Abstract
Background and objectives
Influenza poses a public health threat for children and adults. The CDC recommends annual influenza vaccination for children <18 years, yet vaccine uptake remains low for children (57.9%) and adults (37.1%). Given that parental decision-making is key in childhood vaccine uptake, there is a critical need to understand vaccine hesitancy among parents who decide not to vaccinate their children. This study aims to explore predictors of children’s influenza vaccine status given parental vaccination status and examine the factors that contribute to concordance or discordance between parental and children’s vaccine uptake.
Methods
Classification and regression tree (CART) analyses were used to identify drivers of parental decisions to vaccinate their children against influenza. Hierarchy and interactions of these variables in predicting children’s vaccination status were explored.
Results
From a nationally representative sample of non-Hispanic Black and White parents who completed an online survey (n=328), the main factors influencing parents’ decisions to vaccinate their children were vaccine behavior following physician recommendation, knowledge of influenza recommendations for children, influenza vaccine confidence and disease risk. Among unvaccinated parents, the greatest concordance was observed among parents who usually do not get vaccinated following physician recommendation and had lower knowledge of recommendations for influenza vaccination for children. The greatest discordance was observed among unvaccinated parents who had lower hesitancy about recommended vaccines.
Conclusions
Understanding drivers of parental decisions to vaccinate themselves and their children can provide insights on health communication and provider approaches to increase influenza vaccine coverage and prevent influenza related mortality.
Keywords: Influenza vaccination, Influenza, Child health, Vaccine decision-making
Introduction
Influenza poses a significant threat to children’s health [1]. During the 2017–2018 influenza season, 187 pediatric deaths were reported (74% of whom were not vaccinated) [2]. The Centers for Disease Control and Prevention (CDC) recommends annual influenza vaccination for all children aged 6 months to 18 years as an effective preventive strategy, yet vaccine uptake remains low for children (57.9%) [3] and adults (37.1%). As parental acceptance of influenza vaccination for their children is critical to prevent influenza-related morbidity and mortality, it is necessary to understand what factors may influence parental vaccine decision-making.
Previous research has explored multifaceted factors that influenced parental hesitancy about the influenza vaccine for their children [4,5] such as reduced perceived susceptibility to influenza, and concerns of vaccine safety and efficacy [6–12]. For some parents, vaccination risks outweighed the little perceived benefit of vaccination, reflecting the influence of omission bias [13], the belief that harm from inaction (not receiving the influenza vaccine, risking influenza) is preferred over harm from action (the influenza vaccine resulting in adverse effects). Additional barriers encompass the belief that there was an overabundance of vaccines for childhood immunization schedules [14] and preferences for naturally-acquired immunity [15], potentially leading parents to seek out the use of complementary and alternative medicine (CAM) such as herbal remedies and vitamin supplements [16,17]. Broader external influences included logistical barriers (e.g. lack of time, access, convenience) [22], healthcare providers (HCP), institutional trust, and the media (e.g. television, social media) [13,18]. Parents who did not receive physician recommendations or had lower trust in healthcare providers reported lower vaccine uptake [19]. Also contributing to the loss of trust was negative media coverage, such as vaccine linkage with illness and deleterious side effects (e.g., Guillain-Barré syndrome), leading some parents be skeptical of the benefits of vaccination [20,21].
Research gaps remain on parents’ decision making related to vaccinating themselves and their children. In a nationally-representative survey with 500 parents, Flood et al. (2010) examined factors influencing parents’ decisions regarding influenza vaccination for their children. Parents were asked to measure the degree to which they agreed with statements related to vaccination, elaborating on motivations and barriers that supported their choices. A high likelihood of vaccination was associated with a greater perceived risk of influenza and lower concerns regarding vaccine efficacy and side effects [23]. Thus, increasing perceived risk of influenza while mitigating barriers to receiving the vaccine may contribute to increased influenza vaccine uptake among parents and their children. Tang et al. (2016) recruited 245 parents who responded to hypothetical scenarios describing fatal influenza strains and indicated whether they would accept an influenza vaccine, which carried a small risk of death, for themselves or on behalf of their child. Parents were more likely to vaccinate their children than themselves [24], suggesting differences in perceived risk to their children vs. themselves when deciding to adopt health behaviors, consistent with previous research [25].
Given that parental decision-making is key in childhood vaccination uptake, there is a critical need to understand reasons why parents fail to vaccinate their children. To date, no studies have examined the relation between parental decisions to vaccinate their children and their own vaccination status using classification and regression tree (CART) analyses. Classification trees are useful in assessing the potentially complex interactions among the multitude of variables that may influence vaccine decision-making, which may be difficult to capture adequately with logistic regressions. Moreover, trees provide a visual profile of these potential drivers of influenza vaccination for children given parental vaccination status. Understanding the factors that influence parents’ decisions to vaccinate their children could provide insight for provider approaches to increase influenza vaccination. Therefore, this study aims to (1) explore predictors of children’s influenza vaccine status given parental vaccination status and (2) examine the factors that contribute to concordance or discordance between parental and children’s vaccine receipt.
Methods
Study population and data collection
Data were collected in a national survey, administered online from March to April 2015. We contracted with The GfK Group, which utilized its KnowledgePanel, a probability-based web panel representative of the non-Hispanic Blacks and Whites in the US. The purpose of inclusion of these two groups in our overall study was specifically to examine significant and persistent disparities between Black and White adults, and secondly, to enable us to have adequate sample sizes to allow for within-group analyses. The final sample consisted of 819 non-Hispanic Black and 838 non-Hispanic White, non-institutionalized adults >18 years old. Participants received $5 cash equivalent incentive upon survey completion. Survey items were informed by extensive qualitative research [26]. All materials and procedures were approved by the institutional review board at the University of Maryland.
