This quality improvement study assesses whether and to what extent changes in the default settings in the electronic medical record (EMR) are associated with the quantity of opioids prescribed for patients discharged from emergency departments (EDs).
Key Points
Question
Is changing the electronic medical record default settings for opioid prescriptions associated with the quantity of opioids prescribed for patients discharged from emergency departments?
Findings
In this randomized quality improvement study of 4320 opioid prescriptions, lower default settings were associated with fewer opioids prescribed and a lower proportion of prescriptions that exceeded the opioid prescribing recommendation of the Centers for Disease Control and Prevention.
Meaning
These findings suggest that default electronic medical record settings may influence prescribing behavior and should be modified to decrease the quantity of opioids prescribed.
Abstract
Importance
Prescription opioids play a significant role in the ongoing opioid crisis. Guidelines and physician education have had mixed success in curbing opioid prescriptions, highlighting the need for other tools that can change prescriber behavior, including nudges based in behavioral economics.
Objective
To determine whether and to what extent changes in the default settings in the electronic medical record (EMR) are associated with opioid prescriptions for patients discharged from emergency departments (EDs).
Design, Setting, and Participants
This quality improvement study randomly altered, during a series of five 4-week blocks, the prepopulated dispense quantities of discharge prescriptions for commonly prescribed opioids at 2 large, urban EDs. These changes were made without announcement, and prescribers were not informed of the study itself. Participants included all health care professionals (physicians, nurse practitioners, and physician assistants) working clinically in either of the 2 EDs. Data were collected from November 28, 2016, through July 9, 2017, and analyzed from July 16, 2017, through May 14, 2018.
Interventions
Default quantities for opioids were changed from status quo quantities of 12 and 20 tablets to null, 5, 10, and 15 tablets according to a block randomization scheme. Regardless of the default quantity, each health care professional decided for whom to prescribe opioids and could modify the quantity prescribed without restriction.
Main Outcomes and Measures
The primary outcome was the number of tablets of opioid-containing medications prescribed under each default setting.
Results
A total of 104 health care professionals wrote 4320 prescriptions for opioids during the study period. Using linear regression, an increase of 0.19 tablets prescribed (95% CI, 0.15-0.22) was found for each tablet increase in default quantity. When evaluating each of the 15 pairwise comparisons of default quantities (eg, 5 vs 15 tablets), a lower default was associated with a lower number of pills prescribed in more than half (8 of the 15) of the pairwise comparisons; there was a higher quantity in 1 and no difference in 6 comparisons.
Conclusions and Relevance
These findings suggest that default settings in the EMR may influence the quantity of opioids prescribed by health care professionals. This low-cost, easily implementable, EMR-based intervention could have far-reaching implications for opioid prescribing and could be used as a tool to help combat the opioid epidemic.
Trial Registration
ClinicalTrials.gov identifier: NCT04155229
Introduction
The opioid crisis is a public health emergency: addiction, overdoses, deaths, and their associated burdens have taken a toll on many communities.1,2 Some opioid use disorders may stem from an initial prescription for opioids prescribed for acute pain in opioid-naive individuals.3,4,5,6 Consequently, emergency departments (EDs), hospitals, and government policy makers have made efforts to decrease opioid prescribing.7,8,9
To decrease opioid abuse, health care professionals and policy makers will require easily implementable tools that can positively influence opioid prescribing. Altering the opioid default dispense quantities via electronic medical records (EMRs) is a simple, low-cost nudge, with promising evidence that it can affect the quantity of opioids prescribed.10,11,12
We examined the association between EMR-based defaults and opioid prescribing by ED health care professionals at 2 EDs using a randomized framework. We measured the association of defaults with the quantities prescribed and the proportion of prescriptions for quantities lasting more than 3 days, the maximum advised by guidelines for opioid prescribing.13
Methods
Design
The study protocol is available in Supplement 1. In five 4-week blocks, we altered the prepopulated dispense quantities for discharge prescriptions for commonly prescribed opioids using a block-randomization treatment schedule. Health care professionals in the EDs were not informed of the study or quantity changes. This study was approved as a quality improvement activity and thus exempted by the institutional review boards of the University of California, San Francisco, and Highland Hospital, Oakland, California. The University of California, San Francisco, Office of Ethics and Compliance also reviewed this designation and agreed that this was not a clinical trial. Because this was deemed a quality improvement activity and not human subjects research, no consent was sought, and we did not register this study as a clinical trial. However, because this study could be interpreted as a clinical trial, we retrospectively registered it at clinicaltrials.gov. This study followed the Consolidated Standards of Reporting Trials (CONSORT) reporting guidelines.
