Abstract
Background
Human infections with avian influenza viruses (AIV) represent a persistent public health threat. The principal risk factor governing human infection with AIV is from direct contact with infected poultry and is primarily observed in Asia and Egypt where live-bird markets are common.
Areas of agreement
Changing patterns of virus transmission and a lack of obvious disease manifestations in avian species hampers early detection and efficient control of potentially zoonotic AIV.
Areas of controversy
Despite extensive studies on biological and environmental risk factors, the exact conditions required for cross-species transmission from avian species to humans remain largely unknown.
Growing points
The development of a universal (‘across-subtype’) influenza vaccine and effective antiviral therapeutics are a priority.
Areas timely for developing research
Sustained virus surveillance and collection of ecological and physiological parameters from birds in different environments is required to better understand influenza virus ecology and identify risk factors for human infection.
Keywords: highly pathogenic avian influenza virus, zoonotic viruses, pandemics, virus ecology, live-bird markets, virus spillover
Introduction
To date, influenza A viruses bearing combinations of 16 HA and 9 NA subtypes have been described in wild aquatic birds (ducks, geese, shorebirds and gulls), the natural reservoir of avian influenza virus (AIV).1 All subtypes of influenza A viruses can be found in various bird species, except subtypes H17N10 and H18N11 that are isolated exclusively from bats.2 Influenza A viruses are negative-sense, single-stranded RNA viruses classified in the family Orthomyxoviridae. Their genome consists of eight gene segments that encode for eight structural proteins and up to eight non-structural proteins (Fig. 1A). 3 Hemagglutinin (HA) and neuraminidase (NA) are the two major surface glycoproteins, essential for virus entry and release and are the major targets for neutralizing antibodies.3 Mutations that occur in the HA and NA genes can lead to changes in the protein and facilitate evasion of host humoral immune responses.3 A subset of avian influenza A viruses are commonly found in domestic poultry, and numerous incidental hosts, including humans, have been described.1,4
Fig. 1.
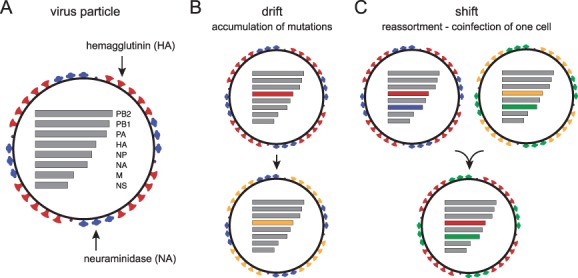
(A) Schematic presentation of the influenza A virus particle. (B and C) Mechanisms of evolution. Antigenic drift results from the accumulation of mutations leading to changes in viral antigenicity, especially on surface proteins (B). Antigenic shift occurs through reassortment that may generate progeny viruses with distinct antigenicity compared to parental strains (C).
Phenotypic diversity of influenza A viruses originates from two mechanisms; the accumulation of substitutions in the HA and NA proteins that results in ‘antigenic drift’, and ‘antigenic shift’ that results from the shuffling of individual gene segments derived from multiple viruses, commonly referred to as ‘reassortment’ (Fig. 1B and C).1,3 The viral RNA-dependent RNA polymerase is error-prone, leading to high mutation rates during genome replication and allows the virus to constantly drift in response to antibody-mediated population immunity.1 Reassortment can only occur when a single host cell is infected with two or more different influenza A virus strains. Antigenic shift is implicated in zoonotic transmission and the emergence of pandemic influenza A viruses.5
AIV are divided into two pathotypes, low pathogenic avian influenza (LPAI) and highly pathogenic avian influenza (HPAI), based on their virulence in chicken. In Asia, spillover of LPAI from wild waterfowl (primarily wild ducks) has led to the establishment of H4, H5, H6, H7 and H9 viruses in combination with various NA subtypes in domestic poultry (mainly farmed ducks and chicken) (Fig. 2A). While AIV infection in ducks is typically mild, influenza A virus subtypes H5 and H7 can evolve into the HPAI pathotype in terrestrial poultry (chicken and turkey) by acquiring mutations in the HA gene that allow virus infection to become systemic.6 The presence of multiple basic amino acids at the cleavage site of the HA is a critical determinant of virus virulence in poultry and employed to classify HPAI and LPAI viruses.7 HPAI viruses have led to significant economic losses due to the death and culling of infected birds, in addition to trade restrictions in order to contain virus outbreaks.8
Fig. 2.

