Abstract
Objective
To perform a standardized review of available mobile health (mHealth) applications (apps) for systemic lupus erythematosus (SLE) and to conduct a systematic review of the literature on mHealth technologies in SLE.
Methods
Google Play and AppStore in the United States of America were queried and the quality of eligible mHealth apps was assessed using the Mobile App Rating Scale (MARS). Web of Science, EMBASE, Medline, and Cochrane databases were systematically searched from inception through June 2019.
Results
Of 324 mHealth apps found, 20 were eligible for inclusion. Ten focused on education, seven offered tools to track patient-reported symptoms, five included interactive online communities, and one enabled emoji sharing. The reviewed apps scored poorly on the MARS quality scale with a mean score 2.3 (0.6) out of 5. Of 1147 studies identified in the literature review, 21 were eligible for inclusion. Eleven studies (52.4%) focused on the development and use of mHealth for providing patient information, while only two (9.5%) were randomized trials of mHealth interventions.
Conclusions
Although there is growing interest in the development of mHealth technologies to support SLE patients, currently available tools are of poor quality and limited functionality, and the literature examining this area is sparse.
INTRODUCTION
Systemic lupus erythematosus (SLE) is a chronic multisystem autoimmune disease accompanied by substantial physical, psychological, and functional disabilities.1,2 SLE is associated with a significant economic burden on individuals and society with estimated direct costs ranging from $33,000 to more than $70,000 dollars per patient annually.1 Current clinical practice guidelines for the management of SLE recommend a combination of pharmacological and non-pharmacological treatment strategies administered by a multidisciplinary team, but treatment options remain limited and poorly tolerated, with frequent toxicities and low medication adherence.1,3–5 Treatment goals include survival, prevention of organ damage and disease flares, and optimization of health-related quality of life.6,7 Strategies to improve SLE patient outcomes such as patient education, peer support, and close monitoring of disease activity can reduce the risk of flares and improve quality of life.7,8
The use of mobile technologies to support health (mHealth technologies), specifically mHealth applications (apps), has the potential to improve outcomes in SLE by empowering patients through education, symptom tracking, and peer support.9–11 mHealth apps can offer numerous functionalities for disease management including home based exercise programs, symptom trackers, medication diaries, educational information, and movement analysis.11 These may be particularly powerful tools in SLE which commonly affects young adults, who are typically avid smartphone users familiar with the use of mobile apps.2,12,13 In addition to directly helping patients monitor and manage their health, mHealth apps can facilitate clinical research by enabling investigators to collect patient outcomes more reliably and precisely through remote longitudinal data tracking.11,14 As a result, there is significant interest in the development and use of mHealth apps among SLE patients, clinicians, and clinical investigators alike.10,15
Understanding the current status of mHealth technologies in SLE, especially the availability and functionality of apps and the literature supporting the use of this technology, is critical to first identifying, and then meeting the needs of this population. To the best of our knowledge, there are no systematic reviews describing mHealth technologies for patients with SLE. Therefore, the aims of this study are: 1) to perform a standardized review of existing mHealth apps for patients with SLE; and 2) to provide a systematic review of the literature on mHealth technologies in SLE. The results of this study will guide the development of more robust patient-centered treatment strategies for SLE, and inform the creation of new technological tools to improve data collection methods for clinical trials.
METHODS
This review was divided into two parts: 1) systematic review of mHealth apps; and 2) systematic review of the literature. For the mHealth app review, we searched two online app stores in the United States of America (USA): AppStore (Apple Inc) and Google Play (Google Inc). For the literature review, we systematically searched Web of Science, EMBASE, Medline, and Cochrane databases according to PRISMA guidelines (Supplementary File 1).16,17
mHealth apps review
We searched for mHealth apps in the USA Google Play Store (Android) and the AppStore (iOS) using an Android device (Motorola Z4, system version Android 9) and an Apple device (iPhone X, system version 12.4) on July 23, 2019. Google Play and AppStore together account for 99.7% of the USA mobile phone market.18 The search terms for both stores included keywords normally used in traditional systematic reviews of SLE: “lupus” and “systemic lupus erythematosus.” No restrictions on app cost were applied.
Apps were included if they were a self-contained product (i.e., did not require add-ons or another type of external device to work). We only included apps in English that were developed or updated in 2017–2019, since updates ensure software functionality and ongoing technical support to the users. We included smartphone apps (1) targeted to SLE, (2) without age restriction, and (3) providing information on at least one of the following recommended strategies for SLE management: education, counseling, or monitoring of patients’ health. Apps advertising a specific clinic or product were excluded.
Unclear app descriptions were discussed between LD and SW to determine inclusion. A third reviewer (SK) was available to adjudicate any disagreements. If the same app was available on both platforms (iOS or Android), the iOS version of the app was used for inclusion and analysis. When both paid and free versions of an app were available, only the paid version was reviewed. If the free app offered additional paid functionalities (in-app purchases), the full content of the app was evaluated. A final list of the included apps was created in an Excel spreadsheet (Microsoft Corp), with metadata about each app extracted from the relevant stores. This included information about the developer, price, app size (in megabytes), app version, and a brief summary of the app contents.
The evaluation of app quality was performed using the 23-item Mobile App Rating Scale (MARS).19 MARS, a validated tool for assessing the quality of apps, is divided into 5 sections: engagement (5 items), functionality (4 items), aesthetics (3 items), information quality (7 items), and subjective app quality scores (4 items). Each of the 23 items is scored using a 5-point scale, with higher scores indicating better quality. An overall mean app quality score was calculated from individual mean scores of engagement, functionality, aesthetics, and information quality. As the subjective quality section of the MARS is optional, it was not included in the analysis in order to strengthen the objectivity of the scale as a measure of app quality.19 A detailed description of each section of the MARS scale is presented in Table 1.
Table 1.
