Key Points
Question
What were the trends in primary care visits among commercially insured children 17 years or younger from 2008 to 2016?
Findings
In this cohort study of more than 71 million pediatric primary care visits over 29 million pediatric child-years, primary care in visits per capita decreased for commercially insured children by −14.4% between 2008 and 2016. Problem-based visit rates decreased by −24.1% while preventive visits increased by 9.9%; visit rates to non–primary care settings increased, and out-of-pocket costs for problem-based visits also increased.
Meaning
In this study, children with commercial insurance appear to visit primary care clinicians less frequently over time; changes in access to care, costs of care, expectations of care, and child health may be factors in this trend.
Abstract
Importance
Primary care is the foundation of pediatric care. While policy interventions have focused on improving access and quality of primary care, trends in overall use of primary care among children have not been described.
Objective
To assess trends in primary care visit rates and out-of-pocket costs, to examine variation in these trends by patient and visit characteristics, and to assess shifts to alternative care options (eg, retail clinics, urgent care, and telemedicine).
Design, Setting, and Participants
Observational cohort study of claims data from 2008 to 2016 for children 17 years and younger covered by a large national commercial health plan. Visit rate per 100 child-years was determined for each year overall, by child and geographic characteristics, and by visit type (eg, primary diagnosis), and trends were assessed with a series of child-year Poisson models. Data were analyzed from November 2017 to September 2019.
Main Outcomes and Measures
Visits to primary care and other settings.
Results
This cohort study included more than 71 million pediatric primary care visits over 29 million pediatric child-years (51% male in 2008 and 2016; 37% between 12-17 years in 2008 and 38% between 12-17 years in 2016). Unadjusted results for primary care visit rates per 100 child-years decreased from 259.6 in 2008 to 227.2 in 2016, yielding a regression-estimated change in primary care visits across the 9 years of −14.4% (95% CI, −15.0% to −13.9%; absolute change: −32.4 visits per 100 child-years). After controlling for shifts in demographics, the relative decrease was −12.8% (95% CI, −13.3% to −12.2%). Preventive care visits per 100 child-years increased from 74.9 in 2008 to 83.2 visits in 2016 (9.9% change in visit rate; 95% CI, 9.0%-10.9%; absolute change: 8.3 visits per 100 child-years), while problem-based visits per 100 child-years decreased from 184.7 in 2008 to 144.1 in 2016 (−24.1%; 95% CI, −24.6% to −23.5%; absolute change: −40.6 visits per 100 child-years). Visit rates decreased for all diagnostic groups except for the behavioral and psychiatric category. Out-of-pocket costs for problem-based primary care visits increased by 42% during the same period. Per 100 child-years, visits to other acute care venues increased from 21.3 to 27.6 (30.3%; 95% CI, 28.5% to 32.1%; absolute change: 6.3 visits per 100 child-years) and visits to specialists from 45.2 to 53.5 (16.4%; 95% CI, 14.8% to 18.0%, absolute change: 8.3 visits per 100 child-years).
Conclusions and Relevance
Primary care visit rates among commercially insured children decreased over the last decade. Increases in out-of-pocket costs and shifts to other venues appear to explain some of this decrease.
This cohort study characterizes US trends in primary care visit rates among individuals 17 or younger covered by a large national commercial health plan from 2008 to 2016 and identifies variables associated with visit rates.
Introduction
Primary care is the foundation of pediatric care, with the American Academy of Pediatrics advocating for the primary care practice to be the center of health supervision, screening, management of acute and chronic conditions, and care coordination.1 Many policy interventions have focused on improving access and quality of primary care.2 For example, a core component of patient-centered medical home initiatives is increasing access to care, including access to after-hours care.1,2 The Affordable Care Act prioritized primary care by eliminating copayments for preventive services.3 Several Healthcare Effectiveness Data and Information Set quality measures focus on whether children receive well-child visits,4 and an increasing percentage of children received at least 1 annual well child visit from 2000 to 2014.5
However, despite these initiatives, there are several factors that may be associated with reduced overall use of primary care. First, while the Affordable Care Act eliminated out-of-pocket costs for preventive visits, many families have seen increased out-of-pocket costs for problem-based primary care visits and increased deductibles over the last decade.6,7 Second, alternatives to primary care, such as retail clinics, urgent care centers, and telemedicine, continue to expand.8,9,10 Third, survey data suggest that families expect more timely access to care by telephone and in person than they are currently receiving within primary care,11,12 potentially leading them to other sources of care. In addition, health care needs of children have also changed in multiple ways. The continued decrease in vaccine-preventable illnesses13,14,15,16 could decrease the need for primary care for these acute illnesses, while increases in chronic conditions and mental health concerns among children17,18 may increase demand for primary care for chronic disease management.
Despite these changing contexts of primary care, trends in overall use of primary care among children have not been described, which may differ for commercially insured and Medicaid insured populations. In the adult population, rates of primary care visits are decreasing.19,20 To address this knowledge gap, we described trends in primary care visits among commercially insured children within a large national health plan overall and by patient and visit characteristics. We also examined trends in use of alternative sites of care and out-of-pocket costs per visit.
Methods
In this cohort study, we used claims data from 2008-2016 for children 17 years and younger covered by a large national commercial health insurance company. This company covers enrollees across all 50 states with a range of benefit options (including high deductible, health maintenance organization, and preferred provider organization), including approximately 4 million child-years annually.
