Abstract
Objective
Our aim was to assess the diagnostic performance of F-18 fluorocholine (FCH) positron emission tomography/computed tomography (PET/CT) in detecting hyperfunctioning parathyroid tissue (HPT) in patients with elevated parathyroid hormone levels with negative or inconclusive conventional imaging results and to compare the findings with those obtained using technetium-99m sestamibi (MIBI) scintigraphy and neck ultrasonography (US).
Materials and Methods
Images of 105 patients with hyperparathyroidism who underwent FCH PET/CT, dual-phase MIBI parathyroid scintigraphy (median interval: 42 days), and neck US were retrospectively analyzed. The gold standard was histopathological findings for 81 patients who underwent parathyroidectomy and clinical follow-up findings in the remaining 24 patients. Sensitivities, positive predictive values (PPVs), and accuracies were calculated for all imaging modalities.
Results
Among the 81 patients who underwent parathyroidectomy, either parathyroid adenoma (n = 64), hyperplasia (n = 9), neoplasia (n = 4), or both parathyroid adenoma and hyperplasia (n = 1) were detected, except 3 patients who did not show HPT. Of the 24 (23%) patients who were followed-up without operation, 22 (92%) showed persistent hyperparathyroidism. FCH PET/CT showed significantly higher sensitivity than MIBI scintigraphy and US in detection of HPT (p < 0.01). Sensitivity, PPV, and accuracy of FCH PET/CT were 94.1% (95/101), 97.9% (95/97), and 92.4% (97/105), respectively. The corresponding values for MIBI scintigraphy and US were 45.1% (46/102), 97.9% (46/47), and 45.7% (48/105) and 44.1% (45/102), 93.8% (45/48), and 42.9% (45/105), respectively. Among the 35 patients showing negative MIBI scintigraphy and neck US findings, 30 (86%) showed positive results on FCH PET/CT. FCH PET/CT could demonstrate ectopic locations of HPT in 11 patients whereas MIBI and US showed positive findings in only 6 and 3 patients, respectively.
Conclusion
FCH PET/CT is an effective imaging modality for detection of HPT with the highest sensitivity among the available imaging techniques. Therefore, FCH PET/CT can be recommended especially for patients who show negative or inconclusive results on conventional imaging.
Keywords: Positron emission tomography, Computed tomography, Fluorocholine, Hyperparathyroidism, Tc-99m sestamibi, Parathyroid adenoma
INTRODUCTION
In patients with hyperparathyroidism, preoperative localization of hyperfunctioning parathyroid tissue (HPT) using noninvasive imaging techniques has become a mainstay in the management of disease because it facilitates targeted surgery such as minimally invasive parathyroidectomy (1). Although the combination of neck ultrasound (US) and technetium-99m (Tc-99m) methoxyisobutylisonitrile [sestamibi (MIBI)] dual-phase scintigraphy is the conventional imaging work-up to localize HPT, it may fail to identify abnormal hyperfunctioning glands in up to 30% of cases (2). Four-dimensional computed tomography (4D-CT) and dynamic magnetic resonance imaging (MRI) have emerged as second-line imaging modalities; however, there is currently no sufficient evidence to recommend their routine use in localizing HPT (3,4). Furthermore, a high radiation burden is another concern associated with the use of 4D-CT (5).
Following the incidental discovery of fluorine-18 (F-18)-labeled fluorocholine (FCH) accumulation in parathyroid adenoma (6), several recent clinical studies showed that FCH positron emission tomography/computed tomography (PET/CT) is a promising modality for detection of HPT, even in patients with multi-glandular disease (7,8,9,10,11,12). However, the available data in the literature is still lacking. Therefore, we designed this study to assess the diagnostic performance of FCH PET/CT for detection of HPT in patients with elevated parathyroid hormone (PTH) levels who showed either negative or inconclusive results on conventional imaging. In addition, we tried to assess whether dual-phase FCH PET/CT offers added benefits over MIBI and US in detecting HPT and to determine whether there is any relationship between FCH uptake intensity in HPT and the serum PTH level.
MATERIALS AND METHODS
This study was approved by Istanbul University Clinical Research Ethics Committee (08/01/2016-7689) and all subjects signed an informed consent form. The study was supported by Istanbul University Scientific Research Fund (project number: 24412) and conducted from June 2015 to May 2018.
Study Population
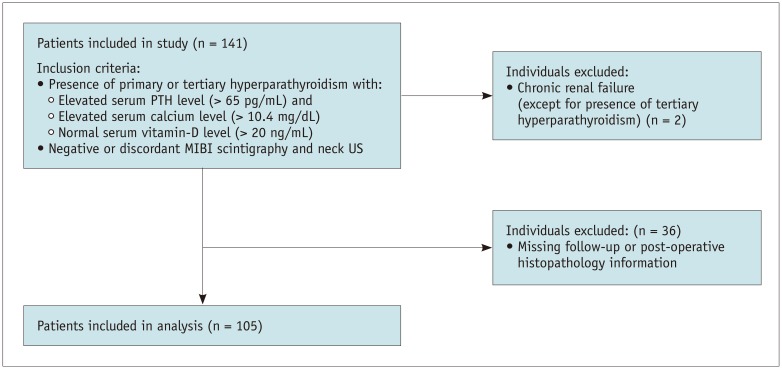
Data for a total of 105 patients with hyperparathyroidism (79 females, 26 males; age range, 16–95 years; mean age ± standard deviation: 55 ± 14.7 years) with negative or discordant results on MIBI and US were retrospectively analyzed (Fig. 1). Twelve (11%) patients had a previous parathyroidectomy operation and 11 patients had a prior thyroidectomy operation due to nodular goiter, of whom 7 were diagnosed as having papillary thyroid cancer. Twelve patients had nodular goiter and 3 patients had a history of radioiodine therapy due to hyperthyroidism.
Fig. 1. Flow chart showing patient selection process.
