Key Points
Question
Is rocuronium noninferior to succinylcholine with regard to first-attempt endotracheal intubation success among patients undergoing rapid sequence intubation in an out-of-hospital emergency setting?
Findings
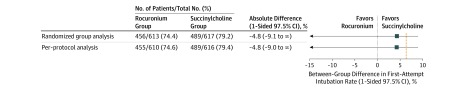
In this randomized clinical trial that included 1248 patients, the number of patients with successful first-attempt intubation was 455 of 610 (74.6%) in the rocuronium group vs 489 of 616 (79.4%) in the succinylcholine group, a difference of −4.8% (1-sided 97.5% CI, −9% to ∞), which did not meet criteria for noninferiority.
Meaning
The study findings failed to demonstrate noninferiority of rocuronium compared with succinylcholine with regard to first-attempt endotracheal intubation success rate.
Abstract
Importance
Rocuronium and succinylcholine are often used for rapid sequence intubation, although the comparative efficacy of these paralytic agents for achieving successful intubation in an emergency setting has not been evaluated in clinical trials. Succinylcholine use has been associated with several adverse events not reported with rocuronium.
Objective
To assess the noninferiority of rocuronium vs succinylcholine for tracheal intubation in out-of-hospital emergency situations.
Design, Setting and Participants
Multicenter, single-blind, noninferiority randomized clinical trial comparing rocuronium (1.2 mg/kg) with succinylcholine (1 mg/kg) for rapid sequence intubation in 1248 adult patients needing out-of-hospital tracheal intubation. Enrollment occurred from January 2014 to August 2016 in 17 French out-of-hospital emergency medical units. The date of final follow-up was August 31, 2016.
Interventions
Patients were randomly assigned to undergo tracheal intubation facilitated by rocuronium (n = 624) or succinylcholine (n = 624).
Main Outcomes and Measures
The primary outcome was the intubation success rate on first attempt. A noninferiority margin of 7% was chosen. A per-protocol analysis was prespecified as the primary analysis.
Results
Among 1248 patients who were randomized (mean age, 56 years; 501 [40.1%] women), 1230 (98.6%) completed the trial and 1226 (98.2%) were included in the per-protocol analysis. The number of patients with successful first-attempt intubation was 455 of 610 (74.6%) in the rocuronium group vs 489 of 616 (79.4%) in the succinylcholine group, with a between-group difference of −4.8% (1-sided 97.5% CI, −9% to ∞), which did not meet criteria for noninferiority. The most common intubation-related adverse events were hypoxemia (55 of 610 patients [9.0%]) and hypotension (39 of 610 patients [6.4%]) in the rocuronium group and hypoxemia (61 of 616 [9.9%]) and hypotension (62 of 616 patients [10.1%]) in the succinylcholine group.
Conclusions and Relevance
Among patients undergoing endotracheal intubation in an out-of-hospital emergency setting, rocuronium, compared with succinylcholine, failed to demonstrate noninferiority with regard to first-attempt intubation success rate.
Trial Registration
ClinicalTrials.gov Identifier: NCT02000674
This noninferiority trial compares the effect of rocuronium vs succinylcholine on first-attempt tracheal intubation success rate in out-of-hospital emergency situations among patients undergoing rapid sequence intubation.
Introduction
Tracheal intubation is one of the most critical interventions in emergency settings.1 Several clinical studies have reported that sedation greatly improves ease and safety of this emergency procedure.2,3 Rapid sequence intubation (RSI) is therefore the most widely recommended sedation technique for patients requiring emergency tracheal intubation.4 RSI involves administration of rapid-onset drugs, including a hypnotic and a paralytic agent. Use of a neuromuscular blocking agent improves the overall intubating conditions and first-attempt intubation success rate, regardless of the choice of induction agent.5,6 Succinylcholine has traditionally been the preferred neuromuscular blocking agent, except when contraindicated.7 Rocuronium, introduced more recently for use in emergency situations, has been proposed as a good alternative to succinylcholine because of its pharmacokinetic characteristics. When used at a dose of 1.2 mg/kg, rocuronium has a similar onset time to succinylcholine.8 Because succinylcholine has several clinical contraindications and rocuronium has no contraindications (except for hypersensitivity to the agent), debate about the paralytic agent of choice for RSI has persisted for several years. Moreover, succinylcholine use has been associated with several adverse events not reported with rocuronium, including hyperkalemia and increase in oxygen consumption leading to rapid desaturation.9,10
Numerous reviews have concluded that succinylcholine provides better intubating conditions than rocuronium, but other observational studies have reported that when rocuronium is used at a dose higher than 1 mg/kg, intubation is as successful as with succinylcholine.11,12,13 Consequently, surveys have reported a marked increase in rocuronium use in emergency settings.11,14 To our knowledge, no randomized study has compared these paralytic agents in emergency settings.15
Given these conflicting results and the lack of high-quality evidence, a randomized clinical trial was conducted to compare rocuronium vs succinylcholine use in emergency out-of-hospital intubation situations. It was hypothesized that rocuronium would be noninferior to succinylcholine for facilitating tracheal intubation.
Methods
Study Design
The Succinylcholine vs Rocuronium for Out-of-Hospital Emergency Intubation (CURASMUR) trial was a nationwide, single-blind, randomized, noninferiority clinical trial conducted from January 2014 through August 2016 at 17 out-of-hospital emergency medical units in France. The study patients were blinded to intervention assignment, but the physicians conducting the intubation procedures were not blinded. The Comité de Protection des Personnes Sud-Ouest et Outre-Mer ethics committee approved the trial protocol (ref 2013-001438-16), which is available in Supplement 1. Patients undergoing out-of-hospital emergency intubation are most often not able to provide informed consent. In accordance with French laws on emergency medical research, if a patient's relative was present when the medical team had to intubate, written consent from the relative of the patient to be included in the clinical study was required. If no relatives were present at the time of intubation, an information letter offering the opportunity to provide consent or to opt out of inclusion in the study was systematically sent to the patient if he or she survived and left the hospital or to a relative if the patient died at the hospital. Additional information on the methods for obtaining consent is available in Supplement 2.
The emergency medical service system in France is a centrally based, 2-tiered system. The first level is composed of basic life support fire department ambulances based at fire stations. The second level comprises advanced life support physician-staffed ambulances. These mobile intensive care units are distributed throughout each region. The physician-staffed ambulances have a minimum team of a trained ambulance driver, a nurse (or a nurse anesthesiologist), a senior physician specializing in either emergency medicine (in more than 90% of cases) or anesthesiology, and, sometimes, a medical student on board. All physicians have at least 2 years of practice and are emergency physicians or anesthesiologists. Tracheal intubation is only performed by advanced life support units.
