Abstract
Deficits in attention, communication, imitation, and play skills reduce opportunities for children with autism to learn from natural interactive experiences that occur throughout the day. These developmental delays are already present by the time these children reach the toddler period. The current study provided a brief 12 week, 1 hour per week, individualized parent–child education program to eight toddlers newly diagnosed with autism. Parents learned to implement naturalistic therapeutic techniques from the Early Start Denver Model, which fuses developmental- and relationship-based approaches with Applied Behavior Analysis into their ongoing family routines and parent–child play activities. Results demonstrated that parents acquired the strategies by the fifth to sixth hour and children demonstrated sustained change and growth in social communication behaviors. Findings are discussed in relation to providing parents with the necessary tools to engage, communicate with, and teach their young children with autism beginning immediately after the diagnosis.
Keywords: autism, Early Start Denver Model, parent education, therapy
Autism is a neurodevelopmental disorder that involves global impairments in social skills and in verbal and non-verbal communication, as well as the presence of stereotyped patterns of behaviors and interests. Epidemiological reports indicate that the number of children diagnosed with autism and autism spectrum disorders (ASDs) is rising (Burton, 2002; Fombonne, 1998; 2003; Gillberg, Steffenburg and Schaumann, 1991; Yeargin-Allsopp et al., 2003). This higher prevalence may be partially due to better detection and assessment procedures and expanded classification criteria.
In the past, children typically received diagnoses around the age of 4 years, shortly before entering school. However, there is now a great deal of knowledge about how to identify toddlers with autism by age 2 (as reviewed by Rogers, 2000). With the rise in the number of children being diagnosed, coupled with the push toward earlier detection, developing interventions that are appropriate to these infants and toddlers that can begin immediately after diagnosis and that can support the needs of parents at a very difficult time in their lives is a strong national priority (National Research Council, 2001).
Many early intervention providers are responding to this challenge by initiating intensive services with varied approaches. However, to date, there are only a few published interventions with demonstrated effectiveness specifically targeted for children under the age of 3 years, some of which are case reports (Green, Brennan and Gein, 2002; Mahoney and Perales, 2005; Mahoney et al., 1998; McGee, Morrier and Daly, 1999). While public law mandates intervention for children with disabilities younger than 3 years, many of the services delivered by professionals average 2 to 3 hours per week (Scarborough et al., 2004), which is far below the intensity level recommended by the National Research Council. Such programs may lack a well-defined and comprehensive set of teaching plans for building functional skills appropriate to the child’s current developmental level. Thus, there is currently a need for validated, empirically based interventions for children with autism in the 0–2 age range.
One way of expanding the quality and availability of services for children with autism has been imparting skills to parents. The inclusion of parents as treatment providers for their own children is now considered an essential component of autism intervention (National Research Council, 2001). Parent education has been shown using single-subject design to benefit children with autism by increasing children’s non-verbal (Anderson and Romanczyk, 1999; Krantz, Koegel, Harrower and Carter, 1993) and verbal communication skills (Charlop and Trasowech, 1991; L.K. Koegel, MacDuff and McClannahan, 1999a; Laski, Charlop and Schreibman, 1988; McGee et al., 1999; Stahmer and Gist, 2001), reducing inappropriate behavior (R.L. Koegel, Koegel and Surrat, 1992; Lutzker and Steed, 1998; Lutzker, Huynen and Bigelow, 1998), increasing appropriate play skills (Stahmer, 1995; Stahmer and Schreibman, 1992), and improving the parent–child relationship (R.L. Koegel, Bimbela and Schreibman, 1996; Mahoney and Perales, 2003). Teaching parents to provide the intervention has also been shown to increase generalization and maintenance of treatment gains over time (R.L. Koegel et al., 1982). In addition, parents who serve as direct treatment providers in their children’s intervention often report reduced feelings of depression and stress and increased feelings of empowerment (Brookman-Frazee, 2004; Ozonoff and Cathcart, 1998) and optimism about their own ability to influence their child’s development (R.L. Koegel et al., 1982; Moes et al., 1992).
Although parent education programs can be effective in teaching parents to change child behaviors, limitations exist with these strategies. Several of the published interventions require an extensive amount of time for parents to learn the intervention techniques, such as the 25 hours necessary to sufficiently learn Pivotal Response Training (PRT: R.L. Koegel et al., 1996). Consequently, enrolled parents may be faced with taking substantial time off work or removing their child from other programs. Further obstacles may involve limited access to validated interventions, as there may be long waiting lists. These programs may be quite expensive for families and are often not covered by insurance or public school systems. A final limitation is the quasi-experimental designs used in these studies, many with three or fewer subjects.
An additional consideration involved in working with toddlers with autism is the impact of a recent diagnosis in the family. This period immediately following diagnosis can be extremely difficult for parents, given that they are very motivated to help their children and yet may be forced to wait a considerable amount of time to move through the diagnostic and treatment referral process. A main goal of this study was to design an intervention that could be implemented over a short period by a diagnostic team immediately following first identification, as occurs with medical diagnosis. Providing parents with concrete strategies that will help their child supports parents as agents of growth and change in autism and provides them with evidence of their child’s capacity to learn at a critical time in family life. In addition, providing information early and effectively has been reported as the most valued assistance parents can receive from professionals (Baxter, 1986).
Recent studies have demonstrated parent mastery of teaching techniques and improvement in children’s language skills as a result of a brief parent delivered program. For example, Stahmer and Gist (2001) examined a PRT parent education program conducted in a community setting. The authors found that a majority of parents were able to learn the techniques after a 12 week accelerated program and most children (between 19 and 48 months of age) improved their language and play skills and showed reduction of difficult behavior. However, child gains were primarily gathered from parent and anecdotal reports.
Another study conducted by Rogers et al. (2006) randomized 10 non-verbal children with autism, ages 20–65 months, into two different models for developing speech, the Denver Model (Rogers et al., 2000) and PROMPT (Prompts for Restructuring Oral Muscular Phonetic Targets: Chumpelik, 1984). Both groups received 12 weekly sessions of 1 hour of therapy and daily home intervention delivered by parents. Eight of the 10 children developed vocabularies of at least multiple single words used spontaneously and routinely throughout the course of intervention. Given that the children received only 12 hours of direct intervention, the authors noted that parent involvement likely played a significant role in promoting language growth. However, the study lacked description on specific parent teaching strategies and measures of parent implementation
An additional study by Baker-Ericzén, Stahmer and Burns (2007) examined whether specific child variables would improve as a result of a 12 week community-based PRT parent education program. One hundred and fifty-eight families with children having an autism spectrum diagnosis participated. The children, regardless of gender, age, or ethnicity, showed improvements in communication and adaptive functioning. Despite the study’s strengths (i.e. parent inclusion in the intervention program, a large-scale investigation of a community-based program), child gains were examined via parent report (i.e. Vineland Adaptive Behavior Scales: Sparrow, Balla and Cicchetti, 2005) with the possibility that parents could be biased reporters of their child’s functioning. In addition, the study did not assess parents’ mastery of the PRT techniques; thus whether the parents applied the procedures correctly is unknown.
