | −3.25 (−4.46 to −2.02) | NA | NA | 0.34 (−0.38 to 1.06) |
| Income-Specific Trends | |||||||||
| Men | |||||||||
| Nondwelling population | 1996 | 1.12 (−0.25 to 2.50) | 2005 | 7.20 (−6.17 to 22.48) | 2008 | −7.41 (−9.58 to −5.19) | NA | NA | −0.85 (−2.99 to 1.34) |
| 1 (lowest decile) | 1996 | 1.31 (0.62 to 2.01) | 2008 | −7.98 (−18.03 to 3.29) | 2011 | −0.47 (−6.61 to 6.08) | NA | NA | −0.60 (−2.57 to 1.41) |
| 2 | 1996 | 1.29 (0.43 to 2.16) | 2008 | −5.54 (−8.12 to −2.89) | NA | NA | NA | NA | −1.04 (−2.02 to −0.05) |
| 3 | 1996 | 0.72 (0.05 to 1.39) | 2008 | −6.09 (−8.12 to −4.01) | NA | NA | NA | NA | −1.60 (−2.37 to −0.83) |
| 4 | 1996 | −0.23 (−1.50 to 1.05) | 2007 | −5.18 (−7.79 to −2.49) | NA | NA | NA | NA | −2.19 (−3.38 to −0.98) |
| 5 | 1996 | −1.02 (−2.05 to 0.01) | 2008 | −4.82 (−7.82 to −1.72) | NA | NA | NA | NA | −2.30 (−3.43 to −1.16) |
| 6 | 1996 | −2.13 (−2.88 to −1.37) | 2011 | −8.40 (−16.94 to 1.02) | NA | NA | NA | NA | −3.20 (−4.74 to −1.64) |
| 7 | 1996 | −2.26 (−2.93 to −1.60) | NA | NA | NA | NA | NA | NA | −2.26 (−2.93 to −1.60) |
| 8 | 1996 | −1.06 (−2.71 to 0.61) | 2002 | −7.16 (−15.66 to 2.20) | 2005 | 2.26 (−8.68 to 14.50) | 2008 | −5.26 (−6.93 to −3.55) | −2.98 (−5.10 to −0.81) |
| 9 | 1996 | −3.91 (−4.44 to −3.38) | NA | NA | NA | NA | NA | NA | −3.91 (−4.44 to −3.38) |
| 10 (highest decile) | 1996 | −3.71 (−4.59 to −2.82) | NA | NA | NA | NA | NA | NA | −3.71 (−4.59 to −2.82) |
| Women | |||||||||
| Nondwelling population | 1996 | 13.39 (0.89 to 27.44) | 1999 | −7.94 (−24.85 to 12.76) | 2002 | 8.66 (2.07 to 15.68) | 2007 | −2.73 (−5.08 to −0.33) | 1.97 (−1.76 to 5.83) |
| 1 (lowest decile) | 1996 | 5.61 (2.36 to 8.96) | 2002 | 1.44 (−2.27 to 5.30) | 2008 | −4.04 (−6.88 to −1.12) | NA | NA | 0.93 (−0.77 to 2.65) |
| 2 | 1996 | 3.02 (2.18 to 3.87) | 2007 | −3.43 (−4.97 to −1.88) | NA | NA | NA | NA | 0.46 (−0.27 to 1.20) |
| 3 | 1996 | 2.68 (1.43 to 3.96) | 2005 | −2.19 (−3.36 to −1.02) | NA | NA | NA | NA | 0.22 (−0.57 to 1.01) |
| 4 | 1996 | 1.31 (0.40 to 2.23) | 2008 | −3.37 (−5.83 to −0.84) | NA | NA | NA | NA | −0.27 (−1.23 to 0.69) |
| 5 | 1996 | 1.58 (0.29 to 2.88) | 2007 | −3.97 (−6.34 to −1.53) | NA | NA | NA | NA | −0.62 (−1.74 to 0.52) |
| 6 | 1996 | 3.77 (1.74 to 5.85) | 2002 | −0.46 (−1.41 to 0.49) | 2012 | −8.99 (−18.33 to 1.42) | NA | NA | −0.07 (−1.37 to 1.25) |
| 7 | 1996 | 2.49 (0.38 to 4.65) | 2005 | −2.12 (−4.00 to −0.21) | NA | NA | NA | NA | 0.16 (−1.13 to 1.47) |
| 8 | 1996 | 7.27 (−1.86 to 17.24) | 2000 | −1.19 (−2.40 to 0.03) | NA | NA | NA | NA | 0.63 (−1.37 to 2.67) |
| 9 | 1996 | 0.06 (−0.81 to 0.93) | 2010 | −5.35 (−10.38 to −0.03) | NA | NA | NA | NA | −1.17 (−2.42 to 0.09) |
| 10 (highest decile) | 1996 | −0.91 (−1.80 to −0.01) | NA | NA | NA | NA | NA | NA | −0.91 (−1.80 to −0.01) |
Abbreviations: AAPC, average annual percentage change; MAAPC, mean AAPC; NA, not applicable.
Standardized to the 2013 European Standard Population by 5-year age groups.