MIBI = technetium-99m sestamibi, n = number of patients, PTH = parathyroid hormone, US = ultrasonography
F-18 FCH Labeling Procedure
In-house FCH labeling via the nucleophilic method was performed using a fully automated radiochemistry synthesis device (Trasis All-in-One; Ans, Belgium) according to the labeling procedure described by Kryza et al. (13). Quality control tests were performed following specifications described in European Pharmacopoeia. The total time for the entire synthesis procedure, including quality control tests, was 80–90 minutes.
Imaging Acquisition
PET/CT was performed after injecting a mean of 325.1 ± 86.7 MBq (8.8 ± 2.3 mCi) F-18 FCH intravenously. Dual-phase PET/CT images were acquired using PET/CT scanners (GE Discovery 710; Waukesha, WI, USA or Siemens Biograph 6, Knoxville, TN, USA) with an initial scan at 15 minutes post-injection (range: 12–17 minutes) covering the neck and upper chest and a late scan at 45 minutes post-injection (range: 36– 60 minutes) covering the whole body (vertex-mid thigh) or the cervico-thoracic region. The CT topogram guide, low-dose (49–76 mAs) CT transmission scan for attenuation correction, and PET emission scan at 3 minutes per bed position were acquired.
Sixty-five patients (62%) underwent dual-phase MIBI scintigraphy at our institution. After injection of 740 ± 74 MBq (20 ± 2 mCi) Tc-99m MIBI, regional static images of the cervico-thoracic region were acquired at 15 and 90 minutes and single-photon emission computed tomography/computed tomography (SPECT/CT) scans of the head, neck, and thorax were acquired at 60 minutes using an integrated SPECT/CT camera (Siemens Symbia T16; Hoffman Estates, IL, USA). For the remaining 40 patients (38%), proper dual-phase MIBI scintigraphy with SPECT or SPECT/CT was performed at the referral centers. The median interval between FCH PET/CT and parathyroid MIBI scintigraphy was 42 days (range: 2–291 days). In all patients, at least one neck US examination was performed by a radiologist using a high-frequency linear probe (5–12 MHz) with a median interval of 30 days (range: 1–232 days).
Image Analysis
All PET/CT images were read separately by two experienced nuclear medicine physicians who were aware of the patients' clinical diagnosis and previous imaging and laboratory data. From the skull base to the lower part of mediastinum, any focal FCH uptake discernible from the background activity that was not related to thyroid tissue or a lymph node seen on CT slices was considered positive for HPT. All lesions involving an initial disagreement between the readers were re-evaluated together by the readers to reach a final consensus. Additionally, maximum standardized uptake values (SUVmax) of all discernible suspicious lesions and mean SUV (SUVmean) from the thyroid gland were calculated for both initial and late FCH PET/CT images. All MIBI scans that were reported by different attending physicians were also re-evaluated by a nuclear medicine physician. Any focal MIBI uptake above the background activity that was not related to the thyroid tissue in the neck and upper mediastinum in the initial scan and/or any remaining focus inside the thyroid bed at the late scan other than the thyroid nodule was considered as positive for parathyroid adenoma. Any focus with initial MIBI uptake with wash-out pattern on late imaging was recorded as a suspicious lesion for parathyroid adenoma.
Parathyroidectomy and Histopathology
Eighty-one out of 105 (77%) patients underwent parathyroidectomy, of which 49 (60%) underwent minimal invasive parathyroidectomy. Of these 81 patients, 53 (65%) were operated on at our institute by an experienced endocrine surgeon, while the remaining 38 (35%) were operated on at different centers. Pathological results were obtained and recorded. Patients who were not operated on due to negative imaging results or because of unwillingness to undergo the surgery or a contraindication for surgery were followed-up and their serum calcium and PTH levels were determined at 3–6-month intervals for at least 12 months.
Statistical Analysis
Statistical analysis was performed using SPSS software version 21.0 (IBM Corp., Armonk, NY, USA), and the level of significance was set at a p value < 0.05. Sensitivity, positive predictive value (PPV), and accuracy were calculated for all three imaging modalities while counting suspicious imaging results as all positive. Specificity and negative predictive value were not calculated due to the bias in selecting patients with discordant or equivocal results in conventional imaging. Postoperative histopathological results or persistently elevated serum PTH and calcium levels in non-operated patients were considered as the reference standards. McNemar's test was used to compare the sensitivity of the imaging modalities. Wilcoxon signed-rank test was used for comparison of early and delayed SUVs. Pearson's correlation coefficient was used for assessment of the correlation between early and delayed SUVs and between the SUVs and serum PTH levels.
RESULTS
Mean serum PTH and calcium levels were 199.3 ± 206.1 pg/mL (reference value: 15–65 pg/mL) and 11.0 ± 0.84 mg/dL (reference value: 8.4–10.2 mg/dL), respectively. There was only weak correlation between SUVs and PTH levels (early SUVmax: r = 0.236, p = 0.026; delayed SUVmax: r = 0.259, p = 0.014).
Of the 81 patients who underwent parathyroidectomy, parathyroid adenoma was diagnosed in 64 (79%), parathyroid hyperplasia in 9 (11%), parathyroid neoplasia in 4 (5%), and both adenoma and hyperplasia in 1 (1%) patient. In the remaining 3 (4%) patients, no parathyroid tissue could be found in histopathological analysis. Among these, 1 patient showed a negative preoperative FCH PET/CT scan, and the follow-up PTH levels decreased to the normal range, while in the remaining 2 patients with positive preoperative FCH PET/CT scans, the raised PTH levels persisted during follow-up. Of the 24 (23%) patients who did not undergo an operation, 22 (92%) had persistently elevated PTH levels during follow-up and were also considered to have proven HPT.
Sensitivity, PPV, and accuracy of FCH PET/CT in the detection of HPT were 94.1%, 97.9%, and 92.4%, respectively. The corresponding values for MIBI and US were 45.1%, 97.9%, and 45.7% and 44.1%, 93.8%, and 42.9%, respectively. The difference between FCH PET/CT and other imaging modalities was statistically significant (p < 0.001) (Table 1).
