Abstract
Background
Post‐traumatic stress disorder (PTSD) is a distressing condition, which is often treated with psychological therapies. Earlier versions of this review, and other meta‐analyses, have found these to be effective, with trauma‐focused treatments being more effective than non‐trauma‐focused treatments. This is an update of a Cochrane review first published in 2005 and updated in 2007.
Objectives
To assess the effects of psychological therapies for the treatment of adults with chronic post‐traumatic stress disorder (PTSD).
Search methods
For this update, we searched the Cochrane Depression, Anxiety and Neurosis Group's Specialised Register (CCDANCTR‐Studies and CCDANCTR‐References) all years to 12th April 2013. This register contains relevant randomised controlled trials from: The Cochrane Library (all years), MEDLINE (1950 to date), EMBASE (1974 to date), and PsycINFO (1967 to date). In addition, we handsearched the Journal of Traumatic Stress, contacted experts in the field, searched bibliographies of included studies, and performed citation searches of identified articles.
Selection criteria
Randomised controlled trials of individual trauma‐focused cognitive behavioural therapy (TFCBT), eye movement desensitisation and reprocessing (EMDR), non‐trauma‐focused CBT (non‐TFCBT), other therapies (supportive therapy, non‐directive counselling, psychodynamic therapy and present‐centred therapy), group TFCBT, or group non‐TFCBT, compared to one another or to a waitlist or usual care group for the treatment of chronic PTSD. The primary outcome measure was the severity of clinician‐rated traumatic‐stress symptoms.
Data collection and analysis
We extracted data and entered them into Review Manager 5 software. We contacted authors to obtain missing data. Two review authors independently performed 'Risk of bias' assessments. We pooled the data where appropriate, and analysed for summary effects.
Main results
We include 70 studies involving a total of 4761 participants in the review. The first primary outcome for this review was reduction in the severity of PTSD symptoms, using a standardised measure rated by a clinician. For this outcome, individual TFCBT and EMDR were more effective than waitlist/usual care (standardised mean difference (SMD) ‐1.62; 95% CI ‐2.03 to ‐1.21; 28 studies; n = 1256 and SMD ‐1.17; 95% CI ‐2.04 to ‐0.30; 6 studies; n = 183 respectively). There was no statistically significant difference between individual TFCBT, EMDR and Stress Management (SM) immediately post‐treatment although there was some evidence that individual TFCBT and EMDR were superior to non‐TFCBT at follow‐up, and that individual TFCBT, EMDR and non‐TFCBT were more effective than other therapies. Non‐TFCBT was more effective than waitlist/usual care and other therapies. Other therapies were superior to waitlist/usual care control as was group TFCBT. There was some evidence of greater drop‐out (the second primary outcome for this review) in active treatment groups. Many of the studies were rated as being at 'high' or 'unclear' risk of bias in multiple domains, and there was considerable unexplained heterogeneity; in addition, we assessed the quality of the evidence for each comparison as very low. As such, the findings of this review should be interpreted with caution.
Authors' conclusions
The evidence for each of the comparisons made in this review was assessed as very low quality. This evidence showed that individual TFCBT and EMDR did better than waitlist/usual care in reducing clinician‐assessed PTSD symptoms. There was evidence that individual TFCBT, EMDR and non‐TFCBT are equally effective immediately post‐treatment in the treatment of PTSD. There was some evidence that TFCBT and EMDR are superior to non‐TFCBT between one to four months following treatment, and also that individual TFCBT, EMDR and non‐TFCBT are more effective than other therapies. There was evidence of greater drop‐out in active treatment groups. Although a substantial number of studies were included in the review, the conclusions are compromised by methodological issues evident in some. Sample sizes were small, and it is apparent that many of the studies were underpowered. There were limited follow‐up data, which compromises conclusions regarding the long‐term effects of psychological treatment.
Keywords: Adult; Humans; Behavior Therapy; Behavior Therapy/methods; Chronic Disease; Cognitive Behavioral Therapy; Cognitive Behavioral Therapy/methods; Psychotherapy; Psychotherapy/methods; Psychotherapy, Group; Randomized Controlled Trials as Topic; Stress Disorders, Post‐Traumatic; Stress Disorders, Post‐Traumatic/psychology; Stress Disorders, Post‐Traumatic/therapy
Plain language summary
Psychological therapies for chronic post‐traumatic stress disorder (PTSD) in adults
Background: Post‐traumatic stress disorder (PTSD) can occur following a traumatic event. It is characterised by symptoms of re‐experiencing the trauma (in the form of nightmares, flashbacks and distressing thoughts), avoiding reminders of the traumatic event, negative alterations in thoughts and mood, and symptoms of hyper‐arousal (feeling on edge, being easily startled, feeling angry, having difficulties sleeping, and problems concentrating).
Previous reviews have supported the use of individual trauma‐focused cognitive behavioural therapy (TFCBT) and eye movement desensitisation and reprocessing (EMDR) in the treatment of PTSD. TFCBT is a variant of cognitive behavioural therapy (CBT), which includes a number of techniques to help a person overcome a traumatic event. It is a combination of cognitive therapy aimed at changing the way a person thinks, and behavioural therapy, which aims to change the way a person acts. TFCBT helps an individual come to terms with a trauma through exposure to memories of the event. EMDR is a psychological therapy, which aims to help a person reprocess their memories of a traumatic event. The therapy involves bringing distressing trauma‐related images, beliefs, and bodily sensations to mind, whilst the therapist guides eye movements from side to side. More positive views of the trauma memories are identified, with the aim of replacing the ones that are causing problems.
TFCBT and EMDR are currently recommended as the treatments of choice by guidelines such as those published by the United Kingdom's National Institute of Health and Clinical Excellence (NICE).
Study characteristics: This review draws together up‐to‐date evidence from 70 studies including a total of 4761 people.
Key findings: There is continued support for the efficacy of individual TFCBT, EMDR, non‐TFCBT and group TFCBT in the treatment of chronic PTSD in adults. Other non‐trauma‐focused psychological therapies did not reduce PTSD symptoms as significantly. There was evidence that individual TFCBT, EMDR and non‐TFCBT are equally effective immediately post‐treatment in the treatment of PTSD. There was some evidence that TFCBT and EMDR are superior to non‐TFCBT between one to four months following treatment, and also that individual TFCBT, EMDR and non‐TFCBT are more effective than other therapies. No specific conflicts of interest were identified.
Quality of the evidence: Although we included a substantial number of studies in this review, each only included small numbers of people and some were poorly designed. We assessed the overall quality of the studies as very low and so the findings of this review should be interpreted with caution. There is insufficient evidence to show whether or not psychological therapy is harmful.
Summary of findings
Summary of findings for the main comparison. Trauma‐focused CBT/Exposure therapy compared with Waitlist/Usual Care for chronic post‐traumatic stress disorder (PTSD) in adults.
| Trauma‐focused CBT/Exposure therapy versus Waitlist/Usual Care | ||||||
| Patient or population: Adults with PTSD for at least 3 months Settings: Primary care, community, outpatient Intervention: Trauma‐focused CBT/Exposure Therapy | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Trauma Focused CBT/ Exposure Therapy | |||||
| Severity of PTSD symptoms ‐ Clinician‐rated | The mean severity of PTSD symptoms ‐ clinician‐rated in the intervention groups was | 1.62 standard deviations lower (2.03 to 1.21 lower) | 1256 (28 studies) | ⊕⊝⊝⊝ very low1,2,3 | ||
| Leaving the study early for any reason | Study population | RR 1.64 (1.30 to 2.06) | 1756 (33 studies) | ⊕⊝⊝⊝ very low1,2,3 | ||
| 130 per 1000 | 189 per 1000 (150 to 240) | |||||
| Moderate | ||||||
| 85 per 1000 | 124 per 1000 (99 to 157) | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1Some studies were judged to pose a high risk of bias 2Unexplained heterogeneity 3Small sample sizes
Summary of findings 2. Trauma‐focused CBT/Exposure therapy compared with non‐TFCBT for chronic post‐traumatic stress disorder (PTSD) in adults.
| Trauma‐focused CBT/Exposure therapy compared with non‐TFCBT for chronic post‐traumatic stress disorder (PTSD) in adults | ||||||
| Patient or population: Adults with PTSD for at least 3 months Settings: Primary care, community, outpatient Intervention: Trauma‐focused CBT/Exposure therapy Comparison: non‐Trauma‐focused CBT | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Non‐TFCBT | Trauma Focused CBT/ Exposure Therapy | |||||
| Severity of PTSD Symptoms ‐ Clinician‐rated | The mean severity of PTSD symptoms ‐ clinician‐rated in the intervention groups was 0.27 standard deviations lower (0.63 lower to 0.10 higher) | 267 (7 studies) | ⊕⊝⊝⊝ very low1,2 | |||
| Leaving the study early for any reason | Study population | RR 1.19 (0.71 to 2.00) | 312 (7 studies) | ⊕⊝⊝⊝ very low1,2,3 | ||
| 154 per 1000 | 183 per 1000 (109 to 308) | |||||
| Moderate | ||||||
| 154 per 1000 | 183 per 1000 (109 to 308) | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1Some studies were judged to pose a high risk of bias 2Unexplained heterogeneity 3Small sample sizes
Summary of findings 3. Trauma‐focused CBT/Exposure therapy compared with other therapies for chronic post‐traumatic stress disorder (PTSD) in adults.
| Trauma‐focused CBT/Exposure therapy compared with other therapies for chronic post‐traumatic stress disorder (PTSD) in adults | ||||||
| Patient or population: Adults with PTSD for at least 3 months Settings: Primary care, community, outpatient Intervention: Trauma‐focused CBT/Exposure therapy Comparison: other therapies | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Other Therapies | Trauma Focused CBT/Exposure Therapy | |||||
| Severity of PTSD symptoms ‐ Clinician‐rated | The mean severity of PTSD symptoms ‐ clinician in the intervention groups was | ‐0.48 standard deviations lower (‐0.83 to ‐0.43 lower) | 612 (10 studies) | ⊕⊝⊝⊝ very low1,2,3 | ||
| Leaving the study early for any reason | Study population | RR 1.39 (1.01 to 1.92) | 762 (11 studies) | ⊕⊝⊝⊝ very low1,2,3 | ||
| 142 per 1000 | 198 per 1000 (144 to 274) | |||||
| Moderate | ||||||
| 138 per 1000 | 192 per 1000 (139 to 265) | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1Some studies were judged to pose a high risk of bias 2Unexplained heterogeneity 3Small sample sizes
Summary of findings 4. EMDR compared with Waitlist/Usual Care for chronic post‐traumatic stress disorder (PTSD) in adults.
| EMDR compared with Waitlist/Usual Care for chronic post‐traumatic stress disorder (PTSD) in adults | ||||||
| Patient or population: Adults with PTSD for at least 3 months Settings: Primary care, community, outpatient Intervention: Eye movement desensitization and reprocessing (EMDR) Comparison: Waitlist/Usual Care | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Waitlist/Usual Care | EMDR | |||||
| Severity of PTSD symptoms ‐ Clinician‐rated | The mean severity of PTSD symptoms ‐ clinician in the intervention groups was | 1.17 standard deviations lower (2.04 to 0.30 lower) | 183 (6 studies) | ⊕⊝⊝⊝ very low1,2,3 | ||
| Leaving study early for any reason | Study population | RR 1.05 (0.62 to 1.79) | 227 (7 studies) | ⊕⊝⊝⊝ very low1,3 | ||
| 178 per 1000 | 188 per 1000 (104 to 313) | |||||
| Moderate | ||||||
| 172 per 1000 | 182 per 1000 (101 to 305) | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: risk ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1Some studies were judged to pose a high risk of bias 2Unexplained heterogeneity 3Small sample sizes
Summary of findings 5. EMDR compared with Trauma‐focused CBT for chronic post‐traumatic stress disorder (PTSD) in adults.
| EMDR compared with Trauma‐focused CBT for chronic post‐traumatic stress disorder (PTSD) in adults | ||||||
| Patient or population: Adults with PTSD for at least 3 months Settings: Primary care, community, outpatient Intervention: Eye movement desensitization and reprocessing (EMDR) Comparison: Trauma‐focused CBT | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Trauma Focused CBT | EMDR | |||||
| Severity of PTSD symptoms ‐ Clinician‐rated | The mean severity of PTSD symptoms ‐ clinician in the intervention groups was | 0.03 standard deviations lower (0.43 lower to 0.38 higher) | 327 (7 studies) | ⊕⊝⊝⊝ very low1,2,3 | ||
| Leaving study early for any reason | Study population | RR 1.00 (0.74 to 1.35) | 400 (8 studies) | ⊕⊝⊝⊝ very low1,2,3 | ||
| 279 per 1000 | 268 per 1000 (191 to 367) | |||||
| Moderate | ||||||
| 257 per 1000 | 247 per 1000 (174 to 342) | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: risk ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1Some studies were judged as posing a high risk of bias 2Unexplained heterogeneity 3Small sample sizes
Summary of findings 6. EMDR compared with non‐TFCBT for chronic post‐traumatic stress disorder (PTSD) in adults.
| EMDR compared with non‐TFCBT for chronic post‐traumatic stress disorder (PTSD) in adults | ||||||
| Patient or population: Adults with PTSD for at least 3 months Settings: Primary care, community, outpatient Intervention: Eye movement desensitization and reprocessing (EMDR) Comparison: non‐trauma‐focused CBT | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Non‐TFCBT | EMDR | |||||
| Severity of PTSD symptoms ‐ Clinician‐rated | The mean severity of PTSD symptoms ‐ clinician in the intervention groups was | 0.35 standard deviations lower (0.90 lower to 0.19 higher) | 53 (2 studies) | ⊕⊝⊝⊝ very low1,2 | ||
| Leaving the study early for any reason | Study population | RR 1.03 (0.37 to 2.88) | 84 (3 studies) | ⊕⊝⊝⊝ very low1,2 | ||
| 140 per 1000 | 144 per 1000 (46 to 367) | |||||
| Moderate | ||||||
| 91 per 1000 | 94 per 1000 (29 to 264) | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: risk ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1Studies reported insufficient information to judge risk of bias 2Small sample sizes. Only two studies.
Summary of findings 7. EMDR compared with other therapies for chronic post‐traumatic stress disorder (PTSD) in adults.
| EMDR compared with other therapies for chronic post‐traumatic stress disorder (PTSD) in adults | ||||||
| Patient or population: Adults with PTSD for at least 3 months Settings: Primary care, community, outpatient Intervention: Eye movement desensitization and reprocessing (EMDR) Comparison: other therapies | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Other Therapies | EMDR | |||||
| Leaving study early for any reason | Study population | RR 1.48 (0.26 to 8.54) | 127 (2 studies) | ⊕⊝⊝⊝ very low1,2 | ||
| 32 per 1000 | 47 per 1000 (8 to 234) | |||||
| Moderate | ||||||
| 32 per 1000 | 48 per 1000 (8 to 236) | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: risk ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1One study was judged to pose a high risk of bias. The other study reported insufficient information for a judgement to be made 2Only two studies. Small sample sizes
Summary of findings 8. Non‐TFCBT compared with Waitlist/Usual Care for chronic post‐traumatic stress disorder (PTSD) in adults.
| Non‐TFCBT compared with Waitlist/Usual Care for chronic post‐traumatic stress disorder (PTSD) in adults | ||||||
| Patient or population: Adults with PTSD for at least 3 months Settings: Primary care, community, outpatient Intervention: non‐trauma‐focused CBT Comparison: Waitlist/Usual Care | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Waitlist/Usual Care | Non‐TFCBT Therapy | |||||
| Severity of PTSD symptoms ‐ Clinician‐rated | The mean severity of PTSD symptoms ‐ clinician in the intervention groups was 1.22 standard deviations lower (1.76 to 0.69 lower) | 106 (4 studies) | ⊕⊝⊝⊝ very low1,2,3 | |||
| Leaving the study early due to any reason | Study population | RR 1.96 (0.70 to 5.48) | 141 (5 studies) | ⊕⊝⊝⊝ very low1,2,3 | ||
| 78 per 1000 | 153 per 1000 (55 to 428) | |||||
| Moderate | ||||||
| 83 per 1000 | 163 per 1000 (58 to 455) | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1Insufficient data to judge risk of bias 2Unexplained heterogeneity 3Small sample sizes
Summary of findings 9. Non‐TFCBT compared with other therapies for chronic post‐traumatic stress disorder (PTSD) in adults.
| Non‐TFCBT compared with other therapies for chronic post‐traumatic stress disorder (PTSD) | ||||||
| Patient or population: Adults with PTSD for at least 3 months Settings: Primary care, community, outpatient Intervention: non‐trauma‐focused CBT Comparison: other therapies | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Non‐TFCBT | ||||||
| Severity of PTSD symptoms ‐ Clincian‐rated | See comment | See comment | Not estimable | 25 (1 study) | ⊕⊝⊝⊝ very low1,2,3 | |
| Leaving the study early for any reason | See comment | See comment | Not estimable | 31 (1 study) | ⊕⊝⊝⊝ very low1,2,3 | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1Some studies were judged to pose a high risk of bias 2Unexplained heterogeneity 3Small sample sizes
Summary of findings 10. Group TFCBT compared with Waitlist/Usual Care for chronic post‐traumatic stress disorder (PTSD) in adults.
| Group TFCBT compared with Waitlist/Usual Care for chronic post‐traumatic stress disorder (PTSD) | ||||||
| Patient or population: Adults with PTSD for at least 3 months Settings: Primary care, community, outpatient Intervention: Group TFCBT Comparison: Waitlist/Usual Care/Minimal Contact | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Group TFCBT | ||||||
| Severity of PTSD symptoms ‐ Clinician‐rated | The mean severity of PTSD symptoms ‐ clinician in the intervention groups was 1.28 standard deviations lower (2.25 to 0.31 lower) | 185 (3 studies) | ⊕⊝⊝⊝ very low1,2,3 | |||
| Leaving the study early for any reason | Study population | RR 1.21 (0.94 to 1.55) | 573 (7 studies) | ⊕⊝⊝⊝ very low1,2,3 | ||
| 262 per 1000 | 317 per 1000 (246 to 406) | |||||
| Moderate | ||||||
| 200 per 1000 | 242 per 1000 (188 to 310) | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1Insufficient information to judge risk of bias 2Unexplained heterogeneity 3Small sample sizes
Summary of findings 11. Group TFCBT compared with Group non‐TFCBT for chronic post‐traumatic stress disorder (PTSD) in adults.
| Group CBT (trauma focused) compared with Group CBT (non‐trauma focused) for chronic post‐traumatic stress disorder (PTSD) in adults | ||||||
| Patient or population: Adults with PTSD for at least 3 months Settings: Primary care, community, outpatient Intervention: Group TFCBT Comparison: Group non‐TFCBT | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Group CBT (non‐trauma focused) | Group CBT (trauma focused) | |||||
| Severity of PTSD symptoms ‐ Clinician‐rated | See comment | See comment | Not estimable | 325 (1 study) | ⊕⊝⊝⊝ very low1,2 | |
| Leaving the study early for any reason | See comment | See comment | Not estimable | 360 (1 study) | ⊕⊝⊝⊝ very low1,2 | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1Insufficient information to judge risk of bias 2One study with a small sample size
Summary of findings 12. Other therapies compared with Waitlist/Usual Care for chronic post‐traumatic stress disorder (PTSD) in adults.
| Other therapies compared with Waitlist/Usual Care for chronic post‐traumatic stress disorder (PTSD) in adults | ||||||
| Patient or population: Adults with PTSD for at least 3 months Settings: Primary care, community, outpatient Intervention: Other therapies Comparison: Waitlist/Usual Care | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Waitlist/Usual Care | Other therapies | |||||
| Severity of PTSD symptoms ‐ Clinician | The mean severity of PTSD symptoms ‐ clinician in the intervention groups was 0.58 standard deviations lower (0.96 to 0.20 lower) | 112 (3 studies) | ⊕⊝⊝⊝ very low1 | |||
| Leaving the study early due to any reason | Study population | RR 2.45 (0.99 to 6.10) | 211 (4 studies) | ⊕⊝⊝⊝ very low1,2 | ||
| 74 per 1000 | 181 per 1000 (73 to 452) | |||||
| Moderate | ||||||
| 72 per 1000 | 176 per 1000 (71 to 439) | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1Small sample sizes 2Studies were judged to pose a low/unclear risk of bias
Summary of findings 13. Group non‐TFCBT compared with Waitlist/Usual Care for chronic post‐traumatic stress disorder (PTSD) in adults.
| Group non‐TFCBT compared to Waitlist/Usual Care for chronic post‐traumatic stress disorder (PTSD) in adults | ||||||
| Patient or population: Adults with PTSD for at least 3 months Settings: Primary care, community, outpatient Intervention: Group non‐TFCBT Comparison: Waitlist/Usual Care | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Waitlist/Usual Care | Group nonTFCBT | |||||
| Leaving the study early for any reason | See comment | See comment | Not estimable | 47 (1 study) | ⊕⊝⊝⊝ very low1,2 | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1Only one study. Risk of bias high/unclear in several domains. 2Only one study
Background
Description of the condition
Post‐traumatic stress disorder (PTSD) is a well recognised psychiatric disorder that occurs following a major traumatic event. Characteristic symptoms include re‐experiencing phenomena such as nightmares and recurrent distressing thoughts of the event, avoidance of talking or being reminded of the traumatic event, negative alterations in thoughts and mood, and hyperarousal symptoms including sleep disturbance, increased irritability and hypervigilance. PTSD can be diagnosed after a one‐month duration of symptoms. The condition is considered chronic once symptoms have been present for three months. PTSD is a relatively common condition. The National Co‐morbidity Survey (Kessler 1995) found that 7.8% of 5877 American adults had suffered from PTSD at some time in their lives. When data were examined from individuals who had been exposed to a traumatic event, rates of PTSD varied according to the type of stressor. For example, physical assaults amongst women led to a lifetime prevalence of 29% and combat experience amongst men to a lifetime prevalence of 39%.
Description of the intervention
Psychological therapies have been advocated as being effective in the treatment of PTSD since its conception. Various forms of psychological therapy have been used including exposure therapy (Creamer 2004), cognitive therapy (Ehlers 2005; Resick 1992), psychodynamic psychotherapy (Brom 1989) and eye movement desensitisation and reprocessing (EMDR) (Shapiro 1989b). Exposure therapy usually involves asking the participant to relive the trauma imaginally. This is often done by creating a detailed present tense account of exactly what happened, making an audio tape recording or transcript of it and asking the individual to listen to/read this over and over again. Another form of exposure therapy involves exposing participants to cues associated with the traumatic event (for example, graded re‐exposure to car travel following a road traffic accident). Trauma‐focused cognitive therapy involves helping the individual to identify distorted thinking patterns regarding themselves, the traumatic incident and the world. Individuals are encouraged to challenge their thoughts by weighing up available evidence and through the utilisation of various techniques by the therapist, including specific questioning that leads the individual to challenge distorted views. EMDR involves the PTSD sufferer focusing on a traumatic image, thought, emotion and a bodily sensation whilst receiving bilateral stimulation, most commonly in the form of eye movements. Non‐TFCBT usually focuses on techniques for the reduction of anxiety. The most widely used protocol for anxiety reduction in PTSD is stress inoculation training (SIT), which teaches skills for managing stress, such as relaxation, thought stopping and guided dialogue. It provides the opportunity to practise acquired skills gradually, across a variety of settings. Psychodynamic psychotherapy focuses on integrating the traumatic experience into the life experience of the individual as a whole; childhood issues are often felt to be important.
How the intervention might work
The psychological therapies considered by this review stem from various theoretical perspectives. Individual protocols describe how therapies might work in detail. TFCBT protocols draw on four core components emphasised in varying degrees: 1) psycho‐education; 2) anxiety management; 3) exposure; and 4) cognitive restructuring. Earlier therapies tended to be more behaviourally based, focusing heavily on exposure work. Cognitive components have become more prominent over time, in line with the popularity of information processing accounts of the disorder. Exposure plays an important role in many TFCBT protocols. It may be carried out in vivo (real life), or imaginally. It is common for both to be used in the treatment of PTSD, to target internally and externally feared stimuli. The rationale behind the use of imaginal exposure varies according to the specific TFCBT protocol. Imaginal exposure is based on principles of habituation (the reduction of anxiety after prolonged exposure) or information processing (allowing re‐evaluation of old information and incorporation of new information into the trauma memory), or a combination of both. In addition, cognitive restructuring has an important role, seeking to identify and modify dysfunctional thoughts by testing and challenging self‐held beliefs, based on the assumption that these usually unquestioned thoughts are distorted or unhelpful. EMDR is an integrative trauma‐focused therapy encompassing elements from various effective psychotherapies in a structured protocol drawn from an information processing model of PTSD. There is no agreed mechanism by which EMDR is thought to operate. Shapiro 1989b discovered EMDR accidentally. Her account implicates personal experience of rapid eye movements easing distress. On the basis of this experience, Shapiro elaborated EMDR for the treatment of Vietnam war veterans and abuse sufferers. It is suggested that bilateral stimulation aids the processing of traumatic memories. Non‐TFCBT interventions such as SIT operate by teaching the individuals techniques to minimise and control their anxiety. In terms of other psychological therapies considered by this review, psychodynamic psychotherapy places emphasis on the unconscious mind, aiming to resolve inner conflict arising from the traumatic event. Person‐centred therapy/supportive counselling allows the individual to talk through problems and resolve difficulties with minimal guidance and direction from the therapist. The therapist is accepting and non‐judgemental. This style encourages the individual to feel comfortable in the expression of feelings, facilitating positive change. Unlike trauma‐focused therapies, person‐centred/supportive counselling does not encourage exploration of the trauma memory.
For a summary of psychological models of PTSD providing the rationale for many of the treatment approaches considered here, see Brewin 2003.
Why it is important to do this review
It is apparent that PTSD causes clinically significant suffering and that developing effective interventions is important. Earlier versions of this review and other meta‐analyses have found psychological therapies to be effective (e.g. Bradley 2005), with trauma‐focused treatments being more effective than non‐trauma‐focused treatments (Bisson 2007a). This is an update of a Cochrane review first published in 2005 and updated in 2007, bringing together current evidence concerning the psychological treatment of chronic PTSD in adults. Other Cochrane Collaboration reviews have considered single‐session psychological 'debriefing' to prevent PTSD (Rose 2002), multiple‐session early psychological interventions for the prevention of PTSD (Roberts 2009), early psychological therapies to treat acute traumatic stress symptoms (Roberts 2010), pharmacological treatments (Stein 2006), combined pharmacotherapy and psychological therapies for PTSD (Hetrick 2010), and psychological therapies for the treatment of PTSD in children and adolescents (Gillies 2012).
Objectives
To assess the effects of psychological therapies for the treatment of adults with chronic post‐traumatic stress disorder (PTSD).
Methods
Criteria for considering studies for this review
Types of studies
We include randomised controlled trials (RCTs) of psychological therapies for chronic PTSD in adults. Cluster‐RCTs and cross‐over trials were considered eligible for inclusion. We did not use sample size, language or publication status to determine whether or not a study was included.
Types of participants
Age
This review considered studies of adults only (aged 18 or over).
Diagnosis
Any individual suffering from chronic traumatic stress symptoms, i.e. with a duration of three months or more. At least 70% of participants were required to be diagnosed as suffering from PTSD according to DSM‐III (APA 1980), DSM‐IIIR (APA 1987), DSM‐IV (APA 2000),ICD‐9 (WHO 1979) or ICD‐10 (WHO 1992) criteria, by means of a structured interview or diagnosis by a clinician. There was no restriction on the basis of severity of PTSD symptoms or the type of traumatic event.
Co‐morbidities
There was no restriction on the basis of comorbidity, although we required that PTSD be the primary diagnosis.
Setting
There was no restriction on the basis of study setting.
Types of interventions
This review considered any psychological therapy designed to reduce symptoms of chronic PTSD. Group interventions were considered separately from those delivered on an individual basis. Psychological therapy provided in a group format is clinically distinct from its individually‐delivered counterparts, not least due to the reduced therapist 'dose' associated with group therapy.
Experimental interventions
Individual trauma‐focused cognitive behavioural therapy (TFCBT): any psychological therapy that predominantly used trauma‐focused cognitive, behavioural or cognitive‐behavioural techniques. This category included exposure therapy. Examples of therapies within this category are cognitive therapy (Ehlers 2005), cognitive processing therapy (Resick 1992) and prolonged exposure (Foa 2000).
Eye movement desensitisation and reprocessing (Shapiro 1989b).
Non‐trauma‐focused CBT: any psychological therapy that predominantly used non‐trauma‐focused cognitive, behavioural or cognitive‐behavioural techniques, for example stress inoculation training (SIT) (Meichenbaum 1988).
Group TFCBT: any approach delivered in a group setting that predominantly used trauma‐focused cognitive, behavioural or cognitive‐behavioural techniques.
Group non‐TFCBT: any approach delivered in a group that predominantly used non‐trauma‐focused cognitive, behavioural or cognitive‐behavioural techniques.
Other psychological therapy: any psychological therapy that predominantly used non‐trauma‐focused techniques that would not be considered cognitive, behavioural or cognitive‐behavioural techniques. This category comprised non‐directive/supportive/person‐centred counselling (Rogers 1961), hypnotherapy, psychodynamic therapy (Brom 1989) and present‐centred treatment.
Comparator interventions
Waitlist, treatment as usual, symptom monitoring, repeated assessment or other minimal attention control group;
An alternative psychological treatment.
Types of outcome measures
Primary outcomes
Reduction in the severity of PTSD symptoms using a standardised measure (i.e. a test that is administered and scored in a consistent way) rated by a clinician (e.g. the Clinician Administered PTSD Symptom Scale (Blake 1995)).
Drop‐out rates.
Secondary outcomes
Severity of self‐reported traumatic stress symptoms using a standardised measure (e.g. the Impact of Event Scale (Horowitz 1979)).
Severity of depressive symptoms (e.g. the Beck Depression Inventory (Beck 1961)).
Severity of anxiety symptoms using scales (e.g. the Spielberger State Trait Anxiety Inventory (Spielberger 1973)).
PTSD diagnosis after treatment.
Any adverse effects, e.g. increased PTSD symptoms.
We produced hierarchies of the standardised measures, based on their frequency of use within the included studies. Where a trial reported data from two or more measures of the same outcome, we used only data from the measure ranked highest.
Timing of outcome assessment
We conducted separate pair‐wise meta‐analyses of follow‐up data at one to four months, five to eight months, nine months to one year, and over one year.
Search methods for identification of studies
Electronic searches
The Cochrane, Depression, Anxiety and Neurosis Group's Specialised Register (CCDANCTR) The Cochrane Depression, Anxiety and Neurosis Group (CCDAN) maintain two clinical trials registers at their editorial base in Bristol, UK: a references register and a studies‐based register. The CCDANCTR‐References Register contains over 33,000 reports of randomised controlled trials in depression, anxiety and neurosis. Approximately 65% of these references have been tagged to individual, coded trials. The coded trials are held in the CCDANCTR‐Studies Register and records are linked between the two registers through the use of unique Study ID tags. Coding of trials is based on the EU‐Psi coding manual. Please contact the CCDAN Trials Search Co‐ordinator for further details. Reports of trials for inclusion in the Group's registers are collated from routine (weekly), generic searches of OVID MEDLINE (1950‐), EMBASE (1974‐) and PsycINFO (1967‐); quarterly searches of the Cochrane Central Register of Controlled Trials (CENTRAL) and review‐specific searches of additional databases. Reports of trials are also sourced from international trials registers c/o the World Health Organization’s trials portal (ICTRP), ClinicalTrials.gov, drug companies, the handsearching of key journals, conference proceedings and other (non‐Cochrane) systematic reviews and meta‐analyses. Details of CCDAN's generic search strategies can be found on the Group's website.
We searched the CCDANCTR (Studies and References Registers, all years to 12th April 2013) on condition alone, using the following terms: (PTSD or posttrauma* or post‐trauma* or “post trauma*” or (combat and disorder*))
Searching other resources
Grey literature We searched abstracts from meetings of the European and International Societies of Traumatic Stress Studies. We also searched websites and discussion fora related to PTSD.
Handsearching We handsearched the Journal of Traumatic Stress and the ISTSS Treatment Guidelines (Foa 2000; Foa 2009) for relevant articles.
Reference lists We scrutinised the reference lists of included studies for additional studies meeting the inclusion criteria.
Correspondence The main correspondence was with the UK NICE guidelines development group who kindly shared the results of their searches and communications (see Acknowledgements).
Data collection and analysis
Selection of studies
Two review authors independently read abstracts of all potential trials identified through the search strategy. If we felt an abstract represented a possible RCT, each review author independently read the full report to determine if the trial met the inclusion criteria. Any differences prompted re‐evaluation of the study, and we discussed disagreements with a third review author to reach a consensus.
Data extraction and management
We extracted data from published reports and entered them into Review Manager 5 Software (RevMan 5). We contacted authors to obtain missing information. Extracted data included demographic details of participants, details of the traumatic event, the randomisation process, the therapy used, and outcome data.
Main comparisons
Individual TFCBT versus waitlist/usual care
Individual TFCBT versus non‐TFCBT
Individual TFCBT versus other therapies
EMDR versus waitlist/usual care
EMDR versus individual TFCBT
EMDR versus non‐TFCBT
EMDR versus other therapies
Non‐TFCBT versus waitlist/usual care
Non‐TFCBT versus other therapy
Group TFCBT versus waitlist/usual care
Group TFCBT versus group non‐TFCBT
Other therapies versus waitlist/usual care
Group non‐TFCBT versus waitlist/usual care
Individual TFCBT versus group TFCBT
Individual TFCBT versus group non‐TFCBT
EMDR versus group TFCBT
EMDR versus group non‐TFCBT
Individual non‐TFCBT versus group TFCBT
Individual non‐TFCBT versus group non‐TFCBT
Assessment of risk of bias in included studies
We assessed all included studies for risk of bias, using the standard approach described in the Cochrane Handbook for Systematic Review of Interventions (Higgins 2011). This considered (1) sequence allocation for randomisation; (2) allocation concealment; (3) blinding of personnel and assessors; (4) incomplete outcome data; (5) selective reporting; and (6) any other notable risks of bias. Each was judged to pose a 'high', 'low' or 'unclear' risk of bias. Two review authors conducted the assessments, discussing any disagreements with a third review author to reach a consensus.
1. Sequence allocation randomisation
Randomisation was judged as posing a 'low' risk of bias if each participant had an equal chance of being randomised to a group. Low‐risk methods included referring to a random number table, use of a computerised random number generator, shuffling sealed envelopes or throwing a dice. Methods judged as posing a 'high' risk of bias included use of a sequence generated by e.g. date of birth, clinic number, date of admission to the study, or allocation by availability of the intervention. When insufficient information was given to permit judgement of high or low risk of bias, we describe the study as being at an 'unclear' risk of bias attributable to sequence allocation.
2. Allocation concealment
Concealment of intervention allocation was said to be at 'low' risk when there was no chance of the investigator foreseeing a participant's assignment. Methods judged as posing a low risk of bias included central allocation (e.g. by telephone or the internet) or sequentially numbered opaque sealed envelopes. High‐risk methods included alternation or rotation of assignment or using an open random allocation schedule (e.g. a list of random numbers). When insufficient information was reported to permit judgement of high or low risk, we describe the study as being at an 'unclear' risk of bias attributable to allocation concealment.
3. Blinding of personnel and assessors
It is not possible to blind either the participants or those administering psychological interventions. However, outcome assessors can be blinded. Those studies which blinded assessors were deemed to be at a low risk of bias, those which did not were judged as being at a high risk of bias. When insufficient information was reported to permit judgement of high or low risk, we describe the study as being at an 'unclear' risk of bias attributable to blinding.
4. Incomplete outcome data
We judged incomplete data to have been handled appropriately when reported completely, including attrition rates and exclusions, with consideration of the issue in terms of analysing the data. Low risk of bias was associated with no missing outcome data, or the use of data imputed using appropriate methods. Methods judged as posing a high risk of bias included analyses that considered only the data of treatment‐completers, or potentially inappropriate application of simple imputation. When insufficient information was reported to permit judgement of high or low risk, we describe the study as being at an 'unclear' risk of bias attributable to incomplete data.
5. Selective reporting
We judged a study to be at a low risk of bias if a protocol was available and all prespecified outcomes were reported. If there was no available protocol, the study was assigned a low risk in this domain if it was clear that the published reports included all expected outcomes, including those prespecified. When insufficient information was reported to permit judgement of high or low risk, we describe the study as being at an 'unclear' risk of bias attributable to selective reporting.
6. Other notable risks of bias
We noted any other potential threats to validity and judged them to be at a high or low risk of bias. We describe them as being at 'unclear' risk of bias when there was insufficient information to assess additional risk of bias.
Measures of treatment effect
Continuous data
We analysed continuous outcomes as standardised mean differences (SMDs) to allow ease of comparison across studies. All outcomes are presented using 95% confidence intervals (CIs).
Dichotomous data
We analysed categorical outcomes as risk ratios (RRs), these being more widely used in medical practice than odds ratios. All outcomes are presented using 95% confidence intervals.
Unit of analysis issues
Cross‐over trials
We included only outcome data from the first randomisation period when a study adopted a cross‐over design.
Studies with multiple treatment groups
If the trial had three (or more) arms, we undertook pair‐wise meta‐analysis with each arm, depending upon the nature of the intervention in each arm and the relevance to the review objectives. We avoided multiple comparisons as far as possible, to limit the risk of false positive results. When a study had three or more arms that were relevant to the review we considered the appropriateness of combining data from two arms if therapies were sufficiently similar or of using data from the arms of the trial which fit closest to the review objective. Decisions followed guidance provided by the Cochrane Handbook (Higgins 2011).
Cluster‐randomised trials
We had planned to include cluster‐RCTs, although none was identified by the searches to date. In future updates of the review, the methodology for dealing with these types of studies will follow that outlined by the Cochrane Handbook (Higgins 2011). We will adjust sample sizes using an estimate of the intracluster or intraclass correlation coefficient (ICC), which describes the 'similarity' of individuals within the same cluster. We will derive this from the trial if possible, or from another source, such as a similar study, or from a resource providing examples of ICCs.
Dealing with missing data
We contacted authors to obtain any data missing from the published report of included studies. We used intention‐to‐treat (ITT) data where possible, but used data from completers analyses when ITT data were not available.
Assessment of heterogeneity
We initially assessed studies included within each comparison for clinical heterogeneity in terms of variability in the experimental and control interventions, participants and settings, and outcomes. To further assess heterogeneity, we used both the I² statistic (Higgins 2003) and the Chi² test of heterogeneity, as well as visual inspection of the forest plots.
Assessment of reporting biases
When sufficient studies were available, we constructed funnel plots and scrutinised them for signs of asymmetry. Since reporting bias is just one possible reason for observed asymmetry, we also considered alternative explanations.
Data synthesis
We pooled data from more than one study using a fixed‐effect meta‐analysis, except where heterogeneity was present, in which case we used a random‐effects model.
Subgroup analysis and investigation of heterogeneity
We performed clinical heterogeneity subgroup analyses (when sufficient data were available) as follows:
Type of traumatic event (combat‐related trauma versus rape and sexual assault versus other civilian trauma)
Participant characteristics (men only versus women only)
Sensitivity analysis
We conducted sensitivity analyses to assess the effect of high or unclear risk of bias in any of the following domains:
Sequence generation
Allocation concealment
Blinding of outcome assessment
These analyses were performed for comparisons including 10 or more studies.
Results
Description of studies
See Characteristics of included studies and Characteristics of excluded studies.
Results of the search
The search yielded 1477 articles for consideration. We reviewed abstracts and obtained full‐text copies for 129 potentially relevant studies. Seventy RCTs (79 comparisons) met the inclusion criteria for the review. Figure 1 presents a flow diagram for study selection.
1.

