This systematic review and meta-analysis provides an updated synthesis of the published randomized clinical trials into the use and advantages of acupuncture and/or acupressure among patients with cancer pain.
Key Points
Question
Is the use of acupuncture and acupressure associated with improved cancer pain management compared with sham intervention and/or analgesic therapy alone?
Findings
In this systematic review of 17 randomized clinical trials and meta-analysis of 14 trials in the current English-language and Chinese-language literature, a significant association was found between real (compared with sham) acupuncture and reduced pain, and acupuncture combined with analgesic therapy was associated with decreased analgesic use. However, heterogeneity lowered the level of certainty of the evidence.
Meaning
This study found a moderate level of evidence that acupuncture and/or acupressure was significantly associated with lower pain intensity in patients with cancer compared with a sham control, which suggests a potential for a combination of acupuncture and acupressure to help reduce opioid doses in patients with cancer.
Abstract
Importance
Research into acupuncture and acupressure and their application for cancer pain has been growing, but the findings have been inconsistent.
Objective
To evaluate the existing randomized clinical trials (RCTs) for evidence of the association of acupuncture and acupressure with reduction in cancer pain.
Data Sources
Three English-language databases (PubMed, Embase, and CINAHL) and 4 Chinese-language biomedical databases (Chinese Biomedical Literature Database, VIP Database for Chinese Technical Periodicals, China National Knowledge Infrastructure, and Wanfang) were searched for RCTs published from database inception through March 31, 2019.
Study Selection
Randomized clinical trials that compared acupuncture and acupressure with a sham control, analgesic therapy, or usual care for managing cancer pain were included.
Data Extraction and Synthesis
Data were screened and extracted independently using predesigned forms. The quality of RCTs was appraised with the Cochrane Collaboration risk of bias tool. Random-effects modeling was used to calculate the effect sizes of included RCTs. The quality of evidence was evaluated with the Grading of Recommendations Assessment, Development and Evaluation approach.
Main Outcomes and Measures
The primary outcome was pain intensity measured by the Brief Pain Inventory, Numerical Rating Scale, Visual Analog Scale, or Verbal Rating Scale.
Results
A total of 17 RCTs (with 1111 patients) were included in the systematic review, and data from 14 RCTs (with 920 patients) were used in the meta-analysis. Seven sham-controlled RCTs (35%) were notable for their high quality, being judged to have a low risk of bias for all of their domains, and showed that real (compared with sham) acupuncture was associated with reduced pain intensity (mean difference [MD], −1.38 points; 95% CI, −2.13 to −0.64 points; I2 = 81%). A favorable association was also seen when acupuncture and acupressure were combined with analgesic therapy in 6 RCTs for reducing pain intensity (MD, −1.44 points; 95% CI, −1.98 to −0.89; I2 = 92%) and in 2 RCTs for reducing opioid dose (MD, −30.00 mg morphine equivalent daily dose; 95% CI, −37.5 mg to −22.5 mg). The evidence grade was moderate because of the substantial heterogeneity among studies.
Conclusions and Relevance
This systematic review and meta-analysis found that acupuncture and/or acupressure was significantly associated with reduced cancer pain and decreased use of analgesics, although the evidence level was moderate. This finding suggests that more rigorous trials are needed to identify the association of acupuncture and acupressure with specific types of cancer pain and to integrate such evidence into clinical care to reduce opioid use.
Introduction
Pain is a distressing symptom experienced by more than 70% of patients with cancer but inadequately controlled in nearly 50% of these patients.1,2 Although the World Health Organization analgesic ladder provides effectual approaches to relieve cancer pain,3 addiction to analgesics and the adverse effects of pharmacological interventions pose critical challenges to pain management.4,5 Because pain is multidimensional, a multidisciplinary, comprehensive approach is needed to control pain successfully.6,7
The ongoing opioid crisis in the United States exacerbates the challenges surrounding cancer pain management,8,9,10,11 with government organizations calling for the use of nonpharmacological interventions12 on the basis of increasing clinical evidence.13,14 Leading organizations in the field, such as the American Society for Clinical Oncology and the National Comprehensive Cancer Network, recommend nonpharmacological interventions, such as acupuncture, for managing cancer pain.15,16
Research on acupuncture for cancer pain has been growing, but the findings have been inconsistent.17 Although more than 20 systematic reviews were conducted to establish the association of acupuncture with cancer pain,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40 none arrived at a definitive conclusion. In addition, more rigorous randomized clinical trials (RCTs) of acupuncture and related therapies published in recent years were not included in previous systematic reviews. For example, a multicenter RCT of acupuncture published in 2018 found that patients with early-stage breast cancer who received aromatase inhibitor therapy experienced significant pain relief.41 The reduction in pain reported in this 2018 study was clinically relevant.42
In light of the growing number of RCTs of acupuncture or acupressure use for cancer pain and the ensuing need for critical evaluation, we conducted a systematic review and meta-analysis of the available evidence to inform clinical practice. The specific research questions were as follows: (1) Are acupuncture and acupressure associated with reduction in cancer pain compared with sham control or usual care control? (2) Is the combination of acupuncture and acupressure associated with reduction in analgesic use in patients with cancer?
Methods
This systematic review and meta-analysis (PROSPERO registration No. CRD42017064113), with its peer-reviewed protocol published online,43 focused on RCTs involving acupuncture and acupressure interventions for addressing pain intensity and analgesic dose in patients with cancer. The quality of RCTs was appraised with the Cochrane Collaboration risk of bias tool.44 The overall evidence and certainty of evidence were evaluated with the Grading of Recommendations Assessment, Development and Evaluation approach.