Table 1. Sensitivity, PPV, and Accuracy of Each Imaging Modality.
| Sensitivity (%) | PPV (%) | Accuracy (%) | |
|---|---|---|---|
| All patients (n = 105) | |||
| FCH PET/CT | 94.1 (95/101) | 97.9 (95/97) | 92.4 (97/105) |
| MIBI scintigraphy | 45.1 (46/102) | 97.9 (46/47) | 45.7 (48/105) |
| US | 44.1 (45/102) | 93.8 (45/48) | 42.9 (45/105) |
| Only histopathology-proven patients (n = 81) | |||
| FCH PET/CT | 96.2 (76/79) | 98.7 (76/77) | 95.1 (77/81) |
| MIBI scintigraphy | 48.8 (39/80) | 97.5 (39/40) | 48.1 (39/81) |
| US | 45.0 (36/80) | 97.3 (36/37) | 44.4 (36/81) |
| MIBI scintigraphy and US negative patients (n = 35) | |||
| FCH PET/CT | 85.7 (30/35) | 100 (30/30) |
FCH = fluorine-18 fluorocholine, MIBI = technetium-99m sestamibi, n = number of patients, PET/CT = positron emission tomography/computed tomography, PPV = positive predictive value, US = ultrasonography
Comparison of FCH PET/CT with Tc-99m MIBI Scintigraphy
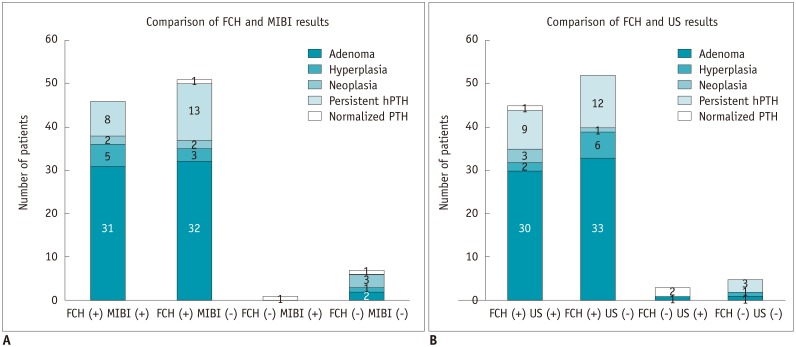
FCH PET/CT and MIBI scintigraphy showed concordant results in 53 patients (50%) (46 positive; 7 negative) and discordant results in 52 (50%) patients (51 with positive FCH versus negative MIBI results; 1 with negative FCH versus positive MIBI results) (Fig. 2A, Table 2). In all 46 patients with concordantly positive results, HPT was proven by either histopathological examination (38 patients) or clinical follow-up (8 patients). Among the 7 patients with concordantly negative results, follow-up PTH levels decreased to the normal range in only 1 patient. However, 3 patients showed proven HPT in parathyroidectomy specimens and the remaining 3 showed persistently elevated PTH levels during follow-up.
Fig. 2. Distribution of concordant and discordant cases between FCH PET/CT and MIBI scintigraphy (A) and neck ultrasonography (B) according to patients' final status based on findings from postoperative histopathological assessments or clinical follow-up examinations.
FCH = fluorine-18 fluorocholine, hPTH = persistent raised PTH, PET/CT = positron emission tomography/computed tomography
Table 2. Comparison of FCH PET/CT and MIBI Scintigraphy Findings in 105 Patients.
| n | |
|---|---|
| FCH and MIBI positive | 46 |
| Parathyroidectomy operation | |
| Adenoma | 31 |
| Hyperplasia | 5 |
| Neoplasia | 2 |
| Parathyroid tissue could not be found at surgery (elevated PTH value during follow-up) | 1 |
| Follow-up without surgery | |
| Persistently elevated PTH values | 7 |
| FCH and MIBI negative | 7 |
| Parathyroidectomy operation | |
| Adenoma | 1 |
| Adenoma and hyperplasia | 1 |
| Hyperplasia | 1 |
| Follow-up without surgery | |
| Persistently elevated PTH values | 3 |
| Normal PTH values | 1 |
| FCH positive and MIBI negative | 51 |
| Parathyroidectomy operation | |
| Adenoma | 32 |
| Hyperplasia | 3 |
| Neoplasia | 2 |
| Parathyroid tissue could not be found at surgery (elevated PTH value during follow-up) | 1 |
| Follow-up without surgery | |
| Persistently elevated PTH values | 12 |
| Normal PTH values | 1 |
| FCH negative and MIBI positive | 1 |
| Parathyroidectomy operation | |
| No parathyroid tissue detected | 1 |
PTH = parathyroid hormone
Among the 51 patients with FCH-PET/CT-positive and MIBI-negative results, 38 received parathyroidectomy, revealing adenoma in 32, parathyroid hyperplasia in 3, and parathyroid neoplasia in 2 patients. One patient was operated on but showed no parathyroid tissue in the postoperative histopathological assessment, and the elevated PTH levels persisted during follow-up. In the remaining 13 patients who did not undergo surgery, 12 had persistently elevated PTH levels (median PTH: 133.5 pg/mL) and one had normalized PTH levels during follow-up (47 pg/mL).
One patient with negative FCH PET/CT and positive MIBI scans underwent parathyroid surgery, but postoperative histopathological assessment revealed no parathyroid tissue and showed benign thyroid nodules instead.
Comparison of FCH PET/CT with Neck US Examination
When FCH PET/CT was compared with neck US, 50 patients showed concordant results (45 positive; 5 negative) and 55 showed discordant results (52 with positive FCH and negative US findings; 3 with negative FCH and positive US findings) (Fig. 2B, Table 3). Among the 45 patients with concordantly positive results, HPT was proven in all except one by either pathological evaluation (35 patients) or clinical follow-up (9 patients). On the other hand, 5 patients with concordantly negative results had proven HPT.