Multivariable Analysis
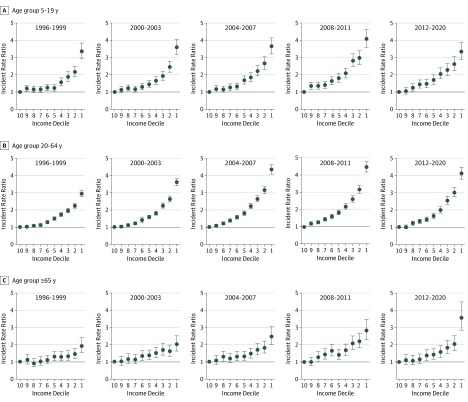
In the Poisson regression model adjusted for potential confounders, a negative income gradient was observed in the IRRs of the first hospital admissions for mental disorders in adults aged 20 to 64 years: the lower the income decile, the higher the IRR compared with the highest decile. In adults, the IRR of the lowest income decile in different periods varied from 2.94 (95% CI, 2.78-3.11) to 4.46 (95% CI, 4.17-4.76) (Figure 3B). The negative income gradient was observed in the 4 most common ICD-10 main groups, and the gradient was steepest in schizophrenia and related psychotic disorders, followed by substance use disorders (ICD-10 diagnoses F20-F29 and F10-F19, respectively). The gradients were less steep in mood disorders and neurotic disorders (ICD-10 diagnoses F30-F39 and F40-F48, respectively). Estimated IRRs of the lowest income decile were 5.89 (95% CI, 5.77-6.02) for schizophrenia and psychotic disorders, 5.21 (95% CI, 5.08-5.33) for substance use disorders, 2.81 (95% CI, 2.68-2.94) for mood disorders, and 2.89 (95% CI, 2.76-3.02) for neurotic disorders (eFigures 11-12 and eTable 7 in the Supplement). In children and adolescents, a constant gradient in the IRRs was observed in the 5 lowest deciles (Figure 3A). In nondwelling children and adolescents, the IRRs compared with the highest-income decile varied from 6.76 (95% CI 5.75-7.94) to 8.83 (95% CI 7.56-10.32) (eFigure 13 in the Supplement). In persons 65 years and older, no clear gradient was observed, but the IRRs were highest in the lowest income decile, varying from 1.93 (95% CI, 1.55-2.41) to 3.56 (95% CI, 2.83-4.47) (Figure 3C). Corresponding analyses were reproduced with income decile statuses 1, 3, and 5 years before the first admissions. The observed income gradients decreased but did not disappear. In adults, the highest IRRs in the lowest income decile were 3.68 (95% CI, 3.45-3.92) 1 year before first admissions, 2.97 (95% CI, 2.79-3.15) 3 years before first admissions, and 2.71 (95% CI, 2.56-2.87) 5 years before first admissions (eFigures 14-16 in the Supplement).
Figure 3. Incidence Rate Ratios for the First Psychiatric Hospital Admissions by Income.
Data markers denote the incidence rate ratio estimates compared with the highest income decile; error bars, 95% CIs. The model is adjusted for age group, sex, urbanicity, and decrease in income decile among those aged 5 to 19 years and for age group, sex, urbanicity, decrease in income decile, educational level, and living alone in those aged 20 to 64 years and 65 years or older. Income is equivalized in disposable income deciles, with 1 indicating the lowest income decile and 10, the highest (reference group).
Discussion
In this comprehensive, nationwide cohort study of register data, we found a clear negative income gradient in the incidence rates of first hospital admissions for mental disorders in the adult population, even after adjusting for potential confounders, including the level of education, urbanicity, living alone, and decrease in income within the previous 3 years. Low household income was associated with higher incidence during the whole study period among different age groups and between men and women, although in those 20 years or younger and 65 years or older, differences between the highest deciles diminished. Trends in incidence varied between income groups. The trends decreased throughout the whole study period only in the high-income groups. To our knowledge, this is the first national-level study showing that a robust income gradient is also present in the incidence rates of first hospitalizations due to mental disorders.
The income gradient in the adult population was evident at all levels of household income in overall and ICD-10 diagnostic main category-specific incidence rates. This finding is in line with the psychosocial theory of health inequalities, which states that adversity and stress associated with lower income increase the risk of a variety of illnesses,46,47 although the mechanisms linking income and mental health vary between disorders.22 Mental disorders have been associated with low future income,48 but changes in income after the first admissions were not evaluated in the present study. The disorder resulting in the first hospital treatment may also have influenced the person’s ability to earn or maintain their level of income already before the first admission.49 However, the income gradient was smaller, although still clearly observed, when income 1, 3, or 5 years before the first admissions was used for grouping the income deciles.
Opposite trends in the beginning of the study period suggested an increase in disparity between the highest and lowest income groups, which is another main finding of this study. Individuals with higher income might be in more stable and secure positions that make them more willing to undergo or more capable of receiving more intense outpatient care and avoiding first hospitalizations. This possibility is in convergence with the diffusion of innovations and cultural capital explanations of health inequalities, which state that adoption of new behaviors and the earlier uptake of new interventions, in this case outpatient care, occur earlier in higher socioeconomic positions.50 This also supports the view that some of the mechanisms linking income and health may be located within the health care system itself.25
The current approach facilitates comparisons in equality of the trends between income groups but offers limited means to interpret the population’s mental health in general. However, the overall rate of first admissions decreased during the study period in men and first increased and then decreased after 2008 in women. This finding is convergent with the decreasing total number of individuals in hospital care in Finland during the same time.32 Some evidence suggests that the true rate of mental health problems has increased in adolescents,51,52 and increasing disparity in mental health has previously been observed in the United States, United Kingdom, and Finland.53,54,55 The present results showed the increasing disparity between income groups also in first hospital-treated mental disorders; this seems to be the case especially in girls and women aged 15 to 19 years.