Detailed Mobile App Rating Scale (MARS) sections
| Section | Description |
|---|---|
| Engagement | This section involves characteristics related to entertainment, interest, customization, interactivity, and fit to target group. |
| Functionality | This section involves characteristics related to performance, ease of use, navigation, and gestural design. |
| Aesthetics | This section involves characteristics related to layout, graphics, and visual appeal. |
| Information | This section involves characteristics related to the accuracy of app description, goals, quality of information, quantity of information, visual information, credibility, and evidence base. |
Following MARS recommendations, the two primary reviewers (LD and SW) were trained to use the MARS scale by studying training slides provided by the authors of the scale.19 For further training, ten randomly selected apps within the health & fitness and medical categories of the iOS AppStore were independently assessed by the two reviewers and their scores were compared to evaluate consensus. Any cases of disagreement (>2 point difference in any of the MARS subscale mean scores) were discussed with a third reviewer (SK).19 In addition, the meaning of any MARS items that could be potentially ambiguous was clarified between reviewers. Online user ratings in app stores were not considered in evaluating apps as these can be falsified and may be invalid indicators of app quality.20
Literature review
We searched EMBASE, Web of Science, Medline/PubMed, and the Cochrane Databases from their inception through June 2019. No restriction on language or publication year was applied. To maximize the search results, controlled vocabulary was searched using Medical Subject Headings (MeSH). The strategies used are presented in the Supplementary File 2. We used a web-based screening tool to conduct abstract and full text screening of the references gathered from the literature search (http://rheumatology.tuftsmedicalcenter.org/CTCIA). We manually searched the reference lists of the most recent systematic reviews and reviewed the conference proceedings published up until June 2019. Inclusion criteria were: original research studies including randomized trials, observational, qualitative and survey-based studies, or review articles related to the development or use of mHealth technologies targeting people of all ages with an SLE diagnosis. The term “mHealth technology” was defined as the use of technology for health purposes deployed in a mobile phone, smartphone, tablet, wearable device, or web-related system. Editorials, abstracts, and opinion pieces were excluded.
Two reviewers (LD, MO) independently assessed the title and abstract of each reference to determine potential eligibility. Articles included during this stage were deemed eligible for full text screening. Full manuscripts for eligible abstracts were obtained and examined thoroughly by the same independent reviewers (LD, MO). Any discrepancies during abstract and full text screening were resolved by a third investigator (SK). Quality of the randomized trials were assessed at the study level using the Cochrane Risk of Bias tool.17 We used the Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies.21
RESULTS
mHealth apps review
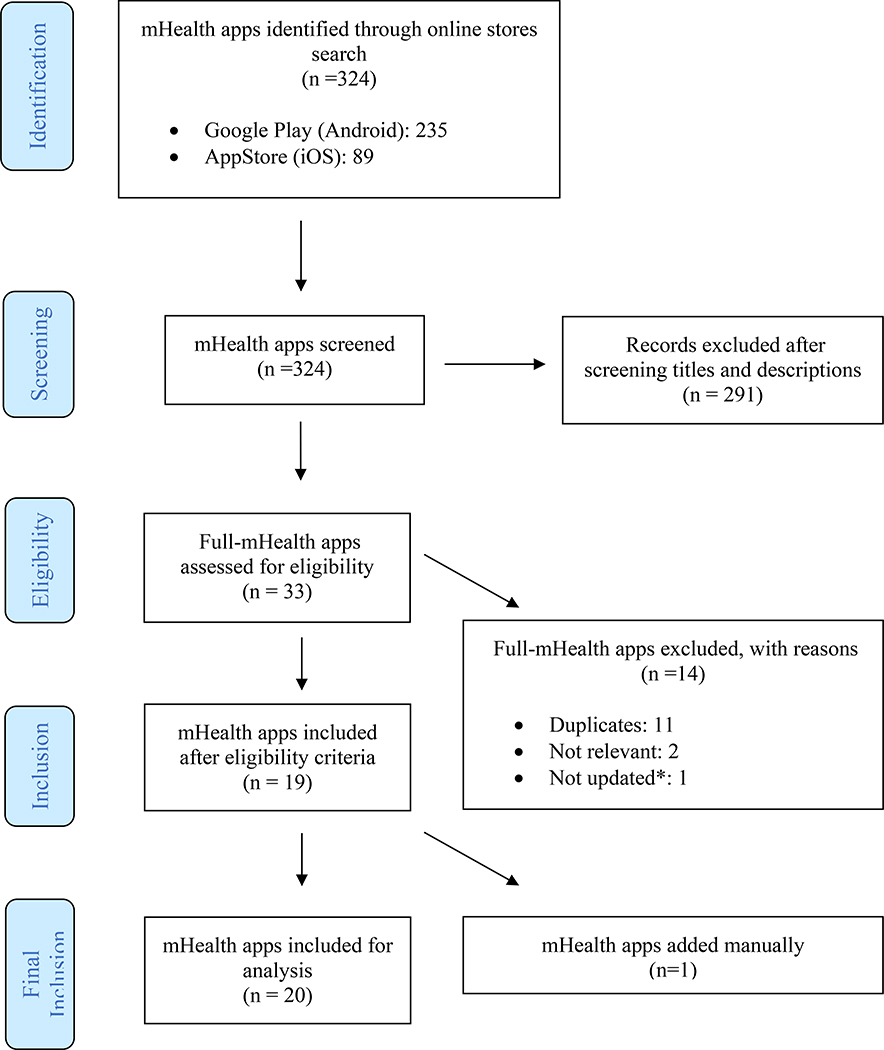
Of the 324 relevant mHealth apps found by our search, only 19 were eligible for inclusion in the analyses (Figure 1). One app (ArthritisPower), which was not found through our search, was included in the study as it was known to the authors to have content of relevance to individuals with SLE. A total of 20 mHealth apps were included in the final analysis. The most common reasons for exclusion were duplicates, apps that were not updated, or apps not relevant to the topic of this review. Of the 20 apps included, one (5%) was found in the AppStore exclusively, six (30%) in Google Play exclusively, and 13 (65%) were found in both Google Play and AppStore. There were three (15%) paid apps, ranging in price from US $0.99 to US $4.99. Only one app offered in-app purchases with 3 package purchases costing US $0.99 each. The detailed characteristics of the included mHealth apps are described in Table 2.
Figure 1.
Flow diagram for mobile health applications (mHealth apps) search results
* To ensure software functionality and ongoing technical support to users, only apps developed or updated in 2017–2019 were included.
Table 2.