Participants
We included health care professionals (physicians, nurse practitioners, and physician assistants) working in the study EDs. Changes to default quantities were made at the system level and applied to all ED patients. Health care professionals decided for whom to prescribe opioids and could choose any quantity by altering the default setting (usual practice). Site 1 (University of California, San Francisco, Medical Center) was an academic, urban, tertiary-care center; site 2 (Highland Hospital) was an urban, level 1 trauma center and safety-net teaching hospital.
Intervention
From November 28, 2016, through July 9, 2017, we randomly assigned default dispense quantities of 5, 10, 15, and null to 4-week periods for each study opioid (eMethods in Supplement 2). One treatment quantity for each of the medications was randomly selected to have two 4-week treatment periods. The null dispense quantity forced the prescriber to enter a dispense quantity in the EMR. Study opioids included oxycodone hydrochloride, combined oxycodone and acetaminophen, and combined hydrocodone bitartrate and acetaminophen (eMethods in Supplement 2).
Before the study, the default dispense quantities at sites 1 and 2 were 20 and 12 tablets, respectively. Each site reverted to these status quo quantities after the intervention period. We used the 8 weeks before and after the 20-week treatment period as preintervention and postintervention periods in our analysis. There was an unplanned change to the treatment schedule at site 2: an error during a software upgrade caused the defaults to change to nonprotocol settings; these dates were excluded from our analysis, as described in detail in the eMethods in Supplement 2.
Outcomes
The primary outcome was the number of opioid tablets prescribed at ED discharge. Secondary outcomes included the distribution of quantity prescribed, the proportion of prescriptions for more than 12 tablets under each default setting, and the proportion of prescriptions written for the default quantity.
Statistical Analysis
Data were analyzed from July 16, 2017, through May 14, 2018. We analyzed the primary outcome using an analysis of variance with a post hoc Tukey honest significance difference analysis for difference in means and compared each default setting with each other default. We tested a dose-response association between default quantity and quantity prescribed using 2 linear regression models: one that reports the unadjusted association between changes in default settings and changes in dispense quantity, and another that also includes patient age, sex, and prescriber fixed effects. We specified default values as a continuous variable and excluded the null treatment. We included a fixed-effect coefficient for each health care professional who wrote 20 or more prescriptions during the study period; those who wrote 19 or fewer prescriptions were grouped together for a single intercept. In addition, we calculated the median, interquartile range, and proportion of prescriptions written for more than 12 tablets under each default quantity (including the preintervention and postintervention periods) and the proportion of prescriptions written for the default quantity in each of the nonzero default settings.
We required 45 prescriptions per group to detect a difference in quantity dispensed of 5 tablets between 2 default groups with an α of .05 and 80% power. Two-sided P < .05 indicated significance. All analyses were performed using STATA, version 13.1 (StataCorp LLC).
Results
A total of 104 ED health care professionals issued 4333 prescriptions for study opioids. Quantity data were missing for 13 prescriptions, leaving a sample size of 4320 prescriptions (99.7%) (Figure 1). The mean (SD) quantity prescribed in the preintervention period was 14.8 (5.8) tablets. Of the total 4320 prescriptions, 3397 (78.6%) were for combined acetaminophen (325 mg) and hydrocodone (5 mg). Site 1 wrote 2160 prescriptions for study drugs; the 2 most common prescriptions were for combined acetaminophen (325 mg) and hydrocodone (5 mg) (1923 [89.0%]) and combined acetaminophen (325 mg) and hydrocodone (7.5 mg) (121 [5.6%]). Site 2 wrote 2160 prescriptions for study drugs; the 2 most common prescriptions were for combined acetaminophen (325 mg) and hydrocodone (5 mg) (1474 [68.2%]) and oxycodone (5 mg) (357 [16.5%]). Table 1 presents the dispense quantity for each default, including preintervention and postintervention (status quo) quantities.