Measures
Survey items assessed vaccine behavior among parents and their children, and both influenza specific and general vaccine constructs such as general vaccine hesitancy [48], general trust in vaccines, perceived risk of the disease and risk of vaccine side effects, influenza knowledge, knowledge of recommendations for the influenza vaccine, and the importance of doctor recommendation of vaccination in general [26]. The 3 C’s of complacency (perceived necessity and importance of the influenza vaccine), confidence (perceived influenza vaccine safety and effectiveness), and convenience (perceived convenience and affordability of influenza vaccine) were also included [47, 48]. Table 1 includes detailed descriptions of measures and corresponding reliability and response scales.
Table 1.
Survey measures
| Variable | Type of scale and number of items | Cronbach’s alpha | Question | Response categories |
|---|---|---|---|---|
| Independent variables | ||||
| Hesitancy about recommended vaccines48 | 1 | - | If your doctor recommends a vaccine for you, do you usually get it? | No, I don’t take any vaccines (1) – Yes, always (3) |
| Importance of doctor recommendation of influenza vaccine | 1 | - | How important are the following in determining whether or not you get a flu vaccination: What my healthcare provider recommends? | Not at all important (1) – Extremely important (4) |
| Hesitancy on intent to get recommended vaccines | 1 | - | For any of these vaccines that you haven’t taken, if your doctor recommended it for you tomorrow, how likely would you be to get it? | Not at all likely (1) – Certain I would (4) |
| Trust in doctor | 1 | - | How much do you trust your own personal doctor when it comes to flu vaccines? | Not at all (1) –Completely (5) |
| Trust in Influenza vaccine | 1 | - | Overall, how much do you trust the flu vaccine? | Not at all (1) – Completely (5) |
| Trust in vaccines | 1 | - | In general, how much do you trust vaccines? | Not at all (1) –Completely (5) |
| Vaccine hesitancy | 1 | - | Overall, how hesitant are you | Not at all hesitant (1) –about getting Very hesitant vaccinations? (4) |
| Influenza knowledge | Count of # truefalse statements correct (7) | - | 1. The flu vaccine helps stimulate a natural immune response? 2. A flu vaccine will protect you from the flu for many years? 3. The flu vaccine does not include all the types of flu circulating in the US this year? 4. Flu vaccines must be tested and approved every year? 5. Flu vaccines change every year because the type of flu virus change all the time? 6. Even if the flu vaccine does not contain all types of virus going around, it can still help reduce the seriousness and length of time I am sick if I get the flu? 7. The flu vaccine this year is less effective than most years? |
True or false |
| Knowledge of influenza vaccine recommendations (children under 18 years old) | Count of # correct statements (3) | - | Based on what you have heard, which of the following groups should get a flu vaccination? | Have not heard/Not sure (0) – Should get the vaccine (1) |
| Knowledge of influenza vaccine recommendations (adults over 18 years old) | 1 | - | Based on what you have heard, which of the following groups should get a flu vaccination? | Should get the vaccine (1) – Have not heard/Not sure (3) |
| Risk of disease | Mean of 4 items | 0.836 | 1. How likely are you to get the flu? 2. How severe do you think the flu would be? 3. How much would you worry about the flu? 4. How much regret do you think you would feel if you did get the flu? |
Not at all (0) –A great deal (3) |
| Vaccine risk | Mean of 4 items | 0.842 | 1. How likely are you to have side effects of the vaccine? 2. How severe do you think the side effects would be? 3. How much would you worry about side effects? 4. How much regret do you think you would feel if you did have side effects? |
Not at all (0) –A great deal (3) |
| Influenza vaccine complacency (necessity and importance) | Mean of 2 items | 0.918 | 1. Thinking specifically about the flu vaccine, do you think the flu vaccine is necessary? 2. Thinking specifically about the flu vaccine, do you think the flu vaccine is important? |
Not at all (1) –Very much (4) |
| Influenza vaccine confidence (safety and effectiveness) | Mean of 2 items | 0.875 | 1. Thinking specifically about the flu vaccine, do you think the flu vaccine is safe? 2. Thinking specifically about the flu vaccine, do you think the flu vaccine is effective? |
Not at all (1) –Very much (4) |
| Influenza vaccine convenience (affordability and convenience) | Mean of 2 items | 0.598 | 1. Thinking specifically about the flu vaccine, do you think the flu vaccine is convenient? 2. Thinking specifically about the flu vaccine, do you think the flu vaccine is affordable? |
Not at all (1) –Very much (4) |
| Parental vaccination status | 1 | - | Did you get a flu vaccine this season? | No or Yes (0 or 1) |
| Outcome variable | ||||
| Children vaccination status | 1 | - | Did you get some, all, or none of your kids vaccinated for flu this season? | No or Yes all/some (0 or 1) |
Statistical Analysis
Analyses were restricted to parents who reported their children’s vaccination status (n=328). To determine which sociodemographic and vaccine-related variables were most predictive of parents’ decision to vaccinate their children against influenza, we applied classification and regression tree (CART) analysis [27], both for vaccinated and non-vaccinated parents. The CART approach, also known as recursive partitioning [28], divides the entire sample (the initial parent node) into smaller, homogeneous groups (child nodes) based on the dependent variable. This approach identifies the predictor variable that best splits data into homogeneous subgroups most relevant to the outcome of interest (child vaccination status) at each partition. This process is repeated until the sample cannot be further divided into homogenous groups or the number of pre-determined partitions are reached (i.e., using stopping rules or pruning), resulting in a classification tree, also known as a decision tree. Each node (data subset resulting from a split) corresponds to a set of decisions related to the outcome variable.