Search Strategy and Study Selection
Three English-language databases (PubMed, Embase, and CINAHL) and 4 Chinese-language databases (Chinese Biomedical Literature Database, VIP Database for Chinese Technical Periodicals, China National Knowledge Infrastructure, and Wanfang) were searched for RCTs published from the database inception through March 31, 2019. The search strategy consisted of 3 components: clinical condition (cancer, tumor/tumour, carcinoma, neoplasm AND pain, analgesia), intervention (manual acupuncture, electroacupuncture, body or auricular acupressure), and study type (randomized clinical trial). Existing systematic reviews were examined to identify additional trials. Two of us (Y.H. and Y.L.) independently screened the records of comprehensive searches by titles and abstracts, or full text as needed, to establish the eligibility of the studies. Articles published in the English or Chinese language were included if they were RCTs (with or without blinding, including crossover design and pragmatic trials) investigating the association of acupuncture and acupressure with cancer pain. Pain directly accompanying the development of cancer and/or chronic pain associated with cancer treatments was included. Studies of acupuncture for short-term analgesia associated with surgical procedures were excluded. Eligible interventions were acupuncture and acupressure regardless of needling techniques and stimulation methods, including manual acupuncture and acupressure, electroacupuncture, or a combination of these techniques. The comparison could be between sham or placebo acupuncture and analgesic therapy or usual care without additional intervention. Studies comparing 2 kinds of acupuncture techniques or acupuncture with another traditional Chinese medicine therapy (eg, herbal medicine, massage) were excluded. Pain intensity was selected as the targeted outcome because of its substantial role in cancer pain assessment and pain management.45 Outcome measures included the Brief Pain Inventory, Numerical Rating Scale, Visual Analog Scale, Verbal Rating Scale, and other validated instruments for assessing the intensity of pain. Studies that reported only improvement rates were excluded.
Data Extraction and Quality Assessment
All data extraction was independently undertaken by 2 of us (Y.H. and X.G.) using predesigned forms. Clinical features (participants, interventions, and outcome measurements), details of the treatments, methodological characteristics, and the results of each outcome were extracted for each study. Two of us (Y.H. and Y.L.) independently appraised the quality of studies included, and disagreements were resolved by discussion and consensus with another reviewer (A.L.Z.). Each RCT was assigned a low, high, or unclear risk of bias for 6 specific domains (sequence generation, allocation concealment, blinding of participants and outcome assessment, incomplete outcome data, selective outcome reporting, and other potential threats), using information identified from the published articles and supplementary materials and by contacting the study authors when needed.
Synthesis of Evidence
Meta-analysis of RCTs with available data was performed by calculating the effect size and 95% CI using the random-effects model. Heterogeneity among trials was identified by the χ2 test and reported as I2. Statistical analyses were performed with Stata, version 14.0 (StataCorp LLC). Two-sided P < .05 was considered statistically significant.
Studies were grouped according to the type of intervention (acupuncture, acupressure, or combination) and the comparator (sham therapy). For studies with more than 1 control group, such as real acupuncture vs sham acupuncture vs wait- list control, the results were split into pairwise comparisons by the different comparators. When different outcomes from the same study were reported in separate publications, the data were merged.
Given the strong correlation between scales of pain assessment,46 the results measured by the Visual Analog Scale were converted to the corresponding grade in the 11-point Numerical Rating Scale (0 points indicating no pain and 10 points indicating most severe pain). For example, a result of 40 mm on the 100-mm version of the Visual Analog Scale was recorded as 4 points for data synthesis. The results of the Numerical Rating Scale, the converted Visual Analog Scale, and the Brief Pain Inventory severity subscale were used in the meta-analysis.
Subgroup sensitivity analyses were conducted to explore potential sources of heterogeneity. When possible and appropriate, planned subgroup analyses included the source of pain (cancerous organ or specific treatment), severity of pain (mild, moderate, or severe16), and type of treatment (manual acupuncture, electroacupuncture, or auricular acupuncture).
Publication bias was assessed by funnel plots and the Egger test for asymmetry when at least 10 trials were included. The quality and certainty of evidence are summarized in the eTable.
Results
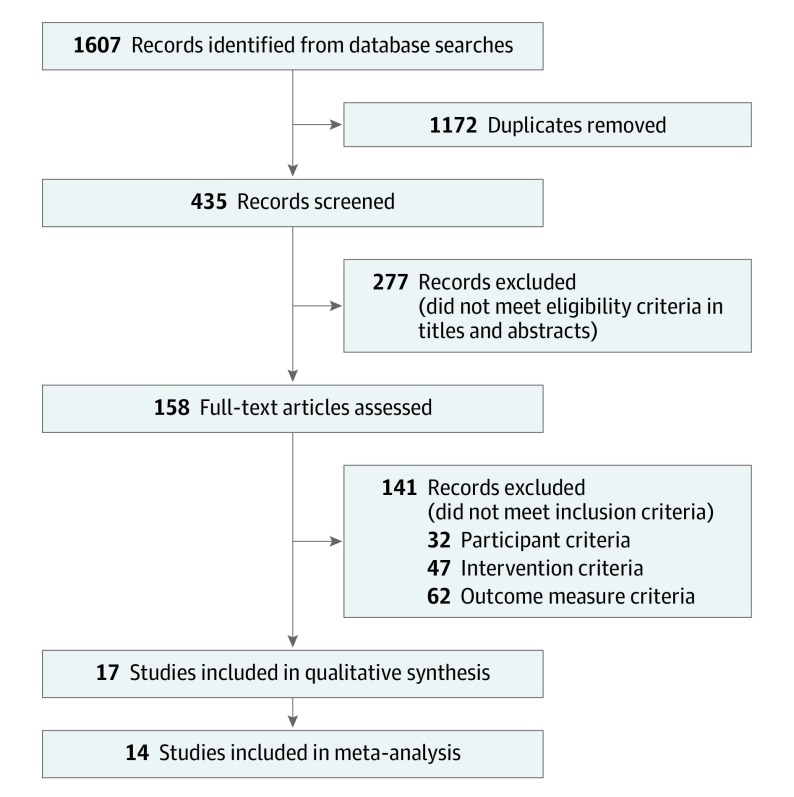
A total of 1607 articles were identified through database searches, from which 1172 duplicate publications (73%) were removed and 418 articles (26%) were excluded for not meeting the inclusion criteria. Seventeen RCTs (1%) were included in the systematic review or qualitative synthesis41,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62 (Figure 1 and Table). The study characteristics of these RCTs are summarized in the eTable in the Supplement. Quantitative synthesis was performed with 14 RCTs (82%) by pooling the results through a meta-analysis; these 14 trials involved 920 patients with cancer. Three (18%) of the 17 trials had insufficient data.55,57,61 Seven of the studies (41%) included were conducted in China, 6 (35%) were in the United States, and 1 (6%) each were in Australia, Brazil, France, and Korea.
Figure 1. Flow Diagram.