Figure 1. Study Flowchart.
Treatment assignment for default quantities of prescription tablets is shown. All exclusions were due to missing dispense quantity data.
Table 1. Number of Opioid Tablets Prescribed at ED Discharge Based on the Prescription Default Quantity.
| Variable | Default Quantity of Tablets for Prescription | ||||||
|---|---|---|---|---|---|---|---|
| Null (n = 415) | 5 (n = 1020) | 10 (n = 620) | 12 (n = 969)a | 15 (n = 448) | 20 (n = 848)a | All (N = 4320) | |
| No. of tablets prescribed, median (IQR) | 12 (10-20) | 12 (8-20) | 14 (10-20) | 12 (12-12) | 15 (10-20) | 20 (10-20) | 12 (10-20) |
| Written prescription for default quantity, No. (%) | NA | 197 (19.3) | 207 (33.4) | 586 (60.5) | 174 (38.8) | 402 (47.4) | 1693 (39.2) |
| Written prescription for ≤12 tablets, No. (%) | 217 (52.3) | 582 (57.1) | 308 (49.7) | 740 (76.4) | 143 (31.9) | 296 (34.9) | 2286 (52.9) |
Abbreviations: ED, emergency department; IQR, interquartile range; NA, not applicable.
Status quo settings include preintervention and postintervention periods.
In our regression model, the coefficient for default quantity was 0.19 (95% CI, 0.15-0.22): for each 1-tablet increase in default quantity, an increase of 0.19 tablets was prescribed (Table 2). In the multivariable model, this coefficient decreased to 0.08 (95% CI, 0.04-0.12). Older patients received slightly more pills (0.01 more pills per year of age; 95% CI, 0.0-0.03), and women received lower dispense quantities (0.93 fewer tablets than men; 95% CI, −1.34 to −0.53). Site 2 prescribed fewer pills per prescription (−2.76; 95% CI, −4.96 to −0.57).
Table 2. Regression Results: Dispense Quantities.
| Variable | Coefficient (95% CI) | P Value |
|---|---|---|
| Bivariate model | ||
| Default quantity | 0.19 (0.15 to 0.22) | <.001 |
| Multivariable model variablea | ||
| Default quantity | 0.08 (0.04 to 0.12) | .001 |
| Age | 0.01 (0.00 to 0.03) | .03 |
| Female | −0.93 (−1.34 to −0.53) | <.001 |
| Site 2 | −2.76 (−4.96 to −0.57) | .02 |
Fixed effects calculated from 64 health care professionals who wrote 20 or more prescriptions; 40 health care professionals who wrote 19 or fewer prescriptions were grouped together, yielding 65 separate prescriber random effects. The results presented are from linear regression models.
Table 3 shows the 15 pairwise comparisons of default settings (eg, 15 vs 5 tablets). In 8 comparisons, when an ED prescription was autopopulated with a lower default quantity of opioid pills, fewer tablets were prescribed; in 1 case, default 10 vs 12, a lower default had a higher number of tablets prescribed (difference of −1.4; 95% CI, −2.3 to −0.4) . Six comparisons had no statistically significant difference in quantity prescribed. The default quantity of 5 yielded lower quantities than the default quantities of 10 (difference of 1.8; 95% CI, 0.8-2.7), 15 (difference of 1.8; 95% CI, 0.8-2.9), and 20 (difference of 2.9; 95% CI, 2.1-3.8). All other default quantities, including the null treatment, yielded lower quantities prescribed than the default 20 setting: compared with the default 20 setting, 1.2 fewer tablets were prescribed under the default quantity 10 setting (95% CI, 0.2-2.2); 2.5 fewer tablets were prescribed under the default quantity 12 (95% CI, 1.7-3.4); 1.1 fewer tablets were prescribed under the default quantity 15 (95% CI, 0.0-2.2); and 2.0 fewer tablets were prescribed under then null setting (95% CI, 0.8-3.1). The default quantity 12 yielded lower quantities than the default quantity 15 (difference of 1.4; 95% CI, 0.4-2.5) and the default quantity 10 (difference of 1.4; 95% CI, 0.4-2.3). The 12 vs 20 comparison represents the status quo at site 2 vs site 1 and shows that these sites differed in their prescribing practices at baseline.