(A) Transmission of influenza virus from wild bird population to domestic poultry and spillover into humans. (B) Number of reported cases of H5 (red numbers and bars) and H7 (green numbers and bars) infection in humans. (C) Timeline of major outbreak events.
The first recorded human deaths caused by HPAI virus occurred in Hong Kong in 1997 when an H5N1 virus infected 18 individuals with six fatalities.9 This virus was derived from an isolate obtained from geese in China in 1996, A/goose/Guangdong/1/1996 (Gs/GD/96), commonly referred to as the ‘goose Guangdong’ virus lineage. Since then, Gs/GD/96 progeny viruses have been detected in more than 70 countries,10 frequently becoming endemic in poultry populations, resulting in 861 recorded human cases with a case fatality rate of 53%.11 The second major AIV zoonosis was caused by an H7N9 virus, which was first detected in China in 2013.12 It has since caused more than 1500 human cases at a case fatality rate of 39% (Fig. 2B).13 Furthermore, this virus has evolved from an LPAI to a HPAI in or prior to 2016.14 In addition to these AIV subtypes, sporadic cases of human infection with H5N6, H6N1, H7N2, H7N3, H7N4, H7N7, H9N2, H10N7 and H10N8 viruses have also been described (Fig. 2C).15,16
Here, we describe the current understanding of the origins, epidemiology and clinical manifestations of zoonotic AIV that continue to pose a potential pandemic threat.
Clinical presentation of zoonotic influenza virus infections
Patients infected with H5N1 or H7N9 viruses commonly present with influenza-like-illness (ILI) symptoms, including fever, dry cough, body aches and nausea.17,18 A sizeable proportion of H5N1- and H7N9-infected patients develop severe symptoms, including inflammation of the lower respiratory tract (e.g. bronchiolitis and pneumonia), respiratory distress and multiple organ dysfunctions.17–19 Notably, high levels of plasma pro-inflammatory cytokines and chemokines are detected in H5N1- and H7N9-infected patients, possibly contributing to pathogenicity in humans.20,21 Incubation periods are estimated at 3–5 days, up to 9 days.17,18 The average time from onset of illness to death is commonly 8–12 days.22 The median age of patients infected with H5N1 is 19 years, while it is 55 years for A/H7N9 influenza virus infections.23,24 Patients infected with A/H7N9 are more likely to have pre-existing medical conditions at the time of infection, resulting in increased severity. Furthermore, conjunctivitis was identified as a prominent manifestation of human infection with H7N7, H7N3, H7N2 and H10N7 viruses, but is rarely found in patients infected with H5N1 or H7N9 viruses.17,18,25 The vast majority of reported infections with subtypes other than H5 or H7 was relatively mild, often resulting in upper respiratory symptoms and conjunctivitis.25
Species barriers, host susceptibility and adaptation markers
The host range of influenza A viruses is largely determined by the match between cellular receptor availability and viral receptor binding capacity, as well as the receptiveness of the infected cell to sustain virus replication and virion release.7 In birds, the main site of replication for AIV is the gastrointestinal tract, whereas mammalian influenza viruses preferentially infect the upper respiratory tract of a wide range of mammals, including humans.1,7 Generally, influenza A viruses that repeatedly infect humans (e.g. seasonal influenza virus subtypes H1N1 and H3N2) preferentially bind to receptors terminated by an N-acetyl sialic acid linked to a residue in a galactose molecule by an α2,6 linkage (α2,6-SA), whereas AIVs preferentially bind to terminal sialic acids with an α2,3 linkage (α2,3-SA).3 Alpha 2,6-SA ‘human-type’ receptors are primarily expressed in the upper airways of humans, while α2,3-SA ‘avian-type’ receptors are abundant in the intestinal tract of birds.7,26 Avian-type receptors are also found at relatively high frequency in the human lung compared to the upper airways that almost exclusively express ‘human-type’ receptors.27 As such, the likelihood of human infection by avian viruses is relatively low, since it requires infectious particles to reach the lower airways to initiate infection. A number of key mutations located in the head domain of the HA protein that determines receptor specificity have been identified.28–30