CART analysis was conducted using SPSS (version 25.0) software (IBM, Chicago, IL). The Gini impurity function was used for the categorical outcome variable (children’s receipt of influenza vaccination), selecting the split that has the largest difference between the impurity (variability in the dependent variable) of the overall sample and a weighted average of the impurity of the subgroups [28]. The overall sample splits into subgroups that are statistically significantly purer (i.e., more homogeneous) and more relevant in terms of the outcome variable. The splitting of the sample is based on variable responses; data are split by optimum cut points for continuous variables (e.g., risk of disease) and by categories for categorical variables (e.g., race/ethnicity). Stopping rules and pruning techniques were employed to grow the decision tree to an appropriate and manageable size, as used in other studies [28,29]. We defined the minimum number of individuals in the subgroup nodes to be 5% of the entire sample to avoid unstable group sizes that are too small to be interpretable. Pruning was used to ensure that remaining nodes are statistically meaningful and interpretable by controlling the size of the final tree. Large trees with multiple nodes but small subgroup sizes due to overfitting tend to be less generalizable and lose predictive power [30]. To avoid such over-fitting, but also avoid underfitting (i.e., growing too small of a tree and losing relations between predictors and the outcome variable), the typical pruning criterion of one standard error (SE) was employed [27,28].
Two separate trees were developed to profile parents’ decision whether to vaccinate their children against influenza, one tree for parents who vaccinated themselves and one for parents who did not vaccinate themselves. Both trees incorporated sociodemographic factors and vaccine-related measures to determine the best combination of contributing factors to concordance or discordance regarding parental vaccination decisions for themselves and their children.
Results
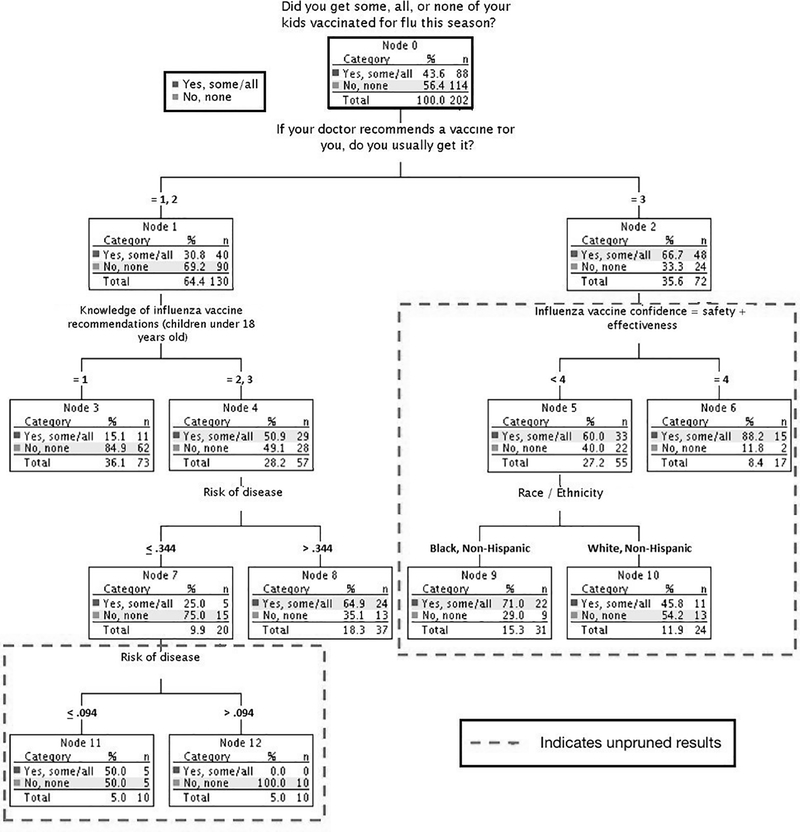
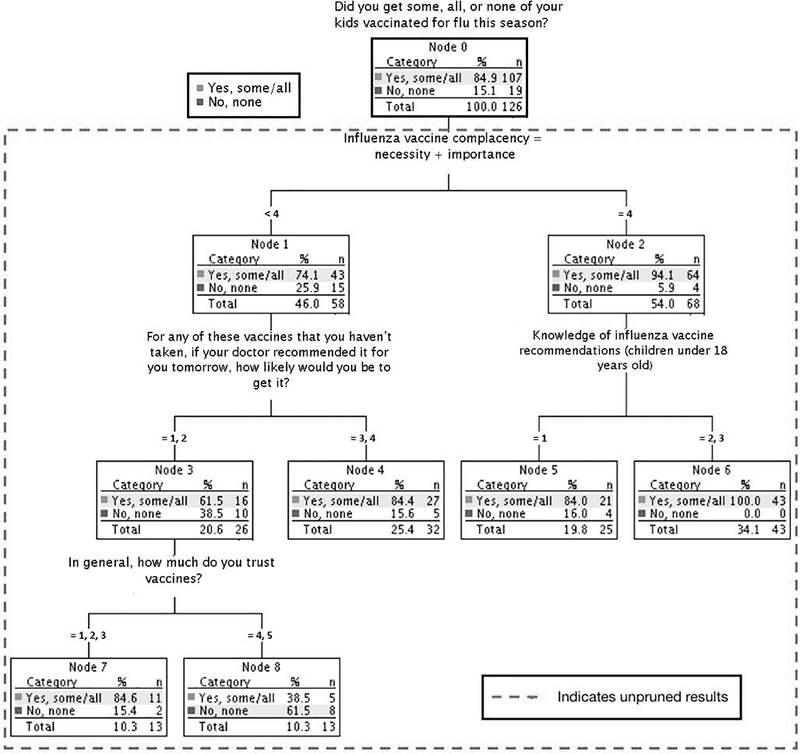
Of the 328 parents, 61.6% (n=202) had received the influenza vaccine and 38.4% (n=126) had not (Table 2). Among parents, 32.6% had vaccinated both themselves and their children, 34.8% had not vaccinated either themselves or their children, 26.8% had vaccinated their children but not themselves, and 5.8% vaccinated themselves but not their children. Pruned results are shown within the larger unpruned trees (Figure 1 for unvaccinated parents; Figure 2 for vaccinated parents). Because the larger unpruned results are generally less stable and generalizable, they will be treated as exploratory and potentially suggestive.