The purpose of the current study was to pilot a brief, time-limited manualized intervention for parent education using the Early Start Denver Model (ESDM: Rogers, Tismara and Colombi, in preparation). The unpublished manualized intervention was designed as a follow-up to diagnosis that would support parents and stimulate child progress as families wait for more intensive services to begin. Parents of recently diagnosed children with autism 10–36 months of age voluntarily enrolled in a research funded parent intervention program of 12 weekly sessions of 1 hour. These parents learned to deliver the teaching procedures for the ESDM, a model that fuses development, relationship, and behavioral methods specifically developed for use with infants and toddlers. This model focuses on supporting all areas of development, with play and natural family routines as the activities for learning. The primary goals of the study were to assess (a) the parents’ acquisition of the ESDM teaching procedures, and (b) changes in the child’s social communicative behaviors as a result of the brief parent education program.
Method
Participants
The first eight consecutive families who enrolled in the intervention were included in the current study. Two of the eight families terminated the intervention before completing the program. One family terminated after 8 weeks in the program because the mother became ill and could not attend the 1 hour clinic session each week. The second family terminated the intervention after 10 weeks because an intensive in-home intervention was scheduled to begin. All eight families’ results are presented in the current study (see Table 1 for participant characteristics).
Table 1.
Participant characteristics at pre-intervention
| Child | CAa | Ethnicity | VMAb | Autism severityc | Baseline length | Primary caregiver’s socioeconomic status | |
|---|---|---|---|---|---|---|---|
| Receptive | Expressive | ||||||
| Child 1 | 2:2 | Caucasian | 0:10 | 0:1 1 | 14 | 2 probes | Single; high school degree, some college; full-time employment |
| Child 2 | 2:7 | Caucasian | 0:9 | 0:14 | 19 | 2 probes | Married; college degree; full-time employment |
| Child 3 | 2:2 | Latino | 0:1 1 | 0:13 | 18 | 3 probes | Separated; high school degree; part-time employment |
| Child 4d | 2:3 | Caucasian | 0:8 | 0:9 | 17 | 4 probes | Separated; high school degree; full-time employment |
| Child 5d | 2:1 1 | Latino | 0:9 | 0:10 | 22 | 4 probes | Married; high school degree; no employment |
| Child 6 | 0:10 | Caucasian | 0:6 | 0:6 | n.a. | 2 probes | Married; college degree; full-time employment |
| Child 7 | 3:0 | Caucasian | 1:1 | 1:0 | 17 | 4 probes | Married; master’s degree; no employment |
| Child 8 | 2:5 | Caucasian | 1:2 | 1:5 | 22 | 2 probes | Married; college degree;full-time employment |
Chronological age.
Verbal mental age in years:months from Mullen Scales of Early Learning.
Cutoff scores on the ADOS, module I: autism = 12; autism spectrum disorder = 7.
Children that terminated program.
Selection criteria included the following: (a) children no older than 36 months of age; (b) no significant health concerns (e.g. lack of functional hand use, lack of ambulation via crawling or walking); (c) no serious or specific medical, genetic, neurological or sensory condition (e.g. fragile X, Down syndrome, cerebral palsy); (d) parental consent for weekly videotaping; (e) parental attendance of 12 concurrent weeks of treatment with four follow-up visits (adjusting for family vacations, child illnesses, etc.); and (f) no participation in intensive treatment during the 12 weeks of treatment. The children with autism were recruited for the study from referrals from other research and clinical facilities in the Sacramento area on a first come, first served basis. All the children were also receiving approximately 1 hour each of speech and occupational therapy and were participating in 30 minutes of playgroup activities on a weekly basis.
Seven out of the eight children received a diagnosis of autistic disorder by an independent physician or psychologist using the DSM–IV criteria (American Psychiatric Association, 2000) and exceeding the autism cutoff on the Autism Diagnostic Observation Schedule (ADOS: Lord, Rutter, DiLavore and Risi, 1999). The children’s diagnoses were reconfirmed at the start of the program by a clinician affiliated with our center (but not the child’s therapist) who administered the ADOS module 1 (Lord et al., 1999) and was supervised by the third author, a certified expert. Child 6 was not diagnosed with autism until age 18 months, at the conclusion of his enrollment. He was enrolled at 12 months of age due to symptoms consistent with ASD, and repeated clinical evaluations over the 12–18 month age period from several different diagnostic groups consistently documented this clinical picture across the treatment period. He was enrolled specifically to examine the effectiveness of the model with young infants.
Settings
Sessions took place in a large clinic playroom. The playrooms contained a large table and adult-sized chairs, a child-sized table and chairs, a couch, and an assortment of toys. Three video cameras were located in the playroom, two of which were mounted on opposite walls and one was behind a two-way mirror. At least one parent, child, and therapist were present during each session.
Experimental design and procedures
Parents were taught to implement strategies from the Early Start Denver Model (ESDM). The ESDM incorporates techniques from two existing methods that have received empirical support for improving skill acquisition in very young children with autism (e.g. Green et al., 2002; McGee et al., 1999). The first method, the Denver Model, was originally developed by Rogers and colleagues (Rogers and Lewis, 1989; Rogers et al., 1986; 2000) and encourages development in a variety of areas known to be affected in autism, following sequences of development seen in children without developmental delays. The Denver Model focuses on creating an affectively warm and rich environment to foster positive relationships between children and adults and approaches language development from a communication science orientation, emphasizing the social function of language (pragmatics) and the development of non-verbal communication and imitation as foundations for verbal language.
The second model, Pivotal Response Training (PRT), is based on the principles of Applied Behavior Analysis. PRT incorporates specific variables associated with motivation within a systematic teaching approach to increase communication, language, and play skills under natural conditions that more closely resemble the way typically developing children acquire developmentally appropriate skills (L.K. Koegel et al., 1999a; 1999b). The motivational variables are delivered in 1:1 interactions consisting of: (a) turn taking; (b) incorporating children’s interests and preferences within learning opportunities; (c) varying the task sequencing and interspersing previously mastered tasks with new acquisition tasks; (d) rewarding children for attempting new skills as well as performing them successfully; and (e) incorporating natural rewards that are directly and inherently related to the child’s response.
A detailed parent manual was developed to highlight 10 therapy strategies (Rogers et al., in preparation) that are essential to the ESDM: (a) increasing the child’s attention and motivation; (b) sensory social routines; (c) dyadic engagement; (d) non-verbal communication; (e) imitation; (f) joint attention; (g) speech development; (h) antecedent–behavior–consequence relationship (ABCs of learning); (i) prompting, shaping, and fading techniques; and (j) functional assessment of behavior. Each strategy was the focus of one session in which the parent was taught to deliver the lesson in the context of a shared activity using age appropriate play materials and aimed at targeting a variety of developmental objectives (e.g. receptive communication, fine motor skills, gestural imitation).