Description of included mobile health applications (mHealth apps) for SLE
| App name | Purpose | Platform | Price ($) | Downloads* | Developer | Affiliations |
|---|---|---|---|---|---|---|
| My Lupus Log | Track and monitor patient reported symptoms | iOS and Android | Free | 10,000 + | Glaxo SmithKline PLC | Commercial |
| ArthritisPower | Track and monitor patient reported symptoms | iOS and Android | Free | 5,000 + | Global Healthy Living Foundation | Non-profit |
| Lupus Health Storylines | Track and monitor patient reported symptoms | iOS and Android | Free | 1,000 + | Self-Care Catalysts Inc | Commercial |
| LupusMinder | Track and monitor patient reported symptoms | iOS and Android | Free | 1,000 + | Hospital for Special Surgery | Non-profit |
| Lupie Diary | Track and monitor patient reported symptoms; educational | iOS and Android | Free | 100 + | Syamsi Dhuha Foundation | Commercial |
| Lupus Diary | Track and monitor patient reported symptoms | iOS and Android | $4.99 | 100 + | cellHigh LLC | Commercial |
| Lupus Corner Health Manager | Track and monitor patient reported symptoms; Social network and support group; educational | iOS and Android | Free | 1,000 + | Progentec Diagnostics, Inc | Commercial |
| Lupus Support | Social network and support group | iOS and Android | Free | 10,000 + | MyHealthTeams | Commercial |
| PatientsLikeMe | Social network and support group | iOS and Android | Free | 5,000 + | PatientsLikeMe | Commercial |
| LupusConnect Inspire Community | Social network and support group | iOS and Android | Free | 100+ | Clinica Health Inc | Commercial |
| HealthUnlocked Communities | Social network and support group | iOS | Free | Not provided | EverythingUnlocked Ltd | Commercial |
| Lupus advice | Educational | Android | Free | 1,000 + | moreFlow | Commercial |
| Nutrition Lupus | Educational | iOS and Android | Free | 500 + | Doctors World Ltd | Commercial |
| Home remedies for lupus | Educational | Android | Free | 500 + | Hilltop_apps | Commercial |
| Lupus info | Educational | Android | Free | 500 + | Programing is Fun | Commercial |
| Lupus: Causes, Diagnosis, and Treatment | Educational | Android | Free | 500 + | Health Info | Commercial |
| Yoga vs. Lupus | Educational | Android | Free | 100 + | PhysUp | Commercial |
| How to Cure Lupus | Educational | Android | Free | 50 + | Apps How to Apps | Commercial |
| Lupus (SLE) | Educational | iOS and Android | $3.49 | 50+ | Personal Remedies LLC | Commercial |
| Butterfly Flare | Emoji for entertainment | iOS and Android | $0.99 for iOS, free for Android** | 10+ | The Lupus Liar LLC | Commercial |
Google Play store (Android) only.
Contains in-app purchases.
Of the 20 apps, ten offered educational content, seven offered tools for tracking patient-reported symptoms, five offered interactive online communities, and one offered emojis to share through text messages or electronic mail for the purpose of entertainment. One app did not provide a login screen when prompted, and therefore could not be fully evaluated. This app was excluded from review with MARS and classified in Table 2 with the available information from the online app stores.
MARS scale
The mean (SD) MARS app quality score for the 19 evaluated apps was 2.3 (0.6) on a 0–5 scale. Most apps scored poorly based on design, user interface, functionality, and credibility. The mean MARS engagement subscale score was 2.5 (0.7); the mean MARS functionality subscale score was 2.9 (0.5), with most apps being functional and easy to use; and the mean MARS aesthetics subscale score was 2.2 (0.5), with apps generally presenting unattractive layouts with low-resolution graphics. The majority of the apps provided low-quality information from questionable sources (i.e., sources were not cited or their legitimacy was unknown or unverifiable) and received a mean MARS information subscale score of 1.6 (0.4). Of note, there was high agreement between the two reviewers using the MARS scale, with scores never differing by more than the 2-point threshold established for consensus. Table 3 presents the assessment of the quality of the reviewed apps using the MARS scale.
Table 3.
Mobile App Rating Scale (MARS) mean scores of apps assessed by domains
| App name | Version | MARS Engagement | MARS Functionality | MARS Aesthetics | MARS Information | Overall mean app quality score |
|---|---|---|---|---|---|---|
| LupusMinder | 1.2 a | 3.7 | 4 | 3.5 | 2.2 | 3.3 |
| Lupus Corner Health Manager | 2.0 a | 3.7 | 3.6 | 3.1 | 2.5 | 3.2 |
| PatientsLikeMe | 4.1.2 a | 3.1 | 4 | 3.6 | 1.7 | 3.1 |
| HealthUnlocked Communities | 3.11.0 a | 2.6 | 3.7 | 3.8 | 1.8 | 2.9 |
| My Lupus Log | N/A (July 2019) a | 3.3 | 3.2 | 2.3 | 2.1 | 2.7 |
| Lupus Health Storylines | N/A (July 2019) a | 3.4 | 2.8 | 3 | 1.8 | 2.7 |
| Lupie Diary | 1.0.2 a | 3.1 | 3.1 | 2.3 | 2 | 2.6 |
| LupusConnect Inspire Community | N/A (July 2019) a | 2.8 | 3 | 3 | 1.5 | 2.5 |
| Lupus Support | N/A (July 2019) a | 2.6 | 2.8 | 2.5 | 1.7 | 2.4 |
| Lupus Diary | 1.7.93 a | 3.5 | 3 | 2.1 | 1.3 | 2.4 |
| ArthritisPower | 2.3.0 a | 2.3 | 2.5 | 1.6 | 2.1 | 2.1 |
| Lupus advice | 1.03.7 b | 2.2 | 2.5 | 1.5 | 2.2 | 2.1 |
| Lupus (SLE) | N/A (July 2019) a | 2.3 | 2.8 | 2.1 | 1.4 | 2.1 |
| Lupus: Causes, Diagnosis, and Treatment | 1.0 b | 1.8 | 2.8 | 1.8 | 1.5 | 1.9 |
| How to Cure Lupus | 3.1 b | 2 | 2.7 | 1.5 | 1.1 | 1.8 |
| Home remedies for lupus | 1.0 b | 1.7 | 3 | 1.1 | 1.5 | 1.8 |
| Butterfly Flare | N/A (July 2019) a | 1.8 | 2.8 | 1.6 | 0.8 | 1.7 |
| Lupus info | 1.0 b | 1.6 | 2.7 | 1 | 1.4 | 1.6 |
| Yoga vs. Lupus | 1.0 b | 1.2 | 1.5 | 1 | 0.6 | 1.0 |
| Nutrition Lupus* | 2.0.5 a | - | - | - | - | - |
MARS: Mobile App Rating Scale. Score ranges from 0 to 5, where a score of 0 means inadequate quality and a score of 5 means excellent quality. The total score is based on the average of each subscale.