Table 2.
Sample demographics and flu vaccination behavior
| Vaccinated Parents (n=126) | Unvaccinated Parents (n=202) | |
|---|---|---|
| Children vaccination status | ||
| Some/all children received flu vaccination | 84.9% | 43.6% |
| Children did not receive flu vaccination | 15.1% | 56.4% |
| Sex | ||
| Female | 59.5% | 58.4% |
| Male | 40.5% | 41.6% |
| Age | ||
| 18–29 | 16.7% | 20.3% |
| 30–44 | 53.2% | 55.0% |
| 45–59 | 25.4% | 21.8% |
| 60+ | 4.8% | 3.0% |
| Race/ethnicity | ||
| Non-Hispanic Black | 51.6% | 57.4% |
| Non-Hispanic White | 48.4% | 42.6% |
| Education | ||
| Less than high school | 10.3% | 5.9% |
| High school | 19.8% | 27.7% |
| Some college | 31.0% | 31.7% |
| Bachelor’s degree or higher | 38.9% | 34.7% |
| Income | ||
| $24,999 or less | 22.2% | 25.7% |
| $25,000 to $49,999 | 18.3% | 20.3% |
| $50,000 to $74,999 | 19.8% | 18.8% |
| $75,000 and above | 39.7% | 35.1% |
| Health Insurance coverage | ||
| Covered | 87.3% | 82.2% |
| Not covered/unsure | 11.1% | 16.3% |
Figure 1. Unpruned and pruned classification tree for children’s vaccination receipt among unvaccinated parents.a.
a Unpruned results indicate findings that have not been subjected to the stopping rule of one standard error.
Figure 2. Unpruned and pruned classification tree for children’s vaccination receipt among vaccinated parentsa.
a Unpruned results indicate findings that have not been subjected to the stopping rule of one standard error.
Unvaccinated parents
Among the 202 unvaccinated parents, 43.6% (n=88) of parents had some or all children vaccinated, while 56.4% (n=114) did not have any children receive the influenza vaccine. After pruning the unvaccinated parents’ tree by one SE (Figure 1), the primary deciding factor for children’s vaccination status was parents’ hesitancy about accepting recommended vaccines in general. Parents who rarely followed doctor recommendations to vaccinate themselves were less likely to vaccinate their children (30.8%), compared to parents who always get vaccinated following a doctor’s recommendation (66.7%). Among the former subgroup, parents with a lower knowledge score of influenza vaccine recommendations (scale response of 1) were less likely to have their children vaccinated (15.1%) compared to parents with a higher score (a scale response of 2 or 3). Within these parents with higher knowledge of influenza vaccine recommendations for children, those with a greater perceived disease risk had a higher likelihood of vaccinating their children (64.9%) compared to those with a lower perceived disease risk (25.0%).
In Figure 1, the unpruned results, which are exploratory and should be interpreted accordingly, included influenza vaccine confidence, risk of disease, and race. Among parents who rarely get vaccinated following doctor recommendations, but have higher knowledge of influenza vaccine recommendations for children, parents with an even lower perceived risk of disease were more likely to have their children vaccinated (50.0%) compared to those with greater perceived disease risk scores (100%). Note, however, that the subgroup size becomes very small (n=10) for both groups; therefore, results need to be interpreted with caution. Groups did not split further for pruned results.
Unpruned results indicated that among parents who always get vaccinated after receiving a physician recommendation for vaccines in general, higher influenza vaccine confidence corresponded with a higher likelihood of vaccinating their children. Among parents with lower influenza vaccine confidence, Black parents were more likely to vaccinate their children compared to White parents. However, these unpruned findings are less generalizable and provides less predictive accuracy compared to pruned results above.
Vaccinated parents
In Figure 2, vaccinated parents were found to be a homogenous group, with no major factors found to statistically significantly contribute to children’s vaccination status. Of these parents, 84.9% (n=107) had some or all children receive the influenza vaccine, while 15.1% (n=10) did not have any children receive the influenza vaccine ─ indicating a high level of concordance between parental decisions to vaccinate themselves and their children.