Table 3. Pairwise Comparisons of Quantities Dispensed at Each Default Settinga.
| Default Quantity | Default Quantity, Difference (95% CI) | |||||
|---|---|---|---|---|---|---|
| 10 | 12 | 15 | 20 | Null | ||
| 5 | 1.8 (0.8 to 2.7)b | 0.4 (−0.4 to 1.2) | 1.8 (0.8 to 2.9)b | 2.9 (2.1 to 3.8)b | 1.0 (−2.1 to 0.1) | |
| 10 | NA | −1.4 (−2.3 to −0.4)c | 0.1 (−1.1 to 1.2) | 1.2 (0.2 to 2.2)c | −0.8 (−2.0 to 0.4) | |
| 12 | NA | NA | 1.4 (0.4 to 2.5)c | 2.5 (1.7 to 3.4)b,d | 0.6 (−0.5 to 1.7) | |
| 15 | NA | NA | NA | 1.1 (0.0 to 2.2)d | −0.9 (−2.2 to −0.4) | |
| 20 | NA | NA | NA | NA | −2.0 (−3.1 to −0.8)b | |
Abbreviation: NA, not applicable.
Values represent the difference in mean number of opioid tablets prescribed between the column and row default assignment.
P < .001.
P < .01.
Default quantity 20 was only conducted at site 1, and default quantity 12 was only conducted at site 2.
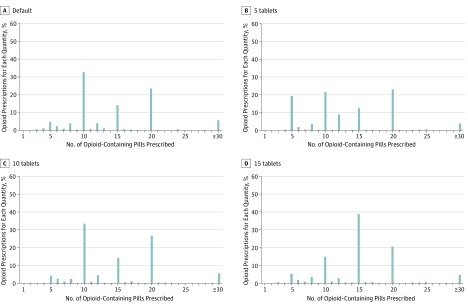
The distribution of tablets prescribed varied according to the default setting (Figure 2). The 12-tablet default setting had a higher proportion of prescriptions (76.4%) for 12 or fewer tablets than any other default; the next highest proportion of prescriptions for 12 or fewer tablets was under the default quantity of 5 (57.1%; difference of 19.2%; 95% CI, 15.2%-23.3%) (Table 1 and eTable in Supplement 2). The proportion of prescriptions for 12 or fewer tablets was higher for the lower default setting for all other default quantity comparisons (default 5 vs 10 tablets: difference of 7.5% [95% CI, 2.5%-12.5%]; default 10 vs 15 tablets: difference of 17.6% [95% CI, 11.8%-23.5%]) except default 15 vs default 20 settings, which showed no difference (difference of 2.9% [95% CI, −2.4% to 8.3%]). The corresponding distributions for the 2 status quo default quantities are presented in the eFigure in Supplement 2.
Figure 2. Distribution of Dispense Quantities by Treatment Assignment.
Each panel shows the results from 1 of 4 default settings.
Discussion
Autopopulating default prescription quantities for opioids appeared to influence the number of tablets prescribed at ED discharge. This EMR nudge was associated with the distribution of quantities of prescribed opioids and an increase in prescriber adherence to guidelines with no deleterious effect on their autonomy.
Our results build on the insights from previous work on default settings and opioid prescribing.10,11 Similar to 1 study of 2 EDs that changed from no default to a default of 10 tablets,10 we found that health care professionals tend to write prescriptions for the default quantity. As with another study,11 which examined a change from a default setting of 15 tablets to no default quantity, we found that the distribution of the number of tablets prescribed depended on the default quantity. Our work improves on the methods of these prior studies and another study12 that evaluated a change in default settings for postprocedural opioid prescriptions. These studies were all limited by before-and-after study designs and only compared 2 default settings. In contrast, our study used 3 different default values and a null setting in addition to the 2 status quo values, allowing us to estimate a dose-response relationship. Not only were our default quantities randomized, but the default quantities also increased and decreased across the 5 treatment blocks, and different default quantities were used simultaneously for different study drugs; thus, our findings are unlikely to be caused by other concurrent policy changes or secular trends.
