Abstract
Purpose
Routine screening for carotid intima-media thickness (CIMT) and cardiovascular (CV) disease in asymptomatic patients has been criticized for the high costs and large number of patients required for detecting one patient with coronary artery disease (CAD). In order to overcome the low cost-effectiveness thereof, we investigated the feasibility of an economic wireless handheld ultrasound (WHUS) device for CIMT measurement in symptomatic patients.
Materials and Methods
A total of 100 consecutive patients with cardiac symptoms were enrolled. CIMT was measured in all patients. Coronary angiography was performed in 75 patients indicated for the exam.
Results
The mean of maximal CIMT measured from left/right common carotid artery and bulb (max-CIMT) by the WHUS device showed excellent agreement [intraclass correlation coefficient (ICC)=0.960] with a standard ultrasound device and great interobserver repeatability (ICC>0.9 between all observers). Receiver operating characteristic curve analysis showed that the predictive power for CAD was improved when max-CIMT and plaque information (plaque≥2) was added [area under the curve (AUC): 0.838] to the traditional clinical CV risk factors (AUC: 0.769). The cutoff values for CAD prediction with the standard device and the WHUS device were 1.05 mm (AUC: 0.807, sensitivity: 0.78, specificity: 0.53) and 1.10 mm (AUC: 0.725, sensitivity: 0.98, specificity: 0.27), respectively.
Conclusion
max-CIMT measured by a WHUS device showed excellent agreement and repeatability, compared with standard ultrasound. Combined max-CIMT and plaque information added predictive power to the traditional clinical CV risk factors in detecting high-risk CAD patients.
Keywords: Carotid intima-media thickness, coronary artery disease, wireless technology, ultrasonography
INTRODUCTION
Increased carotid intima-media thickness (CIMT) in asymptomatic patients is known for its association with elevated cardiovascular (CV) and cerebrovascular disease risk.1,2,3,4,5,6 Recently, the cost-effectiveness of routine screening of general asymptomatic individuals has been questioned due to its low health benefits and inconclusive results from meta-analyses.7,8,9,10,11,12 The reason behind the low-cost-effectiveness of routine CIMT screening is the high cost of CIMT measurements using standard console ultrasound devices and the large number of asymptomatic patients required for screening one patient with coronary artery disease (CAD). As a strategy to resolve such problems, we undertook a study using an economical device to lower costs and evaluated CIMT in a symptomatic population of patients visiting the outpatient department to identify the number of screened patients needed to detect CAD. A wireless handheld ultrasound (WHUS) device was used in the study to reduce the cumbersomeness of either sending the patient to the ultrasound department or bringing the bulky standard console ultrasound device into the outpatient office and to further extend the use of the device not only in symptomatic patients visiting the clinic but also outside the clinic, such as the emergency department. The WHUS used in this study is currently approved by the US, Korea, and China Food and Drug Administration, is officially supplied for humanitarian aid activities by the United Nations Office for Project Services, and has also been validated for its utility in routine clinical practice.13,14,15,16 Herein, we investigated the feasibility of WHUS in CIMT measurement, compared with standard console ultrasound, and whether such data could be translated into outpatient clinic settings for predicting the presence of CAD in symptomatic patients.