Patient Population
Patients were recruited between January 2014 and August 2016. The study included all consecutive out-of-hospital adult patients requiring emergency tracheal intubation as assessed by the emergency physician. Patients with all conditions (trauma, dyspnea, coma, overdoses, and shock), except cardiac arrest, were included. Patients who met any of the following criteria were excluded from the study: younger than 18 years; pregnant women; contraindication to rocuronium (known allergy to rocuronium), succinylcholine (personal or family history of known malignant hyperthermia, known allergy to succinylcholine, congenital muscular dystrophy, myasthenia, specific hyperkalemia, recent open eye surgery, known congenital deficit in plasma pseudocholinesterases), or sugammadex (the selective paralytic binding agent for rocuronium reversal); under guardianship; and no health insurance.
Randomization
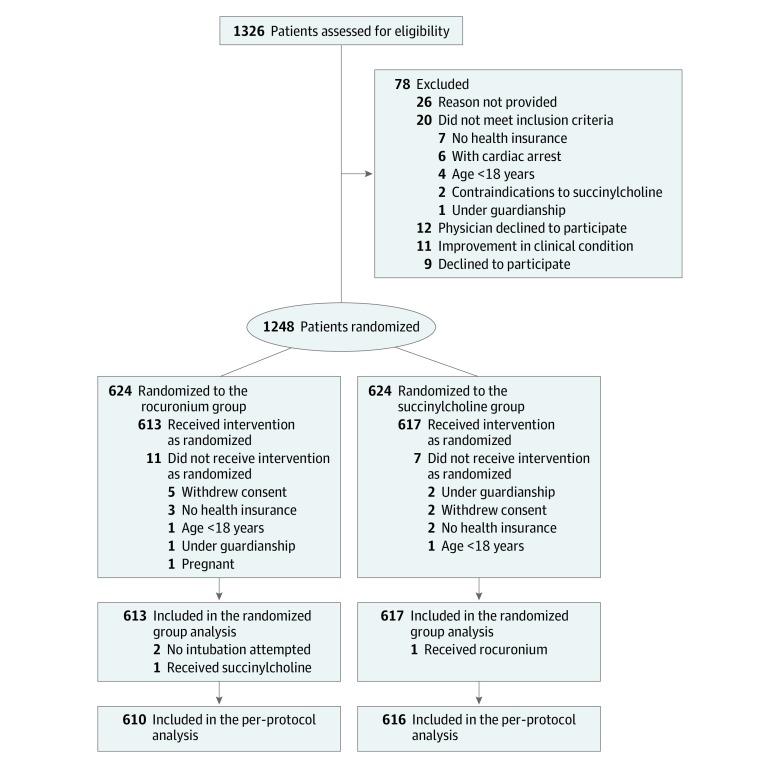
Patients were randomized in a 1:1 ratio to the rocuronium or the succinylcholine group (Figure 1). A statistician at the methodological unit of the La Réunion University Hospital Center, not involved in patient recruitment, generated randomization sequences. The sequences were generated using the PROC PLAN procedure from SAS, version 9.4 (SAS Institute). Balanced and stratified by center, randomization lists were generated using randomly permuted blocks of 4, 6, and 8 patients. Numbered and sealed opaque envelopes were then generated from those lists and used by emergency physicians in each ambulance to assign patients to the rocuronium or succinylcholine group. The emergency physicians conducting the intubation procedures were blinded to the contents of the envelope at the time of assigning an individual patient.
Figure 1. Flow of Participants in CURASMUR, a Study of the Effect of Rocuronium vs Succinylcholine on Endotracheal Intubation Success Rate Among Patients Undergoing Out-of-Hospital Intubation.
Study Intervention
In both groups, sedation induction was performed after preoxygenation. Emergency physicians were asked to follow the French guidelines for sedation and analgesia in emergency departments.4 Two hypnotics were recommended. Etomidate (0.3 mg/kg) or ketamine (2 mg/kg), with dosage based on estimated patient weight, was injected followed immediately by an intravenous bolus injection of either succinylcholine (1 mg/kg) or rocuronium (1.2 mg/kg), with dosage based on estimated patient weight. The use of another hypnotic (propofol or thiopenthal) was allowed, according to the physician's preference. The Sellick maneuver was recommended but optional, according to the physician's preference. It was recommended to perform intubation 60 seconds after administration of the paralytic agent. Single-use Macintosh metallic laryngoscope blades (size 3 and 4) were used. The standard intubation procedure did not include use of a stylet; stylet use was considered an alternative airway procedure. When standard laryngoscopy-assisted intubation was not possible, an alternative procedure was recommended in accordance with the French Society of Anesthesia and Resuscitation guidelines on difficult airway management, including gum elastic bougie, intubating laryngeal mask airway (ILMA), or cricothyrotomy.16 If the patient was randomized to the rocuronium group, the physician could subsequently choose to antagonize the action of the rocuronium with sugammadex, a procedure recommended for patients impossible to intubate under direct laryngoscopy and who could neither be intubated nor ventilated by alternative techniques for difficult intubation. These airway practices were in accordance with the French Society of Anesthesia and Resuscitation consensus guidelines on difficult airway management.16
Aside from the randomization for paralytic agent used for the induction of sedation, there was no change from usual practices. In particular, hypotension was managed via fluid resuscitation with crystalloids and ephedrine and prolonged hypotension was managed with continuous catecholamine administration. Maintenance sedation after intubation was performed according to the French Society of Anesthesia and Resuscitation recommendations and included administration of benzodiazepine or propofol and opioids. Doses of these agents were adapted by the physician to the patient's clinical status and the objectives of sedation, which vary according to the pathology and the indication for mechanical ventilation.
Each physician completed a paper case report form on-site. Later, to ensure the quality and completeness of the study data, a clinical research associate at each center verified the case report form data from the source medical file on-site and recorded the data to a centralized database. Patients were followed up until hospital admission.
Outcomes
The primary outcome measure was the percentage of patients with successful first-attempt orotracheal intubation assessed by the physician and confirmed by a capnography curve consistent over 3 respiratory cycles. A noninferiority margin of 7% was selected.