We focused on all first inpatient treatments rather than on diagnosis-specific rates so that possible sex-, income-, or race/ethnicity-related differences or variation in the temporal stability of the recorded diagnoses did not confound the analysis of the income gradient.56,57,58,59 Diagnosis-specific analysis, on the other hand, offers insight into temporal variations in the overall trends. In addition to changes in population mental health, these variations may reflect changes in the health care system and diagnostic practices. For example, during the deinstitutionalization process, inpatient treatment shifted to other facilities in Finland, which may at least partly explain the reduction in the rate of substance use–related first admission in men.60 In women, an increase in depression severity is a possible explanation for the increased rate of first hospitalizations.55 Decreasing trends in first admission rates of individual disorders, such as schizophrenia, have been associated with increased outpatient care and variations in diagnostic practices.61,62,63
Diagnosis-specific income gradient was steepest in schizophrenia and related psychotic disorders. Interestingly, social selection may be a more important mechanism in this diagnostic group.23 Differences in gradients between disorders need to be interpreted with caution, however, because help-seeking patterns and the proportion of outpatient care may have varied among income groups, disorders, and time. In substance use disorders, social consequences, rather than severity of dependence, may be associated with treatment entry and may partly explain the gradient.64 Mood disorders presented as the most common diagnostic group, with relatively smaller IRRs between the highest and lowest income deciles. This finding may reflect the relatively endogenous and evenly devastating nature of depression severe enough to require hospital treatment.
In terms of increased life expectancy, the deinstitutionalization of mental health care in Finland was successful for people with previous hospitalizations from 1981 to 2003, except for those with alcohol and substance abuse.65 Major legislative changes in 1991 transferred the responsibility to provide mental health services to the municipalities. This change coincided with an economic recession period that lasted until 1993 and led to significant regional differences in the capacity of psychiatric outpatient care. The general increase in the first-time hospitalizations in that era may reflect occasional failures in outpatient management. Nearer the global economic crisis in 2008, service organizing was partly recentralized as larger hospital districts started to take over the managing of psychiatric services. These systemic changes may moderate the general trends in hospitalizations but do not explain the income-related trends. The finding that individuals with low income are overrepresented in first hospitalizations, regardless of their diagnoses or the dominant service provider institutions at the time, should be taken into account even in countries with relatively low income inequality and universal welfare policies, such as Finland.66
Individual household members of different ages contribute differently to their household income. Children and adolescents in Finland have few possibilities of contributing to their families’ income, but family income is associated with many aspects of health.67,68,69 Nondwelling children and adolescents had high incidences of hospitalizations throughout the study period, and being institutionalized under foster care is probably the most common reason for nondwelling. By Nordic standards, foster care is relatively common in Finland,70 and children and adolescents in foster care have a substantial frequency of psychiatric hospitalizations and mental health problems.71
In persons 65 years and older, differences diminished between the highest income deciles, but those in the lowest income decile had the highest IRRs compared with the highest income decile. This finding is in line with some previous research,72 but in these age groups, persons’ economic circumstances are also affected by pension systems, household composition, and wealth and savings. Comorbid medical conditions are associated with mental disorders and low income and hence may partly explain the observed association. Whether the reasons for having low or reduced income are associated with the income gradient in mental health is an interesting question for further study.
Limitations
This study had some important limitations. First, no comprehensive data on outpatient treatments before the first inpatient treatments or population mental health in general were available for the study period. Change in income 3 years before the first admission was controlled instead. Second, not all monetary income and no wealth are captured with the national statistics of equivalized disposable income. Third, owing to the period covered by the registers, we used a 20-year clearance period to define a first hospital admission, which is a relatively short period of time in the group 65 years and older. Finally, the nature of causality and causal inference in epidemiology and health inequality are matters of debate. On its own, the present observational, register-based cohort study can describe the income gradient existing in the incidence of first psychiatric inpatient treatments.
Conclusions
This study observed a robust but temporally varying negative income gradient in first hospital-treated mental disorders. It appears that reduction in the use of inpatient care has not taken place equally between persons at different income levels. Many individuals admitted to psychiatric inpatient care for the first time are from low-income households. Hence, meeting the needs of these individuals in vulnerable positions in society appears to be an ongoing challenge for mental health services.