Table. Summary of Findings.
| Certainty Assessment | No. of Patients | Effect Size | Level of Certainty | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. of Studies | Source | Risk of Bias | Inconsistency | Indirectness | Imprecision | Publication Bias | Acupuncture and/or Acupressure Group | Control Group | Mean Difference (95% CI) | |
| Real vs sham acupuncture for reducing pain intensity | ||||||||||
| 7 | Hershman et al,41 2018; Ruela et al,47 2018; Kim and Lee,48 2018; Mao et al,53 2014; Chen et al,56 2013; Crew et al,60 2010; Alimi et al,62 2003 | Not serious | Seriousa | Not serious | Not serious | Undetected | 226 | 172 | −1.38 points (−2.13 to −0.64) | Moderate |
| Acupuncture and/or acupressure plus analgesics vs analgesics only for reducing pain intensity | ||||||||||
| 6 | Wang et al,49 2017; Shen et al,50 2016; Wang et al,51 2015; Guo et al,52 2015; Zhu et al,54 2013; Jiang,58 2011 | Seriousb | Seriousc | Not serious | Not serious | Undetected | 195 | 195 | −1.44 points (−1.98 to −0.89) | Low |
| Acupuncture vs wait-list control for reducing pain intensity | ||||||||||
| 3 | Hershman et al,41 2018; Mao et al,53 2014; Pfister et al,59 2010 | Seriousb | Not serious | Not serious | Not serious | Undetected | 151 | 104 | −1.63 points (−2.14 to −1.13) | Moderate |
| Acupuncture and/or acupressure plus analgesics vs analgesics only for reducing analgesic dose | ||||||||||
| 2 | Wang et al,49 2017; Zhu et al,54 2013 | Seriousb | Not serious | Not serious | Not serious | Undetected | 53 | 53 | −30.00 mg of morphine equivalent daily dose (−37.5 to −22.5) | Moderate |
Heterogeneity: I2 = 81%.
High risk of performance and detection bias owing to nonblinding.
Heterogeneity: I2 = 92%.
Characteristics of Clinical Studies and Quality of Evidence
Among the 17 RCTs included, 9 (53%) were sham controlled and 8 (47%) were open-label trials. Thirteen studies (76%) employed a 2-group parallel design, 6 of which compared real acupuncture with sham acupuncture47,48,55,56,57,60 and 7 of which compared the combination of acupuncture and acupressure with analgesic therapy49,50,51,52,54,58 or usual care.59 Three 3-group studies (18%) were included; 2 compared real acupuncture with sham acupuncture or wait-list control41,53 and 1 compared acupuncture with 2 kinds of sham control.62 One RCT (6%) assessed the outcome of acupuncture using an open-label crossover design.61 Sample sizes ranged from 21 to 226 patients, and a total of 1111 patients were included, with 515 (46%) in the experimental group, 575 (52%) in the control group, and 21 (2%) in the crossover RCT.
Thirteen studies (76%) focused on a specific kind of cancer pain (6 aromatase inhibitor–induced arthralgia,41,53,55,57,60,61 2 lung cancer pain,49,50 1 gastric cancer pain,52 1 pancreatic cancer pain,56 1 malignant neuropathic pain,54 1 osseous metastatic pain,51 and 1 persistent pain after a surgical procedure59), and 4 (24%) studies investigated general cancer pain with a mix of cancer diagnoses.47,48,58,62 The inclusion criteria in 13 studies limited pain to moderate and severe (at least 3 or 4 points on a 0-to-10 scale) intensity.41,47,50,51,53,54,55,56,57,59,60,61,62 A detailed summary of participants is provided in the eTable in the Supplement. Six sham-controlled studies (35%) were notable for their high quality, as each of the 6 domains in these studies was judged to have a low risk of bias.41,48,53,55,57,60 Because the measurements for pain were subjective patient-reported outcomes, detection bias existed if participants were not blinded to the treatments. Therefore, the 7 open-label, 2-group RCTs (41%) without sham acupuncture were rated as having a high risk of bias for blinding of the participants and outcome assessors.49,50,51,52,54,58,59 For the 3-group studies that compared real acupuncture with sham acupuncture or wait-list controls, blinding was rated as having a low risk of bias for the former comparison and a high risk of bias for the latter.41,53 Two studies (12%)49,61 were unclear about random sequence generation, and 9 (53%)47,49,50,51,52,54,56,58,61 were unclear on allocation concealment. Fifteen studies (88%) were at low risk of attrition bias, and 10 (59%) were at low risk of selective outcome reporting (eTable in the Supplement).
Outcomes of Acupuncture and Acupressure
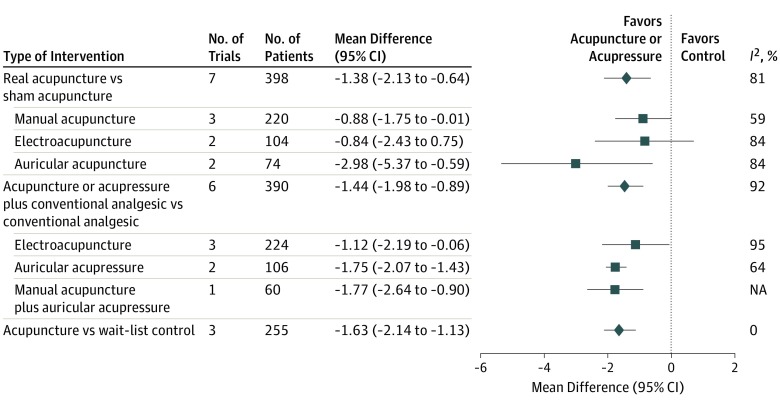
With regard to pain intensity (Figure 2), pooled results from 7 blinded studies showed the association between pain reduction and real acupuncture rather than between pain reduction and sham acupuncture with substantial heterogeneity (mean difference, −1.38 points; 95% CI, −2.13 to −0.64; I2 = 81%). Data from the 6 open-label RCTs showed the reduction in pain intensity was associated with a combination of acupuncture and acupressure when compared with analgesic therapy with considerable heterogeneity (mean difference, −1.44 points; 95% CI, −1.98 to −0.89; I2 = 92%). Significant reduction without heterogeneity was found in 3 studies that compared acupuncture with wait-list controls (mean difference, −1.63 points; 95% CI, −2.14 to −1.13) (Figure 2). Two open-label studies49,54 reported the maintenance dose of analgesics during the trial, and the pooled results showed a significant decrease in analgesic dose in the integrative medicine group (acupuncture plus analgesic therapy) compared with the control group that received analgesics alone (mean difference, −30.00 mg morphine equivalent daily dose; 95% CI, −37.5 mg to −22.5 mg), without heterogeneity.