Secondary prespecified outcomes were (1) the Cormack-Lehane grade of glottis visibility obtained by direct laryngoscopy (range, 1-4; 1 indicates full view of glottis; 2, partial view of glottis; 3, only epiglottis seen; and 4, neither glottis nor epiglottis seen)17; (2) the overall difficulty of the intubation process, measured by the Intubation Difficulty Scale score (range, 0 to infinite; score >5 indicates difficult intubation)18; (3) intubation conditions, assessed by the Copenhagen score (poor, good, or excellent conditions)19; (4) the percentage of patients intubated by alternative techniques (stylet, gum elastic bougie, ILMA [eg, Fastrach], or cricothyrotomy); and (5) intubation-related complications in the first 15 minutes after intubation (cardiac arrest, arterial hypotension [systolic blood pressure <90 mm Hg], hypoxemia [occurrence of new oxygen desaturation <90%], physician-reported aspiration, severe arrhythmia [ventricular tachycardia, ventricular fibrillation], or allergic reaction).
Post hoc exploratory outcomes were the number of intubation attempts, the number of intubation failures under direct laryngoscopy, the time of out-of-hospital care, the number of deaths during out-of-hospital care, the number of unintentional extubations, and the amount of sedative drugs and vasopressors used after intubation.
Sample Size
The sample size was calculated from the previous literature, with an expected percentage of successful first-attempt orotracheal intubation of 75% for patients in the succinylcholine group.3,20,21 After assuming a noninferiority margin of 7% based on out-of-hospital studies that focused on emergency intubation using the same main outcome, with a type I error of 5% and type II error of 20%, it was determined that 602 patients were needed in each group (1204 overall).20,21,22,23 We set targeted enrollment at 1300 patients to take into account risks of protocol deviations in this emergency randomization context. Thus, we planned to include 650 patients in each group.
Statistical Analysis
Characteristics at baseline were described by their frequency and percentages for categorical variables and by means and SDs or medians and interquartile ranges for quantitative variables. To take the randomization stratification factor (ie, the center) into account, a generalized estimating equations model with an identity link function was used to compare the groups for the percentage of patients with a successful first-attempt orotracheal intubation. Therefore, the center was included as the clustering factor and an exchangeable correlation matrix was specified. Based on this model, noninferiority was assessed for the primary outcome by the 1-sided 97.5% CI of the absolute difference. As recommended for noninferiority studies, a per-protocol analysis was conducted first.24,25 Patients who received allocated treatment and for whom intubation was attempted were included in this analysis. An additional analysis was conducted that analyzed patients according to their randomized group and included all patients who were randomized and completed the trial.
In an exploratory post hoc analysis, we performed 2 subgroup analyses to investigate the treatment effect of the primary outcome based on patients’ conditions; 1 analysis was stratified on reason for intubation and the other on patient position at the time of intubation. Analyses included treatment × subgroup interaction and the subgroup as covariates in a generalized estimating equations model defined for analyses of the primary outcome. The absolute difference between treatment groups and 1-sided 97.5% CIs were then estimated from these models.
We compared secondary outcomes using generalized estimating equations models with an identity link function. To take into account potential nonindependence of patients in the same center, the center was included as the clustering factor and an exchangeable correlation matrix was specified. Absolute differences and their 2-sided 95% CIs were derived from these models. All tests for secondary outcomes were performed at a 2-tailed type I error of 5%, with a superiority hypothesis. Because of the potential for type I error due to multiple comparisons, findings for analyses of secondary end points should be interpreted as exploratory.
The amount of missing data in this study was low. Analyses were performed on complete cases and no assumptions were made for the patterns of missing data. All analyses were performed used SAS version 9.4 (SAS Institute). The statistical analysis plan is available in Supplement 3.
Results
Baseline Characteristics
A total of 1248 patients were enrolled in the study. Patients were recruited between January 2014 and August 2016, with final follow-up on August 31, 2016. Of the 1326 patients assessed for eligibility, 1248 were randomized (mean age, 56 years; 501 [40.1%] women). Of the randomized patients, 1230 (98.6%) completed the trial and 1226 (98.2%) were included in the per-protocol analysis (Figure 1). Patient characteristics and clinical indications for intubation are reported in Table 1 and eFigure in Supplement 2 (74 patients with missing data). Coma was the leading reason for intubation.
Table 1. Baseline Patient Data in a Study of the Effect of Rocuronium vs Succinylcholine on Out-of-Hospital Endotracheal Intubation Success.
| Characteristic | No. (%) | |
|---|---|---|
| Rocuronium (n = 610) | Succinylcholine (n = 616) | |
| Age, mean (SD), y | 57.2 (18.7) | 54.6 (19.1) |
| Sex | ||
| Men | 370 (60.7) | 366 (59.3) |
| Women | 240 (39.3) | 250 (40.7) |
| BMI, mean (SD) | 25.5 (5.4) | 25.8 (5.1) |
| Medical history | ||
| Hypertension | 208 (35.9) (n = 580) | 178 (30.1) (n = 592) |
| Smoking | 151 (26.4) (n = 572) | 127 (21.9) (n = 580) |
| Alcoholism | 112 (19.4) (n = 576) | 107 (18.2) (n = 589) |
| Cancer | 55 (9.4) (n = 582) | 42 (7.1) (n = 593) |
| Coronary heart disease | 51 (8.8) (n = 580) | 42 (7.1) (n = 592) |
| Chronic obstructive pulmonary disease | 50 (8.6) (n = 578) | 34 (5.7) (n = 592) |
| Heart failure | 50 (8.6) (n = 579) | 29 (4.9) (n = 591) |
| Chronic kidney failure | 19 (3.3) (n = 580) | 20 (3.4) (n = 591) |
| Reason for intubationa | ||
| Coma due to neurological disease | 313 (51.3) | 304 (49.4) |
| Coma due to self-poisoning | 107 (17.5) | 124 (20.1) |
| Acute respiratory failure | 101 (16.6) | 71 (11.5) |
| Trauma | 51 (8.4) | 52 (8.4) |
| Shock | 8 (1.3) | 9 (1.5) |
| Other | 30 (4.9) | 56 (9.1) |
| Characteristics at enrollment | ||
| Glasgow Coma Scale score, median (IQR)b | 6.0 (3.0-8.0) | 6.0 (3.0-8.0) |
| Heart rate, mean (SD), beats/min | 99.4 (28.4) | 95.6 (27.2) |
| Respiratory rate, mean (SD), breaths/min | 21.4 (9.7) | 21.1 (9.5) |
| Arterial systolic pressure, mm Hg | ||
| <90 | 47 (7.7) | 37 (6.0) |
| >140 | 258 (42.3) | 227 (36.9) |
| Arterial diastolic pressure, mm Hg | ||
| <50 | 43 (7.0) | 35 (5.7) |
| >90 | 193 (31.6) | 168 (27.3) |
| Peripheral oxygen saturation, mean (SD), % | 95.4 (6.8) | 95.4 (7.5) |
| Sedation given for intubation | ||
| Etomidate | 536 (87.9) | 543 (88.1) |
| Total dose, median (IQR), mg | 30 (20-40) | 30 (20-40) |
| Ketamine | 38 (6.2) (n = 609) | 34 (5.5) |
| Total dose, median (IQR), mg | 150 (67-190) | 200 (125-250) |
| Pentothal | 21 (3.4) (n = 609) | 19 (3.1) (n = 615) |
| Total dose, median (IQR), mg | 350 (200-400) | 325 (250-400) |
| Propofol | 21 (3.4) | 21 (3.4) |
| Total dose, median (IQR), mg | 60 (40-150) | 150 (80-160) |
| Combined administration, No. | 6 | 1 |
| Patient position during intubation | ||
| Lying on a stretcher | 324 (53.1) | 307 (49.8) |
| Lying on the ground | 161 (26.4) | 187 (30.4) |
| Lying on a bed | 112 (18.4) | 110 (17.9) |
| Other | 13 (2.1) | 12 (1.9) |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); IQR, interquartile range.