eMethods. Main ICD-10 Categories of Psychiatric Diagnoses
eTable 1. Recorded Main ICD-10 Categories of Psychiatric Discharge Diagnoses of First Psychiatric Hospital Treatments in Finland 1996-2014
eTable 2. Annual Age-Standardized Incidence Rates (IRs) of First Psychiatric Hospital Admissions
eTable 3. JoinPoint Analysis of Sex- and Income-Specific Age-Standardized Incidence Rates of First Psychiatric Hospital Admissions With Diagnosis of Mental and Behavioral Disorders Due to Psychoactive Substance Use
eTable 4. JoinPoint Analysis of Sex- and Income-Specific Age-Standardized Incidence Rates of First Psychiatric Hospital Admissions With Diagnosis of Schizophrenia, Schizotypal and Delusional Disorders
eTable 5. JoinPoint Analysis of Sex- and Income-Specific Age-Standardized Incidence Rates of First Psychiatric Hospital Admissions With Diagnosis of Mood Disorders
eTable 6. JoinPoint Analysis of Sex- and Income-Specific Age-Standardized Incidence Rates of First Psychiatric Hospital Admissions With Diagnosis of Neurotic, Stress-Related and Somatoform Disorders
eTable 7. Contrasts of the Predicted Incidence Rate Ratios Between ICD-10 Diagnostic Main Groups in Different Income Deciles
eFigure 1. Trends in Age-Standardized Incidence Rates of First Psychiatric Hospital Admissions With Organic Mental Disorders, Behavioral Syndromes Associated With Physiological Disturbances, and Personality Disorders
eFigure 2. Trends in Age-Standardized Incidence Rates of First Psychiatric Hospital Admissions With Disorders With Onset Usually Occurring in Childhood and Adolescence
eFigure 3. Trends in Age-Standardized Incidence Rates of First Psychiatric Hospital Admissions With Disorders With Major Psychotic Features
eFigure 4. Trends in Age-Standardized Annual Incidence Rates of First Psychiatric Hospital Admissions in the Nondwelling Finnish Population
eFigure 5. Trends in Income Decile- and Sex-Specific, Age-Standardized Incidence Rates of First Psychiatric Hospital Admissions With Substance Use Disorders (ICD-10 Codes F10-F19)
eFigure 6. Trends in Income Decile- and Sex-Specific, Age-Standardized Incidence Rates of First Psychiatric Hospital Admissions With Schizophrenia, Schizotypal and Delusional Disorders (ICD-10 Codes F20-F29)
eFigure 7. Trends in Income Decile- and Sex-Specific, Age-Standardized Incidence Rates of First Psychiatric Hospital Admissions With Mood Disorders (ICD-10 Codes F30-F39)
eFigure 8. Trends in Income Decile- And Sex-Specific, Age-Standardized Incidence Rates of First Psychiatric Hospital Admissions With Neurotic, Stress-Related and Somatoform Disorders (ICD-10 Codes F40-F48)
eFigure 9. Annual Sex- and Age Group–Specific Incidence Rates of First Psychiatric Hospital Admissions in the Lowest and Highest Income Deciles
eFigure 10. Annual Numbers of Person-Years at Risk of First Psychiatric Inpatient Treatments in the Lowest and Highest Income Deciles
eFigure 11. Incidence Rate Ratios for the First Psychiatric Hospital Admissions by Income With Different Diagnoses in Persons Aged 20-64 Years
eFigure 12. Predicted Incidence Rate Ratios for the First Psychiatric Hospital Admissions in Different ICD-10 Diagnostic Groups in Persons Aged 20-64 Years
eFigure 13. Incidence Rate Ratios for First Psychiatric Hospital Admissions in the Nondwelling Population
eFigure 14. Incidence Rate Ratios for the First Psychiatric Hospital Admissions by Income 1 Year Before First Admission
eFigure 15. Incidence Rate Ratios for the First Psychiatric Hospital Admissions by Income 3 Years Before First Admission
eFigure 16. Incidence Rate Ratios for the First Psychiatric Hospital Admissions by Income 5 Years Before First Admission
References
- 1.Fryers T, Melzer D, Jenkins R. Social inequalities and the common mental disorders: a systematic review of the evidence. Soc Psychiatry Psychiatr Epidemiol. 2003;38(5):229-237. doi: 10.1007/s00127-003-0627-2 [DOI] [PubMed] [Google Scholar]
- 2.Muntaner C, Eaton WW, Miech R, O’Campo P. Socioeconomic position and major mental disorders. Epidemiol Rev. 2004;26:53-62. doi: 10.1093/epirev/mxh001 [DOI] [PubMed] [Google Scholar]
- 3.Byrne M, Agerbo E, Eaton WW, Mortensen PB. Parental socio-economic status and risk of first admission with schizophrenia: a Danish national register based study. Soc Psychiatry Psychiatr Epidemiol. 2004;39(2):87-96. doi: 10.1007/s00127-004-0715-y [DOI] [PubMed] [Google Scholar]
- 4.Pulkki-Råback L, Ahola K, Elovainio M, et al. Socio-economic position and mental disorders in a working-age Finnish population: the Health 2000 Study. Eur J Public Health. 2012;22(3):327-332. doi: 10.1093/eurpub/ckr127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sareen J, Afifi TO, McMillan KA, Asmundson GJ. Relationship between household income and mental disorders: findings from a population-based longitudinal study. Arch Gen Psychiatry. 2011;68(4):419-427. doi: 10.1001/archgenpsychiatry.2011.15 [DOI] [PubMed] [Google Scholar]
- 6.Moustgaard H, Joutsenniemi K, Martikainen P. Does hospital admission risk for depression vary across social groups? a population-based register study of 231,629 middle-aged Finns. Soc Psychiatry Psychiatr Epidemiol. 2014;49(1):15-25. doi: 10.1007/s00127-013-0711-1 [DOI] [PubMed] [Google Scholar]
