Abstract
This cross-sectional study uses nationally representative urine drug test data to analyze changes in positivity rates for methamphetamine, cocaine, heroin, and fentanyl.
Introduction
The US Centers for Disease Control and Prevention recently projected that the number of drug overdose deaths would total approximately 68 000 in 2018, down from 71 000 deaths in 2017.1 This represents the first reported decline since 1990 and is largely attributed to a decrease in deaths involving prescription opioids. However, deaths associated with synthetic opioids, primarily fentanyl, as well as stimulants appear to be increasing.1 In 2019,2 we reported a 798% increase in urine drug test (UDT) positivity rates for nonprescribed fentanyl among results positive for methamphetamine and an 1850% increase among results positive for cocaine. In an effort to conduct ongoing surveillance of the polysubstance use landscape and help characterize these evolving trends in a more timely manner, we examined our UDT data as close to real-time as possible to observe trends in positivity for methamphetamine, cocaine, and heroin, with and without illicit fentanyl. We hypothesize that UDT data are closely aligned with the Centers for Disease Control and Prevention’s overdose death data and the US Drug Enforcement Administration’s drug confiscations data and may have the potential to more quickly inform public health safety officials of possible shifts in these trends.3
Methods
This study’s protocol was approved by the Aspire Independent Review Board and includes a waiver of consent for the use of deidentified data. We conducted a cross-sectional study of UDT results from 1 050 000 unique patient urine specimens submitted for testing by health care professionals as part of routine care from January 1, 2013, to October 31, 2019. The analysis used definitive UDT results performed by liquid chromatography–tandem mass spectrometry for methamphetamine, cocaine, heroin, and fentanyl. Patient specimens were randomly selected from the entire study period with equal specimen numbers per year. Specimens from patients reported to have been prescribed methamphetamine, cocaine, or fentanyl were excluded.
Analyte positivity rates and 95% binomial CIs were calculated for the total sample population and the subpopulation whose results were positive for fentanyl and also positive for methamphetamine, cocaine, or heroin. A 2-sample proportion test was used to evaluate positivity rate changes. R statistical software version 3.5.0 (R Project for Statistical Computing) was used for data analysis. Statistical significance was set at P less than .05, and all tests were 2-tailed. Data analyses were conducted November 1 through 7, 2019. This study is reported following Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Results
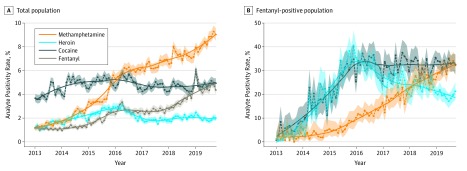
The total sample included UDT results from 1 050 000 unique patients, including 558 111 women (53.2%), and the median (interquartile range) age was 45 (20-70) years, with patients from all 50 US states and multiple health care specialties (Table). From 2013 to 2019, the positivity rate for methamphetamine increased from 1.43% (95% CI, 1.37%-1.49%) to 8.39% (95% CI, 8.25%-8.53%), a 486.71% increase (P < .001); the cocaine positivity rate increased from 4.09% (95% CI, 3.99%-4.19%) to 4.94% (95% CI, 4.83%-5.05%), a 20.78% increase (P < .001); the heroin positivity rate increased from 1.41% (95% CI, 1.35%-1.48%) to 1.99% (95% CI, 1.92%-2.06%), a 41.13% increase (P < .001); and the fentanyl positivity rate increased from 1.09% (95% CI, 1.04%-1.15%) to 4.72% (95% CI, 4.62%-4.83%), a 333.03% increase (P < .001) (Table and Figure, A).
Table. Characteristics of Urine Specimens Tested for Methamphetamine, Cocaine, Heroin, and Fentanyl Between January 1, 2013, and October 31, 2019.