The optimal temperature for virus replication constitutes an additional barrier for zoonotic transmission of AIV, as human influenza viruses are adapted to replicate in the mammalian upper respiratory tract at a relatively low temperature of ~ 33°C.7 In contrast, AIVs favour replication at higher temperatures (>37°C), which corresponds to the temperature range (41.0–42.1°C) found in the intestinal tract of major influenza host species.31 A single mutation in the virus polymerase genes can mediate temperature adaptation to facilitate replication in a broad range of hosts. Substitution from Glu to Lys at position 627 (E627K) in the PB2 gene has been studied extensively as the mutation enhances replication of AIV at lower temperatures.6 Other complementary or facilitating mutations in PB2, for example, D701N and R591Q, were reported in pandemic H1N1 virus and H5/H7 AIV infecting humans.7,32 Recently, experimental studies identified E627K in combination with mutations in the HA protein that allowed avian viruses to transmit via respiratory droplet between ferrets.33,34 These mutations in the HA include substitutions in the HA 220-loop (for example, Q226L and G228S) conferring mammalian-type receptor binding, in addition to substitutions that remove the effects of steric hindrance of glycan molecules (N158D and N186K) or substitutions that stabilize the HA structure (T318). These results highlight essential viral phenotypes that are required for an avian virus to transmit between mammalian hosts involving (i) receptor binding, (ii) stability of the virion and (iii) replication. Those identified amino acid signatures may serve as a powerful tool for risk assessment of other influenza virus subtypes. Nevertheless, the genetic background and poorly understood epistatic interactions may have a great influence on the effect of these substitutions. Thus, caution is required when attempting to directly infer the viral phenotype based on previously identified mutations.
Several of these factors might explain the relative rarity of human infections with AIV in relation to the number of exposed individuals. To date, no AIV has been capable of efficiently transmitting between humans.22,35 Nevertheless, clusters of human infections were reported during H5N1 and H7N9 epidemics suggesting direct contact transmission from infected humans.36,37 In most cases, suspected direct transmission involved the infection of a caregiver or family members that had sustained and intimate contact with the patient, thereby possibly exposing them to high amounts of infectious virus, e.g. H5N1 cases in Thailand in 200438 and H7N9 in China during 2013–2017.39
Another aspect of influenza biology with direct relevance for pandemic emergence in humans is intermediate hosts, such as the role of pigs and some poultry species that may facilitate the adaptation of AIV to ‘human-type’ receptor specificity. Animals, such as pig, quail and turkey possess more human-like receptors than ducks, thereby possibly allowing selection of mutations that confer higher binding affinity to ‘human-type’ receptors.40 In the case of pigs, they may also act more broadly as intermediaries for mammalian adaptation of avian viruses for viral phenotypic adaptation. Although evidence suggests that pigs generally have a low susceptibility for infection with AIV including H5N1,41,42 they act as incidental hosts for both avian and human viruses and are therefore implicated in the selection of novel and pandemic strains.6
Risk factors for human infection by AIV
A major risk factor for human infections with either LPAI or HPAI viruses is the exposure to poultry in farms or live-bird markets (LBM), which are common throughout Asia.22,43 Considering the high number and frequency of people having contact with avian species, zoonotic infections of AIV are rare.25,44 Various aspects of poultry production systems drive the generation and dispersal of zoonotic AIV. Southern China is considered the epicentre for the generation of new avian influenza strains, facilitated by its large population of wild waterfowl, domestic birds and a variety of farming systems.45 The high proportion of poultry produced in backyards and small-scale farming exposes diverse animal species that are susceptible to influenza virus infection to a diverse pool of viruses and allows frequent direct contact of humans with poultry.45,46