A non-concurrent multiple-baseline design (Watson and Workman, 1981) was used to evaluate the efficacy of the intervention. This type of design has the advantage of controlling for developmental maturation and exposure to the treatment setting, and allows for measurement of several concurrent behaviors. In addition, this design is advantageous for looking at individual differences in the effectiveness of an intervention, and highlights the practical significance versus statistical significance. As part of the design, baselines ranged from two to four probes across the participants. For each participant, data were gathered in two 10 minute videos each week of a play activity, one between the child and caregiver and one between the child and therapist during two assessments, 10 intervention sessions, and four follow-up visits (spaced across a 3 month period).
Parent education procedures were as follows.
Assessment
The first two sessions of the 12-week parent education program were used for assessments. In these, we conducted a parent interview concerning short-term goals for their child and an evaluation of the child’s current functioning levels based on the Mullen Scales of Early Learning (Mullen, 1995) and the ADOS module 1 (Lord et al., 1999). We also administered the ESDM curriculum checklist, a 500-item assessment that examines developmental skills in receptive and expressive communication, social interaction, imitation, self-care, cognition, play, and fine and gross motor development.
During each evaluation session, 10 minute samples of child–parent play were gathered at the beginning and end to serve as baseline data. Parents were instructed to play with their child as they typically would at home. In addition, the therapist carried out two 10 minute play interactions in each of the two sessions. These also served as baseline data.
Intervention
At least one parent (the primary caregiver), the child with autism, and the therapist were present during all sessions. For all families, additional family (e.g. parents, grandparents) and educational team members (e.g. speech therapist, teacher, behavioral therapist) occasionally attended the sessions. The therapists included the first author, an educational psychologist and board certified behavior analyst; the second author, a doctoral candidate in human development; and the third author, the principal investigator of the study, who is a licensed psychologist and one of the developers of the intervention program used in the current study. All had extensive experience working with children with autism and providing behavioral interventions to families.
Intervention sessions took place for 1 hour per week over 12 consecutive weeks. All sessions were video recorded. At the start of each session, progress from the past week was reviewed with the parent for 5–10 minutes, followed by a 10 minute parent–child play activity that provided data on child and parent behaviors of interest. The play sample also allowed the therapist to evaluate the parent’s use of the techniques from the prior week’s topic and to provide additional modeling and instruction before proceeding to the next topic. The therapist then introduced the next topic by providing reading materials to the parent, verbally discussing the main points, and demonstrating the teaching strategies involved during a play activity with the child, usually lasting between 10 and 15 minutes. This play activity was videotaped and analyzed to examine therapist and child target behaviors. After the demonstration, the parent was asked to practice the intervention techniques with the child while the therapist coached the parent, provided suggestions and feedback, and modeled until the parent was exhibiting mastery of the behavior. This process typically lasted 10–15 minutes. The therapist then reviewed with the parent the opportunities in their natural routines each day at home to practice the intervention techniques (e.g. playing with toys and games, eating meals, going to the park) and helped the parent formulate a plan for themselves regarding daily review of this lesson, again lasting for 10 minutes.
There was no instruction or requirement that the parents practice these skills for any particular time period or during any particular activity at home. Instead, the skills were taught as general interactive techniques, and activities used in the session were chosen to represent typically occurring activities in the home: play with and without toys, meals, dressing, entering and leaving the room, transitions, and greetings. Any other parental concerns were also addressed during this play period.
Follow-up
After 12 continuous weeks of intervention, the parent and child were scheduled for four additional 1 hour sessions to assess maintenance and generalization. Each generalization probe involved two play samples, one 10-minute parent–child sample and one 10 minute sample with an unfamiliar therapist. The first two follow-up sessions were scheduled 2 weeks apart and the remaining two sessions were scheduled 1 month apart. During the first three sessions, 10 minute parent–child play samples were recorded, parent questions were answered, and any parent techniques that were ‘slipping’ were coached. In the final session, the ADOS and Mullen were re-administered, 10 minute play samples with the parent and unfamiliar adult were recorded, and termination of treatment occurred.
Dependent measures
Outcome data were collected to examine the parents’ level of mastery of ESDM intervention techniques and children’s social communication behaviors during play activities with parents, therapists, and unfamiliar adults. The first and second authors were trained by the principal investigator on the Fidelity of Implementation measure and served as primary and reliability coders of parental behavior. Research assistants served as reliability coders for the child social communication and engagement measures. The assistants were undergraduate students in psychology and had been volunteering at our center for 1 year prior to their involvement in this study. Reliability training involved careful reading of the operational definitions of the dependent variables and practice in recording the responses of the children and adults. The coders were not blind to the goals of the study. Videotaped probes were presented in random order for coding so that expectations regarding child progress could not affect coding. For each dependent variable, inter-rater agreement was calculated for 40 percent of the sessions across all participant children and caregivers.
Fidelity of implementation
The Early Start Denver Model Fidelity Scale was used to evaluate parents’ use of the teaching techniques. The fidelity assessment evaluated 14 adult behaviors that were taught during the coaching sessions. Each behavior was assessed from the 10 minute child–parent play samples occurring at the beginning of each therapy session by using a Likert-scale-based rating system. Inter-rater reliability was established prior to scoring and maintained throughout the study by having two coders independently rate 25 percent of the tapes. An agreement was defined as both coders’ scores being within one point on the Likert scale for each item. The kappa statistic was utilized to assess reliability on parents’ fidelity in order to remove chance agreement. Kappa yielded 0.85 inter-rater agreement.
Child social communication behaviors
To assess changes in the children’s social communication and social engagement, data were collected on two behaviors: (a) number of spontaneous functional verbal utterances, and (b) number of imitative behaviors. Spontaneous functional verbal utterances were defined as verbalizations (1) initiated by the child without an adult model; (2) relevant to the interaction (i.e. no out-of-context, stereotypic, or echolalic responses); (3) combined with body and facial orientation toward the adult and/or relevant stimulus materials; and (4) containing a phonetically correct approximation of the word or word combination (adapted from R.L. Koegel, O’Dell and Dunlop, 1988; Symon, 2005). Imitative behaviors included (1) imitation of actions on objects; (2) imitation of manual acts without objects; and (3) imitation of vocalizations and words (adapted from Uzgiris and Hunt, 1975).
For social communication measures, all behaviors were transcribed. An agreement was defined as both observers recording the same verbal utterance and imitative behavior (i.e. imitative word, action, or gesture), while a disagreement was defined as one of the observers recording a behavior as occurring and the other observer recording the behavior as not occurring during the probe. Reliability ratings were 85 percent (range 76–100%) for spontaneous verbal utterances and 93 percent (range 78–100%) for imitative behaviors.