- 7.Mok PLH, Antonsen S, Pedersen CB, et al. Family income inequalities and trajectories through childhood and self-harm and violence in young adults: a population-based, nested case-control study. Lancet Public Health. 2018;3(10):e498-e507. doi: 10.1016/S2468-2667(18)30164-6 [DOI] [PubMed] [Google Scholar]
- 8.WHO and Calouste Gulbenkian Foundation Social Determinants of Mental Health. Geneva, Switzerland: World Health Organization; 2014. [Google Scholar]
- 9.Lund C, Breen A, Flisher AJ, et al. Poverty and common mental disorders in low and middle income countries: a systematic review. Soc Sci Med. 2010;71(3):517-528. doi: 10.1016/j.socscimed.2010.04.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pinto-Meza A, Moneta MV, Alonso J, et al. Social inequalities in mental health: results from the EU contribution to the World Mental Health Surveys Initiative. Soc Psychiatry Psychiatr Epidemiol. 2013;48(2):173-181. doi: 10.1007/s00127-012-0536-3 [DOI] [PubMed] [Google Scholar]
- 11.Junna L, Moustgaard H, Tarkiainen L, Martikainen P. The association between income and psychotropic drug purchases: individual fixed effects analysis of annual longitudinal data in 2003-2013. Epidemiology. 2019;30(2):221-229. doi: 10.1097/EDE.0000000000000956 [DOI] [PubMed] [Google Scholar]
- 12.Markkula N, Marola N, Nieminen T, et al. Predictors of new-onset depressive disorders: results from the longitudinal Finnish Health 2011 Study. J Affect Disord. 2017;208:255-264. doi: 10.1016/j.jad.2016.08.051 [DOI] [PubMed] [Google Scholar]
- 13.Arcaya MC, Arcaya AL, Subramanian SV. Inequalities in health: definitions, concepts, and theories. Glob Health Action. 2015;8:27106. doi: 10.3402/gha.v8.27106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marmot M, Friel S, Bell R, Houweling TAJ, Taylor S; Commission on Social Determinants of Health . Closing the gap in a generation: health equity through action on the social determinants of health. Lancet. 2008;372(9650):1661-1669. doi: 10.1016/S0140-6736(08)61690-6 [DOI] [PubMed] [Google Scholar]
- 15.Björkenstam E, Cheng S, Burström B, Pebley AR, Björkenstam C, Kosidou K. Association between income trajectories in childhood and psychiatric disorder: a Swedish population-based study. J Epidemiol Community Health. 2017;71(7):648-654. doi: 10.1136/jech-2016-208513 [DOI] [PubMed] [Google Scholar]
- 16.Case A, Lubotsky D, Paxson C. Economic status and health in childhood: the origins of the gradient. Am Econ Rev. 2002;92(5):1308-1334. doi: 10.1257/000282802762024520 [DOI] [PubMed] [Google Scholar]
- 17.Sturm R, Gresenz CR. Relations of income inequality and family income to chronic medical conditions and mental health disorders: national survey. BMJ. 2002;324(7328):20-23. doi: 10.1136/bmj.324.7328.20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kahneman D, Krueger AB, Schkade D, Schwarz N, Stone AA. Would you be happier if you were richer? a focusing illusion. Science. 2006;312(5782):1908-1910. doi: 10.1126/science.1129688 [DOI] [PubMed] [Google Scholar]
- 19.Mogilner C, Norton MI. Time, money, and happiness. Curr Opin Psychol. 2016;10:12-16. doi: 10.1016/j.copsyc.2015.10.018 [DOI] [Google Scholar]
- 20.Jebb AT, Tay L, Diener E, Oishi S. Happiness, income satiation and turning points around the world. Nat Hum Behav. 2018;2(1):33-38. doi: 10.1038/s41562-017-0277-0 [DOI] [PubMed] [Google Scholar]
- 21.Hudson CG. Socioeconomic status and mental illness: tests of the social causation and selection hypotheses. Am J Orthopsychiatry. 2005;75(1):3-18. doi: 10.1037/0002-9432.75.1.3 [DOI] [PubMed] [Google Scholar]
- 22.Miech RA, Caspi A, Moffitt TE, Wright BRE, Silva PA. Low socioeconomic status and mental disorders: a longitudinal study of selection and causation during young adulthood. Am J Sociol. 1999;104(4):1096-1131. doi: 10.1086/210137 [DOI] [Google Scholar]
- 23.Dohrenwend BP, Levav I, Shrout PE, et al. Socioeconomic status and psychiatric disorders: the causation-selection issue. Science. 1992;255(5047):946-952. doi: 10.1126/science.1546291 [DOI] [PubMed] [Google Scholar]
- 24.Costello EJ, Compton SN, Keeler G, Angold A. Relationships between poverty and psychopathology: a natural experiment. JAMA. 2003;290(15):2023-2029. doi: 10.1001/jama.290.15.2023 [DOI] [PubMed] [Google Scholar]
- 25.Øversveen E, Rydland HT, Bambra C, Eikemo TA. Rethinking the relationship between socio-economic status and health: making the case for sociological theory in health inequality research. Scand J Public Health. 2017;45(2):103-112. doi: 10.1177/1403494816686711 [DOI] [PubMed] [Google Scholar]
- 26.Braveman P, Gottlieb L. The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep. 2014;129(suppl 2):19-31. doi: 10.1177/00333549141291S206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Forbes A, Wainwright SP. On the methodological, theoretical and philosophical context of health inequalities research: a critique. Soc Sci Med. 2001;53(6):801-816. doi: 10.1016/S0277-9536(00)00383-X [DOI] [PubMed] [Google Scholar]
- 28.Deaton AS. What does the empirical evidence tell us about the injustice of health inequalities? https://ssrn.com/abstract=1746951. Updated 2011. Accessed November 9, 2018.