Figure 2. Forest Plot of the Estimated Association of Acupuncture and Acupressure With Cancer Pain Intensity.
The squares show the results of each subgroup analysis, and the diamond indicates the pooled effect size of all subgroups. NA indicates not applicable.
In the subgroup analyses for intervention type (Figure 2), the pooled result of sham-controlled RCTs favored manual acupuncture (3 studies) with reduced heterogeneity (mean difference, −0.88 points; 95% CI, −1.75 to −0.01; I2 = 59%) and auricular acupuncture (2 studies) with increased effect size (mean difference, −2.98 points; 95% CI, −5.37 to −0.59; I2 = 84%). By pooling the 2 open-label studies on acupressure, the effect size increased with reduced heterogeneity (mean difference, −1.75 points; 95% CI, −2.07 to −1.43; I2 = 64%) (Figure 2).
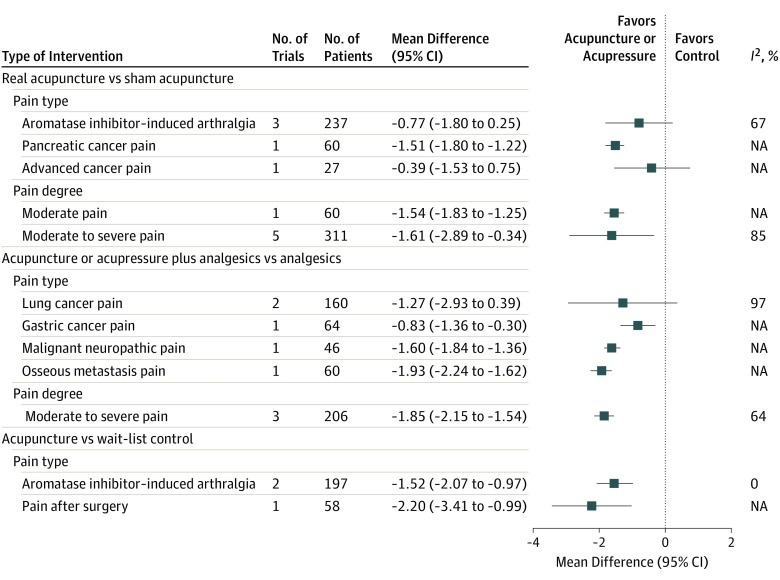
In the sensitivity analyses for pain type (Figure 3), the effect sizes significantly increased for the 5 blinded trials in which pain was rated as moderate to severe with substantial heterogeneity (mean difference, −1.61 points; 95% CI, −2.89 to −0.34; I2 = 85%). In the 3 open-label studies, the effect size also increased with reduced heterogeneity (mean difference, −1.85 points; 95% CI, −2.15 to −1.54; I2 = 64%) (Figure 3).
Figure 3. Forest Plot of the Subgroup Analyses of the Association of Acupuncture and Acupressure With Different Cancer Pain Intensity.
NA indicates not applicable.
Safety of Acupuncture and Acupressure and Overall Evidence
The adverse events reported were minor, did not require medical evaluation or any specific intervention, and consisted predominantly of skin and subcutaneous tissue disorder or slight pain from the application of treatment to the skin. Six RCTs reported no adverse events during the study period. In all of the trials included, no dropouts were attributed to adverse effects associated with acupuncture treatment. Evidence from RCTs indicated with a moderate level of certainty that real acupuncture was associated with reduced pain intensity as compared with sham acupuncture or wait-list controls. Moderate-quality evidence also suggested that acupuncture and acupressure were associated with reduced analgesic use.
Discussion
The systematic review included 17 RCTs involving 1111 patients with cancer, whereas the meta-analysis included 14 RCTs with 920 patients. Evidence was found of an association between real acupuncture and greater reduction in pain intensity, with a moderate level of certainty. Acupuncture may also be associated with reduced opioid use when added to analgesic therapy. Relatively few adverse events from acupuncture were reported, an observation consistent with findings in previous studies and reviews.63,64 The present study provides an updated synthesis of the current evidence of acupuncture and acupressure for cancer pain and identifies research gaps that remain to be addressed.
Consistent with findings of past systematic reviews and meta-analyses, acupuncture was associated with significant reductions in cancer pain in open-label studies.23,27 However, the present meta-analysis found acupuncture to be associated with greater pain reduction compared with sham control, which differs from findings of the previous reviews.23,27,31 This difference may be owing to the inclusion of recent high-quality trials.41,48 In addition, we applied more stringent inclusion criteria to ensure the quality of source RCTs. Considerable effort was made to conduct an extensive literature search. Seven of the 17 studies were conducted in China, 6 in the United States, and 1 study each in Australia, Brazil, France, and Korea.
The positive results from sham-controlled RCTs suggest the potential efficacy of acupuncture in reducing cancer pain, as sham acupuncture helps prevent bias in evaluating the specific outcome of acupuncture needling.65 Evidence from open-label studies revealed the increased risk of bias from nonblinding. However, in recent years, nonblinded pragmatic trials have been recommended for achieving clinically relevant results because of their emphasis on the practical applicability and extrapolation in real-world situations (increased external validity) over treatment efficacy.66 This design is particularly appropriate for researching complex and flexible interventions, such as acupuncture.66,67,68 It has also been suggested that pragmatic trials can provide more informative evidence for developing clinical guidelines for acupuncture.69 Nevertheless, a gap remains between acupuncture research and its flexible application in clinical practice.
From a clinical perspective, available evidence focuses on acupuncture as 1 component of pain management. Heterogeneity in the results suggests that the outcomes of acupuncture may be variable; thus, it may not be suitable as a stand-alone therapy for cancer pain. However, meta-analyses have reported reductions in various types of pain70,71 and opioid use after surgical procedures.72 A recent study from Italy reported the advantages of acupuncture for cancer-related symptoms in a palliative setting.73 However, few trials were available for certain types of pain (eg, neuropathic, osseous metastasis); thus, further research is needed to investigate the association of acupuncture with specific pain syndromes.74,75
How to integrate acupuncture into pain and symptom management plans for patients with cancer remains a challenge. With the move to patient-centered care76 and personalized medicine in cancer therapy,77 oncological practice and palliative care services need to provide information about treatment options and ways to access them, which can include evidence-based nonpharmacological approaches.78 Given that pain is a common reason that patients with cancer visit emergency departments, often followed by hospital admission,79 hospitals need to establish appropriate acupuncture services. With the growing evidence of the efficacy of acupuncture, most National Cancer Institute–designated comprehensive cancer centers have begun offering acupuncture.80 However, the cost of treatments and exclusion from insurance coverage were identified as major barriers to using acupuncture. A recent survey found that 47.9% of patients with cancer were willing to undergo acupuncture if treatments were covered by insurance.81 Therefore, systematic insurance coverage is needed to allow equitable access to acupuncture as part of comprehensive cancer pain management.