Study flow diagram.
Included studies
Design
All included studies were RCTs.
Sample sizes
The number of participants randomised in the trials ranged from 9 (Ready 2010) to 360 (Schnurr 2003). Eleven studies included sample sizes of over 100: Brom 1989 (n = 112); Cloitre 2010 (n = 104); Foa 2005 (n = 171); Krakow 2000 (n = 169); Krakow 2001 (n = 114); Mueser 2008 (n = 108); Nijdam 2012 (n = 140); Power 2002 (n = 105); Resick 2002 (n = 121); Schnurr 2003 (n = 360); Schnurr 2007 (n = 284).
Settings
USA (33 studies), UK (6 studies), Australia (7 studies), Netherlands (4 studies), Hawaii (3 studies), Germany (3 studies), Turkey (2 studies), Sweden (2 studies), Uganda (2 studies), Japan (1 study), Romania (1 study), Thailand (1 study), Canada (1 study), Portugal (1 study), Cambodia (1 study), China (1 study), Spain (1 study).
Participants
The study populations were varied and often not directly comparable (i.e. there was significant clinical heterogeneity). Studies included individuals traumatised by combat (13 studies), sexual assault (13 studies), war/persecution (6 studies), road traffic accidents (4 studies), earthquake (3 studies), childhood sexual abuse (3 studies), political detainment (1 study), terrorism (1 study), sexual or physical assault (1 study) and serving in the police force. The remainder of the studies included individuals traumatised by various traumatic events (24 studies).
Time post‐trauma
All studies included individuals at least three months after the trauma. The range was large, from three months to over 40 years (Bichescu 2007). There was often a wide range of times since trauma included in individual studies.
Interventions
In order to present the results in a meaningful way, we decided to pool data that used a similar theoretical methodology. This was conducted a priori, resulting in the establishment of six groups: individual TFCBT, non‐TFCBT, EMDR, group TFCBT, group non‐TFCBT and other therapies (psychodynamic therapy, hypnotherapy, supportive counselling and present‐centred counselling).
1. Trauma‐focused cognitive behavioural therapy: Forty‐nine studies considered individual TFCBT ‐ Adenauer 2011; Asukai 2010; Basoglu 2005; Basoglu 2007; Bichescu 2007; Blanchard 2003; Brom 1989; Bryant 2003; Bryant 2011; Cloitre 2002; Cloitre 2010; Cooper 1989; Devilly 1999; Duffy 2007; Dunne 2012; Echeburua 1997; Ehlers 2005; Fecteau 1999; Feske 2008; Foa 1991; Foa 1999; Foa 2005; Forbes 2012; Galovski 2012; Gamito 2010; Gersons 2000; Hensel‐Dittmann 2011; Hinton 2005; Ironson 2002; Keane 1989; Kubany 2003; Kubany 2004; Lindauer 2005; McDonagh 2005; Marks 1998; Monson 2006; Mueser 2008; Neuner 2004; Neuner 2008; Neuner 2010; Paunovic 2011; Peniston 1991; Power 2002; Ready 2010; Resick 2002; Schnurr 2007; Taylor 2003; Vaughan 1994; Nijdam 2012; Zang 2013.
2. Non‐TFCBT: Eight studies considered non‐TFCBT ‐ Carlson 1998; Echeburua 1997; Foa 1991; Foa 1999; Kearney 2013; Marks 1998; Taylor 2003; Vaughan 1994.
3. Eye Movement Desensitisation and Reprocessing: Sixteen studies considered eye movement desensitisation and reprocessing ‐ Carlson 1998; Devilly 1998; Devilly 1999; Hogberg 2007; Ironson 2002; Jensen 1994; Lee 2002; Marcus 1997; Power 2002; Rothbaum 1997; Rothbaum 2005; Scheck 1998; Taylor 2003; Vaughan 1994; Nijdam 2012. 4. Group TFCBT: Ten studies considered group TFCBT ‐ Beck 2009; Chard 2005; Classen 2001; Hinton 2011; Hollifield 2007; Kearney 2013; Krakow 2000; Krakow 2001; Schnurr 2003; Zlotnick 1997.
5. Group non‐TFCBT: One study considered group non‐TFCBT: Schnurr 2003
6. Other therapies: Nine studies considered other therapies (supportive counselling, present‐centred therapy, hypnotherapy and psychodynamic therapy) ‐ Blanchard 2003; Brom 1989; Bryant 2003; Cloitre 2010; Feske 2008; Foa 1991; McDonagh 2005; Ready 2010; Schnurr 2007.
Comparisons
The included trials compared (i) Psychological therapy versus waitlist or usual care control (some studies allowed the control group to receive pharmacological treatments and/or psychological therapies that were not being considered specifically); (ii) Psychological therapy versus other psychological therapy.
We made the following specific comparisons:
1. Individual TFCBT versus waitlist/usual care:Adenauer 2011; Asukai 2010; Basoglu 2005; Basoglu 2007; Bichescu 2007; Blanchard 2003; Brom 1989; Cloitre 2002; Cooper 1989; Duffy 2007; Dunne 2012; Ehlers 2003; Ehlers 2005; Fecteau 1999; Foa 1991; Foa 1999; Foa 2005; Forbes 2012; Galovski 2012; Gamito 2010; Gersons 2000; Hinton 2005; Keane 1989; Kubany 2003; Kubany 2004; Lindauer 2005; McDonagh 2005; Monson 2006; Mueser 2008; Neuner 2010; Paunovic 2011; Peniston 1991; Power 2002; Resick 2002; Vaughan 1994; Wells 2012; Zang 2013.
2. Individual TFCBT versus non‐TFCBT:Echeburua 1997; Foa 1991; Foa 1999; Hensel‐Dittmann 2011; Marks 1998; Taylor 2003; Vaughan 1994.
3.Individual TFCBT versus other therapies:Blanchard 2003; Brom 1989; Bryant 2003; Bryant 2011; Cloitre 2010; Feske 2008; Foa 1991; McDonagh 2005; Neuner 2004; Ready 2010; Schnurr 2007.
4. EMDR versus waitlist/usual care:Carlson 1998; Devilly 1998; Hogberg 2007; Jensen 1994; Power 2002; Rothbaum 1997; Rothbaum 2005; Vaughan 1994.
5. EMDR versus individual TFCBT:Devilly 1999: Ironson 2002: Lee 2002: Nijdam 2012; Power 2002: Rothbaum 2005; Taylor 2003; Vaughan 1994.
6. EMDR versus non‐TFCBT:Carlson 1998; Taylor 2003; Vaughan 1994.
7. EMDR versus other therapy:Marcus 1997; Scheck 1998.
8. Individual non‐TFCBT versus waitlist/usual care:Carlson 1998; Foa 1991; Foa 1999; Vaughan 1994; Wells 2012.
9. Non‐TFCBT versus other therapy:Foa 1991.
10. Group TFCBT versus waitlist/usual care:Beck 2009; Chard 2005; Hinton 2011; Hollifield 2007; Krakow 2001, Krakow 2000, Zlotnick 1997.
11. Group TFCBT versus group non‐TFCBT:Schnurr 2003.
12.Other therapies versus waitlist/usual care:Blanchard 2003; Brom 1989; Foa 1991; McDonagh 2005.
13. Group non‐TFCBT versus waitlist/usual care: no studies
14. Individual TFCBT versus group TFCBT: no studies
15. Individual TFCBT versus group non‐TFCBT: no studies
16. EMDR versus group TFCBT: no studies
17. EMDR versus group non‐TFCBT: no studies
18. Individual non‐TFCBT versus group TFCBT: no studies
19. Individual non‐TFCBT versus group non‐TFCBT: no studies
Outcomes
Primary outcomes were reduction in severity of clinician‐rated PTSD symptoms and drop‐out rate. Secondary outcome measures were severity of self‐reported PTSD symptom, severity of depressive symptoms, severity of anxiety symptoms, PTSD diagnosis after treatment and adverse side effects (such as increased PTSD symptoms).
Excluded studies
We excluded studies if they did not satisfy the inclusion criteria. Some studies made no formal diagnosis of PTSD (Abbasnejad 2007; Classen 2001; Classen 2010; Cole 2007; Edmond 1999; Edmond 2004; Falsetti 2001; Ginzberg 2009; Hiari 2005;, Knaevelsrud 2007; Lange 2001; Lange 2003; Litz 2007; Price 2007; Ryan 2005; Shapiro 1989a; Sloan 2004; Sloan 2005), and in other studies fewer than 70% of participants met full diagnostic criteria for the disorder (Davis 2007; Difede 2007a; DuHamel 2010; Maercker 2006; Rabe 2008; Van Emmerik 2008; Wilson 1995). Other reasons for excluding specific studies were a duration of less than three months following trauma (Echeburua 1996; some participants within, Foa 2006; Spence 2011), treatment did not target traumatic stress symptoms (Dunn 2007; Chemtob 1997), comparison of two psychological therapies in the same category (Arntz 2007; Mithoefer 2011; Paunovic 2001; Tarrier 1999; Watson 1997), the intervention was not a psychological therapy (Gidron 1996), including individuals under 18 years of age (Jaberghaderi 2004; Najavits 2006; Schaal 2009), comparison of two non‐TFCBT therapies, and comparison with pharmacotherapy (Frommberger 2004; Rothbaum 2006).
See Characteristics of excluded studies table for further details.
Studies awaiting classification
Krupnick 2008 is awaiting classification as we need to obtain further information.
Risk of bias in included studies
A graphical representation of the overall risk of bias for each domain and each study is available in Figure 2 and Figure 3 respectively.
2.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Sequence allocation randomisation
Fifteen studies reported a method of allocation that we felt to be appropriate, and which we judged to be at low risk of bias (Adenauer 2011; Asukai 2010; Basoglu 2005; Basoglu 2007; Bryant 2003; Bryant 2011; Fecteau 1999; Hensel‐Dittmann 2011; Hogberg 2007; Hollifield 2007; Lindauer 2005; Neuner 2004; Power 2002; Scheck 1998; Wells 2012). We judged the method of allocation to be at high risk of bias in six studies (Bichescu 2007; Blanchard 2003; Cooper 1989; Devilly 1999; Ehlers 2003; Schnurr 2003). The remainder of the studies reported insufficient information for us to make a judgement.
Allocation concealment
Many studies did not provide full details of the method of randomisation and we therefore judged concealment to be at unclear risk of bias in the majority. Fifteen studies reported adequate allocation concealment, representing a low risk of bias (Basoglu 2005; Basoglu 2007; Bryant 2011; Cloitre 2010; Duffy 2007; Ehlers 2003; Foa 2005; Forbes 2012; Krakow 2001; Lindauer 2005; Monson 2006; Mueser 2008; Nijdam 2012; Power 2002; Scheck 1998). We judged one study to be at high risk in terms of failure to conceal allocation (Cooper 1989). None of the other studies reported any methods of concealing allocation and we judged them to be at unclear risk of bias in this domain.
Blinding
In common with all studies of psychological therapies a double‐blind methodology is virtually impossible, as it is clear to the participant what treatment they are receiving. However, a well‐designed study should ensure blinding of the assessor of outcome measures. In six of the included studies, the assessor was aware of the participant's allocation (Basoglu 2005; Carlson 1998; Ironson 2002; Keane 1989; Marcus 1997; Paunovic 2011). It was unclear whether or not the assessor was blind in 14 studies (Brom 1989; Cooper 1989; Duffy 2007; Dunne 2012; Echeburua 1997; Fecteau 1999; Feske 2008; Forbes 2012; Gamito 2010; Hinton 2011; Jensen 1994; Kearney 2013; Krakow 2000; Scheck 1998).
Incomplete outcome data
Loss to follow‐up
Drop‐out rates were high in many of the studies and reasons for attrition were generally poorly reported. We judged 21 studies to be at high risk of bias for incomplete outcome data (Adenauer 2011; Basoglu 2005; Basoglu 2007; Beck 2009; Brom 1989; Carlson 1998; Cooper 1989; Devilly 1998; Devilly 1999; Ehlers 2003; Fecteau 1999; Feske 2008; Foa 1991; Hogberg 2007; Jensen 1994; Krakow 2000; Paunovic 2011; Power 2002; Rothbaum 1997; Rothbaum 2005; Scheck 1998; Zlotnick 1997). It was unclear how missing data were handled in six studies (Gamito 2010; Keane 1989; Marcus 1997; Peniston 1991; Ready 2010). We judged the remainder to have dealt with drop‐outs appropriately, i.e. at low risk of bias.
Selective reporting
It was difficult to draw any meaningful conclusions with regards to the issue of selective reporting. Very few of the included studies had published protocols available. It was therefore impossible to know whether prespecified outcome measures were adequately reported. The majority of studies adequately reported all outcomes outlined within the Methods section of the trial report.
Other potential sources of bias
A strength of the majority of the studies was having clear objectives, but sample sizes were often small and the follow‐up period was limited. The treatments delivered were reasonably well‐described and the majority of studies reported on the credentials and experience of therapists. A high proportion of the included studies made some assessment of treatment adherence. Most studies used well‐validated outcome measures although there was considerable variation in the actual measures used. For practical and ethical reasons there were rarely follow‐up data available from waitlist groups. We could not rule out potential researcher allegiance in many of the studies. A number of the included trials were of interventions that were evaluated by their originators.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4; Table 5; Table 6; Table 7; Table 8; Table 9; Table 10; Table 11; Table 12; Table 13
The full results are contained in the Tables and are summarised below.
Comparison 1. Individual TFCBT/Exposure therapy versus waitlist/usual care
37 studies including 1830 participants contributed to this comparison.
Primary outcomes
1.1. Clinician‐rated PTSD symptoms
Twenty‐eight studies considered this outcome with a total of 1256 individuals (Analysis 1.1). There was heterogeneity between these trials (Chi² = 237.95, P = 0.00001; I² = 89%) and we used a random‐effects model to pool the data. The individual TFCBT group did better than the waitlist/usual care group immediately after treatment (standardised mean difference (SMD) ‐1.62; 95% confidence interval (CI) ‐2.03 to ‐1.21).
1.1. Analysis.

Comparison 1 Trauma‐focused CBT/Exposure therapy vs waitlist/usual care, Outcome 1 Severity of PTSD symptoms ‐ clinician.
At 1‐ to 4‐month follow‐up four studies compared this outcome with 336 individuals (Analysis 1.2). There was heterogeneity between these trials (Chi² = 52.30; P < 0.00001; I² = 94%). The individual TFCBT group did significantly better than the waitlist/usual care group (SMD ‐1.18; 95% CI ‐2.20 to ‐0.17).
1.2. Analysis.

Comparison 1 Trauma‐focused CBT/Exposure therapy vs waitlist/usual care, Outcome 2 Severity of PTSD symptoms at 1 ‐ 4 month follow‐up.
At 5‐ to 8‐month follow‐up three studies compared this outcome with 192 individuals (Analysis 1.3). There was little heterogeneity between these trials (Chi² = 0.68; P = 0.71; I² = 0%). The individual TFCBT group did better than the waitlist/usual care group (SMD ‐0.47; 95% CI ‐0.77 to ‐0.18).
1.3. Analysis.
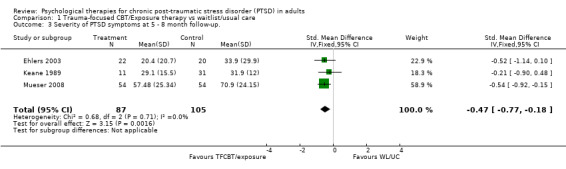
Comparison 1 Trauma‐focused CBT/Exposure therapy vs waitlist/usual care, Outcome 3 Severity of PTSD symptoms at 5 ‐ 8 month follow‐up..
At 9‐ to 12‐month follow‐up one study reported this outcome with 109 individuals (Analysis 1.4). The individual TFCBT group did significantly better than the waitlist/usual care group (SMD ‐0.78; 95% CI ‐1.18 to ‐0.39).
1.4. Analysis.

Comparison 1 Trauma‐focused CBT/Exposure therapy vs waitlist/usual care, Outcome 4 Severity of PTSD symptoms 9 ‐ 12 month follow‐up.
1.2. Drop‐outs
Thirty‐four studies with a total of 1776 individuals recorded whether individuals left the study early for any reason by group (Analysis 1.5). There was considerable clinical heterogeneity between these trials. The individual TFCBT group did significantly worse than the waitlist/usual care group (RR 1.64; 95% CI 1.30 to 2.06).
1.5. Analysis.

Comparison 1 Trauma‐focused CBT/Exposure therapy vs waitlist/usual care, Outcome 5 Leaving the study early for any reason.
Secondary outcomes
1.3 Self‐reported PTSD symptoms
Seventeen studies considered this outcome with a total of 686 individuals (Analysis 1.1.4). There was heterogeneity between these trials (Chi² = 82.15; P < 0.00001; I² = 81%) and we used a random‐effects model to pool the data. The individual TFCBT group did better than the waitlist/usual care group immediately after treatment (SMD ‐1.60; 95% CI ‐2.02 to ‐1.18).
At 1‐ to 4‐month follow‐up two studies compared this outcome with 181 individuals (Analysis 1.6). There was marked heterogeneity between these trials (Chi² = 40.04; P = 0.00001; I² = 98%). There were no significant differences between groups (SMD ‐3.03; 95% CI ‐6.51 to 0.45).
1.6. Analysis.
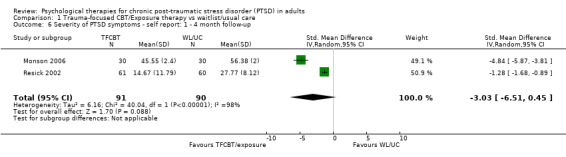
Comparison 1 Trauma‐focused CBT/Exposure therapy vs waitlist/usual care, Outcome 6 Severity of PTSD symptoms ‐ self report: 1 ‐ 4 month follow‐up.
At 5‐ to 8‐month follow‐up two studies compared this outcome with 208 individuals (Analysis 1.7). The individual TFCBT group did better than the waitlist/usual care group (SMD ‐0.61; 95% CI ‐0.90 to ‐0.32).
1.7. Analysis.

Comparison 1 Trauma‐focused CBT/Exposure therapy vs waitlist/usual care, Outcome 7 Severity of PTSD symptoms ‐ self report: 5 ‐ 8 months).
At 9‐ to 12‐month follow‐up one study compared this outcome with 121 individuals (Analysis 1.8). The individual TFCBT group did better than the waitlist/usual care group (SMD ‐1.22; 95% CI ‐1.61 to ‐0.83).
1.8. Analysis.

Comparison 1 Trauma‐focused CBT/Exposure therapy vs waitlist/usual care, Outcome 8 Severity of PTSD symptoms ‐ self report: 9 ‐ 12 month follow up.
1.4 Depression
Twenty‐nine studies considered this outcome with a total of 1233 individuals (Analysis 1.9). There was heterogeneity between these trials (Chi² = 174.84, P < 0.00001; I² = 84%) and we used a random‐effects model to pool the data. The individual TFCBT group did better than the waitlist/usual care group immediately after treatment (SMD ‐1.31; 95% CI ‐1.65 to ‐0.98).
1.9. Analysis.

Comparison 1 Trauma‐focused CBT/Exposure therapy vs waitlist/usual care, Outcome 9 Depression.
At 1‐ to 4‐month follow‐up seven studies compared this outcome with 413 individuals (Analysis 1.10). There was heterogeneity between these trials (Chi² = 41.24; P < 0.00001; I² = 85%). The individual TFCBT group did better than the waitlist/usual care group (SMD ‐0.75; 95% CI ‐1.33 to ‐0.18).
1.10. Analysis.

Comparison 1 Trauma‐focused CBT/Exposure therapy vs waitlist/usual care, Outcome 10 Depression 1 ‐ 4 month follow‐up.
At 5‐ to 8‐month follow‐up two studies compared this outcome with 150 individuals (Analysis 1.11). The individual TFCBT group did better than the waitlist/usual care group (SMD ‐0.50; 95% CI ‐0.82 to ‐0.17).
1.11. Analysis.

Comparison 1 Trauma‐focused CBT/Exposure therapy vs waitlist/usual care, Outcome 11 Depression 5 ‐ 8 month follow‐up.
At 9‐ to 12‐month follow‐up one study compared this outcome with 108 individuals (Analysis 1.12). The individual TFCBT group did better than the waitlist/usual care group (SMD ‐0.60; 95% CI ‐0.99 to ‐0.21).
1.12. Analysis.

Comparison 1 Trauma‐focused CBT/Exposure therapy vs waitlist/usual care, Outcome 12 Depression 9 ‐ 12 month follow‐up.
1.5 Anxiety
Eighteen studies considered this outcome with a total of 664 individuals (Analysis 1.13). There was heterogeneity between these trials (Chi² = 27.43; P = 0.04; I² = 38%) and we used a random‐effects model to pool the data. The individual TFCBT group did better than the waitlist/usual care group immediately after treatment (SMD ‐0.82; 95% CI ‐1.03 to ‐0.61).
1.13. Analysis.

Comparison 1 Trauma‐focused CBT/Exposure therapy vs waitlist/usual care, Outcome 13 Anxiety.
At 1‐to 4‐month follow‐up three studies compared this outcome with 189 individuals (Analysis 1.14). There was little heterogeneity between trials (Chi² = 2.16; P = 0.34; I² = 7%). The TFCBT group did better than the waitlist/usual care group (SMD ‐0.32; 95% CI ‐0.60 to ‐0.03).
1.14. Analysis.

Comparison 1 Trauma‐focused CBT/Exposure therapy vs waitlist/usual care, Outcome 14 Anxiety 1 ‐ 4 month follow‐up.
At 9‐ to 12‐month follow‐up one study compared this outcome with 108 individuals (Analysis 1.15). There was no difference between the two groups (SMD ‐0.33; 95% CI ‐0.71 to 0.05).
1.15. Analysis.

Comparison 1 Trauma‐focused CBT/Exposure therapy vs waitlist/usual care, Outcome 15 Anxiety 9 ‐ 12 month follow‐up.
1.6 PTSD diagnosis after treatment
Nineteen studies with a total of 910 individuals reported this outcome (Analysis 1.18). There was significant heterogeneity between these trials (Chi² = 101.56; P < 0.00001; I² = 82%) and we used a random‐effects model to pool the data. The individual TFCBT group did better than the waitlist/usual care group (RR 0.51; 95% CI 0.41 to 0.64).
1.18. Analysis.
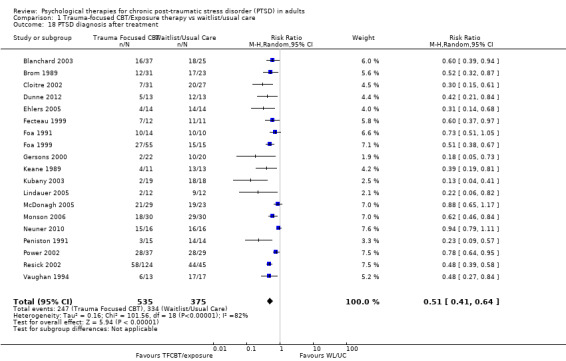
Comparison 1 Trauma‐focused CBT/Exposure therapy vs waitlist/usual care, Outcome 18 PTSD diagnosis after treatment.
1.7 Adverse effects
No studies formally considered adverse effects.
Comparison 2. TFCBT versus non‐TFCBT
Seven studies including 267 participants contributed to this comparison.
Primary outcomes
2.1 Clinician‐rated PTSD symptoms
Seven studies considered this outcome with a total of 267 individuals (Analysis 2.1). There was evidence of heterogeneity between these trials (Chi² = 11.25; P = 0.08; I² = 47%), and we used a random‐effects model to pool the data. There was no difference between TFCBT and non‐TFCBT in terms of clinician‐rated PTSD symptoms immediately after treatment (SMD ‐0.27; 95% CI ‐0.63 to 0.10).
2.1. Analysis.
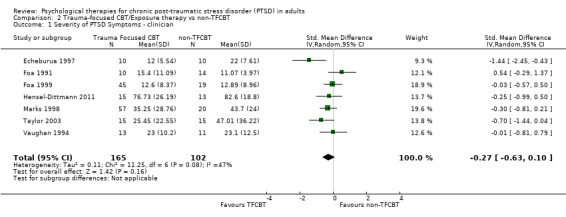
Comparison 2 Trauma‐focused CBT/Exposure therapy vs non‐TFCBT, Outcome 1 Severity of PTSD Symptoms ‐ clinician.
At 1‐ to 4‐month follow‐up five studies considered this outcome with a total of 127 individuals (Analysis 2.2). There was evidence of heterogeneity between these trials (Chi² = 7.30; P = 0.12; I² = 45%), and we used a random‐effects model to pool the data. The individual TFCBT group did better than the non‐TFCBT group (SMD ‐0.51; 95% CI ‐1.00 to ‐0.01).
2.2. Analysis.

Comparison 2 Trauma‐focused CBT/Exposure therapy vs non‐TFCBT, Outcome 2 Severity of PTSD symptoms ‐ clinician ‐ follow‐up (1 ‐ 4 months).
At 5‐ to 8‐month follow‐up two studies compared this outcome with 48 individuals (Analysis 2.3). There was evidence of heterogeneity between these trials (Chi² = 3.32; P = 0.07; I² = 70%) and we used a random‐effects model to pool the data. Based on these two trials, there was no difference between TFCBT and non‐TFCBT in terms of clinician‐rated PTSD symptoms at five to eight months (SMD ‐1.00; 95% CI ‐2.17 to 0.17).
2.3. Analysis.

Comparison 2 Trauma‐focused CBT/Exposure therapy vs non‐TFCBT, Outcome 3 Severity of PTSD symptoms ‐ clinician ‐ follow‐up (5 ‐ 8 months).
At 9‐ to 12‐month follow‐up two studies compared this outcome with 48 individuals (Analysis 2.4). There was no evidence of heterogeneity between these trials (Chi² = 0.08; P = 0.78; I² = 0%) and we used a random‐effects model to pool the data. Based on these two trials, there was no difference between TFCBT and non‐TFCBT in terms of clinician‐rated PTSD symptoms at 9 to 12 months (SMD ‐12.93; 95% CI ‐18.72 to ‐7.14).
2.4. Analysis.
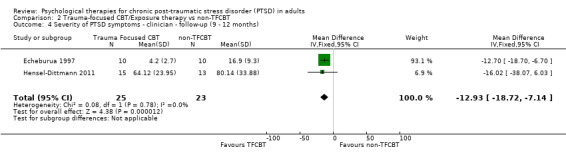
Comparison 2 Trauma‐focused CBT/Exposure therapy vs non‐TFCBT, Outcome 4 Severity of PTSD symptoms ‐ clinician ‐ follow‐up (9 ‐ 12 months).
2.2 Drop‐outs
Seven studies with a total of 312 individuals recorded whether individuals left the study early for any reason by group (Analysis 2.5). There was no difference between the TFCBT group and the non‐TFCBT on this measure (RR 1.19; 95% CI 0.71 to 2.0).
2.5. Analysis.

Comparison 2 Trauma‐focused CBT/Exposure therapy vs non‐TFCBT, Outcome 5 Leaving the study early for any reason.
Secondary outcomes
2.3 Self‐reported PTSD symptoms
Three studies considered this outcome with a total of 127 individuals (Analysis 2.6). There was no evidence of significant heterogeneity between these trials. The individual TFCBT group did better than the non‐TFCBT group (SMD ‐0.37; 95% CI ‐0.74 to 0.01).
2.6. Analysis.

Comparison 2 Trauma‐focused CBT/Exposure therapy vs non‐TFCBT, Outcome 6 Severity of PTSD symptoms ‐ self report.
At 1‐ to 4‐month follow‐up two studies considered this outcome with a total of 54 individuals (Analysis 2.7). There was no significant heterogeneity between these trials (Chi² = 0.78; P = 0.38; I² = 0%). There was no difference between the TFCBT group and the non‐TFCBT on this measure (SMD ‐0.44; 95% CI ‐0.99 to 0.10).
2.7. Analysis.
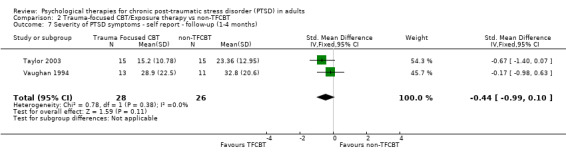
Comparison 2 Trauma‐focused CBT/Exposure therapy vs non‐TFCBT, Outcome 7 Severity of PTSD symptoms ‐ self report ‐ follow‐up (1‐4 months).
2.4 Depression
Six studies considered this outcome with a total of 189 individuals (Analysis 2.8). There was no evidence of heterogeneity between these trials (Chi² = 4.23; P = 0.52; I² = 0%). There was no difference between the individual TFCBT group and the non‐TFCBT group immediately after treatment (SMD ‐0.27; 95% CI ‐0.56 to 0.03).
2.8. Analysis.

Comparison 2 Trauma‐focused CBT/Exposure therapy vs non‐TFCBT, Outcome 8 Depression.
At 1‐ to 4‐month follow‐up five studies considered this outcome with a total of 147 individuals (Analysis 2.9). There was no evidence of significant heterogeneity between these trials (Chi² = 4.47; P = 0.35; I² = 11%). There was no difference between the individual TFCBT group and the non‐TFCBT group (SMD ‐0.28; 95% CI ‐0.62 to 0.06).
2.9. Analysis.
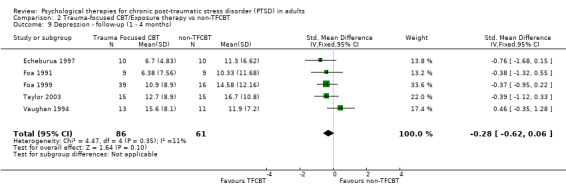
Comparison 2 Trauma‐focused CBT/Exposure therapy vs non‐TFCBT, Outcome 9 Depression ‐ follow‐up (1 ‐ 4 months).
At 5‐ to 8‐month follow‐up two studies compared this outcome with 48 individuals (Analysis 2.10). There was no evidence of significant heterogeneity between these trials (Chi² = 0.26; P = 0.61; I² = 0%). The individual TFCBT group did better than the non‐TFCBT group (SMD ‐0.71; 95% CI ‐1.30 to ‐0.12).
2.10. Analysis.

Comparison 2 Trauma‐focused CBT/Exposure therapy vs non‐TFCBT, Outcome 10 Depression ‐ follow‐up (5 ‐ 8 months).
At 9‐ to 12‐month follow‐up one study compared this outcome with 20 individuals (Analysis 2.11). The individual TFCBT group did better than the non‐TFCBT group (SMD ‐8.00; 95% CI ‐14.44 to ‐1.86).
2.11. Analysis.

Comparison 2 Trauma‐focused CBT/Exposure therapy vs non‐TFCBT, Outcome 11 Depression ‐ follow‐up (9 ‐ 12 months).
2.5 Anxiety
Four studies considered this outcome with a total of 127 individuals (Analysis 2.12). There was no evidence of significant heterogeneity between these trials (Chi² = 3.12; P = 0.37; I² = 4%). There was no difference between the individual TFCBT group and the non‐TFCBT group (SMD ‐0.12; 95% CI ‐0.49 to 0.26).
2.12. Analysis.
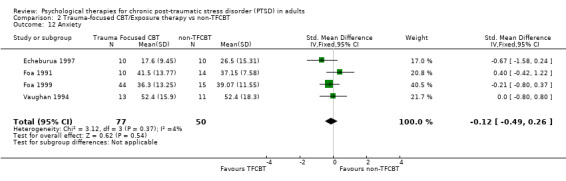
Comparison 2 Trauma‐focused CBT/Exposure therapy vs non‐TFCBT, Outcome 12 Anxiety.
At 1‐ to 4‐month follow‐up four studies considered this outcome with a total of 117 individuals (Analysis 2.13). There was evidence of heterogeneity between these trials (Chi² = 5.56; P = 0.13; I² = 46%). There was no difference between the individual TFCBT group and the non‐TFCBT group (SMD ‐0.24; 95% CI ‐0.79 to 0.30).
2.13. Analysis.
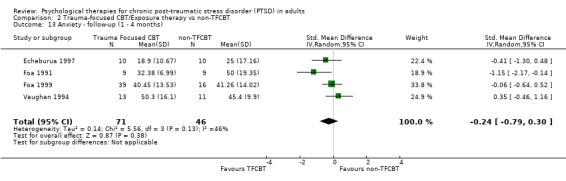
Comparison 2 Trauma‐focused CBT/Exposure therapy vs non‐TFCBT, Outcome 13 Anxiety ‐ follow‐up (1 ‐ 4 months).
At 5‐ to 8‐month follow‐up one study compared this outcome with 20 individuals (Analysis 2.14). There was no difference between the individual TFCBT group and the non‐TFCBT group (SMD ‐0.62; 95% CI ‐1.52 to 0.28).
2.14. Analysis.
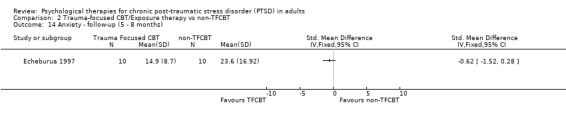
Comparison 2 Trauma‐focused CBT/Exposure therapy vs non‐TFCBT, Outcome 14 Anxiety ‐ follow‐up (5 ‐ 8 months).
At 9‐ to 12‐month follow‐up one study compared this outcome with 20 individuals (Analysis 2.15). There were no significant differences between groups (SMD ‐0.88; 95% CI ‐1.81 to 0.04).
2.15. Analysis.

Comparison 2 Trauma‐focused CBT/Exposure therapy vs non‐TFCBT, Outcome 15 Anxiety ‐ follow‐up (9 ‐ 12 months).
2.6 PTSD diagnosis after treatment
Six studies with a total of 284 individuals reported this outcome (Analysis 2.16). There was no difference between the individual TFCBT group and the stress non‐TFCBT group (RR 0.83; 95% CI 0.60 to 1.17), using a random‐effects model due to moderate heterogeneity (Chi² = 8.59; P = 0.13; I² = 42%).
2.16. Analysis.
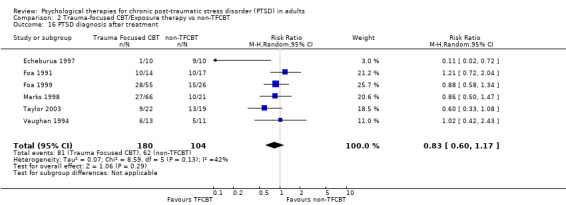
Comparison 2 Trauma‐focused CBT/Exposure therapy vs non‐TFCBT, Outcome 16 PTSD diagnosis after treatment.
2.7 Adverse effects
No studies formally considered adverse effects.
Comparison 3. TFCBT versus other therapies
Eleven studies including 762 participants contributed to this comparison.
Primary outcomes
3.1 Clinician rated PTSD symptoms
Ten studies considered this outcome with a total of 625 individuals (Analysis 3.1). There was evidence of heterogeneity between these trials (Chi² = 29.33; P = 0.0006; I² = 69%) and we used a random‐effects model to pool the data The individual TFCBT group did better than the 'other therapies' group immediately after treatment (SMD ‐0.48; 95% CI ‐0.83 to ‐0.14).
3.1. Analysis.
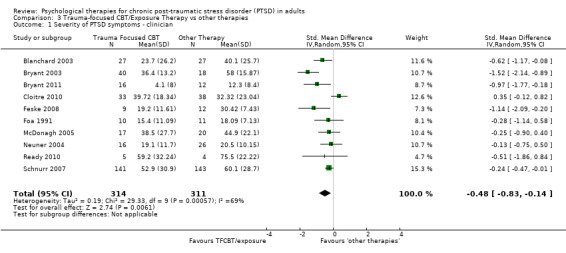
Comparison 3 Trauma‐focused CBT/Exposure Therapy vs other therapies, Outcome 1 Severity of PTSD symptoms ‐ clinician.
At 1‐ to 4‐month follow‐up eight studies considered this outcome with a total of 548 individuals (Analysis 3.2). There was evidence of significant heterogeneity between these trials (Chi² = 15.13; P = 0.03; I² = 54%). The individual TFCBT group did better than the 'other therapies' group (SMD ‐0.34; 95% CI ‐0.64 to ‐0.04).
3.2. Analysis.

Comparison 3 Trauma‐focused CBT/Exposure Therapy vs other therapies, Outcome 2 Severity of PTSD symptoms ‐ clinician ‐ 1 ‐ 4 month follow‐up.
At 5‐ to 8‐month follow‐up four studies compared this outcome with 434 individuals (Analysis 3.3). There was evidence of significant heterogeneity between these trials (Chi² = 19.43; P = 0.0002; I² = 85%), and we used a random‐effects model to pool the data. There were no differences between groups (SMD ‐0.58; 95% CI ‐1.20 to 0.04).
3.3. Analysis.
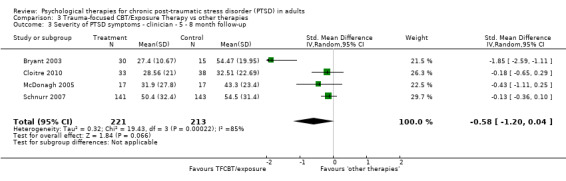
Comparison 3 Trauma‐focused CBT/Exposure Therapy vs other therapies, Outcome 3 Severity of PTSD symptoms ‐ clinician ‐ 5 ‐ 8 month follow‐up.
At 9‐ to 12‐month follow‐up two studies compared this outcome with 90 individuals (Analysis 3.4). There was significant heterogeneity between these trials (Chi² = 1.75; P = 0.19; I² = 43%), and we used a random‐effects model to pool the data. The individual TFCBT group did better than the 'other therapies' group (SMD ‐0.76; 95% CI ‐1.35 to ‐0.17).
3.4. Analysis.