Observation ratings of child engagement
The Child Behavior Rating Scale (CBRS: Mahoney and Wheeden, 1998) was used to assess children’s engagement across a five-point Likert rating scale ranging from 1 (very low) to 5 (very high). The CBRS evaluates the child across seven items, ranging from abilities to attend and problem-solve during the activity, to cooperate with adult instructions or tasks, to initiate new play ideas, and to share enjoyment and enthusiasm with the adult during the play activity. These items are organized into two main categories of behavior: child attention and child initiations.
For Likert-scale ratings of child engagement, an agreement was defined as both observers giving the exact rating on a probe-by-probe basis. Reliability ratings were 85 percent (range 76–100%) for spontaneous verbal utterances, 93 percent (range 78–100% ) for imitative behaviors, and 88 percent (range 72–100%) for child engagement. The kappa statistic was also utilized to assess reliability on child engagement measures in order to remove chance agreement. Kappa statistics were 0.82 and 0.79 for child attention and initiations respectively during parent–child interactions, and were 0.77 and 0.78 for child attention and initiations respectively during therapist–child interactions.
Results
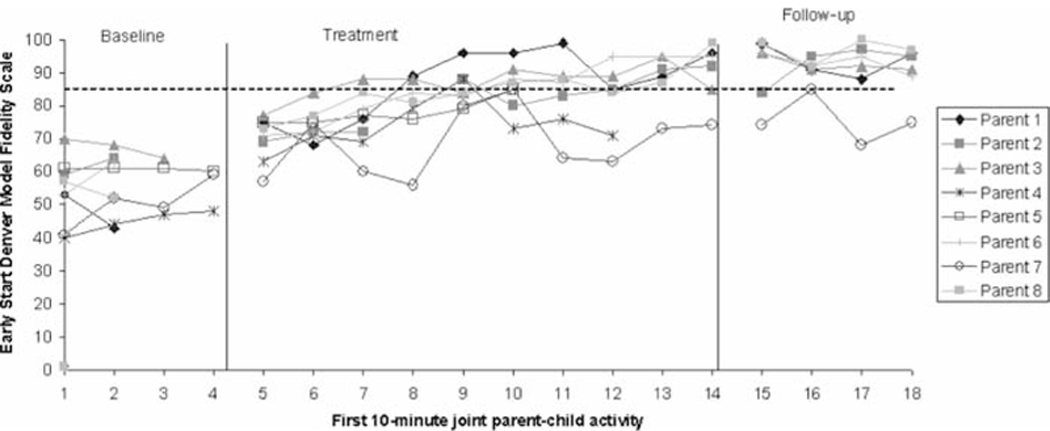
Parent acquisition
Figure 1 displays the Fidelity of Implementation scores for the parents during interactions with the children at baseline, intervention, and follow-up phases. The baseline data show a moderate level of correct implementation of the ESDM techniques by the parents, averaging 48 percent for parent 1, 62 percent for parent 2, 67 percent for parent 3, 45 percent for parent 4, 60 percent for parent 5,58 percent for parent 6, 50 percent for parent 7, and 55 percent for parent 8. For those parents that completed the parent training program, all but one acquired mastery of the ESDM techniques at or above the 85 percent criterion by the fifth to sixth intervention session. These high levels of correct implementation of the ESDM techniques were maintained at follow-up probes for those parents who initially met fidelity and completed the intervention program, averaging 94 percent for parent 1, 93 percent for parents 2, 3, and 6, and 97 percent for parent 8.
Figure 1.
Parents’ acquisition of Early Start Denver Model treatment techniques across parent-child play activities
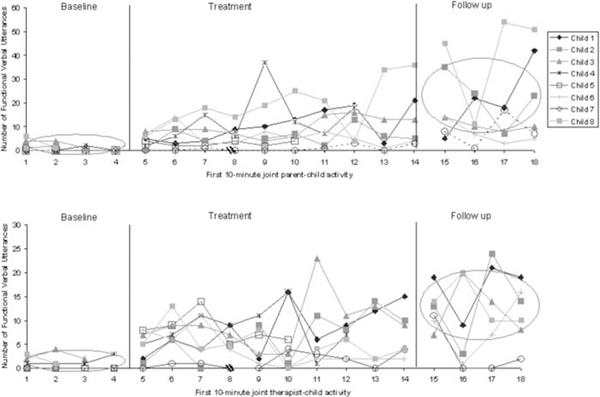
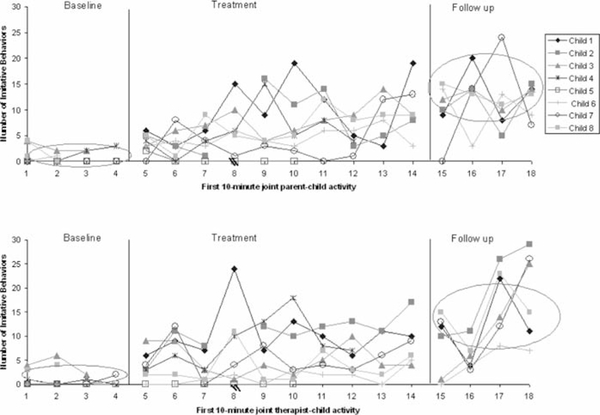
Child change
Figures 2 and 3 present the frequency of children’s spontaneous functional verbal utterances and imitative behaviors over a 10-minute period for each session during parent–child (i.e. top tier) and therapist–child (i.e. bottom tier) play interactions. Prior to intervention, all children produced at or close to zero level of verbal production and imitative behavior during 10-minute interactions with both the parent and the therapist. Once the intervention began, the children’s production of functional verbal responses increased to higher levels during both 10-minute parent–child and therapist–child–interactions compared to initial rates of speech production. Further visual inspection of parent–child versus therapist–child interactions showed similar rates of spontaneous vocalizations. In addition, seven out of eight children demonstrated a consistent increase in their use of imitative behaviors in both parent and therapist play activities. The six children who entered the follow-up phase continued to demonstrate a higher level of spontaneous functional verbal utterances and imitative behavior compared to baseline levels during 10-minute interactions with parents and unfamiliar therapists.
Figure 2.
Number of spontaneous functional verbal utterances across parent-child and therapist-child play activities
Figure 3.