Table 3. Comparison of FCH PET/CT and Neck US Findings in 105 Patients.
| n | |
|---|---|
| FCH and US positive | 45 |
| Parathyroidectomy operation | |
| Adenoma | 30 |
| Hyperplasia | 2 |
| Neoplasia | 3 |
| Follow-up | |
| Persistently elevated PTH values | 9 |
| Normal PTH values | 1 |
| FCH and US negative | 5 |
| Parathyroidectomy operation | |
| Adenoma and hyperplasia | 1 |
| Hyperplasia | 1 |
| Follow-up | |
| Persistently elevated PTH values | 3 |
| FCH positive and US negative | 52 |
| Parathyroidectomy operation | |
| Adenoma | 33 |
| Hyperplasia | 6 |
| Neoplasia | 1 |
| Parathyroid tissue could not be found at surgery (elevated PTH value during follow-up) | 2 |
| Follow-up | |
| Persistently elevated PTH values | 10 |
| FCH negative and US positive | 3 |
| Parathyroidectomy operation | |
| Adenoma | 1 |
| Parathyroid tissue could not be found at surgery (decreased PTH value during follow-up) | 1 |
| Follow-up | |
| Normal PTH values | 1 |
Fifty-two patients showed positive FCH PET/CT findings despite showing negative US results. Of these, 42 were operated on and HPT was found in 40 (adenoma in 33, hyperplasia in 6, and neoplasia in one) while no parathyroid tissue was found in 2 patients despite showing persistently elevated PTH levels during follow-up, with one of these patients showing a positive focus in the mediastinum on FCH PET/CT. Among the 10 patients with positive FCH-PET/CT and negative US findings who did not undergo surgery, all had persistently elevated PTH levels during follow-up. Of the 3 patients with negative FCH-PET/CT and positive US findings, 2 patients underwent surgery, which revealed parathyroid adenoma in one. However, no parathyroid tissue was detected in the other patient on histopathological examination. Among the remaining 5 patients with concordantly negative results, 2 were operated on and showed HPT, whereas the remaining 3 did not undergo surgery and showed persistently elevated PTH levels during follow-up.
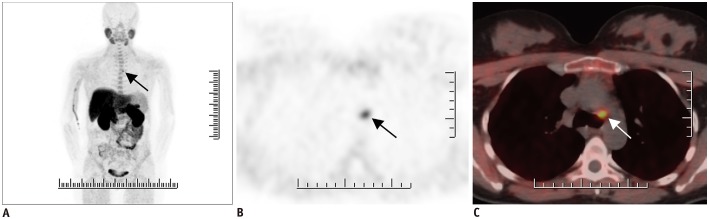
Among the 35 (33%) patients with both negative MIBI and US findings, 30 (86%) showed positive FCH PET/CT findings resulting in a proven HPT (22 by histopathology and 8 by clinical follow-up) (Fig. 3). In addition, FCH PET/CT demonstrated an ectopic location of HPT (1 submandibular, 4 para/retroesophageal, 6 mediastinal) in 11 patients (Fig. 4). MIBI and US showed positive results in only 6 and 3 of these cases, respectively.
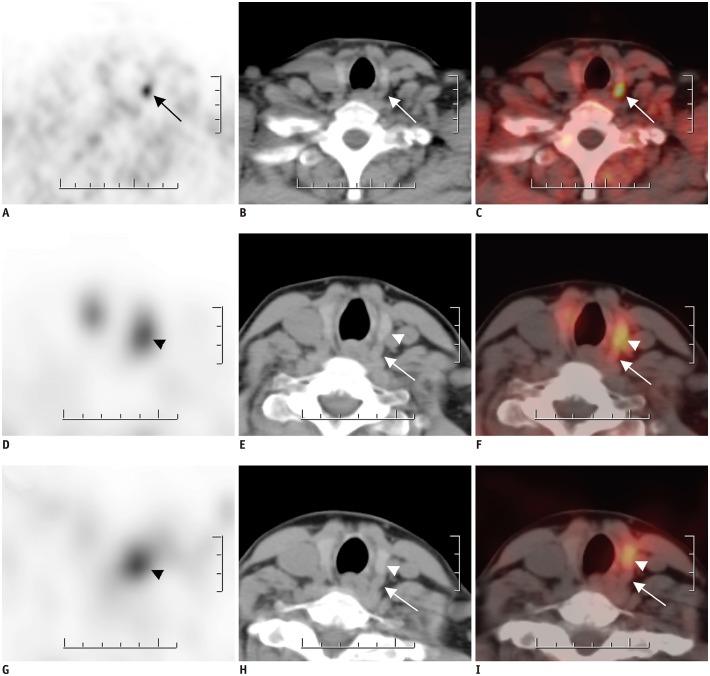
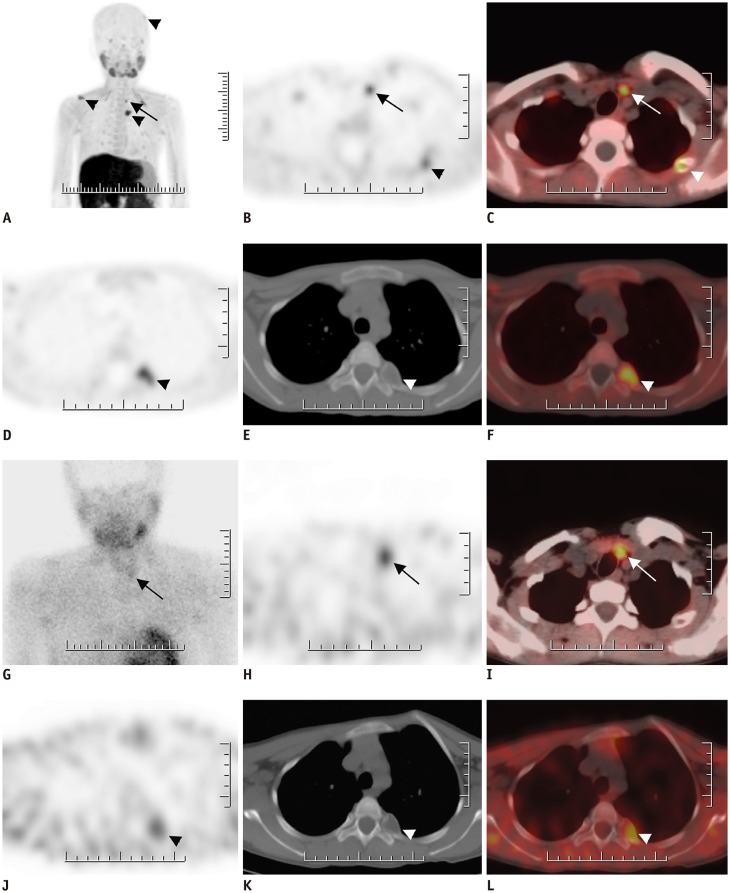
Fig. 3. FCH PET/CT (A–C) and MIBI SPECT/CT (D–I) findings for 48-year-old female with hyperparathyroidism (PTH level: 191 pg/mL).