Comparison 3 Trauma‐focused CBT/Exposure Therapy vs other therapies, Outcome 4 Severity of PTSD symptoms ‐ clinician ‐ 9 ‐ 12 month follow‐up.
3.2 Drop‐outs
Eleven studies with a total of 762 individuals reported this outcome (Analysis 3.5). There was little heterogeneity between these trials. 'Other therapies' did better than TFCBT (RR 1.39; 95% CI 1.01 to 1.92).
3.5. Analysis.
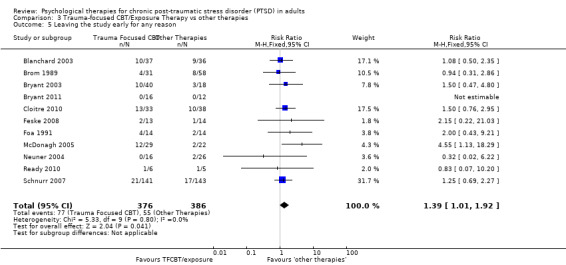
Comparison 3 Trauma‐focused CBT/Exposure Therapy vs other therapies, Outcome 5 Leaving the study early for any reason.
Secondary outcomes
3.3 Self‐reported PTSD symptoms
Six studies considered this outcome with a total of 574 individuals (Analysis 3.6). There was evidence of heterogeneity between these trials (Chi² = 39.39; P < 0.00001; I² = 87%) and we used a random‐effects model to pool the data. The individual TFCBT group did better than the 'other therapies' group immediately after treatment (SMD ‐0.60; 95% CI ‐1.15 to ‐0.06).
3.6. Analysis.
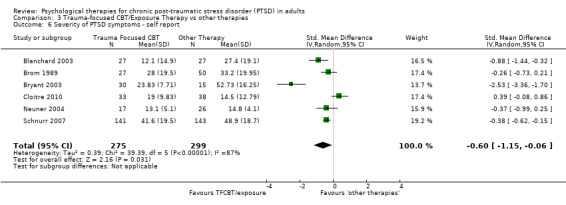
Comparison 3 Trauma‐focused CBT/Exposure Therapy vs other therapies, Outcome 6 Severity of PTSD symptoms ‐ self report.
At 1‐ to 4‐month follow‐up five studies considered this outcome with a total of 526 individuals (Analysis 3.7). There was no evidence of heterogeneity between these trials. The individual TFCBT group did better than the 'other therapies' group (SMD ‐0.29; 95% CI ‐0.47 to ‐0.12).
3.7. Analysis.

Comparison 3 Trauma‐focused CBT/Exposure Therapy vs other therapies, Outcome 7 Severity of PTSD symptoms ‐ self report ‐ follow‐up (1 ‐ 4 months).
At 5‐ to 8‐month follow‐up three studies compared this outcome with 338 individuals (Analysis 3.8). There was significant heterogeneity between these trials (Chi² = 16.14; P = 0.0003; I² = 88%) and we used a random‐effects model to pool the data. There were no differences between groups (SMD ‐0.90; 95% CI ‐2.05 to 0.25).
3.8. Analysis.

Comparison 3 Trauma‐focused CBT/Exposure Therapy vs other therapies, Outcome 8 Severity of PTSD symptoms ‐ self‐report ‐ follow‐up (5 ‐ 8 months).
At 9‐ to 12‐month follow‐up two studies compared this outcome with 90 individuals (Analysis 3.9). There was no evidence of heterogeneity between these trials (Chi² = 0.26; P = 0.61; I² = 0%). Based on these two trials, there was no difference between TFCBT and 'other therapies' in terms of clinician‐rated PTSD symptoms (SMD ‐2.66; 95% CI ‐5.71 to 0.38).
3.9. Analysis.

Comparison 3 Trauma‐focused CBT/Exposure Therapy vs other therapies, Outcome 9 Severity of PTSD symptoms ‐ self‐report ‐ follow‐up (9 ‐ 12 months).
3.4 Depression
Nine studies considered this outcome with a total of 570 individuals (Analysis 3.10). There was evidence of heterogeneity between these trials (Chi² = 13.34; P = 0.10; I² = 40%), and we used a random‐effects model to pool the data. The individual TFCBT group did better than the 'other therapies' group (SMD ‐0.37; 95% CI ‐0.63 to ‐0.11).
3.10. Analysis.

Comparison 3 Trauma‐focused CBT/Exposure Therapy vs other therapies, Outcome 10 Depression ‐ self report.
At 1‐ to 4‐month follow‐up seven studies considered this outcome with a total of 510 individuals (Analysis 3.11). There was heterogeneity between these trials (Chi² = 13.28; P = 0.04; I² = 55%). There was no difference between the groups (SMD ‐0.29; 95% CI ‐0.62 to 0.03).
3.11. Analysis.
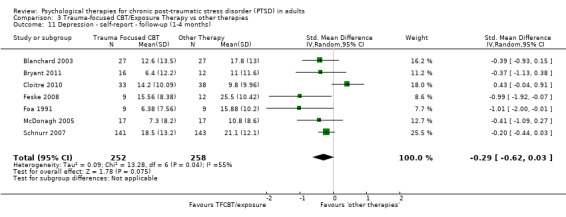
Comparison 3 Trauma‐focused CBT/Exposure Therapy vs other therapies, Outcome 11 Depression ‐ self‐report ‐ follow‐up (1‐4 months).
At 5‐ to 8‐month follow‐up five studies considered this outcome with a total of 443 individuals (Analysis 3.12). There was heterogeneity between these trials (Chi² = 12.31; P = 0.02; I² = 68%), and we used a random‐effects model to pool the data. There were no differences between groups (SMD ‐0.43; 95% CI ‐0.87 to 0.01).
3.12. Analysis.

Comparison 3 Trauma‐focused CBT/Exposure Therapy vs other therapies, Outcome 12 Depression ‐ follow‐up (5‐8 months).
At 9‐ to 12‐month follow‐up
3.5 Anxiety
Seven studies considered this outcome with a total of 539 individuals (Analysis 3.14). There was heterogeneity between these trials (Chi² = 14.75; P = 0.02; I² = 59%), and we used a random‐effects model to pool the data. The individual TFCBT group did better than the 'other therapies' group (SMD ‐0.45; 95% CI ‐0.77 to ‐0.12).
3.14. Analysis.
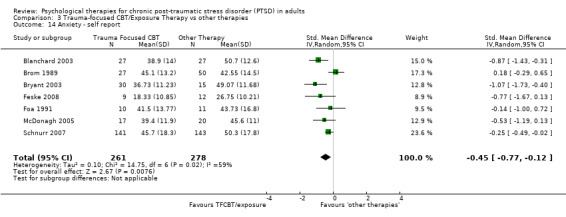
Comparison 3 Trauma‐focused CBT/Exposure Therapy vs other therapies, Outcome 14 Anxiety ‐ self report.
At 1‐ to 4‐month follow‐up five studies considered this outcome with a total of 454 individuals (Analysis 3.15). There was heterogeneity between these trials (Chi² = 8.54; P = 0.07; I² = 53%), and we used a random‐effects model to pool the data. There was no difference between the individual TFCBT and the 'other therapies' groups (SMD ‐0.33; 95% CI ‐0.68 to 0.02).
3.15. Analysis.

Comparison 3 Trauma‐focused CBT/Exposure Therapy vs other therapies, Outcome 15 Anxiety ‐ self‐report ‐ follow‐up (1 ‐ 4 months).
Two trials reported this outcome at 5‐ to 8‐month follow‐up with a total of 329 individuals (Analysis 3.16). There was heterogeneity between these trials (Chi² = 10.28; P = 0.001; I² = 90%), and we used a random‐effects model to pool the data. There was no difference between groups (SMD ‐0.56; 95% CI ‐1.69 to 0.58).
3.16. Analysis.

Comparison 3 Trauma‐focused CBT/Exposure Therapy vs other therapies, Outcome 16 Anxiety ‐ follow‐up (5 ‐ 8 months).
3.6 PTSD diagnosis after treatment
Seven studies with a total of 358 individuals reported this outcome (Analysis 3.17). There was evidence of significant heterogeneity between these trials (Chi² = 9.54; P = 0.15; I² = 37%), and we used a random‐effects model to pool the data. The individual TFCBT group did better than the 'other therapies' group (RR 0.75; 95% CI 0.59 to 0.96).
3.17. Analysis.
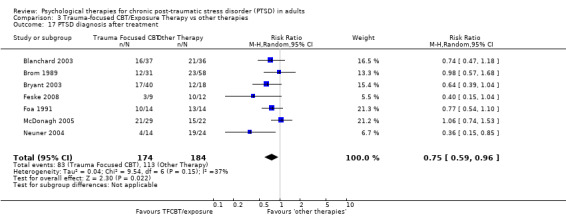
Comparison 3 Trauma‐focused CBT/Exposure Therapy vs other therapies, Outcome 17 PTSD diagnosis after treatment.
3.7 Adverse effects
No studies formally considered adverse effects.
Comparison 4. EMDR versus waitlist/usual care
Eight studies including 301 participants contributed to this comparison.
Primary outcomes
4.1 Clinician‐rated PTSD symptoms
Six studies considered this outcome with a total of 183 individuals (Analysis 4.1). There was evidence of heterogeneity between these trials (Chi² = 31.52; P = 0.00001; I² = 84%) and we used a random‐effects model to pool the data. The EMDR group did better than the waitlist/usual care group immediately after treatment (SMD ‐1.17; 95% CI ‐2.04 to ‐0.30).
4.1. Analysis.

Comparison 4 EMDR vs waitlist/usual care, Outcome 1 Severity of PTSD symptoms ‐ Clinician.
4.2 Drop‐outs
Seven studies with a total of 227 individuals recorded whether individuals left the study early for any reason by group (Analysis 4.2). There was no evidence of heterogeneity between these trials. There was no difference between the EMDR and waitlist/usual care groups (RR 1.05; 95% CI 0.62 to 1.79).
4.2. Analysis.
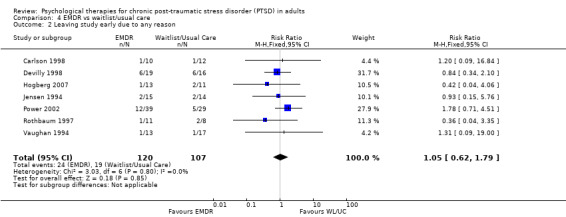
Comparison 4 EMDR vs waitlist/usual care, Outcome 2 Leaving study early due to any reason.
Secondary outcomes
4.3 Self‐reported PTSD symptoms
Six studies considered this outcome with a total of 159 individuals (Analysis 4.3). There was heterogeneity between these trials (Chi² = 30.66; P < 0.00001; I² = 84%) and we used a random‐effects model to pool the data. There was no difference between studies (SMD ‐0.80; 95% CI ‐1.68 to 0.07).
4.3. Analysis.

Comparison 4 EMDR vs waitlist/usual care, Outcome 3 Severity of PTSD symptoms ‐ self report.
4.4 Depression
Seven studies considered this outcome with a total of 226 individuals (Analysis 4.4). There was heterogeneity between these trials (Chi² = 9.61; P = 0.14; I² = 38%), and we used a random‐effects model to pool the data. The EMDR group did better than the control group (SMD ‐1.15; 95% CI ‐1.52 to ‐0.78).
4.4. Analysis.

Comparison 4 EMDR vs waitlist/usual care, Outcome 4 Depression.
4.5 Anxiety
Six studies considered this outcome with a total of 160 individuals (Analysis 4.5). There was no evidence of significant heterogeneity between these trials (Chi² = 3.20; P = 0.67; I² = 0%). The EMDR group did better than the control group (SMD ‐1.02; 95% CI ‐1.36 to ‐0.69).
4.5. Analysis.
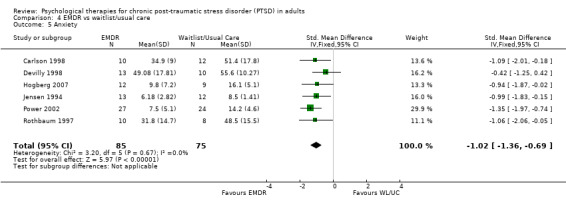
Comparison 4 EMDR vs waitlist/usual care, Outcome 5 Anxiety.
4.7 PTSD diagnosis after treatment
Six studies with a total of 209 individuals reported this outcome (Analysis 4.6). There was no significant heterogeneity between these trials. The EMDR group did better than the controls (RR 0.51; 95% CI 0.42 to 0.62).
4.6. Analysis.
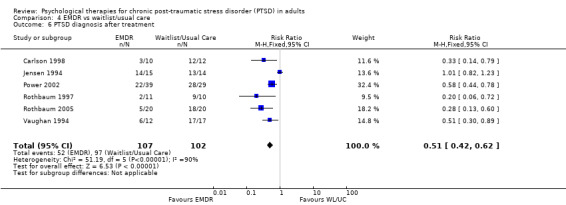
Comparison 4 EMDR vs waitlist/usual care, Outcome 6 PTSD diagnosis after treatment.
4.6 Adverse effects
No studies formally considered adverse effects.
Comparison 5. EMDR versus individual TFCBT/Exposure therapy
Eight studies including 400 participants contributed to this comparison.
Primary outcomes
5.1 Clinician‐rated PTSD symptoms
Seven studies considered this outcome with a total of 327 individuals (Analysis 5.1). There was evidence of heterogeneity between these trials (Chi² = 16.49; P = 0.01; I² = 64%), and we used a random‐effects model to pool the data. There was no difference between groups (SMD ‐0.03; 95% CI ‐0.43 to 0.38).
5.1. Analysis.

Comparison 5 EMDR vs Trauma‐focused CBT, Outcome 1 Severity of PTSD symptoms ‐ clinician.
At 1‐ to 4‐month follow‐up three studies considered this outcome with a total of 76 individuals (Analysis 5.2). There was significant heterogeneity between these trials (Chi² = 5.56; P = 0.06; I² = 64%), and we used a random‐effects model to pool the data. There was no difference between groups (SMD ‐0.19; 95% CI ‐0.97 to 0.58).
5.2. Analysis.

Comparison 5 EMDR vs Trauma‐focused CBT, Outcome 2 Severity of PTSD symptoms ‐ clinician ‐ follow‐up (1 ‐ 4 months).
5.2 Drop‐outs
Eight studies with a total of 400 individuals recorded whether individuals left the study early for any reason by group (Analysis 5.3). There was little heterogeneity (I² = 3%) between these trials. There was no difference between groups (RR 1.00; 95% CI 0.74 to 1.35).
5.3. Analysis.
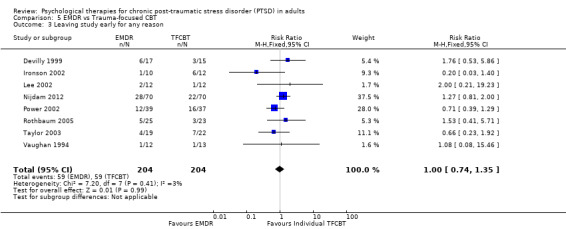
Comparison 5 EMDR vs Trauma‐focused CBT, Outcome 3 Leaving study early for any reason.
Secondary outcomes
5.3 Self‐reported PTSD symptoms
Seven studies considered this outcome with a total of 306 individuals (Analysis 5.4). There was heterogeneity between these trials (Chi² = 8.82; P = 0.18; I² = 32%). There was no significant difference between the EMDR group and the individual TFCBT group immediately after treatment (SMD ‐0.30; 95% CI ‐0.60 to 0.01).
5.4. Analysis.

Comparison 5 EMDR vs Trauma‐focused CBT, Outcome 4 Severity of PTSD symptoms ‐ self report.
At 1‐ to 4‐month follow‐up five studies considered this outcome with a total of 111 individuals (Analysis 5.5). There was evidence of heterogeneity (Chi² = 8.46; P = 0.08; I² = 53%), and we used a random‐effects model to pool the data. There was no difference between groups (SMD ‐0.04; 95% CI ‐0.61 to 0.52).
5.5. Analysis.
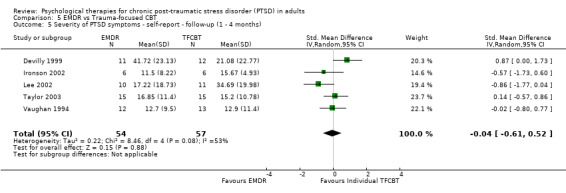
Comparison 5 EMDR vs Trauma‐focused CBT, Outcome 5 Severity of PTSD symptoms ‐ self‐report ‐ follow‐up (1 ‐ 4 months).
At 9‐ to 12‐mont follow‐up
5.4 Depression
Eight studies considered this outcome with a total of 346 individuals (Analysis 5.6. There was heterogeneity between these trials (Chi² = 24.04; P = 0.001; I² = 71%), and we used a random‐effects model to pool the data. There was no difference between groups (SMD ‐0.31; 95% CI ‐0.75 to 0.13).
5.6. Analysis.
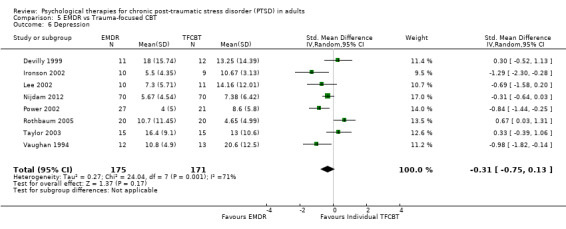
Comparison 5 EMDR vs Trauma‐focused CBT, Outcome 6 Depression.
At 1‐ to 4‐month follow‐up five studies considered this outcome with a total of 111 individuals (Analysis 5.7). There was heterogeneity between these trials (Chi² = 6.93; P = 0.14; I² = 42%). There was no difference between groups (SMD ‐0.13; 95% CI ‐0.64 to 0.38).
5.7. Analysis.
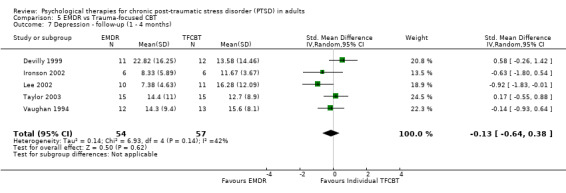
Comparison 5 EMDR vs Trauma‐focused CBT, Outcome 7 Depression ‐ follow‐up (1 ‐ 4 months).
5.5 Anxiety
Four studies considered this outcome with a total of 236 individuals (Analysis 5.8). There was little heterogeneity between these trials (Chi² = 1.94; P = 0.58; I² = 0%). The EMDR group did better than the TFCBT group (SMD ‐0.28; 95% CI ‐0.53 to ‐0.02).
5.8. Analysis.

Comparison 5 EMDR vs Trauma‐focused CBT, Outcome 8 Anxiety.
At 1‐ to 4‐month follow‐up two studies considered this outcome with a total of 48 individuals (Analysis 5.9). There was little heterogeneity between these trials (Chi² = 0.70; P = 0.40; I² = 0%). There was no difference between groups (SMD 0.24; 95% CI ‐0.33 to 0.81).
5.9. Analysis.

Comparison 5 EMDR vs Trauma‐focused CBT, Outcome 9 Anxiety ‐ follow‐up (1 ‐ 4 months).
5.6 PTSD diagnosis after treatment
Eight studies with a total of 400 individuals reported this outcome (Analysis 5.10). There was heterogeneity between these trials (Chi² = 15.56; P = 0.03; I² = 55%), and we used a random‐effects model to pool the data. There was no difference between the groups (RR 0.95; 95% CI 0.74 to 1.22).
5.10. Analysis.
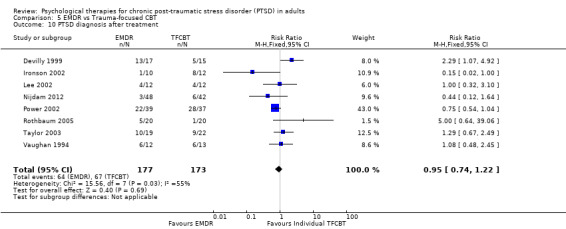
Comparison 5 EMDR vs Trauma‐focused CBT, Outcome 10 PTSD diagnosis after treatment.
5.7 Adverse effects
No studies formally considered adverse effects.
Comparison 6. EMDR versus non‐TFCBT
Three studies including 84 participants contributed to this comparison.
Primary outcomes
6.1 Clinician‐rated PTSD symptoms
Two studies considered this outcome with a total of 53 individuals (Analysis 6.1). There was little heterogeneity between these trials (Chi² = 0.69; P = 0.41; I² = 0%). There was no difference between groups (SMD ‐0.35; 95% CI ‐0.90 to 0.19).
6.1. Analysis.

Comparison 6 EMDR vs non‐TFCBT, Outcome 1 Severity of PTSD symptoms ‐ clinician.
At 1‐ to 4‐month follow‐up three studies considered this outcome with a total of 71 individuals (Analysis 6.2). There was heterogeneity between these trials (Chi² = 6.16; P = 0.05; I² = 68%), and we used a random‐effects model to pool the data. There was no difference between groups (SMD ‐0.74; 95% CI ‐1.64 to 0.15).
6.2. Analysis.
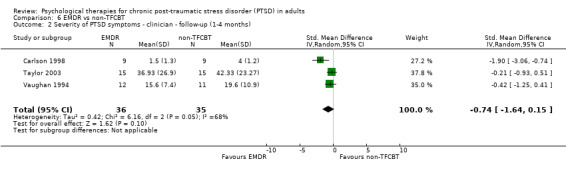
Comparison 6 EMDR vs non‐TFCBT, Outcome 2 Severity of PTSD symptoms ‐ clinician ‐ follow‐up (1‐4 months).
6.2 Drop‐outs
Three studies with a total of 84 individuals recorded whether individuals left the study early for any reason by group (Analysis 6.3). There was little heterogeneity between these trials. There was no difference between groups (RR 1.03; 95% CI 0.37 to 2.88).
6.3. Analysis.

Comparison 6 EMDR vs non‐TFCBT, Outcome 3 Leaving the study early for any reason.
Secondary outcomes
6.3 Self‐reported PTSD symptoms
Three studies considered this outcome with a total of 75 individuals (Analysis 6.4). There was little heterogeneity between these trials (Chi² = 0.64; P = 0.73; I² = 0%). There was no difference between groups (SMD ‐0.40; 95% CI ‐0.86 to 0.06).
6.4. Analysis.
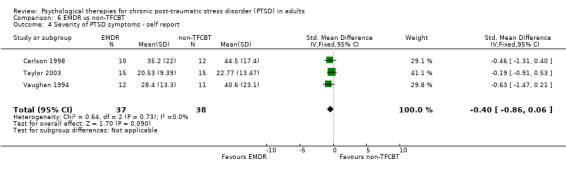
Comparison 6 EMDR vs non‐TFCBT, Outcome 4 Severity of PTSD symptoms ‐ self report.
At 1‐ to 4‐month follow‐up three studies considered this outcome with a total of 75 individuals (Analysis 6.5). There was little heterogeneity between these trials (Chi² = 0.89; P = 0.64; I² = 0%).The EMDR group did significantly better than the non‐TFCBT group immediately after treatment (SMD ‐0.52; 95% CI ‐0.98 to ‐0.05).
6.5. Analysis.

Comparison 6 EMDR vs non‐TFCBT, Outcome 5 Severity of PTSD symptoms ‐ self‐report ‐ follow‐up (1 ‐ 4 months).
6.4 Depression
Three studies considered this outcome with a total of 75 individuals (Analysis 6.6). There was little heterogeneity between these trials. (Chi² = 1.02; P = 0.60; I² = 0%). The EMDR group did better than the non‐TFCBT group (SMD ‐0.67; 95% CI ‐1.14 to ‐0.20).
6.6. Analysis.
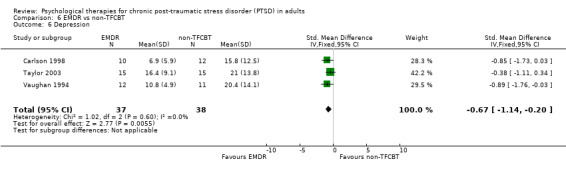
Comparison 6 EMDR vs non‐TFCBT, Outcome 6 Depression.
At 1‐ to 4‐month follow‐up three studies considered this outcome with a total of 75 individuals (Analysis 6.7). There was heterogeneity between these trials. (Chi² = 3.45; P = 0.18; I² = 42%), and we used a random‐effects model to pool the data. There was no difference between groups (SMD ‐0.25; 95% CI ‐0.86 to 0.36).
6.7. Analysis.

Comparison 6 EMDR vs non‐TFCBT, Outcome 7 Depression ‐ follow‐up (1 ‐ 4 months).
6.5 Anxiety
Two studies considered this outcome with a total of 45 individuals (Analysis 6.8). There was little heterogeneity between these trials (Chi² = 0.37; P = 0.54; I² = 0%). The EMDR group did better than the non‐TFCBT group (SMD ‐0.75; 95% CI ‐1.36 to ‐0.13).
6.8. Analysis.

Comparison 6 EMDR vs non‐TFCBT, Outcome 8 Anxiety.
At 1‐ to 4‐month follow‐up two studies considered this outcome with a total of 45 individuals (Analysis 6.9). There was heterogeneity between these trials (Chi² = 8.09; P = 0.004; I² = 88%), and we used a random‐effects model to pool the data. There was no difference between groups (SMD ‐0.42; 95% CI ‐2.21 to 1.37).
6.9. Analysis.

Comparison 6 EMDR vs non‐TFCBT, Outcome 9 Anxiety ‐ follow‐up (1 ‐ 4 months).
6.6 PTSD diagnosis after treatment
Three studies with a total of 84 individuals reported this outcome (Analysis 6.10). There was significant heterogeneity between these trials. There was no difference between groups ((RR 0.71; 95% CI 0.41 to 1.22).
6.10. Analysis.
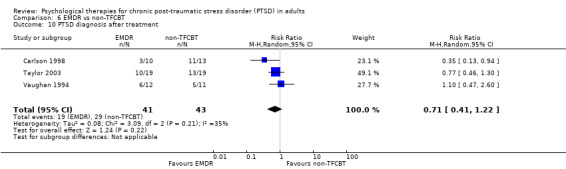
Comparison 6 EMDR vs non‐TFCBT, Outcome 10 PTSD diagnosis after treatment.
6.7 Adverse effects
No studies formally considered adverse effects.
Comparison 7. EMDR versus 'other therapies'
Two studies including 127 participants contributed to this comparison.
Primary outcomes
7.1 Clinician rated PTSD symptoms
No studies formally considered this outcome.
7.2 Drop‐outs
Two studies with a total of 127 individuals recorded whether individuals left the study early for any reason by group (Analysis 7.1). There was little heterogeneity between these trials. There was no difference between groups (RR 1.48; 95% CI 0.26 to 8.54).
7.1. Analysis.

Comparison 7 EMDR vs other therapies, Outcome 1 Leaving study early for any reason.
Secondary outcomes
7.3 Self‐reported PTSD symptoms
Two studies considered this outcome with a total of 124 individuals (Analysis 7.2). There was little heterogeneity between these trials (Chi² = 0.19; P = 0.66; I² = 0%). The EMDR group did better than the 'other therapies' group immediately after treatment (SMD ‐0.84; 95% CI ‐1.21 to ‐0.47).
7.2. Analysis.

Comparison 7 EMDR vs other therapies, Outcome 2 Severity of PTSD symptoms ‐ self report.
7.4 Depression
Two studies considered this outcome with a total of 127 individuals (Analysis 7.3). There was little heterogeneity between these trials (Chi² = 0.05; P = 0.82; I² = 0%). The EMDR group did better than the 'other therapies' group (SMD ‐0.67; 95% CI ‐1.03 to ‐0.32).
7.3. Analysis.
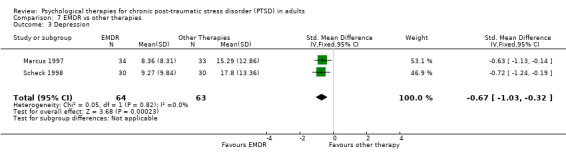
Comparison 7 EMDR vs other therapies, Outcome 3 Depression.
7.5 Anxiety
Two studies considered this outcome with a total of 126 individuals (Analysis 7.4). There was little heterogeneity between these trials (Chi² = 0.10; P = 0.75; I² = 0%). The EMDR group did better than the 'other therapies' group (SMD ‐0.72; 95% CI ‐1.08 to ‐0.36).
7.4. Analysis.

Comparison 7 EMDR vs other therapies, Outcome 4 Anxiety.
7.6 PTSD diagnosis after treatment (Analysis 7.5)
7.5. Analysis.

Comparison 7 EMDR vs other therapies, Outcome 5 PTSD diagnosis after treatment.
7.7 Adverse effects
No studies formally considered adverse effects.
Comparison 8. Non‐TFCBT versus waitlist/usual care
Five studies including 141 participants contributed to this comparison.
Primary outcomes
8.1 Clinician‐rated PTSD symptoms
Four studies considered this outcome with a total of 106 individuals (Analysis 8.1). There was heterogeneity between these trials (Chi² = 4.62; P = 0.2; I² = 35%), and we used a random‐effects model to pool the data. The non‐TFCBT group did better than the controls (SMD ‐1.22; 95% CI ‐1.76 to ‐0.69).
8.1. Analysis.

Comparison 8 Non‐TFCBT vs waitlist/usual care, Outcome 1 Severity of PTSD symptoms ‐ Clinician.
8.2 Drop‐outs
Four studies with a total of 121 individuals recorded whether individuals left the study early for any reason by group (Analysis 8.2). There was no significant heterogeneity between these trials (Chi² = 1.10; P = 0.89; I² = 0%). There was no difference between the groups (RR 1.96; 95% CI 0.70 to 5.48).
8.2. Analysis.
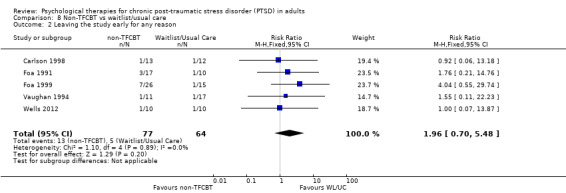
Comparison 8 Non‐TFCBT vs waitlist/usual care, Outcome 2 Leaving the study early for any reason.
Secondary outcomes
8.3 Self‐reported PTSD symptoms
Two studies considered this outcome with a total of 44 individuals (Analysis 8.3). There was considerable heterogeneity between the groups (Chi² = 11.83; P = 0.0006; I² = 92%), and we used a random‐effects model to pool the data. There was no difference between the non‐TFCBT group and the waitlist/usual care group immediately after treatment (SMD ‐0.86; 95% CI ‐3.27 to 1.55).
8.3. Analysis.
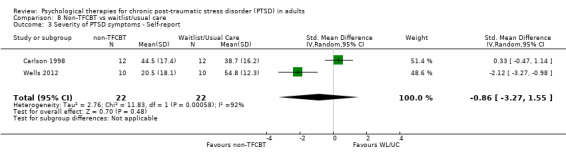
Comparison 8 Non‐TFCBT vs waitlist/usual care, Outcome 3 Severity of PTSD symptoms ‐ Self‐report.
8.4 Depression
Five studies considered this outcome with a total of 129 individuals (Analysis 8.4). There was heterogeneity between these trials (Chi² = 7.04; P = 0.13; I² = 43%), and we used a random‐effects model to pool the data. The non‐TFCBT group did better than the waitlist/usual care group immediately after treatment (SMD ‐0.93; 95% CI ‐1.43 to ‐0.42).
8.4. Analysis.
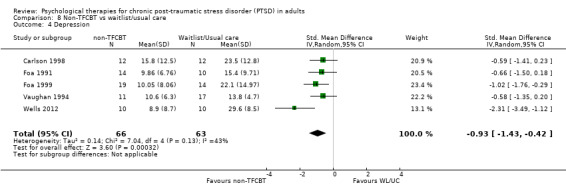
Comparison 8 Non‐TFCBT vs waitlist/usual care, Outcome 4 Depression.
8.5 Anxiety
Four studies considered this outcome with a total of 102 individuals (Analysis 8.5). There was no heterogeneity between these trials (Chi² = 2.38; P = 0.50; I² = 0%). Non‐TFCBT did better than the waitlist/usual care group immediately after treatment (SMD ‐0.83; 95% CI ‐1.24 to ‐0.42).
8.5. Analysis.

Comparison 8 Non‐TFCBT vs waitlist/usual care, Outcome 5 Anxiety.
8.6 PTSD diagnosis after treatment
Four studies with a total of 121 individuals reported this outcome (Analysis 8.6). There was heterogeneity between these trials (Chi² = 6.15; P = 0.10; I² = 51%), and we used a random‐effects model to pool the data. The non‐TFCBT group did better than the waitlist/usual care group (RR 0.65; 95% CI 0.50 to 0.86).
8.6. Analysis.

Comparison 8 Non‐TFCBT vs waitlist/usual care, Outcome 6 PTSD diagnosis after treatment.
8.7 Adverse effects
No studies formally considered adverse effects.
Comparison 9. Non‐TFCBT versus other therapies
One study including 31 participants contributed to this comparison.
Primary outcomes
9.1 Clinician‐rated PTSD symptoms
One study considered this outcome with a total of 25 individuals (Analysis 9.1). The stress non‐TFCBT group did better than the other therapies group immediately after treatment (SMD ‐1.22; 95% CI ‐2.09 to ‐0.35).
9.1. Analysis.

Comparison 9 Non‐TFCBT vs other therapies, Outcome 1 Severity of PTSD symptoms ‐ Clincian.
At 1‐ to 4‐month follow‐up one study considered this outcome with a total of 18 individuals (Analysis 9.2). The stress non‐TFCBT group did no better than the 'other therapies' group (SMD ‐0.38; 95% CI ‐1.31 to 0.55).
9.2. Analysis.

Comparison 9 Non‐TFCBT vs other therapies, Outcome 2 Severity of PTSD symptoms ‐ clinician ‐ follow‐up (3 months).
9.2 Drop‐outs
One study with a total of 31 individuals recorded whether individuals left the study early for any reason by group (Analysis 9.3). There was no difference between groups (RR 0.82; 95% CI 0.20 to 3.46).
9.3. Analysis.

Comparison 9 Non‐TFCBT vs other therapies, Outcome 3 Leaving the study early for any reason.
Secondary outcomes
9.3 Self‐reported PTSD symptoms
No studies considered this outcome.
9.4 Depression
One study considered this outcome with a total of 25 individuals (Analysis 9.4). There was no difference between groups (SMD ‐0.51; 95% CI ‐1.31 to 0.30).
9.4. Analysis.

Comparison 9 Non‐TFCBT vs other therapies, Outcome 4 Depression ‐ self report.
At 1‐ to 4‐month follow‐up one study considered this outcome with a total of 18 individuals (Analysis 9.5). There was no difference between groups (SMD ‐0.48; 95% CI ‐1.42 to 0.46).
9.5. Analysis.

Comparison 9 Non‐TFCBT vs other therapies, Outcome 5 Depression ‐ self report ‐ follow‐up (3 months).
9.5 Anxiety
One study considered this outcome with a total of 25 individuals (Analysis 9.6). There was no difference between groups (SMD ‐0.51; 95% CI ‐1.32 to 0.29).
9.6. Analysis.

Comparison 9 Non‐TFCBT vs other therapies, Outcome 6 Anxiety ‐ self report.
At 1‐ to 4‐month follow‐up one study considered this outcome with a total of 18 individuals (Analysis 9.7). There was no difference between groups (SMD ‐0.68; 95% CI ‐1.64 to 0.28).
9.7. Analysis.
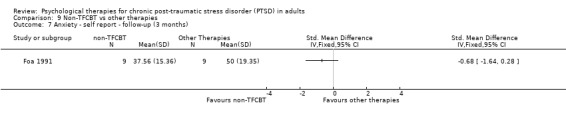
Comparison 9 Non‐TFCBT vs other therapies, Outcome 7 Anxiety ‐ self report ‐ follow‐up (3 months).
9.6 PTSD diagnosis after treatment
One study with a total of 31 individuals reported this outcome (Analysis 9.8). There was no difference between groups (RR 0.58; 95% CI 0.30 to 1.11).
9.8. Analysis.

Comparison 9 Non‐TFCBT vs other therapies, Outcome 8 PTSD diagnosis after treatment.
9.7 Adverse effects
No studies formally considered adverse effects.
Comparison 10. Group TFCBT versus waitlist/usual care
Seven studies including 573 participants contributed to this comparison.
Primary outcomes
10.1 Clinician‐rated PTSD symptoms
Three studies considered this outcome with a total of 185 individuals (Analysis 10.1). There was heterogeneity between these trials (Chi² = 15.60; P = 0.0004; I² = 87%), and we used a random‐effects model to pool the data. The Group TFCBT group did better than the waitlist/usual care group immediately after treatment (SMD ‐1.28; 95% CI ‐2.25 to ‐0.31).
10.1. Analysis.

Comparison 10 Group TFCBT vs waitlist/usual care/minimal contact, Outcome 1 Clinician‐rated.
At 5‐ to 8‐month follow‐up one study compared this outcome with 97 individuals (Analysis 10.2). The Group TFCBT group did better than the waitlist/usual care group (SMD ‐0.72; 95% CI ‐1.14 to ‐0.31).
10.2. Analysis.

Comparison 10 Group TFCBT vs waitlist/usual care/minimal contact, Outcome 2 Severity of PTSD 5 ‐ 8 month follow‐up.
10.2 Drop‐outs
Seven studies with a total of 573 individuals recorded whether individuals left the study early for any reason by group (Analysis 10.3). There was no significant heterogeneity between these trials (Chi² = 2.28; P = 0.81; I² = 0%). There was no difference between the Group TFCBT group and the waitlist/usual care group (RR 1.21; 95% CI 0.94 to 1.55).
10.3. Analysis.