| Characteristic | Specimens Tested, No. (%) | Positivity Rate, % (95% CI) | |||
|---|---|---|---|---|---|
| Methamphetamine | Cocaine | Heroin | Fentanyl | ||
| Unique patients, No. | 1 050 000 | ||||
| Age, median (IQR), y | 45 (20-70) | ||||
| Sex | |||||
| Men | 489 957 (46.66) | 5.48 (5.42-5.55) | 5.73 (5.66-5.79) | 2.49 (2.45-2.54) | 2.75 (2.70-2.80) |
| Women | 558 111 (53.15) | 4.65 (4.59-4.70) | 3.9 (3.85-3.95) | 1.62 (1.59-1.66) | 2.3 (2.26-2.34) |
| Specialty of the referring health care practice | |||||
| Substance use disorder | 238 036 (22.67) | 10.82 (10.69-10.94) | 9.59 (9.48-9.71) | 5.26 (5.17-5.35) | 5.94 (5.85-6.04) |
| Pain management | 349 097 (33.25) | 1.40 (1.36-1.44) | 2.37 (2.32-2.43) | 0.56 (0.53-0.58) | 1.32 (1.29-1.36) |
| Primary care | 239 382 (22.80) | 3.57 (3.50-3.64) | 3.89 (3.81-3.97) | 1.36 (1.31-1.41) | 1.28 (1.23-1.32) |
| Behavioral health | 139 137 (13.25) | 7.69 (7.55-7.83) | 5.00 (4.88-5.11) | 1.94 (1.87-2.02) | 2.16 (2.08-2.24) |
| Obstetrics and gynecology | 18 468 (1.76) | 2.38 (2.17-2.61) | 1.87 (1.68-2.07) | 1.16 (1.01-1.33) | 0.53 (0.43-0.65) |
| Multispecialty or other | 65 880 (6.27) | 4.07 (3.92-4.22) | 3.39 (3.25-3.53) | 1.11 (1.03-1.19) | 2.33 (2.22-2.45) |
| Total sample population | |||||
| 2013 | 150 000 (14.29) | 1.43 (1.37-1.49) | 4.09 (3.99-4.19) | 1.41 (1.35-1.48) | 1.09 (1.04-1.15) |
| 2014 | 150 000 (14.29) | 2.22 (2.14-2.29) | 4.88 (4.77-4.99) | 1.97 (1.90-2.04) | 1.20 (1.15-1.26) |
| 2015 | 150 000 (14.29) | 3.71 (3.62-3.81) | 5.10 (4.99-5.22) | 2.53 (2.45-2.61) | 1.93 (1.86-2.00) |
| 2016 | 150 000 (14.29) | 5.89 (5.78-6.01) | 5.13 (5.02-5.25) | 2.54 (2.46-2.62) | 2.69 (2.61-2.78) |
| 2017 | 150 000 (14.29) | 6.46 (6.34-6.59) | 4.60 (4.49-4.70) | 1.79 (1.72-1.86) | 2.60 (2.52-2.68) |
| 2018 | 150 000 (14.29) | 7.22 (7.09-7.35) | 4.57 (4.47-4.68) | 2.02 (1.95-2.09) | 3.40 (3.31-3.50) |
| 2019a | 150 000 (14.29) | 8.39 (8.25-8.53) | 4.94 (4.83-5.05) | 1.99 (1.92-2.06) | 4.72 (4.62-4.83) |
| Total | 1 050 000 (100) | 5.05 (5.01-5.09) | 4.76 (4.72-4.8) | 2.03 (2.01-2.06) | 2.52 (2.49-2.55) |
| 2013-2019 Change, % | 486.71 | 20.78 | 41.13 | 333.03 | |
| P valueb | <.001 | <.001 | <.001 | <.001 | |
| 2016-2019 Change, % | 42.44 | −3.70 | −21.65 | 75.46 | |
| P valueb | <.001 | .01 | <.001 | <.001 | |
| Fentanyl-positive population | |||||
| 2013 | 1638 (6.19) | 2.20 (1.54-3.03) | 5.31 (4.28-6.51) | 2.99 (2.22-3.94) | NA |
| 2014 | 1804 (6.82) | 3.05 (2.30-3.95) | 15.47 (13.83-17.22) | 14.91 (13.30-16.64) | NA |
| 2015 | 2895 (10.94) | 6.18 (5.33-7.12) | 27.29 (25.67-28.95) | 29.29 (27.64-30.99) | NA |
| 2016 | 4039 (15.26) | 11.98 (11.00-13.02) | 33.45 (31.99-34.93) | 31.74 (30.31-33.20) | NA |
| 2017 | 3896 (14.72) | 18.35 (17.15-19.60) | 31.93 (30.47-33.42) | 25.39 (24.02-26.78) | NA |
| 2018 | 5105 (19.29) | 25.99 (24.80-27.22) | 31.17 (29.90-32.46) | 23.25 (22.10-24.44) | NA |
| 2019a | 7086 (26.78) | 30.37 (29.30-31.46) | 33.47 (32.38-34.59) | 19.64 (18.72-20.59) | NA |
| Total | 26 463 (100) | 18.70 (18.23-19.17) | 29.15 (28.60-29.70) | 22.73 (22.23-23.24) | NA |
| 2013-2019 Change, % | 1280.45 | 530.32 | 556.86 | NA | |
| P valueb | <.001 | <.001 | <.001 | ||
| 2016-2019 Change, % | 153.51 | 0.06 | −38.12 | NA | |
| P valueb | <.001 | >.99 | <.001 | ||
Abbreviations: IQR, interquartile range; NA, not applicable.