Version at App Store (iOS)
Version at Google Play (Android)
Not included for assessment since developers did not provide login to access the app.
Highest scoring apps for SLE
The three highest scoring apps for SLE received overall mean app quality scores in the range of 3, indicating moderate overall scores. While all three apps focused on tracking patient-reported outcomes, none of them utilized validated outcome measures. In addition, the apps neither offered connectivity with wearable devices nor incorporated methods of passive data collection such as steps count, walking distances, flights climbed, calories expenditure, or sleep monitoring. Two of them (Lupus Corner Health Manager and PatientsLikeMe) provided social network components and interactive support groups.
All three apps were interactive and customizable with a reasonable level of content and visual appeal. However, none offered features for patients to create and track goals, directly connect with a physician or expert in the field, or synchronize data with electronic health records. None of the apps provided patients with feedback by analyzing data that was collected.
LupusMinder (overall mean app quality score 3.3)
This app was developed with the input of patients with SLE and promotes monitoring and management of lupus by enabling patients to track appointments, medications, and symptoms. Users can rate their symptoms according to a 5-level emoji representation, a 4-level nominal scale, or a 10-point numeric scale. In addition, the app allows users to add notes and pictures to each symptom tracked. Other major functionalities include tracking of appointments and physician information, as well as medication management, and reminders. The app also provides unreferenced information about SLE, frequently asked questions by patients, and links to external SLE websites. In addition, patients can print their log of tracked outcomes to share with health care providers.
Lupus Corner Health Manager (overall mean app quality score 3.2)
This app enables users to track symptoms including pain, fatigue, and ability to plan activities by answering three questions using a 5-level nominal scale. Users can also answer a general question about how they are doing and log side effects experienced. Other major functionalities include appointment tracking and medication logs/reminders. Additionally, users can engage in a community within the app, where they can post questions and receive feedback from other users through comments. The app also provides updated, but unverified information about SLE formatted in articles.
PatientsLikeMe (overall mean app quality score 3.1)
The main purpose of this app is to create an active community where people can post questions and receive feedback from other users about their health conditions through comments or inbox messages. Users can follow other users and send positive feedback through buttons such as “like”, “applause”, and “support”. Other major functionalities include the ability to post pictures, track moods, and answer a standardized monthly questionnaire created by the app developers about the disease and associated symptoms.
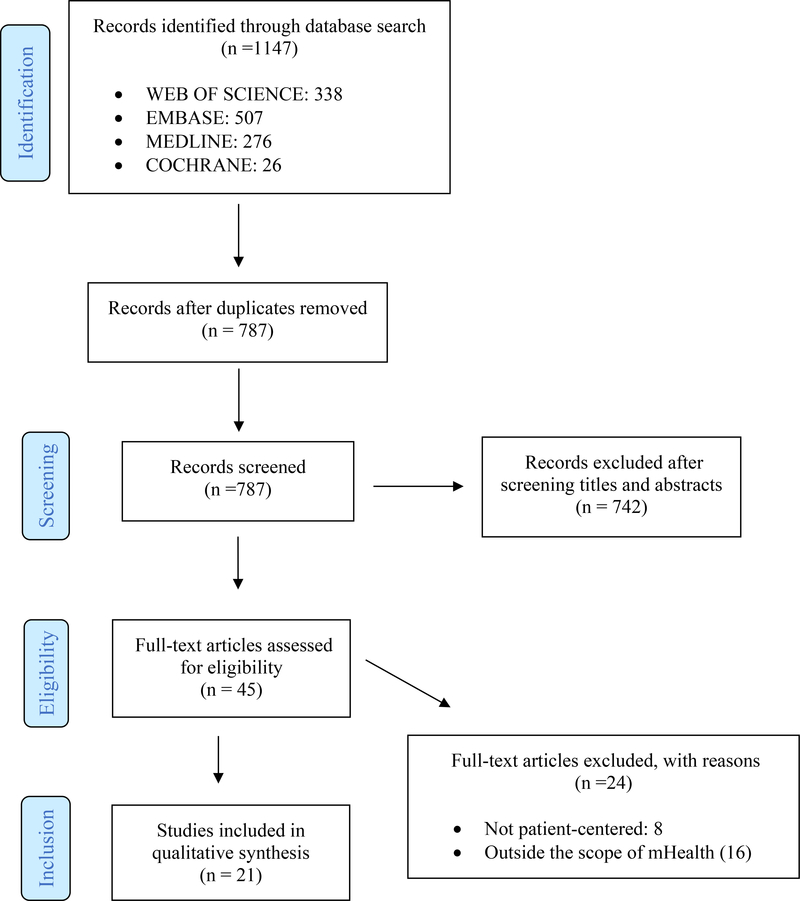
Literature review
Of the 1147 relevant references found in our systematic search, only 21 studies were eligible for inclusion in the final review (Figure 2). The most common reason for exclusion was a focus outside the scope of mHealth. Included studies were published between the years of 2002 and 2018. Of the included studies, 10 (48%) were observational, four (19%) were qualitative, three (14%) were reviews, two (9.5%) were randomized trials, and two (9.5%) were study protocols for future randomized trials.10,22–41 The detailed characteristics of the included studies are described in Table 4.
Figure 2.
Flow diagram for literature search
mHealth = Mobile Health
Table 4.