We categorized visits by incorporating Current Procedural Terminology (CPT) codes, place of service codes, national provider identifiers, and tax identification numbers.9,10,21 Specifically, we categorized visits as urgent care or as retail-based clinic visits based on place of service codes, organizational national provider identifiers, or tax identification numbers indicating these venues.10,22 We categorized visits as telemedicine based on CPT codes (eg, 99444) or CPT modifiers (GT, GQ) indicating a telemedicine visit. We categorized visits as emergency department visits using CPT codes and place of service codes. Among the remaining visits, primary care provider visits were defined as outpatient CPT codes (eg, 99201-99205, 99211-99215, 99381-99387, and 99391-99397) performed by a clinician with a primary care specialty code (eg, physician, nurse practitioner, or physician assistant in the specialty of general pediatrics, family practice, internal medicine, or general practice). The specialty codes for the remaining visits were reviewed and categorized as specialty visits after excluding specialties unlikely to engage in direct patient care (eg, radiology, pathology).
We examined visit rates by assessing visits per child-years, which accounts for the variation in months of enrollment for each child during a given calendar year. We excluded child-years with more than 100 primary care visits in a given year (n = 11) to avoid inclusion of extreme outliers. Patient and geographic characteristics in our analysis included child age, sex, zip code median income, rural or urban status, health plan type, and chronic disease status. We determined demographic characteristics from health plan enrollment files for each year, such that covariates updated annually. The zip code median income was determined based on US Census Bureau data for the child’s zip code, which we then categorized by percentage of the federal poverty level for a family of 4 in 2015.23 Metropolitan statistical areas (MSAs) were distinguished from non-MSAs based on zip code categorization from the National Bureau of Economic Research.24 Chronic disease status was determined independently for each child-year by applying the Patient Medical Complexity Algorithm to the patient’s inpatient and outpatient medical files for each year of claims.25
Primary care visit characteristics in our analysis included visit type (preventive vs problem-based), primary diagnosis group, and out-of-pocket costs. We categorized primary care visits as preventive vs problem-based using CPT codes, with preventive care visit CPT codes including 99381-99387 and 99391-99397 and the remaining visits categorized as problem-based. Among problem-based primary care visits, we determined the diagnosis group of the primary diagnosis using a diagnosis grouping system developed for categorization of acute pediatric diagnoses.26 Out-of-pocket costs for problem-based visits were determined by summing the deductible, copayment, and co-insurance payments on the claim for that visit and adjusting for inflation27 to 2016 dollar amounts. Out-of-pocket costs were winsorized to the 1st and 99th percentile. We also categorized each visit on whether it was associated with any deductible payments. The Harvard University Institutional Review Board determined that this study met criteria for review exemption and waiver of informed patient consent as a secondary analysis of deidentified data.
Statistical Analysis
To describe trends in primary care visits, we calculated unadjusted visit rates per child-year from 2008-2016 for the entire sample and by patient demographics (age, sex, chronic medical complexity, zip code median income, MSA designation, and census region). To assess trends across the 9-year study period, we used log-linear Poisson regression models with child-year as the unit of analysis, examining the visit rate with an offset accounting for the number of enrolled months in a given year. We first examined child-year visit rate with year as a continuous variable in an unadjusted Poisson model. We tested models with and without a quadratic term for year and found that the quadratic term did not significantly improve the explanatory value of the model and therefore only used linear models.
To account for changes in member demographics when assessing trends, we next examined child-year visit rate with year as a continuous variable in a Poisson model adjusting for demographic and geographic variables (age, sex, chronic medical complexity, MSA designation, zip code median income, and census region) as well as an indicator variable for 2009 to account for the higher volume in the setting of H1N1 influenza. To examine trends within specific levels of demographic and geographic variables or across visit types, we next used a series of Poisson models, each including year as a continuous variable–the categorical demographic variable of interest–and interaction terms between year and the categorical demographic variable, allowing separate determination of trends within different levels of each category. We tested for effect modification by assessing the statistical significance of interaction terms. The small number of child-years in which zip code median income or MSA designation was missing (<0.3% of the sample) was excluded from Poisson models in which these variables were included.
To examine the potential concurrent shifts to alternative sites of care, we determined unadjusted visit rates per child-year to urgent care, retail clinics, direct-to-consumer telemedicine, specialists, and emergency departments. In addition, we examined costs over time and the percentage of visits associated with a deductible over time by using generalized linear models with a γ distribution and log link and using logistic models, respectively, to test for trends.
Analyses were performed in SAS, version 9.4 (SAS Institute Inc), with statistical significance set at P < .05. Visit rates are reported for the full 100% sample; Poisson models were performed with a random 5% of children from each calendar year to ease computational burden. While most children contributed multiple child-years to the 100% sample, only 7% of children contributed more than 1 child-year in the 5% analytic sample. In sensitivity analysis, we repeated main analyses after further restricting the analytic sample to 1 randomly selected child-year per child.
Results
This cohort study included more than 71 million pediatric primary care visits over 29 million pediatric child-years from 2008 to 2016 (51% male in 2008 and 2016; 37% between 12-17 years in 2008 and 38% between 12-17 years in 2016). The demographic characteristics of beneficiaries changed little during this time period, with a slight increase (1%-2%) in the proportion of the population residing in the West (from 19% to 20%) and South (from 41% to 43%) and a slight decrease in the Northeast and Midwest (Table 1). Rates of chronic medical complexity were similar across all years.