Limitations
This study has several limitations. Substantial heterogeneity was observed and contributed to lowering the evidence grade from high to moderate. Sensitivity analyses were attempted through subgroup analyses, which showed reduced heterogeneity (Figures 2 and 3) for manual acupuncture and moderate to severe pain. Because cancer pain is highly complex, the type of pain, cancer treatment (eg, surgical procedure, chemotherapy, and hormone therapy as well as phase of care such as active treatment, survivorship, and palliative care), and acupuncture method are likely factors in the variability of estimates. More research in specific areas is needed to fully assess how these factors play a role in heterogeneity. Among the open-label studies, high risk of bias existed owing to lack of blinding. In most of these studies, baseline analgesic use was not specified, and in 2 studies, participants did not use analgesic therapy at baseline.50,51 Consequently, variations in analgesic type and dose among participants within each study and between studies also likely contributed to heterogeneity. Because of the limited number of trials included for each comparison in the meta-analysis, funnel plots were not feasible. Therefore, we could not fully evaluate publication bias.
Conclusions
The findings of this systematic review and meta-analysis suggest that, based on moderate-level evidence, acupuncture and/or acupressure may be associated with significant reductions in pain intensity and opioid use.
eTable. Characteristics of Trials Included in the Analysis and Summary of Trial Quality Assessment
References
- 1.Neufeld NJ, Elnahal SM, Alvarez RH. Cancer pain: a review of epidemiology, clinical quality and value impact. Future Oncol. 2017;13(9):833-841. doi: 10.2217/fon-2016-0423 [DOI] [PubMed] [Google Scholar]
- 2.van den Beuken-van Everdingen MH, Hochstenbach LM, Joosten EA, Tjan-Heijnen VC, Janssen DJ. Update on prevalence of pain in patients with cancer: systematic review and meta-analysis. J Pain Symptom Manage. 2016;51(6):1070-1090.e9. doi: 10.1016/j.jpainsymman.2015.12.340 [DOI] [PubMed] [Google Scholar]
- 3.Carlson CL. Effectiveness of the World Health Organization cancer pain relief guidelines: an integrative review. J Pain Res. 2016;9:515-534. doi: 10.2147/JPR.S97759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Simone CB II, Vapiwala N, Hampshire MK, Metz JM. Cancer patient attitudes toward analgesic usage and pain intervention. Clin J Pain. 2012;28(2):157-162. doi: 10.1097/AJP.0b013e318223be30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim YC, Ahn JS, Calimag MM, et al. ; ACHEON Working Group . Current practices in cancer pain management in Asia: a survey of patients and physicians across 10 countries. Cancer Med. 2015;4(8):1196-1204. doi: 10.1002/cam4.471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kwon JH. Overcoming barriers in cancer pain management. J Clin Oncol. 2014;32(16):1727-1733. doi: 10.1200/JCO.2013.52.4827 [DOI] [PubMed] [Google Scholar]
- 7.Pachman DR, Barton DL, Swetz KM, Loprinzi CL. Troublesome symptoms in cancer survivors: fatigue, insomnia, neuropathy, and pain. J Clin Oncol. 2012;30(30):3687-3696. doi: 10.1200/JCO.2012.41.7238 [DOI] [PubMed] [Google Scholar]
- 8.Vowles KE, McEntee ML, Julnes PS, Frohe T, Ney JP, van der Goes DN. Rates of opioid misuse, abuse, and addiction in chronic pain: a systematic review and data synthesis. Pain. 2015;156(4):569-576. doi: 10.1097/01.j.pain.0000460357.01998.f1 [DOI] [PubMed] [Google Scholar]
- 9.Miller M, Barber CW, Leatherman S, et al. . Prescription opioid duration of action and the risk of unintentional overdose among patients receiving opioid therapy. JAMA Intern Med. 2015;175(4):608-615. doi: 10.1001/jamainternmed.2014.8071 [DOI] [PubMed] [Google Scholar]
- 10.Sharfstein JM, Olsen Y. Lessons learned from the opioid epidemic [published online August 5, 2019]. JAMA. 2019;322(9):809-810. doi: 10.1001/jama.2019.9794 [DOI] [PubMed] [Google Scholar]
- 11.Chua IS, Leiter RE, Brizzi KT, et al. . US national trends in opioid-related hospitalizations among patients with cancer. JAMA Oncol. 2019;5(5):734-735. doi: 10.1001/jamaoncol.2019.0042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tick H, Nielsen A, Pelletier KR, et al. ; Pain Task Force of the Academic Consortium for Integrative Medicine and Health . Evidence-based nonpharmacologic strategies for comprehensive pain care: the Consortium Pain Task Force white paper. Explore (NY). 2018;14(3):177-211. doi: 10.1016/j.explore.2018.02.001 [DOI] [PubMed] [Google Scholar]
- 13.Clark SD, Bauer BA, Vitek S, Cutshall SM. Effect of integrative medicine services on pain for hospitalized patients at an academic health center. Explore (NY). 2019;15(1):61-64. doi: 10.1016/j.explore.2018.07.006 [DOI] [PubMed] [Google Scholar]
- 14.Miller KR, Patel JN, Symanowski JT, Edelen CA, Walsh D. Acupuncture for cancer pain and symptom management in a palliative medicine clinic. Am J Hosp Palliat Care. 2019;36(4):326-332. doi: 10.1177/1049909118804464 [DOI] [PubMed] [Google Scholar]
- 15.Swarm R, Anghelescu DL, Benedetti C, et al. ; National Comprehensive Cancer Network (NCCN) . Adult cancer pain. J Natl Compr Canc Netw. 2007;5(8):726-751. [PubMed] [Google Scholar]
- 16.National Comprehensive Cancer Network NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines). Adult Cancer Pain. Version 1. https://www.nccn.org/professionals/default.aspx. Published January 22, 2018. Accessed June 10, 2018.