Characteristics of included studies
| Author & Year | Study Location | Study Design | Category | mHealth intervention | Number of patients | Study Objective | Key Findings |
|---|---|---|---|---|---|---|---|
| Young et al. 39 2002 | Birmingham, UK | Qualitative / Structured Interviews + Surveys | Development - Patient Information | N/A | 16 SLE patient interviews/ questionnaires; 510 SLE patient poststudy questionnaires | To investigate the value of web-based information for SLE patients. | Good quality web- based information located on patient- oriented websites can increase disease knowledge. |
| Mendelson et al. 34 2003 | Albuquerque, USA | Qualitative | Development - Patient Information | N/A | N/A | To examine the type of online support and information provided by three different Internet listservs that cater to lupus patient needs. | Virtual communities such as listservs can be valuable sources of support and information in individuals with chronic diseases. |
| Richter et al.28 2009 | Dusseldorf, Germany | Observational | Development - Patient Information | N/A | 153 (60 SLE patients) | To explore and detect trends in rheumatology patients’ Internet use, expectations, and attitudes in order to optimize a Rheumatology Internet platform. | Rheumatology patients’ high demand of disease and other health-related information should be met with interactive applications and high-quality information online and in routine patient care. |
| Rhee et al. 39 2013 | Philadelphia, USA | Observational | Development - Patient Information | N/A | N/A | To assess patient materials on rheumatologic conditions for readability and suitability. | Most patient education materials are written at higher readability levels than recommended and are only adequately suitable. |
| Tani et al.10 2016 | Pisa, Italy | Review/Persp ective | Development - Patient Information | N/A | N/A | To review literature regarding efficacy of current health information technologies (HIT) in SLE and propose future avenues for research and development. | SLE patient-centered apps suggest a demand for tracking and communicating symptoms and increased self-management. |
| Meunier et al.26 2016 | Marseille, France | Observational | Development - Patient Information | N/A | 112 SLE patients | To compile and assess French SLE patient needs through an online community platform for patients with chronic diseases. | An SLE community interacting through an online platform generated unbiased information that can help improve and target information provision. |
| Sciascia et al.29 2017 | Turin, Italy | Observational | Development - Patient Information | N/A | N/A | To examine trends in SLE-related Internet searches through Big Data monitoring and mining. | Big data trends that factor in media influence can estimate SLE health-related demand and behavior. |
| Reynolds et al.25 2018 | Hobart, Australia | Observational | Development - Patient Information | N/A | N/A | To systematically assess the quality, reliability, and readability of online SLE and lupus information available to patients. | Overall, the studied online health information regarding SLE had fair quality and acceptable readability, but poor reliability. |
| Callejas- Rubio et al.27 2014 | Granada, Spain | Observational | Development - Patient Information | N/A | 150 SLE patients | To analyze online health information searches in SLE patients from southern Spain. | Studied lupus patients frequently utilize the Internet for health- related information, indicating the need for websites with high- quality information. |
| Ting et al. 38 2012 | Cincinnati, USA | RCT | mHealth Intervention | Text Messaging | 41 | To determine efficacy of cellular text messaging reminders (CTMR) in increasing medication and clinical visit adherence among childhood-onset SLE (cSLE) patients. | CTMR was shown to improve visit adherence among adolescents and young adults with cSLE, but did not affect medication adherence. |
| Rimmer et al.37 2013 | Alabama, USA | RCT | mHealth Intervention | Web-based remote coaching tool w/ telephone intervention | 102 (1 SLE patient) | To assess the effect of a 9-month weight management program involving telephone-based coaching and a web- based health promotion program in adults with physical disabilities. | A telehealth weight management program is effective for weight maintenance or reduction in adults with physical disabilities. |
| Sarabi et al.36 2016 | Tehran, Iran | Review | mHealth Intervention | Text Messaging | N/A | To provide evidence regarding text message reminder efficacy in improving medication adherence. | Current literature shows text messaging medication reminders is potentially effective for decreasing medication non-adherence. |
| Balderas-Diaz et al.23 2017 | Granada, Spain | Observational/ Case-Control | mHealth Intervention | Actigraphy wearable (wristband) | 9 SLE patients, 11 matched controls | To assess impacts of environmental conditions on sleep quality of SLE patients via relatively objective measurement devices such as actigraphy and mobile systems. | Actigraphy objectively complements traditional subjective evaluation of sleep, thereby providing a more complete assessment relevant to SLE. |
| Scalzi et al41 2018 | Hershey, USA | Observational/ Feasibility pilot | mHealth Intervention | Online Educational Program | 37 SLE patients | To investigate feasibility and value of web-based education with and without a social media component in adolescent and young adult SLE patients. | Subjects had a significant improvement in medication adherence using the web-based system and even higher improvements if they also had social media support. Empowerment, sense of agency and sense of community appear to play key roles in the possible mechanisms of this improvement. |
| Richter et al.24 2008 | Dusseldorf, Germany | Observational | Feasibility Pilot | N/A | 153 (60 SLE patients) | To evaluate the feasibility of capturing data from self-administered patient questionnaires and integrating it into routine rheumatologic patient management electronically (via Tablet PC) rather than through paper and pencil. | Electronic self- administered questionnaires are a viable and reliable option to monitor patients with rheumatic diseases. |
| Jamilloux et al. 40 2015 | Lyon, France | Observational | Feasibility Pilot | N/A | 128 | To determine feasibility of electronically collecting monthly patient-reported outcomes (PROs) in patients with chronic inflammatory diseases (CIDs). | Electronically collecting PROs from home was feasible and efficient in patients with CIDs. |
| Williams et al.22 2016 | Charleston, USA | Study Protocol for Randomized Trial | Protocol (wait-list controlled) | Access to arthritis care kit, message board, support group, and self-management program | 150 | To determine feasibility and value of patient-tailored interventions in African-American lupus patients. | N/A |
| Li et al. 33 2017 | Vancouver, Canada | Study Protocol for Randomized Trial | Protocol (delayed control) | Fitbit and biweekly calls from PT | 130 (rheumatoid arthritis or systemic lupus erythematosus) | To test feasibility and efficacy of a remote counseling intervention in improving physical activity in patients with inflammatory arthritis. | N/A |
| Neville et al.30 2014 | Quebec, Canada | Qualitative/Fo cus Groups | Development - App/Website | N/A | 29 SLE patients, 8 providers, and 8 allied health professionals | To identify lupus- related informational and resource needs of patients and health care providers. | Lupus patients and healthcare providers noted engagement in healthcare and resources with specific information and helpful tools in self-management as opportunities for growth. |
| Herschman et al.31 2014 | Qualitative/Focu s Groups | Qualitative/Fo cus Groups | Development - App | N/A | 18 stakeholders | To develop a mobile app for adolescents with lupus through input from multiple stakeholders. | N/A |
| Van Mierlo et al.35 2015 | Toronto, Canada | Review | Development - mHealth Intervention | N/A | N/A | To stratify factors of medication nonadherence in individuals with autoimmune diseases. | Patient-centric interventions that provide education regarding their disease and the role of medication are needed to increase medication adherence. |
mHealth = Mobile Health; App = Apsplications
Among studies specifying a sample size, the median (range) number of SLE patients included was 84 (1 – 153). The most common category of papers focused on the development and use of mHealth for providing patient information (Development – Patient Information) and was comprised of 11 studies (52.4%). The remaining studies described mHealth interventions (23.8%); study protocols (9.5%), and the development of mHealth apps, websites, or mHealth interventions (Development – App) (14.3%).