MATERIALS AND METHODS
Study sample
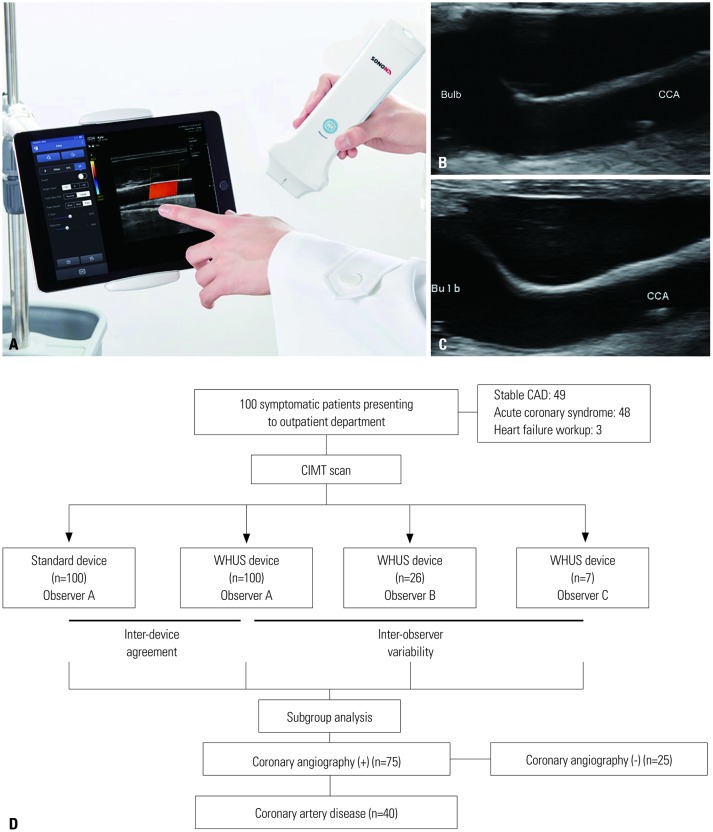
A total of 100 consecutive Korean patients with cardiac symptoms were enrolled through the outpatient Department of Cardiology at Gachon University Gil Medical Center between January 1, 2017 and December 31, 2017. This study conformed to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in its priori approval by the Institutional Review Board of Gachon University Gil Hospital (IRB No. GDIRB2017-030). Informed consent was obtained from all enrolled patients. Inclusion criteria were as follows: 1) age ≥18 years and 2) presence of anginal symptoms or dyspnea regardless of the history of underlying CAD. Exclusion criteria were as follows: 1) debilitating underlying comorbidities, such as cancer, end stage heart failure, and aortic dissection, and 2) structural deformities in the neck that hampered ultrasonographic access to the carotid arteries. All enrolled patients underwent carotid ultrasound scans by both the WHUS (Fig. 1A and B) and a standard device (Fig. 1C). Detailed information regarding enrollment is shown in Fig. 1D.
Fig. 1. Images of the WHUS device, carotid scans from both devices, and details on patient enrollment. (A) The WHUS device can be connected to cellphones or tablets through its built-in Wi-Fi feature from virtually anywhere. The carotid bulb and CCA of the same patient acquired by the (B) WHUS and (C) standard device. (D) The carotid intima-media thickness of a total of 100 patients with cardiac symptoms was evaluated both by the standard and WHUS devices. WHUS, wireless handheld ultrasound; CIMT, carotid intima-media thickness; CAD, coronary artery disease; CCA, common carotid artery.
Ultrasonographic assessment of CIMT
All 100 patients underwent carotid scans by a standard ultrasonographic device (Alpha 7, Aloka, Tokyo, Japan) with a 12-mHz linear probe (UST-5412, Aloka) and the WHUS (SONON 300L, Healcerion, Seoul, Korea) device equipped with a built-in 10-mHz linear probe. The left and right longitudinal projection of the common carotid artery (CCA), the carotid bulb, and the internal carotid artery were observed where the site of the greatest thickness (excluding the plaque lesion) was measured bilaterally along both the near and far walls. The mean value of maximal CIMT measured from four sites (left/right CCA and bulb) was defined as max-CIMT17 and was investigated for its association with CAD. Carotid plaque was defined as a focal region either with more than 50% or 0.5-mm thickening of the CIMT, compared with the surrounding tissue. The CIMT of the CCA was measured 1 cm proximal to the bifurcation, whereas the CIMT of the bulb was examined 1 cm distal to the bifurcation. One highly trained and experienced sonographer performed all of the exams for both the standard and the WHUS device. The acquired images were then measured once manually through a standard computer monitor (SyncMaster 2333, Samsung, Seoul, Korea). A total of three observers were allocated for interdevice and interobserver variability. As shown in Fig. 1D, one observer was designated for interdevice variability from all 100 patients (observer A), while the two other independent observers (observers B and C) measured max-CIMT for the assigned 26 patient images and 7 patient images, respectively, that were attained from the WHUS device to assess interobserver variability. All observers were experienced sonographers and were unaware of each patient's clinical information or status.
Coronary angiography
For subgroup analysis, 75 patients with stable angina with a positive stress test, acute coronary syndrome (ACS), or indication for coronary evaluation during heart failure workup underwent coronary angiography (CAG). CAG was performed using standard Judkins or Amplatz diagnostic catheters. Angiographic CAD was defined as moderate (50–70%) stenosis or severe (≥70%) CAD or a vessel with a previous stent. Minimal atherosclerosis was defined as <50% stenosis of the coronary arteries.