Table 1. Demographic and Geographic Characteristics of Commercially Insured US Children, 2008 and 2016.
| Characteristic | Child-Years, No. (%) | |
|---|---|---|
| 2008 | 2016 | |
| Total | 3 441 187 | 3 018 558 |
| Age, y | ||
| 0-1 | 254 364 (7) | 212 859 (7) |
| 2-5 | 730 694 (21) | 615 154 (20) |
| 6-11 | 1 180 922 (34) | 1 043 978 (35) |
| 12-17 | 1 275 207 (37) | 1 146 567 (38) |
| Sex | ||
| Female | 1 685 124 (49) | 1 476 335 (49) |
| Male | 1 756 063 (51) | 1 542 223 (51) |
| Presence of chronic conditions | ||
| None | 3 011 698 (88) | 2 649 605 (88) |
| Noncomplex | 321 253 (9) | 286 018 (9) |
| Complex | 108 236 (3) | 82 935 (3) |
| Zip code median income, FPL | ||
| 0%-200% | 772 306 (22) | 675 564 (22) |
| 201%-300% | 1 203 951 (35) | 1 013 753 (34) |
| 301%-400% | 827 129 (24) | 749 548 (25) |
| ≥401% | 626 940 (18) | 574 977 (19) |
| Missing | 10 861 (0.3) | 4716 (0.2) |
| MSA designation | ||
| Non-MSA | 794 669 (23) | 731 122 (24) |
| MSA | 2 639 408 (77) | 2 285 285 (76) |
| Missing | 7111 (0.2) | 2152 (0.1) |
| Region | ||
| Northeast | 846 681 (25) | 705 049 (23) |
| Midwest | 540 926 (16) | 410 469 (14) |
| South | 1 409 773 (41) | 1 305 977 (43) |
| West | 643 807 (19) | 597 063 (20) |
Abbreviations: FPL, federal poverty limit; MSA, metropolitan statistical area.
In unadjusted results, primary care visit rates per 100 child-years decreased from 259.6 in 2008 to 227.2 in 2016 (absolute change: −32.4 visits per 100 child-years; Figure). The Poisson regression yielded an estimated change in primary care visit rate across the 9 years of −14.4% (95% CI, −15.0% to −13.9%) (Table 2). After adjusting for demographic characteristics, the regression-estimated change in primary care visit rate across the 9 years was similar (−12.9%; 95% CI, −13.3% to 12.4%). Sensitivity analysis including only 1 child-year per child yielded similar results (−12.8%; 95% CI, −13.3% to −12.2%).
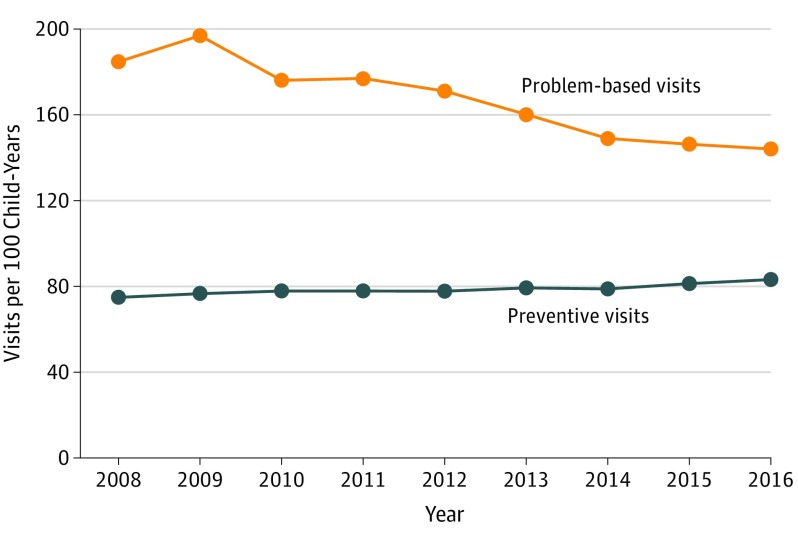
Figure. Primary Care Visit Rates Among Commercially Insured US Children, 2008-2016.
Table 2. Change in Primary Care Visit Rates Overall and by Patient Characteristics Among Commercially Insured US Children, 2008 to 2016.