We identified certain nuances that may inform our understanding of how default settings affect prescribing. For example, a higher mean quantity and a higher proportion of prescriptions for 20 tablets occurred under the 10- compared with the 12-tablet default assignment. This finding suggests that prescribers might respond to a lower default setting by overcompensating to increase the quantity. Also, the widest distribution in the quantity of opioids prescribed occurred when the default was blank, potentially explaining mixed results in previous studies.10,11 This default-free active choice forced health care professionals to consider the quantity they prescribed. As a result, quantities prescribed under this treatment best approximate what the prescribers believe to be the most appropriate quantity.14 Identifying prescriber beliefs about appropriate quantities of opioids is useful in itself and also provides a base for comparison with observed behaviors under the other treatments.
Of note, some prescribing patterns emerged in addition to the mean and median quantities prescribed. Each default setting showed peaks of quantities at 10, 15, and 20 tablets. Our study was not designed to identify what might cause these patterns, but we hypothesize that these are simply round numbers that prescribers chose when modifying the dispense quantity from the default setting. These numbers are less likely to correspond to a more medical rationale, such as duration of therapy. Another pattern that emerged was that prescribers were least likely to modify the default quantity of 12 tablets. This could be due to local practice at site 2, because this was the established status quo, but could also reflect a balance between putting patients at risk of developing opioid use disorder owing to overprescribing and undertreating pain owing to underprescribing.15
Our findings also align with the broader literature regarding defaults in health care. Defaults have been used to improve prescribing of generic over brand-name medications, increase adherence to Centers for Disease Control and Prevention HIV-testing guidelines, influence end-of-life decisions in advance directives, and increase recruitment rates for participation in diabetes care.16,17,18,19 Although our results suggest that EMR nudges may influence opioid prescribing, as with other studies of defaults, the mechanism by which this occurs remains unclear. Likely explanations include inertia (ie, prescribers follow the path of least resistance),20 inattention (prescribers simply overlook the updated default setting), and the possibility that prescribers assume that default settings are set according to some evidence or guidelines.
There is some concern that changing default settings repeatedly and without announcement could result in patient harm. We considered the risk of patient harm to be very low. We believed that the potential to patients due to overprescribing was much greater than the risk due to underprescribing opioids, because nonopioid medications have recently been shown to have similar effectiveness to opioids in treating acute pain.21,22 We had only 1 situation in which patients were potentially exposed to greater quantities of opioids than would have otherwise been prescribed, based on the default of 15 tablets for site 2. Overall, the range of default settings we tested—from no default to a total of 20 tablets (a 5- to 6-day supply depending on dosing frequency)—were well within an acceptable range based on current Centers for Disease Control and Prevention guidelines designed to reduce opioid misuse.13 Importantly, whether changing default settings affects opioid prescribing is precisely what we set out to study, given the limited evidence in this area.
Limitations
Our findings may not generalize to non-ED health care professionals or to other areas of the country. Of note, California has one of the lowest per capita opioid prescribing rates. It does not have a day supply limit on opioid prescriptions,23 but recent legislation mandates that ED health care professionals who are prescribing opioid quantities for 7 or more days must consult the statewide prescription data monitoring system for evidence of high-risk medication use (eg, opioid prescriptions from multiple health care professionals, use of opioids with other potentially sedating prescription medications such as benzodiazepines) before doing so.24 The EDs in the present study, to our knowledge, do not have different prescribing practices compared with other local hospitals, but they have certainly witnessed the harms some of our patients have experienced owing to opioids. Further, patient populations and local prescribing patterns vary greatly within and across settings, and responses to changes in defaults likely vary.