Statistical analysis
Data analysis was performed using IBM SPSS Statistics for Windows (Version 23.0, IBM Corp., Armonk, NY, USA). Continuous, normally distributed data are expressed as a mean±SD. A paired sample t-test was used to compare differences in max-CIMT values between the standard device and the WHUS device. Categorical values are expressed as percentages. The difference between the WHUS and the standard device was defined as max-CIMT of WHUS subtracted by the max-CIMT of the standard device. The Bland-Altman plot was used to assess interdevice agreement and interobserver repeatability. Linear logistic regression was utilized to determine proportional bias between the two devices. Interdevice repeatability and interobserver variability were examined by Pearson's correlation and intraclass correlation coefficient (ICC). The correlation coefficient of Pearson's correlation was denoted as R. Student's one-way ANOVA test was applied to compare intergroup differences in CIMT values in patients with different numbers of pathologic coronary arteries. Predictive power for clinical factors with or without max-CIMT or plaque information was tested by the receiver operating characteristic (ROC) curves. The optimal cutoff value for max-CIMT in predicting CAD was also examined using the ROC curves.
RESULTS
Baseline characteristics
A total of 100 patients with cardiac symptoms, such as chest pain, dyspnea, palpitation, and syncope, were enrolled. As shown in Table 1, the mean age of the total patient population was 65±15 years. Men comprised 66% of the study population. The prevalences of hypertension, diabetes, and dyslipidemia were 59, 30, and 31%, respectively. Of all patients, 75 were indicated for CAG (Table 1).
Table 1. Baseline Characteristics of Patients with or without CAD.
| Total (n=100) | Patients who had CAG (n=75) | CAD(+) (n=40) | CAD(-) (n=34) | p | |
|---|---|---|---|---|---|
| Age (yr) | 65±15 | 65±13 | 70.6±12.3 | 60.9±12.0 | 0.001 |
| Men, n (%) | 66 | 49 (65) | 28 (68) | 21 (64) | 0.805 |
| Hypertension, n (%) | 59 | 43 (57) | 25 (61) | 17 (52) | 0.483 |
| Diabetes mellitus, n (%) | 30 | 22 (29) | 13 (32) | 9 (27) | 0.800 |
| Dyslipidemia, n (%) | 31 | 24 (32) | 13 (32) | 10 (30) | 1.000 |
| Smoking, n (%) | 38 | 31 (41) | 18 (44) | 13 (39) | 0.814 |
| Diagnosis, n (%) | 0.158 | ||||
| Stable angina | 49 | 24 (32) | 9 (23) | 15 (43) | |
| Acute coronary syndrome | 48 | 48 (64) | 30 (75) | 18 (51) | |
| Heart failure | 3 | 3 (4.0) | 2 (5) | 1 (3) | |
| Number of diseased vessels, n (%) | 40 | 40 (53) | 40 (100) | - | <0.001 |
| 1 VD | 10 | 10 (13) | 10 (25) | - | |
| 2 VD | 14 | 14 (19) | 14 (35) | - | |
| 3 VD | 16 | 16 (21) | 16 (40) | - |
CAG, coronary angiography; CAD, coronary artery disease; VD, vessel disease.
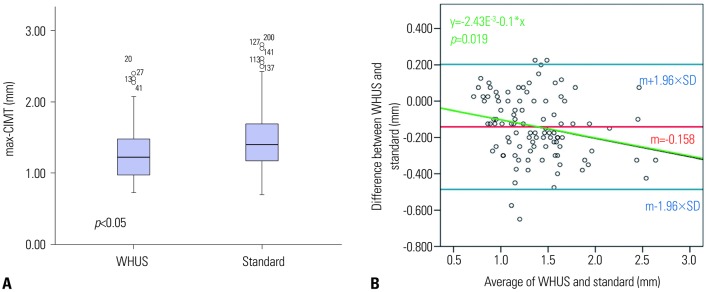
Agreement between the standard device and WHUS device
The comparison between the standard device and the WHUS device is shown in Table 2. The max-CIMT of the standard device ranged from 0.70 mm to 2.80 mm, with a mean value of 1.447±0.443 mm. The max-CIMT of the WHUS ranged from 0.72 mm to 2.50 mm, and the mean value was 1.289±0.393 mm. The absolute difference between two devices was −0.158±0.228 mm (p<0.05) by the paired sample t-test, although Pearson's correlation coefficient and ICC were both above 0.9, suggestive of excellent interdevice correlation and agreement (Table 3, Fig. 2A).