- 17.Zia FZ, Olaku O, Bao T, et al. . The National Cancer Institute’s Conference on Acupuncture for Symptom Management in Oncology: state of the science, evidence, and research gaps. J Natl Cancer Inst Monogr. 2017;2017(52):lgx005. doi: 10.1093/jncimonographs/lgx005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bae K, Yoo HS, Lamoury G, Boyle F, Rosenthal DS, Oh B. Acupuncture for aromatase inhibitor-induced arthralgia: a systematic review. Integr Cancer Ther. 2015;14(6):496-502. doi: 10.1177/1534735415596573 [DOI] [PubMed] [Google Scholar]
- 19.Bardia A, Barton DL, Prokop LJ, Bauer BA, Moynihan TJ. Efficacy of complementary and alternative medicine therapies in relieving cancer pain: a systematic review. J Clin Oncol. 2006;24(34):5457-5464. doi: 10.1200/JCO.2006.08.3725 [DOI] [PubMed] [Google Scholar]
- 20.Chao LF, Zhang AL, Liu HE, Cheng MH, Lam HB, Lo SK. The efficacy of acupoint stimulation for the management of therapy-related adverse events in patients with breast cancer: a systematic review. Breast Cancer Res Treat. 2009;118(2):255-267. doi: 10.1007/s10549-009-0533-8 [DOI] [PubMed] [Google Scholar]
- 21.Chen L, Lin CC, Huang TW, et al. . Effect of acupuncture on aromatase inhibitor-induced arthralgia in patients with breast cancer: a meta-analysis of randomized controlled trials. Breast. 2017;33:132-138. doi: 10.1016/j.breast.2017.03.015 [DOI] [PubMed] [Google Scholar]
- 22.Chien TJ, Liu CY, Chang YF, Fang CJ, Hsu CH. Acupuncture for treating aromatase inhibitor-related arthralgia in breast cancer: a systematic review and meta-analysis. J Altern Complement Med. 2015;21(5):251-260. doi: 10.1089/acm.2014.0083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chiu HY, Hsieh YJ, Tsai PS. Systematic review and meta-analysis of acupuncture to reduce cancer-related pain. Eur J Cancer Care (Engl). 2017;26(2):e12457. doi: 10.1111/ecc.12457 [DOI] [PubMed] [Google Scholar]
- 24.Choi TY, Lee MS, Kim TH, Zaslawski C, Ernst E. Acupuncture for the treatment of cancer pain: a systematic review of randomised clinical trials. Support Care Cancer. 2012;20(6):1147-1158. doi: 10.1007/s00520-012-1432-9 [DOI] [PubMed] [Google Scholar]
- 25.Dos Santos S, Hill N, Morgan A, Smith J, Thai C, Cheifetz O. Acupuncture for treating common side effects associated with breast cancer treatment: a systematic review. Med Acupunct. 2010;22(2):81-97. doi: 10.1089/acu.2009.0730 [DOI] [Google Scholar]
- 26.Garcia MK, McQuade J, Haddad R, et al. . Systematic review of acupuncture in cancer care: a synthesis of the evidence. J Clin Oncol. 2013;31(7):952-960. doi: 10.1200/JCO.2012.43.5818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hu C, Zhang H, Wu W, et al. . Acupuncture for pain management in cancer: a systematic review and meta-analysis. Evid Based Complement Alternat Med. 2016;2016:1720239. doi: 10.1155/2016/1720239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lau CH, Wu X, Chung VC, et al. . Acupuncture and related therapies for symptom management in palliative cancer care: systematic review and meta-analysis. Medicine (Baltimore). 2016;95(9):e2901. doi: 10.1097/MD.0000000000002901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lee H, Schmidt K, Ernst E. Acupuncture for the relief of cancer-related pain—a systematic review. Eur J Pain. 2005;9(4):437-444. doi: 10.1016/j.ejpain.2004.10.004 [DOI] [PubMed] [Google Scholar]
- 30.Lee PL, Tam KW, Yeh ML, Wu WW. Acupoint stimulation, massage therapy and expressive writing for breast cancer: a systematic review and meta-analysis of randomized controlled trials. Complement Ther Med. 2016;27:87-101. doi: 10.1016/j.ctim.2016.06.003 [DOI] [PubMed] [Google Scholar]
- 31.Li H. A Systematic Review of Randomized Controlled Trials of Acupuncture Treatment for Cancer Pain [master's thesis]. Harbin, China: Heilongjiang University Of Chinese Medicine; 2016. [Google Scholar]
- 32.Lian WL, Pan MQ, Zhou DH, Zhang ZJ. Effectiveness of acupuncture for palliative care in cancer patients: a systematic review. Chin J Integr Med. 2014;20(2):136-147. doi: 10.1007/s11655-013-1439-1 [DOI] [PubMed] [Google Scholar]
- 33.Paley CA, Johnson MI, Tashani OA, Bagnall AM. Acupuncture for cancer pain in adults. Cochrane Database Syst Rev. 2015;(10):CD007753. doi: 10.1002/14651858.7753.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pan CX, Morrison RS, Ness J, Fugh-Berman A, Leipzig RM. Complementary and alternative medicine in the management of pain, dyspnea, and nausea and vomiting near the end of life: a systematic review. J Pain Symptom Manage. 2000;20(5):374-387. doi: 10.1016/S0885-3924(00)00190-1 [DOI] [PubMed] [Google Scholar]
- 35.Peng H, Peng HD, Xu L, Lao LX. Efficacy of acupuncture in treatment of cancer pain: a systematic review [in Chinese]. Zhong Xi Yi Jie He Xue Bao. 2010;8(6):501-509. doi: 10.3736/jcim20100601 [DOI] [PubMed] [Google Scholar]
- 36.Robb KA, Bennett MI, Johnson MI, Simpson KJ, Oxberry SG. Transcutaneous electric nerve stimulation (TENS) for cancer pain in adults. Cochrane Database Syst Rev. 2008;(3):CD006276. doi: 10.1002/14651858.CD006276.pub2 [DOI] [PubMed] [Google Scholar]
- 37.Tao WW, Jiang H, Tao XM, Jiang P, Sha LY, Sun XC. Effects of acupuncture, tuina, tai chi, qigong, and traditional Chinese medicine five-element music therapy on symptom management and quality of life for cancer patients: a meta-analysis. J Pain Symptom Manage. 2016;51(4):728-747. doi: 10.1016/j.jpainsymman.2015.11.027 [DOI] [PubMed] [Google Scholar]