| Characteristic | Visits per 100 Child-Years | Absolute Change | Relative Change, % (95% CI)a | P Value for Interaction Term | |
|---|---|---|---|---|---|
| 2008 | 2016 | ||||
| Full cohort | 259.6 | 227.2 | −32.4 | −14.4 (−15.0 to −13.9) | NA |
| Child age, y | |||||
| 0-1 | 833.1 | 786.3 | −46.8 | −6.0 (−6.9 to −5.1) | <.001 |
| 2-5 | 336.8 | 285.1 | −51.7 | −16.7 (−17.5 to −15.9) | |
| 6-11 | 196.9 | 171.0 | −25.9 | −17.0 (−17.7 to −16.2) | |
| 12-17 | 158.9 | 143.6 | −15.3 | −13.3 (−14.2 to −12.5) | |
| Sex | |||||
| Female | 259.8 | 226.4 | −33.4 | −14.2 (−14.9 to −13.4) | .21 |
| Male | 259.4 | 228.1 | −31.3 | −14.8 (−15.5 to −14.0) | |
| Presence of chronic conditions | |||||
| None | 237.0 | 205.1 | −31.9 | −15.6 (−16.1 to −15.0) | <.001 |
| Noncomplex | 402.1 | 368.7 | −33.4 | −9.9 (−11.2 to −8.5) | |
| Complex | 464.9 | 447.6 | −17.3 | −5.3 (−7.5 to −3.0) | |
| Zip code median income, FPLb | |||||
| 0%-200% | 214.0 | 182.0 | −32.0 | −16.9 (−18.1 to −15.7) | <.001 |
| 201%-300% | 250.6 | 226.9 | −23.7 | −12.2 (−13.1 to −11.2) | |
| 301%-400% | 278.4 | 241.7 | −36.7 | −14.7 (−15.7 to −13.7) | |
| ≥401% | 309.3 | 262.9 | −46.4 | −16.2 (−17.3 to −15.2) | |
| MSA designationb | |||||
| Non-MSA | 221.4 | 209.1 | −12.3 | −5.4 (−6.6 to −4.2) | <.001 |
| MSA | 271.3 | 233.2 | −38.1 | −16.5 (−17.1 to −15.9) | |
| Region | |||||
| Northeast | 300.7 | 274.0 | −26.7 | −11.2 (−12.2 to −10.2) | <.001 |
| Midwest | 241.2 | 235.4 | −5.8 | −6.4 (−7.8 to −4.9) | |
| South | 266.9 | 219.4 | −47.4 | −19.8 (−20.5 to −19.0) | |
| West | 204.9 | 183.5 | −21.3 | −9.9 (−11.2 to −8.6) | |
Abbreviations: FPL, federal poverty limit; MSA, metropolitan statistical area; NA, not applicable.
Relative change during study period was estimated from Poisson regression using data from 2008-2016 accounting for member time in the plan in a given year.
Between 0.1% and 0.3% of child-years had missing zip code median income and missing MSA designation in each year. Child-years with missing status for these 2 variables were excluded from regressions modeling that variable only.
We observed a decrease in primary care visit rates across all patient subgroups (Table 2). The interactions between patient characteristics and year were all statistically significant except for sex. The regression-estimated change in primary care visit rate was smaller for the youngest children (0- to 1-year-olds: −6.0% change in primary care visit rate; 95% CI, −6.9% to −5.1%) and those in non-MSAs (−5.4%; 95% CI, −6.6% to −4.2%). Change in the primary care visit rate was larger for children residing in zip codes with the lowest median incomes (−16.9%; 95% CI, −18.1 to −15.0%) and those in the South (−19.8%; 95% CI, −20.5% to −19.0%).
During the study period, preventive primary care visit rates increased from 74.9 to 83.2 visits per 100 child-years, yielding a regression-estimated change in preventive primary care visit rate across the 9 years of 9.9% (95% CI, 9.0%-10.9%) (Table 3). In contrast, problem-based primary care visits decreased from 184.7 to 144.1 per 100 child-years, yielding a regression-estimated change of −24.1% (95% CI, −24.6% to −23.5%). Among problem-based visits, we observed decreases in all diagnosis groups except for psychiatric and behavioral health visits, which increased by 42.0% across the 9-year study period (95% CI, 36.8%-47.3%).
Table 3. Change in Primary Care Visit Rate by Visit Characteristics Among Commercially Insured US Children, 2008 to 2016.
| Characteristic | Visits per 100 Child-Years | Absolute Change | Relative Change, % (95% CI)a | |
|---|---|---|---|---|
| 2008 | 2016 | |||
| Visit type | ||||
| Preventive | 74.9 | 83.2 | 8.3 | 9.9 (9.0 to 10.9) |
| Problem-based | 184.7 | 144.1 | −40.6 | −24.1 (−24.6 to −23.5) |
| Problem-based visit diagnosis group | ||||
| Ear/nose/throat/mouth/dental | 78.9 | 55.7 | −23.2 | −33.0 (−33.7 to −32.3) |
| Respiratory | 20.3 | 13.7 | −6.7 | −33.4 (−34.6 to −32.3) |
| Skin | 16.4 | 11.4 | −5.0 | −29.6 (−30.8 to −28.4) |
| Systemic | 14.1 | 10.7 | −3.4 | −17.6 (−19.1 to −16.1) |
| Gastrointestinal | 11.3 | 8.8 | −2.5 | −20.8 (−22.7 to −19.0) |
| Trauma | 7.0 | 5.1 | −1.9 | −24.8 (−26.6 to −23.0) |
| Eye | 4.5 | 3.6 | −0.9 | −22.3 (−24.7 to −19.9) |
| Psychiatric or behavioral | 4.4 | 6.1 | 1.7 | 42.0 (36.8 to 47.3) |
| Musculoskeletal | 4.1 | 3.6 | −0.5 | −14.0 (−16.6 to −11.3) |
| Urinary | 3.0 | 2.1 | −0.9 | −32.0 (−34.7 to −29.2) |
| Neurologic | 2.4 | 2.1 | −0.2 | −8.0 (−11.8 to −3.9) |
| Endocrine or metabolic | 2.3 | 2.1 | −0.2 | −5.4 (−10.9 to −0.5) |
| Genitourinary | 1.4 | 1.2 | −0.2 | −19.4 (−23.5 to −15.1) |
| Allergic | 1.4 | 1.1 | −0.3 | −13.9 (−18.7 to −8.8) |
| Otherb | 13.2 | 16.7 | 3.5 | 10.9 (9.9 to 11.8) |
Relative change during study period was estimated from Poisson regression accounting for member time in the plan in a given year.