Number of imitative behaviors across parent-child and therapist-child play activities
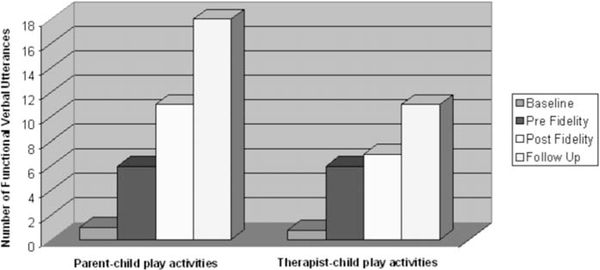
An analysis of change in the children’s spontaneous functional language use was also conducted to determine whether parents’ acquisition of the teaching techniques affected the children’s skill level. Figure 4 shows the group average number of spontaneous functional verbal utterances during parent–child and therapist–child play activities across baseline, pre-fidelity (i.e. treatment sessions before the parents met criteria for the teaching techniques), post-fidelity (i.e. treatment sessions after the parents met criteria), and follow-up sessions. As a group, the children’s number of spontaneous verbal utterances showed the largest gains once the parents demonstrated mastery of the intervention techniques. These gains continued to occur during the 3 month follow-up period after the treatment had ended. For three of these six children, no other treatment began during this period. For children 1,2, and 8, intense Discrete Trial Training (DTT) services began.
Figure 4.
Average number of spontaneous functional verbal utterances across parent-child and therapist-child play activities
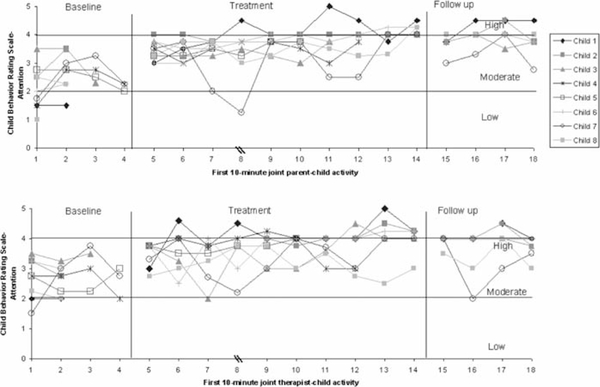
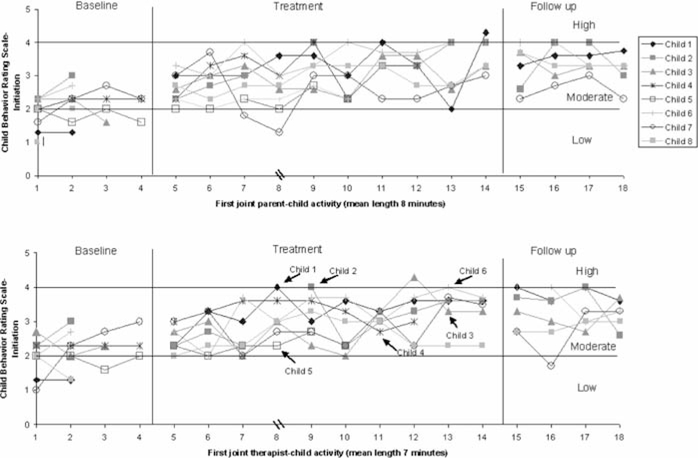
Figures 5 and 6 present data on observed child engagement by examining levels of attentiveness and social initiative behaviors during caregiver–child (i.e. top tier) and therapist–child (i.e. bottom tier) interactions. Prior to intervention, the graphs indicate that all children demonstrated low to moderate levels of attentiveness and initiations to both the caregiver and the therapist during play samples. During intervention, the children’s attentive and social initiative behaviors reached moderately high levels with their parents and therapists. For the six children who completed follow-up, child attention and social initiative behaviors remained at positive levels during 10 minute parent and therapist interactions.
Figure 5.
Child attentiveness ratings across parent-child play activities
Figure 6.
Child initiation ratings across parent-child and therapist-child play activities
Discussion
The results of this study suggest the feasibility of a short-term parent education program using the ESDM and its fusion of developmental and basic behavioral techniques, for families that have recently received a diagnosis of autism for their toddler. All parents showed improvement in technique use on a variety of interactive, communicative, and teaching skills that foster child attention, positive affect, imitation, and communication. Individual parent behavior revealed a significant increase in skills from baseline to mastery of the techniques (previously defined as 85% of the total score on the fidelity instrument) by the fifth to sixth week of coaching for seven out of eight parents who completed the treatment. Once acquired, each parent maintained their skill level through the rest of the treatment period, and for the 3 months following the end of all treatment. Thus, the parent data suggest that the treatment led to lasting behavior change, and that the parents integrated these interactive skills into their daily lives with their child and maintained them long after the treatment ended.
Two parents dropped out of the treatment before completion, one due to health problems and distance, the other due to initiation of an intensive home treatment program. Had there been a choice to have intervention delivered at home, the first parent may well have completed the treatment. She demonstrated excellent learning of the techniques, and her child demonstrated positive responses in many behaviors, though no speech acquisition, during his enrollment. The second parent and child also demonstrated progress in the intervention. Since the intervention was designed to fill the gap between diagnosis and the initiation of intensive treatment, this family was seen not as a treatment failure but rather as demonstrating the progression that was expected and desired for all the children. Had intervention been able to be delivered in the home, and had intensive treatment not have been an exclusion option, this family may have continued the treatment as well. Thus, parents demonstrated successful learning, and those who completed the treatment program (with the exception of one parent) demonstrated maintenance of the skills taught.
Although parent 7 showed improvement in technique use compared to baseline levels, this mother never reached consistent levels of fidelity. Both parents worked full-time, and as a result the child spent a large portion of his day with the grandmother. To accommodate the family’s needs, the mother, father, and grandmother were invited to attend all sessions. The therapists focused primarily on the mother’s interactions and technique use with the child (as she was identified as the primary care giver), while the father and grandmother observed and practiced when time allotted. Perhaps the presence of additional family members prevented the mother from receiving the full attention she needed in order to incorporate the teaching techniques in an effective and consistent manner. Individualization of intervention and flexibility of partnership relationships, with the larger family unit, may be an important area of future research in order to find the balance between meeting the family’s needs and still maintaining efficacy of the treatment model.
The individual data from each child demonstrate that the children emitted almost no social communicative behaviors, initiation, imitation, or speech during baseline. As expected from this type of sample, there is much inconsistency from week to week for each individual child and much inconsistency in a single week across children. However, the weekly treatment data with both therapist and parent reveal a gradual increase in all behaviors for all children. Visual comparison of the last 2 weeks of treatment, and the four follow-up measurement points with the baseline points, reveal consistent and sustained gains in all target behaviors following the 12 week treatment for the six children who completed treatment. The two children who dropped out show gains during their participation periods in most of the targeted behaviors as well.
A question that arises from the data concerns whether the child behavior is being directly elicited by the therapeutic techniques, and thus represents a latent set of skills that are being elicited by a changed social environment. Does the therapy ‘pull’ communication from the child so that all that is being reflected here represents increased frequency in the immediate situation due to changed environmental contingencies? To some extent this must be true. Behaviors must be elicited and reinforced in order to be learned, and the treatment is designed to prompt, elicit, scaffold, and reinforce communication and social engagement.