Table 2. Measured CIMT from Three Observers and the Standard Device.
| Sample size (n) | max-CIMT (mm) | CCA CIMT (mm) | Bulb CIMT (mm) | Number of plaques | |
|---|---|---|---|---|---|
| WHUS observer A | 100 | 1.289±0.393 | 1.036±0.344 | 1.542±0.527 | 0.9±1.3 |
| WHUS observer B | 26 | 1.378±0.502 | - | - | - |
| WHUS observer C | 7 | 1.940±0.603 | - | - | - |
| Standard (reference) | 100 | 1.447±0.443 | 1.289±0.393 | 1.289±0.393 | 1.1±1.4 |
CIMT, carotid intima-medial thickness; max-CIMT, mean of the maximal values of carotid intima-medial thickness of a patient; WHUS, wireless handheld ultrasound; CCA, common carotid artery.
Table 3. Absolute Difference and ICC between the WHUS and the Standard Device.
| Sample size (n) | Absolute difference (mm) | pabs | R | pR | ICC | |
|---|---|---|---|---|---|---|
| WHUS vs. Standard (reference) | 100 | -0.158±0.228 | <0.050 | 0.858 | <0.001 | 0.960 |
| Observer A vs. observer B | 26 | 0.024±0.078 | 0.109 | 0.991 | <0.001 | 0.988 |
| Observer A vs. observer C | 7 | 0.028±0.116 | 0.406 | 0.777 | 0.005 | 0.998 |
| Observer B vs. observer C | 7 | -0.009±0.035 | 0.445 | 0.760 | 0.007 | 0.978 |
WHUS, wireless handheld ultrasound; ICC, intraclass correlation coefficient; pabs, p value of absolute difference; pR, p value of correlation coefficient R.
Fig. 2. Interdevice agreement and proportional bias. (A) A plot showing the CIMT of the WHUS and the standard device. (B) A Bland-Altman plot of the relationship between the average of WHUS and standard device and differences between the two devices. m, mean of differences between the WHUS and standard device; max-CIMT, mean of the maximal values of carotid intima-medial thickness of a patient; WHUS, wireless handheld ultrasound.
Repeatability of the WHUS device
Data regarding interobserver variability of the WHUS is shown in Table 3. The max-CIMT between three observers were comparable, and the ICC for the interobserver variability was over 0.9, suggesting excellent agreement between observers (Table 3). In the Bland-Altman plot, the red middle line represents the mean value (m=−0.158 mm) of the difference between two devices, whereas the two blue lines indicates the 1.96×SD above and below the mean value (Fig. 2B). A linear equation (y=−2.43E−3−0.1*x) that was derived from linear logistic regression, shown as a green line, suggested that the differences between two devices were negatively proportional (p=0.019) to the average max-CIMT values between two devices: the discrepancy between two devices was bigger with decreasing max-CIMT (Fig. 2B).
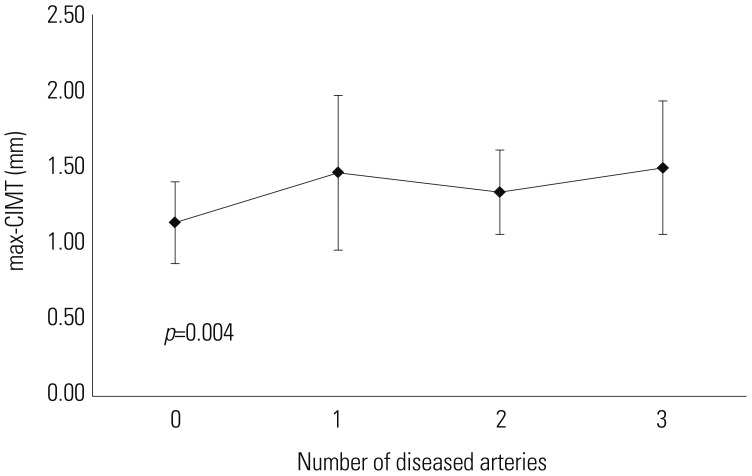
CIMT and number of diseased coronary arteries
The max-CIMT of patients with different numbers of diseased coronary arteries is shown in Supplementary Table 1 (only online) and Fig. 3. A significantly increasing trend of max-CIMT with increasing number of diseased coronary arteries was observed (p=0.004).