“Other” includes visits categorized as “other” (11.9 visits per 100 child-years in 2008) and visits categorized in diagnosis groups with <1 visit per child-year (cardiovascular: 0.5; hematologic: 0.3; child abuse: 0.2; oncologic: 0.1; toxin: 0.1; and fluids/electrolyte/nutrition: 0.1).
Among problem-based visits, 75th percentile out-of-pocket costs increased from $31 (median: $26) in 2008 to $50 (median: $25) in 2016 (P < .001), while 75th percentile out-of-pocket costs for preventive visits decreased from $26 (median: $19) to $0 (median: $0; P < .001). The percentage of problem-based visits associated with a deductible increased 9% to 25% (P < .001).
Visits to alternative venues increased over time (Table 4). Visit to acute care venues (emergency department, urgent care, retail-based clinic, and telemedicine) increased during the study period from 21.3 to 27.6 visits per 100 child-years, yielding a regression-estimated change of 30.3% (95% CI, 28.5%-32.1%; absolute change: 6.3 visits per 100 child-years). Visits to specialists increased from 45.2 to 53.5 per 100 child-years (16.4%; 95% CI, 14.8%-18.0%; absolute change: 8.3 visits per 100 child-years). Visits across all settings (primary care, acute venues, and specialists) decreased by −0.9% over the last decade (95% CI, −1.4% to −0.4%) from 326.1 visits per 100 child-years in 2008 to 308.4 visits per 100 child-years in 2016.
Table 4. Trends in Visits to ED, Urgent Care, Retail Clinic, Telemedicine, and Specialist Venues.
| Visit | Visits per 100 Child-Years | Change, % (95% CI)a | ||
|---|---|---|---|---|
| 2008 | 2016 | Absolute Change | ||
| Primary care | 259.6 | 227.2 | −32.4 | −14.4 (−15.0 to −13.9) |
| Preventive | 74.9 | 83.2 | 8.3 | NA |
| Problem-based | 184.7 | 144.1 | −40.6 | NA |
| Acute care outside of primary care | 21.3 | 27.6 | 6.3 | 30.3 (28.5 to 32.1) |
| ED | 15.4 | 15.3 | −0.1 | NA |
| Urgent care | 5.1 | 8.8 | 3.7 | NA |
| Retail clinic | 0.8 | 2.7 | 1.9 | NA |
| Telemedicine | 0.007 | 0.8 | 0.8 | NA |
| Specialist | 45.2 | 53.5 | 8.3 | 16.4 (14.8 to 18.0) |
| Total | 326.1 | 308.4 | −17.7 | −0.9 (−1.4 to −0.4) |
Abbreviations: ED, emergency department; NA, not applicable.
Percent change during study period was estimated from Poisson regression accounting for member time in the plan in a given year.
Discussion
From 2008 to 2016, visit rates among children to primary care clinicians substantially decreased. This decrease occurred across all demographic groups, geographic regions, and diagnosis groups with the exception of the behavioral and psychiatric diagnosis group. Potential explanations for these trends could include (1) replacement of primary care visits with other sites of care; (2) increased out-of-pocket costs creating a disincentive to primary care; (3) rise in other nonfinancial barriers to primary care; or (4) decreased need for primary care.
Visits to other settings (urgent care, retail clinics, emergency departments, telemedicine, and specialty care) did increase during this period, particularly among urgent care, retail-based clinics, and direct-to-consumer telemedicine (consistent with other studies10), while emergency department visit rates were relatively stable. Altogether, the absolute increase in visits to these other sites (6.3 to acute care settings and 8.3 to specialists per 100 child-years) offset nearly half of the absolute decrease in primary care visits (−32.4 per 100 child-years), suggesting that replacement of primary care visits with visits to other sites of care may explain a portion of our findings.
An increase in financial barriers is another potential factor associated with the decrease. We observed a 42% increase in out-of-pocket costs for problem-based visits, while inflation-adjusted median household income increased by only 5% during this time period.28 Children in families reporting higher out-of-pocket costs are more likely to have unmet health care needs,29 and increases of even $1.00 to $10.00 in copayments are associated with fewer visits.30,31 Using the price elasticity estimates from prior work (which have ranged from approximately −0.1 to −0.232) and the 42% observed increase in out-of-pocket costs, we estimate that a 4% to 8% decrease in problem-based primary care visits (approximately 8-16 fewer problem-based visits per 100 child-years) could be associated with the observed increase in out-of-pocket costs. While increasing financial barriers do not fully explain the decrease in primary care visits, they likely explain some portion of the trend.
Nonfinancial barriers may also be factors, such as the balance of clinician supply and patient demand and the geographic distribution of clinicians. With the increase in the percentage of people with insurance after the Affordable Care Act, more individuals may be vying for the same pool of primary care clinicians, which might have led to a decrease in availability of timely appointments in some regions of the country.33 Other shifts in family circumstances, such as more parents working multiple jobs, may further constrain the opportunities to seek care for patients, potentially contributing to an unmet need for care. We were unable to directly evaluate these factors in our study.