FCH PET (A), CT (B), and fused PET/CT (C) images in FCH PET/CT reveal nodular lesion with intense FCH uptake (arrows) posterior to left thyroid lobe, which was confirmed to be parathyroid adenoma. Patient also showed papillary thyroid microcarcinoma in left thyroid lobe with no FCH uptake. In early MIBI SPECT (D), CT (E), and fused SPECT/CT (F) images, MIBI uptake was noted on left thyroid lobe. Moreover, MIBI uptake persisted in late SPECT (G), CT (H), and fused SPECT/CT (I) images (arrowheads). However, parathyroid lesion posterior to left thyroid lobe did not exhibit any MIBI uptake in early and late SPECT/CT scans (arrows). SPECT = single-photon emission computed tomography
Fig. 4. 39-year-old female patient with hyperparathyroidism (PTH level: 203.0 pg/mL) showing negative MIBI and ultrasonography results (not shown).
FCH PET/CT MIP image (A) shows focus of FCH uptake on upper mediastinum (arrow). Axial PET (B) and fused PET/CT (C) images reveal 1-cm nodular lesion with intense FCH uptake in aortopulmonary window (arrows). Postoperative histopathology revealed presence of ectopic mediastinal parathyroid adenoma. MIP = maximum intensity projection
Of the 12 patients showing clinical findings of recurrent hyperparathyroidism, 11 showed positive FCH PET/CT findings, and HPT was confirmed by histopathological examination in 10 of these patients. Among these 10 patients, 5 showed positive findings with FCH PET/CT despite showing negative MIBI and US findings. MIBI yielded true-positive findings in 5 patients while US showed true-positive findings in 4 patients in this subgroup.
There were 4 cases with parathyroid neoplasia in our series. In all of them, FCH PET/CT yielded positive results with higher early SUVmax (10.8 ± 5.0 vs. 7.1 ± 3.5) and late SUVmax (11.8 ± 5.8 vs. 7.3 ± 3.6) compared to the mean values for whole patients. There was no finding suggestive of local or distant metastasis in whole-body FCH PET/CT in this particular subgroup. MIBI showed 2 true-positive cases and US showed 3 true-positive cases in the neoplasia group.
Two patients with chronic renal failure were included as possible cases of tertiary hyperparathyroidism, since both FCH PET/CT and US demonstrated a single parathyroid adenoma. One of these cases also showed brown tumors that were identified by both FCH PET/CT and MIBI (Fig. 5).
Fig. 5. 16-year-old female patient with chronic renal failure.
A–F. FCH PET/CT MIP image (A) reveals multiple foci of increased FCH uptake. Axial PET (B) and fused PET/CT (C) images on lower neck region reveal intense FCH uptake on left side that was found to be in accordance with parathyroid adenoma in surgical specimen (arrows). Brown tumors also demonstrate increased FCH uptake (arrowheads). G–L. MIBI SPECT/CT images of same patient. MIBI uptake at late planar (G), SPECT (H), and fused SPECT/CT (I) images reveal MIBI uptake on parathyroid adenoma (arrows). Brown tumors also demonstrate increased MIBI uptake (arrow heads).
Comparison of Early and Delayed FCH PET/CT Imaging
A total of 97 patients showed positive findings with FCH PET/CT. There was no statistically significant difference between the SUVmax of parathyroid lesions in early (mean SUVmax: 7.1 ± 3.5, median SUVmax: 6.1, range: 1.9–19.4) and late imaging (mean SUVmax: 7.3 ± 3.6, median SUVmax: 6.4, range: 2.0–22.4) (p = 0.190). However, significant differences were found in the parathyroid SUVmax/thyroid SUVmean ratio between early (mean ratio: 2.5 ± 1.5, range: 0.8–7.8) and delayed imaging (mean ratio: 2.9 ± 1.5, range: 1.0–10.0) (p < 0.001) among patients without any previous thyroidectomy operation. Strong positive correlations were observed between early and delayed SUVmax of parathyroid lesions (r = 0.898), as well as for parathyroid/thyroid SUV ratios (r = 0.896). On visual analysis, 12 lesions were more prominent on early imaging, whereas 10 were more prominent on delayed imaging. For the remaining lesions, the results were equivocal for both early and delayed imaging.
DISCUSSION
Following incidental detection of FCH uptake in parathyroid adenoma, several clinical studies have been published on the role of FCH PET/CT in hyperparathyroidism, and they have shown better diagnostic performance of FCH PET/CT in comparison with other conventional imaging methods, with higher sensitivity and equally high specificity (7,8,9,10,11,12,14,15,16,17). A recent meta-analysis evaluating the diagnostic performance of FCH PET/CT in hyperparathyroidism revealed that the sensitivity and specificity of FCH PET/CT were 90% and 94%, respectively (18), and another study also reported excellent sensitivity, PPV, and detection rate of 95%, 97%, and 91%, respectively (19). Furthermore, PET/MRI was reported to have better diagnostic performance than MRI alone in 10 patients with primary HPT (20).