Fig. 3. Relationship between maximal carotid intima-media thickness (max-CIMT) and the number of each patient's diseased coronary vessels.
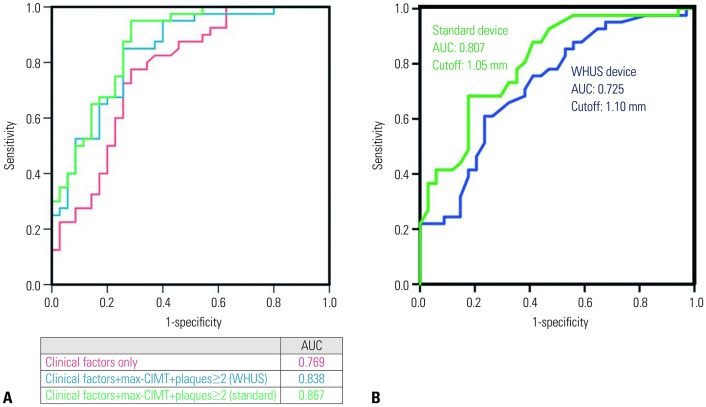
Predictive power for CAD using ROC curves
As a subgroup analysis, patients who underwent CAG were evaluated to analyze the predictive power of WHUS-measured max-CIMT. The baseline characteristics between CAD (+) and CAD (−) groups are presented in Table 1. Except for age, baseline characteristics between the CAD (+) and CAD (−) groups were comparable.
ROC curves constructed using conventional clinical risk factors (age, hypertension, diabetes, smoking, and dyslipidemia) with or without max-CIMT and carotid plaque information are shown in Fig. 4A. The area under the curve (AUC) for the clinical risk factors only was 0.769. When CIMT information (max-CIMT and plaque ≥2) was added to clinical factors, the AUC was increased to 0.838 and 0.867 for WHUS and the standard device, respectively.
Fig. 4. ROC curves for predicting high-risk CAD patients. (A) A plot showing the predictive power of traditional clinical risk factors alone (red), mean maximal CIMT measured from left/right CCA and bulb (max-CIMT), and carotid plaques ≥2, in addition to clinical risk factors, using the WHUS and the standard device, shown in blue and green, respectively. (B) The cutoff max-CIMT values and in predicting high-risk CAD patients using the standard (1.05 mm) and WHUS (1.10 mm) device. ROC, receiver operating characteristic; AUC, area under the curve; CAD, coronary artery disease; WHUS, wireless hand-held ultrasound.
The AUC and cutoff value of max-CIMT for predicting CAD are presented in Fig. 4B. The AUC values of the standard device and the WHUS device were 0.807 and 0.725, respectively, while the cutoff values were 1.05 and 1.10 mm, respectively. The WHUS device had a higher sensitivity (0.976 to 0.781) and lower specificity (0.265 to 0.781) than the standard device (Table 4). The estimated numbers of patients with CAD using the cutoff values were 63 and 60 for the WHUS and standard device, respectively (Table 4). Both devices were able to detect 39 (97.5%) out of the 40 patients who had angiographic CAD.
Table 4. Diagnostic Properties Regarding the WHUS and Standard Devices.
| AUC | Cutoff value (mm) | Sensitivity | Specificity | PPV | NPV | Estimated number of CAD patients using cutoff | Number of true CAD | |
|---|---|---|---|---|---|---|---|---|
| max-CIMT of standard device | 0.807 | 1.05 | 0.78 | 0.53 | 0.98 | 0.29 | 60 | 39 (97.5%) |
| max-CIMT of WHUS | 0.725 | 1.10 | 0.98 | 0.27 | 0.78 | 0.53 | 63 | 39 (97.5%) |
max-CIMT, mean of maximal value of carotid intima-medial thickness of a patient; AUC, area under the curve; PPV, positive predictive value; NPV, negative predictive value; WHUS, wireless handheld ultrasound; CAD, coronary artery disease.