Of note, we found that geographic areas with higher rates of visits at baseline (MSAs, the Northeast, and the South) experienced larger relative decreases in problem-based visits over time than those with lower visit rates at baseline (non-MSAs, the Midwest). One possible interpretation of this finding could include that some areas had a higher rate of discretionary visits at baseline, which could result in a larger decrease if the system became more constrained regardless of mechanism (eg, increased copays or decreased availability). Alternatively, it could be that some areas already had significantly constrained access (eg, lack of availability and transportation barriers in non-MSAs) and that additional barriers within an already constrained system did not translate into as substantial a decrease in visit rates.
Children may also have less need for primary care owing to public health improvements. The introduction of specific vaccines has been associated with decreased outpatient visits and fewer hospitalizations for vaccine-preventable illnesses, such as pneumococcal, Haemophilus influenzae serotype B, and rotavirus illnesses.13,14,15,16 Reductions in rates of otitis media have been reported over the last 2 decades in association with relevant vaccination16,34,35,36,37,38,39 as well as increasing stringency of diagnostic criteria.40 Antibiotic stewardship efforts led by national and local organizations may also be associated with reductions in visits for acute respiratory tract infections more broadly by reducing the perceived necessity of antibiotics when children are ill.41,42 However, it is notable that the reduction in visits was similar among skin diagnoses, which would presumably not be affected by increased vaccination rates or antibiotic stewardship.
Another potential factor is shifting expectations of care. On the physician side, guidelines have noted the lack of scientific evidence to support routine follow-up visits after common childhood illnesses, such as ear infections.40 To the degree that physicians change their practice patterns in response to such guidelines, illnesses that previously received multiple visits may now result in a single visit, with follow-up advised only if symptoms do not resolve. Additionally, increasing numbers of parents use electronic messaging with pediatricians,43 and it is possible that this virtual contact decreases the need for some visits. On the family side, families are increasingly using internet searches and social media to seek medical advice,44,45 which may also reduce demand for care.
The key underlying question is whether the decrease in the primary care visit rate among children is a positive or negative finding. Some of the possible mechanisms, such as decreased burden of disease, greater parental self-efficacy in caring for minor illnesses at home, and fewer unnecessary recheck visits, would be positive mechanisms for reduced visit volume, indicating healthier children, more efficient health care systems, and reduced burden of low-value visits on families. However, any decrease in visits owing to worsening affordability, availability, or accessibility of care could result in an increased unmet need for care, which would warrant attention and intervention. Even when not resulting in immediate sequelae measurable in claims data (eg, increased emergency department visits or hospitalizations), unmet need may result in unmeasured consequences or worse health outcomes over a longer time period (eg, increased family anxiety or progression of undiagnosed or undertreated chronic disease). Investigation focused on testing these potential mechanisms and consequences of identified trends may be warranted to inform appropriate action.
Limitations
Limitations of our study include that, as an analysis based on claims data, we lack clinical records and data on severity of illness or follow-up recommendations. Because of lack of data, we also could not assess other potentially relevant variables such as health literacy, proximity to care, transportation availability, language barriers, and experiences of marginalization within the health care system. We also lack data on parent or physician perceptions of need for care or of unmet need for care. Future analysis incorporating such measures could substantially add to our understanding of the implications of these findings. While the children in this analysis are geographically diverse and represent a wide range of health plan products, the data are limited to a single commercial insurer and do not include uninsured children or children insured by Medicaid. In these other populations, the trends may be different. In addition, as an observational analysis, we were unable to test the causality of these different factors, so co-occurring trends in access and utilization over time were described.
Conclusions
In this study, we estimated that a 14.4% decrease in primary care visit rates occurred among children from 2008 to 2016, and we observed decreased visit rates among different sociodemographic groups and across most diagnosis groups. The decrease occurred specifically among problem-based visits, and the decrease was partially offset by an increase in preventive visits and visits to other settings.
References
- 1.Medical Home Initiatives for Children With Special Needs Project Advisory Committee; American Academy of Pediatrics . The medical home. Pediatrics. 2002;110(1, pt 1):184-186. [PubMed] [Google Scholar]
- 2.Cooley WC, McAllister JW, Sherrieb K, Kuhlthau K. Improved outcomes associated with medical home implementation in pediatric primary care. Pediatrics. 2009;124(1):358-364. doi: 10.1542/peds.2008-2600 [DOI] [PubMed] [Google Scholar]
- 3.Koh HK, Sebelius KG. Promoting prevention through the Affordable Care Act. N Engl J Med. 2010;363(14):1296-1299. doi: 10.1056/NEJMp1008560 [DOI] [PubMed] [Google Scholar]
- 4.National Committee for Quality Assurance. HEDIS and performance measures. https://www.ncqa.org/hedis/. Accessed April 5, 2019.
- 5.Larson K, Cull WL, Racine AD, Olson LM. Trends in access to health care services for US children: 2000-2014. Pediatrics. 2016;138(6):e20162176. doi: 10.1542/peds.2016-2176 [DOI] [PubMed] [Google Scholar]
- 6.Claxton G, Rae M, Long M, Damico A Employer Health Benefits: 2018 Annual Survey. https://www.kff.org/health-costs/report/2018-employer-health-benefits-survey/. Published October 13, 2018. Accessed April 5, 2019.