China is the world’s largest producer of poultry, accounting for the majority of domestic chicken and duck production worldwide, with a duck population of over 700 million birds.47 As mentioned above, ducks (Anas spp.) are considered the principal natural reservoir of influenza A viruses. Given that domestic ducks in Asia are primarily mallards (Anas platyrhynchos domesticus), it is not surprising that they are highly susceptible to infection by avian influenza strains, including H5N1. However, domestic (and wild) ducks generally show little to no clinical signs of infection and are insensitive to vaccination against AIV.48,49 These factors allow domestic ducks to carry and shed influenza A viruses for extended periods, thus playing a crucial role in the generation, maintenance and spread of zoonotic influenza viruses.45,50
In backyard and multi-species farming, biosecurity is generally poor and viruses are more easily transmitted between different hosts (mainly between different species of poultry or between birds and pigs, incidentally from birds to humans). This transmission occurs primarily by the faecal-oral route, leading to both maintenance of viruses and increased viral genetic diversity through reassortment.45,46 Likewise, local LBMs can serve as places where live domestic birds from a wide geographic scope (industry and small-scale farming), and a range of avian species including song birds and minor domestic birds (e.g. quail and pheasant) come into close contact and possibly exchange viruses. In addition, contaminated items including droppings, cages, feed and dead animals can become the source of infections even in remote regions away from LBMs if those contaminated items or infected animal are returned to local farms. Closure of LBMs appears to be the most effective control measure implemented during outbreaks of H5N1 and H7N9 in China.51 Besides LBMs, international poultry trade is a major driving force for influenza transmission, exemplified by the introduction of HPAI H5N1 to several South-East Asian countries since 2003.
In contrast to terrestrial wild birds, infected migratory birds, including the Anseriformes (waterfowl) and Charadriiformes (shorebirds), are more likely to disperse viruses across long geographical distances.50,52 This is exemplified by the Qinghai Lake outbreak in China in 2005 during which an H5N1 virus was transmitted from poultry to wild waterfowl, specifically bar-headed geese.45,46 Qinghai Lake is a major migratory stopover and breeding site for birds transiting flyways to India, Siberia and Southeast Asia.46 In 2007, an H5N1 virus distinctive from Qinghai Lake viruses was introduced in local wild birds or poultry in more than 20 countries in Asia, the Middle East and Europe.36,50 These viruses were established in domestic birds in Egypt, which became one of the major areas for human infection and deaths caused by AIV.50 Although HPAI viruses have varying clinical symptoms, their impact on different wild bird species, e.g. by affecting long-distance movements of the hosts, is poorly understood.52,53 It is now established that wild birds are involved in repeated virus introductions to Europe and the United States.54,55 However, control efforts in these regions have successfully prevented endemic circulation and human infection.
Zoonotic avian influenza A viruses
H5N1 viruses
Human H5N1 infection was first detected in Hong Kong in 1997, when 18 cases were identified leading to six deaths. This also marked the first recorded lethal case in humans infected by AIV, previously thought to be impossible. The viruses responsible for the Hong Kong outbreak were found to be similar to those present in poultry in wet markets.46 Genetic analyses further indicated that the HA gene from human and chicken isolates was most closely related to a virus isolated from a goose from an outbreak that occurred in Guangdong, China in 1996.56 This H5N1 virus, named A/goose/Guangdong/1996 in the official influenza nomenclature, is commonly abbreviated as ‘Gs/GD’ and is the progenitor to all viruses responsible for the HPAI H5N1 panzootic.57 The remaining seven gene segments of the Hong Kong H5N1 viruses were closely related to H6N1 and H9N2 viruses, also commonly found in poutlry.58,59 The 1997 outbreak in Hong Kong was eventually contained by culling and disinfection at LBMs.58 The virus responsible has not been detected in poultry since and is assumed to be extinct.