Coded by the emergency physician.
Range, 3 (deep coma) to 15 (normal consciousness).
Primary Outcome
The number of patients with successful first-attempt intubation was 455 of 610 (74.6%) in the rocuronium group vs 489 of 616 (79.4%) in the succinylcholine group, a difference of −4.8% (1-sided 97.5% CI, −9% to ∞), which did not meet criteria for noninferiority (margin of 7%; Figure 2). Additional analysis of patients according to their randomized group that included all patients who were randomized and completed the trial is presented in the eTable 1 in Supplement 2. Subgroup analyses for the primary outcome are reported in eTable 2 in Supplement 2.
Figure 2. Difference in Successful First-Attempt Intubation Rate Between Patients Given Rocuronium vs Succinylcholine While Undergoing Out-of-Hospital Rapid Sequence Intubation .
The dashed line represents the noninferiority margin of 7%. Because the CI lines go above the prespecified noninferiority margin of 7%, the null hypothesis that succinylcholine is superior cannot be rejected.
Secondary Outcomes
Among the secondary end points assessing tracheal intubation difficulty, there was no statistically significant between-group difference for the mean (SD) Intubation Difficulty Scale score (4.2 [2.9] for the rocuronium group vs 4.1 [2.4] for the succinylcholine group; difference, 0.1 [95% CI, −0.2 to 0.4]). There was also no statistically significant difference in the Copenhagen score between the groups; 327 of 580 (56.4%) patients in the rocuronium group vs 313 of 584 (53.6%) in the succinylcholine group had excellent intubation conditions (difference, 2.8 [95% CI, −0.5 to 6.4]) and 206 of 580 (35.5%) patients in the rocuronium group vs 222 of 584 (38.0%) in the succinylcholine group had good intubation conditions (difference, −2.5 [95% CI, −6.1 to 0.5]).
There was no significant difference between the 2 groups in the use of alternative intubation techniques, such as stylet or gum elastic bougie, although significantly more patients in the rocuronium group had use of the ILMA, and 1 patient in the succinylcholine group underwent cricothyrotomy. Intubation-related complications reported within 15 minutes after intubation were observed more frequently in patients in the succinylcholine group than the rocuronium group (143 of 616 [23.2%] vs 111 of 610 [18.2%]; absolute difference, −5% [95% CI, −9.8% to −0.03%]; P = .04; Table 2).
Table 2. Intubation Characteristics and Outcomes of Patients in a Study of the Effect of Rocuronium vs Succinylcholine on Out-of-Hospital Endotracheal Intubation Success.
| No./Total No. (%) | Absolute Difference (95% CI), %a | P Valueb | ||
|---|---|---|---|---|
| Rocuronium Group | Succinylcholine Group | |||
| Primary Outcome (Successful First-Attempt Intubation) | ||||
| Per-protocol analysis | 455/610 (74.6) | 489/616 (79.4) | −4.8 (1-sided 97.5% CI, −9.0 to ∞)c | |
| Randomized group analysis | 456/613 (74.4) | 489/617 (79.2) | −4.8 (1-sided 97.5% CI, −9.1 to ∞)c | |
| Secondary Outcomes | ||||
| Prespecified analyses | ||||
| Cormack-Lehane graded | ||||
| I (best view) | 375/609 (61.6) | 346/616 (56.2) | 5.4 (−0.3 to 10.9) | .06 |
| II | 125/609 (20.5) | 173/616 (28.1) | −7.6 (−11.5 to −3.7) | <.001 |
| III | 81/609 (13.3) | 72/616 (11.7) | 1.6 (−2.9 to 6.2) | .49 |
| IV (worst view) | 28/609 (4.6) | 25/616 (4.0) | 0.6 (−1.5 to 2.6) | .60 |
| Intubation Difficulty Scale score, mean (SD)e | 4.2 (2.9) | 4.1 (2.4) | 0.1 (−0.2 to 0.4) | .52 |
| Intubation Difficulty Scale score >5 | 138/605 (22.8) | 130/614 (21.2) | 1.6 (−3.5 to 6.8) | .53 |
| Copenhagen score (reflecting intubation conditions)f | ||||
| Excellent | 327/580 (56.4) | 313/584 (53.6) | 2.8 (−0.5 to 6.4) | .09 |
| Good | 206/580 (35.5) | 222/584 (38.0) | −2.5 (−6.1 to 0.5) | .10 |
| Poor | 47/580 (8.1) | 49/584 (8.4) | −0.3 (−3.0 to 2.6) | .87 |
| Need for alternative intubation techniques | ||||
| Stylet | 55/610 (9.0) | 51/616 (8.3) | 0.7 (−1.9 to 2.0) | .97 |
| Gum elastic bougie | 114/610 (18.7) | 107/616 (17.4) | 1.3 (−1.2 to 3.8) | .31 |
| Intubating laryngeal mask airway | 10/610 (1.6) | 2/616 (0.3) | 1.3 (0.5 to 2.4) | .003 |
| Cricothyrotomy | 0/610 (0.0) | 1/616 (0.2) | −0.2 (−0.5 to 0.2) | |
| Early intubation-related complications | .04 | |||
| Patients with at least 1 complication | 111/610 (18.2) | 143/616 (23.2) | −5 (−9.8 to −0.03) | |
| Hypoxemia episodesg | 55/610 (9.0) | 61/616 (9.9) | −0.9 (−4.4 to 2.6) | |
| Severe arrhythmiah | 12/610 (2.0) | 26/616 (4.2) | −2.2 (−3.8 to −0.7) | |
| Cardiac arrest | 22/609 (3.6) | 13/615 (2.1) | 1.5 (−0.1 to 3.3) | |
| Pulmonary aspirationi | 19/610 (3.1) | 21/616 (3.4) | −0.3 (−1.7 to 1.1) | |
| Hypotension episodesj | 39/610 (6.4) | 62/615 (10.1) | −3.7 (−6.8 to −0.3) | |
| Exploratory analysesk | ||||
| No. of intubation attempts, mean (SD) | 1.4 (0.8) | 1.3 (0.6) | 0.1 (0.05 − 0.2) | <.001 |
| 2 | 110/609 (18.1) | 96/615 (15.6) | 2.5 (−2.2 to 6.9) | .31 |
| 3 | 34/609 (5.6) | 27/615 (4.4) | 1.2 (−0.8 to 3.2) | .23 |
| ≥4 | 10/609 (1.6) | 3/615 (0.5) | 1.1 (0.2 to 2.0) | .01 |
| Intubation failure under direct laryngoscopy | 11/610 (1.8) | 4/616 (0.7) | 1.1 (0.3 − 2.3) | .01 |
| Time of prehospital care, median (IQR), min | 55 (38 to 78) | 55 (39 to 80) | −2.2 (−6.9 to 2.5) | .35 |