- 29.Kröger H, Pakpahan E, Hoffmann R. What causes health inequality? a systematic review on the relative importance of social causation and health selection. Eur J Public Health. 2015;25(6):951-960. doi: 10.1093/eurpub/ckv111 [DOI] [PubMed] [Google Scholar]
- 30.van Doorslaer E, Masseria C, Koolman X; OECD Health Equity Research Group . Inequalities in access to medical care by income in developed countries. CMAJ. 2006;174(2):177-183. doi: 10.1503/cmaj.050584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chow WS, Priebe S. Understanding psychiatric institutionalization: a conceptual review. BMC Psychiatry. 2013;13(1):169. doi: 10.1186/1471-244X-13-169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pirkola S, Sohlman B, Heilä H, Wahlbeck K. Reductions in postdischarge suicide after deinstitutionalization and decentralization: a nationwide register study in Finland. Psychiatr Serv. 2007;58(2):221-226. doi: 10.1176/ps.2007.58.2.221 [DOI] [PubMed] [Google Scholar]
- 33.National Institute for Health and Welfare. Statistical Information on Welfare and Health in Finland. Psychiatric inpatient care, average length of stay and patients per 1000 inhabitants. https://sotkanet.fi/sotkanet/en/taulukko/?indicator=s87yjjcCAA==®ion=s07MBAA=&year=sy4rtc7U0zUEAA==&gender=t&abs=f&color=f&buildVersion=3.0-SNAPSHOT&buildTimestamp=201802280718. Published September 12, 2019. Accessed May 17, 2019.
- 34.Daly A, Walsh D. Activities of Irish Psychiatric Units and Hospitals 2014. Health Research Board Statistics Series 26. Dublin, Ireland: Health Research Board; 2015. [Google Scholar]
- 35.Joensen S, Wang AG. First admissions for psychiatric disorders: a comparison between the Faroe Islands and Denmark. Acta Psychiatr Scand. 1983;68(1):66-71. doi: 10.1111/j.1600-0447.1983.tb06982.x [DOI] [PubMed] [Google Scholar]
- 36.Castillejos MC, Martín-Pérez C, Moreno-Küstner B. A systematic review and meta-analysis of the incidence of psychotic disorders: the distribution of rates and the influence of gender, urbanicity, immigration and socio-economic level. Psychol Med. 2018;48(13):1-15. doi: 10.1017/S0033291718000235 [DOI] [PubMed] [Google Scholar]
- 37.Pulkki-Råback L, Kivimäki M, Ahola K, et al. Living alone and antidepressant medication use: a prospective study in a working-age population. BMC Public Health. 2012;12(1):236. doi: 10.1186/1471-2458-12-236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Barbaglia MG, ten Have M, Dorsselaer S, Alonso J, de Graaf R. Negative socioeconomic changes and mental disorders: a longitudinal study. J Epidemiol Community Health. 2015;69(1):55-62. doi: 10.1136/jech-2014-204184 [DOI] [PubMed] [Google Scholar]
- 39.Official Statistics of Finland (OSF) Statistical grouping of municipalities. https://www.stat.fi/meta/kas/til_kuntaryhmit_en.html. Accessed January 5, 2019.
- 40.UNESCO Institute for Statistics International Standard Classification of Education 2011. http://uis.unesco.org/sites/default/files/documents/international-standard-classification-of-education-isced-2011-en.pdf. Updated 2012. Accessed January 5, 2019.
- 41.Sund R. Quality of the Finnish Hospital Discharge register: a systematic review. Scand J Public Health. 2012;40(6):505-515. doi: 10.1177/1403494812456637 [DOI] [PubMed] [Google Scholar]
- 42.Förster MF. Mira D’Ercole M. The OECD approach to measuring income distribution and poverty: strengths, limits and statistical issues. http://umdcipe.org/conferences/oecdumd/conf_papers/Papers/The_OECD_Approach_to_Measuring_Income_Distribution_and_Poverty.pdf. Updated 2009. Accessed November 7, 2018.
- 43.Official Statistics of Finland (OSF) Household-dwelling units and housing conditions [e-publication]. Helsinki: Statistics Finland. http://www.stat.fi/til/asuolo/kas_en.html. Accessed November 8, 2018.
- 44.Eurostat. Revision of the European Standard Population. Report of Eurostat’s task force. https://ec.europa.eu/eurostat/documents/3859598/5926869/KS-RA-13-028-EN.PDF/e713fa79-1add-44e8-b23d-5e8fa09b3f8f. Updated 2013. Accessed October 8, 2018.
