Abstract
This study uses China’s National Maternal and Child Health Statistics data set to characterize trends in cesarean delivery rates overall and by urban and rural areas in China between 2008 and 2018.
Inappropriate cesarean delivery rates pose a risk to the health of women and infants. In 2014, the cesarean delivery rate in China was 34.9%, with geographic variation ranging from greater than 60% in some supercities to less than 10% in some rural areas.1
During the past decade, China has implemented many local, regional, and national efforts to decrease cesarean delivery rates.1,2,3,4 It also has continued to improve health services in rural areas.
We assessed trends in cesarean delivery rates between 2008 and 2018, highlighting differences between urban and rural areas.
Methods
The National Maternal and Child Health Statistics data set was used, consisting of county-level data on maternal and child health and use of health services. Detailed information about the data set and procedures for data collection are described elsewhere.1 The analysis was limited to live births among residents and was disaggregated by degree of urbanization using the same definitions as previously published: supercity (urban areas with a population of ≥5 million), general city (urban areas with a population of <5 million), and rural areas (nonurban counties).1
For analysis of these aggregated data, the Peking University institutional review board waived review. To model trends, we used Joinpoint software version 4.7 (National Cancer Institute), which required input of 12 years of data for some analyses. For those, we estimated values for 2007 using linear extrapolation. For descriptive analyses, we used SPSS version 20.0 (IBM). We used 2-tailed tests and a significance level of P < .05.
Results
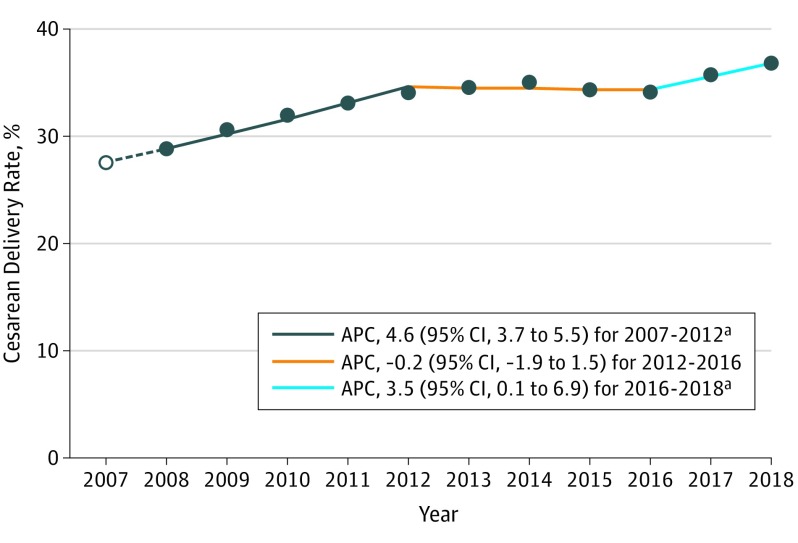
There were 160 278 075 births between 2008 and 2018. Cesarean delivery rates increased from 28.8% (3 788 029 of 13 160 634 live births) in 2008 to 34.9% (5 280 124 of 15 123 276 live births) in 2014, and in 2018 reached 36.7% (4 997 685 of 13 608 933 live births). The annual percentage change (APC) in cesarean delivery rates was 1.8 (95% CI, 1.2-2.5) between 2008 and 2018. The joinpoint analysis revealed 3 distinct segments: an initial period of growth (APC, 4.6 [95% CI, 3.7-5.5] for 2007-2012), a plateau period (APC, −0.2 [95% CI, −1.9 to 1.5] for 2012-2016), and a period of renewed growth (APC, 3.5 [95% CI, 0.1-6.9] for 2016-2018) (Figure 1).
Figure 1. Trends in Cesarean Delivery Rates in China, 2008-2018.
The solid circles indicate annual cesarean delivery rates from China’s National Maternal and Child Health Statistics data set. The open circle indicates an estimate for 2007 based on linear extrapolation. Joinpoint regression was used to estimate the overall annual percentage change (APC) for 2008 to 2018 (1.8 [95% CI, 1.2-2.5]; P < .001). Joinpoint regression also identified 3 segments using the additional extrapolated point for 2007. The superimposed trend lines show the 3 segments identified by joinpoint regression.
aP < .05.