| Death during prehospital care | 6/608 (1.0) | 3/615 (0.5) | 0.5 (−0.4 to 1.3) | .26 |
| Complications | ||||
| No. of complications per patient, median (IQR) | 0 | 0 | −0.09 (−0.17 to −0.08) | .03 |
| ≥1 severe complication | 115/608 (18.9) | 150/615 (24.4) | −5.5 (−10.8 to −0.05) | .04 |
| Unintentional extubation | 1/609 (0.2) | 4/615 (0.6) | 0.4 (−1.0 to 0.03) | .06 |
Abbreviation: IQR, interquartile range.
The estimated difference between the groups was calculated with a 2-sided 95% CI using a generalized estimated equation model, in which center was specified as the clustering factor.
Not corrected for multiple comparisons.
The estimated difference between the groups was calculated with a 1-sided 97.5% CI using a generalized estimated equation model, in which center was specified as the clustering factor. The margin for noninferiority was set at −7%. A lower bound of the CI that did not exceed this margin indicated noninferiority.
Reflects glottis visualization. Range, 1-4; higher scores indicate less glottis visualization.
Range, 0 (intubation without difficulty) to infinity; a value greater than 5 indicates difficult intubation.
The Copenhagen score is composed of 5 items with responses coded as “excellent,” “good,” or “poor”: laryngoscopy (easy, fair, difficult), vocal cords position (abducted, intermediate, closed), vocal cords movement (none, moving, closing), movements of the tube during insertion (none, slight, vigorous), and coughing during tracheal tube insertion (none, diaphragm, sustained); intubation conditions are defined as excellent if all items are excellent, good if all items are excellent or good, and poor if a single item is poor.
Defined as any oxygen saturation reading of less than 90%.
Ventricular tachycardia and ventricular fibrillation.
Visually detected by the physician during laryngoscopy.
Defined as a new episode of arterial systolic pressure of less than 90 mm Hg.
Post hoc outcomes.
Post Hoc Exploratory Outcomes
Significantly more intubation attempts were required in the rocuronium group than in the succinylcholine group (Table 2). Six patients in the rocuronium group and 3 in the succinylcholine group died during out-of-hospital care. No deaths were attributed to difficult intubation. In the succinylcholine group, 100 of 606 (16.5%) patients were treated with norepinephrine during the immediate postintubation period, compared with 60 of 604 (9.9%) in the rocuronium group (difference, −6.6% [95% CI, −10.8% to −1.9%]; P < .001; Table 3). Fifteen patients could not be intubated under direct laryngoscopy in the out-of-hospital care period. Among them, 6 were intubated blindly through a laryngeal intubation mask. Six more were effectively ventilated by ILMA and were intubated at the hospital. One patient had a cricothyrotomy and 2 patients were ventilated with a face mask until arrival at the hospital (Table 2). Eleven of these 15 patients were assigned to receive rocuronium. Two patients received sugammadex to antagonize rocuronium. Airway control was obtained for 1 of these 2 patients by application of the recommended algorithm; an intubating laryngeal mask was put in place and enabled effective mechanical ventilation until arrival at the hospital. For the second patient, sugammadex was injected after only 1 intubation attempt failure under direct laryngoscopy, without attempting any alternative technique. That is, this physician did not follow the recommended algorithm for difficult intubation for this patient. The patient awoke 45 minutes later, and the final diagnosis was status epilepticus.
Table 3. Sedative and Vasopressor Use During the Postintubation Period in a Study of the Effect of Rocuronium vs Succinylcholine on Out-of-Hospital Endotracheal Intubation Success.
| Drug | No. Who Received Some of the Agent/No. With Available Data (%) | Absolute Difference (95% CI), %a,b | |
|---|---|---|---|
| Rocuronium (n = 610) | Succinylcholine (n = 616) | ||
| Hypnotics | |||
| Midazolam | 521/610 (85.4) | 546/616 (88.6) | −3.2 (−5.9 to 0.4) |
| Total dose, median (IQR), mgc | 5.0 (4.0 to 10.0) | 8.0 (5.0 to 13.0) | −3.0 (−4.3 to −2.3) |
| No. of boluses, mean (SD) | 1.3 (0.7) | 1.5 (0.9) | −0.2 (−0.3 to −0.02) |
| Propofol | 34/608 (5.6) | 40/613 (6.5) | −0.9 (−2.5 to 0.2) |
| Total dose, median (IQR), mgc | 133.0 (50.0 to 200.0) | 200.0 (100.0 to 250.0) | −52.3 (−98.9 to −6.0) |
| No. of boluses, mean (SD) | 1.0 (1.0) | 1.5 (1.4) | −0.5 (−1.1 to 0.04) |
| Analgesics | |||
| Fentanyl | 50/610 (8.2) | 48/614 (7.8) | 0.4 (−0.1 to 1.8) |
| Total dose, median (IQR), μgc | 100.0 (50.0 to 200.0) | 100.0 (67.5 to 200.0) | −13.5 (−59.2 to 32.4) |
| No. of boluses, mean (SD) | 0.9 (0.8) | 1.4 (1.0) | −0.3 (−0.4 to −0.2) |
| Sufentanyl | 491/610 (80.5) | 513/616 (83.3) | −2.8 (−6.3 to 0.7) |
| Total dose, median (IQR), μgc | 15.0 (10.0 to 25.0) | 20.0 (10.0 to 34.0) | −8.0 (−12.0 to −4.0) |
| No. of boluses, mean (SD) | 1.2 (0.5) | 1.5 (0.8) | −0.3 (−0.4 to −0.2) |
| Vasopressors | |||
| Epinephrine | 26/605 (4.3) | 26/605 (4.3) | 0.0 (−4.1 to 4.1) |
| Norepinephrine | 60/604 (9.9) | 100/606 (16.5) | − 6.6 (−10.8 to −1.9) |
| Dopamine | 1/604 (0.2) | 0/605 (0.0) | 0.2 (−0.2 to 0.5) |
| ≥1 vasopressor | 77/604 (12.7) | 121/608 (19.9) | −7.2 (−11.0 to −2.8) |
Abbreviation: IQR, interquartile range.