After the Hong Kong H5N1 outbreak, viruses derived from Gs/GD became endemic in poultry farms and LBMs in southern China; however, no human infections were recorded in this period.36 In early 2003, two humans were diagnosed with H5N1 infection in Hong Kong after returning from China.46 In the same year, Vietnam reported the first human H5N1 infection in Southeast Asia.11 From 2003 to 2005, H5N1 outbreaks in birds and increasing numbers of human infections were reported in Southeast Asia, including Vietnam, Thailand, Cambodia and Indonesia.11,36 It is thought that H5N1 viruses were introduced into these countries via poultry trade with China.45,50 The rapid spread of H5N1 viruses throughout Asia and the corresponding increase in human infections and deaths led to concerns that these infections would represent a nascent pandemic.60 As mentioned above, the HPAI H5N1 outbreaks in wild aquatic birds at Qinghai Lake in China resulted in the geographic expansion of this virus. A study on the interaction of domestic and wild bird populations found that wild birds are primarily responsible for long-distance dispersal, whereas virus spread among poultry populations drives regional spread of H5N1.61
From 2003 to 2018, H5N1 human cases have been reported from a total of 16 countries.11,57 The further geographic expansion of H5N1 viruses was linked to increased human infections occurring in Turkey (2006), Iraq (2006), Egypt (2006), Pakistan (2007) and Nigeria (2007).36 Notably, while the majority of new H5N1 virus detections in humans were reported in Indonesia during 2003–2008 (141 cases with 115 deaths), the burden of human disease later shifted to Egypt, where H5N1 infections persisted and a total of 359 cases and 120 deaths were reported from 2009 to 2017.11 In the period 2003–2018, 80% of human H5N1 detections were restricted to Indonesia, Egypt and Vietnam, with a highest annual number of cases amounting to 136 cases in Egypt in 2015 alone. A drop in the number of human H5N1 infections has been observed in recent years with no cases reported in 2018 worldwide and just a single case in 2019 with fatal outcome.11
Along with the geographic expansion of the H5N1 infections, the virus diverged into geographically and genetically distinct HA clades that have developed individual antigenic profiles leading to limited cross-reactivity where antibodies from prior infections often do not neutralize currently circulating strains.26,50 This antigenic variation has greatly complicated control efforts in poultry and pre-pandemic preparation, requiring multiple vaccine candidates recommended by WHO in order to achieve protection against diverse H5N1 viruses.62 Since 2005, WHO, OIE and FAO have employed a formal system of H5-HA nomenclature to assist with tracking viral diversity based on the phylogenetic analysis of the HA gene.57 Currently, the majority of H5 viruses circulating globally belong to two different clusters called Clade 2.3.2.1 and Clade 2.3.4.4.57,62
H5Nx viruses
From the first detection in 1996 through 2008, almost all known Gs/GD HPAI H5 viruses possessed an N1–NA gene, i.e. all these viruses were H5N1 subtype.57 However, since 2008, Gs/GD HPAI H5 viruses with different NA genes emerged that had reassorted with LPAI viruses circulating in poultry, resulting in five novel Gs/GD HPAI H5 virus subtypes (H5N2, H5N3, H5N5, H5N6 and H5N8).63,64 Before 2014, the vast majority of Gs/GD-derived viruses were subtype H5N1, with only a few viruses with non-N1 NA subtypes detected in China,57,65 and only H5N1 viruses responsible for human infections.66 In early 2014, the first human H5N6 cases were identified in mainland China, and to date, there have been 23 confirmed human H5N6 cases including seven deaths reported from China.66,67 Continuing surveillance demonstrated that by 2016, H5N6 had become predominant in poultry, replacing H5N1 in China.68
Following similar transmission routes as H5N1 viruses, migratory birds have spread H5Nx viruses, primarily H5N6 and H5N8, to Korea, Japan and Europe before and during 2014.55,64,69 Of note, H5N8 infections were detected in North America in late 2014 and the virus subsequently reassorted with local LPAI viruses, sparking multiple H5N1 and H5N2 outbreaks in poultry in the United States.70,71 These events marked the first detection of Gs/GD-derived viruses in North America. While the estimated risk of human infections from these new HPAI H5Nx viruses is currently low,72 the wide geographical distribution of multiple subtypes requires continued close monitoring and assessment of their transmission potential.