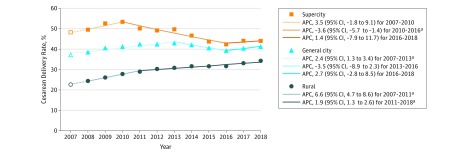
During the study period, 7.8% of births occurred in supercities, 20.5% in general cities, and 71.7% in rural areas. Cesarean delivery rates in rural areas were consistently lower than in the cities and each had different net trends: the cesarean delivery rates consistently increased in rural areas, the rates in general cities showed no net change, and the rates in supercities showed a net decrease (Figure 2).
Figure 2. Trends in Cesarean Delivery Rates in China by Type of Geographical Area, 2008-2018.
Supercities were defined as urban areas with a population of 5 million or greater, general cities as urban areas with a population of less than 5 million, and rural areas as nonurban counties. Solid data markers indicate annual cesarean delivery rates for each type of geographical area from China’s National Maternal and Child Health Statistics data set. The open data markers indicate estimates for 2007 based on linear extrapolation. Joinpoint regression was used to estimate the overall annual percentage change (APC) for 2008 to 2018 for each type of geographic area: supercity, −2.1 (95% CI, −2.9 to −1.3; P < .001); general city, 0 (95% CI, −0.7 to 0.8; P = .95); and rural area, 2.9 (95% CI, 2.1-3.6; P < .001). Pairwise comparisons of these changes for each of the 3 types of geographical areas rejected the null hypothesis of parallelism in each case at P < .001. Joinpoint regression also was used to identify up to 3 segments and relied on the additional extrapolated point for 2007. Three segments were identified for supercities and general cities and 2 for rural areas. The superimposed trend lines show the segments.
aP < .05.
Urban-rural differences decreased over time. The differences between supercities and rural areas in the cesarean delivery rates decreased by 62% from a difference of 25.1 percentage points (95% CI, 24.9-25.2 percentage points) in 2008 (49.4% in supercities and 24.3% in rural areas) to 9.6 percentage points (95% CI, 9.5-9.7 percentage points) in 2018 (43.8% in supercities and 34.2% in rural areas).
Discussion
The previously reported increase in cesarean delivery rates in China between 2008 and 2014 extended through 2018. Although rates plateaued between 2012 and 2016, they increased from 2016 to 2018. During the study period, cesarean delivery rates decreased in some cities, but increased in rural areas, where most of the nation’s births occur.
Factors that might have contributed to the plateau include initiatives to decrease cesarean delivery rates, such as the national Baby Friendly Hospital program from 2014 to 2016.2,3 The increase in cesarean delivery rates at the end of the study period might be attributed to improved rural health services, the end of the Baby Friendly Hospital program, or the effect of the 2016 2-child policy with increases among women who had previously had cesarean deliveries and among older women.5,6
An observational study recently reported that cesarean delivery rates were decreasing in China based on an analysis of data from 2012 to 2016.4 However, the study disproportionately sampled urban hospitals and ended before the increase captured in this study.
The analysis is limited by the use of crude rates without adjustment for need or appropriateness and potential changes in maternal characteristics like parity. In addition, factors that underlie the reported trends were not investigated.
Section Editor: Jody W. Zylke, MD, Deputy Editor.
References
- 1.Li HT, Luo S, Trasande L, et al. Geographic variations and temporal trends in cesarean delivery rates in China, 2008-2014. JAMA. 2017;317(1):69-76. doi: 10.1001/jama.2016.18663 [DOI] [PubMed] [Google Scholar]
- 2.National Health Commission of China Notice on carrying out the reassessment of the Baby Friendly Hospitals [in Chinese]. http://www.nhc.gov.cn/fys/s3585/201406/556c0b7673e8470f9641c28d119a9f31.shtml. Accessed August 1, 2019.
- 3.National Health Commission of China The name list of Baby Friendly Hospitals in China [in Chinese]. http://www.nhc.gov.cn/fys/s7906/201511/e5650712dbcd449e9d2e01129a698b9c.shtml. Accessed August 1, 2019.
- 4.Liang J, Mu Y, Li X, et al. Relaxation of the one child policy and trends in caesarean section rates and birth outcomes in China between 2012 and 2016: observational study of nearly seven million health facility births. BMJ. 2018;360:k817. doi: 10.1136/bmj.k817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li HT, Xue M, Hellerstein S, et al. Association of China’s universal two child policy with changes in births and birth related health factors: national, descriptive comparative study. BMJ. 2019;366:l4680. doi: 10.1136/bmj.l4680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Health Commission of China Progress report on maternal and child health in China [in Chinese]. http://www.nhc.gov.cn/fys/s7901/201905/bbd8e2134a7e47958c5c9ef032e1dfa2.shtml. Accessed August 1, 2019.