- 38.Yang GS, Kim HJ, Griffith KA, Zhu S, Dorsey SG, Renn CL. Interventions for the treatment of aromatase inhibitor-associated arthralgia in breast cancer survivors: a systematic review and meta-analysis. Cancer Nurs. 2017;40(4):E26-E41. doi: 10.1097/NCC.0000000000000409 [DOI] [PubMed] [Google Scholar]
- 39.Zheng Y, Yu YH, Fang FF. Meta-analysis on wrist-ankle acupuncture of cancerous pain [in Chinese]. Liaoning Zhongyiyao Daxue Xuebao. 2014;16:152-155. [Google Scholar]
- 40.Zhou J, Liang Y, Chen Q, Fang JQ. Meta-analysis on randomized controlled clinical trials of auricular acupuncture on cancer pain [in Chinese]. Zhonghua Zhongyiyao Xuekan. 2014;10:2326-2330. [Google Scholar]
- 41.Hershman DL, Unger JM, Greenlee H, et al. . Effect of acupuncture vs sham acupuncture or waitlist control on joint pain related to aromatase inhibitors among women with early-stage breast cancer: a randomized clinical trial. JAMA. 2018;320(2):167-176. doi: 10.1001/jama.2018.8907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mao JJ, Farrar JT. Acupuncture for aromatase inhibitor–related joint pain among breast cancer patients. JAMA. 2018;320(21):2269-2270. doi: 10.1001/jama.2018.16736 [DOI] [PubMed] [Google Scholar]
- 43.He Y, Liu Y, May BH, et al. . Effectiveness of acupuncture for cancer pain: protocol for an umbrella review and meta-analyses of controlled trials. BMJ Open. 2017;7(12):e018494. doi: 10.1136/bmjopen-2017-018494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Higgins JPT, Altman DG. Assessing risk of bias in included studies In: Higgins JPT, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions. Chichester, UK: John Wiley & Sons; 2008:chap 8. doi: 10.1002/9780470712184.ch8 [DOI] [Google Scholar]
- 45.Fainsinger RL, Fairchild A, Nekolaichuk C, Lawlor P, Lowe S, Hanson J. Is pain intensity a predictor of the complexity of cancer pain management? J Clin Oncol. 2009;27(4):585-590. doi: 10.1200/JCO.2008.17.1660 [DOI] [PubMed] [Google Scholar]
- 46.Hjermstad MJ, Fayers PM, Haugen DF, et al. ; European Palliative Care Research Collaborative (EPCRC) . Studies comparing numerical rating scales, verbal rating scales, and visual analogue scales for assessment of pain intensity in adults: a systematic literature review. J Pain Symptom Manage. 2011;41(6):1073-1093. doi: 10.1016/j.jpainsymman.2010.08.016 [DOI] [PubMed] [Google Scholar]
- 47.Ruela LO, Iunes DH, Nogueira DA, Stefanello J, Gradim CVC. Effectiveness of auricular acupuncture in the treatment of cancer pain: randomized clinical trial [article in English, Portuguese, Spanish; abstract available in Portuguese and Spanish from the publisher]. Rev Esc Enferm USP. 2018;52:e03402.doi: 10.1590/S1980-220X2017040503402 [DOI] [PubMed] [Google Scholar]
- 48.Kim K, Lee S. Intradermal acupuncture along with analgesics for pain control in advanced cancer cases: a pilot, randomized, patient-assessor-blinded, controlled trial. Integr Cancer Ther. 2018;17(4):1137-1143. doi: 10.1177/1534735418786797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wang Y, Wang XY, Wang H, Zhang Y, Fang H. Clinical study of electro-acupuncture combined with hydroxycodone sustained-release tablets for cancer pain in advanced non-small cell lung cancer. Zhejiang J Tradit Chin Med. 2017;9:684-685. doi: 10.13633/j.cnki.zjtcm.2017.09.039 [DOI] [Google Scholar]
- 50.Shen LF, Chen WY, Luv XD, et al. . Effects of electro-acupuncture on improving sleep quality for patients with lung cancer pain. J Med Res. 2016;(06):87-90. doi: 10.11969/j.issn.1673-548X.2016.06.022 [DOI] [Google Scholar]
- 51.Wang J, Lu DR, Bi R, Shu XN. Clinical observation on 30 cases of moderate and severe cancer pain of bone metastasis treated by auricular acupressure. Yunnan J Tradit Chin Med Materia Medica. 2015;02:43-45. [Google Scholar]
- 52.Guo ZB, Guo GH, Yang JP, Shao Y. Effects of acupuncture on pain and quality of life for patients with advanced gastric cancer. International journal of traditional. Int J Chin Med. 2015;37(4):371-373. doi: 10.3760/cma.j.issn.1673-4246.2015.04.023 [DOI] [Google Scholar]
- 53.Mao JJ, Xie SX, Farrar JT, et al. . A randomised trial of electro-acupuncture for arthralgia related to aromatase inhibitor use. Eur J Cancer. 2014;50(2):267-276. doi: 10.1016/j.ejca.2013.09.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zhu LN, Wang RL, Zong H, Fan QX. Effects of auricular acupressure combined with oxycontin for malignant neuropathic pain. Chin J Physic Med Rehabil. 2013;35(7):579-581. doi: 10.3760/cma.j.issn.0254-1424.2013.07.020 [DOI] [Google Scholar]
- 55.Oh B, Kimble B, Costa DS, et al. . Acupuncture for treatment of arthralgia secondary to aromatase inhibitor therapy in women with early breast cancer: pilot study. Acupunct Med. 2013;31(3):264-271. doi: 10.1136/acupmed-2012-010309 [DOI] [PubMed] [Google Scholar]
- 56.Chen H, Liu TY, Kuai L, Zhu J, Wu CJ, Liu LM. Electroacupuncture treatment for pancreatic cancer pain: a randomized controlled trial. Pancreatology. 2013;13(6):594-597. doi: 10.1016/j.pan.2013.10.007 [DOI] [PubMed] [Google Scholar]
- 57.Bao T, Cai L, Giles JT, et al. . A dual-center randomized controlled double blind trial assessing the effect of acupuncture in reducing musculoskeletal symptoms in breast cancer patients taking aromatase inhibitors. Breast Cancer Res Treat. 2013;138(1):167-174. doi: 10.1007/s10549-013-2427-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Jiang KR. Clinical Research on Acupuncture on Siguan Points Combined with Auricular Acupressure for Cancer Pain [doctoral thesis]. Guangzhou, China: Guangzhou University of Chinese Medicine; 2011. [Google Scholar]