Comparison 10 Group TFCBT vs waitlist/usual care/minimal contact, Outcome 3 Leaving the study early for any reason.
Secondary outcomes
10.3 Self‐reported PTSD symptoms
Six studies considered this outcome with a total of 274 individuals (Analysis 10.4). There was heterogeneity between these trials (Chi² = 17.53; P = 0.004; I² = 71%), and we used a random‐effects model to pool the data. The Group TFCBT group did better than the waitlist/usual care group immediately after treatment (SMD ‐1.20; 95% CI ‐1.70 to ‐0.69).
10.4. Analysis.
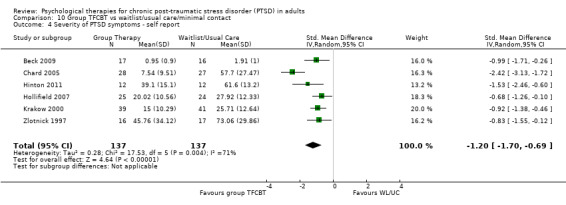
Comparison 10 Group TFCBT vs waitlist/usual care/minimal contact, Outcome 4 Severity of PTSD symptoms ‐ self report.
At 1‐ to 4‐month follow‐up two studies compared this outcome with 73 individuals (Analysis 10.5). There was some heterogeneity between these trials (Chi² = 1.45; P = 0.23; I² = 31%). The Group TFCBT group did better than the waitlist/usual care group immediately after treatment (SMD ‐1.14; 95% CI ‐1.78 to ‐ 0.50).
10.5. Analysis.

Comparison 10 Group TFCBT vs waitlist/usual care/minimal contact, Outcome 5 Severity of PTSD ‐ self report ‐ 1 ‐ 4 months.
10.4 Depression
Three studies with a total of 137 individuals reported this outcome (Analysis 10.6). There was heterogeneity between these trials (Chi² = 9.91; P = 0.007; I² = 80%), and we used a random‐effects model to pool the data. The Group TFCBT group did significantly better than the waitlist/usual care group (SMD ‐1.15; 95% CI ‐1.98 to ‐0.32).
10.6. Analysis.

Comparison 10 Group TFCBT vs waitlist/usual care/minimal contact, Outcome 6 Depression.
At 1‐ to 4‐month follow‐up one study compared this outcome with 49 individuals (Analysis 10.7). The Group TFCBT group did better than the waitlist/usual care group (SMD ‐0.62; 95% CI ‐1.00 to ‐0.24).
10.7. Analysis.

Comparison 10 Group TFCBT vs waitlist/usual care/minimal contact, Outcome 7 Depression 1 ‐ 4 month follow‐up.
10.5 Anxiety
Three studies with a total of 106 individuals reported this outcome (Analysis 10.8). There was little heterogeneity between these trials. The Group TFCBT group did significantly better than the waitlist/usual care group immediately after treatment (SMD ‐0.66; 95% CI ‐1.06 to ‐0.27).
10.8. Analysis.
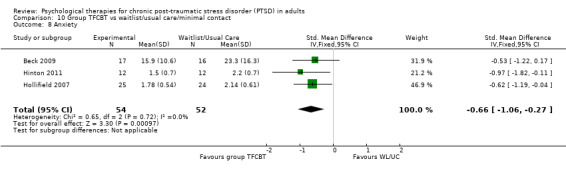
Comparison 10 Group TFCBT vs waitlist/usual care/minimal contact, Outcome 8 Anxiety.
At 1‐ to 4‐month follow‐up two studies compared this outcome with 61 individuals (Analysis 10.9). There was little heterogeneity between these trials (Chi² = 1.20; P = 0.27; I² = 17%). The Group TFCBT group did significantly better than the waitlist/usual care group (SMD ‐0.43; 95% CI ‐0.72 to ‐0.14).
10.9. Analysis.

Comparison 10 Group TFCBT vs waitlist/usual care/minimal contact, Outcome 9 Anxiety 1 ‐ 4 month follow‐up.
10.6 PTSD diagnosis after treatment
One study with a total of 48 individuals reported this outcome (Analysis 10.10).There was no significant difference between the Group TFCBT group and the waitlist/usual care group (RR 0.56; 95% CI 0.31 to 1.01).
10.10. Analysis.
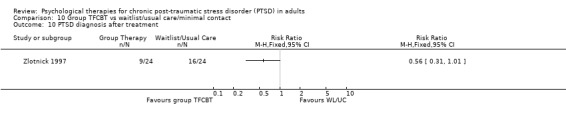
Comparison 10 Group TFCBT vs waitlist/usual care/minimal contact, Outcome 10 PTSD diagnosis after treatment.
10.7 Adverse effects
No studies formally considered adverse effects.
Comparison 11. Group TFCBT versus group non‐TF CBT
One study including 360 participants contributed to this comparison.
Primary outcomes
11.1 Clinician‐rated PTSD symptoms
One study considered this outcome with a total of 325 individuals (Analysis 11.1). There was no difference between the Group trauma‐focused CBT and Group non‐trauma‐focused CBT (SMD ‐0.12; 95% CI ‐0.34 to 0.10).
11.1. Analysis.
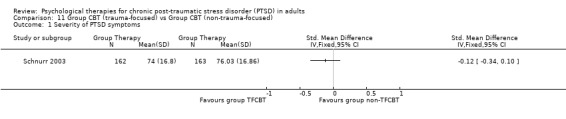
Comparison 11 Group CBT (trauma‐focused) vs Group CBT (non‐trauma‐focused), Outcome 1 Severity of PTSD symptoms.
11.2 Drop‐outs
One study with a total of 360 individuals recorded whether individuals left the study early for any reason by group (Analysis 11.2). There was no significant difference between the Group trauma‐focused CBT and Group non‐trauma‐focused CBT groups (RR 1.38; 95% CI 1.00 to 1.90).
11.2. Analysis.
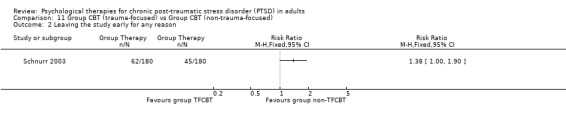
Comparison 11 Group CBT (trauma‐focused) vs Group CBT (non‐trauma‐focused), Outcome 2 Leaving the study early for any reason.
Secondary outcomes
11.3 Self‐reported PTSD symptoms
No studies considered this outcome.
11.4 Depression
No studies considered this outcome.
11.5 Anxiety
No studies considered this outcome.
11.6 PTSD diagnosis after treatment
One study with a total of 360 individuals reported this outcome (Analysis 11.3). There was no difference between the Group trauma‐focused CBT and Group non‐trauma‐focused CBT groups (RR 0.98; 95% CI 0.83 to 1.16).
11.3. Analysis.

Comparison 11 Group CBT (trauma‐focused) vs Group CBT (non‐trauma‐focused), Outcome 3 PTSD diagnosis after treatment.
11.7 Adverse effects
No studies formally considered adverse effects.
Comparison 12. Other therapies versus waitlist/usual care
Four studies including 211 participants contributed to this comparison.
Primary outcomes
12.1 Clinician‐rated PTSD symptoms
Three studies considered this outcome with a total of 112 individuals (Analysis 12.1). There was no heterogeneity between these trials (Chi² = 1.61; P = 0.45; I² = 0%). The 'other therapies' group did better than the waitlist/usual care group immediately after treatment (SMD ‐0.58; 95% CI ‐0.96 to ‐0.20).
12.1. Analysis.

Comparison 12 Other therapies vs waitlist/usual care, Outcome 1 Severity of PTSD symptoms ‐ clinician.
12.2 Drop‐outs
Four studies with a total of 211 individuals recorded whether individuals left the study early for any reason by group (Analysis 12.2). There was no heterogeneity between these trials. The waitlist group did better than the 'other therapies' group (RR 2.45; 95% CI 0.99 to 6.10).
12.2. Analysis.

Comparison 12 Other therapies vs waitlist/usual care, Outcome 2 Leaving the study early due to any reason.
Secondary outcomes
12.3 Self‐reported PTSD symptoms
Two studies considered this outcome with a total of 132 individuals (Analysis 12.3). There was no heterogeneity between these trials (Chi² = 0.29; P = 0.59; I² = 0%). The 'other therapies' group did better than the waitlist/usual care group immediately after treatment (SMD ‐0.61; 95% CI ‐0.98 to ‐0.24).
12.3. Analysis.
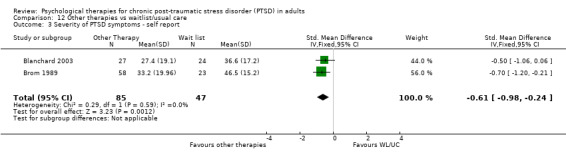
Comparison 12 Other therapies vs waitlist/usual care, Outcome 3 Severity of PTSD symptoms ‐ self report.
12.4 Depression
Three studies considered this outcome with a total of 112 individuals (Analysis 12.4). There was little heterogeneity between these trials (Chi² = 2.62; P = 0.27; I² = 24%). The 'other therapies' group did better than the waitlist/usual care group immediately after treatment (SMD ‐0.45; 95% CI ‐0.83 to ‐0.07).
12.4. Analysis.
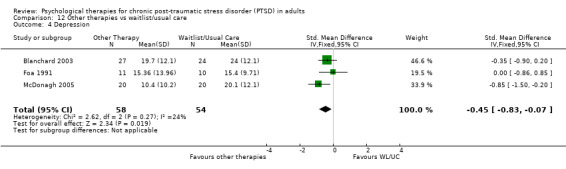
Comparison 12 Other therapies vs waitlist/usual care, Outcome 4 Depression.
12.5 Anxiety
Four studies considered this outcome with a total of 193 individuals (Analysis 12.5). There was no heterogeneity between these trials (Chi² = 0.70; P = 0.87; I² = 0%). The 'other therapies' group did significantly better than the waitlist/usual care group immediately after treatment (SMD ‐0.52; 95% CI ‐0.82 to ‐0.22).
12.5. Analysis.
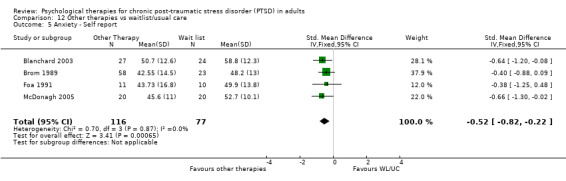
Comparison 12 Other therapies vs waitlist/usual care, Outcome 5 Anxiety ‐ Self report.
12.6 PTSD diagnosis after treatment
Four studies with a total of 210 individuals reported this outcome (Analysis 12.6). There was heterogeneity between these trials (Chi² = 8.34; P = 0.04; I² = 64%), and we used a random‐effects model to pool the data. There was no difference between the 'other therapies' and the waitlist/usual care group (RR 0.80; 95% CI 0.61 to 1.05).
12.6. Analysis.

Comparison 12 Other therapies vs waitlist/usual care, Outcome 6 PTSD diagnosis after treatment.
12.7 Adverse effects
No studies formally considered adverse effects.
Comparison 13. Group non‐TFCBT versus waitlist/usual care
One study including 47 participants contributed to this comparison.
Primary outcomes
13.1 Clinician‐rated PTSD symptoms
No studies considered this outcome.
13.2 Drop‐outs
One study with a total of 47 individuals recorded whether individuals left the study early for any reason by group (Analysis 13.1). There was no difference between groups (RR 1.76; 95% CI 0.17 to 18.11).
13.1. Analysis.
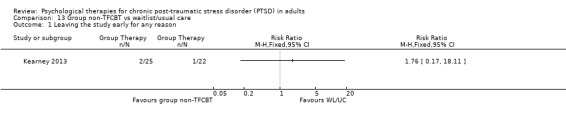
Comparison 13 Group non‐TFCBT vs waitlist/usual care, Outcome 1 Leaving the study early for any reason.
Secondary outcomes
13.3 Self‐reported PTSD symptoms
One study considered this outcome with a total of 47 individuals (Analysis 13.2). There was no difference between groups (SMD ‐0.49; 95% CI ‐1.07 to 0.09).
13.2. Analysis.

Comparison 13 Group non‐TFCBT vs waitlist/usual care, Outcome 2 Severity of PTSD symptoms ‐ self report.
At 1‐ to 4‐month follow‐up one study considered this outcome with a total of 47 individuals (Analysis 13.3). There was no difference between groups (SMD ‐0.40; 95% CI ‐0.98 to 0.18).
13.3. Analysis.
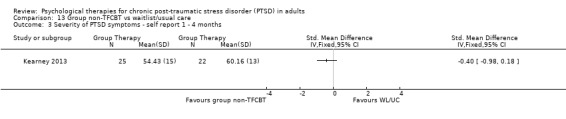
Comparison 13 Group non‐TFCBT vs waitlist/usual care, Outcome 3 Severity of PTSD symptoms ‐ self report 1 ‐ 4 months.
13.4 Depression
One study considered this outcome with a total of 47 individuals (Analysis 13.4). There was no difference between groups (SMD ‐0.06; 95% CI ‐0.64 to 0.51).
13.4. Analysis.
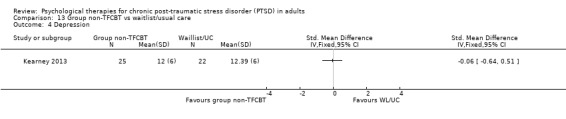
Comparison 13 Group non‐TFCBT vs waitlist/usual care, Outcome 4 Depression.
At 1‐ to 4‐month follow‐up one study considered this outcome with a total of 47 individuals (Analysis 13.5). There was no difference between groups (SMD ‐0.03; 95% CI ‐0.60 to 0.54).
13.5. Analysis.

Comparison 13 Group non‐TFCBT vs waitlist/usual care, Outcome 5 Depression ‐ 1 ‐ 4 months.
13.5 Anxiety
No studies considered this outcome.
13.6 PTSD diagnosis after treatment
No studies considered this outcome.
13.7 Adverse effects
No studies formally considered adverse effects.
Comparison 14. Individual TFCBT versus group TFCBT
No studies made this comparison.
Comparison 15. Individual TFCBT versus group non‐TFCBT
No studies made this comparison.
Comparison 16. EMDR versus group TFCBT
No studies made this comparison.
Comparison 17. EMDR versus group non‐TFCBT
No studies made this comparison.
Comparison 18. Individual non‐TFCBT versus group TFCBT
No studies made this comparison.
Comparison 19. Individual non‐TFCBT versus group non‐TFCBT
No studies made this comparison.
19. Risk of bias sensitivity analysis
19.1 Comparison 1. Individual TFCBT/Exposure therapy versus waitlist/usual care
Clinician‐rated PTSD symptoms
Only one trial ( Basoglu 2005) including 59 participants had a low risk of bias for sequence generation, allocation concealment and blinding of the outcome assessor. Analysis restricted only to this trial (Analysis 1.17) showed no difference between TFCBT and waitlist/usual care (SMD ‐0.44; 95% CI ‐0.95 to 0.08), which differs from the overall meta‐analysis, which showed a statistically significant difference in favour of TFCBT (SMD ‐1.62; 95% CI ‐2.03 to ‐1.21). However, the intervention was a single session of TFCBT.
1.17. Analysis.

Comparison 1 Trauma‐focused CBT/Exposure therapy vs waitlist/usual care, Outcome 17 Sensitivity analysis ‐ clinician‐rated PTSD symptoms ‐ studies at low risk of bias only.
Drop‐outs
The intervention was a single session of TFCBT. On this basis, drop‐out was not a relevant comparison.
19.2 Comparison 2. TFCBT versus non‐TFCBT
Fewer than 10 studies made this comparison.
19.3 Comparison 3. TFCBT versus other therapies
Clinician‐rated PTSD symptoms
Only one trial (Bryant 2003) including 58 participants had a low risk of bias in terms of sequence generation, allocation concealment and blinding of the outcome assessor. Analysis restricted only to this trial (Analysis 3.19) favoured TFCBT (SMD ‐1.52; 95% CI ‐2.14 to ‐0.89).
3.19. Analysis.
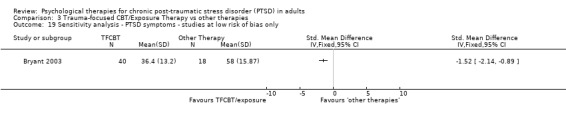
Comparison 3 Trauma‐focused CBT/Exposure Therapy vs other therapies, Outcome 19 Sensitivity analysis ‐ PTSD symptoms ‐ studies at low risk of bias only.
Drop‐outs
One study with a total of 58 participants had a low risk of bias in terms of sequence generation, allocation concealment and blinding of the outcome assessor. There was no difference between TFCBT and other therapy when the analysis was restricted to this study (Analysis 3.20) (RR 1.50; 95% CI 0.47 to 4.8).
3.20. Analysis.
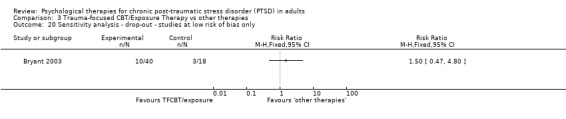
Comparison 3 Trauma‐focused CBT/Exposure Therapy vs other therapies, Outcome 20 Sensitivity analysis ‐ drop‐out ‐ studies at low risk of bias only.
19.4 Comparison 4. EMDR versus waitlist/usual care
Fewer than 10 studies made this comparison.
19.5 Comparison 5. EMDR versus individual TFCBT/Exposure therapy
Fewer than 10 studies made this comparison.
19.6 Comparison 6. EMDR versus non‐TFCBT
Fewer than 10 studies made this comparison.
19.7 Comparison 7. EMDR versus other therapies
Fewer than 10 studies made this comparison.
19.8 Comparison 8. Non‐TFCBT versus waitlist/usual care
Fewer than 10 studies made this comparison.
19.9 Comparison 9. Non‐TFCBT versus other therapies
Fewer than 10 studies made this comparison.
19.10 Comparison 10. Group TFCBT versus waitlist/usual care
Fewer than 10 studies made this comparison.
19.11 Comparison 11. Group TFCBT versus group non‐TFCBT
Fewer than 10 studies made this comparison.
19.12 Comparison 12. Other therapies versus waitlist/usual care
Fewer than 10 studies made this comparison.
19.13 Comparison 13. Group non‐TFCBT versus waitlist/usual care
Fewer than 10 studies made this comparison.
20. Clinical heterogeneity sensitivity analyses
In order to explore clinical heterogeneity, we conducted two subgroup analyses for the two comparisons including more than 10 studies.
20.1 Comparison 1. Individual TFCBT/Exposure therapy versus waitlist/usual care
Twenty‐eight studies considered this outcome with a total of 1256 individuals (Analysis 1.1.1). There was heterogeneity between these trials (Chi² = 237.95; P = 0.00001; I² = 89%), and we used a random‐effects model to pool the data. The individual TFCBT group did better than the waitlist/usual care group immediately after treatment (SMD ‐1.62; 95% CI ‐2.03 to ‐1.21).
Women‐only studies Nine studies met this criterion, with a total of 562 women (Analysis 1.1.2). There was heterogeneity between these trials (Chi² = 37.39; P = 0.00001; I² = 79%), and we used a random‐effects model to pool the data.The individual TFCBT group did better than the waitlist/usual care group immediately after treatment (SMD ‐1.83; 95% CI ‐2.31 to ‐1.36), demonstrating a larger difference in favour of individual TFCBT than in the overall analyses.
Studies excluding Vietnam war veterans Twenty‐seven studies met this criterion, with a total of 1232 individuals (Analysis 1.1.3). There was heterogeneity between these trials (Chi² = 230.39; P = 0.00001; I² = 89%), and we used a random‐effects model to pool the data.The individual TFCBT group did significantly better than the waitlist/usual care group immediately after treatment (SMD ‐1.67; 95% CI ‐2.09 to ‐1.25), demonstrating little difference from the overall analyses. Excluding these two trials made little difference to the observed statistically significant heterogeneity or to the effect estimate.
20.2 Comparison 3. TFCBT versus other therapies
Ten studies considered this outcome with a total of 608 individuals (Analysis 3.1). There was evidence of heterogeneity between these trials (Chi² = 25.08; P = 0.003; I² = 64%), and we used a random‐effects model to pool the data The individual TFCBT group did better than the 'other therapies' group immediately after treatment (SMD ‐0.46; 95% CI ‐0.79 to ‐0.13).
Women‐only studies (sexual assault/abuse) Three studies met this criterion, with a total of 129 women (Analysis 3.21). There was no difference between groups (SMD 0.03; 95% CI ‐0.42 to 0.47).
3.21. Analysis.
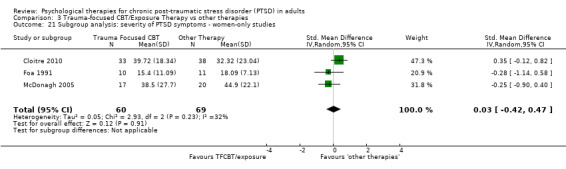
Comparison 3 Trauma‐focused CBT/Exposure Therapy vs other therapies, Outcome 21 Subgroup analysis: severity of PTSD symptoms ‐ women‐only studies.
Studies excluding Vietnam war veterans Nine studies met this criterion, with a total of 599 individuals (Analysis 3.22).The individual TFCBT group did better than the 'other therapies' group (SMD ‐0.46; 95% CI ‐0.80 to ‐0.11), demonstrating minimal difference from the overall analyses. Excluding this one trial made little difference to the observed statistically significant heterogeneity or to the effect estimate.
3.22. Analysis.

Comparison 3 Trauma‐focused CBT/Exposure Therapy vs other therapies, Outcome 22 Subgroup analysis: severity of PTSD symptoms ‐ clinician ‐ excluding Vietnam veterans.
20.3 Publication bias
All the studies identified for this review were published, and many of the trials were undertaken relatively recently. We explored the potential effects of publication bias using funnel plots. We constructed two funnel plots using data from the individual TFCBT versus waitlist/usual care comparison (comparison 1), one involving continuous data in the primary outcome, and the second involving dichotomous data in a secondary outcome. We also looked at the TFCBT versus 'other therapies' comparison (3.1).
The first funnel plot examined the measure of clinician‐rated PTSD symptoms (see Figure 4) and was roughly symmetrical with the exception of one outlier and an absence of smaller studies demonstrating no difference or a difference in favour of waitlist/usual care. This suggests the possibility of publication bias. As the studies become less precise the results of the studies tended be more variable and scattered to either side of the more precise larger studies. The same was found for the comparison of TFCBT with other therapies (see Figure 5).
4.
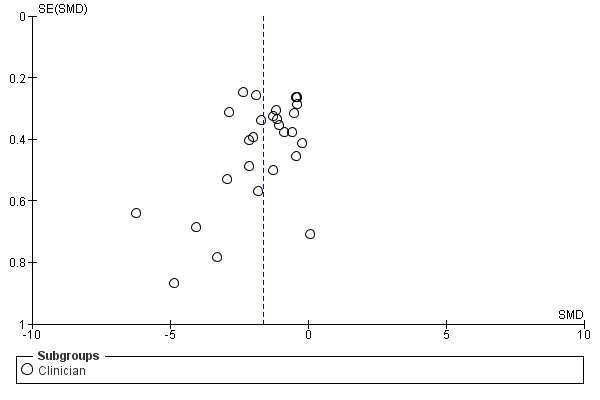
Funnel plot of comparison: 1 Individual trauma‐focused CBT/Exposure therapy vs waitlist/usual care, outcome: 3.1 Severity of PTSD symptoms ‐ clinician‐rated.
5.

Funnel plot of comparison: 3 Trauma‐focused CBT/Exposure Therapy vs other therapies, outcome: 3.1 Severity of PTSD symptoms ‐ clinician‐rated.
The second funnel plot using data from the individual TFCBT versus waitlist/usual care comparison examined the dichotomous measure of PTSD diagnosis after treatment (see Figure 6). This funnel plot shows that larger studies demonstrated smaller differences between individual TFCBT and waitlist/usual care, and also suggests an absence of smaller studies demonstrating no difference or a difference in favour of waitlist/usual care. This funnel plot therefore shows some evidence of publication bias. It is possible that, due to the greater likelihood of publication of positive studies, the true difference between groups is smaller than is suggested by this review.
6.

Funnel plot of comparison: 1 Individual trauma‐focused CBT/Exposure therapy vs waitlist/usual care, outcome: 1.7 PTSD diagnosis after treatment.
Discussion
Summary of main results
We include 70 studies of 4761 participants in this review. We have created a 'Summary of findings' table for each of the 13 comparisons we were able to conduct. We assessed the quality of the evidence for each comparison as very low. Statistically, individual trauma‐focused cognitive behavioural therapy (TFCBT) and eye movement desensitisation and reprocessing (EMDR) did better than waitlist/usual care in reducing clinician‐assessed post‐traumatic stress disorder (PTSD) symptoms. Non‐TFCBT did significantly better than waitlist/usual care and other therapies. Other therapies did significantly better than waitlist/usual care control, as did group‐TFCBT. There was no difference between group non‐TFCBT and waitlist/usual care. There was no statistically significant difference between individual TFCBT, EMDR and non‐TFCBT immediately post‐treatment although there was some evidence that individual TFCBT and EMDR are superior to non‐TFCBT at between one and four months following treatment, and that individual TFCBT, EMDR and non‐TFCBT were more effective than other therapies. There was some evidence of greater drop‐out in active treatment groups. The considerable unexplained heterogeneity observed in these comparisons, and the potential impact of publication bias on these data, suggest the need for caution in interpreting the results of this review.
Trauma‐focused cognitive behavioural therapy
There was very low quality evidence that individual TFCBT was better than waitlist/usual care in reducing traumatic stress symptoms and associated symptoms of depression and anxiety. The overall standardised mean difference for traumatic stress symptoms post‐treatment represents an effect size generally accepted as indicating a strong positive effect. After exploration of heterogeneity this finding remains robust although there is statistically significant heterogeneity present in all analyses. There is not enough evidence to confirm whether this advantage is maintained over time. There is evidence that individual TFCBT is a more effective treatment than non‐trauma‐focused therapies classed as 'other therapies'. There is also evidence that individual TFCBT is superior to non‐TFCBT, although this is not apparent immediately after treatment.
Eye movement desensitisation and reprocessing
There was very low quality evidence that EMDR was better than waitlist/usual care in reducing traumatic stress symptoms and additionally associated symptoms of depression and anxiety. The overall standardised mean differences for clinician‐rated and self‐rated traumatic stress symptoms post‐treatment represents a strong positive effect size. There is not enough evidence to determine whether these improvements are maintained in the long‐term as there were no follow‐up comparisons of EMDR and waitlist groups. There were limited data to suggest a better outcome than non‐TFCBT at between one‐ and four‐month follow‐up. EMDR appeared to have similar effectiveness to individual TFCBT in the studies that compared them directly. There was some evidence that EMDR was a more effective treatment than other therapies.
Non‐trauma‐focused cognitive behavioural therapy
There was very low quality evidence that non‐TFCBT was better than waitlist/usual care in reducing traumatic stress symptoms and additionally associated symptoms of depression and anxiety. It is worth noting that the meta‐analyses of non‐TFCBT included fewer participants than TFCBT and EMDR, and demonstrated high heterogeneity, indicating that these results should be interpreted with caution. There was some evidence that non‐TFCBT is a more effective treatment than other non‐trauma‐focused therapies, but this was from the results of one study only. Non‐TFCBT was less effective than TFCBT at follow‐up. Whilst this might indicate insufficient statistical power, it may also indicate that non‐TFCBT provides only temporary relief of symptoms, or that TFCBT provides a basis for continued improvement.
Other therapies
There was very low quality evidence that other therapies were better than waitlist/usual care in reducing traumatic stress symptoms and associated symptoms of depression and anxiety. As stated above, other therapies were statistically significantly worse in terms of the primary outcome measure of reducing traumatic stress symptoms when directly compared with individual TFCBT and non‐TFCBT. There was a statistically significant difference in favour of other therapies in comparison with individual TFCBT in terms of drop‐out. This finding suggests the possibility of non‐trauma‐focused therapies being easier to tolerate than individual TFCBT, although this finding is based on studies of variable quality.
Group TFCBT
There was very low quality evidence that group TFCBT was better than waitlist/usual care in reducing traumatic stress symptoms. There was no difference between group TFCBT and non‐trauma‐focused group CBT.
Group non‐TFCBT
There was no evidence that group non‐TFCBT was any better than waitlist/usual care in reducing traumatic stress symptoms or depression immediately after treatment or at four‐month follow‐up in the one study making this comparison.
Drop‐outs
Individual TFCBT and other therapies both did worse than waitlist/usual care on this outcome measure. There was also some evidence that individual TFCBT incurred a greater drop‐out rate than other therapies.
Adverse effects
Unfortunately no studies reported adverse effects. It is well recognised that these may occur, such as increased re‐experiencing following exposure treatment (e.g. Pitman 1991), and the absence of any reporting of them is of major concern.
Anxiety and depression
Symptoms of anxiety and depression generally improved in line with improvements in traumatic stress symptoms. This is no surprise for treatments such as cognitive restructuring where many of the approaches used for PTSD would also be used for anxiety and depression. However other treatments such as exposure therapy do not address depressive symptoms per se yet still appeared to reduce depressive and anxiety symptoms. This suggests that the anxiety and depressive symptoms found in many PTSD sufferers in these studies were secondary to the PTSD rather than being discrete conditions requiring specific treatment.
Heterogeneity
The forest plots of the pooled results demonstrated statistically significant heterogeneity between the studies. For example, heterogeneity levels of P < 0.00001 were observed in several analyses of the primary outcome measure. There are likely to be several factors that contribute to this heterogeneity. There is clearly considerable clinical diversity within the studies considered. We attempted to explore this by performing subgroup analyses on the primary outcome measure of individual TFCBT versus waitlist/usual care. Those studies including only women, all of whom had been sexually or non‐sexually assaulted, produced more positive results than the overall results. Possible explanations include the treatments having been superior, women being more responsive to individual TFCBT than men, traumatisation by assault being more responsive to individual TFCBT, a combination of these and/or other factors. Those studies that did not include only Vietnam war veterans produced a slightly more positive result than all studies. However there was only one study excluded from this subgroup analysis, which may therefore lack power to show a real difference; great caution must be exercised in interpreting this finding.
Overall completeness and applicability of evidence
This review considers randomised controlled trials (RCTs) of a wide range of psychological therapies for chronic PTSD, including individual TFCBT, EMDR, non‐TFCBT, group TFCBT, group non‐TFCBT, and other psychological therapies (see Types of interventions). Studies included participants from different countries and backgrounds, who had been exposed to a variety of different traumatic events (see Types of participants). The majority of studies reported on the use of qualified and experienced therapists, and a high proportion included assessment of adherence to a treatment protocol (see Characteristics of included studies). Many factors, however, limit the generalisability of conclusions reached by this review. Most studies to date have been conducted in the USA, Canada, Australia and Europe, limiting generalisability of results to the rest of the world. Although we have included the full range of psychological therapies for PTSD considered by RCTs to date, insufficient data preclude meta‐analysis of a number of outcomes in some treatment groups. There are many more studies of individual TFCBT than other therapies, for example, those taking a person‐centred only or psychodynamic approach, which were considered within a single category. The majority of studies did not include participants with comorbid psychiatric diagnoses and substance dependence, excluding individuals who are arguably more difficult to treat. This may have resulted in the exclusion of individuals with complicated histories and the experience of multiple traumatic events. Generalising the results to more complex presentations of the disorder is therefore problematic. There were very limited long‐term follow‐up data, especially for waitlist groups. This prevents determination of the long‐term efficacy of therapies, but the incremental improvement of the active treatment groups in the trials with longer follow‐ups suggests that benefits are maintained. Comparison on the basis of trauma type, study setting and participant variables would be an interesting addition to future versions of this review.
Most studies reported on drop‐outs by group; drop‐out rates are likely to be influenced by adverse effects along with other factors. The major distinction between the treatments classed as TFCBT and those classed as 'other therapies' was the inclusion of exposure‐based components. Since the treatments that included exposure had a significantly greater drop‐out rate, this raises questions surrounding the tolerability of exposure work. Although it is well documented that exposure‐based treatments can cause short‐term exacerbation of symptoms (e.g. Tarrier 1999), we have little understanding of how this impacts on drop‐out rates. Given that the included studies provide little disclosure of adverse events and few explanations for drop‐outs, it is difficult to ascertain why participants were less able to tolerate exposure‐based treatments. This is an important finding and one that should stimulate the development of interventions that are more acceptable to those who receive them.
Quality of the evidence
Methodological quality varied considerably (see Characteristics of included studies). Risk of bias was high or unclear for multiple domains in a large proportion of older studies, especially those published before 2000. Most studies rated as having a low risk of bias were of individual TFCBT. In a large proportion of studies, the information provided by the published report was insufficient to determine the risk of bias associated with key methodological indicators. There was considerable unexplained heterogeneity for some analyses and the quality of evidence for each of the comparisons was rated as very low.
As with all psychological therapy trials, there are issues with the control groups. The development of a 'psychological therapy placebo' is very difficult, if not impossible, as is blinding of participants and therapists. It is possible that the efficacy of psychological therapies is stronger than suggested by the data, as in several studies the waitlist/usual care group received some contact and the expectation that they would be treated, which may have been therapeutic. It is, however, also possible that waitlist groups do worse than usual care groups because they do not expect to improve until they receive the active therapy.
Potential biases in the review process
The review followed guidelines set out by The Cochrane Collaboration (Higgins 2011). Two authors independently read all the candidate studies, assessed them for inclusion, and rated them for risk of bias. We discussed any disagreements with a third review author with the aim of reaching a consensus. This will have minimised potential bias, but several unavoidable issues remain. For example, all studies included in the review were published, resulting in the possibility of publication bias. We explored and confirmed this using funnel plots (Figures 4, 5 and 6). Several studies reported incomplete data, although we contacted authors to obtain missing results where possible. Although we searched numerous online databases systematically, scrutinised reference lists, contacted experts in the field, and handsearched relevant additional sources, we cannot rule out the possibility of missed RCTs. There was a great deal of heterogeneity between trials of the psychological therapies included within specific categories. This was especially notable within the 'other therapies' group. Although all were examples of non‐trauma‐focused psychological therapies that were not based on the principles of CBT, interventions included psychodynamic therapy, hypnotherapy, supportive counselling and present‐centred counselling, which differ in terms of proposed active ingredients and the way in which they are delivered. There was also considerable statistical heterogeneity evident in many of the comparisons. In circumstances where heterogeneity was thought to be an issue, we used a random‐effects model, and reported this. In addition, therapies within the 'other therapies' category were not always delivered with the intention of being as effective as the other treatment under study, but to act as a control (e.g.Bryant 2003; Bryant 2011; Feske 2008). It is clear that TFCBT performed very well versus waitlist/usual care comparison, but it must also be considered that this comparison included by far the most studies. It is fair to say that other categories (e.g. other therapies) may have performed better had they been represented by a larger number of studies. Finally, it is worth noting that there were differences in terms of acceptance into treatment protocols (for example, the requirement of diagnosis through structured interview versus self‐reported measures), which is likely to have resulted in some studies that were overly inclusive and others that exercised more conservative guidelines.
Agreements and disagreements with other studies or reviews
This review supports the efficacy of psychological therapy for chronic PTSD, which is consistent with the results of many other reviews (e.g. Bisson 2007b; Bradley 2005; Van Etten 1988). It is also consistent with current practice guidelines which recommend individual TFCBT and EMDR as frontline treatments for the disorder (ACPMH 2007; NICE 2005).
Authors' conclusions
Implications for practice.
Psychological therapies are more effective than waitlist or usual care in treating adults with chronic PTSD.
Trauma‐focused cognitive behavioural therapy and eye movement desensitisation and reprocessing have the best evidence for efficacy at present.
There is evidence that non‐TFCBT is effective in the short term.
There is more limited evidence that some other non‐trauma‐focused psychological therapies may be effective.
Drop‐out from treatment is an issue with currently available psychological therapies. Issues of engagement are an important consideration.
Although a substantial number of studies were included in the review, the conclusions are compromised by methodological issues evident in some. Sample sizes were small, and it is apparent that many of the studies were underpowered. There were limited follow‐up data, which compromise conclusions regarding the long‐term effects of psychological treatment. We assessed the evidence for each of the comparisons made in this review as of very low quality.
Implications for research.
Further well‐designed trials of psychological therapies are required, incorporating appropriate methods of randomisation, blinding of assessors, long‐term follow up and appropriate training of therapists and monitoring of treatment adherence.
There is a requirement for further comparison studies of one type of psychological therapy against another.
Future trials should consider adverse events and tolerability of treatment in more detail.
The role of psychological therapy in combination and as an alternative to medication is unclear. Further research in this area would be useful.
What's new
| Date | Event | Description |
|---|---|---|
| 26 August 2015 | Amended | Corrected typographical error in results section. |
History
Protocol first published: Issue 4, 2001 Review first published: Issue 2, 2005
| Date | Event | Description |
|---|---|---|
| 13 December 2013 | New citation required but conclusions have not changed | Major update |
| 13 December 2013 | New search has been performed | Updated to include studies completed by 12th April 2013. |
| 5 November 2008 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
We should like to thank the Cochrane Depression, Anxiety and Neurosis Group (CCDAN) editorial base for their help with searches, helpful comments on the protocol and assistance with the methodology. We should also like to thank the NICE PTSD guideline development group for allowing us access to their data sets. We also thank the following:
Arnoud Arntz (Scientific Director of the Research Institute of Experimental Psychopathology, Maastricht University) Merel Kindt (Head of the Department of Clinical Psychology at the University of Amsterdam) Richard Bryant (Professor at the University of New South Wales) Willi Butollo (Professor at Ludwig‐Maximilian University of Munich) Claude Chemtob (Research Professor in the Departments of Psychiatry and Child and Adolescent Psychiatry at the NYU School of Medicine) Judith Cohen (Medical Director of the Center for Traumatic Stress in Children & Adolescents at Allegheny General Hospital in Pittsburgh) Mark Creamer (Director of the Australian Centre for Posttraumatic Mental Health (ACPMH)) Jonathan Davidson (Director of the Anxiety and Traumatic Stress Program at Duke University Medical Centre, North Carolina) Enrique Echeburua (Professor of Clinical Psychology at the University of the Basque Country (Spain)) Paul Emmelkamp (Academy Professor, Royal Academy of Arts and Sciences (KNAW), University of Amsterdam) Edna Foa (Director of the Centre for the Treatment and Study of Anxiety) Chris Freeman (Consultant Psychiatrist, Royal Edinburgh Hospital) Matt Friedman (Executive Director of the National Centre for PTSD) Berthold Gersons (Distinguished AMC‐Professor and Professor of Psychiatry at the Academical Medical Center of the University of Amsterdam) Louise Humprheys Terry Keane (Director of the Behavioral Science Division of the National Center for PTSD, USA) Dean Kilpatrick (Professor and Director, National Crime Victims Center, Medical University of South Carolina) Edward Kubany (University of Hawaii) Brett Litz (Professor in the Departments of Psychiatry and Psychology at Boston University) Andreas Maercker (Head of Division, Department of Psychology Psychopathology and Clinical Intervention, University of Zurich) Charles Marmar (Chair of the Department of Psychiatry, New York University Langone Medical Center) Sandy McFarlane (Director of the Centre for Traumatic Stress Studies, the University of Adelaide) Thomas Mellman (Director, Clinical and Translational Research and Stress and Sleep Studies Programs, Howard University College of Medicine) Lars‐Goran Öst (Professor of Clinical Psychology, Department of Psychology, Stockholm University, Sweden) Michael Otto (Director, Translational Research Program at the Center for Anxiety and Related Disorders, Boston University) Roger Pitman (Professor of Psychiatry at Harvard Medical School) Mark Pollack (Director of the Center for Anxiety and Traumatic Stress Disorders, Massachusetts General Hospital) Patti Resick (Director of the Women’s Health Sciences Division of the National Center for PTSD at the Veterans Affairs (VA) Boston Healthcare System) David Riggs (Executive Director of the Center for Deployment Psychology (CDP)) Sue Rose Barbara Rothbaum (Associate Vice Chair of Clinical Research Department of Psychiatry, Emory School of Medicine) Joe Ruzek (Director of the Dissemination and Training Division of the National Center for Post‐Traumatic Stress Disorder) Paula Schnurr (Deputy Executive Director of the VA National Center for PTSD) Arieh Shalev (Professor of Psychiatry in the Department of Psychiatry at Hadassah University Hospital in Jerusalem) Dan Stein (Chair of the Department of Psychiatry and Mental Health at the University of Cape Town) Nick Tarrier (Professor of Clinical Psychology in the Faculty of Medical and Human Sciences at the University of Manchester) Agnes van Minnen (Professor at Behavioural Science Institute, Radboud University Nijmegen) Simon Wessely (Chair and Head of the Department of Psychological Medicine at the Institute of Psychiatry, King's College London) Patricia White Rachel Yehuda (Director of the Traumatic Stress Studies Division at Icahn School of Medicine, and the Mental Health Patient Care Center Director at the James J. Peters Veterans Affairs Medical Center)
CRG Funding Acknowledgement: The National Institute for Health Research (NIHR) is the largest single funder of the Cochrane Depression, Anxiety and Neurosis Group.
Disclaimer: The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the NIHR, NHS or the Department of Health.
Data and analyses
Comparison 1. Trauma‐focused CBT/Exposure therapy vs waitlist/usual care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Severity of PTSD symptoms ‐ clinician | 32 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Clinician PTSD | 28 | 1256 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.62 [‐2.03, ‐1.21] |
| 1.2 Clinician PTSD severity women‐only subgroup analysis) | 9 | 562 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.83 [‐2.31, ‐1.36] |
| 1.3 Clinician PTSD excluding studies of Vietnam War veterans | 27 | 1232 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.67 [‐2.09, ‐1.25] |
| 1.4 Self report | 16 | 666 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.57 [‐2.01, ‐1.14] |
| 2 Severity of PTSD symptoms at 1 ‐ 4 month follow‐up | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Clinician | 4 | 336 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.18 [‐2.20, ‐0.17] |
| 3 Severity of PTSD symptoms at 5 ‐ 8 month follow‐up. | 3 | 192 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.47 [‐0.77, ‐0.18] |
| 4 Severity of PTSD symptoms 9 ‐ 12 month follow‐up | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5 Leaving the study early for any reason | 33 | 1756 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.64 [1.30, 2.06] |
| 6 Severity of PTSD symptoms ‐ self report: 1 ‐ 4 month follow‐up | 2 | 181 | Std. Mean Difference (IV, Random, 95% CI) | ‐3.03 [‐6.51, 0.45] |
| 7 Severity of PTSD symptoms ‐ self report: 5 ‐ 8 months) | 2 | 208 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.61 [‐0.90, ‐0.32] |
| 8 Severity of PTSD symptoms ‐ self report: 9 ‐ 12 month follow up | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 9 Depression | 28 | 1213 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.28 [‐1.62, ‐0.94] |
| 10 Depression 1 ‐ 4 month follow‐up | 7 | 413 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.75 [‐1.33, ‐0.18] |
| 11 Depression 5 ‐ 8 month follow‐up | 2 | 150 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.50 [‐0.82, ‐0.17] |
| 12 Depression 9 ‐ 12 month follow‐up | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 13 Anxiety | 17 | 644 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.81 [‐1.03, ‐0.59] |
| 14 Anxiety 1 ‐ 4 month follow‐up | 3 | 189 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.32 [‐0.60, ‐0.03] |
| 15 Anxiety 9 ‐ 12 month follow‐up | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 16 Exploration of publication bias | 28 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 16.1 Clinician | 28 | 1256 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.62 [‐2.03, ‐1.21] |
| 17 Sensitivity analysis ‐ clinician‐rated PTSD symptoms ‐ studies at low risk of bias only | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 18 PTSD diagnosis after treatment | 19 | 910 | Risk Ratio (M‐H, Random, 95% CI) | 0.51 [0.41, 0.64] |
1.16. Analysis.