The unpruned results, while less stable, provide exploratory variables that may contribute to decision-making about children’s vaccination uptake. Parents that perceived the influenza vaccine as less necessary or effective (i.e. were more complacent) and were more hesitant on their intent to get recommended vaccines in general were less likely to have their children vaccinated. Lower influenza complacency and higher levels of knowledge of influenza vaccine recommendations for children were associated with greater rates of childhood vaccination. Surprisingly, parents with lower trust in vaccines in general were more likely to vaccinate their children compared to those with higher levels of general vaccine trust. These findings potentially indicate salient factors that may contribute to vaccination decisions for children. However, given the decreased predictive accuracy of unpruned trees, these results are exploratory in nature and need to be interpreted as such.
Contributing factors of concordance or discordance among unvaccinated parents
Among unvaccinated parents in the pruned results (Figure 1), the greatest concordance (parents and children who were both unvaccinated) was observed among parents who usually do not get vaccinated following physician recommendation of vaccines in general and had lower knowledge of recommendation of influenza vaccination for children, (84.9% of unvaccinated children). The greatest discordance (unvaccinated parents whose children received the influenza vaccine) was observed among a subgroup of parents who always received vaccination following physician recommendations of general vaccines. Higher levels of discordance were also observed among a subset of parents who usually do not get vaccinated following physician recommendation of general vaccines but had greater knowledge of recommendation of influenza vaccination for children, and greater perceived risk of disease.
Similarly, unpruned results suggest higher levels of concordance among parents who usually do not get vaccinated following physician recommendation, had lower knowledge of influenza vaccine recommendations and had a lower perception of disease risk. Factors that contributed to discordance were observed among parents who always received vaccination following physician recommendations and had higher influenza vaccine confidence.
Contributing factors of concordance or discordance among vaccinated parents
Upon pruning, the effect of major factors that contributed to parental decision making for children vaccination among vaccinated parents were attenuated (Figure 2). Exploratory observations in the unpruned trees suggest that among vaccinated parents, less complacent parents with greater knowledge of children’s influenza vaccine recommendations were more likely to have concordance with vaccinating their children. Factors that contributed to discordance (i.e. vaccinated parents who were less likely to have their children vaccinated) were higher influenza complacency, previous general vaccination behavior following physician recommendation, and counterintuitively, greater trust in vaccines in general.
Discussion
This study is the first to use classification trees to identify drivers of parental decisions to vaccinate their children against influenza. For unvaccinated parents, the main factors influencing parents’ decisions to vaccinate their children were hesitancy about recommended vaccines in general, knowledge of influenza vaccine recommendations for children, influenza vaccine confidence, and disease risk, which is consistent with prior research examining drivers of childhood influenza vaccination among parents [31]. Among vaccinated parents, no major factors were found after pruning due to homogeneity of this subgroup. Unpruned results, though less generalizable, suggest potentially modifiable factors that drive decisions to vaccinate children such as influenza vaccine complacency, hesitancy to get recommended vaccines, knowledge of recommendations about influenza vaccine for children, and general vaccine trust. Differences in drivers of childhood vaccination between parental groups highlight unique opportunities to increase uptake by targeting parents based on their vaccination status [49]. Additionally, identifying factors that contribute to discordance between parental and children vaccination statuses (i.e. likelihood of vaccination following physician recommendation of vaccines in general, knowledge of influenza vaccine recommendations, disease risk) may provide insights for developing strategies to increase uptake. Given the homogeneity of vaccinated parents, intervention efforts may have more impact for unvaccinated parents.
Consistent with the prior studies [19,23,32], the role of physician recommendation is among the primary reasons for parents in our sample who chose to vaccinate their children [36,37] with parents who always get vaccinated following a doctor’s recommendation of vaccines in general being more likely to vaccinate their children (66.7%), compared to those who do not follow recommendations (30.8%). We know that beliefs of health care providers may be influential in parental decisions to accept vaccination, as patients trust physicians as credible sources of health information [18,33,34]. Mergler et al. (2013) found a strong association between parental and HCP beliefs regarding risk and benefits of vaccination [35]. Providers are also essential in relaying influenza vaccine confidence (i.e. safety and effectiveness), another key driver identified in our results.
Increased perception of disease risk and knowledge of recommendations of the influenza vaccine for children drove uptake. Results indicate that parents with a lower knowledge of influenza vaccine recommendations for children were less likely to have their children vaccinated (15.1%) compared to parents with higher knowledge. Findings are consistent with previous research reporting parents who lack knowledge are more likely to have negative attitudes toward vaccines [31,38,39]. As parents weigh the costs and benefits of vaccination, HCPs can acknowledge parental concerns by underscoring disease risk and addressing knowledge gaps, including about recommendations. Hilyard et al. found that the combination of emphasis on disease risk, acknowledgement of the comparatively smaller vaccine risks and focus on cues to action (e.g. modeling of vaccine acceptance) may improve vaccine uptake [4].
There are several strengths of our study. First, we utilized a novel approach to examine predictors of influenza vaccination uptake based on parental vaccination status. Using classification trees allows us to visualize the interactive and hierarchical nature of predictors in ways that traditional methods such as logistic regressions do not [28,41]. Further, tree-based models are useful in identifying segments of populations toward which to target efforts to increase vaccination. Our results indicated modifiable factors related to vaccine uptake (e.g. knowledge of influenza recommendation), were more salient than non-modifiable factors (e.g. age). These factors lend themselves to targeted and tailored communication approaches to increase vaccine uptake among different groups of parents.
Findings need to be considered with limitations of our cross-sectional study. Although our final sample size was 328, our sample derived from a nationally representative sample of African Americans and Whites. Given the current lack of research on parental decision making related to vaccinating themselves and their children, our study suggest future research opportunities that can inform development of approaches to increase influenza vaccine uptake for children.