DISCUSSION
In this study, we demonstrated that WHUS-measured CIMT values have great repeatability and agreement with a standard ultrasound device. The WHUS-measured CIMT information also improved predictive power when added to the traditional CV risk factors in detecting CAD, compared with clinical CV risk factors alone. To our knowledge, this is the first study to investigate the feasibility and clinical applicability of WHUS-measured CIMT for point-of-care in symptomatic patients presenting to the clinic.
Our data showed that WHUS-measured CIMT results are reproducible. The ICCs between three observers, which is a barometer of combined agreement and correlation, were all over 0.9, suggestive of excellent interobserver variability. This indicates that WHUS-generated data may be consistent between different users and therefore may be a legitimate diagnostic tool. The gap observed between the conventional and the WHUS device (Table 3, Fig. 2A) may be explained by the relatively blurry image quality of the WHUS in smaller CIMT values (Fig. 1B), compared with the standard device (Fig. 1C). The negative slope (−2.43) of the linear regression for proportional bias suggested that the gap between two devices is wider with smaller CIMT (Fig. 2B).
Previous studies regarding the relationship between CIMT or carotid artery stenosis and CV outcomes have generally investigated asymptomatic patients with or without traditional CV risk factors.5,6,7,8,9,10,18 Moreover, CIMT evaluation for CV screening in such large asymptomatic populations requires many patients for the purpose of preventing a single CV event. The high prices of the conventional ultrasound devices (approximately 150000 USD)19 may also lead to high CIMT test costs (330 USD).11 Most governments or insurance companies worldwide, including the US and Korea, do not reimburse for CIMT: the state of Texas was the only state in the US that covered CIMT for CV screening in 2009.20 Major clinical guidelines also no longer recommend routine CIMT screening for similar reasons.8,12 Accordingly, using a readily accessible economical WHUS device (8000 USD), which costs approximately 5% of the standard device, may dramatically lower the expenses for each CIMT exam. Evaluating symptomatic populations in the outpatient clinic may also reduce the number of patients required to detect a single CV event. Reducing the device cost and focusing on symptomatic populations may collectively improve cost-effectiveness.
The WHUS device may also improve timely decision-making process adding to clinical information gathered by patient examination or history taking. For physicians, determining whether a patient is at high-risk for CAD can be challenging in an outpatient clinical setting. Our data show that WHUS-measured max-CIMT and plaque information (number of plaques ≥2) may improve the precision of detecting CAD patients. As both devices detected 39 patients (97.5%) out of 40 patients with CAD, there was no underestimation by the WHUS device, although the underestimation may have been masked by the small sample size. The high sensitivity and negative predictive value of the WHUS-generated max-CIMT may help physicians to effectively rule out patients at low risk of CAD. With its additive predictability and high sensitivity, physicians may effectively focus their diagnostic process on higher risk patients.
These promising features, however, are only useful when the ultrasound can be readily accessible. Conventional ultrasound devices may not meet such necessities in the clinic, as they are usually heavy and bulky: it may be cumbersome to bring a conventional ultrasound console in and out of the clinic every time a patient with cardiac symptoms present or to send the patient to the ultrasound department. Additionally, the current WHUS device can be connected to cellphones or tablets through its built-in Wi-Fi feature, which enables physicians to evaluate CIMT of patients from virtually anywhere. Such accessibility may improve point-of-care quality for cardiologists, general practitioners, or emergency physicians not only in clinics but in triaging systems in underprivileged regions throughout the world.
The significant proportional bias between the two devices, especially in the lower values, may indicate that the WHUS device may not be able to accurately depict lower CIMT values due to lower resolution. Future efforts for fine-tuning image quality may improve the proportional bias and eventually close the gap between conventional ultrasound devices. Additionally, the small sample size (n=75) for CAD prediction may be a limitation of our study. The non-association between the presence of carotid plaque and CAD risk is inconsistent with previous findings, which may have been caused by the small sample size. Further investigation using a larger sample size in a more homogeneous patient population, such as patients with ACS, for identifying the association between WHUS-measured CIMT and coronary artery plaque burden using intravascular ultrasound is warranted to add precision to the device.
The current study showed that the novel WHUS device has excellent agreement with the standard ultrasound device and offers repeatability among observers. Additionally, CIMT information combined with clinical CV risk factors improved predictability for detecting high-risk patients for CAD, compared with the CV clinical risk factors alone.