- 45.Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for JoinPoint regression with applications to cancer rates. Stat Med. 2000;19(3):335-351. doi: [DOI] [PubMed] [Google Scholar]
- 46.Marmot M, Wilkinson RG. Psychosocial and material pathways in the relation between income and health: a response to Lynch et al. BMJ. 2001;322(7296):1233-1236. doi: 10.1136/bmj.322.7296.1233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mackenbach JP. Persistence of social inequalities in modern welfare states: explanation of a paradox. Scand J Public Health. 2017;45(2):113-120. doi: 10.1177/1403494816683878 [DOI] [PubMed] [Google Scholar]
- 48.Hakulinen C, Elovainio M, Arffman M, et al. Mental disorders and long-term labour market outcomes: nationwide cohort study of 2 055 720 individuals. [published online June 29, 2019]. Acta Psychiatr Scand. 2019;140(4):371-381. doi: 10.1111/acps.13067 [DOI] [PubMed] [Google Scholar]
- 49.Agerbo E, Byrne M, Eaton WW, Mortensen PB. Marital and labor market status in the long run in schizophrenia. Arch Gen Psychiatry. 2004;61(1):28-33. doi: 10.1001/archpsyc.61.1.28 [DOI] [PubMed] [Google Scholar]
- 50.Mackenbach JP. The persistence of health inequalities in modern welfare states: the explanation of a paradox. Soc Sci Med. 2012;75(4):761-769. doi: 10.1016/j.socscimed.2012.02.031 [DOI] [PubMed] [Google Scholar]
- 51.Bor W, Dean AJ, Najman J, Hayatbakhsh R. Are child and adolescent mental health problems increasing in the 21st century? a systematic review. Aust N Z J Psychiatry. 2014;48(7):606-616. doi: 10.1177/0004867414533834 [DOI] [PubMed] [Google Scholar]
- 52.Collishaw S. Annual research review: secular trends in child and adolescent mental health. J Child Psychol Psychiatry. 2015;56(3):370-393. doi: 10.1111/jcpp.12372 [DOI] [PubMed] [Google Scholar]
- 53.Weinberger AH, Gbedemah M, Martinez AM, Nash D, Galea S, Goodwin RD. Trends in depression prevalence in the USA from 2005 to 2015: widening disparities in vulnerable groups. Psychol Med. 2018;48(8):1308-1315. doi: 10.1017/S0033291717002781 [DOI] [PubMed] [Google Scholar]
- 54.Ross A, Kelly Y, Sacker A. Time trends in mental well-being: the polarisation of young people’s psychological distress. Soc Psychiatry Psychiatr Epidemiol. 2017;52(9):1147-1158. doi: 10.1007/s00127-017-1419-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Torikka A, Kaltiala-Heino R, Rimpelä A, Marttunen M, Luukkaala T, Rimpelä M. Self-reported depression is increasing among socio-economically disadvantaged adolescents: repeated cross-sectional surveys from Finland from 2000 to 2011. BMC Public Health. 2014;14:408. doi: 10.1186/1471-2458-14-408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Minsky S, Vega W, Miskimen T, Gara M, Escobar J. Diagnostic patterns in Latino, African American, and European American psychiatric patients. Arch Gen Psychiatry. 2003;60(6):637-644. doi: 10.1001/archpsyc.60.6.637 [DOI] [PubMed] [Google Scholar]
- 57.Blow FC, Zeber JE, McCarthy JF, Valenstein M, Gillon L, Bingham CR. Ethnicity and diagnostic patterns in veterans with psychoses. Soc Psychiatry Psychiatr Epidemiol. 2004;39(10):841-851. doi: 10.1007/s00127-004-0824-7 [DOI] [PubMed] [Google Scholar]
- 58.Piccinelli M, Wilkinson G. Gender differences in depression: critical review. Br J Psychiatry. 2000;177(6):486-492. doi: 10.1192/bjp.177.6.486 [DOI] [PubMed] [Google Scholar]
- 59.Baca-Garcia E, Perez-Rodriguez MM, Basurte-Villamor I, et al. Diagnostic stability of psychiatric disorders in clinical practice. Br J Psychiatry. 2007;190(3):210-216. doi: 10.1192/bjp.bp.106.024026 [DOI] [PubMed] [Google Scholar]
- 60.Kaltiala-Heino R, Laippala P, Joukamaa M. Has the attempt to reduce psychiatric inpatient treatment been successful in Finland? Eur Psychiatry. 2001;16(4):215-221. doi: 10.1016/S0924-9338(01)00567-3 [DOI] [PubMed] [Google Scholar]
- 61.Suvisaari JM, Haukka JK, Tanskanen AJ, Lönnqvist JK. Decline in the incidence of schizophrenia in Finnish cohorts born from 1954 to 1965. Arch Gen Psychiatry. 1999;56(8):733-740. doi: 10.1001/archpsyc.56.8.733 [DOI] [PubMed] [Google Scholar]
- 62.Kendell RE, Malcolm DE, Adams W. The problem of detecting changes in the incidence of schizophrenia. Br J Psychiatry. 1993;162(2):212-218. doi: 10.1192/bjp.162.2.212 [DOI] [PubMed] [Google Scholar]
- 63.Chiang CL, Chen PC, Huang LY, et al. Time trends in first admission rates for schizophrenia and other psychotic disorders in Taiwan, 1998-2007: a 10-year population-based cohort study. Soc Psychiatry Psychiatr Epidemiol. 2017;52(2):163-173. doi: 10.1007/s00127-016-1326-0 [DOI] [PubMed] [Google Scholar]
- 64.Weisner C, Matzger H, Tam T, Schmidt L. Who goes to alcohol and drug treatment? understanding utilization within the context of insurance. J Stud Alcohol. 2002;63(6):673-682. doi: 10.15288/jsa.2002.63.673 [DOI] [PubMed] [Google Scholar]
- 65.Westman J, Gissler M, Wahlbeck K. Successful deinstitutionalization of mental health care: increased life expectancy among people with mental disorders in Finland. Eur J Public Health. 2012;22(4):604-606. doi: 10.1093/eurpub/ckr068 [DOI] [PubMed] [Google Scholar]
- 66.Bubbico RL, Freytag L Inequality in Europe. https://www.eib.org/attachments/efs/econ_inequality_in_europe_en.pdf. Published 2018. Accessed July 20, 2019.