Comparison 1 Trauma‐focused CBT/Exposure therapy vs waitlist/usual care, Outcome 16 Exploration of publication bias.
Comparison 2. Trauma‐focused CBT/Exposure therapy vs non‐TFCBT.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Severity of PTSD Symptoms ‐ clinician | 7 | 267 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.27 [‐0.63, 0.10] |
| 2 Severity of PTSD symptoms ‐ clinician ‐ follow‐up (1 ‐ 4 months) | 5 | 127 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.51 [‐1.00, ‐0.01] |
| 3 Severity of PTSD symptoms ‐ clinician ‐ follow‐up (5 ‐ 8 months) | 2 | 48 | Std. Mean Difference (IV, Random, 95% CI) | 1.00 [‐2.17, 0.17] |
| 4 Severity of PTSD symptoms ‐ clinician ‐ follow‐up (9 ‐ 12 months) | 2 | 48 | Mean Difference (IV, Fixed, 95% CI) | ‐12.93 [‐18.72, ‐7.14] |
| 5 Leaving the study early for any reason | 7 | 312 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.19 [0.71, 2.00] |
| 6 Severity of PTSD symptoms ‐ self report | 3 | 127 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.37 [‐0.74, 0.01] |
| 7 Severity of PTSD symptoms ‐ self report ‐ follow‐up (1‐4 months) | 2 | 54 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.44 [‐0.99, 0.10] |
| 8 Depression | 6 | 189 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.27 [‐0.56, 0.03] |
| 9 Depression ‐ follow‐up (1 ‐ 4 months) | 5 | 147 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.28 [‐0.62, 0.06] |
| 10 Depression ‐ follow‐up (5 ‐ 8 months) | 2 | 48 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.71 [‐1.30, ‐0.12] |
| 11 Depression ‐ follow‐up (9 ‐ 12 months) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 12 Anxiety | 4 | 127 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.12 [‐0.49, 0.26] |
| 13 Anxiety ‐ follow‐up (1 ‐ 4 months) | 4 | 117 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.24 [‐0.79, 0.30] |
| 14 Anxiety ‐ follow‐up (5 ‐ 8 months) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 15 Anxiety ‐ follow‐up (9 ‐ 12 months) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 16 PTSD diagnosis after treatment | 6 | 284 | Risk Ratio (M‐H, Random, 95% CI) | 0.83 [0.60, 1.17] |
Comparison 3. Trauma‐focused CBT/Exposure Therapy vs other therapies.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Severity of PTSD symptoms ‐ clinician | 10 | 625 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.48 [‐0.83, ‐0.14] |
| 2 Severity of PTSD symptoms ‐ clinician ‐ 1 ‐ 4 month follow‐up | 8 | 548 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐0.64, ‐0.04] |
| 3 Severity of PTSD symptoms ‐ clinician ‐ 5 ‐ 8 month follow‐up | 4 | 434 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.58 [‐1.20, 0.04] |
| 4 Severity of PTSD symptoms ‐ clinician ‐ 9 ‐ 12 month follow‐up | 2 | 90 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.76 [‐1.35, ‐0.17] |
| 5 Leaving the study early for any reason | 11 | 762 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.39 [1.01, 1.92] |
| 6 Severity of PTSD symptoms ‐ self report | 6 | 574 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.60 [‐1.15, ‐0.06] |
| 7 Severity of PTSD symptoms ‐ self report ‐ follow‐up (1 ‐ 4 months) | 5 | 526 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.29 [‐0.47, ‐0.12] |
| 8 Severity of PTSD symptoms ‐ self‐report ‐ follow‐up (5 ‐ 8 months) | 3 | 338 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.90 [‐2.05, 0.25] |
| 9 Severity of PTSD symptoms ‐ self‐report ‐ follow‐up (9 ‐ 12 months) | 2 | 90 | Mean Difference (IV, Fixed, 95% CI) | ‐2.66 [‐5.71, 0.38] |
| 10 Depression ‐ self report | 9 | 570 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐0.63, ‐0.11] |
| 11 Depression ‐ self‐report ‐ follow‐up (1‐4 months) | 7 | 510 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.29 [‐0.62, 0.03] |
| 12 Depression ‐ follow‐up (5‐8 months) | 5 | 443 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.43 [‐0.87, 0.01] |
| 13 Depression 9‐12 month follow up | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 14 Anxiety ‐ self report | 7 | 539 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.45 [‐0.77, ‐0.12] |
| 15 Anxiety ‐ self‐report ‐ follow‐up (1 ‐ 4 months) | 5 | 454 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.33 [‐0.68, 0.02] |
| 16 Anxiety ‐ follow‐up (5 ‐ 8 months) | 2 | 329 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.56 [‐1.69, 0.58] |
| 17 PTSD diagnosis after treatment | 7 | 358 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.59, 0.96] |
| 18 Severity of PTSD symptoms ‐ clinician ‐ 13‐24 month follow‐up | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 19 Sensitivity analysis ‐ PTSD symptoms ‐ studies at low risk of bias only | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 20 Sensitivity analysis ‐ drop‐out ‐ studies at low risk of bias only | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 21 Subgroup analysis: severity of PTSD symptoms ‐ women‐only studies | 3 | 129 | Std. Mean Difference (IV, Random, 95% CI) | 0.03 [‐0.42, 0.47] |
| 22 Subgroup analysis: severity of PTSD symptoms ‐ clinician ‐ excluding Vietnam veterans | 9 | 599 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.46 [‐0.80, ‐0.11] |
3.13. Analysis.