Our study also demonstrated the encouraging performance of FCH PET/CT in the detection of HPT. Because our study population included a difficult series of selected patients with negative or discrepant US and MIBI results, the sensitivities of both US and MIBI were lower than those reported in the literature (2,21,22,23). Even in this difficult population, FCH PET/CT presented impressive results with high sensitivity, PPV, and accuracy of 94.1%, 97.9%, and 92.4%, respectively, whereas the corresponding values for MIBI and US were 45.1%, 97.9%, and 45.7% and 44.1%, 93.5%, and 42.9%, respectively.
Even though our study included 10 histopathologically proven recurrent HPT cases, FCH PET/CT was able to localize all lesions, providing excellent sensitivity (100%) in comparison with MIBI (5 true-positive results) and US (4 true-positive results). FCH PET/CT could also identify all 4 cases with parathyroid neoplasia, whereas both MIBI and US showed positive findings in only 2 cases. Furthermore, FCH PET/CT was superior in demonstrating ectopic localization of HPT in comparison with US and MIBI. Similar to MIBI scintigraphy, FCH PET/CT could identify brown tumors, which are bone lesions that arise as a result of increased osteoclastic activity in hyperparathyroidism and mimic bone metastasis (24,25,26), which was also documented by Taywade et al. (27) previously.
We believe that the superior spatial resolution of PET technology over SPECT is one of the important factors influencing the better diagnostic performance of FCH PET/CT. Indeed, in this study, MIBI could reveal only 5 (55.6%) of 9 cases of parathyroid hyperplasia while FCH PET/CT demonstrated the lesions in 7 (78%) cases. In addition, the differences in the molecular properties and uptake mechanisms of FCH and MIBI may be responsible for the superiority of FCH PET/CT. Therefore, the additional molecular potential of FCH in terms of its uptake mechanism in HPT should be elucidated. MIBI is a lipophilic cationic isonitrile derivative that is accumulated in mitochondria-rich oxyphilic cells (28). P-glycoprotein may also be responsible for MIBI uptake (29). In contrast, increased FCH uptake in HPT may be related to accelerated phosphatidylcholine turnover or upregulation of phospholipid-dependent choline kinase activity (30,31,32). FCH uptake in benign secreting tumors such as parathyroid adenomas was proposed to be related to cholinergic autocrine loop upregulation and increased expression of choline transporters rather than the membrane proliferation rate (33). In contrast to studies showing that MIBI is preferentially accumulated by oxyphilic cells, there is no study yet demonstrating the type of parathyroid cells that preferentially accumulate FCH. As a proposal, if FCH was capable of accumulating in chief cells rather than oxyphilic cells, then it might have a molecular advantage over MIBI in detecting HPT. Further research is needed to elucidate the exact biological processes underlying the FCH uptake in HPT.
Another advantage of FCH PET/CT would be the shorter imaging time. Early imaging within the first 15 minutes appeared to be good enough to reveal the majority of the lesions in this study. However, among the proven HPT cases (n = 102), we found an SUVmax increase of more than 5% (up to 37%) in 46 (45%) parathyroid lesions and an SUVmax decrease of more than 5% (up to 54%) in 33 (32%) parathyroid lesions in late scans. These findings suggest that single time-point imaging either in early (15 minutes) or late (45–60 minutes) imaging may be associated with a potential risk of missing lesions. Nevertheless, we have not seen any lesion that was identified in early imaging and completely disappeared in late scans or vice versa. Lezaic et al. (7) reported better lesion contrast at 60-minute imaging compared to the 5-minute scan. We also demonstrated a significantly higher parathyroid-SUVmax/thyroid-SUVmean ratio at 45 minutes compared to that obtained with 15-minute imaging, even though 32% of the cases showed reduced SUVmax in late imaging. Accordingly, we suggest early imaging at 15 minutes with late imaging at 45–60 minutes for selected patients with inconclusive or negative early imaging findings.
Because the biggest disadvantage of FCH PET/CT is its high cost in comparison with MIBI, the use of FCH PET/CT as a second-line imaging tool for difficult cases with negative or discordant conventional imaging findings seems to be more feasible. Another potential drawback of FCH PET/CT is that FCH is not a specific tracer for parathyroid tissue. Therefore, physiological uptake of FCH in thyroid parenchyma and preferential accumulation in well-differentiated thyroid cancers and metastatic or inflammatory lymph nodes may occur. In our study, there were 2 cases with papillary thyroid cancer with increased FCH uptake in which the parathyroid lesions could be differentiated accurately by considering their location. In another case, we considered an FCH-positive lesion in the neck as an enlarged parathyroid tissue, but histopathological examination did not confirm any parathyroid tissue and indicated an inflammatory lymph node instead. Although we do not recommend routine intravenous contrast medium administration for FCH PET/CT imaging, its usage may further improve results in selected cases with inconclusive results.
There are several limitations in this study. First, there was a bias in selecting the patient population, which mainly included patients with negative or discrepant conventional imaging findings, leading to reduced sensitivity values for both US and MIBI in comparison with those reported in previous studies. Second, more than half of the US examinations and 38% (40/105) of MIBI examinations were performed at different referral centers and reported by various physicians, which may also have created severe imaging variability and bias. Finally, 24 out of 105 patients (23%) were not operated on after imaging. Instead, follow-up serum PTH and serum calcium level measurements were used as reference standards, which might have the potential to create a bias. However, the sensitivity, PPV, and accuracy of the histopathology-proven group were similar to those of the entire study population.
In conclusion, FCH PET/CT is an effective imaging modality for localization of HPT with the highest sensitivity among the available imaging techniques. Therefore, FCH PET/CT may play a key role as a problem-solving imaging modality in difficult cases such as those showing recurrent hyperparathyroidism and ectopic localizations of HPT.
Footnotes
This research was supported by Istanbul University Scientific Research Projects (BAP) (Project number: 24412).