- 67.Reiss F. Socioeconomic inequalities and mental health problems in children and adolescents: a systematic review. Soc Sci Med. 2013;90:24-31. doi: 10.1016/j.socscimed.2013.04.026 [DOI] [PubMed] [Google Scholar]
- 68.Noble KG, Houston SM, Brito NH, et al. Family income, parental education and brain structure in children and adolescents. Nat Neurosci. 2015;18(5):773-778. doi: 10.1038/nn.3983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Patton GC, Sawyer SM, Santelli JS, et al. Our future: a Lancet commission on adolescent health and wellbeing. Lancet. 2016;387(10 036):2423-2478. doi: 10.1016/S0140-6736(16)00579-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kääriälä A, Hiilamo H. Children in out-of-home care as young adults: a systematic review of outcomes in the nordic countries. Child Youth Serv Rev. 2017;79:107-114. doi: 10.1016/j.childyouth.2017.05.030 [DOI] [Google Scholar]
- 71.Egelund T, Lausten M. Prevalence of mental health problems among children placed in out-of-home care in Denmark. Child Fam Soc Work. 2009;14(2):156-165. doi: 10.1111/j.1365-2206.2009.00620.x [DOI] [Google Scholar]
- 72.Huisman M, Kunst AE, Mackenbach JP. Socioeconomic inequalities in morbidity among the elderly: a European overview. Soc Sci Med. 2003;57(5):861-873. doi: 10.1016/S0277-9536(02)00454-9 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. Main ICD-10 Categories of Psychiatric Diagnoses
eTable 1. Recorded Main ICD-10 Categories of Psychiatric Discharge Diagnoses of First Psychiatric Hospital Treatments in Finland 1996-2014
eTable 2. Annual Age-Standardized Incidence Rates (IRs) of First Psychiatric Hospital Admissions
eTable 3. JoinPoint Analysis of Sex- and Income-Specific Age-Standardized Incidence Rates of First Psychiatric Hospital Admissions With Diagnosis of Mental and Behavioral Disorders Due to Psychoactive Substance Use
eTable 4. JoinPoint Analysis of Sex- and Income-Specific Age-Standardized Incidence Rates of First Psychiatric Hospital Admissions With Diagnosis of Schizophrenia, Schizotypal and Delusional Disorders
eTable 5. JoinPoint Analysis of Sex- and Income-Specific Age-Standardized Incidence Rates of First Psychiatric Hospital Admissions With Diagnosis of Mood Disorders
eTable 6. JoinPoint Analysis of Sex- and Income-Specific Age-Standardized Incidence Rates of First Psychiatric Hospital Admissions With Diagnosis of Neurotic, Stress-Related and Somatoform Disorders
eTable 7. Contrasts of the Predicted Incidence Rate Ratios Between ICD-10 Diagnostic Main Groups in Different Income Deciles
eFigure 1. Trends in Age-Standardized Incidence Rates of First Psychiatric Hospital Admissions With Organic Mental Disorders, Behavioral Syndromes Associated With Physiological Disturbances, and Personality Disorders
eFigure 2. Trends in Age-Standardized Incidence Rates of First Psychiatric Hospital Admissions With Disorders With Onset Usually Occurring in Childhood and Adolescence
eFigure 3. Trends in Age-Standardized Incidence Rates of First Psychiatric Hospital Admissions With Disorders With Major Psychotic Features
eFigure 4. Trends in Age-Standardized Annual Incidence Rates of First Psychiatric Hospital Admissions in the Nondwelling Finnish Population
eFigure 5. Trends in Income Decile- and Sex-Specific, Age-Standardized Incidence Rates of First Psychiatric Hospital Admissions With Substance Use Disorders (ICD-10 Codes F10-F19)
eFigure 6. Trends in Income Decile- and Sex-Specific, Age-Standardized Incidence Rates of First Psychiatric Hospital Admissions With Schizophrenia, Schizotypal and Delusional Disorders (ICD-10 Codes F20-F29)
eFigure 7. Trends in Income Decile- and Sex-Specific, Age-Standardized Incidence Rates of First Psychiatric Hospital Admissions With Mood Disorders (ICD-10 Codes F30-F39)
eFigure 8. Trends in Income Decile- And Sex-Specific, Age-Standardized Incidence Rates of First Psychiatric Hospital Admissions With Neurotic, Stress-Related and Somatoform Disorders (ICD-10 Codes F40-F48)
eFigure 9. Annual Sex- and Age Group–Specific Incidence Rates of First Psychiatric Hospital Admissions in the Lowest and Highest Income Deciles
eFigure 10. Annual Numbers of Person-Years at Risk of First Psychiatric Inpatient Treatments in the Lowest and Highest Income Deciles
eFigure 11. Incidence Rate Ratios for the First Psychiatric Hospital Admissions by Income With Different Diagnoses in Persons Aged 20-64 Years
eFigure 12. Predicted Incidence Rate Ratios for the First Psychiatric Hospital Admissions in Different ICD-10 Diagnostic Groups in Persons Aged 20-64 Years
eFigure 13. Incidence Rate Ratios for First Psychiatric Hospital Admissions in the Nondwelling Population
eFigure 14. Incidence Rate Ratios for the First Psychiatric Hospital Admissions by Income 1 Year Before First Admission
eFigure 15. Incidence Rate Ratios for the First Psychiatric Hospital Admissions by Income 3 Years Before First Admission
eFigure 16. Incidence Rate Ratios for the First Psychiatric Hospital Admissions by Income 5 Years Before First Admission