Three studies (14.3%) focused on evaluating the use of web-based systems, two (9.5%) evaluated the use of text messaging, and two (9.5%) examined the use of wearable devices.23,32,33,36–38,41 These studies had mixed results, and due to small sample sizes (ranging from 9 to 41 SLE patients), their interpretability is limited. Some studies explored the development of mHealth technologies, including preferences for patient information and apps. Seven of these studies (33.3%) identified a need for more interactive educational platforms with high-quality information, two (9.5%) demonstrated a need for the development of novel methods of disease monitoring, and two (9.5%) established a need for sources of support such as virtual communities.24–28,30,32,34,35,39
Randomized Trials using mHealth technologies for SLE
The first randomized trial identified in the review compared the effects of cellular text messaging reminders with education on adherence to clinic visits (standard of care) in a cohort of 70 patients with childhood-onset SLE. Authors demonstrated that the use of text messaging reminders improved visit adherence, but not adherence to hydroxychloroquine.38 This finding is contrary to established literature showing that text messaging approximately doubles the odds of medication adherence in individuals with chronic diseases.42 The second trial tested a telephone-based weight management program associated with a web-based health interface that collected information on patient demographics, barriers to physical activity, physical activity participation, nutritional intake, goal setting, and implementation strategies. The interface also provided links to health promotional materials for adults with physical disabilities.37 The study found a small but significant effect of the intervention in reducing the body mass index of adults with significant physical disabilities, but, notably, only one patient (1.1%) in the study had SLE. The risk of bias distribution and assessment of both trials are presented in Supplementary Files 3 and 4, respectively.
The literature review demonstrated that individuals with SLE seek mHealth tools that promote disease management by including reliable educational information, functionalities to track and communicate symptoms, features to assist with medication adherence, and peer support.10,35,36,41 However, the majority of the included studies (90.4%) did not focus on evaluating the effectiveness of mHealth interventions in SLE patients. The quality of the observational studies are presented in the Supplementary File 5.
DISCUSSION
To the best of our knowledge, this is the first systematic review evaluating the use of mHealth technologies in SLE. Our study demonstrates that mHealth technologies supporting patients with SLE is an area of significant unmet need. Our review of currently available mHealth apps for SLE demonstrated that the majority of the existing apps scored poorly on the MARS scale and lacked the evidence-based information and functionalities desired by patients such as relevant educational material, symptom and medication trackers, and discussion groups to communicate with experts and peers. Though our systematic literature review found that patients seek to use mHealth technologies to aid with disease management,10,36 we identified few studies exploring mHealth-based interventions to improve health outcomes, with the limited published literature devoted to the use of mHealth platforms to provide educational information.
Interpretation of the main findings
mHealth apps review
Our review of available mHealth apps for SLE reveals a significant lack of functional, user-centered tools that meet the described needs of SLE patients. Among the included apps, Lupus Corner Health Manager is the only one that addresses the majority of the preferences of SLE patients identified in our literature review. This app provides educational material, a symptom and medication tracker, and a discussion group for communicating with others living with lupus- all key features of mHealth technologies in the management of chronic diseases.20,43,44 However, the majority of the other apps reviewed offered educational information or symptom trackers exclusively, only partially satisfying SLE patients’ stated needs.
The MARS results revealed low scores for all the apps reviewed, suggesting that major improvements are needed. The information domain scored the lowest, mainly because none of the available apps for SLE provided verifiable information. In addition to providing low quality educational content, none of the assessed apps used validated patient-reported outcome measures to evaluate symptoms, limiting the reliability and external validity of the data collected. The engagement domain scored poorly primarily because the apps did not use specific strategies to entertain users and stimulate repeat use.
Apps that are successful in engaging users in self-management of chronic conditions often incorporate gamification, the use of enjoyable mechanics of video games, in non-video game contexts.45 Gamification tools such as badges, dashboards, scores, goals and challenges, and social interaction with community members can improve user adherence to mHealth technology. Apps for the management of SLE would benefit from the inclusion of such features, particularly given the chronicity of this condition. In addition, the input of end-users - the people living with SLE - in all stages of the app development process is essential for ensuring engaging design. Focus groups of prospective users can guide content, functionality, and user-interface design, increasing the likelihood of sustained use after product development. It is unclear if any of the currently available apps reviewed in this study other than the LupusMinder were developed with the input of patients with SLE.
The assessed SLE apps also lacked several important features available in other chronic disease management apps. Currently available SLE apps do not have useful mHealth capabilities including Bluetooth connectivity to allow pairing with external hardware devices, the option for users to create personalized health goals and upload objective biometric measurements as part of symptom logs, the provision of tailored feedback based on data collected, two-way communication between users and health care providers, and clinical decision support systems for providers to interpret app data collected.43,46 The addition of these features should be explored to enrich user experience and enhance app functionality for research and clinical care.
Literature review
Although our review of the literature identified significant patient and provider interest in the use of mHealth technology to enhance the management of SLE, we were surprised to identify only two randomized controlled trials evaluating mHealth interventions in SLE patients. Two other papers identified in the review were study protocols for planned randomized controlled trials evaluating mHealth technologies as a part of an intervention for disease self-management (inclusion of an online message board as part of a broader program) and a physical activity counseling intervention (use of a Fitbit wearable device and web-based application for tracking activity).22,33
Overall, our literature review reveals an absence of high-quality studies evaluating the efficacy of mHealth technologies in SLE, with the few published studies suffering from small sample sizes and non-reproducible results. Our findings contrast with the robust evidence supporting the effectiveness of mHealth interventions in improving outcomes in several chronic conditions.47–50 Collaboration between clinical researchers and app developers is critical to creating and testing the unique capabilities of mHealth technologies in rigorously designed intervention studies.
This study suggests that the use of mHealth technologies for SLE is still a relatively new and unexplored topic, with much potential for future investigation. Strengths of our study include its rigorous systematic approach that follows well-established reporting guidelines.16,17 Investigators underwent structured training in the use of the MARS scale prior to initiation of the study and demonstrated strong agreement. However, due to a lack of direct patient input, we lacked insight into the utility of the reviewed apps for patients living with this condition. Other limitations of the study include the high heterogeneity of the included studies and the small sample sizes, which precluded any kinds of meta-analyses.