Several aspects of the current data can shed some light on this question. The first is the finding that the child behaviors with the parent change significantly as the parent acquires the skills (seen in Figure 4), while the child behaviors with the therapist do not change during that same period. This is likely because the therapist is using consistent behaviors throughout the treatment sessions, unlike the parents, who are learning new skills. However, there are other indications that the child change reflects permanent, sustained changes and growth in their social-communicative skills. The strongest argument is that if the behaviors were only being elicited by the treatment, then the child behaviors with the therapist, who already possesses all the skills, should show an immediate and dramatic change from baseline, in contrast to child behaviors with the parents, who do not know these techniques at the start of treatment, as shown in their baseline measures. Instead, the child change data occur slowly over the 12 weeks and are quite similar in their interactions with parent and with therapist. This argues that the changes represent real child learning and change in the child repertoire.
The second argument is that for all children who completed treatment, though no child spoke during baseline, they all are using speech as an intentional communication tool during final sessions, which increases during the follow-up sessions, after treatment has ended. Continued child growth without any therapist contact suggests that the parent’s new skills are indeed the agent of change and that parental interactions are the main source of child change. All of these findings argue that the change in children represents child acquisition of new social-communicative skills. However, the design of this experiment would have been enhanced if the generalization probes used throughout the treatment had been carried out in unfamiliar and very different environments, as Yoder has suggested (Yoder and Stone, 2006). This is an important methodological issue that is now being addressed in subsequent studies at our center.
A primary goal of the present study was to examine whether a 1-hour weekly clinic visit could result in real benefit to young children with autism. The 1-hour weekly visit is still a primary delivery system for allied health professionals like speech and language pathologists, occupational therapists, and psychologists. The study indicates that a brief and economical 1-hour a week intervention for only 12 weeks can lead to lasting change, if it targets parent skills that can easily be incorporated into children’s natural environments. The finding adds to other findings (Rogers et al., 2006; Stahmer and Gist, 2001) that short-term 1-hour 1:1 interventions can result in significant change in children with autism if the treatment incorporates significant parent training and parent implementation of the techniques in natural settings.
A second goal was to develop a generalist intervention that could be delivered by a range of early childhood professionals. All of the therapists in this study had psychology degrees rather than speech-language pathology training. They followed the parent manual exactly in the weekly sessions. While this team was successful in implementing the intervention, there was still considerable expertise in early autism communication treatment in the group. To what extent community early interventionists can deliver this model to diverse community populations in real-world settings and achieve these results is currently being tested at our site.
A third goal was to develop an intervention that could be implemented immediately following diagnosis, by one or another member of the diagnostic team. The goal of diagnosis is treatment, and being able to offer an immediate, brief, and effective intervention program to parents allows clinicians to provide parents with support and help at what we imagine must be one of the most painful times of their lives. This was intended to be not a comprehensive intervention but rather a very targeted one, to provide immediate treatment and supports for parents and children, and to fill the gap that often occurs between the time a family receives a diagnosis and the time that more intensive interventions begin. Children with autism need multiple interventions that target their various needs. This was developed to be one of many interventions that a child with autism will receive in their lives.
A final point of discussion involves the children’s level of disruptive behavior during the intervention program. We examined this variable for two of the eight children who displayed extremely aggressive behaviors, including biting, head-banging, and knocking down furniture. For these children, the topics on behavior management were taught early in the intervention. Functional assessments were conducted during the first few intervention sessions, we taught the three relevant topics (10–12) to the parents, and we monitored children’s aggressive behaviors on a weekly basis for the remaining sessions. As parents implemented positive replacement behavior techniques, both children showed immediate decreases in disruptive behavior across environments during subsequent sessions, and the problem behaviors occurred at very low rates for the rest of the treatment. The remaining six children rarely engaged in challenging behaviors. The low level of disruptive behaviors may have been prevented by the use of motivational components within naturalistic play routines. Research has shown that techniques such as reinforcing child attempts (R.L. Koegel et al., 1988), child-preferred activities (R.L. Koegel et al., 1987a), stimulus variation (Dunlap and Koegel, 1980), and direct response–reinforcer relationships (R.L. Koegel and Williams, 1980; Williams et al., 1981) incorporated within teaching opportunities are likely to heighten children’s motivation to respond and to interact with people in their environment.
There are several weaknesses to this study that are currently being addressed in replications and extensions in multisite replication studies. One involves the clinic-based delivery, which limits accessibility for parents, though it economizes on clinician time. Having home delivery in addition to clinic delivery would strengthen this model. A possible criticism concerning delivery in natural versus artificial settings (R.L. Koegel et al., 1987b; 1992) might be raised. We argue that a clinic is one natural setting for parents who are seeking help with their children, and parent delivery throughout a child’s daily life assures natural settings for the intervention for their children. A second weakness involves the nature of our generalization probes, as described above. A third weakness is the lack of a control group of children, which we are now addressing in a randomized controlled design examining the efficacy of our intervention model compared to community intervention programs for young children with autism. A final limitation, though not weakness, is that the intervention was conducted at a university, with all the supports that come with a research institution. This study involved pilot work of a new intervention, and as such it follows the sequence of efficacy studies suggested for autism treatment research (Lord et al., 2005; Smith et al., 2007), beginning with single-subject design in lab settings, and moving to randomized controlled trials. If efficacy is replicated in more rigorous designs, the question then becomes one of exportability, of community effectiveness. That question needs to be answered for this and many other autism therapies, and we are currently conducting effectiveness studies of this model.
In summary, looking back to our original question of whether 1 hour of weekly therapy can lead to lasting changes in young, non-verbal children with autism, our data suggest the affirmative. However, future empirical study is needed to determine whether this particular intervention is more effective than others for producing parent and child change and the extent to which parent coaching skills transmit meaningful, permanent developmental growth in toddlers with autism.
Contributor Information
LAURIE A. VISMARA, MIND Institute, Sacramento, USA
COSTANZA COLOMBI, MIND Institute, Sacramento, USA.