Conflicts of Interest: The authors have no potential conflicts of interest to disclose.
References
- 1.Wilhelm SM, Wang TS, Ruan DT, Lee JA, Asa SL, Duh QY, et al. The American Association of Endocrine Surgeons guidelines for definitive management of primary hyperparathyroidism. JAMA Surg. 2016;151:959–968. doi: 10.1001/jamasurg.2016.2310. [DOI] [PubMed] [Google Scholar]
- 2.Ciappuccini R, Morera J, Pascal P, Rame JP, Heutte N, Aide N, et al. Dual-phase 99mTc sestamibi scintigraphy with neck and thorax SPECT/CT in primary hyperparathyroidism: a single-institution experience. Clin Nucl Med. 2012;37:223–228. doi: 10.1097/RLU.0b013e31823362e5. [DOI] [PubMed] [Google Scholar]
- 3.Hunter GJ, Schellingerhout D, Vu TH, Perrier ND, Hamberg LM. Accuracy of four-dimensional CT for the localization of abnormal parathyroid glands in patients with primary hyperparathyroidism. Radiology. 2012;264:789–795. doi: 10.1148/radiol.12110852. [DOI] [PubMed] [Google Scholar]
- 4.Nael K, Hur J, Bauer A, Khan R, Sepahdari A, Inampudi R, et al. Dynamic 4D MRI for characterization of parathyroid adenomas: multiparametric analysis. AJNR Am J Neuroradiol. 2015;36:2147–2152. doi: 10.3174/ajnr.A4425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mahajan A, Starker LF, Ghita M, Udelsman R, Brink JA, Carling T. Parathyroid four-dimensional computed tomography: evaluation of radiation dose exposure during preoperative localization of parathyroid tumors in primary hyperparathyroidism. World J Surg. 2012;36:1335–1339. doi: 10.1007/s00268-011-1365-3. [DOI] [PubMed] [Google Scholar]
- 6.Quak E, Lheureux S, Reznik Y, Bardet S, Aide N. F18-choline, a novel PET tracer for parathyroid adenoma? J Clin Endocrinol Metab. 2013;98:3111–3112. doi: 10.1210/jc.2013-2084. [DOI] [PubMed] [Google Scholar]
- 7.Lezaic L, Rep S, Sever MJ, Kocjan T, Hocevar M, Fettich J. 18F-Fluorocholine PET/CT for localization of hyperfunctioning parathyroid tissue in primary hyperparathyroidism: a pilot study. Eur J Nucl Med Mol Imaging. 2014;41:2083–2089. doi: 10.1007/s00259-014-2837-0. [DOI] [PubMed] [Google Scholar]
- 8.Kluijfhout WP, Vorselaars WM, Vriens MR, Borel Rinkes IH, Valk GD, de Keizer B. Enabling minimal invasive parathyroidectomy for patients with primary hyperparathyroidism using Tc-99m-sestamibi SPECT-CT, ultrasound and first results of (18) F-fluorocholine PET-CT. Eur J Radiol. 2015;84:1745–1751. doi: 10.1016/j.ejrad.2015.05.024. [DOI] [PubMed] [Google Scholar]
- 9.Michaud L, Balogova S, Burgess A, Ohnona J, Huchet V, Kerrou K, et al. A pilot comparison of 18F-fluorocholine PET/CT, ultrasonography and 123I/99mTc-sestaMIBI dual-phase dual-isotope scintigraphy in the preoperative localization of hyperfunctioning parathyroid glands in primary or secondary hyperparathyroidism: influence of thyroid anomalies. Medicine (Baltimore) 2015;94:e1701. doi: 10.1097/MD.0000000000001701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kluijfhout WP, Vorselaars WM, van den Berk SA, Vriens MR, Borel Rinkes IH, Valk GD, et al. Fluorine-18 fluorocholine PET-CT localizes hyperparathyroidism in patients with inconclusive conventional imaging: a multicenter study from the Netherlands. Nucl Med Commun. 2016;37:1246–1252. doi: 10.1097/MNM.0000000000000595. [DOI] [PubMed] [Google Scholar]
- 11.Thanseer N, Bhadada SK, Sood A, Mittal BR, Behera A, Gorla AKR, et al. Comparative effectiveness of ultrasonography, 99mTc-sestamibi, and 18F-fluorocholine PET/CT in detecting parathyroid adenomas in patients with primary hyperparathyroidism. Clin Nucl Med. 2017;42:e491–e497. doi: 10.1097/RLU.0000000000001845. [DOI] [PubMed] [Google Scholar]
- 12.Michaud L, Burgess A, Huchet V, Lefèvre M, Tassart M, Ohnona J, et al. Is 18F-fluorocholine-positron emission tomography/computerized tomography a new imaging tool for detecting hyperfunctioning parathyroid glands in primary or secondary hyperparathyroidism? J Clin Endocrinol Metab. 2014;99:4531–4536. doi: 10.1210/jc.2014-2821. [DOI] [PubMed] [Google Scholar]
- 13.Kryza D, Tadino V, Filannino MA, Villeret G, Lemoucheux L. Fully automated [18F]fluorocholine synthesis in the TracerLab MX FDG coincidence synthesizer. Nucl Med Biol. 2008;35:255–260. doi: 10.1016/j.nucmedbio.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 14.Rep S, Lezaic L, Kocjan T, Pfeifer M, Sever MJ, Simoncic U, et al. Optimal scan time for evaluation of parathyroid adenoma with [(18)F]-fluorocholine PET/CT. Radiol Oncol. 2015;49:327–333. doi: 10.1515/raon-2015-0016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hocevar M, Lezaic L, Rep S, Zaletel K, Kocjan T, Sever MJ, et al. Focused parathyroidectomy without intraoperative parathormone testing is safe after pre-operative localization with 18F-fluorocholine PET/CT. Eur J Surg Oncol. 2017;43:133–137. doi: 10.1016/j.ejso.2016.09.016. [DOI] [PubMed] [Google Scholar]