Although there is a growing need and desire for mHealth technologies to support patients with SLE, the availability of apps designed specifically for SLE and the evidence for their efficacy is still limited. The ideal mHealth app for patients with SLE would incorporate evidence-based educational material, customizable symptom and medication trackers, logs for personalized health goals, and connectivity with external hardware devices to enrich data collection. Additional useful features would include gamification components to engage users, the provision of tailored feedback based on collected data, and secure mechanisms of communication and data access between users and health care providers to facilitate treatment planning and coordination of care. However, currently available tools are of poor quality with limited functionality that fails to fulfill the needs of SLE patients. This study calls for the creation of new user-centered mHealth apps to empower the SLE community. To achieve this unmet need, comprehensive multidisciplinary partnerships between clinical researchers, patients, and app developers are critical.
Supplementary Material
ACKNOWLEDGEMENTS
We would like to thank Shreya Shetty for technical assistance.
FUNDING
L.O. Dantas is financially supported by the Sao Paulo Research Foundation (FAPESP, Process number #2018/23705-3). R. R. Bannuru is supported by the National Center for Complementary and Integrative Health of the National Institutes of Health (K23AT009374). S. Kasturi is supported by the National Center for Advancing Translational Sciences (NCATS) grant number 1KL2TR002545-01.
Footnotes
COMPETING INTEREST STATEMENT
The authors declare that they have no conflicts of interest.
REFERENCES
- 1.Carter EE, Barr SG, Clarke AE. The global burden of SLE: Prevalence, health disparities and socioeconomic impact. Nat Rev Rheumatol 2016; 12: 605–620. [DOI] [PubMed] [Google Scholar]
- 2.Yeoh S-A, Dias SS, Isenberg DA. Advances in systemic lupus erythematosus. Medicine (Baltimore) 2018; 46: 84–92. [Google Scholar]
- 3.Fava A, Petri M. Systemic lupus erythematosus: Diagnosis and clinical management. J Autoimmun 2019; 96: 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gordon C, Amissah-Arthur M-B, Gayed M, et al. The British Society for Rheumatology guideline for the management of systemic lupus erythematosus in adults. Rheumatology 2018; 57: 1502–1503. [DOI] [PubMed] [Google Scholar]
- 5.Mehat P, Atiquzzaman M, Esdaile JM, et al. Medication Nonadherence in Systemic Lupus Erythematosus: A Systematic Review. Arthritis Care Res 2017; 69: 1706–1713. [DOI] [PubMed] [Google Scholar]
- 6.Williams EM, Hyer JM, Viswanathan R, et al. Peer-to-Peer Mentoring for African American Women With Lupus: A Feasibility Pilot. Arthritis Care Res (Hoboken) 2018; 70: 908–917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fanouriakis A, Kostopoulou M, Alunno A, et al. 2019 update of the EULAR recommendations for the management of systemic lupus erythematosus. Ann Rheum Dis 2019; 736–745. [DOI] [PubMed] [Google Scholar]
- 8.Improving DJW the prognosis of SLE without prescribing lupus drugs and the primary care paradox. Lupus 2008; 17: 91–92. [DOI] [PubMed] [Google Scholar]
- 9.Ryu S mHealth: New Horizons for Health through Mobile Technologies: Based on the Findings of the Second Global Survey on eHealth. Healthc Inform Res; 18: 231. [Google Scholar]
- 10.Tani C, Trieste L, Lorenzoni V, et al. Health information technologies in systemic lupus erythematosus: Focus on patient assessment. Clin Exp Rheumatol 2016; 34: 54–56. [PubMed] [Google Scholar]
- 11.Nussbaum R, Kelly C, Quinby E, et al. Systematic Review of Mobile Health Applications in Rehabilitation. Arch Phys Med Rehabil 2019; 100: 115–127. [DOI] [PubMed] [Google Scholar]
- 12.Center PR. Mobile Fact Sheet. https://www.pewinternet.org/fact-sheet/mobile/ Accessed June 2019 2019; 1–6.
- 13.Robbins R, Krebs P, Jagannathan R, et al. Health App Use Among US Mobile Phone Users: Analysis of Trends by Chronic Disease Status. JMIR mHealth uHealth 2017; 5: e197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cvrkel T The ethics of mHealth: Moving forward. J Dent 2018; 74: S15–S20. [DOI] [PubMed] [Google Scholar]
- 15.Levine AB, Batterman A, Bykerk VP, et al. Patient preferences for the development of a mobile health (mHealth) application (app) for systemic lupus erythematosus (SLE) patients: A qualitative study. Arthritis Rheumatol Conf Am Coll Rheumatol Rheumatol Heal Prof Annu Sci Meet ACR/ARHP 2015; 67: 5–7. [Google Scholar]
- 16.Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015; 4: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Higgins JPTGS. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.handbook.cochrane.org Cochrane Collab. [Google Scholar]
- 18.StatCounter 1999–2019, All rights reserved. Mobile Operating System Market Share Worldwide. [Google Scholar]
- 19.Stoyanov SR, Hides L, Kavanagh DJ, et al. Mobile App Rating Scale: A New Tool for Assessing the Quality of Health Mobile Apps. JMIR mHealth uHealth 2015; 3: e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Machado GC, Pinheiro MB, Lee H, et al. Smartphone apps for the self-management of low back pain: A systematic review. Best Pract Res Clin Rheumatol 2016; 30: 1098–1109. [DOI] [PubMed] [Google Scholar]
- 21.Wells G, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses. (Available from URL http//www.ohri.ca/programs/clinical_epidemiology/oxford.asp). DOI: 10.2307/632432. [DOI]
- 22.Williams EM, Lorig K, Glover S, et al. Intervention to Improve Quality of life for African-AmericaN lupus patients (IQAN): study protocol for a randomized controlled trial of a unique a la carte intervention approach to self-management of lupus in African Americans. BMC Health Serv Res 2016; 16: 339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Balderas-Díaz S, Martínez MP, Guerrero-Contreras G, et al. Using Actigraphy and mHealth Systems for an Objective Analysis of Sleep Quality on Systemic Lupus Erythematosus Patients. Methods Inf Med 2017; 56: 171–179. [DOI] [PubMed] [Google Scholar]
- 24.Richter JG, Becker A, Koch T, et al. Self-assessments of patients via Tablet PC in routine patient care: comparison with standardised paper questionnaires. Ann Rheum Dis 2008; 67: 1739–1741. [DOI] [PubMed] [Google Scholar]