SALLY J. ROGERS, MIND Institute, Sacramento, USA
References
- AMERICAN PSYCHIATRIC ASSOCIATION (2000) Diagnostic and Statistical Manual of Mental Disorders, 4th edn text rev. (DSM-IV-TR). Washington, DC: APA. [Google Scholar]
- ANDERSON SR & ROMANCZYK RG (1999) ‘Early Intervention for Young Children with Autism: Continuum-Based Behavioral Models’, Journal of The Association for Persons with Severe Handicaps 24: 162–73. [Google Scholar]
- BAKER-ERICZEN MJ, STAHMER AC & BURNS A (2007) ‘Child Demographics Associated with Outcomes in a Community-Based Pivotal Response Training Program’, Journal of Positive Behavior Interventions 9: 52–60. [Google Scholar]
- BAXTER C (1986) ‘Intellectual Disability: Parental Perceptions and Stigma as Stress’, unpublished doctoral dissertation, Monash University, Victoria, Australia. [Google Scholar]
- BROOKMAN-FRAZEE L (2004) ‘Using Parent/Clinician Partnerships in Parent Education Programs for Children with Autism’, Journal of Positive Behavior Interventions 6: 195–213. [Google Scholar]
- burton D (2002) ‘The Autism Epidemic: Is the NIH and CDC Adequate?’, opening statement at the 18 April 2002 hearing of the Committee on Government Reform, Washington, DC. [Google Scholar]
- CHARLOP MH & TRASOWECH JE (1991) ‘Increasing Autistic Children’s Daily Spontaneous Speech’, Journal of Applied Behavior Analysis 24: 747–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CHUMPELIK D (1984) ‘The PROMPT System of Therapy: Theoretical Framework and Applications for Developmental Apraxia of Speech’, Seminars in Speech and Language 5: 139–56. [Google Scholar]
- DUNLAP G & KOEGEL RL (1980) ‘Motivating Autistic Children through Stimulus Variation’, Journal of Applied Behavior Analysis 13: 619–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FOMBONNE E (1998) ‘Epidemiological Surveys of Autism’, in VOLKMAR FR (ed.) Autism and Pervasive Developmental Disorders, pp. 32–63. New York: Cambridge University Press. [Google Scholar]
- FOMBONNE E (2003) ‘Epidemiological Surveys of Autism and other Pervasive Developmental Disorders: An Update’, Journal of Autism and Developmental Disorders 33: 365–82. [DOI] [PubMed] [Google Scholar]
- GILLBERG C, STEFFENBURG S & SCHAUMANN H (1991) ‘Is Autism More Common Now than Ten Years Ago?’, British Journal of Psychiatry 158: 403–9. [DOI] [PubMed] [Google Scholar]
- GREEN G, BRENNAN LC & FEIN D (2002) ‘Intensive Behavioral Treatment for a Toddler at High Risk for Autism’, Behavior Modification 26: 69–103. [DOI] [PubMed] [Google Scholar]
- INGERSOLL B & GERGANS S (in press) ‘The Effect of a Parent-Implemented Imitation Intervention on Spontaneous Imitation Skills in Young Children with Autism’, Research in Developmental Disabilities. [DOI] [PubMed] [Google Scholar]
- KOEGEL LK, KOEGEL RL, HARROWER JK & CARTER CM (1999a) ‘Pivotal Response Intervention. I. Overview of Approach’, Journal of The Association for Persons with Severe Handicaps 24: 174–85. [Google Scholar]
- KOEGEL LK, KOEGEL RL, SHOSHAN Y & MCNERNEY E (1999b) ‘Pivotal Response Intervention. II. Preliminary Long-Term Outcome Data’, Journal of The Association for Persons with Severe Handicaps 24: 186–98. [Google Scholar]
- KOEGEL RL & WILLIAMS JA (1980) ‘Direct vs. Indirect Response–Reinforcer Relationships in Teaching Autistic Children’, Journal of Abnormal Child Psychology 8:537–47. [DOI] [PubMed] [Google Scholar]
- KOEGEL RL, SCHREIBMAN L, BRITTEN KR, BURKE JC & O’NEILL RE(1982) ‘A Comparison of Parent Training to Direct Child Treatment’, in KOEGEL RL, RINCOVER A, & EGEL AL (eds) Educating and Understanding Autistic Children. pp. 260–79. San Diego, CA: College Hill Press. [Google Scholar]
- KOEGEL RL, DYER K & BELL LK (1987a) ‘The Influence of Child-Preferred Activities on Autistic Children’s Social Behavior’, Journal of Applied Behavior Analysis 20: 243–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KOEGEL RL, O’DELL MC & KOEGEL LK (1987b) ‘A Natural Language Teaching Paradigm for Nonverbal Autistic Children’, Journal of Autism and Developmental Disorders 17: 187–99. [DOI] [PubMed] [Google Scholar]
- KOEGEL RL, O’DELL MC & DUNLAP G (1988) ‘Producing Speech Use in Nonverbal Autistic Children by Reinforcing Attempts’, Journal of Autism and Developmental Disorders 18: 525–38. [DOI] [PubMed] [Google Scholar]
- KOEGEL RL, KOEGEL LK & SURRATT AV (1992) ‘Language Intervention and Disruptive Behavior in Preschool Children with Autism’, Journal of Autism and Developmental Disorders 22: 141–53. [DOI] [PubMed] [Google Scholar]
- KOEGEL RL, BIMBELA A & SCHREIBMAN L (1996) ‘Collateral Effects of Parent Training on Family Interactions’, Journal of Autism and Developmental Disorders 26: 347–59. [DOI] [PubMed] [Google Scholar]
- KRANTZ PJ, MACDUFF MT & MCCLANNAHAN LE (1993) ‘Programming Participation in Family Activities for Children with Autism: Parents’ Use of Photographic Activity Schedules’, Journal of Applied Behavior Analysis 26: 137–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LASKI KE, CHARLOP MH & SCHREIBMAN L (1988) ‘Training Parents to Use the Natural Language Paradigm to Increase Their Autistic Children’s Speech’, Journal of Applied Behavior Analysis 21: 391–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LORD C, RUTTER M, DILAVORE PC & RISI S (1999) The Autism Diagnostic Observation Schedule: The Manual. Los Angeles, CA: Western Psychological Services. [Google Scholar]
- LORD C, WAGNER A, ROGERS S, SZATMARI P, AMAN M, CHARMAN T,et al. (2005) ‘Challenges in Evaluating Psychosocial Interventions for Autistic Spectrum Disorders’, Journal of Autism and Developmental Disorders 35: 695–708. [DOI] [PubMed] [Google Scholar]
- LUTZKER JR & STEED SE (1998) ‘Parent Training for Families of Children with Developmental Disabilities’, in BRIESMEISTER JM & SCHAEFER CE (eds) Handbook of Parent Training: Parents as Co-Therapists for Children’s Behavior Problems, 2nd edn, pp. 281–307. Hoboken, NJ: Wiley. [Google Scholar]
- LUTZKER JR, HUYNEN KB & BIGELOW KM (1998) ‘Parent Training’, in VAN HASSELT VB & HERSEN M (eds) Handbook of Psychological Treatment Protocols for Children and Adolescents, pp. 467–500. Mahwah, NJ: Erlbaum. [Google Scholar]