- 7.Claxton G, Rae M, Long M, Damico A, Whitmore H, Foster G. Health benefits in 2016: family premiums rose modestly, and offer rates remained stable. Health Aff (Millwood). 2016;35(10):1908-1917. doi: 10.1377/hlthaff.2016.0951 [DOI] [PubMed] [Google Scholar]
- 8.Mehrotra A, Lave JR. Visits to retail clinics grew fourfold from 2007 to 2009, although their share of overall outpatient visits remains low. Health Aff (Millwood). 2012;31(9):2123-2129. doi: 10.1377/hlthaff.2011.1128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ray KN, Shi Z, Poon SJ, Uscher-Pines L, Mehrotra A. Use of commercial direct-to-consumer telemedicine by children. Acad Pediatr. 2019;19(6):665-669. doi: 10.1016/j.acap.2018.11.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Poon SJ, Schuur JD, Mehrotra A. Trends in low-acuity visits to acute care venues in the United States from 2008 to 2015. JAMA Intern Med. 2018;178(10):1342-1349. doi: 10.1001/jamainternmed.2018.3205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ray KN, Mehrotra A. Trends in access to primary care for children in the United States, 2002-2013. JAMA Pediatr. 2016;170(10):1023-1025. doi: 10.1001/jamapediatrics.2016.0985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zickafoose JS, DeCamp LR, Prosser LA. Parents’ preferences for enhanced access in the pediatric medical home: a discrete choice experiment. JAMA Pediatr. 2015;169(4):358-364. doi: 10.1001/jamapediatrics.2014.3534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Burnett E, Jonesteller CL, Tate JE, Yen C, Parashar UD. Global impact of rotavirus vaccination on childhood hospitalizations and mortality from diarrhea. J Infect Dis. 2017;215(11):1666-1672. doi: 10.1093/infdis/jix186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.MacNeil JR, Cohn AC, Farley M, et al. Current epidemiology and trends in invasive Haemophilus influenzae disease–United States, 1989-2008. Clin Infect Dis. 2011;53(12):1230-1236. doi: 10.1093/cid/cir735 [DOI] [PubMed] [Google Scholar]
- 15.Jacobs DM, Yung F, Hart E, Nguyen MNH, Shaver A. Trends in pneumococcal meningitis hospitalizations following the introduction of the 13-valent pneumococcal conjugate vaccine in the United States. Vaccine. 2017;35(45):6160-6165. doi: 10.1016/j.vaccine.2017.09.050 [DOI] [PubMed] [Google Scholar]
- 16.Singleton R, Seeman S, Grinnell M, et al. Trends in otitis media and myringotomy with tube placement among American Indian and Alaska Native children and the US general population of children after introduction of the 13-valent pneumococcal conjugate vaccine. Pediatr Infect Dis J. 2018;37(1):e6-e12. doi: 10.1097/INF.0000000000001704 [DOI] [PubMed] [Google Scholar]
- 17.Garfield CF, Dorsey ER, Zhu S, et al. Trends in attention deficit hyperactivity disorder ambulatory diagnosis and medical treatment in the United States, 2000-2010. Acad Pediatr. 2012;12(2):110-116. doi: 10.1016/j.acap.2012.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Van Cleave J, Gortmaker SL, Perrin JM. Dynamics of obesity and chronic health conditions among children and youth. JAMA. 2010;303(7):623-630. doi: 10.1001/jama.2010.104 [DOI] [PubMed] [Google Scholar]
- 19.Chou SC, Venkatesh AK, Trueger NS, Pitts SR. Primary care office visits for acute care dropped sharply in 2002-15, while ED visits increased modestly. Health Aff (Millwood). 2019;38(2):268-275. doi: 10.1377/hlthaff.2018.05184 [DOI] [PubMed] [Google Scholar]
- 20.Ganguli I, Lee TH, Mehrotra A. Evidence and implications behind a national decline in primary care visits. J Gen Intern Med. 2019;34(10):2260-2263. doi: 10.1007/s11606-019-05104-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shi Z, Mehrotra A, Gidengil CA, Poon SJ, Uscher-Pines L, Ray KN. Quality of care for acute respiratory infections during direct to consumer telemedicine visits for adults. Health Aff (Millwood). 2018;37(12):2014-2023. doi: 10.1377/hlthaff.2018.05091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ray KN, Shi Z, Gidengil CA, Poon SJ, Uscher-Pines L, Mehrotra A. Antibiotic prescribing during pediatric direct-to-consumer telemedicine visits. Pediatrics. 2019;143(5):e20182491. doi: 10.1542/peds.2018-2491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.United States Census Bureau 2010. Census. https://www.census.gov/programs-surveys/decennial-census/data/datasets.2010.html. Accessed December 3, 2019.
- 24.The National Bureau of Economic Research CMS's SSA to FIPS CBSA and MSA county crosswalk. https://www.nber.org/data/cbsa-msa-fips-ssa-county-crosswalk.html. Updated April 25, 2017. Accessed May 4, 2019.