The 2019 data are restricted to January 1 to October 31, 2019.
A 2-sample proportion test (Z test) with continuity correction was used to calculate P values.
Figure. Analyte Positivity Rates .
Positivity rates were calculated at 1-month intervals over the study period for the entire sample population (A) and for a subset of the sample population with urine drug test results positive for fentanyl and methamphetamine, cocaine, or heroin (B). Dots indicate point estimates; shaded areas, binomial 95% CIs; line, Loess smoothing curve with a span of 0.5.
In 2016, positivity rates peaked for cocaine (5.13% [95% CI, 5.02%-5.25%]) and heroin (2.54% [95% CI, 2.46%-2.62%]); by 2019, the cocaine positivity rate declined by 3.70% (P = .01) and the heroin positivity rate declined by 21.65% (P < .001). In contrast, the 2016 positivity rates for methamphetamine (5.89% [95% CI, 5.78%-6.01%]) and fentanyl (2.69% [95% CI, 2.61%-2.78%) have continued to increase, by 42.44% for methamphetamine (P < .001) and by 75.46% for fentanyl (P < .001) (Table and Figure, A).
Among UDT results positive for fentanyl, the positivity rates of co-occurring methamphetamine, cocaine, and heroin have increased since 2013. (Table and Figure, B). From 2013 to 2019, positivity rates increased by 1280.45% for methamphetamine (2.20% [95% CI, 1.54%-3.03%] vs 30.37 [95% CI, 29.30%-31.46%]; P < .001), 530.32% for cocaine (5.31% [95% CI, 4.28%-6.51%] vs 33.47% [95% CI, 32.38%-34.59%]; P < .001), and 556.86% for heroin (2.99% [95% CI, 2.22%-3.94%] vs 19.64% [95% CI, 18.72%-20.59%]; P < .001). Methamphetamine positivity rates from 2016 (11.98% [95% CI, 11.00%-13.02%]) continued to increase in the fentanyl-positive sample by 153.51% (P < .001). Compared with 2019, the cocaine positivity rate within this sample did not significantly increase from the 2016 rate of 33.45% (95% CI, 31.99%-34.93%), a rate change of only 0.06%, but the heroin positivity rate decreased significantly from the 2016 rate of 31.74% (95% CI, 30.31 to 33.20), a difference of 38.12% (P < .001).
Discussion
This cross-sectional study found that an increasing number of UDT results were positive for methamphetamine from 2013 to 2019, with and without illicit fentanyl, suggesting that methamphetamine-related overdose deaths may continue to increase. However, this study has limitations. Data are limited to specimens collected in a health care setting and may not reflect the general population. Individuals included in the analysis may have had an incomplete or inaccurate medication list. Nonetheless, nontraditional data sources, including UDTs, may provide a more timely estimation of emerging drug use prior to the reporting of drug overdose deaths. Earlier identification of these trends supports the development of targeted interventions to curb the effect of drug abuse on public health.
References
- 1.Ahmad FB, Escobedo LA, Rossen LM, Spencer MR, Warner M, Sutton P; National Center for Health Statistics . Provisional drug overdose death counts. https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm. Accessed November 19, 2019.
- 2.LaRue L, Twillman RK, Dawson E, et al. Rate of fentanyl positivity among urine drug test results positive for cocaine or methamphetamine. JAMA Netw Open. 2019;2(4):e192851. doi: 10.1001/jamanetworkopen.2019.2851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.US Drug Enforcement Administration, Diversion Control Division . National Forensic Laboratory Information System: NFLIS-Drug 2018 annual report. https://www.nflis.deadiversion.usdoj.gov/DesktopModules/ReportDownloads/Reports/NFLIS-Drug-AR2018.pdf. Accessed November 19, 2019.