The estimated difference between the groups was calculated with a 2-sided 95% CI using a generalized estimated equation model, in which center was specified as the clustering factor.
Not corrected for multiple comparisons.
Calculated only from patients who received the agent.
Discussion
This randomized clinical trial failed to demonstrate noninferiority for the success rate of rocuronium compared with succinylcholine for first-attempt intubation in adult patients receiving emergency intubation at a noninferiority margin of 7%.
To our knowledge, this study is the first randomized clinical trial comparing rocuronium and succinylcholine in emergency settings, even though reports indicate that emergency physicians are adopting rocuronium as a standard practice, with some departments using this drug more often than succinylcholine.26,27 Most of the published trials comparing these neuromuscular-blocking agents have examined operating room settings.28,29 To our knowledge only 1 randomized trial has examined the intensive care setting, and none have examined emergency departments or out-of-hospital settings.30 Accordingly, the systematic reviews of this comparison essentially analyze operating room studies only.12,29,31
For many years, succinylcholine has been the principal paralytic agent recommended for facilitating tracheal intubation in patients needing out-of-hospital tracheal intubation. One of the main characteristics of succinylcholine is its very quick onset, which enables optimal intubation conditions to be obtained in less than a minute after intravenous administration. Rocuronium, a nondepolarizing paralytic agent, has pharmacokinetic characteristics that provide optimal intubation conditions in almost the same time as succinylcholine, as long as the dose administered is at least 1 mg/kg. For this reason, it has been proposed as an alternative paralytic agent when RSI is indicated.32
The primary end point chosen for this trial was the first-attempt intubation success rate. This criterion is often used in clinical studies assessing tracheal intubation in the emergency setting context because several studies of emergency intubations report that the complication rate related to airway control increases with the number of intubation attempts.33,34,35,36 It appears to be a more relevant and direct criterion than intubation condition, measured by scores that take into account many elements that may be difficult to accurately assess in the emergency context, which was assessed here only as a secondary outcome and did not differ significantly between the groups. Nonetheless, none of the published meta-analyses that compared succinylcholine with rocuronium used this primary end point. Instead, all used intubation conditions considered to be good or excellent as their primary outcome.
Design of a noninferiority study seemed necessary because succinylcholine has a tolerance profile that appears to be lower than that of rocuronium. The choice of a margin of noninferiority is a major element when performing a noninferiority study. For this study, determination of this value was not straightforward because very little data have been published on this topic. No randomized trials have been conducted in an emergency setting to compare succinylcholine and rocuronium. All randomized trials were conducted in a hospital setting, primarily in the operating room, and the primary end point of these trials was the intubation conditions assessment and not the first-attempt intubation success rate. Some observational studies conducted in an emergency situation compared the first-attempt intubation rate between patients who did vs patients who did not receive a paralytic agent, such as succinylcholine. The difference in first-attempt intubation rate varies in these observational studies between 20% and 17%, in favor of succinylcholine use.20,23 Therefore, in the present study the standard comparator was succinylcholine and the new agent was rocuronium. As suggested for noninferiority trials, the margin of noninferiority was set to less than half of the difference previously reported for the first-attempt intubation rate, depending on whether succinylcholine was used.25
While the results of the primary outcome analysis showed that rocuronium cannot be considered noninferior to succinylcholine in terms of ease of intubation, fewer complications were observed with rocuronium. These results must be interpreted cautiously. Cardiovascular complications, such as hypotension or cardiac arrhythmia, were more frequent after succinylcholine use. However, it should be noted that more deaths were recorded during the prehospital period of care in the rocuronium group, although this difference was not statistically significant. Nearly all patients in both groups received postintubation sedation, usually a hypnotic agent (generally midazolam) and an opioid analgesic (most commonly sufentanil). The total doses of opioids and midazolam administered were greater in the succinylcholine group, which might have contributed to the higher frequency of hemodynamic disorders in that group. Continuous sedation began as soon as tracheal intubation was in place. The total dose of hypnotic administered during the out-of-hospital period differed between the groups because of more frequent bolus administration of sedative agents in the succinylcholine group. It appears likely that in patients with frequent hemodynamic instability, using a longer-acting paralytic agent might reduce the likelihood of the patient fighting the ventilator, which may lead emergency physicians to administer a bolus of midazolam or an opioid to avoid adverse respiratory events.37
Limitations
This study has several limitations. First, this trial was not double-blinded, and the physician might have been influenced by knowledge of which drug was administered. In emergency situations, it would have been extremely difficult to mask the fasciculations observed in more than 90% of individuals who receive succinylcholine. Moreover, the time between the injection of the paralytic agent and the first tracheal intubation attempt was not recorded. It is possible that patients in the rocuronium group might have been intubated before the recommended 60-second delay with incomplete paralysis, whereas the fasciculations most often indicated to physicians the effectiveness of paralysis after succinylcholine administration before the intubation attempt.
Second, these results were obtained in a specific physician-staffed out-of-hospital emergency medical system and may not be generalizable to a paramedical-based care system. Third, awareness phenomena was not evaluated. Nevertheless, all patients were sedated according to recommendations, most often with a combination of an opioid and a benzodiazepine. Fourth, only the early intubation-related complications during the out-of-hospital period were collected and later hospital complications were not evaluated. Fifth, although a recommended dose of 1 mg/kg of succinylcholine was used, a higher dose may have been given to patients, as suggested by some clinical studies that have reported higher intubation success rates with administration of 1.5 mg/kg of succinylcholine.38
Sixth, because patients were intubated without use of a stylet or video laryngoscope and with only Macintosh metallic blades, this limits the generalization of the results to other out-of-hospital systems where these practices are widespread. Seventh, the number of intubations performed per year and per physician and the number of years of practice for each physician who participated in this study were not reported. Eighth, the sample size calculation was carried out starting from a hypothesis of a first-attempt intubation success rate of 75% with succinylcholine, whereas in the present study, a success rate close to 80% was observed in the succinylcholine group. Ninth, the noninferiority margin of 7% that was selected was based in part on an expert opinion, which can be considered as a methodological limitation.