Comparison 3 Trauma‐focused CBT/Exposure Therapy vs other therapies, Outcome 13 Depression 9‐12 month follow up.
3.18. Analysis.
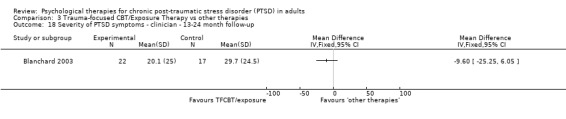
Comparison 3 Trauma‐focused CBT/Exposure Therapy vs other therapies, Outcome 18 Severity of PTSD symptoms ‐ clinician ‐ 13‐24 month follow‐up.
Comparison 4. EMDR vs waitlist/usual care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Severity of PTSD symptoms ‐ Clinician | 6 | 183 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.17 [‐2.04, ‐0.30] |
| 2 Leaving study early due to any reason | 7 | 227 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.62, 1.79] |
| 3 Severity of PTSD symptoms ‐ self report | 6 | 159 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.80 [‐1.68, 0.07] |
| 4 Depression | 7 | 226 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.15 [‐1.52, ‐0.78] |
| 5 Anxiety | 6 | 160 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐1.02 [‐1.36, ‐0.69] |
| 6 PTSD diagnosis after treatment | 6 | 209 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.51 [0.42, 0.62] |
Comparison 5. EMDR vs Trauma‐focused CBT.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Severity of PTSD symptoms ‐ clinician | 7 | 327 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.43, 0.38] |
| 2 Severity of PTSD symptoms ‐ clinician ‐ follow‐up (1 ‐ 4 months) | 3 | 76 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.19 [‐0.97, 0.58] |
| 3 Leaving study early for any reason | 8 | 408 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.74, 1.35] |
| 4 Severity of PTSD symptoms ‐ self report | 7 | 306 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.60, 0.01] |
| 5 Severity of PTSD symptoms ‐ self‐report ‐ follow‐up (1 ‐ 4 months) | 5 | 111 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.61, 0.52] |
| 6 Depression | 8 | 346 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.31 [‐0.75, 0.13] |
| 7 Depression ‐ follow‐up (1 ‐ 4 months) | 5 | 111 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.64, 0.38] |
| 8 Anxiety | 4 | 236 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.28 [‐0.53, ‐0.02] |
| 9 Anxiety ‐ follow‐up (1 ‐ 4 months) | 2 | 48 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.24 [‐0.33, 0.81] |
| 10 PTSD diagnosis after treatment | 8 | 350 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.74, 1.22] |
Comparison 6. EMDR vs non‐TFCBT.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Severity of PTSD symptoms ‐ clinician | 2 | 53 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.35 [‐0.90, 0.19] |
| 2 Severity of PTSD symptoms ‐ clinician ‐ follow‐up (1‐4 months) | 3 | 71 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.74 [‐1.64, 0.15] |
| 3 Leaving the study early for any reason | 3 | 84 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.37, 2.88] |
| 4 Severity of PTSD symptoms ‐ self report | 3 | 75 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.40 [‐0.86, 0.06] |
| 5 Severity of PTSD symptoms ‐ self‐report ‐ follow‐up (1 ‐ 4 months) | 3 | 75 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.52 [‐0.98, ‐0.05] |
| 6 Depression | 3 | 75 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.67 [‐1.14, ‐0.20] |
| 7 Depression ‐ follow‐up (1 ‐ 4 months) | 3 | 75 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.86, 0.36] |
| 8 Anxiety | 2 | 45 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.75 [‐1.36, ‐0.13] |
| 9 Anxiety ‐ follow‐up (1 ‐ 4 months) | 2 | 45 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.42 [‐2.21, 1.37] |
| 10 PTSD diagnosis after treatment | 3 | 84 | Risk Ratio (M‐H, Random, 95% CI) | 0.71 [0.41, 1.22] |
Comparison 7. EMDR vs other therapies.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Leaving study early for any reason | 2 | 127 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.48 [0.26, 8.54] |
| 2 Severity of PTSD symptoms ‐ self report | 2 | 124 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.84 [‐1.21, ‐0.47] |
| 3 Depression | 2 | 127 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.67 [‐1.03, ‐0.32] |
| 4 Anxiety | 2 | 126 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.72 [‐1.08, ‐0.36] |
| 5 PTSD diagnosis after treatment | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Comparison 8. Non‐TFCBT vs waitlist/usual care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Severity of PTSD symptoms ‐ Clinician | 4 | 106 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.22 [‐1.76, ‐0.69] |
| 2 Leaving the study early for any reason | 5 | 141 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.96 [0.70, 5.48] |
| 3 Severity of PTSD symptoms ‐ Self‐report | 2 | 44 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.86 [‐3.27, 1.55] |
| 4 Depression | 5 | 129 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.93 [‐1.43, ‐0.42] |
| 5 Anxiety | 4 | 102 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.83 [‐1.24, ‐0.42] |
| 6 PTSD diagnosis after treatment | 4 | 121 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.50, 0.86] |
Comparison 9. Non‐TFCBT vs other therapies.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Severity of PTSD symptoms ‐ Clincian | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Severity of PTSD symptoms ‐ clinician ‐ follow‐up (3 months) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Leaving the study early for any reason | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Depression ‐ self report | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5 Depression ‐ self report ‐ follow‐up (3 months) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6 Anxiety ‐ self report | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7 Anxiety ‐ self report ‐ follow‐up (3 months) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8 PTSD diagnosis after treatment | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Comparison 10. Group TFCBT vs waitlist/usual care/minimal contact.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Clinician‐rated | 3 | 185 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.28 [‐2.25, ‐0.31] |
| 2 Severity of PTSD 5 ‐ 8 month follow‐up | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Leaving the study early for any reason | 7 | 573 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.21 [0.94, 1.55] |
| 4 Severity of PTSD symptoms ‐ self report | 6 | 274 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.20 [‐1.70, ‐0.69] |
| 5 Severity of PTSD ‐ self report ‐ 1 ‐ 4 months | 2 | 73 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.14 [‐1.78, ‐0.50] |
| 6 Depression | 3 | 137 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.15 [‐1.98, ‐0.32] |
| 7 Depression 1 ‐ 4 month follow‐up | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8 Anxiety | 3 | 106 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.66 [‐1.06, ‐0.27] |
| 9 Anxiety 1 ‐ 4 month follow‐up | 2 | 73 | Mean Difference (IV, Fixed, 95% CI) | ‐0.43 [‐0.72, ‐0.14] |
| 10 PTSD diagnosis after treatment | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Comparison 11. Group CBT (trauma‐focused) vs Group CBT (non‐trauma‐focused).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Severity of PTSD symptoms | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Leaving the study early for any reason | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 PTSD diagnosis after treatment | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Comparison 12. Other therapies vs waitlist/usual care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Severity of PTSD symptoms ‐ clinician | 3 | 112 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.58 [‐0.96, ‐0.20] |
| 2 Leaving the study early due to any reason | 4 | 211 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.45 [0.99, 6.10] |
| 3 Severity of PTSD symptoms ‐ self report | 2 | 132 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.61 [‐0.98, ‐0.24] |
| 4 Depression | 3 | 112 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.45 [‐0.83, ‐0.07] |
| 5 Anxiety ‐ Self report | 4 | 193 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.52 [‐0.82, ‐0.22] |
| 6 PTSD diagnosis after treatment | 4 | 210 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.61, 1.05] |
Comparison 13. Group non‐TFCBT vs waitlist/usual care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Leaving the study early for any reason | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Severity of PTSD symptoms ‐ self report | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Severity of PTSD symptoms ‐ self report 1 ‐ 4 months | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4 Depression | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5 Depression ‐ 1 ‐ 4 months | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Adenauer 2011.
| Methods | Randomised controlled trial | |
| Participants | 34 refugees (in Germany) with a history of violence and persecution, suffering PTSD (15 women, 19 men) | |
| Interventions | 12 sessions of Narrative Exposure Therapy (NET) (n = 16) vs waitlist control (n = 18) in parallel | |
| Outcomes | CAPS, HDRS, ssVEF | |
| Notes | Experienced therapists delivered therapy. Treatment adherence was not assessed, but monitored in supervision sessions. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Participants that fulfilled the inclusion criteria were randomized into the two groups using a computer‐generated list of random numbers". |
| Allocation concealment (selection bias) | Unclear risk | Comment: Allocation concealment was not reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: " As this study focuses on brain changes through psychotherapy rather than examining the clinical efficacy of the treatment, we restricted all analyses to the sample of study completers". Drop‐out rates were one participant from treatment and two from waitlist, all due to deportation. Data for a further 4 participants were excluded from the treatment group, and another 8 from waitlist, due to no/poor‐quality MEG data. |
| Selective reporting (reporting bias) | High risk | www.clinicaltrials.gov‐/ct2/show/NCT00563888 specified the CAPS as primary outcome and ssVEFs as secondary. The paper is written in terms of ssVEF as primary outcome. The paper trials register also specifies a 4‐ and 9‐month follow‐up. |
| Other bias | High risk | There was a mean difference of 16 points in pretreatment CAPS scores between the two groups (NET being greater). |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Two independent female masters‐level psychologists, who were unaware of the patients’ treatment group, performed all assessments at pretreatment, posttreatment, and 3‐ and 6‐month follow‐up. The 12‐month follow‐up assessment was conducted via mail. Blindness was maintained by ensuring that the assessors had no access to group allocation and never talked with patients about which group they were in." |
Asukai 2010.
| Methods | Randomised controlled trial | |
| Participants | 24 individuals (Japanese) with DSM‐IV PTSD after various traumas (21 women, 3 men) | |
| Interventions | 8 ‐ 15 90‐minute sessions of Prolonged Exposre (TFCBT) (n = 12) sessions vs treatment as usual (TAU) (n = 12) | |
| Outcomes | CAPS, IES‐R, CES‐D, GHQ‐28 | |
| Notes | Therapists were masters level psychologists. TAU included pharmacotherapy. Baseline demographics were similar within both groups. The difference in scores between both groups was nonsignificant at baseline on any of the assessment scales. Treatment adherence was measured. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "randomized by the study site based on computer‐generated random digit numbers by permuted blocks between 4 and 8." |
| Allocation concealment (selection bias) | Unclear risk | Comment: Allocation concealment was not reported. Participants were randomised at the study site. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "intention‐to‐treat analysis was performed to determine the relative effect between the two treatment groups for each periodic posttreatment assessment, and those between pre‐PE (after the waiting period) and post‐PE treatment in the control group (CAPS total score, IES‐R, CES‐D, and GHQ‐28)." Comment: 3 dropped out from TFCBT, and one from TAU. A reason was only reported for one of these drop‐outs. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified and expected outcomes appear to have been reported. |
| Other bias | Low risk | Comment: There were no other obvious sources of bias. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Two independent female masters‐level psychologists, who were unaware of the patients’ treatment group, performed all assessments at pretreatment, posttreatment, and 3‐ and 6‐month follow‐up. The 12‐month follow‐up assessment was conducted via mail. Blindness was maintained by ensuring that the assessors had no access to group allocation and never talked with patients about which group they were in." |
Basoglu 2005.
| Methods | Randomised controlled trial | |
| Participants | 59 earthquake survivors in Turkey with DSM‐IV PTSD (50 women, 9 men) | |
| Interventions | Single session of CBT (n = 31) vs waitlist control (n = 28) | |
| Outcomes | CAPS, TSSC, FAQ, BDI, WSA | |
| Notes | Treatment delivered by psychologists trained in the approach. Treatment adherence was measured. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Random allocation was conducted according to a computer‐generated randomization list. Blocking was used to ensure approximately equal cell sizes." |
| Allocation concealment (selection bias) | Low risk | Quote: "The participants were recruited into the study by four independent assessors, who did not have access to the random assignment schedule. The latter was implemented by the project coordinator, who did not take part in the assessments at any stage during the trial." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "As a result of case attrition after week 6, two types of end‐point imputation analyses were carried out. First, the treatment effects were examined at each follow‐up, carrying forward the scores of the non‐improved non‐completers at their last available assessment to subsequent follow‐up points. As this procedure did not involve the improved non‐completers and assumed that the non‐improved non‐completers would have remained non‐improved had they stayed in the study, it led to a conservative analysis of the treatment effects." Comment: participants who did not have at least one follow‐up after treatment were replaced. Eight individuals dropped out of treatment group and 2 from waitlist. No reasons were given. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified and expected outcomes appear to have been reported. |
| Other bias | Low risk | Comment: Baseline demographics are poorly reported. Groups were reported to be similar in every baseline variable but gender (only 1 man in WL group vs 8 in the treatment group). |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote "The assessments were conducted by four independent assessors (three psychologists and one psychiatrist), who were blind as to the participants’ experimental condition. A Blindness Integrity Assessment Form was used to elicit information about whether assessor blindness was maintained at the second assessment and the assessor’s guess as to the study participant’s experimental condition." |
Basoglu 2007.
| Methods | Randomised controlled trial | |
| Participants | 31 earthquake survivors in Turkey with DSM‐IV PTSD (27 women, 4 men) | |
| Interventions | Single session of CBT (n = 16) vs repeated assessments (n = 15) | |
| Outcomes | CAPS, FAQ, BDI, WSA, GIS‐S, GIS‐A | |
| Notes | Treatment was delivered by therapists who were experienced in delivering the intervention on the basis of having done so as part of earlier trials. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote "A computer‐generated sequence of random numbers that ensured equal cell sizes and did not lead to allocation of more than two consecutive cases to the same experimental condition was used in the randomization." |
| Allocation concealment (selection bias) | Low risk | Quote "Participants were enrolled by two independent assessors (psychologists) and randomizations was conducted by the second author, who did not participate in baseline assessments." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: Participants who did not have at least one follow‐up after treatment were replaced. ITT analyses were performed after this point. One person dropped out of treatment group. No one dropped out from waitlist group. No reasons were given. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified and expected outcomes appear to have been reported. |
| Other bias | High risk | Comment: Treatment adherence was not assessed, since the treatment was said to closely reflect the way treatment was delivered in routine fieldwork. Poor reporting of baseline characteristics. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote: "The assessors were blind as to the participants’ experimental condition at the week 4 and week 8 assessments." Test of blinding included. However, 6 cases were followed up by therapists due to an unexpected shortage of funding. |
Beck 2009.
| Methods | Randomised controlled trial | |
| Participants | 44 motor vehicle accident survivors (in the USA) with DSM‐IV PTSD (36 women, 8 men) | |
| Interventions | Group TFCBT (n = 17) vs minimum contact (n = 16) | |
| Outcomes | CAPS, IES‐R, BAI, BDI, ODI, PS‐MPI | |
| Notes | Experienced therapists. Treatment adherence was assessed, as was competence. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote "Groups of four to seven individuals were formed as participants became eligible; a given group then was randomly assigned to either GCBT or MCC conditions." Comment: Method used to generate the allocation sequence is not described in sufficient detail to assess the probability that it would produce comparable groups. |
| Allocation concealment (selection bias) | Unclear risk | Quote "Groups of four to seven individuals were formed as participants became eligible; a given group then was randomly assigned to either GCBT or MCC conditions." Comment: There is no mention of any measures taken to conceal allocation |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: Completers data were analysed. 7 individuals dropped out of the treatment group and 2 from minimum contact. No reasons were given for drop‐out. |
| Selective reporting (reporting bias) | Low risk | All specified outcomes appear to have been reported, although results are discussed in terms of completers. |
| Other bias | Low risk | Comment: There were no other obvious sources of bias. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote "Interviews for the POST and FU assessments were administered by an individual who had not conducted the pre‐treatment assessment and was unaware of patients' treatment status and their time of assessment (POST versus FU)." |
Bichescu 2007.
| Methods | Randomised controlled trial | |
| Participants | 18 former political detainees (in Romania) with PTSD (17 men, 1 woman) | |
| Interventions | Narrative Exposure Therapy (n = 9) vs psychoeducation (n = 9) | |
| Outcomes | CIDI, BDI | |
| Notes | All treatment carried out by a PhD psychology student. Unclear whether adherence was measured, but supervision was provided by email. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "Participants were assigned through a random selection procedure of participants name‐cards to one of two treatment groups: NET and PED." Comment: It is unclear how exactly this was performed. |
| Allocation concealment (selection bias) | Unclear risk | Comment: The authors do not report any methods of allocation concealment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: No drop‐outs. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified and expected outcomes appear to have been reported. |
| Other bias | High risk | Comment: Very small sample size |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Our intent was to perform a blinded assessment by keeping the interviewers unaware of the treatment condition and pre‐test scores of the individual patients and by instructing the patients not to inform the interviewers about their treatment. However, due to the large differences in procedures and number of sessions between the two treatment conditions, it was not possible for us to achieve complete blindness in all cases. Occasionally, a patient revealed details about his treatment that might have affected the blindness of the interviewer." |
Blanchard 2003.
| Methods | Randomised controlled trial | |
| Participants | 98 road traffic accident survivors in the USA (72 women, 26 men) | |
| Interventions | 8 ‐ 12 sessions TFCBT (n = 27) vs 8 ‐ 12 sessions supportive psychotherapy (n = 27) vs waiting list (n = 24) (all three arms included in meta‐analyses) | |
| Outcomes | IES,STAI | |
| Notes | Therapists were practising psychologists, with over 5 years experience. Each had a cognitive behavioural orientation, but treated participants in both active treatment arms. Adherence was assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote "The senior author matched participants into triads, based on the CAPS score and diagnosis,and then randomly assigned triads to a therapist and to conditions within the triad." Comment: Indicates that the method of sequence generation poses the potential for bias. |
| Allocation concealment (selection bias) | Unclear risk | Comment: there were no reported measures of allocation concealment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote "When we could not obtain dropout assessment data, we substituted the initial assessment data in the intent to treat analysis." However, no reasons were reported for drop‐outs (10 from CBT, 9 from supportive psychotherapy, and 1 from waitlist). |
| Selective reporting (reporting bias) | Low risk | Comment: All specified and expected outcomes appear to have been reported. |
| Other bias | Low risk | Comment: no other sources of bias detected. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote "The assessors were kept blind to treatment condition." |
Brom 1989.
| Methods | Randomised controlled trial | |
| Participants | 112 outpatients in the Netherlands. Various traumas, 89 bereaved. (88 women, 24 men) | |
| Interventions | 14 ‐ 18 sessions of trauma desensitisation (n = 31), hypnotherapy (n = 29), psychodynamic therapy (n = 29) or waiting list (n = 23) (data could not be entered into meta‐analysis, included only intrusion and avoidance sub‐scales) | |
| Outcomes | "trauma symptoms" on SCL‐90 | |
| Notes | Therapists with over 10 years experience in the specific method. Therapists conducted the therapies they preferred outside the research setting (i.e. there were different therapists treating each treatment arm). Supervision sessions ensured adherence. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: The method of sequence generation is not reported. It is simply stated that treatment assignment was random. |
| Allocation concealment (selection bias) | Unclear risk | Comment: The method of sequence allocation is not reported, |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: There were no reported reasons for drop‐out. There was inadequate statistical correction for these drop‐outs. 3 individuals dropped out of each of the treatment arms. |
| Selective reporting (reporting bias) | Unclear risk | Quote: "We focus in this article on the data from the standardized questionnaires, disregarding the physiological and behavioral tests that were administered. The domains that were covered by the questionnaires were general symptoms, symptoms of the coping process, and personality." Comment: It is unclear whether it had originally been the intention to report the behavioural tests. |
| Other bias | High risk | Comment: Inadequate reporting of baseline characteristics. Each treatment arm had its own dedicated therapists (i.e. differences in outcome may have been attributable to expertise as opposed to the intervention). |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: There is no mention of blinding outcome assessors. |
Bryant 2003.
| Methods | Randomised controlled trial | |
| Participants | 58 outpatient survivors of non‐sexual assaults or road traffic accidents in Australia (30 women, 28 men) | |
| Interventions | 8 weekly 90‐minute sessions of imaginal exposure (n = 20), imaginal exposure/cognitive restructuring (n = 20) or supportive counselling (n = 18). (imaginal exposure and imaginal exposure/cognitive restructuring were combined for meta‐analysis). | |
| Outcomes | CAPS, IES, STAI, BDI | |
| Notes | Therapists were masters level clinical psychologists. Treatment adherence was assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was conducted by a process of minimization stratified on gender, trauma type, and PTSD total score. Participants were randomly assigned according to a random numbers system and each month Richard A. Bryant amended the allocation to ensure that gender, trauma type, and PTSD severity were balanced across conditions." |
| Allocation concealment (selection bias) | Unclear risk | Comment: It is unclear if/how allocation was concealed. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote "Intent‐to‐treat values were devised by using a last‐value‐carried forward procedure to provide data for missing values that occurred because of dropout." Comment: Reasons for drop‐out are not fully reported. ITT analyses were however reported. Drop‐out by group was as follows: imaginal exposure (5), imaginal exposure/cognitive restructuring (5) or supportive counselling (3). |
| Selective reporting (reporting bias) | Low risk | Comment: All specified and expected outcomes appear to have been reported. |
| Other bias | Low risk | Comment: no other sources of bias detected. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Initial assessments were conducted at pretreatment, posttreatment, and 6‐month follow‐up by independent clinicians who were unaware of the treatment condition of participants. Blindness was maintained by ensuring that clinicians who conducted assessments did not have access to (a) participant notes, (b) treatment allocation of participants, or (c) supervision discussions of therapy sessions." |
Bryant 2011.
| Methods | Randomised controlled trial | |
| Participants | 28 survivors of terrorist attacks in Southern Thailand (27 women, 1 man) | |
| Interventions | 8 weekly 60‐minute sessions of CBT (n = 16) vs TAU (n = 12) | |
| Outcomes | PSS, BDI, ICG | |
| Notes | Therapy was conducted by Thai psychologists or psychiatric nurses who were trained to use the treatment manual in 3 2‐day workshops occurring over 12 months. They had no previous experience of CBT. During the trial itself, therapists conducted treatment without formal supervision. TAU comprised the equivalent number of sessions of supportive counselling being provided by psychiatrists who were not trained in CBT. Adherence was not assessed, but checklists indicated components of treatment completed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were randomised according to a random numbers system administered by health officials in Bangkok (fully independent of counsellors and the study co‐ordinator)." |
| Allocation concealment (selection bias) | Low risk | Quote: "Patients were randomised according to a random numbers system administered by health officials in Bangkok (fully independent of counsellors and the study co‐ordinator)." Comment: Allocation was independent and remote from study site. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "There were no treatment drop‐outs, and so analyses focus on all patients who were randomised into the study." |
| Selective reporting (reporting bias) | Low risk | Comment: All specified and expected outcomes appear to have been reported. |
| Other bias | High risk | Recruitment was terminated prematurely due to health workers being targeted by the terrorists. Small sample size (n = 28) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Assessments conducted at post‐treatment and 3 months following treatment were conducted by independent personnel unaware of patients’ treatment condition." |
Carlson 1998.
| Methods | Randomised controlled trial | |
| Participants | 35 men with combat‐related PTSD in Hawaii | |
| Interventions | 12 bi‐weekly sessions of 60‐75 minutes EMDR (n = 10) vs 40 minutes biofeedback‐assisted relaxation vs routine care (n = 13) vs TAU (n = 12) (all interventions included in meta‐analysis) | |
| Outcomes | Mississippi PTSD scale, IES, STAI, BDI | |
| Notes | Experienced therapists | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: The method of sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Comment: The method of allocation concealment (if any) was not reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: There was 1 drop‐out from the biofeedback‐assisted relaxation. There was no reason given for this drop‐out. These were not properly accounted for in terms of statistical tests. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified and expected outcomes appear to have been reported. The CAPS is emphasised as the primary outcome measure throughout. |
| Other bias | Unclear risk | Comment: There were no other obvious sources of bias. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: Assessors were not blind, although a second CAPS was administered by a blind assessor. |
Chard 2005.
| Methods | Randomised controlled trial | |
| Participants | 71 female child sexual abuse survivors in the USA | |
| Interventions | 17 weekly 90‐minute group sessions of cognitive processing therapy for sexual abuse survivors and a 60‐minute individual session for first 9 weeks and 17th week (n = 36) vs minimal attention (weekly 5 to 10‐minute phone call providing supportive counselling) (n = 35) | |
| Outcomes | CAPS, MPSS, BDI‐II, DES‐II | |
| Notes | Experienced therapists delivered therapy and treatment adherence was assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: The method of sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Comment: The method of allocation concealment (if any) was not reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: ITT analyses were conducted. No reasons were given for withdrawals from the study (8 in the treatment arm and 7 from the minimal‐attention group.) |
| Selective reporting (reporting bias) | Unclear risk | Comment: All specified and expected outcomes appear to have been reported. |
| Other bias | Low risk | Comment: There were no other obvious sources of bias. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Research assistants blind to the assigned condition of the subject conducted all interviews, and treatment completers were asked not to mention having been in therapy at posttreatment assessments." |
Cloitre 2002.
| Methods | Randomised controlled trial | |
| Participants | 58 female child sexual abuse survivors in the USA | |
| Interventions | 16 bi‐weekly sessions of 1½ hours of prolonged exposure and affect regulation (n = 22) vs waitlist (n = 24) | |
| Outcomes | CAPS, BDI, STAI | |
| Notes | Experienced therapists. Treatment adherence measured. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: The method of sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Comment: The method of allocation concealment (if any) was not reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: There was a relatively high drop‐out rate (9 from active treatment, 3 from the waitlist). There were no reasons given for drop‐outs, but there were said to be no sociodemographic, clinical or symptom differences between completers and drop‐outs. ITT analyses were performed |
| Selective reporting (reporting bias) | High risk | There is emphasis on reporting improvements in affect regulation and interpersonal skills as opposed to PTSD symptoms. The Methods section does not seem to indicate that these were the primary outcome measures. |
| Other bias | Low risk | Comment: There were no other obvious sources of bias. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Clinician raters were blind to treatment condition at pre‐ and posttreatment." |
Cloitre 2010.
| Methods | Randomised controlled trial | |
| Participants | 104 female child sexual abuse survivors in the USA | |
| Interventions | STAIR/exposure vs support/exposure vs STAIR/support | |
| Outcomes | CAPS, PSS‐SR, negative mood regulation scale, BDI, STAI, Inventory of Interpersonal Problems, Interpersonal Support Evaluation List | |
| Notes | Treatment was delivered by doctoral level psychologists, who had been trained by leading experts in the field. Adherence was measured. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: The method of sequence generation was not reported. |
| Allocation concealment (selection bias) | Low risk | Quote "Randomization blocks of nine (three instances of each of the three conditions) were employed, generated by an individual not otherwise involved with the study. Within each randomly assigned condition, the participant was assigned to one of three therapists, based on a match in availability." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Analyses for all symptom outcome measures were performed on the intent‐to‐treat sample using data from all participants according to their randomizations assignment. Missing data were imputed using PROC MI in SAS (SAS Institute, Cary, N.C.) to generate 10 imputed data sets." |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | Low risk | Comment: There were no other obvious sources of bias. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Comment: Assessors were blinded. |
Cooper 1989.
| Methods | Randomised controlled trial | |
| Participants | 16 male Vietnam War veterans in the USA. All DSM‐III PTSD | |
| Interventions | 6 ‐ 14 90‐minute flooding sessions plus standard treatment (n = 8) vs standard treatment (n = 8) | |
| Outcomes | STAI, BDI | |
| Notes | No information was provided with regards to the therapists delivering treatment or any measures of treatment adherence. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "Efforts were made to preclude bias in assessment by maintaining as nearly random a procedure as possible" Comment: There were no details of the method of sequence generation, but the authors indicate that it was not entirely random. |
| Allocation concealment (selection bias) | High risk | Quote: "In all cases group assignment was pre‐decided before the participant agreed to participate...there were three exceptions to the rule of pre‐determined random assignment" Comment: Allocation does not seem to have been concealed. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | All 16 participants provided posttreatment data, but 2 were removed from the analysis of data from the experimental group due to not completing therapy (1 from each group). These individuals were said to have a more severe presentation. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | High risk | Comment: Very small sample. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Self‐report measures only, but it is not clear how these were administered. |
Devilly 1998.
| Methods | Randomised controlled trial | |
| Participants | 51 male combat veterans with DSM‐III‐R PTSD in Australia | |
| Interventions | 12 sessions of EMDR (n = 19) vs biofeedback‐assisted relaxation (n = 16) vs routine clinical care (n = 16) (all interventions included in meta‐analyses) | |
| Outcomes | Mississippi scale, PTSD symptom scale, IES, STAI, BDI | |
| Notes | Therapist trained by Francine Shapiro. No mention of an assessment of treatment adherence. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: The method of sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Comment: There is no mention of any measures taken to conceal allocation. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: There were no reasons given for drop‐outs (6 drop‐outs from EMDR, 4 drop‐outs from relaxation and 6 drop‐outs from usual care). Data from the completers were analysed. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported, |
| Other bias | Low risk | There were no other obvious sources of bias. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Comment: All measures were self‐reported and administered by post. |
Devilly 1999.
| Methods | Randomised controlled trial | |
| Participants | 32 participants with DSM‐IIIR PTSD (11 men, 21 women) in Australia | |
| Interventions | 8 sessions EMDR (n = 17) vs 9 sessions TFCBT (n = 15) in parallel. | |
| Outcomes | BDI, SCL‐90 Global distress, CMS, IES, PSS‐SR, PTSD Interview (DSM‐III‐R) | |
| Notes | Therapists were appropriately trained and experienced. Treatment adherence was measured. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "Participants were assigned to their experimental group using a stratified randomization technique: the first 10 referrals were assigned to the TTP condition (after a 50% chance of either TTP or EMDR) and the following 10 were assigned to the EMDR condition. This was done in order to consolidate therapist skills in each protocol and offset cross‐pollination of the two, different, therapeutic protocols. Subsequently, subjects were assigned alternatively to the two conditions until a full cohort was obtained in each condition." |
| Allocation concealment (selection bias) | Unclear risk | Comment: It is unclear whether any measures were in place for concealing allocation. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: Only the data of completers were included in analyses. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | High risk | Comment: There were differences in the baseline characteristics of the two groups, for example, medication profiles (which were continued through the course of the trial). |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: It is unclear whether outcome assessors were blinded. |
Duffy 2007.
| Methods | Randomised controlled trial | |
| Participants | 58 participants mostly resulting from the troubles in Northern Ireland (23 women, 35 men) | |
| Interventions | 12 weekly sessions of cognitive therapy (n = 29) vs waiting list (n = 29). Cross‐over trial. | |
| Outcomes | PDS, BDI, SDS | |
| Notes | Experienced therapists (1 social worker, 1 psychiatrist, and 3 nurse therapists). Treatment adherence does not seem to have been assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: The method of sequence generation was not reported. Participants were randomised remotely. |
| Allocation concealment (selection bias) | Low risk | Quote: "An independent office allocated patients to immediate therapy or to wait followed by therapy on a stratified random basis using the minimisation method of Pocock. Assessors were not aware of the allocation algorithm". |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "We carried out analyses on an intention to treat basis". Reasons for drop‐out were reported (9 from cognitive therapy and 3 from waiting list). |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported, |
| Other bias | High risk | Treatment adherence was not measured. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: Measures were self‐reported, but it is unclear how these were administered. |
Dunne 2012.
| Methods | Randomised controlled trial | |
| Participants | 26 adults (13 men, 13 women) with chronic motor vehicle collision PTSD with chronic whiplash‐associated disorders, in Australia | |
| Interventions | 10 weekly sessions of TFCBT (n = 13) vs waiting list (n = 13) | |
| Outcomes | SCID‐PTSD, PDS, IES‐R, DASS, SF‐36 | |
| Notes | Comment: All therapy delivered by 1 psychologist with 12 months experience of delivering TFCBT. It is unclear whether or not treatment adherence was assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: The method of sequence generation was not reported |
| Allocation concealment (selection bias) | Unclear risk | Comment: There is no mention of any measures taken to conceal allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: Reasons for leaving the study were fully reported, ITT analyses were performed. Appropriate methods of imputing data were used. One participant dropped out of the treatment group and 2 from the waitlist group. Reasons for attrition were not fully reported. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | High risk | Comment: All therapy delivered by 1 psychologist with 12 months experience of delivering TFCBT. It is unclear whether or not treatment adherence was assessed. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: It is unclear whether the outcome assessor was blind. |
Echeburua 1997.
| Methods | Randomised controlled trial | |
| Participants | 20 female sexual aggression survivors in Spain | |
| Interventions | 6 weekly sessions of graded self exposure (n = 10) vs relaxation therapy (n = 10) | |
| Outcomes | Global PTSD scale, STAI, BDI | |
| Notes | Treatment delivered by an experienced clinical psychologist. Treatment adherence was not measured. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: The method of sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Comment: There is no mention of any measures taken to conceal allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: No drop‐outs. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | High risk | Comment: Small sample size. Treatment adherence was not measured. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: It is unclear whether assessors were blinded. |
Ehlers 2003.
| Methods | Randomised controlled trial | |
| Participants | 69 participants with duration of PTSD greater than 3 months from a larger RCT of 85 participants with DSM‐IV PTSD in the UK. Various traumas. | |
| Interventions | 12 x weekly sessions of CT (n = 22) vs repeated assessment (n = 20) vs self help (n = 27) (CT and repeated assessment included in a meta‐analysis). | |
| Outcomes | CAPS, PDS, BDI, BAI | |
| Notes | Therapist details/credentials are not reported and it is unclear whether treatment adherence was measured. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Randomization was stratified by sex and severity of PTSD symptoms using the random permuted blocks within strata algorithm." Comment: The method of random sequence generation was not reported. |
| Allocation concealment (selection bias) | Low risk | Quote: "Assessors who decided whether patients were suitable for inclusion in the study could not predict what treatment condition would be assigned to the patient, as (1) the allocation list was kept locked in a separate central office and the patient’s allocation was only revealed 3 weeks later, following the self‐monitoring assessment, and (2) the study was conducted at 2 sites." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "As the most conservative estimate of the efficacy of CT, we report a completer analysis for the continuous outcome measures, comparing the full sample of patients allocated to CT (as there were no dropouts) with the completers in the SH and RA conditions." There were three drop‐outs from self help and two from repeated assessment. Reasons for drop‐outs were fully reported. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | High risk | Comment: Therapist details/credentials are not reported and it is unclear whether treatment adherence was measured. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Independent assessors (trained clinical psychologists or research nurses) who were not aware of the treatment condition gave the Clinician‐Administered PTSD Scale (CAPS‐SX) interview." Comment: There was a test of blinding. |
Ehlers 2005.
| Methods | Randomised controlled trial | |
| Participants | 28 individuals with DSM‐IV PTSD in the UK. Various traumas. | |
| Interventions | 12 x weekly sessions of CT (n=14) vs WL (n=14) | |
| Outcomes | CAPS, PDS, BDI, BAI | |
| Notes | Therapist details/credentials are not reported and it is unclear whether treatment adherence was measured. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were randomly allocated to either immediate cognitive therapy" Comment: The method of randomisation is clear. |
| Allocation concealment (selection bias) | Unclear risk | Comment: The method of allocation concealment was unclear. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: ITT analyses were performed. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | High risk | Comment: Therapist details/credentials are not reported and it is unclear whether treatment adherence was measured. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: Independent assessors were used. |
Fecteau 1999.
| Methods | Randomised controlled trial | |
| Participants | 23 road traffic accidents in Canada. 14 women, 6 men completed the study. It is unclear how many men and women entered the study originally | |
| Interventions | 8 ‐ 10 hours CBT (n = 12) vs waitlist (n = 11) | |
| Outcomes | CAPS, IES, BDI, BAI | |
| Notes | Experienced therapists delivered therapy and treatment adherence was assessed | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "participants were then randomly assigned to the treatment or WLC groups by the flip of a coin". |
| Allocation concealment (selection bias) | Unclear risk | Comment: There is no mention of any measures taken to conceal allocation. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: 2 participants dropped out of the treatment group and 1 dropped off the waitlist. Reasons for attrition are reported. Only the data of completers are included in the analysis. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported, although the lack of effect on the measure of depression is not divulged in the abstract. |
| Other bias | High risk | Comment: Small sample size. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: Outcome measures were rated by an "independent assessor". |
Feske 2008.
| Methods | Randomised controlled trial | |
| Participants | 27 low‐income African‐Americans with complex trauma histories and | |
| Interventions | 9 ‐ 12 weekly sessions of PE vs 9 ‐ 12 sessions of non‐TF supportive counselling DSM‐IV PTSD | |
| Outcomes | PTSD Diagnostic Scale, BDI, BAI, BSQ, Anger Expression Inventory, Brief Symptom Inventory | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: The method of sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Comment: There is no mention of any measures taken to conceal allocation. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: Drop‐outs reported (2 for unknown reasons). Completers Analysis. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | High risk | Comment: Small sample size. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: It is unclear whether outcome assessors were blinded. |
Foa 1991.
| Methods | Randomised controlled trial | |
| Participants | 55 female rape victims in the USA. All DSM‐IIIR PTSD | |
| Interventions | 9 1½‐hour sessions of prolonged exposure (n = 14) vs stress inoculation training (n = 17) vs supportive counselling (n = 14) vs waiting list (n = 10) control (all interventions included in meta‐analyses). | |
| Outcomes | PTSD severity, BDI, STAI | |
| Notes | Experienced therapists delivered therapy and treatment adherence was assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: The method of sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Comment: There is no mention of any measures taken to conceal allocation. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "Subsequent analyses were conducted on data from the 45 completers." Comment: 10 participants dropped out of treatment (prolonged exposure (4) vs stress inoculation training (3) vs supportive counselling (3) vs waiting list control (0)). No reasons reported for drop‐outs. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | Low risk | Comment: There were no other obvious sources of bias. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Assessments at pre‐treatment, posttreatment, and follow‐up consisted of clinical interviews conducted by an independent assessor, who was blind to treatment conditions, and self report questionnaires" |
Foa 1999.
| Methods | Randomised controlled trial | |
| Participants | 96 female sexual assault victims (69 sexual assault) in the USA | |
| Interventions | 9 sessions (2 x 2 hours, 7 x 1½ hours) prolonged exposure (n = 25) vs stress inoculation training (n = 26) vs combination PE‐SIT (n = 30) vs waiting list (n = 15) (all interventions included in meta‐analyses). | |
| Outcomes | PSS‐I, BDI, STAI | |
| Notes | Experienced therapists delivered therapy and treatment adherence was assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: The method of sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Comment: There is no mention of any measures taken to conceal allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: ITT analyses performed. 17 participants dropped out of treatment (2 from prolonged exposure, 7 from SIT and 8 from PE‐SIT). |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | High risk | Comment: There were no other obvious sources of bias. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Independent evaluators... were unaware of treatment assignment". |
Foa 2005.
| Methods | Randomised controlled trial | |
| Participants | 171 female sexual assault survivors in the USA | |
| Interventions | 9 ‐ 12 weekly 90‐ to 120‐minute sessions of prolonged exposure (n = 79) vs 9 ‐ 12 weekly 90‐ to 120‐minute sessions of prolonged exposure and cognitive restructuring (n = 74) vs waiting list (n = 26) (all interventions included in meta‐analyses). | |
| Outcomes | PSS‐I, BDI, SAS | |
| Notes | Experienced therapists delivered therapy and treatment adherence was assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The study statistician assigned participants who provided informed consent to one of the three conditions using a weighted randomizations procedure such that participants were assigned to one of the active treatment conditions at a greater rate than to WL." Comment: Although reported to be carried out by a statistician, the method of sequence generation is unclear. |
| Allocation concealment (selection bias) | Low risk | Quote: "The study statistician assigned participants who provided informed consent to one of the three conditions using a weighted randomizations procedure such that participants were assigned to one of the active treatment conditions at a greater rate than to WL." Comment: Participants were assigned to a group by an external person. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: ITT analyses were performed. Reasons for drop‐out were not fully reported. There were many drop‐outs (1 from waiting list, 30 from PE/CR and 27 from PE). |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported |
| Other bias | Low risk | Comment: There were no other obvious sources of bias. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "All evaluations were conducted by trained doctoral or master’s level CTSA clinicians who were blind to study condition." "Participants were instructed by their therapists and the evaluators to not reveal any information that might unblind the evaluator to treatment condition." |
Forbes 2012.
| Methods | Randomised controlled trial | |
| Participants | 59 veterans (57 men) with military‐related PTSD in Australia | |
| Interventions | 12 sessions of cognitive processing therapy (n = 30) vs treatment as usual (n = 29) | |
| Outcomes | CAPS, PCL, BDI‐II, STAI‐State, DAR‐7, AUDIT, PTCI, ADAS, WHOQOL | |
| Notes | Experienced therapists delivered therapy and treatment adherence was assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: The method of random sequence generation was not reported. |
| Allocation concealment (selection bias) | Low risk | Comment: A central method of allocation was employed. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: Reasons for leaving the study were fully reported, ITT analyses were performed. Appropriate methods of imputing data were used. 9 participants dropped out of each group. Reasons for attrition are not fully reported. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | High risk | Comment: Different therapists provided CPT and TAU. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote: "All assessments were conducted by an independent clinical assessor blind to allocation and treatment. To maintain blindness at post‐treatment and 3 month follow‐up appointments the participants were reminded not to reveal what treatment they had received." |
Galovski 2012.
| Methods | Randomised controlled trial (cross‐over) | |
| Participants | 100 individuals (unclear how many were men and women) with PTSD after sexual or physical assault in childhood or adulthood in the USA | |
| Interventions | CPT (n = 47) vs symptom monitoring delayed treatment (n = 53) | |
| Outcomes | CAPS, BDI‐II, TRGI, QOLI, SF‐36 | |
| Notes | Experienced therapists delivered therapy and treatment adherence was assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: The method of sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Comment: There is no mention of any measures taken to conceal allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: 7 participants dropped out of symptom monitoring delayed treatment and 14 dropped out of CPT. The reason for drop‐out was unknown in 50% of cases. ITT analyses were performed. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | Low risk | Comment: There were no other obvious sources of bias. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Posttreatment and follow‐up assessments were conducted by raters blind to both randomization and dropout status." |
Gamito 2010.
| Methods | Randomised controlled trial | |
| Participants | 10 male war veterans of the Portugese Colonial War between 1963 and 1970 with DSM‐IV PTSD | |
| Interventions | Virtual reality exposure (n = 5) vs exposure in imagination versus WL (n = 3) vs exposure in imagination (n = 3) in parallel | |
| Outcomes | CAPS, IES | |
| Notes | Comment: It is unclear who delivered the therapy | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The participants were randomly assigned to three study groups". Comment: The method of sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Comment: There is no mention of any measures taken to conceal allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: There was 1 drop‐out (from virtual reality exposure) without a reason. It is unclear how these missing data were handled. |