- 25.Simon TD, Cawthon ML, Popalisky J, Mangione-Smith R; Center of Excellence on Quality of Care Measures for Children with Complex Needs (COE4CCN) . Development and validation of the Pediatric Medical Complexity Algorithm (PMCA) version 2.0. Hosp Pediatr. 2017;7(7):373-377. doi: 10.1542/hpeds.2016-0173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Alessandrini EA, Alpern ER, Chamberlain JM, Shea JA, Gorelick MH. A new diagnosis grouping system for child emergency department visits. Acad Emerg Med. 2010;17(2):204-213. doi: 10.1111/j.1553-2712.2009.00635.x [DOI] [PubMed] [Google Scholar]
- 27.Federal Reserve Bank of St Louis Consumer price index for all urban consumers: medical care. https://fred.stlouisfed.org/series/CPIMEDSL#0. Accessed December 3, 2019.
- 28.United States Census Bureau Historical income tables: households. https://www.census.gov/data/tables/time-series/demo/income-poverty/historical-income-households.html. Accessed May 5, 2019.
- 29.Karaca-Mandic P, Choi-Yoo SJ, Lee J, Scal P. Family out-of-pocket health care burden and children’s unmet needs or delayed health care. Acad Pediatr. 2014;14(1):101-108. doi: 10.1016/j.acap.2013.10.005 [DOI] [PubMed] [Google Scholar]
- 30.Sen B, Blackburn J, Morrisey MA, et al. Did copayment changes reduce health service utilization among CHIP enrollees? evidence from Alabama. Health Serv Res. 2012;47(4):1603-1620. doi: 10.1111/j.1475-6773.2012.01384.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Trivedi AN, Moloo H, Mor V. Increased ambulatory care copayments and hospitalizations among the elderly. N Engl J Med. 2010;362(4):320-328. doi: 10.1056/NEJMsa0904533 [DOI] [PubMed] [Google Scholar]
- 32.Cecil WT, Barnes J, Shea T, Coulter SL. Relationship of the use and costs of physician office visits and prescription drugs to travel distance and increases in member cost share. J Manag Care Pharm. 2006;12(8):665-676. doi: 10.18553/jmcp.2006.12.8.665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Miller S, Wherry LR. Health and access to care during the first 2 years of the ACA Medicaid expansions. N Engl J Med. 2017;376(10):947-956. doi: 10.1056/NEJMsa1612890 [DOI] [PubMed] [Google Scholar]
- 34.Tong S, Amand C, Kieffer A, Kyaw MH. Trends in healthcare utilization and costs associated with acute otitis media in the United States during 2008-2014. BMC Health Serv Res. 2018;18(1):318. doi: 10.1186/s12913-018-3139-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Marom T, Tan A, Wilkinson GS, Pierson KS, Freeman JL, Chonmaitree T. Trends in otitis media-related health care use in the United States, 2001-2011. JAMA Pediatr. 2014;168(1):68-75. doi: 10.1001/jamapediatrics.2013.3924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Finkelstein JA, Raebel MA, Nordin JD, Lakoma M, Young JG. Trends in outpatient antibiotic use in 3 health plans. Pediatrics. 2019;143(1):e20181259. doi: 10.1542/peds.2018-1259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vaz LE, Kleinman KP, Raebel MA, et al. Recent trends in outpatient antibiotic use in children. Pediatrics. 2014;133(3):375-385. doi: 10.1542/peds.2013-2903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Greene SK, Kleinman KP, Lakoma MD, et al. Trends in antibiotic use in Massachusetts children, 2000-2009. Pediatrics. 2012;130(1):15-22. doi: 10.1542/peds.2011-3137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Grijalva CG, Nuorti JP, Griffin MR. Antibiotic prescription rates for acute respiratory tract infections in US ambulatory settings. JAMA. 2009;302(7):758-766. doi: 10.1001/jama.2009.1163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lieberthal AS, Carroll AE, Chonmaitree T, et al. The diagnosis and management of acute otitis media. Pediatrics. 2013;131(3):e964-e999. doi: 10.1542/peds.2012-3488 [DOI] [PubMed] [Google Scholar]
- 41.Zetts RM, Stoesz A, Smith BA, Hyun DY. Outpatient antibiotic use and the need for increased antibiotic stewardship efforts. Pediatrics. 2018;141(6):e20174124. doi: 10.1542/peds.2017-4124 [DOI] [PubMed] [Google Scholar]
- 42.Gerber JS, Prasad PA, Fiks AG, et al. Effect of an outpatient antimicrobial stewardship intervention on broad-spectrum antibiotic prescribing by primary care pediatricians: a randomized trial. JAMA. 2013;309(22):2345-2352. doi: 10.1001/jama.2013.6287 [DOI] [PubMed] [Google Scholar]
- 43.Zuckerman KE, Mattox KM, Sinche BK, Blaschke GS. Disparities in family health-related internet and email use in the general pediatrics setting. Clin Pediatr (Phila). 2014;53(13):1295-1298. doi: 10.1177/0009922814540203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Demirci JR, Cohen SM, Parker M, Holmes A, Bogen DL. Access, use, and preferences for technology-based perinatal and breastfeeding support among childbearing women. J Perinat Educ. 2016;25(1):29-36. doi: 10.1891/1058-1243.25.1.29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Laws R, Walsh AD, Hesketh KD, Downing KL, Kuswara K, Campbell KJ. Differences between mothers and fathers of young children in their use of the internet to support healthy family lifestyle behaviors: cross-sectional study. J Med Internet Res. 2019;21(1):e11454. doi: 10.2196/11454 [DOI] [PMC free article] [PubMed] [Google Scholar]