Secondly, we examined vaccine behavior among parents and children at one time point. However, the literature has demonstrated that prior vaccination status is a predictor of vaccine uptake [42–44]. We would call for future studies, longitudinal in nature, to examine past parental decision-making about children’s vaccination and how that may inform future behavior. If additional research confirms findings from our exploratory study, results can provide opportunities to develop and test interventions to increase uptake.
Given today’s atmosphere of concerns about vaccines and vaccine hesitancy, HCP could benefit from new communication strategies that focus on increasing parental knowledge of influenza vaccine recommendation for children and enhance their ability to help parents weigh the risks and benefits of vaccination. Future research could examine the feasibility and effectiveness of Broniatowski et al.’s proposed ‘gist’ communication framework [40] for HCP working with parents. The framework combines factual evidence with the use of a linking phrase such as “so, the reason that is important is… the thing to remember is…”, and fosters an underlying gist or a bottom-line meaning. In the context of parental decision-making, addressing perceived risk and trust in the vaccine itself and fostering knowledge about the vaccination recommendations for children is essential. To do so, HCP can use gist to communicate about influenza risks, coupled with a linking phrase that addresses risk of vaccine side effects. For example, addressing both types of perceived risk could sound like this, “We know that the flu vaccine is approved annually and safe, with only minor side effects for few people. The reason that is important is that flu can be dangerous for children and the CDC recommends that children over 6 months be vaccinated. I strongly recommend you have your child vaccinated today” (p. 3227). When gist is coupled with an offer to give the vaccine at that same encounter, we believe it can facilitate comprehension, trust and vaccine uptake.
While we examined multiple vaccine-related variables, hesitancy about recommended vaccines, was intentionally broader and not influenza specific. However, our flu vaccine specific scales (complacency, confidence, convenience) measure specific aspects from the vaccine hesitancy and confidence literature and provide useful data, which could inform future research examining influenza-specific vaccination recommendations and strategies on providing effective messages from HCPs [45,46,48].
Conclusion
Predictors of children’s influenza vaccination varied between vaccinated and unvaccinated parents, highlighting the importance of utilizing different approaches for the two groups to promote vaccination for children. These factors emphasize a critical need to strengthen public health communication in relaying the risks of influenza and the benefits of vaccination to reduce preventable influenza-related illness among children.
Acknowledgments
Funding Source: This study was funded by the Center of Excellence in Race, Ethnicity and Health Disparities Research (NIH-NIMHD: P20MD006737; PIs, Quinn and Thomas).
Abbreviations
- CART
Classification and regression tree analysis
- CAM
Complementary and alternative medicine
- CDC
Centers for Disease Control and Prevention
- HCP
Health care providers
Footnotes
Conflict of Interest: The authors have indicated they have no potential conflicts of interest to disclose.
Financial Disclosure Statement: The authors have indicated they have no financial relationships relevant to this article to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Shang M, Blanton L, Brammer L, Olsen SJ, Fry AM. Influenza-Associated Pediatric Deaths in the United States, 2010–2016. Pediatrics. 2018;141(4):e20172918. doi: 10.1542/peds.2017-2918 [DOI] [PubMed] [Google Scholar]
- 2.Garten R, Blanton L, Elal AIA, et al. Update: Influenza Activity in the United States During the 2017–18 Season and Composition of the 2018–19 Influenza Vaccine. MMWR Morb Mortal Wkly Rep. 2018;67(22):634–642. Published 2018 Jun 8. doi: 10.15585/mmwr.mm6722a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.The Centers for Disease Control and Prevention. Estimates of Flu Vaccination Coverage among Children — United States, 2017–18 Flu Season. 2018. Retrieved from: https://www.cdc.gov/flu/fluvaxview/coverage-1718estimates.htm
- 4.Hilyard KM, Quinn SC, Kim KH, Musa D, Freimuth VS. Determinants of Parental Acceptance of the H1N1 Vaccine. Health Educ Behav. 2014;41(3):307–314. doi: 10.1177/1090198113515244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Imburgia TM, Hendrix KS, Donahue KL, Sturm LA, Zimet GD. Predictors of influenza vaccination in the U.S. among children 9–13years of age. Vaccine. 2017;35(18):2338–2342. doi: 10.1016/j.vaccine.2017.03.060 [DOI] [PubMed] [Google Scholar]
- 6.Allison MA, Reyes M, Young P, et al. Parental attitudes about influenza immunization and school-based immunization for school-aged children. Pediatr Infect Dis J. 2010;29(8):751–755. doi: 10.1097/INF.0b013e3181d8562c [DOI] [PubMed] [Google Scholar]