| Selective reporting (reporting bias) | High risk | Comment: Improvements in depression and anxiety were emphasised, despite measures of PTSD being indicated as the primary outcome measure. |
| Other bias | High risk | Very small sample size. It is unclear who delivered the therapy. Treatment adherence was not measured. Baseline characteristics are poorly reported. The issue of researcher allegiance cannot be ruled out. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: It is unclear whether outcome assessors were blinded. |
Gersons 2000.
| Methods | Randomised controlled trial | |
| Participants | 42 police officers. DSM‐IIIR PTSD. Various workplace traumas (5 women, 37 men) in the Netherlands | |
| Interventions | 16 x 60‐minute sessions of brief eclectic therapy (n = 22) vs wait list (n = 20) in parallel | |
| Outcomes | SI‐PTSD, SCL‐90 | |
| Notes | Experienced therapists delivered therapy. It is unclear whether or not treatment adherence was assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: The method of sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Comment: There is no mention of any measures taken to conceal allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: ITT analyses were conducted. Only 1 participant dropped out, from the waitlist. A reason was given for this individual leaving the study. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | High risk | Comment: The issue of researcher allegiance cannot be ruled out. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "All assessments were performed by one of three independent assessors". |
Hensel‐Dittmann 2011.
| Methods | Randomised controlled trial | |
| Participants | 28 asylum seekers who had experienced war and torture | |
| Interventions | Narrative Exposure Therapy (n = 15) vs Stress Innoculation Therapy (n = 13) | |
| Outcomes | CAPS, HAM‐D | |
| Notes | Experienced therapists delivered therapy and treatment adherence was assessed | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Subjects were randomly assigned to either NET or SIT. Participants were matched pairwise according to gender, age, and region of origin and were then allocated to NET or SIT by flipping a coin." |
| Allocation concealment (selection bias) | Low risk | Comment: There is no mention of any measures taken to conceal allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Aiming at an intention‐to‐treat analysis, all subjects who were randomised were included in the outcome analysis. Much of the recent literature indicates that last‐observation‐ carried‐forward procedures may produce seriously biased results. Hence we used mixed effects models." Comment: There were 3 drop‐outs from TFCBT and 2 from non‐TFCBT. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | Low risk | Comment: There were no other obvious sources of bias. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote "We aimed to keep the assessors blind to the treatment conditions of the subjects; however, occasionally the treatment condition was revealed to the rater by responses from the patient." |
Hinton 2005.
| Methods | Randomised controlled trial | |
| Participants | 40 treatment‐resistant Cambodian refugees with comorbid panic attacks (24 women, 16 men) | |
| Interventions | 12 weekly sessions of CBT (n = 10) vs delayed treatment (n = 10) | |
| Outcomes | CAPS, ASI, N‐PASS, O‐PASS, N‐FSS, O‐FSS, SCL | |
| Notes | Experienced therapists delivered therapy. It is unclear whether or not treatment adherence was assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: The method of sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Comment: There is no mention of any measures taken to conceal allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "All randomised patients completed the study, and there were no missing data." |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | Low risk | Comment: There were no other obvious sources of bias. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Blind to treatment condition, all assessments were made by a Cambodian bicultural worker (D.C., V.P.) with over 2 years of mental health experience." |
Hinton 2011.
| Methods | Randomised controlled trial | |
| Participants | 24 Latino women with treatment‐resistant PTSD | |
| Interventions | 14 weekly sessions of TFCBT (n = 12) vs applied muscle relaxation (n = 12) | |
| Outcomes | PTSD checklist, nervios scale, emotion regulation scale, SCL anxiety scale | |
| Notes | Experienced therapists delivered therapy. It is unclear whether or not treatment adherence was assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: The method of sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Comment: There is no mention of any measures taken to conceal allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: There were no drop‐outs. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | High risk | Small sample size. Participants continued medication and supportive therapy. Details were not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Self‐report questionnaires were used, but not clear how they were administered |
Hogberg 2007.
| Methods | Randomised controlled trial | |
| Participants | 24 transportation workers with DSM‐IV PTSD (19 men, 5 women) in Sweden. | |
| Interventions | EMDR (n = 13) vs waitlist (n = 11) | |
| Outcomes | GAF, HAM‐A, HAM‐D, IES, BAI | |
| Notes | Experienced therapists delivered therapy and treatment adherence was assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote "The randomisation was done by picking a sealed ballot in the presence of a research nurse who coordinated the study and followed the participants through all phases." |
| Allocation concealment (selection bias) | Unclear risk | Comment: The method of random sequence generation was not reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "We decided not to use an intention to treat analysis because there were no drop‐outs during EMDR". Comment: 2 individuals dropped out of the waitlist group. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | High risk | Comment: Small sample size. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "by a psychiatrist not otherwise engaged in the study and blind to the experimental condition of the participants." |
Hollifield 2007.
| Methods | Randomised controlled trial | |
| Participants | 84 individuals with DSM‐IV PTSD, various traumas in the USA | |
| Interventions | CBT (n = 28) vs acupuncture (n = 29) vs WL (n = 27) (CBT and WL included in a meta‐analysis). | |
| Outcomes | PSS‐SR, HSCL‐25, Sheehan Disability Scale | |
| Notes | There were no reported assessments of treatment fidelity, and little information about the individuals who delivered the treatments. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: “before enrolling participants, 90 study ID numbers were pre‐randomized using a computerized random numbers procedure without restrictions. This allocation procedure was concealed from clinicians.” |
| Allocation concealment (selection bias) | Low risk | Quote: “before enrolling participants, 90 study ID numbers were pre‐randomized using a computerized random numbers procedure without restrictions. This allocation procedure was concealed from clinicians.” |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: ITT analyses were performed using acceptable methods. Reasons for withdrawal were fully reported (10 from acupuncture, 7 from CBT and 27 from wait list). |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | High risk | Comment: Each intervention was delivered by a single practitioner. There were no reported assessments of treatment fidelity, and little information about the individuals who delivered the treatments. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Self‐report measures only. Quote “The RC collected the data which were concealed from investigator/clinician.” |
Ironson 2002.
| Methods | Randomised controlled trial | |
| Participants | 22 victims of various traumas with DSM‐IIIR PTSD (17 women, 5 men) in the USA | |
| Interventions | 3 preparatory sessions followed by 1 ‐ 3 sessions of EMDR (n = 10) or prolonged exposure (n = 12) | |
| Outcomes | PSS‐SR, BDI | |
| Notes | Experienced therapists delivered therapy and treatment adherence was assessed. Therapists delivered both treatments. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: The method of sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Comment: There is no mention of any measures taken to conceal allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: ITT analyses were performed. Reasons for drop‐out were not fully reported (1 from EMDR, 6 from TFCBT). |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | High risk | Comment: Baseline characteristics are poorly reported. Small sample size. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: All measures were self report, but assessors were not blind. |
Jensen 1994.
| Methods | Randomised controlled trial | |
| Participants | 29 male Vietnam War veterans with PTSD in the USA | |
| Interventions | 3 sessions of EMDR (n = 15) usually within 10 days vs usual care (n = 14) | |
| Outcomes | SI‐PTSD | |
| Notes | Experienced therapists delivered therapy. It is unclear whether or not treatment adherence was assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: The method of sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Comment: There is no mention of any measures taken to conceal allocation. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: Only the data of completers are included in the analysis. Reasons for drop‐outs were not fully reported. 2 participants dropped out from each group. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | High risk | Comment: Small sample size. Baseline characteristic are poorly reported. Unclear whether treatment adherence was measured. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: It is unclear whether outcome assessors were blinded. |
Keane 1989.
| Methods | Randomised controlled trial | |
| Participants | 24 male Vietnam War veterans with DSM‐IIIR PTSD in the USA | |
| Interventions | 14 ‐ 16 sessions implosive (flooding) (n = 11) versus waiting list control (n = 13) | |
| Outcomes | PTSD subscale, BDI, STAI | |
| Notes | Experienced therapists delivered therapy. It is unclear whether or not treatment adherence was assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: The method of sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Comment: There is no mention of any measures taken to conceal allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | There is emphasis in the reporting on those scales where improvements were evident. |
| Selective reporting (reporting bias) | Unclear risk | Comment: Only the data of completers are included in the analysis. One participant dropped out of each group. |
| Other bias | High risk | Comment: Small sample size. Poor reporting of baseline characteristics. Unclear whether or not treatment adherence was measured. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote: "therapists rated their own patients progress following treatment." |
Kearney 2013.
| Methods | Randomised controlled trial | |
| Participants | 47 veterans (37 men) with chronic PTSD in the USA | |
| Interventions | Mindfulness‐Based Stress Reduction (MBSR) (n = 25) group intervention vs TAU (n = 22) | |
| Outcomes | PCL, PHQ‐9, BADS, SF‐8, FFMQ | |
| Notes | Therapist credentials/experience is not reported. It is unclear whether or not treatment adherence was assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: The method of random sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "assessment subjects were randomized using concealed allocation to the intervention group" ‐ precise methods of allocation concealment were not reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: Reasons for leaving the study were fully reported, ITT analyses were performed. Appropriate methods of imputing data were used. 2 participants dropped out from the treatment group and 1 from the waitlist. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | High risk | Comment: Therapist credentials/experience is not reported. It is unclear whether or not treatment adherence was assessed. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | There is no mention of the blinding of assessors. Measures were self report. |
Krakow 2000.
| Methods | Randomised controlled trial | |
| Participants | 169 female sexual abuse survivors reporting nightmares at least once a week in the USA | |
| Interventions | 3 sessions (2 x 3‐hour 1 week apart and 1 x 1‐hour follow‐up 3 weeks later) of cognitive imagery rehearsal for nightmares (n = 87) vs waiting list (n = 82). | |
| Outcomes | Nightmare Frequency Questionnaire, PSS, Pittsburgh Sleep Quality Index, Nightmare Effects Survey | |
| Notes | It is unclear who delivered the intervention or whether or not treatment adherence was measured. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: The method of sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Comment: There is no mention of any measures taken to conceal allocation. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "The main analysis was conducted on the 91 completers". The drop‐out rate was very high and reasons for leaving the study were not fully reported. |
| Selective reporting (reporting bias) | High risk | Comment: Completer data were reported despite a very high drop‐out rate. |
| Other bias | High risk | Comment: The issue of researcher allegiance cannot be ruled out. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: All measures were self‐reported but it is unclear how these were administered. |
Krakow 2001.
| Methods | Randomised controlled trial | |
| Participants | 168 female sexual assault survivors. 95% DSM‐IIIR PTSD in the USA | |
| Interventions | 2 x 3‐hour and 1 x 1‐hour sessions of group imagery rehearsal (n = 88) versus waiting list (n = 80) | |
| Outcomes | PSS | |
| Notes | Therapist credentials/experience is not reported. It is unclear whether or not treatment adherence was assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "To mask treatment assignment, patients mailed back a postcard after intake to complete entry into the protocol The postcard’s time and date were logged into a computer and entered into a previously generated list of numbers that randomly assigned participants to treatment and control groups. All numbers and group assignments were generated at the start of the protocol". Comment: The method of sequence generation was not reported |
| Allocation concealment (selection bias) | Low risk | Quote: "To mask treatment assignment, patients mailed back a postcard after intake to complete entry into the protocol The postcard’s time and date were logged into a computer and entered into a previously generated list of numbers that randomly assigned participants to treatment and control groups. All numbers and group assignments were generated at the start of the protocol". |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: ITT analyses were performed. 20 withdrew from waitlist and 22 from the treatment group. Reasons for attrition are not fully reported. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported |
| Other bias | High risk | Comment: The issue of researcher allegiance cannot be ruled out. Therapist credentials/experience is not reported. It is unclear whether or not treatment adherence was assessed. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote "To limit external bias, blinding occurred at 3 points of data collection: (1) at intake, group assignment had not been established; (2) at 3‐month follow‐up, questionnaires were completed through the mail; and (3) at 6‐month follow‐up, interviewers were unaware of group status." |
Kubany 2003.
| Methods | Randomised controlled trial | |
| Participants | 37 female survivors of assault in Hawaii | |
| Interventions | 8 ‐ 11 bi‐weekly 90‐minute sessions of cognitive trauma therapy (n = 19) vs waitlist with delayed treatment (n = 18) | |
| Outcomes | CAPS, BDI | |
| Notes | Lead author was therapist for all participants. It is unclear whether treatment adherence was addressed | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "After these assessments, the women were randomly assigned to either an Immediate or a Delayed CTT‐BW condition." Comment: The method of random sequence generation was not reported, |
| Allocation concealment (selection bias) | Unclear risk | Comment: There is no mention of any measures taken to conceal allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: ITT analyses. 1 participant dropped out from the treatment group and 4 from the waitlist. |
| Selective reporting (reporting bias) | Unclear risk | Comment: All specified outcomes were reported. |
| Other bias | High risk | Comment: The issue of researcher allegiance cannot be ruled out. Lead author originated CTT‐BW and conducted all therapy. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The assessors were blind to participants’ condition assignments." |
Kubany 2004.
| Methods | Randomised controlled trial | |
| Participants | 125 female survivors of assault in Hawaii | |
| Interventions | 8 ‐ 11 bi‐weekly 90‐minute sessions of cognitive trauma therapy (n = 63) vs waitlist (n = 62) | |
| Outcomes | CAPS, BDI | |
| Notes | Experienced therapists delivered therapy and treatment adherence was assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: The method of sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Comment: There is no mention of any measures taken to conceal allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: ITT analyses. Data were only available for 84 participants posttreatment. 22 dropped out of waitlist and 18 from TFCBT. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | High risk | Comment: The issue of researcher allegiance cannot be ruled out. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Comment: Assessors were blinded |
Lee 2002.
| Methods | Randomised controlled trial | |
| Participants | 24 DSM‐IV PTSD sufferers. Various traumas (11 women, 13 men) in Australia. | |
| Interventions | 7 weekly 90‐minute sessions of stress inoculation training with prolonged exposure (n = 12) vs EMDR (n = 12) | |
| Outcomes | SI‐PTSD, IES, BDI | |
| Notes | Experienced therapists delivered therapy and treatment adherence was assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "There was random assignment to all conditions and multiple therapists were used to deliver each of the treatments." Comment: The method of random sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Comment: There is no mention of any measures taken to conceal allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "treatment non‐completers were included in the analysis". Comment: 3 participants dropped out from treatment, 1 from EMDR and one from stress management. It is unclear what group the third drop‐out was in. Reasons for drop‐out were not fully reported. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | High risk | Comment: Small sample size. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "assessments by a blind independent observer". |
Lindauer 2005.
| Methods | Randomised controlled trial | |
| Participants | 24 DSM‐IV PTSD sufferers. Various traumas (11 men, 13 women) in the Netherlands | |
| Interventions | 16 weekly 45‐ to 60‐minute sessions of Brief Eclectic Psychotherapy (n = 12) vs waiting list (n = 12) | |
| Outcomes | SI‐PTSD, HADS | |
| Notes | Experienced therapists delivered therapy and treatment adherence was assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A colleague who had done no assessments used a computer program to randomly assign 12 patients to each condition in a block design." |
| Allocation concealment (selection bias) | Low risk | Quote: "A colleague who had done no assessments used a computer program to randomly assign 12 patients to each condition in a block design." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Intention‐to‐treat and per‐protocol analyses were calculated." Comment: 5 participants dropped out of the treatment group and 1 from the waitlist group. Reasons were fully reported. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | High risk | Comment: Small sample size. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. The issue of researcher allegiance cannot be ruled out. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Each patient was assessed by a researcher (R.J.L.L. or E.P.M.M.), who were blind to all patients’ condition." |
Marcus 1997.
| Methods | Randomised controlled trial | |
| Participants | 67 DSM‐IIIR PTSD. Various traumas. (53 women, 14 men) in the USA | |
| Interventions | Variable number of 50‐minute sessions of EMDR (n = 34) vs standard care (n = 33) | |
| Outcomes | IES, M‐PTSD, BDI, STAI, SCL‐90 | |
| Notes | Therapists were psychologists with experience ranging from less than one year to over 18. It is unclear what experience the therapists delivering usual care had. There was no report of assessing treatment adherence. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: The method of sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Comment: There is no mention of any measures taken to conceal allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: 1 participant dropped out of each group. It is unclear how this was handled. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | High risk | Comment: The usual care group, which included an array of interventions was not aimed at being optimally effective in terms of reducing symptom severity. There is little detail regarding the interventions offered as part of usual care and the credentials/experience of therapists delivering these interventions is not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote: "It was not possible to keep the independent evaluator blind to the treatment condition". |
Marks 1998.
| Methods | Randomised controlled trial | |
| Participants | 87 DSM‐IIIR PTSD, various traumas, in the UK | |
| Interventions | 10 x 90‐minute sessions of exposure (n = 23) vs cognitive restructuring (n = 19) vs exposure and cognitive restructuring (n = 24) vs relaxation therapy (n = 21) (the three exposure/cognitive‐restructuring groups were combined). | |
| Outcomes | CAPS, IES, BDI, STAI | |
| Notes | Experienced therapists delivered therapy. Treatment adherence was assessed, as was homework compliance. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: The method of sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Comment: There is no mention of any measures taken to conceal allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "analyses were also done on end‐point imputed‐scores carrying forward non‐completers last available ratings". Comment: There were drop‐outs from each group: exposure (3) cognitive restructuring (1) exposure and cognitive restructuring (5) and relaxation therapy (1). Reasons for drop‐out were not fully reported. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | Low risk | Comment: no other sources of bias detected. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "assessors were kept unaware of the treatment condition". |
McDonagh 2005.
| Methods | Randomised controlled trial | |
| Participants | 74 female childhood sexual abuse survivors with DSM‐IV PTSD in the USA | |
| Interventions | 7 x 2‐hour and 7 x 1½‐hour sessions of CBT (n = 29) versus 7 x 2‐hour and 7 x 1½‐hour sessions of PCT (n = 22) versus waitlist control (n = 23). (all interventions included in meta‐analyses). | |
| Outcomes | CAPS, BDI, STAI, TSI, DES, STAXI | |
| Notes | Experienced therapists delivered therapy and treatment adherence was assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: The method of sequence generation was not reported |
| Allocation concealment (selection bias) | Unclear risk | Comment: There is no mention of any measures taken to conceal allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: ITT analyses using the LOCF method were performed. Reasons for drop‐out were not fully reported. 12 participants dropped out of CBT, 2 from PCT and 3 from the waitlist. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | Low risk | Comment: There were no other obvious sources of bias. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "A separate group of female clinicians, who were blind to treatment condition and who had no other role in the study conducted the four CAPS interviews". |
Monson 2006.
| Methods | Randomised controlled trial | |
| Participants | 60 DSM‐IV‐TR PTSD. Combat veterans (54 men, 6 women) in the USA | |
| Interventions | 12 sessions of cognitive processing therapy conducted twice weekly when possible (n = 30) vs waitlist (n = 30) | |
| Outcomes | CAPS, PCL, BDI, STAI | |
| Notes | Experienced therapists delivered therapy and treatment adherence was assessed | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote "Eligible participants were randomised to receive the treatment immediately or to wait for 10 weeks to receive the treatment (10 weeks was equivalent to the ideal 6 weeks of twice weekly sessions and the 1‐month follow‐up period for those in the CPT condition). The study biostatistician provided the participants’ condition assignment to the study coordinator." Comment: The method of random sequence generation was not reported. |
| Allocation concealment (selection bias) | Low risk | Quote "Eligible participants were randomised to receive the treatment immediately or to wait for 10 weeks to receive the treatment (10 weeks was equivalent to the ideal 6 weeks of twice weekly sessions and the 1‐month follow‐up period for those in the CPT condition). The study biostatistician provided the participants’ condition assignment to the study coordinator." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote "Primary analyses were performed according to the intention‐to‐treat principle; data from all participants were used regardless of their treatment completion." Comment: 6 participants dropped out from the treatment group. 4 participants dropped out from the waitlist group. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | Low risk | Comment: There were no other obvious sources of bias. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote "The independent clinician assessors were blinded to condition assignment and participants were instructed to not disclose their condition assignment to them." |
Mueser 2008.
| Methods | Randomised controlled trial | |
| Participants | 108 DSM‐IV PTSD individuals with severe mental illness receiving treatment at community health centres (46 men, 62 women) in the USA | |
| Interventions | 12 ‐ 16 sessions of TFCBT (n = 54) or TAU (n = 54) | |
| Outcomes | CAPS, PTSD knowledge test, BAI, BDI, BPRS, WAI, SF‐12 | |
| Notes | Experienced therapists delivered therapy and treatment adherence was assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: The method of random sequence generation was not reported. |
| Allocation concealment (selection bias) | Low risk | Quote: "Randomization was conducted at a central location in the research centre by a computer‐based randomizations program, with assignments not known in advance by either clinical or research staff." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: ITT analyses were performed. 11 participants dropped out of the treatment group and 11 from TAU. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | High risk | Comment: There were no other obvious sources of bias. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: “All assessments were conducted by master’s or Ph.D. level trained clinical interviewers who were blind to treatment assignment. Clients were instructed at the beginning of interviews to not talk about any treatments for trauma‐related problems they may have received. Interviewers were requested to inform the project coordinator if the client broke the blind during an interview. Interviewers were not asked to guess clients’ treatment assignments, to avoid directly encouraging them to formulate hypotheses about how treatment may have affected clients’ symptoms, which could have influenced subsequent ratings. No specific instances of blind breaking were noted in the study.” |
Neuner 2004.
| Methods | Randomised controlled trial | |
| Participants | 43 Sudanese refugees in Uganda. All diagnosed with PTSD. (16 men, 27 women) | |
| Interventions | 4 sessions of NET (n = 17) vs 4 sessions of supportive counselling (n = 14) vs one session of psychoeducation (n = 12) (NET and supportive counselling groups included in meta‐analysis). | |
| Outcomes | PDS | |
| Notes | Experienced therapists delivered therapy. Treatment adherence was not monitored, | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Each participant was randomly assigned (using a dice) to one of three treatment groups: narrative exposure therapy, supportive counselling, or psychoeducation only." |
| Allocation concealment (selection bias) | Unclear risk | Comment: There is no mention of any measures taken to conceal allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: One participant dropped out from NET and two from supportive counselling. ITT analyses were performed. Reasons for drop‐out were not fully reported. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | High risk | Comment: The issue of researcher allegiance cannot be ruled out. Treatment adherence was not monitored. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The local and expert interviewers who carried out the posttests, as well as the follow‐up tests, were blind for the individual participant’s treatmentcondition." |
Neuner 2008.
| Methods | Randomised controlled trial | |
| Participants | 277 Rwandan and Somalian refugees diagnosed with PTSD (142 women, 135 men) | |
| Interventions | NET (n = 111) vs trauma counselling (n = 111) vs monitoring (n = 55) (NET and monitoring included in meta‐analysis). | |
| Outcomes | PDS, DFMQ, SRQ‐20, SF‐12 | |
| Notes | Experienced therapists delivered therapy. Treatment adherence was not monitored, | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The participants were assigned to the groups in the following way: The list of participants was ordered randomly; the first 4 were consecutively assigned to the NET, TC, NET, and TC groups; and the fifth was assigned to the MG (monitoring) group. This procedure was repeated until all 277 participants were assigned." Comment: The method of random sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Comment: There is no mention of any measures taken to conceal allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Aiming at an intention‐to‐treat analysis, we included in the outcome analysis all participants who were randomised. In anticipation of a high rate of missing data, we considered a last observation‐ carried‐forward procedure as too conservative. Instead we chose to apply mixed‐effects models that allow the inclusion of all available data without the arbitrary replacement or imputation of missing values." |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | Low risk | Comment: A large number of participants could not be located for follow‐up. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The participants who received treatment were reassessed 3 and 6 months later by the same local research assistants who had carried out the interviews for the survey. They were blind with respect to the particular treatment condition."` |
Neuner 2010.
| Methods | Randomised controlled trial | |
| Participants | 32 asylum seekers with DSM‐IV PTSD (22 men, 10 women) in Germany | |
| Interventions | NET (n = 16) vs TAU (n = 16) | |
| Outcomes | Posttraumatic Stress Diagnostic Scale, Hopkins Symptom Checklist‐25 depression Scale, Composite International Diagnostic Interview ‐ C Pain Score | |
| Notes | Experienced therapists delivered therapy. Treatment adherence was not monitored | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: The method of sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Comment: There is no mention of any measures taken to conceal allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "all the participants who were randomised were included in the outcome analysis." Comment: 2 participants dropped out of the treatment group. Reasons for drop‐out are not fully reported. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | High risk | Comment: The authors acknowledged having little information about the interventions prescribed as part of TAU. The issue of researcher allegiance cannot be ruled out. Treatment adherence was not monitored. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "we aimed at keeping interviewers blind to each participants condition." |
Nijdam 2012.
| Methods | Randomised controlled trial | |
| Participants | 140 adults with PTSD after a variety of different traumas (79 women, 61 men) | |
| Interventions | Brief ecclectic psychotherapy (n = 70) or EMDR (n = 70) | |
| Outcomes | IES‐R, SI‐PTSD, HADS depression, HADS anxiety | |
| Notes | Experienced therapists delivered therapy. It is unclear whether or not treatment adherence was assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: The method of random sequence generation was not reported. |
| Allocation concealment (selection bias) | Low risk | A method of central allocation was employed, whereby a psychologist unassociated with the rest of the study used a computer programme. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: ITT analyses were performed. Reasons for treatment drop‐out are fully reported, and unlikely to have caused bias. Missing data were imputed using appropriate methods. 28 individuals dropped out of EMDR and 22 from BEP. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | Low risk | Comment: The issue of researcher allegiance cannot be ruled out. Treatment adherence was not monitored. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "To ensure masking of assessors, one psychologist who had no other engagement in the study, had access to the computer program, kept a log file of all random assignments and assigned the patients to the therapists." |
Paunovic 2011.
| Methods | Randomised controlled trial | |
| Participants | 29 adult victims of crime with chronic PTSD (12 men, 17 women) | |
| Interventions | Exposure Inhibition Therapy (n = 14) vs waitlist (n = 15) | |
| Outcomes | CAPS, PCL, IES‐R, BAI, BDI, CSE, PTSI | |
| Notes | Experienced therapists delivered therapy. It is unclear whether or not treatment adherence was assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: The method of random sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Comment: The method of allocation concealement (if any) was not reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: Reasons for drop‐outs are not given. It is unclear how missing data were handled. There was one drop‐out from each group. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | High risk | There was only one author, who was seemingly responsible for all aspects of the study (recruitment, randomisation, assessment, therapy, analysis). The author had conceived the therapy that was being evaluated, based on a theory of PTSD they had previously formulated. The author acknowledged "this study must be replicated with a more rigorous design that fulfills all of the golden criteria for a randomized controlled study." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote: "The assessor was both the therapist and the author of the current study." |
Peniston 1991.
| Methods | Randomised controlled trial | |
| Participants | 29 male Vietnam War combat veterans with DSM‐III PTSD | |
| Interventions | 48 x 30‐minute sessions of EMG (n = 15) assisted desensitisation vs no treatment (n = 14) | |
| Outcomes | Nightmare and flashback frequency | |
| Notes | Therapist credentials/experience is not reported. It is unclear whether or not treatment adherence was assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: The method of sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Comment: There is no mention of any measures taken to conceal allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: It is unclear if there were any missing data, or how this was handled. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | Unclear risk | Comment: The study is not well‐reported. It is difficult to judge other sources of bias. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Comment: Blind assessors were used. |
Power 2002.
| Methods | Randomised controlled trial | |
| Participants | 105 outpatients with DSM‐IV PTSD. Various traumas (gender of those starting the study unclear) | |
| Interventions | 10 x 90‐minute weekly sessions of EMDR (n = 39) vs exposure plus cognitive restructuring (n = 37) vs waitlist (n = 29) (all interventions included in meta‐analyses). | |
| Outcomes | CAPS, HAM‐A, MADRS | |
| Notes | Experienced therapists delivered therapy, and treatment adherence was assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Following completion of the entire initial assessment, for those patients who met entry criteria, the blind assessor then opened a sealed envelope that informed as to which group patients were to be allocated." |
| Allocation concealment (selection bias) | Low risk | Quote: "Following completion of the entire initial assessment, for those patients who met entry criteria, the blind assessor then opened a sealed envelope that informed as to which group patients were to be allocated." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "Comparison between the 33 drop‐outs and the 72 completers regarding presentation at time of initial assessment produced no significant differences on any of the demographic characteristics or treatment outcome measures with the sole exception of a higher frequency score on the CAPS‐C Avoidance subscale for the drop‐outs t D 2.2, df D 103, p < 0.05. Subsequent analysis was conducted on the 72 completers." Comment: There were 12 drop‐outs from EMDR, 16 from EMDR plus cognitive restructuring and 5 from the waiting list. Reasons for drop‐out were not fully reported. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | Low risk | Comment: no other sources of bias detected. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "However, assessment at entry, end‐point and follow‐up were conducted by ‘blind’ assessors." |
Ready 2010.
| Methods | Randomised controlled trial | |
| Participants | 11 Vietnam War veterans with DSM‐IV PTSD with a CAPS score greater than 60 in the USA | |
| Interventions | 10 sessions of Virtual Reality Exposure (n = 6) vs 10 sessions of person‐centred therapy (n = 5) | |
| Outcomes | CAPS, BDI | |
| Notes | Therapist credentials/experience is not reported. It is unclear whether or not treatment adherence was assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: The method of sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Comment: There is no mention of any measures taken to conceal allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: One participant dropped out of each group. Reasons for drop‐out are not reported. It is unclear how missing data were handled. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | High risk | Comment: PCT was developed as a control condition for the purposes of the study. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: “Participants were administered the measures or interviews at pretreatment, posttreatment, and six‐month follow‐up by a licensed clinical psychologist with 3 years of experience working with Vietnam veterans. She remained blind to treatment condition.” |
Resick 2002.
| Methods | Randomised controlled trial | |
| Participants | 171 female rape victims with DSM‐IV PTSD | |
| Interventions | 13 hours of cognitive processing therapy or exposure bi‐weekly over 6 weeks (n = 124) versus minimal attention (n = 47). | |
| Outcomes | CAPS, PSS, BDI | |
| Notes | Experienced therapists delivered therapy, and treatment adherence was assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: The method of sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Comment: There is no mention of any measures taken to conceal allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: ITT analyses using LOCF. 33 participants dropped out from TFCBT and 47 from the waitlist. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | High risk | Comment: The issue of researcher allegiance cannot be ruled out. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Independent raters who were not otherwise involved in the project conducted assessments of treatment adherence and therapist competence." |
Rothbaum 1997.
| Methods | Randomised controlled trial | |
| Participants | 21 female sexual assault victims with DSM‐IIIR PTSD in the USA | |
| Interventions | 3 weekly 90‐minute sessions of EMDR (n = 11) vs wait list control (n = 9) (1 dropped out immediately after assessment). | |
| Outcomes | PSS, IES, BDI, STAI | |
| Notes | Experienced therapists delivered therapy, and treatment adherence was assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: The method of sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Comment: There is no mention of any measures taken to conceal allocation. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: 3 participants dropped out: 1 immediately after assessment, and 1 from each of the groups. ITT analyses were not performed. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | Unclear risk | Comment: Small sample size. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "independent assessor kept blind to the treatment condition". |
Rothbaum 2005.
| Methods | Randomised controlled trial | |
| Participants | 74 female rape victims in the USA | |
| Interventions | 9 x 90‐minute sessions of EMDR (25) vs 9 x 90‐minute sessions of prolonged exposure (23) vs waiting list (24) (two dropped out prior to randomisation). | |
| Outcomes | CAPS, SLESQ, PSS‐SR, IES‐R, BDI, DES‐II, STAI | |
| Notes | Experienced therapists delivered therapy, and treatment adherence was assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote "If the participant met criteria and gave consent, she was then randomised and scheduled accordingly". Comment: It is unclear how the sequence was generated. |
| Allocation concealment (selection bias) | Unclear risk | Comment: There is no mention of any measures taken to conceal allocation. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "Because only 2 of 14 participants who did not complete the study (1 in each of the active treatments) provide data other than baseline, intent‐to‐treat analyses provide no consequentially different results and are not included here." |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | Low risk | Comment: No other sources of bias detected. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "All assessments were conducted by IAs who were kept blind to the treatment condition." |
Scheck 1998.
| Methods | Randomised controlled trial | |
| Participants | 60 16‐ to 25‐year old female victims of various traumas. 77% DSM‐IV PTSD in the USA | |
| Interventions | 2 usually weekly sessions of EMDR (n = 30) vs active listening (n = 30) | |
| Outcomes | BDI, STAI, PENN, IES, TSCS | |
| Notes | Experienced therapists (volunteers) delivered therapy. It is unclear whether or not treatment adherence was assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Envelopes filled with papers labelled either EMDR or AL were shuffled and numbered 1 through 100. During each interview, envelopes were opened consecutively". |
| Allocation concealment (selection bias) | Low risk | Quote: "Envelopes filled with papers labelled either EMDR or AL were shuffled and numbered 1 through 100. During each interview, envelopes were opened consecutively". |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: Reasons for drop‐out were not fully reported (1 participant from AL, 1 from EMDR) . Only the data of completers are included in the analysis. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | High risk | Comment: It is unclear whether or not treatment adherence was assessed. Active listening was not intended as an effective intervention. The aim was to create a control that offered rapport, expectation of gain and sympathetic attention. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: Insufficient information. |
Schnurr 2003.
| Methods | Randomised controlled trial | |
| Participants | 360 male Vietnam War veterans with DSM‐IV PTSD in the USA | |
| Interventions | Weekly present‐focused group CBT for 30 weeks (n = 180) vs weekly trauma‐focused CBT group therapy for 30 weeks (n = 180) | |
| Outcomes | CAPS, GHQ, SF36 | |
| Notes | Experienced therapists delivered therapy, and treatment adherence was assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "The randomizations were performed using permuted blocks of 4 in 3 blocks of CAPS severity scores to ensure balance in treatment groups by CAPS score." Comment: The method of random sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Comment: There is no mention of any measures taken to conceal allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Often, intention‐to‐treat analysis is performed by using an individual’s last measurement before treatment dropout as the last outcome or by carrying it forward. This method has been criticized for the bias it can introduce. Instead, we attempted to measure participants regardless of the number of treatment sessions they attended or their treatment dropout status. To our knowledge, no previous studies of PTSD treatment have taken this approach, which is standard in clinical trials in other fields of medicine. Therefore, we also performed secondary analyses to examine the effect of TFGT among participants who completed most of the scheduled sessions." Comment: 62 dropped out from the TF group and 45 from the non‐TF group. |
| Selective reporting (reporting bias) | Unclear risk | Comment: All specified outcomes were reported. |
| Other bias | Low risk | Comment: no other sources of bias detected. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote "Assessments were performed by a master’s‐ or doctoral level clinician who was unaware of treatment assignment." |
Schnurr 2007.
| Methods | Randomised controlled trial | |
| Participants | 284 female veterans and active duty personnel in the USA | |
| Interventions | 10 weekly 90‐minute sessions of prolonged exposure (n = 141) vs 10 weekly 90‐minute sessions of present‐centred therapy (n = 143) | |
| Outcomes | CAPS, SF36, SSAI, BDI, ASI, PTSD checklist | |
| Notes | Experienced therapists delivered therapy, and treatment adherence was assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Verified eligible participants were randomised within each site to prolonged exposure or present‐centred therapy using permuted blocks with random block sizes of 4 or 6. All study data were stored at the study coordinating center." Comment: The method of random sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Comment: There is no mention of any measures taken to conceal allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Primary analyses were performed on the intention‐to‐treat sample, using data from all randomised participants." Reasons for drop‐out were fully reported (21 from PE and 17 from PCT). |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | Low risk | Comment: No other sources of bias detected. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Blinded assessors collected data before and after treatment and at 3‐ and 6‐month follow‐up." |
Taylor 2003.
| Methods | Randomised controlled trial | |
| Participants | 60 outpatients. Various traumas. DSM‐IV PTSD.(45 women, 15 men) in the USA | |
| Interventions | 8 90‐minute sessions of exposure therapy (n = 22), EMDR (n = 19) or relaxation training (n = 19) (all interventions included in meta‐analyses). | |
| Outcomes | CAPS, PDS, BDI | |
| Notes | Experienced therapists delivered therapy. It is unclear whether or not treatment adherence was assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: The method of sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Comment: There is no mention of any measures taken to conceal allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: ITT analyses. Drop‐outs were from each group (exposure therapy (7), EMDR (4) or relaxation training (4). |
| Selective reporting (reporting bias) | Unclear risk | Comment: Only measures of PTSD and depression are reported. It is unclear whether any other data were collected. |
| Other bias | Low risk | Comment: no other sources of bias detected. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "All interviews were conducted by clinic staff, who were blind to the participants’ treatment assignment." |
Vaughan 1994.
| Methods | Randomised controlled trial | |
| Participants | 36 various traumas. 78% DSM‐IIIR PTSD. (23 women, 13 men) in Australia | |
| Interventions | 3 ‐ 5 50‐minute sessions of image habituation training (n = 13), EMDR (n = 12) or applied muscular relaxation (n = 11) (all interventions included in meta‐analyses). | |
| Outcomes | PTSD structured interview, IES, STAI, BDI | |
| Notes | Therapist credentials/experience is not reported. It is unclear whether or not treatment adherence was assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: The method of random sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "After assessment each subject was randomly assigned to a treatment group and also to a wait list or non‐waitlist group. The procedure resulted in unequal numbers of subjects in the treatment groups ‐12 in EMD, 13 in IHT and 11 in AMR." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: No drop‐outs. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | Low risk | Comment: no other sources of bias detected. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "As a check of the independent rater’s blindness as to patients’ treatment categories, the rater was asked to guess the category post‐treatment but was unable to do this better than by chance (x2 = 3.72, P = ns)." |
Wells 2012.
| Methods | Randomised controlled trial | |
| Participants | 20 individuals with DSM‐IV PTSD (11 women, 9 men) in the UK | |
| Interventions | Meta cognitive therapy (n = 10) vs delayed treatment (n = 10) | |
| Outcomes | PDS, IES, BDI, BAI, TSQ | |
| Notes | Therapist credentials/experience is not reported. Treatment adherence was not formally assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: Allocated by a coin toss. |
| Allocation concealment (selection bias) | Low risk | Comment: Allocation was performed by an individual otherwise not involved with the study. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: ITT analyses were performed. One participant dropped out of the MCT group. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | High risk | Comment: Small sample size. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Comment: The assessor was blind. |
Zang 2013.
| Methods | Randomised controlled trial | |
| Participants | 22 (17 women, 5 men) adult survivors of the Sichuan earthquake with PTSD | |
| Interventions | NET (n = 11) versus WL (n = 11) | |
| Outcomes | IES‐R, GHQ‐28, HADS, CIOQ, MSPSS, SCSQ | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: The method of random sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Comment: Specific methods of allocation concealment were not reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: No‐one left the study early. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | High risk | Comment: Very small sample size. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The pre and post treatment assessments were carried out by a researcher not involved in treatment and blind to the treatment conditions." |
Zlotnick 1997.
| Methods | Randomised controlled trial | |
| Participants | 48 female sexual abuse survivors. All DSM‐IIIR PTSD in the USA | |
| Interventions | 15 2‐hour sessions of group affective management (n = 24) vs waiting list control (n = 24) | |
| Outcomes | DTS, CR‐PTSD, DES | |
| Notes | Therapist credentials/experience is not reported. It is unclear whether or not treatment adherence was assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: The method of sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Comment: There is no mention of any measures taken to conceal allocation. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: There were no reported reasons for drop‐out (7 from treatment and 6 from the waitlist).Only the data of completers are included in the analysis. |
| Selective reporting (reporting bias) | Low risk | Comment: All specified outcomes were reported. |
| Other bias | High risk | Therapist credentials/experience is not reported. It is unclear whether or not treatment adherence was assessed. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Self report measures only. |