- 59.Pfister DG, Cassileth BR, Deng GE, et al. . Acupuncture for pain and dysfunction after neck dissection: results of a randomized controlled trial. J Clin Oncol. 2010;28(15):2565-2570. doi: 10.1200/JCO.2009.26.9860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Crew KD, Capodice JL, Greenlee H, et al. . Randomized, blinded, sham-controlled trial of acupuncture for the management of aromatase inhibitor-associated joint symptoms in women with early-stage breast cancer. J Clin Oncol. 2010;28(7):1154-1160. doi: 10.1200/JCO.2009.23.4708 [DOI] [PubMed] [Google Scholar]
- 61.Crew KD, Capodice JL, Greenlee H, et al. . Pilot study of acupuncture for the treatment of joint symptoms related to adjuvant aromatase inhibitor therapy in postmenopausal breast cancer patients. J Cancer Surviv. 2007;1(4):283-291. doi: 10.1007/s11764-007-0034-x [DOI] [PubMed] [Google Scholar]
- 62.Alimi D, Rubino C, Pichard-Léandri E, Fermand-Brulé S, Dubreuil-Lemaire ML, Hill C. Analgesic effect of auricular acupuncture for cancer pain: a randomized, blinded, controlled trial. J Clin Oncol. 2003;21(22):4120-4126. doi: 10.1200/JCO.2003.09.011 [DOI] [PubMed] [Google Scholar]
- 63.MacPherson H, Thomas K, Walters S, Fitter M. The York acupuncture safety study: prospective survey of 34 000 treatments by traditional acupuncturists. BMJ. 2001;323(7311):486-487. doi: 10.1136/bmj.323.7311.486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Chan MWC, Wu XY, Wu JCY, Wong SYS, Chung VCH. Safety of acupuncture: overview of systematic reviews. Sci Rep. 2017;7(1):3369. doi: 10.1038/s41598-017-03272-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Briggs JP, Shurtleff D. Acupuncture and the complex connections between the mind and the body. JAMA. 2017;317(24):2489-2490. doi: 10.1001/jama.2017.7214 [DOI] [PubMed] [Google Scholar]
- 66.Sox HC, Lewis RJ. Pragmatic trials: practical answers to “real world” questions. JAMA. 2016;316(11):1205-1206. doi: 10.1001/jama.2016.11409 [DOI] [PubMed] [Google Scholar]
- 67.Ford I, Norrie J. Pragmatic trials. N Engl J Med. 2016;375(5):454-463. doi: 10.1056/NEJMra1510059 [DOI] [PubMed] [Google Scholar]
- 68.Chalkidou K, Tunis S, Whicher D, Fowler R, Zwarenstein M. The role for pragmatic randomized controlled trials (pRCTs) in comparative effectiveness research. Clin Trials. 2012;9(4):436-446. doi: 10.1177/1740774512450097 [DOI] [PubMed] [Google Scholar]
- 69.Kaptchuk TJ, Chen KJ, Song J. Recent clinical trials of acupuncture in the West: responses from the practitioners. Chin J Integr Med. 2010;16(3):197-203. doi: 10.1007/s11655-010-0197-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Vickers AJ, Linde K. Acupuncture for chronic pain. JAMA. 2014;311(9):955-956. doi: 10.1001/jama.2013.285478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Fan AY, Miller DW, Bolash B, et al. . Acupuncture’s role in solving the opioid epidemic: evidence, cost-effectiveness, and care availability for acupuncture as a primary, non-pharmacologic method for pain relief and management—white paper 2017. J Integr Med. 2017;15(6):411-425. doi: 10.1016/S2095-4964(17)60378-9 [DOI] [PubMed] [Google Scholar]
- 72.Tedesco D, Gori D, Desai KR, et al. . Drug-free interventions to reduce pain or opioid consumption after total knee arthroplasty: a systematic review and meta-analysis. JAMA Surg. 2017;152(10):e172872. doi: 10.1001/jamasurg.2017.2872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Franco C, Bernardini S, Ferreri R. Acupuncture in palliative care. OBM Integrative Complementary Med. 2019;4(1):1. doi: 10.21926/obm.icm.1901006 [DOI] [Google Scholar]
- 74.Portenoy RK. Treatment of cancer pain. Lancet. 2011;377(9784):2236-2247. doi: 10.1016/S0140-6736(11)60236-5 [DOI] [PubMed] [Google Scholar]
- 75.Krajnik M, Zylicz Z. Pain assessment, recognising clinical patterns, and cancer pain syndromes In: Hanna M, Zylicz ZB, eds. Cancer Pain. London, UK: Springer London; 2013:95-108. doi: 10.1007/978-0-85729-230-8_7 [DOI] [Google Scholar]
- 76.MacLeod J, Wolff E, McAllister A, Mao JJ, Garland SN. Including the patient voice in patient-centered outcomes research in integrative oncology. J Natl Cancer Inst Monogr. 2017;2017(52):46-47. doi: 10.1093/jncimonographs/lgx008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Hui D, Park M, Shamieh O, et al. . Personalized symptom goals and response in patients with advanced cancer. Cancer. 2016;122(11):1774-1781. doi: 10.1002/cncr.29970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ben-Arye E, Samuels N. Patient-centered care in lung cancer: exploring the next milestones. Transl Lung Cancer Res. 2015;4(5):630-634. doi: 10.3978/j.issn.2218-6751.2015.03.07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Elsayem AF, Elzubeir HE, Brock PA, Todd KH. Integrating palliative care in oncologic emergency departments: challenges and opportunities. World J Clin Oncol. 2016;7(2):227-233. doi: 10.5306/wjco.v7.i2.227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Yun H, Sun L, Mao JJ. Growth of integrative medicine at leading cancer centers between 2009 and 2016: a systematic analysis of NCI-designated comprehensive cancer center websites. J Natl Cancer Inst Monogr. 2017;2017(52):29-32. doi: 10.1093/jncimonographs/lgx004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Liou KT, Hung TKW, Meghani SH, et al. . What if acupuncture were covered by insurance for pain management? a cross-sectional study of cancer patients at one academic center and 11 community hospitals. Pain Med. 2019;20(10):2060-2068. doi: 10.1093/pm/pnz087 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Characteristics of Trials Included in the Analysis and Summary of Trial Quality Assessment