- 7.Brunson EK. How parents make decisions about their children’s vaccinations. Vaccine. 2013;31(46):5466–5470. doi: 10.1016/j.vaccine.2013.08.104 [DOI] [PubMed] [Google Scholar]
- 8.Chen M-F, Wang R-H, Schneider JK, et al. Using the Health Belief Model to Understand Caregiver Factors Influencing Childhood Influenza Vaccinations. Journal of Community Health Nursing. 2011;28(1):29–40. doi: 10.1080/07370016.2011.539087 [DOI] [PubMed] [Google Scholar]
- 9.Gust DA, Darling N, Kennedy A, Schwartz B. Parents With Doubts About Vaccines: Which Vaccines and Reasons Why. Pediatrics. 2008;122(4):718–725. doi: 10.1542/peds.2007-0538 [DOI] [PubMed] [Google Scholar]
- 10.Smith LE, Webster RK, Weinman J, Amlôt R, Yiend J, Rubin GJ. Psychological factors associated with uptake of the childhood influenza vaccine and perception of post-vaccination side-effects: A cross-sectional survey in England. Vaccine. 2017;35(15):1936–1945. doi: 10.1016/j.vaccine.2017.02.031 [DOI] [PubMed] [Google Scholar]
- 11.Dubé E, Laberge C, Guay M, Bramadat P, Roy R, Bettinger JA. Vaccine hesitancy. Hum Vaccin Immunother. 2013;9(8):1763–1773. doi: 10.4161/hv.24657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Paterson P, Chantler T, Larson HJ. Reasons for non-vaccination: Parental vaccine hesitancy and the childhood influenza vaccination school pilot programme in England. Vaccine. 2018;36(36):5397–5401. doi: 10.1016/j.vaccine.2017.08.016 [DOI] [PubMed] [Google Scholar]
- 13.Brown KF, Kroll JS, Hudson MJ, et al. Omission bias and vaccine rejection by parents of healthy children: Implications for the influenza A/H1N1 vaccination programme. Vaccine. 2010;28(25):4181–4185. doi: 10.1016/j.vaccine.2010.04.012 [DOI] [PubMed] [Google Scholar]
- 14.Kennedy A, Basket M, Sheedy K. Vaccine attitudes, concerns, and information sources reported by parents of young children: results from the 2009 HealthStyles survey. Pediatrics. 2011;127 Suppl 1:S92–99. doi: 10.1542/peds.2010-1722N [DOI] [PubMed] [Google Scholar]
- 15.Poland GA, Jacobson RM. The clinician’s guide to the anti-vaccinationists’ galaxy. Human Immunology. 2012;73(8):859–866. doi: 10.1016/j.humimm.2012.03.014 [DOI] [PubMed] [Google Scholar]
- 16.Bleser WK, Elewonibi BR, Miranda PY, BeLue R. Complementary and Alternative Medicine and Influenza Vaccine Uptake in US Children. Pediatrics. 2016;138(5):e20154664. doi: 10.1542/peds.2015-4664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dubé E, Vivion M, Sauvageau C, Gagneur A, Gagnon R, Guay M. “Nature Does Things Well, Why Should We Interfere?”: Vaccine Hesitancy Among Mothers. Qual Health Res. 2016;26(3):411–425. doi: 10.1177/1049732315573207 [DOI] [PubMed] [Google Scholar]
- 18.Jamison AM, Quinn SC, Freimuth VS. “You don’t trust a government vaccine”: Narratives of institutional trust and influenza vaccination among African American and white adults. Soc Sci Med. 2019;221:87–94. doi: 10.1016/j.socscimed.2018.12.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Malosh R, Ohmit SE, Petrie JG, Thompson MG, Aiello AE, Monto AS. Factors associated with influenza vaccine receipt in community dwelling adults and their children. Vaccine. 2014;32(16):1841–1847. doi: 10.1016/j.vaccine.2014.01.075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bhat-Schelbert K, Lin CJ, Matambanadzo A, Hannibal K, Nowalk MP, Zimmerman RK. Barriers to and facilitators of child influenza vaccine - perspectives from parents, teens, marketing and healthcare professionals. Vaccine. 2012;30(14):2448–2452. doi: 10.1016/j.vaccine.2012.01.049 [DOI] [PubMed] [Google Scholar]
- 21.Kata A A postmodern Pandora’s box: Anti-vaccination misinformation on the Internet. Vaccine. 2010;28(7):1709–1716. doi: 10.1016/j.vaccine.2009.12.022 [DOI] [PubMed] [Google Scholar]
- 22.Schmid P, Rauber D, Betsch C, Lidolt G, Denker M-L. Barriers of Influenza Vaccination Intention and Behavior – A Systematic Review of Influenza Vaccine Hesitancy, 2005 – 2016. PLoS One. 2017;12(1). doi: 10.1371/journal.pone.0170550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Flood EM, Rousculp MD, Ryan KJ, et al. Parents’ decision-making regarding vaccinating their children against influenza: A web-based survey. Clinical Therapeutics. 2010;32(8):1448–1467. doi: 10.1016/j.clinthera.2010.06.020 [DOI] [PubMed] [Google Scholar]
- 24.Tang MY, Shahab L, Robb KA, Gardner B. Are parents more willing to vaccinate their children than themselves? Journal of Health Psychology. 2016;21(5):781–787. doi: 10.1177/1359105314539527 [DOI] [PubMed] [Google Scholar]
- 25.Dore RA, Stone ER, Buchanan CM. A Social Values Analysis of Parental Decision Making. The Journal of Psychology. 2014;148(4):477–504. doi: 10.1080/00223980.2013.808603 [DOI] [PubMed] [Google Scholar]
- 26.Quinn SC, Jamison A, Freimuth VS, An J, Hancock GR, Musa D. Exploring racial influences on flu vaccine attitudes and behavior: Results of a national survey of White and African American adults. Vaccine. 2017;35(8):1167–1174. doi: 10.1016/j.vaccine.2016.12.046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Breiman L, Friedman J, Olshen R, & Stone C Classification and Regression Trees. 1984. Monterey, California: Wadsworth. [Google Scholar]