- 16.Huber GF, Hüllner M, Schmid C, Brunner A, Sah B, Vetter D, et al. Benefit of 18F-fluorocholine PET imaging in parathyroid surgery. Eur Radiol. 2018;28:2700–2707. doi: 10.1007/s00330-017-5190-4. [DOI] [PubMed] [Google Scholar]
- 17.Quak E, Blanchard D, Houdu B, Le Roux Y, Ciappuccini R, Lireux B, et al. F18-choline PET/CT guided surgery in primary hyperparathyroidism when ultrasound and MIBI SPECT/CT are negative or inconclusive: the APACH1 study. Eur J Nucl Med Mol Imaging. 2018;45:658–666. doi: 10.1007/s00259-017-3911-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim SJ, Lee SW, Jeong SY, Pak K, Kim K. Diagnostic performance of F-18 fluorocholine PET/CT for parathyroid localization in hyperparathyroidism: a systematic review and meta-analysis. Horm Cancer. 2018;9:440–447. doi: 10.1007/s12672-018-0347-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Treglia G, Piccardo A, Imperiale A, Strobel K, Kaufmann PA, Prior JO, et al. Diagnostic performance of choline PET for detection of hyperfunctioning parathyroid glands in hyperparathyroidism: a systematic review and meta-analysis. Eur J Nucl Med Mol Imaging. 2019;46:751–765. doi: 10.1007/s00259-018-4123-z. [DOI] [PubMed] [Google Scholar]
- 20.Kluijfhout WP, Pasternak JD, Gosnell JE, Shen WT, Duh QY, Vriens MR, et al. 18F fluorocholine PET/MR imaging in patients with primary hyperparathyroidism and inconclusive conventional imaging: a prospective pilot study. Radiology. 2017;284:460–467. doi: 10.1148/radiol.2016160768. [DOI] [PubMed] [Google Scholar]
- 21.Lavely WC, Goetze S, Friedman KP, Leal JP, Zhang Z, Garret-Mayer E, et al. Comparison of SPECT/CT, SPECT, and planar imaging with single- and dual-phase (99m)Tc-sestamibi parathyroid scintigraphy. J Nucl Med. 2007;48:1084–1089. doi: 10.2967/jnumed.107.040428. [DOI] [PubMed] [Google Scholar]
- 22.Cheung K, Wang TS, Farrokhyar F, Roman SA, Sosa JA. A meta-analysis of preoperative localization techniques for patients with primary hyperparathyroidism. Ann Surg Oncol. 2012;19:577–583. doi: 10.1245/s10434-011-1870-5. [DOI] [PubMed] [Google Scholar]
- 23.Smith RB, Evasovich M, Girod DA, Jorgensen JB, Lydiatt WM, Pagedar NA, et al. Ultrasound for localization in primary hyperparathyroidism. Otolaryngol Head Neck Surg. 2013;149:366–371. doi: 10.1177/0194599813491063. [DOI] [PubMed] [Google Scholar]
- 24.Uslu L, Calis¸kan A, Sağer S, Teksöz S, Halaç M. Preoperative and postoperative 18FDG PET/CT and bone scintigraphy images in a patient with parathyroid adenoma. Clin Nucl Med. 2013;38:456–458. doi: 10.1097/RLU.0b013e31828e96f7. [DOI] [PubMed] [Google Scholar]
- 25.van Baardwijk A, de Jong J, Arens A, Thimister P, Verseput G, Kremer B, et al. False-positive FDG-PET scan due to brown tumours. Eur J Nucl Med Mol Imaging. 2006;33:393–394. doi: 10.1007/s00259-005-1979-5. [DOI] [PubMed] [Google Scholar]
- 26.Vaishya R, Agarwal AK, Singh H, Vijay V. Multiple ‘brown tumors’ masquerading as metastatic bone disease. Cureus. 2015;7:e431. doi: 10.7759/cureus.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Taywade SK, Damle NA, Behera A, Devasenathipathy K, Bal C, Tripathi M, et al. Comparison of 18F-fluorocholine positron emission tomography/computed tomography and four-dimensional computed tomography in the preoperative localization of parathyroid adenomas-initial results. Indian J Endocrinol Metab. 2017;21:399–403. doi: 10.4103/ijem.IJEM_536_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.O'Doherty MJ, Kettle AG, Wells P, Collins RE, Coakley AJ. Parathyroid imaging with technetium-99m-sestamibi: preoperative localization and tissue uptake studies. J Nucl Med. 1992;33:313–318. [PubMed] [Google Scholar]
- 29.Piwnica-Worms D, Chiu ML, Budding M, Kronauge JF, Kramer RA, Croop JM. Functional imaging of multidrug-resistant P-glycoprotein with an organotechnetium complex. Cancer Res. 1993;53:977–984. [PubMed] [Google Scholar]
- 30.Ratnam S, Kent C. Early increase in choline kinase activity upon induction of the H-ras oncogene in mouse fibroblast cell lines. Arch Biochem Biophys. 1995;323:313–322. doi: 10.1006/abbi.1995.9959. [DOI] [PubMed] [Google Scholar]
- 31.Glunde K, Bhujwalla ZM, Ronen SM. Choline metabolism in malignant transformation. Nat Rev Cancer. 2011;11:835–848. doi: 10.1038/nrc3162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ishizuka T, Kajita K, Kamikubo K, Komaki T, Miura K, Nagao S, et al. Phospholipid/Ca2+-dependent protein kinase activity in human parathyroid adenoma. Endocrinol Jpn. 1987;34:965–968. doi: 10.1507/endocrj1954.34.965. [DOI] [PubMed] [Google Scholar]
- 33.van der Hiel B, Stokkel MPM, Buikhuisen WA, Janssen H, van Velthuysen MLF, Rhodius RJ, et al. 18F-choline PET/CT as a new tool for functional imaging of non-proliferating secreting neuroendocrine tumors. J Endocrinol Metab. 2015;5:267–271. [Google Scholar]