Our design did not allow us to investigate whether the default settings affected what proportion of patients was prescribed an opioid, which opioid was prescribed, or which patients received opioid prescriptions; nor do we report on nonstudy prescriptions. Our design also did not allow us to differentiate between prescriptions written for new conditions, acute exacerbations of chronic pain, or short-term refills of long-term prescriptions. We had an unexpected change of default settings from those of our protocol, but we were able to exclude those dates and resume the study as originally planned, albeit with an unplanned gap, and we doubt that this had any effect on the prescriber response to the study treatments. Although we analyzed a regression model that included site and prescriber effects, we were unable to account for these in our pairwise comparisons and instead present the unadjusted results.
The changes to the default settings were unannounced, which is usual practice when updating prescription settings in the EMR. However, we cannot anticipate how prescribers would respond to announced changes to the default settings; they could differ if the announcement carries with it a real or perceived rationale for the choice of quantity. Future research should investigate default opioid quantities in other settings (especially those outside the ED, where prescribing levels are higher25), interventions to reduce the use of opioids in situations in which opioids are not needed, and downstream effects of short courses of opioids; research should also consider unintended consequences, such as effects on workflow or return visits due to inadequately treated pain.
Conclusions
We identified a low-cost, easily implementable EMR-based intervention that was associated with a decrease in the quantities of opioids prescribed. Our findings demonstrate a promising method to improve prescription practices while maintaining prescriber autonomy.
Trial Protocol
eMethods. Treatment Assignment Schedule
eTable. Percentage of Prescriptions Written for a Given Quantity Prescribed According to Default Setting
eFigure. Distribution of Dispense Quantities According to Default Setting
References
- 1.Rudd RA, Aleshire N, Zibbell JE, Gladden RM; Centers for Disease Control and Prevention . Increases in drug and opioid overdose deaths—United States, 2000-2014. MMWR Morb Mortal Wkly Rep. 2016;64(50-51):1378-1382. doi: 10.15585/mmwr.mm6450a3 [DOI] [PubMed] [Google Scholar]
- 2.Unick GJ, Rosenblum D, Mars S, Ciccarone D. Intertwined epidemics: national demographic trends in hospitalizations for heroin- and opioid-related overdoses, 1993-2009. PLoS One. 2013;8(2):e54496. doi: 10.1371/journal.pone.0054496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bohnert AS, Valenstein M, Bair MJ, et al. . Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011;305(13):1315-1321. doi: 10.1001/jama.2011.370 [DOI] [PubMed] [Google Scholar]
- 4.Alam A, Gomes T, Zheng H, Mamdani MM, Juurlink DN, Bell CM. Long-term analgesic use after low-risk surgery: a retrospective cohort study. Arch Intern Med. 2012;172(5):425-430. doi: 10.1001/archinternmed.2011.1827 [DOI] [PubMed] [Google Scholar]
- 5.Hoppe JA, Kim H, Heard K. Association of emergency department opioid initiation with recurrent opioid use. Ann Emerg Med. 2015;65(5):493-499.e4. doi: 10.1016/j.annemergmed.2014.11.015 [DOI] [PubMed] [Google Scholar]
- 6.Barnett ML, Olenski AR, Jena AB. Opioid-prescribing patterns of emergency physicians and risk of long-term use. N Engl J Med. 2017;376(7):663-673. doi: 10.1056/NEJMsa1610524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Volkow ND, McLellan TA, Cotto JH, Karithanom M, Weiss SR. Characteristics of opioid prescriptions in 2009. JAMA. 2011;305(13):1299-1301. doi: 10.1001/jama.2011.401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sun BC, Charlesworth CJ, Lupulescu-Mann N, et al. . Effect of automated prescription drug monitoring program queries on emergency department opioid prescribing. Ann Emerg Med. 2018;71(3):337-347.e6. doi: 10.1016/j.annemergmed.2017.10.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kuehn BM. Scientists, officials eye tools aimed at combating abuse of painkillers. JAMA. 2012;307(1):19-21. doi: 10.1001/jama.2011.1900 [DOI] [PubMed] [Google Scholar]