- 28.Lemon SC, Roy J, Clark MA, Friedmann PD, Rakowski W. Classification and regression tree analysis in public health: Methodological review and comparison with logistic regression. ann behav med. 2003;26(3):172–181. doi: 10.1207/S15324796ABM2603_02 [DOI] [PubMed] [Google Scholar]
- 29.Frisman L, Prendergast M, Lin H-J, Rodis E, Greenwell L. Applying classification and regression tree analysis to identify prisoners with high HIV risk behaviors. J Psychoactive Drugs. 2008;40(4):447–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Crawley MJ. The R Book. John Wiley & Sons; 2012. [Google Scholar]
- 31.Smith LE, Amlôt R, Weinman J, Yiend J, Rubin GJ. A systematic review of factors affecting vaccine uptake in young children. Vaccine. 2017;35(45):6059–6069. doi: 10.1016/j.vaccine.2017.09.046 [DOI] [PubMed] [Google Scholar]
- 32.Hofstetter AM, Robinson JD, Lepere K, Cunningham M, Etsekson N, Opel DJ. Clinicianparent discussions about influenza vaccination of children and their association with vaccine acceptance. Vaccine. 2017;35(20):2709–2715. doi: 10.1016/j.vaccine.2017.03.077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Freed GL, Clark SJ, Butchart AT, Singer DC, Davis MM. Sources and Perceived Credibility of Vaccine-Safety Information for Parents. Pediatrics. 2011;127(Supplement 1):S107–S112. doi: 10.1542/peds.2010-1722P [DOI] [PubMed] [Google Scholar]
- 34.Freimuth VS, Jamison AM, An J, Hancock GR, Quinn SC. Determinants of trust in the flu vaccine for African Americans and Whites. Social Science & Medicine. 2017;193:70–79. doi: 10.1016/j.socscimed.2017.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mergler MJ, Omer SB, Pan WKY, et al. Association of vaccine-related attitudes and beliefs between parents and health care providers. Vaccine. 2013;31(41):4591–4595. doi: 10.1016/j.vaccine.2013.07.039 [DOI] [PubMed] [Google Scholar]
- 36.Byington CL. Vaccines: Can Transparency Increase Confidence and Reduce Hesitancy? Pediatrics. 2014;134(2):377–379. doi: 10.1542/peds.2014-1494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tafuri S, Gallone MS, Cappelli MG, Martinelli D, Prato R, Germinario C. Addressing the anti-vaccination movement and the role of HCWs. Vaccine; Kidlington. 2014;32(38):4860–4865. doi: 10.1016/j.vaccine.2013.11.006 [DOI] [PubMed] [Google Scholar]
- 38.Gust D, Brown C, Sheedy K, Hibbs B, Weaver D, Nowak G. Immunization Attitudes and Beliefs Among Parents: Beyond a Dichotomous Perspective. American Journal of Health Behavior. 2005;29(1):81–92. doi: 10.5993/AJHB.29.1.7 [DOI] [PubMed] [Google Scholar]
- 39.Lau JT, Mo PK, Cai YS, Tsui HY, Choi KC. Coverage and parental perceptions of influenza vaccination among parents of children aged 6 to 23 months in Hong Kong. BMC Public Health. 2013;13(1):1026. doi: 10.1186/1471-2458-13-1026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Broniatowski DA, Hilyard KM, Dredze M. Effective vaccine communication during the disneyland measles outbreak. Vaccine. 2016;34(28):3225–3228. doi: 10.1016/j.vaccine.2016.04.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kuhn L, Page K, Ward J, Worrall-Carter L. The process and utility of classification and regression tree methodology in nursing research. J Adv Nurs. 2014;70(6):1276–1286. doi: 10.1111/jan.12288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Liu S, Yuan H, Liu Y, et al. Attitudes of seasonal influenza vaccination among healthcare worker and general community population after pandemic influenza A/H1N1 in Hangzhou. Human Vaccines. 2011;7(10):1072–1076. doi: 10.4161/hv.7.10.16781 [DOI] [PubMed] [Google Scholar]
- 43.Marentette T, El-Masri MM. Predicting seasonal influenza vaccination among hospital-based nurses. Clin Nurs Res. 2011;20(4):422–438. doi: 10.1177/1054773811409032 [DOI] [PubMed] [Google Scholar]
- 44.Offutt-Powell TN, Ojha RP, Qualls-Hampton R, Stonecipher S, Singh KP, Cardarelli KM. Parental risk perception and influenza vaccination of children in daycare centres. Epidemiol Infect. 2014;142(1):134–141. doi: 10.1017/S0950268813000782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Leask J, Kinnersley P, Jackson C, Cheater F, Bedford H, Rowles G. Communicating with parents about vaccination: a framework for health professionals. BMC Pediatrics. 2012;12(1):154. doi: 10.1186/1471-2431-12-154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Opel DJ, Heritage J, Taylor JA, et al. The Architecture of Provider-Parent Vaccine Discussions at Health Supervision Visits. Pediatrics. 2013;132(6):1037–1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.MacDonald NE. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015;33(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036 [DOI] [PubMed] [Google Scholar]
- 48.Quinn SC, Jamison AM, An J, Hancock GR, Freimuth VS. Measuring vaccine hesitancy, confidence, trust and flu vaccine uptake: Results of a national survey of White and African American adults. Vaccine. 2019;37(9):1168–1173. doi: 10.1016/j.vaccine.2019.01.033 [DOI] [PubMed] [Google Scholar]
- 49.Robison SG, Osborn AW. The Concordance of Parent and Child Immunization. Pediatrics. 2017;139(5):e20162883. doi: 10.1542/peds.2016-2883 [DOI] [PubMed] [Google Scholar]