- MAHONEY G & PERALES F (2003) ‘Using Relationship-Focused Intervention to Enhance the social-Emotional Functioning of Young Children with Autism Spectrum Disorders’, Topics in Early Childhood Special Education 23: 77–89. [Google Scholar]
- MAHONEY G & PERALES F (2005) ‘The Impact of Relationship Focused Intervention on Young Children with Autism spectrum Disorders: A Comparative Study’, Journal of Development and Behavioral Pediatrics 26: 77–85. [DOI] [PubMed] [Google Scholar]
- MAHONEY G & WHEEDEN CA (1998) ‘Effects of Teacher Style on the Engagement of Preschool Aged Children with Special Learning Needs’, Journal of Developmental and Learning Disorders 2: 293–315. [Google Scholar]
- MAHONEY G, BOYCE G, FEWELL P, SPIKER D & WHEEDEN CA (1998) ‘The Relationship of Parent-Child Interaction to the Effectiveness of Early Intervention Services for At-Risk Children and Children with Disabilities’, Topics in Early Childhood Special Education 18: 5–17. [Google Scholar]
- MCGEE GG, MORRIER MJ & DALY T (1999) ‘An Incidental Teaching Approach to Early Intervention for Toddlers with Autism’, Journal of The Association for Persons with Severe Handicaps 24: 133–46. [Google Scholar]
- MOES D, KOEGEL RL, SCHREIBMAN L & LOOS LM (1992) ‘Stress Profiles for Mothers and Fathers of Children with Autism’, Psychological Reports 71: 1272–4. [DOI] [PubMed] [Google Scholar]
- MULLEN EM (1995) Mullen Scales of Early Learning (AGS Edition). Circle Pines, MN: American Guidance Service. [Google Scholar]
- NATIONAL RESEARCH COUNCIL (2001) Educating Children with Autism. Washington, DC: National Academy Press. [Google Scholar]
- OZONOFF S & CATHCART K (1998) ‘Effectiveness of a Home Program Intervention for Young Children with Autism’, Journal of Autism and Developmental Disorders 28: 25–32. [DOI] [PubMed] [Google Scholar]
- ROGERS SJ (2000) ‘Differential Diagnosis of Autism before Age 3’, International Review of Research in Mental Retardation 23: 1–31. [Google Scholar]
- ROGERS SJ & LEWIS H (1989) ‘An Effective Day Treatment Model for Young Children with Pervasive Developmental Disorders’, Journal of the American Academy of Child and Adolescent Psychiatry 28: 207–14. [DOI] [PubMed] [Google Scholar]
- ROGERS SJ, HERBISON J, LEWIS H, PANTONE J & REIS K (1986) ‘An Approach for Enhancing the Symbolic, Communicative, and Interpersonal Functioning of Young Children with Autism and Severe Emotional Handicaps’, Journal of the Division of Early Childhood 10: 135–48. [Google Scholar]
- ROGERS SJ, HALL T, OSAKI D, REAVEN J & HERBISON J (2000) ‘A Comprehensive, Integrated, Educational Approach to Young Children with Autism and Their Families’,in HARRIS SL & HANDLEMAN JS (eds) Preschool Education Programs for Children with Autism, pp. 95–134. Austin, TX: Pro-Ed. [Google Scholar]
- ROGERS SJ, HAYDEN D, HEPBURN S, CHARLIFUE-SMITH R, HALL T & HAYES A (2006) ‘Teaching Young Nonverbal Children with Autism Useful Speech: A Pilot Study of the Denver Model and PROMPT Interventions’, Journal of Autism & Developmental Disorders 36: 1007–24. [DOI] [PubMed] [Google Scholar]
- ROGERS SJ & LEWIS H (1989) ‘An Effective Day Treatment Model for Young Children with Pervasive Developmental Disorders’, Journal of the American Academy of Child and Adolescent Psychiatry 28: 207–214. [DOI] [PubMed] [Google Scholar]
- ROGERS SJ, VISMARA LA & COLOMBI C (in preparation) The Early Start Denver Model Parent Manual. Davis: University of California. [Google Scholar]
- ROGERS SJ, DAWSON G, SMITH CM, WINTER JM & DONALDSON AL (in press) Early Start Denver Model Intervention for Young Children with Autism Manual. Seattle: University of Washington. [Google Scholar]
- SCARBOROUGH AA, SPIKER D, MALLIK S, HEBBELER KM, BAILEY DB JR & Simeonsson RJ (2004) ‘A National Look at Children and Families Entering Early Intervention’, Exceptional Children 70: 469–83. [Google Scholar]
- SMITH T, SCAHILL L, DAWSON G, GUTHRIE D, LORD C, ODOM S, et al. (2007) ‘Designing Research Studies on Psychosocial Interventions in Autism’, Journal of Autism and Developmental Disorders 37: 354–66. [DOI] [PubMed] [Google Scholar]
- SPARROW SS, BALLA DA & CICCHETTI DV (2005) Vineland Adaptive Behavior Scales, Second Edition Shoreview, MN: AGS Publishing. [Google Scholar]
- STAHMER AC (1995) ‘Teaching Symbolic Play Skills to Children with Autism Using Pivotal Response Training’, Journal of Autism and Developmental Disorders 25: 123–41. [DOI] [PubMed] [Google Scholar]
- STAHMER AC & GIST K (2001) ‘The Effects of an Accelerated Parent Education Program on Technique Mastery and Child Outcome’, Journal of Positive Behavior Interventions 3: 75–82. [Google Scholar]
- STAHMER AC & SCHREIBMAN L (1992) ‘Teaching Children with Autism Appropriate Play in Unsupervised Environments Using a Self-Management Treatment Package’, Journal of Applied Behavior Analysis 25: 447–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SYMON JB (2005) ‘Expanding Interventions for Children with Autism: Parents as Trainers’, Journal of Positive Behavior Interventions 7: 159–73. [Google Scholar]
- UZGIRIS IE & HUNT JM (1975) Assessment in Infancy: Ordinal Scales of Psychological Development. Champaign: University of Illinois Press. [Google Scholar]
- WATSON PJ & WORKMAN EA (1981) ‘The Non-Concurrent Multiple Baseline Across-Individuals Design: An Extension of the Traditional Multiple Baseline Design’, Journal of Behavior Therapy and Experimental Psychiatry 12: 257–9. [DOI] [PubMed] [Google Scholar]
- WILLIAMS JA, KOEGEL RL & EGEL AL (1981) ‘Response-Reinforcer Relationships and Improved Learning in Autistic Children’, Journal of Applied Behavior Analysis 14: 53–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- YEARGIN-ALLSOPP M, RICE C, KARAPURKAR T, DOERNBERG T, BOYLE C & Murphy E (2003) ‘Prevalence of Autism in a US Metropolitan Area’,Journal of the American Medical Association 289: 49–55. [DOI] [PubMed] [Google Scholar]
- YODER P & STONE WL (2006) ‘Randomized Comparison of Two Communication Interventions for Preschoolers with Autism Spectrum Disorders’, Journal of Consulting and Clinical Psychology 74: 426–35. [DOI] [PubMed] [Google Scholar]