ACKNOWLEDGEMENTS
This research was partly supported by the Gachon University Gil Medical Center (Grant number: FDR2015-02) and the Next-Generation Medical Device Development Program for Newly-Created Market of the NRF funded by the Korean government, MSIT (No. 2015M3D5A1066043). This research was also supported by grants [2018-ER6304-00 (2018) and 2018-ER6304-01 (2019)] for research from the Korea Centers for Disease Control, Prevention and partially supported by KSC 200403-17 from the Korean Society of Cardiology, and Seoul R&D Program (BT190153) through the Research and Development for Regional Industry. Wook-Jin Chung works as a nonprofit consultant for Healcerion Co., Ltd. Wook-Jin Chung and the CEO of Healcerion, Jeongwon Ryu, have jointly applied and received a research grant (MSIT No. 2015M3D5A1066043) from NRF of Korea. No fundingbodies or Jeongwon Ryu were involved in either the measurement/analysis of CIMT data of the current research project or writing/revising the manuscript. No other author reported potential conflicts of interest relevant to this article.
We thank Hanul Choi, Kyoung Min You, and Je Hyeong Park for performing ultrasonography for the study.
Footnotes
The authors have no potential conflicts of interest to disclose.
- Conceptualization: Wook-Jin Chung and Jeongwon Ryu.
- Data curation: Wook-Jin Chung, Pyung Chun Oh, and Jeunggeun Moon.
- Formal analysis: Albert Youngwoo Jang and Wook-Jin Chung.
- Funding acquisition: Wook-Jin Chung and Jeongwon Ryu.
- Investigation: Wook-Jin Chung.
- Methodology: Wook-Jin Chung.
- Project administration: Wook-Jin Chung.
- Resources: Wook-Jin Chung.
- Software: Wook-Jin Chung.
- Supervision: Wook-Jin Chung.
- Validation: Albert Youngwoo Jang and Wook-Jin Chung.
- Visualization: Albert Youngwoo Jang and Wook-Jin Chung.
- Writing—original draft: Albert Youngwoo Jang and Wook-Jin Chung.
- Writing—review & editing: Albert Youngwoo Jang and Wook-Jin Chung.
- Approval of final manuscript: All authors.
SUPPLEMENTARY MATERIAL
The Relationship between the max-CIMT and Number of Diseased Coronary Arteries
References
- 1.Nambi V, Chambless L, Folsom AR, He M, Hu Y, Mosley T, et al. Carotid intima-media thickness and presence or absence of plaque improves prediction of coronary heart disease risk: the ARIC (Atherosclerosis Risk In Communities) study. J Am Coll Cardiol. 2010;55:1600–1607. doi: 10.1016/j.jacc.2009.11.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cao JJ, Arnold AM, Manolio TA, Polak JF, Psaty BM, Hirsch CH, et al. Association of carotid artery intima-media thickness, plaques, and C-reactive protein with future cardiovascular disease and all-cause mortality: the Cardiovascular Health Study. Circulation. 2007;116:32–38. doi: 10.1161/CIRCULATIONAHA.106.645606. [DOI] [PubMed] [Google Scholar]
- 3.Øygarden H. Carotid intima-media thickness and prediction of cardiovascular disease. J Am Heart Assoc. 2017;6:e005313. doi: 10.1161/JAHA.116.005313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zanchetti A, Hennig M, Hollweck R, Bond G, Tang R, Cuspidi C, et al. Baseline values but not treatment-induced changes in carotid intima-media thickness predict incident cardiovascular events in treated hypertensive patients: findings in the European Lacidipine Study on Atherosclerosis (ELSA) Circulation. 2009;120:1084–1090. doi: 10.1161/CIRCULATIONAHA.108.773119. [DOI] [PubMed] [Google Scholar]