- 10.Delgado MK, Shofer FS, Patel MS, et al. . Association between electronic medical record implementation of default opioid prescription quantities and prescribing behavior in two emergency departments. J Gen Intern Med. 2018;33(4):409-411. doi: 10.1007/s11606-017-4286-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zwank MD, Kennedy SM, Stuck LH, Gordon BD. Removing default dispense quantity from opioid prescriptions in the electronic medical record. Am J Emerg Med. 2017;35(10):1567-1569. doi: 10.1016/j.ajem.2017.04.002 [DOI] [PubMed] [Google Scholar]
- 12.Chiu AS, Jean RA, Hoag JR, Freedman-Weiss M, Healy JM, Pei KY. Association of lowering default pill counts in electronic medical record systems with postoperative opioid prescribing. JAMA Surg. 2018;153(11):1012-1019. doi: 10.1001/jamasurg.2018.2083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain—United States, 2016. JAMA. 2016;315(15):1624-1645. doi: 10.1001/jama.2016.1464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carroll GD, Choi JJ, Laibson D, Madrian BC, Metrick A. Optimal defaults and active decisions. Q J Econ. 2009;124(4):1639-1674. doi: 10.1162/qjec.2009.124.4.1639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ballantyne JC, Sullivan MD. Intensity of chronic pain—the wrong metric? N Engl J Med. 2015;373(22):2098-2099. doi: 10.1056/NEJMp1507136 [DOI] [PubMed] [Google Scholar]
- 16.Montoy JCC, Dow WH, Kaplan BC. Patient choice in opt-in, active choice, and opt-out HIV screening: randomized clinical trial. BMJ. 2016;532:h6895. doi: 10.1136/bmj.h6895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Patel MS, Day S, Small DS, et al. . Using default options within the electronic health record to increase the prescribing of generic-equivalent medications: a quasi-experimental study. Ann Intern Med. 2014;161(10)(suppl):S44-S52. doi: 10.7326/M13-3001 [DOI] [PubMed] [Google Scholar]
- 18.Halpern SD, Loewenstein G, Volpp KG, et al. . Default options in advance directives influence how patients set goals for end-of-life care. Health Aff (Millwood). 2013;32(2):408-417. doi: 10.1377/hlthaff.2012.0895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aysola J, Tahirovic E, Troxel AB, et al. . A randomized controlled trial of opt-in versus opt-out enrollment into a diabetes behavioral intervention. Am J Health Promot. 2018;32(3):745-752. doi: 10.1177/0890117116671673 [DOI] [PubMed] [Google Scholar]
- 20.Choi J, Laibson D, Madrian B, Metrick A. Saving for retirement on the path of least resistance In: McCaffery EJ, Slemrod J, eds. Behavioral Public Finance: Toward a New Agenda. New York, NY: Russell Sage Foundation; 2006:304-351. [Google Scholar]
- 21.Chang AK, Bijur PE, Esses D, Barnaby DP, Baer J. Effect of a single dose of oral opioid and nonopioid analgesics on acute extremity pain in the emergency department: a randomized clinical trial. JAMA. 2017;318(17):1661-1667. doi: 10.1001/jama.2017.16190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Graudins A, Meek R, Parkinson J, Egerton-Warburton D, Meyer A. A randomised controlled trial of paracetamol and ibuprofen with or without codeine or oxycodone as initial analgesia for adults with moderate pain from limb injury. Emerg Med Australas. 2016;28(6):666-672. doi: 10.1111/1742-6723.12672 [DOI] [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention US state prescribing rates, 2016. Opioid overdose. https://www.cdc.gov/drugoverdose/maps/rxstate2016.html. Updated July 31, 2017. Accessed September 3, 2018.
- 24.Cal Health & Safety Code § 1165.4.
- 25.Axeen S, Seabury SA, Menchine M. Emergency department contribution to the prescription opioid epidemic. Ann Emerg Med. 2018;71(6):659-667.e3. doi: 10.1016/j.annemergmed.2017.12.007 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol
eMethods. Treatment Assignment Schedule
eTable. Percentage of Prescriptions Written for a Given Quantity Prescribed According to Default Setting
eFigure. Distribution of Dispense Quantities According to Default Setting