Conclusions
Among patients undergoing endotracheal intubation in a medical-based out-of-hospital emergency care system, rocuronium, compared with succinylcholine, failed to demonstrate noninferiority with regard to first-attempt intubation success rate.
Trial protocol
eMethods. Process for obtaining consent
eTable 1. ITT analysis
eTable2. Subgroup analyses for the primary outcome
eFigure1. Randomized patients age distribution
Statistical analysis plan
Data sharing statement
References
- 1.Jabre P, Avenel A, Combes X, et al. Morbidity related to emergency endotracheal intubation—a substudy of the KETAmine SEDation trial. Resuscitation. 2011;82(5):517-522. doi: 10.1016/j.resuscitation.2011.01.015 [DOI] [PubMed] [Google Scholar]
- 2.Adnet F, Minadeo JP, Finot MA, et al. A survey of sedation protocols used for emergency endotracheal intubation in poisoned patients in the French prehospital medical system. Eur J Emerg Med. 1998;5(4):415-419. [PubMed] [Google Scholar]
- 3.Combes X, Jabre P, Jbeili C, et al. Prehospital standardization of medical airway management: incidence and risk factors of difficult airway. Acad Emerg Med. 2006;13(8):828-834. doi: 10.1197/j.aem.2006.02.016 [DOI] [PubMed] [Google Scholar]
- 4.de La Coussaye JE, Adnet F; groupe d’experts Sfar–SFMU . Sedation and analgesia in emergency structure: which sedation and/or analgesia for tracheal intubation? [article in French]. Ann Fr Anesth Reanim. 2012;31(4):313-321. doi: 10.1016/j.annfar.2012.01.008 [DOI] [PubMed] [Google Scholar]
- 5.Bozeman WP, Kleiner DM, Huggett V. A comparison of rapid-sequence intubation and etomidate-only intubation in the prehospital air medical setting. Prehosp Emerg Care. 2006;10(1):8-13. doi: 10.1080/10903120500366854 [DOI] [PubMed] [Google Scholar]
- 6.Okubo M, Gibo K, Hagiwara Y, Nakayama Y, Hasegawa K; Japanese Emergency Medicine Network Investigators . The effectiveness of rapid sequence intubation (RSI) versus non-RSI in emergency department: an analysis of multicenter prospective observational study. Int J Emerg Med. 2017;10(1):1. doi: 10.1186/s12245-017-0129-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sakles JC, Laurin EG, Rantapaa AA, Panacek EA. Rocuronium for rapid sequence intubation of emergency department patients. J Emerg Med. 1999;17(4):611-616. doi: 10.1016/S0736-4679(99)00046-3 [DOI] [PubMed] [Google Scholar]
- 8.Magorian T, Flannery KB, Miller RD. Comparison of rocuronium, succinylcholine, and vecuronium for rapid-sequence induction of anesthesia in adult patients. Anesthesiology. 1993;79(5):913-918. doi: 10.1097/00000542-199311000-00007 [DOI] [PubMed] [Google Scholar]
- 9.Tang L, Li S, Huang S, Ma H, Wang Z. Desaturation following rapid sequence induction using succinylcholine vs. rocuronium in overweight patients. Acta Anaesthesiol Scand. 2011;55(2):203-208. doi: 10.1111/j.1399-6576.2010.02365.x [DOI] [PubMed] [Google Scholar]
- 10.Taha SK, El-Khatib MF, Baraka AS, et al. Effect of suxamethonium vs rocuronium on onset of oxygen desaturation during apnoea following rapid sequence induction. Anaesthesia. 2010;65(4):358-361. doi: 10.1111/j.1365-2044.2010.06243.x [DOI] [PubMed] [Google Scholar]
- 11.Patanwala AE, Stahle SA, Sakles JC, Erstad BL. Comparison of succinylcholine and rocuronium for first-attempt intubation success in the emergency department. Acad Emerg Med. 2011;18(1):10-14. doi: 10.1111/j.1553-2712.2010.00954.x [DOI] [PubMed] [Google Scholar]
- 12.Tran DTT, Newton EK, Mount VAH, et al. Rocuronium vs. succinylcholine for rapid sequence intubation: a Cochrane systematic review. Anaesthesia. 2017;72(6):765-777. doi: 10.1111/anae.13903 [DOI] [PubMed] [Google Scholar]
- 13.Mallon WK, Keim SM, Shoenberger JM, Walls RM. Rocuronium vs. succinylcholine in the emergency department: a critical appraisal. J Emerg Med. 2009;37(2):183-188. doi: 10.1016/j.jemermed.2008.07.021 [DOI] [PubMed] [Google Scholar]
- 14.April MD, Arana A, Pallin DJ, et al. ; NEAR Investigators . Emergency department intubation success with succinylcholine versus rocuronium: a National Emergency Airway Registry study. Ann Emerg Med. 2018;72(6):645-653. doi: 10.1016/j.annemergmed.2018.03.042 [DOI] [PubMed] [Google Scholar]
- 15.Perry JJ, Lee JS, Sillberg VA, Wells GA. Rocuronium versus succinylcholine for rapid sequence induction intubation. Cochrane Database Syst Rev. 2008;(2):CD002788. doi: 10.1002/14651858.CD002788.pub2 [DOI] [PubMed] [Google Scholar]
- 16.Langeron O, Bourgain JL, Laccoureye O, Legras A, Orliaguet G. [Difficult airway algorithms and management: question 5. Société Française d’Anesthésie et de Réanimation]. Ann Fr Anesth Reanim. 2008;27(1):41-45. doi: 10.1016/j.annfar.2007.10.025 [DOI] [PubMed] [Google Scholar]
- 17.Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia. 1984;39(11):1105-1111. doi: 10.1111/j.1365-2044.1984.tb08932.x [DOI] [PubMed] [Google Scholar]
- 18.Adnet F, Borron SW, Racine SX, et al. The Intubation Difficulty Scale (IDS): proposal and evaluation of a new score characterizing the complexity of endotracheal intubation. Anesthesiology. 1997;87(6):1290-1297. doi: 10.1097/00000542-199712000-00005 [DOI] [PubMed] [Google Scholar]
- 19.Viby-Mogensen J, Engbaek J, Eriksson LI, et al. Good clinical research practice (GCRP) in pharmacodynamic studies of neuromuscular blocking agents. Acta Anaesthesiol Scand. 1996;40(1):59-74. doi: 10.1111/j.1399-6576.1996.tb04389.x [DOI] [PubMed] [Google Scholar]