- 5.Kwon HJ, Park JH, Lee JH, Jeong HS, Song HJ, Kim J, et al. Low common carotid artery systolic occlusion pressure and symptomatic carotid artery stenosis are associated with development of neurologic intolerance during proximal protected carotid artery stenting. Korean Circ J. 2018;48:217–226. doi: 10.4070/kcj.2017.0031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dwivedi A, Al'Aref SJ, Lin FY, Min JK. Evaluation of atherosclerotic plaque in non-invasive coronary imaging. Korean Circ J. 2018;48:124–133. doi: 10.4070/kcj.2017.0392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bots ML, Groenewegen KA, Anderson TJ, Britton AR, Dekker JM, Engström G, et al. Common carotid intima-media thickness measurements do not improve cardiovascular risk prediction in individuals with elevated blood pressure: the USE-IMT collaboration. Hypertension. 2014;63:1173–1181. doi: 10.1161/HYPERTENSIONAHA.113.02683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–3104. doi: 10.1093/eurheartj/ehy339. [DOI] [PubMed] [Google Scholar]
- 9.Costanzo P, Perrone-Filardi P, Vassallo E, Paolillo S, Cesarano P, Brevetti G, et al. Does carotid intima-media thickness regression predict reduction of cardiovascular events? A meta-analysis of 41 randomized trials. J Am Coll Cardiol. 2010;56:2006–2020. doi: 10.1016/j.jacc.2010.05.059. [DOI] [PubMed] [Google Scholar]
- 10.Lorenz MW, Polak JF, Kavousi M, Mathiesen EB, Völzke H, Tuomainen TP, et al. Carotid intima-media thickness progression to predict cardiovascular events in the general population (the PROG-IMT collaborative project): a meta-analysis of individual participant data. Lancet. 2012;379:2053–2062. doi: 10.1016/S0140-6736(12)60441-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.den Ruijter HM, Vaartjes I, Sutton-Tyrrell K, Bots ML, Koffijberg H. Long-term health benefits and costs of measurement of carotid intima-media thickness in prevention of coronary heart disease. J Hypertens. 2013;31:782–790. doi: 10.1097/HJH.0b013e32835e8ee5. [DOI] [PubMed] [Google Scholar]
- 12.Goff DC, Jr, Lloyd-Jones DM, Bennett G, Coady S, D'Agostino RB, Sr, Gibbons R, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:2935–2959. doi: 10.1016/j.jacc.2013.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim EY, Park KH, Choi SJ, Chung WJ. Educational value of pocket-sized ultrasound devices to improve understanding of ultrasound examination principles and sonographic anatomy for medical student. PLoS One. 2017;12:e0185031. doi: 10.1371/journal.pone.0185031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee SH, Kim YJ. Managing a seroma with wireless mobile ultrasound device. J Plast Reconstr Aesthet Surg. 2017;70:e7–e9. doi: 10.1016/j.bjps.2016.11.014. [DOI] [PubMed] [Google Scholar]
- 15.Kim J, Kim S, Jeon S, Jung S. A longitudinal study investigating cervical changes during labor using a wireless ultrasound device. J Matern Fetal Neonatal Med. 2018;31:1787–1791. doi: 10.1080/14767058.2017.1329292. [DOI] [PubMed] [Google Scholar]
- 16.Oh NR, Woo JH, Kim DY, Baek MK. Wireless mobile ultrasonography-assisted parotid duct stone removal. Ear Nose Throat J. 2018;97:E36–E38. doi: 10.1177/0145561318097004-503. [DOI] [PubMed] [Google Scholar]
- 17.Dogan S, Kastelein JJ, Grobbee DE, Bots ML. Mean common or mean maximum carotid intima-media thickness as primary outcome in lipid-modifying intervention studies. J Atheroscler Thromb. 2011;18:946–957. doi: 10.5551/jat.8623. [DOI] [PubMed] [Google Scholar]
- 18.Seo J, Kim GS, Lee HY, Byun YS, Jung IH, Rhee KJ, et al. Prevalence and clinical outcomes of asymptomatic carotid artery stenosis in patients undergoing concurrent coronary and carotid angiography. Yonsei Med J. 2019;60:542–546. doi: 10.3349/ymj.2019.60.6.542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tse KH, Luk WH, Lam MC. Pocket-sized versus standard ultrasound machines in abdominal imaging. Singapore Med J. 2014;55:325–333. doi: 10.11622/smedj.2014078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Polak JF, Pencina MJ, Pencina KM, O'Donnell CJ, Wolf PA, D'Agostino RB., Sr Carotid-wall intima-media thickness and cardiovascular events. N Engl J Med. 2011;365:213–221. doi: 10.1056/NEJMoa1012592. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The Relationship between the max-CIMT and Number of Diseased Coronary Arteries