ADAS ‐ Abbreviated Dyadic Adjustment Scale ADIS‐R – Anxiety Disorders Interview Schedule ‐Revised ASI – Addiction Severity Index AUDIT ‐ Alcohol Use Disorders Identification Test BADS ‐ Behavioural Activation for Depression Scale BAI – Beck Anxiety Inventory BDI – Beck Depression Inventory BPRS ‐ Brief Psychiatric Rating Scale BSQ – Body Sensations Questionnaire CAPS ‐ Clinician‐Administered PTSD Scale CES‐D ‐ Centre for Epidemiologic Studies Depression Scale CIDI ‐ Composite International Diagnostic Interview CIOQ ‐ Changes in Outlook Questionnaire CMS – Civilian Mississippi Scale CPT ‐ Continuous Performance Test CT ‐ Cognitive Therapy CTSA ‐ Centre for Treatment and Study of Anxiety DAR‐7 ‐ Dimensions of Anger Reactions DASS ‐ Depression Anxiety and Stress Scale DES‐II – Dissociative Experiences Scale II DFMQ ‐ Demography of Forced Migration Scale DTS – Davidson Trauma Scale EMDR ‐ eye movement desensitisation and reprocessing EMG ‐Electromyographic FAQ – Fear and Avoidance Scale FFMQ ‐ Five Facet Mindfulness Questionnaire GAF ‐ Global Assessment of Functioning GHQ‐28 ‐ General Health Questionnaire 28 GIS‐A – Global Improvement Scale – Assessor GIS‐S – Global Improvement Scale ‐ Self HADS ‐ Hospital Anxiety and Depression Scale HAM‐A – Hamilton Rating Scale for Anxiety HAM‐D ‐ Hamilton Rating Scale for Depression HDRS ‐ Hamilton Rating Scale for Depression HSCL‐25 – Hopkins Symptom Checklist‐25 IES – Impact of Event Scale IES‐R Impact of Event Scale ‐ Revised ICG ‐ Inventory of Complicated Grief ITT ‐ intention‐to‐treat LOCF ‐ last observation carried forward MADRS ‐ Montgomery‐Asberg Depression Rating Scale MEG ‐Magnetoencephalography M‐PTSD ‐ Mississippi Post‐Traumatic Stress Disorder Scale MPSS ‐ Modified PTSD Symptom Scale N‐FSS – Neck‐Focused Flashback Severity Scale N‐PASS – Neck‐Focused Panic Attack Severity Scale NET ‐ narrative exposure therapy ODI – Oswestry Disability Index O‐FSS – Orthostatic‐Focused Panic Attack Severity Scale O‐PASS ‐ Orthostatic Panic Attack Severity Scale PCL ‐ PTSD Checklist PCT ‐ Psychological Commitment to Team Scale PDS – Posttraumatic Diagnostic Scale PE‐SIT ‐ Prolonged Exposure ‐ Stress Innoculation Training PENN ‐ Penn Inventory for PTSD PHQ‐9 ‐ Patient Health Questionnaire ‐ 9 PS‐MPI – Pain Subscale – Multidimensional Pain Inventory PSS‐I ‐ PTSD Symptom Scale ‐ Interview PSS‐SR ‐ PTSD Symptom Scale – Self Report PTCI ‐ Posttraumatic Cognitions Inventory QOLI ‐ Quality of Life Inventory SAS – Social Adjustment Scale SAS‐SR ‐ Social Adjustment Scale Self Report SCID‐PTSD ‐ Structured Clinical Interview for DSM‐IV ‐ PTSD SCL‐90 ‐ Symptom Checklist ‐ 90 SDS ‐ Sheehan Disability Scale SF‐8 ‐ 8‐item Short Form Health Survey SF‐36 ‐ 36‐item Short Form Health Survey SI‐PTSD – Structured Interview for PTSD SLESQ ‐ Stressful Life Events Screening Questionnaire SPSI ‐ Social Problem Solving Inventory SRQ‐20 ‐ Self Regualtion Questionnaire ‐ 20 SSAI ‐ Spielberger State Anxiety Inventory ssVEF ‐ steady‐state visual evoked fields STAI ‐ Spielberger State—Trait Anxiety Inventory STAXI ‐ State‐Trait Anger Expression Inventory TAU ‐ treatment as usual TRGI ‐ Trauma Related Guilt Inventory TSCS ‐ Tennessee Self Concept Scale TSI – Trauma Symptom Inventory TSQ ‐ Trauma Screening Questionnaire TSSC – Traumatic Stress Symptom Checklist WAI ‐ Working Alliance Inventory WHOQOL ‐ World Health Organisation Quality of Life WSA – Work and Social Adjustment Scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Abbasnejad 2007 | No formal diagnosis of PTSD. |
| Arntz 2007 | TFCBT vs TFCBT. |
| Barabasz 2013 | Unclear how many participants were suffering ASD as opposed to PTSD (length of time since trauma was not reported). Not a true RCT. |
| Boudewyns 1990 | Group treatment with exposure or conventional one‐to‐one counselling. |
| Chemtob 1997 | Treatment designed for anger vs PTSD with anger measures used as primary outcomes. |
| Classen 2001 | No formal diagnosis of PTSD. |
| Classen 2010 | No formal diagnosis of PTSD. |
| Cole 2007 | No formal diagnosis of PTSD. |
| Davis 2007 | Only 67.3% of participants met diagnostic criteria for PTSD before entry into study. |
| Difede 2007a | Only 67.7% of participants met diagnostic criteria for PTSD before entry into study. |
| DuHamel 2010 | Only 19% of participants met diagnostic criteria for PTSD before entry into study. |
| Dunn 2007 | Treatment for depression not PTSD. |
| Echeburua 1996 | Trauma < 3 months before entry into study. |
| Edmond 1999 | No formal diagnosis of PTSD. |
| Falsetti 2001 | No formal diagnosis of PTSD. |
| Falsetti 2005 | |
| Foa 2006 | Trauma < 3 months before entry into study. |
| Frommberger 2004 | Psychological therapy vs pharmacotherapy. |
| Gidron 1996 | Not psychological treatment. |
| Ginzberg 2009 | No diagnosis of PTSD. |
| Glynn 1999 | Not an individual or group therapy. |
| Hiari 2005 | Participants only required to meet re‐experiencing and avoidance criteria of DSM‐IV criteria for PTSD. |
| Jaberghaderi 2004 | Participants under 18 (study included in Gillies 2012). |
| Knaevelsrud 2007 | No formal diagnosis of PTSD. |
| Lange 2001 | No formal diagnosis of PTSD. |
| Lange 2003 | No formal diagnosis of PTSD. |
| Litz 2007 | No formal diagnosis of PTSD. |
| Maercker 2006 | Only 48% of participants met diagnostic criteria for PTSD. Remainder had a diagnosis of "sub‐syndromal PTSD". |
| Mithoefer 2011 | TFCBT vs TFCBT. |
| Najavits 2006 | Mean age of participants 16 years [study included in Gillies 2012] |
| Paunovic 2001 | TFCBT vs TFCBT. |
| Price 2007 | No formal diagnosis of PTSD made. |
| Rabe 2008 | Only 48.5% of participants met diagnostic criteria for PTSD before entry into study. |
| Rothbaum 2006 | Pharmacotherapy versus pharmacotherapy plus psychological therapy. |
| Ryan 2005 | No formal diagnosis of PTSD. |
| Schaal 2009 | Age range 14 ‐ 28. |
| Shapiro 1989a | No formal diagnosis of PTSD. |
| Sloan 2004 | No formal diagnosis of PTSD. |
| Sloan 2005 | No formal diagnosis of PTSD. |
| Spence 2011 | Information on duration was not collected. Unkown whether participants had acute/chronic PTSD. |
| Tarrier 1999 | Compared trauma focused cognitive therapy with exposure therapy therefore both treatments = TFCBT. |
| Tucker 2007 | Pharmacotherapy versus placebo. |
| Van Emmerik 2008 | Only 46.6% diagnosis of PTSD. |
| Watson 1997 | Considered 3 different types of relaxation training with no other comparison group. |
| Wilson 1995 | < 50% PTSD at entry to study. |
| Yeomans 2010 | No formal diagnosis of PTSD. |
Characteristics of studies awaiting assessment [ordered by study ID]
Krupnick 2008.
| Methods | Randomised Controlled Trial |
| Participants | 37 female victims of domestic violence with DSM‐III R PTSD |
| Interventions | Group interpersonal psychotherapy (n = 32) versus WL (n = 16). |
| Outcomes | CAPS, Interpersonal Sensitivity, Need for Social Approval, Lack of Sociability, and Interpersonal Ambivalence |
| Notes |
Contributions of authors
JIB has been involved in the identification of studies, quality appraisal, data entry, analysis and writing of the review. NPR has been involved in quality appraisal. MA has been involved in the identification of studies, quality appraisal and writing of the review. RC has been involved in the identification of studies, quality appraisal and data entry. CL has been involved in the identification of studies, quality appraisal, data entry, analysis and writing of the review.
Declarations of interest
None known.
Edited (no change to conclusions)
References
References to studies included in this review
Adenauer 2011 {published data only}
- Adenauer H, Catani C, Gola H, Keil J, Ruf M, Schauer M, et al. Narrative exposure therapy for PTSD increases top‐down processing of aversive stimuli ‐evidence from a randomized controlled treatment trial. BMC Neuroscience 2011;12:127. [DOI: 10.1186/1471-2202-12-127] [DOI] [PMC free article] [PubMed] [Google Scholar]
Asukai 2010 {published data only}
- Asukai N, Saito A, Tsuruta N, Kishimoto J, Nishikawa, T. Efficacy of exposure therapy for Japanese patients with posttraumatic stress disorder due to mixed traumatic events: A randomized controlled study. Journal of Traumatic Stress 2010;23(6):744‐50. [DOI] [PubMed] [Google Scholar]
Basoglu 2005 {published data only}
- Basoglu H, Saleioglu E, Livanou M, Kalender D, Acar G. Single‐session behavioral treatment of earthquake‐related posttraumatic stress disorder: A randomised waiting list controlled trial. Journal of Traumatic Stress 2005;18(1):1‐11. [DOI] [PubMed] [Google Scholar]
- Salcioglu E, Basoglu M, Livanou M. Effects of live exposure on symptoms of posttraumatic stress disorder: The role of reduced behavioral avoidance in improvement. Behaviour Research and Therapy 2007;45(10):2268‐79. [DOI] [PubMed] [Google Scholar]
Basoglu 2007 {published data only}
- Basoglu M, Salcioglu E, Livanou M. A randomized controlled study of single‐session behavioural treatment of earthquake‐related post‐traumatic stress disorder using an earthquake simulator. Psychological Medicine 2007;37(2):203‐13. [DOI] [PubMed] [Google Scholar]
Beck 2009 {published data only}
- Beck JG, Coffey SF, Foy DW, Keane TM, Blanchard EB. Group cognitive behavior therapy for chronic posttraumatic stress disorder: an initial randomized pilot study. Behavior Therapy 2009;40(1):82‐92. [DOI] [PubMed] [Google Scholar]
Bichescu 2007 {published data only}
- Bichescu D, Neuner F, Schauer M, Elbert T. Narrative exposure therapy for political imprisonment‐related chronic posttraumatic stress disorder and depression. Behaviour Research and Therapy 2007;45(9):2212‐20. [DOI] [PubMed] [Google Scholar]
Blanchard 2003 {published data only}
- Blanchard EB, Hickling EJ. The Albany treatment study: A randomized, controlled comparison of cognitive‐behavioral therapy and support in the treatment of chronic PTSD secondary to MVAs. After the crash: Psychological assessment and treatment of survivors of motor vehicle accidents. 2nd Edition. Washington, DC: American Psychological Association, 2004:315‐47. [Google Scholar]
- Blanchard EB, Hickling EJ, Devineni T, Veazey CH, Galovski TE, Mundy E, et al. A controlled evaluation of cognitive behavioural therapy for posttraumatic stress in motor vehicle accident survivors. Behaviour Research & Therapy 2003;41(1):79‐96. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Hickling EJ, Malta LS, Freidenberg BM, Canna MA, Kuhn E, et al. One‐ and two‐year prospective follow‐up of cognitive behavior therapy or supportive psychotherapy. Behaviour Research and Therapy 2004;42(7):745‐59. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Hickling EJ, Malta LS, Jaccard J, Devineni T, Veazey CH, et al. Prediction of response to psychological treatment among motor vehicle accident survivors with PTSD. Behavior Therapy 2003;34(3):351‐63. [Google Scholar]
- Blanchard EB, Hickling EJ, Veazey CH, Buckley TC, Freidenberg BM, Walsh JD, et al. Treatment‐related changes in cardiovascular reactivity to trauma cues in motor vehicle accident‐related PTSD. Behavior Therapy 2002;33(3):417‐26. [Google Scholar]
Brom 1989 {published data only}
- Brom D, Kleber RJ, Defares PB. Brief psychotherapy for posttraumatic stress disorders. Journal of Consulting and Clinical Psychology 1989;57(5):607‐12. [DOI] [PubMed] [Google Scholar]
Bryant 2003 {published data only}
- Bryant RA, Moulds ML, Guthrie RM, Dang ST, Nixon RD. Imaginal exposure alone and imaginal exposure with cognitive restructuring in treatment of posttraumatic stress disorder. Journal of Consulting and Clinical Psychology 2003;71(4):706‐12. [DOI] [PubMed] [Google Scholar]
Bryant 2011 {published data only}
- Bryant RA, Ekasawin S, Chakrabhand S, Suwanmitri S, Duangchun O, Chantaluckwong T. A randomised controlled effectiveness trial of cognitive behaviour therapy for post‐traumatic stress disorder in terrorist‐affected people in Thailand. World Psychiatry 2011;10(3):205‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Carlson 1998 {published data only}
- Carlson JG, Chemtob CM, Rusnak K, Hedlund NL, Muraoka MY. Eye movement desensitization and reprocessing (EDMR) treatment for combat‐related posttraumatic stress disorder. Journal of Traumatic Stress 1998;11(1):3‐24. [DOI] [PubMed] [Google Scholar]
Chard 2005 {published data only}
- Chard KM. An evaluation of cognitive processing therapy for the treatment of posttraumatic stress disorder related to childhood sexual abuse. Journal of Consulting and Clinical Psychology 2005;73(5):965‐71. [DOI] [PubMed] [Google Scholar]
Cloitre 2002 {published data only}
- Cloitre M. Emotion regulation and interpersonal skills training for chronic PTSD related to childhood abuse and multiple traumatization. Proceedings of the 157th Annual Meeting of the American Psychiatric Association; 2004 May 1 ‐ 6; New York, NY. 2004:26c.
- Cloitre M. Emotional regulation and interpersonal skill as a prerequisite to emotional processing of traumatic memories. Proccedings of the 156th Annual Meeting of the American Psychiatric Association; 2003 May 17 ‐ 22; San Francisco, CA. 2003:96b.
- Cloitre M. Skills training and exposure: Are both better than one?. Proccedings of the 18th Annual Meeting, International Society for Traumatic Stress Studies; 2002 Nov 7 ‐ 10; Baltimore, MD. 2002.
- Cloitre M, Koenen KC, Cohen LR, Han H. Skills training in affective and interpersonal regulation followed by exposure: a phase‐based treatment for PTSD related to childhood abuse. Journal of Consulting and Clinical Psychology 2002;70(5):1067‐74. [DOI] [PubMed] [Google Scholar]
Cloitre 2010 {published data only}
- Cloitre M, Stovall‐McClough KC, Nooner K, Zorbas P, Cherry S, Jackson CL, et al. Treatment for PTSD related to childhood abuse: a randomised controlled trial. American Journal of Psychiatry 2010;167(8):915‐24. [DOI] [PubMed] [Google Scholar]
Cooper 1989 {published data only}
- Cooper NA, Clum GA. Imaginal flooding as a supplementary treatment for PTSD in combat veterans: a controlled study. Behavior Therapy 1989;20(3):381‐91. [Google Scholar]
Devilly 1998 {published data only}
- Devilly GJ, Spence SH, Rapee RM. Statistical and reliable change with eye movement desensitization and reprocessing: treating trauma within a veteran population. Behavior Therapy 1998;29(3):435‐55. [Google Scholar]
Devilly 1999 {published data only}
- Devilly GJ. The successful treatment of PTSD through overt cognitive behavioral therapy in non‐responders to EMDR. Behavioural and Cognitive Psychotherapy 2001;29(1):57‐70. [Google Scholar]
- Devilly GJ, Spence SH. The relative efficacy and treatment distress of EMDR and a cognitive‐behavior trauma treatment protocol in the amelioration of posttraumatic stress disorder. Journal of Anxiety Disorders 1999;13(1‐2):131‐57. [DOI] [PubMed] [Google Scholar]
Duffy 2007 {published data only}
- Duffy M, Gillespie K, Clark DM. Cognitive therapy for post‐traumatic stress disorder in the context of terrorism and other civil conflict in Northern Ireland. Proceedings of the 34th Annual Conference of the British Association for Behavioural and Cognitive Psychotherapies; 2006 Jul 19 ‐ 21, Warwick. 2006:44.
- Duffy M, Gillespie K, Clark DM. Post‐traumatic stress disorder in the context of terrorism and other civil conflict in Northern Ireland: Randomised Controlled Trial. BMJ 2007;334(7604):1147‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dunne 2012 {published data only}
- Dunne RL, Kenardy J, Sterling M. A randomized controlled trial of cognitive behavioural therapy for the treatment of PTSD in the context of chronic whiplash. Clinical Journal of Pain 2012;28(9):755‐65. [DOI] [PubMed] [Google Scholar]
Echeburua 1997 {published data only}
- Echeburua E, Corral P, Zubizarreta I, Sarasua B. Psychological treatment of chronic posttraumatic stress disorder in victims of sexual aggression. Behavior Modification 1997;21(4):433‐56. [DOI] [PubMed] [Google Scholar]
Ehlers 2003 {published data only}
- Ehlers A, Clark DM, Hackmann A, McManus F, Fennell M, Herbert C, et al. A randomised controlled trial of cognitive therapy, a self help booklet, and repeated assessments as early interventions for posttraumatic stress disorder. Archives of General Psychiatry 2003;60(10):1024‐32. [DOI] [PubMed] [Google Scholar]
Ehlers 2005 {published data only}
- Ehlers A, Clark DM, Hackmann A, McManus F, Fennell M. Cognitive therapy for post‐traumatic stress disorder: development and evaluation. Behaviour Research and Therapy 2005;43(4):413‐31. [DOI] [PubMed] [Google Scholar]
Fecteau 1999 {published data only}
- Fecteau G, Nicki R. Cognitive behavioural treatment of post traumatic stress disorder after motor vehicle accident. Behavioural and Cognitive Psychotherapy 1999;27(3):201‐14. [Google Scholar]
- Fecteau GW. Treatment of posttraumatic stress reactions to traffic accidents [thesis]. Dissertation Abstracts International 2000;61(1‐B):527. [Google Scholar]
Feske 2008 {published data only}
- Feske, U. Treating low income and minority women with post traumatic stress disorder. Journal of Interpersonal Violence 2008;23(8):1027‐40. [DOI] [PubMed] [Google Scholar]
Foa 1991 {published data only}
- Foa EB, Rothbaum BO, Riggs DS, Murdock TB. Treatment of posttraumatic stress disorder in rape victims: a comparison between cognitive‐behavioral procedures and counselling. Journal of Consulting and Clinical Psychology 1991;59(5):715‐23. [DOI] [PubMed] [Google Scholar]
Foa 1999 {published data only}
- Foa EB, Dancu CV, Hembree EA, Jaycox LH, Meadows EA, Street GP. A comparison of exposure therapy, stress inoculation training, and their combination for reducing posttraumatic stress disorder in female assault victims. Journal of Consulting and Clinical Psychology 1999;67(2):194‐200. [DOI] [PubMed] [Google Scholar]
- Zoellner LA, Feeny NC, Fitzgibbons LA, Foa EB. Response of African American and caucasian women to cognitive behavioral therapy for PTSD. Behavior Therapy 1999;30(4):581‐95. [Google Scholar]
Foa 2005 {published data only}
- Foa EB, Hembree EA, Cahill SP, Rauch SAM, Riggs DS. Randomized trial of prolonged exposure for posttraumatic stress disorder with and without cognitive restructuring: Outcome at academic and community clinics. Journal of Consulting and Clinical Psychology 2005;73(5):953‐64. [DOI] [PubMed] [Google Scholar]
Forbes 2012 {published data only}
- Forbes D, Lloyd D, Nixon RD, Elliott P, Varker T, Perry D, et al. A multisite randomized controlled effectiveness trail of cognitive processing therapy for military‐related post traumatic stress disorder. Journal of Anxiety Disorders 2012;26(3):442‐452. [DOI] [PubMed] [Google Scholar]
Galovski 2012 {published data only}
- Galovski T, Blain LM, Mott JM, Elwood L, Houle T. Manualized therapy for PTSD: flexing the structure of cognitive processing therapy. Journal of Consulting and Clinical Psychology 2012;80(6):968‐81. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gamito 2010 {published data only}
- Gamito P, Oliveira J, Rosa P, Morais D, Duarte N, Oliveira S, et al. PTSD elderly war veterans: a clinical controlled pilot study. Cyberpsychology, Behavior and Social Networking 2010;13(1):43‐8. [DOI] [PubMed] [Google Scholar]
Gersons 2000 {published data only}
- Gersons BP, Carlier IV, Lamberts RD, Kolk BA. Randomized clinical trial of brief eclectic psychotherapy for police officers with posttraumatic stress disorder. Journal of Traumatic Stress 2000;13(2):333‐47. [DOI] [PubMed] [Google Scholar]
Hensel‐Dittmann 2011 {published data only}
- Hensel‐Dittmann D, Schauer M, Ruf M, Catani C, Odenwald M, Elbert T, et al. Treatment of traumatized victims of war and torture: A randomized controlled comparison of narrative exposure therapy and stress innoculation therapy. Psychotherapy and Psychosomatics 2011;80(6):345‐52. [DOI] [PubMed] [Google Scholar]
Hinton 2005 {published data only}
- Hinton DE, Chhean D, Pich V, Safren SA, Hofmann SG, Pollack MH. A randomised controlled trial of cognitive behaviour therapy for Cambodian refugees with treatment resistant PTSD and panic attacks: a cross over design. Journal of Traumatic Stress 2005;18(6):617‐29. [DOI] [PubMed] [Google Scholar]
- Hinton DE, Hofmann SG, Pollack MH, Otto MW. Mechanisms of efficacy of CBT for Cambodian refugees with PTSD: improvement in emotion regulation and orthostatic blood pressure response. CNS Neuroscience and Therapeutics 2009;15(3):255‐63. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hinton 2011 {published data only}
- Hinton DE, Hofmann SG, Rivera E, Otto MW, Pollack MH. Culturally adapted CBT (CA‐CBT) for Latino women with treatment‐resistant PTSD: A pilot study comparing CA‐CBT to applied muscle relaxation. Behaviour Research and Therapy 2011;49(4):275‐80. [DOI] [PubMed] [Google Scholar]
Hogberg 2007 {published data only}
- Hogberg G, Pagani M, Sundin O, Soares J, Aberg‐Wistedt A, Tarnell B, et al. On treatment with eye movement desensitization and reprocessing of chronic post‐traumatic stress disorder in public transportation workers ‐ a randomized controlled trial. Nordic Journal of Psychiatry 2007;61(1):54‐60. [DOI] [PubMed] [Google Scholar]
Hollifield 2007 {published data only}
- Hollifield M, Sinclair‐Lian N, Warner TD, Hammerschlag R. Acupuncture for posttraumatic stress disorder. Journal of Nervous and Mental Disease 2010;195(6):504‐13. [DOI] [PubMed] [Google Scholar]
Ironson 2002 {published data only}
- Ironson G, Freund B, Strauss JL, Williams J. Comparison of two treatments for traumatic stress: a community based study of EMDR and prolonged exposure. Journal of Clinical Psychology 2002;58(1):113‐28. [DOI] [PubMed] [Google Scholar]
Jensen 1994 {published data only}
- Jensen JA. An investigation of eye movement desensitisation and reprocessing as a treatment for posttraumatic stress disorder symptoms of Vietnam combat veterans. Behavior Therapy 1994;25(2):311‐25. [Google Scholar]
Keane 1989 {published data only}
- Keane TM, Fairbank JA, Caddell JM, Zimering RT. Implosive (flooding) therapy reduces symptoms of PTSD in Vietnam combat veterans. Behavior Therapy 1989;20(2):245‐60. [Google Scholar]
Kearney 2013 {published data only}
- Kearney DJ, McDermott K, Malte C, Martinez M, Simpson TL. Effects of participation in a mindfulness program for veterans with posttraumatic stress disorder: a randomised controlled trial. Journal of Clinical Psychology 2013;69(1):14‐27. [DOI] [PubMed] [Google Scholar]
Krakow 2000 {published data only}
- Krakow B, Hollifield M, Schrader R, Koss M, Tandberg D, Lauriello J, et al. A controlled study of imagery rehearsal for chronic nightmares in sexual assault survivors with PTSD: A preliminary report. Journal of Traumatic Stress 2000;13(4):589‐609. [DOI] [PubMed] [Google Scholar]
Krakow 2001 {published data only}
- Krakow B, Hollifield M, Johnston L, Koss M, Schrader R, Warner TD, et al. Imagery rehearsal therapy for chronic nightmares in sexual assault survivors with posttraumatic stress disorder. A randomized controlled trial. JAMA 2001;286(5):537‐45. [DOI] [PubMed] [Google Scholar]
Kubany 2003 {published data only}
- Kubany ES, Hill EE, Owens JA. Cognitive trauma therapy for battered women with PTSD: preliminary findings. Journal of Traumatic Stress 2003;16(1):81‐91. [DOI] [PubMed] [Google Scholar]
Kubany 2004 {published data only}
- Kubany ES, Hill EE, Owens JA. Cognitive trauma therapy for battered women with PTSD (CTT‐BW). Journal of Consulting and Clinical Psychology 2004;72(1):3‐18. [DOI] [PubMed] [Google Scholar]
Lee 2002 {published data only}
- Lee C, Gavriel H, Drummond P, Richards J, Greenwald R. Treatment of PTSD: stress inoculation training with prolonged exposure compared to EMDR. Journal of Clinical Psychology 2002;58(9):1071‐89. [DOI] [PubMed] [Google Scholar]
Lindauer 2005 {published data only}
- Lindauer JL, Gersons BPR, Meijel EPM, Blom K, Carlier IVE, Vrijlandt I, et al. Effects of brief eclectic psychotherapy in patients with posttraumatic stress disorder: randomised clinical trial. Journal of Traumatic Stress 2005;18(3):205‐12. [DOI] [PubMed] [Google Scholar]
Marcus 1997 {published data only}
- Marcus S, Marquis P, Sakai C. Three and 6 month follow up of EMDR treatment of PTSD in an HMO setting. International Journal of Stress Management 2004;11(3):195‐208. [Google Scholar]
- Marcus SV, Marquis P, Sakai C. Controlled study of treatment of PTSD using EMDR in an HMO setting. Psychotherapy 1997;34(3):307‐15. [Google Scholar]
Marks 1998 {published data only}
- Marks I, Lovell K, Noshirvani H, Livanou M, Thrasher S. Treatment of posttraumatic stress disorder by exposure and/or cognitive restructuring: a controlled study. Archives of General Psychiatry 1998;55(4):317‐25. [DOI] [PubMed] [Google Scholar]
- Thrasher S, Power M, Morant N, Marks I, Dalgleish T. Social support moderates outcome in a randomized controlled trial of exposure therapy and (or) cognitive restructuring for chronic posttraumatic stress disorder. Canadian Journal of Psychiatry 2010;55(3):187‐90. [DOI] [PubMed] [Google Scholar]
McDonagh 2005 {published data only}
- McDonagh A, Friedman M, McHugo G, Ford J, Sengupta A, Mueser K, et al. Randomized controlled trial of cognitive‐behavioural therapy for chronic posttraumatic stress disorder in adult female survivors of childhood sexual abuse. Journal of Consulting and Clinical Psychology 2005;73(3):515‐24. [DOI] [PubMed] [Google Scholar]
Monson 2006 {published data only}
- Monson CM, Gradus JL, Young‐Xu Y, Schnurr P, Price JL, Schumm JA. Change in posttraumatic stress disorder symptoms: Do clinicians and patients agree?. Psychological Assessment 2008;20(2):131‐8. [DOI] [PubMed] [Google Scholar]
- Monson CM, Schnurr PP, Resick PA, Friedman MJ, Young‐Xu Y, Stevens SP. Cognitive processing therapy for veterans with military related posttraumatic stress disorder. Journal of Consulting and Clinical Psychology 2006;74(5):898‐907. [DOI] [PubMed] [Google Scholar]
Mueser 2008 {published data only}
- Gottlieb JD, Mueser KT, Rosenberg SD, Xie H, Wolfe RS. Psychotic depression, posttraumatic stress disorder, and engagement in cognitive‐behavioral therapy within an outpatient sample of adults with serious mental illness. Comprehensive Psychiatry 2011;52(1):41‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueser K. Cognitive‐behavioural treatment of posttraumatic stress disorder in people with severe mental illness. Proceedings of the 30th Annual Conference of the British Association for Behavioural and Cognitive Psychotherapies; 2002 July 17 ‐ 20; Warwick. 2002.
- Mueser KT, Rosenberg S, Jankowski K, Hamblen J, Carty P. Cognitive‐behavioral treatment of PTSD in clients with severe mental illness. Proceedings of the 157th Annual Meeting of the American Psychiatric Association; 2004 May 1 ‐ 6; New York, NY. 2004:11d.
- Mueser KT, Rosenburg SD, Xie H, Jankowski MK, Bolton EE, Lu W, et al. A randomized controlled trial of cognitive‐behavioral treatment for posttraumatic stress disorder in severe mental illness. Journal of Consulting and Clinical Psychology 2008;76(2):259‐71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Neuner 2004 {published data only}
- Neuner F, Schauer M, Klaschik C, Karunakara U, Elbert T. A comparison of narrative exposure therapy, supportive counselling, and psychoeducation for treating posttraumatic stress disorder in an African refugee settlement. Journal of Consulting and Clinical Psychology 2004;72(4):579‐87. [DOI] [PubMed] [Google Scholar]
- Schauer M, Neuner F, Rockstroh BS, Elber TR. Narrative exposure treatment as intervention for survivors of organized violence in refugee camps. Proceedings of the XII World Congress of Psychiatry; 2002 Aug 24 ‐ 29; Yokohama, Japan. 2002:FC‐56‐3.
Neuner 2008 {published data only}
- Neuner F, Onyut PL, Ertl V, Odenwald M, Schauer E, Elbert T. Treatment of posttraumatic stress disorder by trained lay counselors in an African refugee settlement: A randomised controlled trial. Journal of Consulting and Clinical Psychology 2008;76(4):686‐94. [DOI] [PubMed] [Google Scholar]
Neuner 2010 {published data only}
- Neuner F, Kurreck S, Ruf M, Odenwald M, Elbert T, Schauer M. Can asylum seekers with posttraumatic stress disorder be successfully treated? A randomized controlled pilot study. Cognitive Behaviour Therapy 2010;39(2):81‐91. [DOI] [PubMed] [Google Scholar]
Nijdam 2012 {published data only}
- Nijdam M, Gersons BPR, Reitsma JB, Olff M. Brief eclectic psychotherapy v. eye movement desensitisation and reprocessing for post traumatic stress disorder: randomised controlled trial. British Journal of Psychiatry 2012;200(3):224‐31. [DOI] [PubMed] [Google Scholar]
Paunovic 2011 {published data only}
- Paunovic N. Exposure Inhibition Therapy as a treatment for chronic posttraumatic stress disorder: A controlled pilot study. Psychology 2011;2(6):605‐14. [Google Scholar]
Peniston 1991 {published data only}
- Peniston EG, Kulkosky PJ. Alpha‐theta brainwave neuro‐feedback therapy for Vietnam veterans with combat‐related post‐traumatic stress disorder. Medical Psychotherapy 1991;4:47‐60. [Google Scholar]
Power 2002 {published data only}
- Power K, McGoldrick T, Brown K, Buchanan R, Sharp D, Swanson V, et al. A controlled comparison of eye movement desensitisation and reprocessing versus exposure plus cognitive restructuring versus waiting list in the treatment of post‐traumatic stress disorder. Clinical Psychology and Psychotherapy 2002;9(4):229‐318. [Google Scholar]
Ready 2010 {published data only}
- Ready DJ, Gerardi RJ, Backscheider AG, Mascaro N, Rothbaum BO. Comparing virtual reality exposure therapy to present centred therapy with 11 US Vietnam Veterans with PTSD. Cyberpsychology, Behavior and Social Networking 2010;13(1):49‐54. [DOI] [PubMed] [Google Scholar]
Resick 2002 {published data only}
- Nishith P, Nixon RDV, Resick PA. Resolution of trauma‐related guilt following treatment of PTSD in female rape victims: A result of cognitive processing therapy targeting comorbid depression?. Journal of Affective Disorders 2005;86(2‐3):259‐65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resick PA, Nishith P, Griffin MG. How well does cognitive‐behavioral therapy treat symptoms of complex PTSD? An examination of child sexual abuse survivors within a clinical trial. CNS Spectrums 2003;8(5):340‐55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resick PA, Nishith P, Weaver TL, Astin MC, Feuer CA. A comparison of cognitive‐processing therapy with prolonged exposure and a waiting condition for the treatment of chronic posttraumatic stress disorder in female rape victims. Journal of Consulting and Clinical Psychology 2002;70(4):867‐79. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rothbaum 1997 {published data only}
- Rothbaum BO. A controlled study of eye movement desensitization and reprocessing in the treatment of posttraumatic stress disordered sexual assault victims. Bulletin of the Menninger Clinic 1997;61(3):317‐34. [PubMed] [Google Scholar]
Rothbaum 2005 {published data only}
- Rothbaum BO, Astin MC, Marsteller F. Prolonged exposure versus eye movement desensitisation and reprocessing (EMDR) for PTSD rape victims. Journal of Traumatic Stress 2005;18:607‐616. [DOI] [PubMed] [Google Scholar]
Scheck 1998 {published data only}
- Scheck MM, Schaeffer JA, Gillette C. Brief psychological intervention with traumatized young women: the efficacy of eye movement desensitisation and reprocessing. Journal of Traumatic Stress 1998;11(1):25‐44. [DOI] [PubMed] [Google Scholar]
Schnurr 2003 {published data only}
- Monson CM, Gradus JL, Young‐Xu Y, Schnurr P, Price JL, Schumm JA. Change in posttraumatic stress disorder symptoms: Do clinicians and patients agree?. Psychological Assessment 2008;20(2):131‐8. [DOI] [PubMed] [Google Scholar]
- Schnurr PP, Friedman MJ, Foy DW, Shea MT, Hsieh FY, Lavori PW, et al. Randomized trial of trauma‐focused group therapy for posttraumatic stress disorder. Archives of General Psychiatry 2003;60(5):481‐9. [DOI] [PubMed] [Google Scholar]
Schnurr 2007 {published data only}
- Engel C, Friedman M, Foa E, Shea MT, Schnurr P, Resick P. CSP #494: Primary Findings. Proceedings of the 22nd Annual Meeting, International Society for Traumatic Stress Studies; 2006 November 4 ‐ 7; Hollywood, CA. 2006:58.
- Engel C, Friedman M, Foa E, Shea MT, Schnurr P, Resick P. Design and Rationale for CSP #494. Proceedings of the 22nd Annual Meeting, International Society for Traumatic Stress Studies; 2006 Nov 4 ‐ 7; Hollywood, CA. 2006:58.
- Schnurr PP, Friedman MJ, Engel CC, Foa EB, Shea MT, Chow BK, et al. Cognitive behavioural therapy for posttraumatic stress disorder in women. JAMA 2007;28(8):820‐30. [DOI] [PubMed] [Google Scholar]
- Schnurr PP, Friedman MJ, Engel CC, Foa EB, Shea MT, Resick PM, et al. Issues in the design of multisite clinical trials of psychotherapy: VA Cooperative Study No. 494 as an example. Contemporary Clinical Trials. 2005;26(6):626‐36. [DOI] [PubMed] [Google Scholar]
Taylor 2003 {published data only}
- Taylor S. PTSD treatment outcome predictors: Exposure therapy, EMDR and relaxation. Proceedings of the 19th Annual Meeting, International Society for Traumatic Stress Studies; 2003 Oct 29 ‐ Nov 1; Chicago, IL. 2003.
- Taylor S, Thordarson DS, Maxfield L, Fedoroff IC, Lovell K, Ogrodniczuk J. Comparative efficacy, speed, and adverse effects of three PTSD treatments: exposure therapy, EMDR, and relaxation training. Journal of Consulting and Clinical Psychology 2003;71(2):330‐8. [DOI] [PubMed] [Google Scholar]
Vaughan 1994 {published data only}
- Vaughan K, Armstrong MS, Gold R, O'Connor N, Jenneke W, Tarrier N. A trial of eye movement desensitization compared to image habituation training and applied muscle relaxation in post‐traumatic stress disorder. Journal of Behavior Therapy and Experimental Psychiatry 1994;25(4):283‐91. [DOI] [PubMed] [Google Scholar]
Wells 2012 {published data only}
- Wells A, Colbear JS. Treating posttraumatic stress disorder with metacognitive therapy: A preliminary controlled study. Journal of Clinical Psychology 2012;68:373‐81. [DOI] [PubMed] [Google Scholar]
Zang 2013 {published data only}
- Zang Y, Hunt N, Cox T. A randomised controlled pilot study: the effectiveness of narrative exposure therapy with adult survivors of the Sichuan earthquale. BMC Psychiatry 2013;13:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zlotnick 1997 {published data only}
- Zlotnick C, Shea MT, Pearlstein TB, Rosen KJ, Mulrenin K, Simpson EB. Affect management group for survivors of sexual abuse with PTSD. Proceedings of the 149th Annual Meeting of the American Psychiatric Association; 1996 May 4 ‐ 9; New York, NY. 1996:0292.
- Zlotnick C, Shea TM, Rosen K, Simpson E, Mulrenin K, Begin A, et al. An affect‐management group for women with posttraumatic stress disorder and histories of childhood sexual abuse. Journal of Traumatic Stress 1997;10(3):425‐36. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Abbasnejad 2007 {published data only}
- Abbasnejad M, Mahani KN, Zamyad A. Efficacy of "eye movement desensitization and reprocessing" in reducing anxiety and unpleasant feelings due to earthquake experience. Psychological Research 2007;9(1):104‐117. [Google Scholar]
Arntz 2007 {published data only}
- Arntz A, Tiesema M, Kindt M. Treatment of PTSD: a comparison of imaginal exposure with and without imagery rescripting. Journal of Behavior Therapy and Experimental Psychiatry 2007;38(4):345‐70. [DOI] [PubMed] [Google Scholar]
Barabasz 2013 {published data only}
- Barabasz A, Barabasz M, Christensen C, French B, Watkins JG. Efficacy of single‐session abreactive ego state therapy for combat stress injury, PTSD, and ASD. International Journal of Clinical and Experimental Hypnosis 2013;61(1):1‐19. [DOI] [PubMed] [Google Scholar]
Boudewyns 1990 {published data only}
- Boudewyns PA, Hyer L. Physiological response to combat memories and preliminary treatment outcome in Vietnam veteran PTSD patients treated with direct therapeutic exposure. Behavior Therapy 1990;21(1):63‐87. [Google Scholar]
Chemtob 1997 {published data only}
- Chemtob CM, Novaco RW, Hamada RS, Gross DM. Cognitive‐behavioral treatment for severe anger in posttraumatic stress disorder. Journal of Consulting and Clinical Psychology 1997;65(1):184‐9. [DOI] [PubMed] [Google Scholar]
Classen 2001 {published data only}
- Classen C, Butler LD, Koopman C, Miller E, DiMiceli S, Giese‐Davis J, et al. Supportive‐expressive group therapy and distress in patients with metastatic breast cancer: a randomized clinical intervention trial. Archives of General Psychiatry 2001;58(5):494‐501. [DOI] [PubMed] [Google Scholar]
Classen 2010 {published data only}
- Classen CC, Palesh OG, Cavanaugh CE, Koopman C, Kaupp JW, Kraemer HC, et al. A comparison of trauma‐focused and present focused group therapy for survivors of childhood sexual abuse: a randomised controlled trial. Psychological Trauma: Theory, Research, Practice and Policy 2010;3(1):84‐93. [Google Scholar]
Cole 2007 {published data only}
- Cole KL, Sarlund‐Heinrich P, Brown LS. Developing and assessing effectiveness of a time limited therapy group for incarcerated women survivors of childhood sexual abuse. Journal of Trauma and Dissociation 2007;8(2):97‐121. [DOI] [PubMed] [Google Scholar]
Davis 2007 {published data only}
- Davis JL, Wright DC. Randomized clinical trial for treatment of chronic nightmares in trauma exposed adults. Journal of Traumatic Stress 2007;20(2):123‐33. [DOI] [PubMed] [Google Scholar]
Difede 2007a {published data only}
- Difede J, Malta LS, Best S, Hen‐Haase C, Metzler T, Bryant R, et al. A randomized controlled trial for world trade centre attack related PTSD in disaster workers. Journal of Nervous and Mental Disease 2007;195(10):861‐5. [DOI] [PubMed] [Google Scholar]
DuHamel 2010 {published data only}
- DuHamel KN, Mosher CE, Winkel G, Labay LE, Rini C, Meschian YM, et al. Randomized clinical trial of telephone administered cognitive behavioural therapy to reduce post‐traumatic stress disorder and distress symptoms after hematopoietic stem‐cell transplantation. Journal of Clinical Oncology 2010;28(23):3754‐61. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dunn 2007 {published data only}
- Dunn NJ, Rehm LP, Schillaci J, Souchek J, Mehta P, Ashton CM, et al. A randomized controlled trial of self‐management and psychoeducational group therapies for comorbid chronic posttraumatic stress disorder and depressive disorder. Journal of Traumatic Stress 2007;20(3):221‐37. [DOI] [PubMed] [Google Scholar]
Echeburua 1996 {published data only}
- Echeburua E, Corral P, Sarasua B, Zubizarreta I. Treatment of acute posttraumatic stress disorder in rape victims: an experimental study. Journal of Anxiety Disorders 1996;10(3):185‐99. [Google Scholar]
Edmond 1999 {published data only}
- Edmond T, Rubin A. Assessing the long‐term effects of EMDR: Results from an 18 month follow‐up study with adult female survivors of CSA. Journal of Child Sexual Abuse 2004;13(1):69‐86. [DOI] [PubMed] [Google Scholar]
- Edmond T, Rubin A, Wambach KG. The effectiveness of EMDR with adult female survivors of childhood sexual abuse. Social Work Research 1999;23:103‐16. [Google Scholar]
Falsetti 2001 {published data only}
- Falsetti SA, Resnick HS, Davis J. Multiple channel exposure therapy ‐ combining cognitive‐behavioral therapies for the treatment of posttraumatic stress disorder with panic attacks. Behavior Modification 2005;29(1):70‐94. [DOI] [PubMed] [Google Scholar]
- Falsetti SA, Resnick HS, Davis J, Gallagher NG. Treatment of posttraumatic stress disorder with comorbid panic attacks: combining cognitive processing therapy with panic control treatment techniques. Group Dynamics: Theory, Research and Practice 2001;5(4):252‐60. [Google Scholar]
- Falsetti SA, Erwin BA, Resnick HS, Davis J, Combs‐Lane AM. Multiple channel exposure therapy of PTSD: Impact of treatment on functioning and resources. Journal of Cognitive Psychotherapy 2003;17(2):133‐47. [Google Scholar]
Falsetti 2005 {published data only}
- Falsetti S.A, Resnick H.S, Davis J. Multiple channel exposure therapy. Behavior Modification 2005;29(1):70‐94. [DOI] [PubMed] [Google Scholar]
Foa 2006 {published data only}
- Foa EB, Zoellner LA, Feeny NC. An evaluation of three brief programmes for facilitating recovery after assault. Journal of Traumatic Stress 2006;19(1):29‐43. [DOI] [PubMed] [Google Scholar]
Frommberger 2004 {published data only}
- Frommberger U, Nyberg E, Richter H, Stieglitz R‐D, Berger M. Paroxetine vs. cognitive‐behavioral therapy in the treatment of depression in PTSD patients. Proceedings of the 21st Collegium Internationale Neuro psychopharmacologicum; 1998 Jul 12 ‐ 16; Glasgow, Scotland. 1998:PM02013.
- Frommberger U, Stieglitz R, Nyberg E, Richter H, Novelli‐Fischer U, Angenendt J, et al. Comparison between paroxetine and behaviour therapy in patients with posttraumatic stress disorder (PTSD): a pilot study. International Journal of Psychiatry in Clinical Practice 2004;8(1):19‐23. [DOI] [PubMed] [Google Scholar]
Gidron 1996 {published data only}
- Gidron Y, Peri T, Connolly JF, Shalev AY. Written disclosure in posttraumatic stress disorder: is it beneficial for the patient?. Journal of Nervous and Mental Disease 1996;184(8):505‐7. [DOI] [PubMed] [Google Scholar]
Ginzberg 2009 {published data only}
- Ginzburg K, Butler LD, Giese‐Davis J, Cavanaugh CE, Neri E, Koopman C, et al. Shame, guilt, and posttraumatic stress disorder in adult survivors of childhood sexual abuse at risk for human immunodeficiency virus: outcomes of a randomized clinical trial of group psychotherapy treatment. Journal od Nervous and Mental Disorders 2009;197(7):536‐42. [DOI] [PubMed] [Google Scholar]
Glynn 1999 {published data only}
- Glynn SM, Eth S, Randolph ET, Foy DW, Urbaitis M, Boxer L, et al. A test of behavioral family therapy to augment exposure for combat‐related posttraumatic stress disorder. Journal of Consulting and Clinical Psychology 1999;67(2):243‐51. [DOI] [PubMed] [Google Scholar]
Hiari 2005 {published data only}
- Hiari M, Clum GA. An internet based self‐change programme for traumatic event related fear, distress and maladaptive coping. Journal of Traumatic Stress 2005;18(6):631‐6. [DOI] [PubMed] [Google Scholar]
Jaberghaderi 2004 {published data only}
- Jaberghaderi N, Greenwald R, Rubin A, Dalatabadi S, Zand SO. A comparison of CBT and EMDR for sexually‐abused Iranian girls. Proceedings of the 18th Annual Meeting, International Society for Traumatic Stress Studies. Baltimore, MD, Nov 7 ‐ 12, 2002.
- Jaberghaderi N, Greenwald R, Rubin A, Zand SO, Dolatabadi S. A comparison of CBT and EMDR for sexually‐abused Iranian girls. Clinical Psychology and Psychotherapy 2004;11(5):358‐68. [Google Scholar]
Knaevelsrud 2007 {published data only}
- Knaevelsrud C, Maercker A. Internet‐based treatment for PTSD reduces distress and facilitates the development of a strong therapeutic alliance. BMC Psychiatry 2007;7:142‐147. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lange 2001 {published data only}
- Lange A, Ven JP, Schrieken B, Emmelkamp PMG. Interapy: Treatment of posttraumatic stress through the internet: A controlled trial. Journal of Behaviour Therapy and Experimental Psychiatry 2001;55(6):603‐11. [DOI] [PubMed] [Google Scholar]
Lange 2003 {published data only}
- Lange A, Rietdijk D, Hudcovicova M, Ven JP, Schrieken B, Emmelkamp PM. Interapy: a controlled randomised trial of standardised treatment of post‐traumatic stress through the internet. Journal of Consulting and Clinical Psychology 2003;71(5):901‐9. [DOI] [PubMed] [Google Scholar]
Litz 2007 {published data only}
- Litz BT, Engel CC, Bryant RA, Papa A. A randomized, controlled proof‐of‐concept trial of an internet‐based, therapist‐assisted self‐management treatment for posttraumatic stress disorder. American Journal of Psychiatry 2007;164(11):1676‐83. [DOI] [PubMed] [Google Scholar]
Maercker 2006 {published data only}
- Maercker A, Zollner T, Menning H, Rabe S, Karl A. Dresden PTSD treatment study: randomized controlled trial of motor vehicle accident survivors. BMC Psychiatry 2006;29(6):1‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mithoefer 2011 {published data only}
- Mithoefer MC, Wagner MT, Mithoefer T, Jerome L, Doblin R. The safety and efficacy of {+/‐}3,4‐methylenedioxymethamphetamine‐ assisted psychotherapy in subjects with chronic, treatment‐resistant posttraumatic stress disorder: the first randomized controlled pilot study. Journal of Psychopharmacology 2011;25(4):439‐52. [DOI] [PMC free article] [PubMed] [Google Scholar]
Najavits 2006 {published data only}
- Najavits LM, Gallop RJ, Weiss RD. Seeking safety: Therapy for adolescent girls with PTSD and substance use disorder: A randomised controlled trial. Journal of Behavioural Health Services and Research 2006;33(4):453‐63. [DOI] [PubMed] [Google Scholar]
Paunovic 2001 {published data only}
- Paunovic N, Ost LG. Cognitive‐behavior therapy versus exposure therapy in the treatment of PTSD in refugees. Behaviour Research and Therapy 2001;39(10):1183‐97. [DOI] [PubMed] [Google Scholar]
Price 2007 {published data only}
- Price CJ, McBride B, Hyerle L, Kivlahan DR. Mindful awareness in body‐oriented therapy for female veterans with post‐traumatic stress disorder taking prescription analgesics for chronic pain: A feasibility study. Alternative Therapies 2007;13(6):32‐40. [PMC free article] [PubMed] [Google Scholar]
Rabe 2008 {published data only}
- Rabe S, Zoellner T, Beauducel A, Maercker A, Karl A. Changes in brain electrical activity after cognitive behavioural therapy for posttraumatic stress disorder in patients injured in motor vehicle accidents. Psychosomatic Medicine 2008;70(1):13‐9. [DOI] [PubMed] [Google Scholar]
Rothbaum 2006 {published data only}
- Rothbaum BO, Cahill SP, Foa EB, Davidson JR, Compton J, Connor KM, et al. Augmentation of sertraline with prolonged exposure in the treatment of posttraumatic stress disorder. Journal of Traumatic Stress 2006;19(5):625‐38. [DOI] [PubMed] [Google Scholar]
Ryan 2005 {published data only}
- Ryan M, Nitsun M, Gilbert L, Mason H. A prospective study of the effectiveness of group and individual psychotherapy for women CSA survivors. Psychology and Psychotherapy: Theory, Research and Practice 2005;78(Pt 4):465‐79. [DOI] [PubMed] [Google Scholar]
Schaal 2009 {published data only}
- Schaal S, Elbert T, Neuner F. Narrative exposure therapy versus interpersonal psychotherapy. A pilot randomized controlled trial with Rwandan genocide orphans. Psychotherapy and Psychosomatics 2009;78(5):298‐306. [DOI] [PubMed] [Google Scholar]
Shapiro 1989a {published data only}
- Shapiro F. Efficacy of eye movement desensitization procedure in the treatment of traumatic memories. Journal of Traumatic Stress 1989;2(2):199‐223. [Google Scholar]
Sloan 2004 {published data only}
- Sloan DM, Marx BP. A closer examination of the structured written disclosure paradigm. Journal of Consulting and Clinical Psychology 2004;72(2):165‐75. [DOI] [PubMed] [Google Scholar]
Sloan 2005 {published data only}
- Sloan DM, Marx, BP, Epstein EM. Further examination of the exposure model underlying the efficacy of written emotional disclosure. Journal of Consulting and Clinical Psychology 2005;73(3):549‐54. [DOI] [PubMed] [Google Scholar]
Spence 2011 {published data only}
- Spence J, Titov N, Dear BF, Johnston L, Solley K, Lorian C, et al. Randomised controlled trial of internet delivered cognitive behavioural therapy for posttraumatic stress disorder. Depression and Anxiety 2011;28(7):541‐50. [DOI] [PubMed] [Google Scholar]
Tarrier 1999 {published data only}
- Tarrier N, Pilgrim H, Sommerfield C. A randomised trial of cognitive therapy and imaginal exposure in the treatment of chronic posttraumatic stress disorder. Journal of Consulting and Clinical Psychology 1999;67(1):13‐8. [DOI] [PubMed] [Google Scholar]
Tucker 2007 {published data only}
- Tucker P, Trautman RP, Wyatt DB, Thompson J, Wu SC, Capece JA, et al. Efficacy and safety of topiramate monotherapy in civilian posttraumatic stress disorder: a randomized, double‐blind, placebo‐controlled study. Journal of Clinical Psychiatry 2007;68(2):201‐6. [DOI] [PubMed] [Google Scholar]
Van Emmerik 2008 {published data only}
- Emmerik AAP, Kamphuis JH, Emmelkamp PMG. Treating acute stress disorder and posttraumatic stress disorder with cognitive behavioural therapy. Psychotherapy and Psychosomatics 2008;77(2):93‐100. [DOI] [PubMed] [Google Scholar]
Watson 1997 {published data only}
- Watson CG, Tuorila JR, Vickers KS, Gearhart LP, Mendez CM. The efficacies of three relaxation regimens in the treatment of PTSD in Vietnam war veterans. Journal of Clinical Psyhcology 1997;53(8):917‐23. [DOI] [PubMed] [Google Scholar]
Wilson 1995 {published data only}
- Wilson SA, Becker LA, Tinker RH. Eye movement desensitisation and reprocessing treatment for psychologically traumatised individuals. Journal of Consulting and Clinical Psychology 1995;63(6):928‐37. [DOI] [PubMed] [Google Scholar]
Yeomans 2010 {published data only}
- Yeomans PD, Forman EM, Herbert JD, Yuen E. A randomized trial of a reconciliation workshop with and without PTSD psychoeducation in Burundian sample. Journal of Traumatic Stress 2010;23(3):305‐12. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Krupnick 2008 {published data only}
- Krupnick JL, Green BL, Stockton P, Miranda J, Krause E, Mete M. Group interpersonal psychotherapy for low‐income women with posttraumatic stress disorder. Psychotherapy Research 2008;18(5):497‐507. [DOI] [PubMed] [Google Scholar]
Additional references
ACPMH 2007
- Australian Centre for Posttraumatic Mental Health. Australian Guidelines for the Treatment of Adults with Acute Stress Disorder and Posttraumatic Stress Disorder. Melbourne: Australian Centre for Posttraumatic Mental Health, 2007. [Google Scholar]
APA 1980
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM‐III) 3rd edition. Washington DC: American Psychiatric Association, 1980. [Google Scholar]
APA 1987
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3rd Edition. Washington DC, 1987. [Google Scholar]
APA 2000
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th Edition. Washington DC, 2000. [Google Scholar]
Beck 1961
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry 1961;4:561‐71. [DOI] [PubMed] [Google Scholar]
Bisson 2007a
- Bisson JI. Post‐traumatic stress disorder. British Medical Journal 2007;334:789‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bisson 2007b
- Bisson JI, Ehlers A, Matthews R, Pilling S, Richards D, Turner S. Psychological treatments for chronic post‐traumatic stress disorder: Systematic review and meta‐analysis. British Journal of Psychiatry 2007;190(2):97‐104. [DOI] [PubMed] [Google Scholar]
Blake 1995
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, et al. The development of a clinician administered PTSD scale. Journal of Traumatic Stress 1995;8(1):75‐90. [DOI] [PubMed] [Google Scholar]
Bradley 2005
- Bradley R, Green J, Russ E, Dutra L, Westen D. A multidimensional meta‐analysis of psychotherapy for PTSD. American Journal of Psychiatry 2005;162(2):214‐27. [DOI] [PubMed] [Google Scholar]
Brewin 2003
- Brewin CR, Holmes EA. Psychological theories of posttraumatic stress disorder. Clinical Psychology Review 2003;23(3):339‐76. [DOI] [PubMed] [Google Scholar]
Creamer 2004
- Creamer M, Forbes D, Phelps A, Humphreys L. .. Treating Traumatic Stress: Conducting Imaginal Exposure. Australian Centre for Posttraumatic Mental Health, 2004. [Google Scholar]
Foa 2000
- Foa EB, Keane T, Friedman M. Effective Treatments for PTSD: Practice Guidelines from the International Society for Traumatic Stress Studies. New York, NY: Guildford Press, 2000. [Google Scholar]
Foa 2009
- Foa, EB, Keane TM, Friedman MJ. Effective Treatments for PTSD: Practice Guidelines from the International Society for Traumatic Stress Studies. New York: Guilford Press, 2009. [Google Scholar]
Gillies 2012
- Gillies D, Taylor F, Gray C, O'Brien L, D'Abrew N. Psychological therapies for the treatment of post‐traumatic stress disorder in children and adolescents. Cochrane Database of Systematic Reviews 2012, Issue 12. [DOI: 10.1002/14651858.CD006726.pub2] [DOI] [PubMed] [Google Scholar]
Hetrick 2010
- Hetrick SE, Purcell R, Garner B, Parslow R. Combined pharmacotherapy and psychological therapies for post traumatic stress disorder (PTSD). Cochrane Database of Systematic Reviews 2010, Issue 7. [DOI: 10.1002/14651858.CD007316.pub2] [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327(7414):557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Horowitz 1979
- Horowitz MJ, Wilner N, Alvarez W. Impact of Event Scale: a measure of subjective stress. Psychosomatic Medicine 1979;41(3):209‐18. [DOI] [PubMed] [Google Scholar]
Kessler 1995
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry 1995;52(12):1048‐60. [DOI] [PubMed] [Google Scholar]
Meichenbaum 1988
- Meichenbaum D, Deffenbacher JL. Stress inoculation training. Counseling Psychologist 1988;16:69‐90. [Google Scholar]
NICE 2005
- National Collaborating Centre for Mental Health (NCCMH). Post‐traumatic Stress Disorder (PTSD): The Management of PTSD in Adults and Children in Primary and Secondary Care (CG26). London: Gaskell and the British Psychological Society, 2005. [Google Scholar]
Pitman 1991
- Pitman RK, Altman B, Greenwald E, Longpre RE, Macklin ML, Poire RE, et al. Psychiatric complications during flooding therapy for post‐traumatic stress disorder. Journal of Clinical Psychiatry 1991;52(1):17‐20. [PubMed] [Google Scholar]
Resick 1992
- Resick PA, Schnicke MK. Cognitive processing therapy for sexual assault victims. Journal of Consulting and Clinical Psychology 1992;60(5):748‐56. [DOI] [PubMed] [Google Scholar]
RevMan 5 [Computer program]
- The Nordic Cochrane Centre. Review Manager (RevMan). Version 5.2. Copenhagen: The Nordic Cochrane Centre, 2012.
Roberts 2009
- Roberts NP, Kitchiner NJ, Kenardy J, Bisson JI. Multiple session early psychological interventions for the prevention of post‐traumatic stress disorder. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD006869.pub2] [DOI] [PubMed] [Google Scholar]
Roberts 2010
- Roberts NP, Kitchiner NJ, Kenardy J, Bisson JI. Early psychological interventions to treat acute traumatic stress symptoms. Cochrane Database of Systematic Reviews 2010, Issue 3. [DOI: 10.1002/14651858.CD007944.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rogers 1961
- Rogers C. On Becoming a Person: A Therapist's View of Psychotherapy. London: Constable, 1961. [Google Scholar]
Rose 2002
- Rose S, Bisson J, Wessely S. Psychological debriefing for preventing post traumatic stress disorder (PTSD). Cochrane Database of Systematic Reviews 2002, Issue 2. [DOI: 10.1002/14651858.CD000560] [DOI] [PubMed] [Google Scholar]
Shapiro 1989b
- Shapiro F. Eye movement desensitisation: a new treatment for post‐traumatic stress disorder. Journal of Behavior Therapy and Experimental Psychiatry 1989;20:211‐7. [DOI] [PubMed] [Google Scholar]
Spielberger 1973
- Spielberger CD, Gorsuch RL, Lushene R. Manual for the State‐Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologist Press, 1973. [Google Scholar]
Stein 2006
- Stein DJ, Ipser JC, Seedat, S. Pharmacotherapy for post traumatic stress disorder (PTSD). Cochrane Database of Systematic Reviews 2006, Issue 1. [DOI: 10.1002/14651858.CD002795.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Van Etten 1988
- Etten ML, Taylor S. Comparative efficacy of treatments for post‐traumatic stress disorder: a meta‐analysis. Clinical Psychology and Psychotherapy 1988;5:126‐45. [Google Scholar]
WHO 1979
- World Health Organization. ICD‐ 9 Clinical Descriptions and Diagnostic Guidelines. Geneva: World Health Organization, 1992. [Google Scholar]
WHO 1992
- World Health Organization. ICD‐10 Classifications of Mental and Behavioural Disorder: Clinical Descriptions and Diagnostic Guidelines. Geneva: World Health Organization, 1992. [Google Scholar]
References to other published versions of this review
Bisson 2005
- Bisson J, Andrew M. Psychological treatment of post‐traumatic stress disorder (PTSD). Cochrane Database of Systematic Reviews 2005, Issue 2. [DOI: 10.1002/14651858.CD003388.pub3] [DOI] [PubMed] [Google Scholar]
Bisson 2007
- Bisson J, Andrew M. Psychological treatment of post‐traumatic stress disorder (PTSD). Cochrane Database of Systematic Reviews 2007, Issue 3. [DOI: 10.1002/14651858.CD003388.pub3] [DOI] [PubMed] [Google Scholar]