- 20.Ricard-Hibon A, Chollet C, Leroy C, Marty J. Succinylcholine improves the time of performance of a tracheal intubation in prehospital critical care medicine. Eur J Anaesthesiol. 2002;19(5):361-367. doi: 10.1097/00003643-200205000-00008 [DOI] [PubMed] [Google Scholar]
- 21.Jabre P, Galinski M, Ricard-Hibon A, et al. Out-of-hospital tracheal intubation with single-use versus reusable metal laryngoscope blades: a multicenter randomized controlled trial. Ann Emerg Med. 2011;57(3):225-231. doi: 10.1016/j.annemergmed.2010.10.011 [DOI] [PubMed] [Google Scholar]
- 22.Jabre P, Leroux B, Brohon S, et al. A comparison of plastic single-use with metallic reusable laryngoscope blades for out-of-hospital tracheal intubation. Ann Emerg Med. 2007;50(3):258-263. doi: 10.1016/j.annemergmed.2007.04.022 [DOI] [PubMed] [Google Scholar]
- 23.Kociszewski C, Thomas SH, Harrison T, Wedel SK. Etomidate versus succinylcholine for intubation in an air medical setting. Am J Emerg Med. 2000;18(7):757-763. doi: 10.1053/ajem.2000.18033 [DOI] [PubMed] [Google Scholar]
- 24.Piaggio G, Elbourne DR, Pocock SJ, Evans SJ, Altman DG; CONSORT Group . Reporting of noninferiority and equivalence randomized trials: extension of the CONSORT 2010 statement. JAMA. 2012;308(24):2594-2604. doi: 10.1001/jama.2012.87802 [DOI] [PubMed] [Google Scholar]
- 25.Jones B, Jarvis P, Lewis JA, Ebbutt AF. Trials to assess equivalence: the importance of rigorous methods. BMJ. 1996;313(7048):36-39. doi: 10.1136/bmj.313.7048.36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.April MD, Schauer SG, Brown Rd CA, et al. A 12-month descriptive analysis of emergency intubations at Brooke Army Medical Center: a National Emergency Airway Registry study. US Army Med Dep J. 2017(3-17):98-104. [PubMed] [Google Scholar]
- 27.Johnson EG, Meier A, Shirakbari A, Weant K, Baker Justice S. Impact of rocuronium and succinylcholine on sedation initiation after rapid sequence intubation. J Emerg Med. 2015;49(1):43-49. doi: 10.1016/j.jemermed.2014.12.028 [DOI] [PubMed] [Google Scholar]
- 28.Sørensen MK, Bretlau C, Gätke MR, Sørensen AM, Rasmussen LS. Rapid sequence induction and intubation with rocuronium-sugammadex compared with succinylcholine: a randomized trial. Br J Anaesth. 2012;108(4):682-689. doi: 10.1093/bja/aer503 [DOI] [PubMed] [Google Scholar]
- 29.Tran DT, Newton EK, Mount VA, Lee JS, Wells GA, Perry JJ. Rocuronium versus succinylcholine for rapid sequence induction intubation. Cochrane Database Syst Rev. 2015;(10):CD002788. doi: 10.1002/14651858.CD002788.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Marsch SC, Steiner L, Bucher E, et al. Succinylcholine versus rocuronium for rapid sequence intubation in intensive care: a prospective, randomized controlled trial. Crit Care. 2011;15(4):R199. doi: 10.1186/cc10367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Herbstritt A, Amarakone K. Towards evidence-based emergency medicine: best BETs from the Manchester Royal Infirmary. BET 3: is rocuronium as effective as succinylcholine at facilitating laryngoscopy during rapid sequence intubation? Emerg Med J. 2012;29(3):256-258. doi: 10.1136/emermed-2012-201100.4 [DOI] [PubMed] [Google Scholar]
- 32.Higgs A, McGrath BA, Goddard C, et al. ; Difficult Airway Society; Intensive Care Society; Faculty of Intensive Care Medicine; Royal College of Anaesthetists . Guidelines for the management of tracheal intubation in critically ill adults. Br J Anaesth. 2018;120(2):323-352. doi: 10.1016/j.bja.2017.10.021 [DOI] [PubMed] [Google Scholar]
- 33.Wang HE, Yealy DM. How many attempts are required to accomplish out-of-hospital endotracheal intubation? Acad Emerg Med. 2006;13(4):372-377. doi: 10.1197/j.aem.2005.11.001 [DOI] [PubMed] [Google Scholar]
- 34.Mort TC. Emergency tracheal intubation: complications associated with repeated laryngoscopic attempts. Anesth Analg. 2004;99(2):607-613. doi: 10.1213/01.ANE.0000122825.04923.15 [DOI] [PubMed] [Google Scholar]
- 35.Sakles JC, Chiu S, Mosier J, Walker C, Stolz U. The importance of first pass success when performing orotracheal intubation in the emergency department. Acad Emerg Med. 2013;20(1):71-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hasegawa K, Shigemitsu K, Hagiwara Y, et al. Association between repeated intubation attempts and adverse events in emergency departments: an analysis of a multicenter prospective observational study. Ann Emerg Med. 2012;60(6):749-754. [DOI] [PubMed] [Google Scholar]
- 37.Jaffrelot M, Jendrin J, Floch Y, et al. Prevention of awakening signs after rapid-sequence intubation: a randomized study. Am J Emerg Med. 2007;25(5):529-534. doi: 10.1016/j.ajem.2006.09.016 [DOI] [PubMed] [Google Scholar]
- 38.Naguib M, Samarkandi AH, El-Din ME, Abdullah K, Khaled M, Alharby SW. The dose of succinylcholine required for excellent endotracheal intubating conditions. Anesth Analg. 2006;102(1):151-155. doi: 10.1213/01.ANE.0000181320.88283.BE [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial protocol
eMethods. Process for obtaining consent
eTable 1. ITT analysis
eTable2. Subgroup analyses for the primary outcome
eFigure1. Randomized patients age distribution
Statistical analysis plan
Data sharing statement