- 25.Reynolds M, Hoi A, Buchanan RRC. Assessing the quality, reliability and readability of online health information regarding systemic lupus erythematosus. Lupus 2018; 27: 1911–1917. [DOI] [PubMed] [Google Scholar]
- 26.Meunier B, Jourde-Chiche N, Mancini J, et al. Characteristics and information searched for by French patients with systemic lupus erythematosus: A web-community data-driven online survey. Lupus 2016; 25: 370–375. [DOI] [PubMed] [Google Scholar]
- 27.Callejas-Rubio J-L, Ríos-Fernández R, Barnosi-Marín A-C, et al. Health-related Internet use by lupus patients in southern Spain. Clin Rheumatol 2014; 33: 567–573. [DOI] [PubMed] [Google Scholar]
- 28.Richter JG, Becker A, Koch T, et al. Internet use in rheumatology outpatients in 2006: gender less important. Clin Exp Rheumatol 2009; 27: 15–21. [PubMed] [Google Scholar]
- 29.Sciascia S, Radin M. What can Google and Wikipedia can tell us about a disease? Big Data trends analysis in Systemic Lupus Erythematosus. Int J Med Inform 2017; 107: 65–69. [DOI] [PubMed] [Google Scholar]
- 30.N C, C DD, M C, et al. The needs of persons with lupus and health care providers: A qualitative study aimed toward the development of the Lupus Interactive NavigatorTM. Lupus 2014; 23: 176–182. [DOI] [PubMed] [Google Scholar]
- 31.Herschman J, Kasenberg T, Levy D, Ruth N, Taberner C, Kaufman MRA. Development of a smartphone app for adolescents with lupus: a collaborative meeting-based methodology inclusive of a wide range of stakeholders. Rev Panam Salud Publica; May-Jun;35. [PubMed] [Google Scholar]
- 32.Young SP, Henderson E, Cheseldine DL, et al. Development and assessment of a World Wide Web site for systemic lupus erythematosus patient information. Lupus 2002; 11: 478–484. [DOI] [PubMed] [Google Scholar]
- 33.Li LC, Feehan LM, Shaw C, et al. A technology-enabled Counselling program versus a delayed treatment control to support physical activity participation in people with inflammatory arthritis: study protocol for the OPAM-IA randomized controlled trial. BMC Rheumatol 2017; 1: 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mendelson C Gentle hugs: Internet listservs as sources of support for women with lupus. ANS Adv Nurs Sci 2003; 26: 299–306. [DOI] [PubMed] [Google Scholar]
- 35.van Mierlo T, Fournier R, Ingham M. Targeting Medication Non-Adherence Behavior in Selected Autoimmune Diseases: A Systematic Approach to Digital Health Program Development. PLoS One 2015; 10: e0129364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sarabi RE, Sadoughi F, Orak RJ. The Effectiveness of Mobile Phone Text Messaging in Improving Medication Adherence for Patients with Chronic Diseases : A Systematic Review. 18 Epub ahead of print 2016. DOI: 10.5812/ircmj.25183.Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rimmer JH, Wang E, Pellegrini CA, et al. Telehealth Weight Management Intervention for Adults with Physical Disabilities. Am J Phys Med Rehabil 2013; 92: 1084–1094. [DOI] [PubMed] [Google Scholar]
- 38.TING TV, KUDALKAR D, NELSON, et al. Usefulness of Cellular Text Messaging for Improving Adherence Among Adolescents and Young Adults with Systemic Lupus Erythematosus. J Rheumatol 2012; 39: 174–179. [DOI] [PubMed] [Google Scholar]
- 39.Rhee RL, Von Feldt JM, Schumacher HR, et al. Readability and suitability assessment of patient education materials in rheumatic diseases. Arthritis Care Res (Hoboken) 2013; 65: n/a–n/a. [DOI] [PubMed] [Google Scholar]
- 40.Jamilloux Y, Sarabi M, Kérever S, et al. Adherence to online monitoring of patient-reported outcomes by patients with chronic inflammatory diseases: a feasibility study. Lupus 2015; 24: 1429–1436. [DOI] [PubMed] [Google Scholar]
- 41.Scalzi LV, Hollenbeak CS, Mascuilli E, et al. Improvement of medication adherence in adolescents and young adults with SLE using web-based education with and without a social media intervention, a pilot study. Pediatr Rheumatol 2018; 16: 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Thakkar J, Kurup R, Laba TL, et al. Mobile telephone text messaging for medication adherence in chronic disease a meta-analysis. JAMA Intern Med 2016; 176: 340–349. [DOI] [PubMed] [Google Scholar]
- 43.Lee JA, Choi M, Lee SA, et al. Effective behavioral intervention strategies using mobile health applications for chronic disease management: A systematic review. BMC Med Inform Decis Mak; 18 Epub ahead of print 2018. DOI: 10.1186/s12911-018-0591-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sleurs K, Seys SF, Bousquet J, et al. Mobile health tools for the management of chronic respiratory diseases. Allergy Eur J Allergy Clin Immunol 2019; 1292–1306. [DOI] [PubMed] [Google Scholar]
- 45.Miller AS, Cafazzo JA, Seto E. A game plan: Gamification design principles in mHealth applications for chronic disease management. Health Informatics J 2014; 22: 184–193. [DOI] [PubMed] [Google Scholar]
- 46.Donevant SB, Estrada RD, Culley JM, et al. Exploring app features with outcomes in mHealth studies involving chronic respiratory diseases, diabetes, and hypertension: A targeted exploration of the literature. J Am Med Informatics Assoc 2018; 25: 1407–1418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Blödt S, Pach D, Roll S, et al. Effectiveness of app-based relaxation for patients with chronic low back pain (Relaxback) and chronic neck pain (Relaxneck): study protocol for two randomized pragmatic trials. Trials 2014; 15: 490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kravitz RL, Schmid CH, Marois M, et al. Effect of Mobile Device-Supported Single-Patient Multi-crossover Trials on Treatment of Chronic Musculoskeletal Pain: A Randomized Clinical Trial. JAMA Intern Med 2018; 178: 1368–1377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Morawski K, Ghazinouri R, Krumme A, et al. Association of a smartphone application with medication adherence and blood pressure control: The MedISAFE-BP randomized clinical trial. JAMA Intern Med 2018; 178: 802–809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Buller DB, Berwick M, Lantz K, et al. Smartphone mobile application delivering personalized, real-time sun protection advice: A randomized clinical trial. JAMA Dermatology 2015; 151: 497–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.