H7 viruses
Before the emergence and dissemination of Gs/GD HPAI H5N1 viruses, H7 subtype AIV accounted for the majority of documented zoonotic infections25,44 and poultry outbreaks in North America and Europe. H7 outbreaks were detected in the USA in 2002 (H7N2), the Netherlands in 2003 (H7N7), Canada in 2004 (H7N3) and the UK in 2007 (H7N2).73,74 Human infections typically occur in poultry workers or personnel involved in control measurements. Conjunctivitis is the major clinical manifestation of individuals infected with either LPAI or HPAI H7 viruses, but individual severe cases have been documented.25
A major H7N7 outbreak occurred in the Netherlands in early 2003, and subsequently spread to poultry in Belgium and Germany in the same year,75,76 leading to the culling of more than 30 million chicken. During the culling exercises, a total of 89 people involved in the operations were confirmed to be infected with H7N7,75,77 which distinguished the event from prior H7 outbreaks in birds during which no or only a few zoonoses were reported.25 One of the 89 cases developed severe symptoms and died 15 days after visiting an affected farm. Several amino acid residues associated with human adaptation were identified in the genome of the virus from this fatal case, including the E627K mutation in PB275 that confers the ability to replicate at lower temperatures present in the human upper respiratory tract.7
H7N9 viruses
In March 2013, China reported its first cases of human infection with LPAI H7N9 viruses in Shanghai and Anhui.13,78 Unlike HPAI viruses that cause widespread mortality in chicken and are therefore easily detected, LPAI viruses can remain hidden unless active surveillance is undertaken, thereby greatly complicating effective responses to these outbreaks. Remarkably, before the end of 2015, the H7N9 virus quickly surpassed the total number of human infections caused by HPAI H5N1 and H5Nx viruses, reaching 684 cases.13 During the first wave of the epidemic (February–May 2013), a total of 132 cases were reported, including 37 deaths.79 The viruses continued to cause human cases in six additional epidemic waves from mid-2013 to present.13 The 5th wave of epidemics occurred from October 2016 to September 2017 totalling more than 750 cases with 300 deaths in the most severe H7N9 outbreak to date.13 There were also cases identified in Taiwan, Macao, Hong Kong, Canada and Malaysia that were all associated with recent travel to mainland China.13
Isolation of genetically identical H7N9 viruses from chickens in LBMs in China and humans confirmed that the infecting virus was of direct avian origin.80 Further phylogenetic studies showed that the H7-HA gene was derived from viruses circulating in domestic ducks (H7N3 subtype), and that the same H7-HA lineage was introduced into domestic ducks from migratory birds before 2010.80 In addition, the N9 NA gene was closely related to those of viruses isolated in wild birds in Hong Kong (H2N9, H11N9), and the internal genes were derived from a H9N2 sub-lineage virus endemic to China.81 These viruses were generated by reassortment in domestic ducks before being transmitted to and amplified in chickens.80
The presence of a leucine or isoleucine substitution at position 226 (in H3 numbering), which favours human-like receptor binding of the H7-HA protein of these H7N9 viruses, is of particular concern.2,81 Interestingly, this amino acid substitution was present in H7N9 viruses in chickens, but it was not found in the same H7N9 viruses found in ducks.80 From 2017 onwards, HPAI H7N9 viruses were identified in patients in Guangdong, Southern China.14,82 These HPAI viruses evolved directly from the previous LPAI viruses and accounted for 32 human cases in the same wave.66 While there is no evidence that an increase in pathogenicity in chicken would directly influence human epidemics, this change may have a profound effect on chicken mortality and greatly increase the economic impact of H7N9 outbreaks. Currently, H7 outbreaks appear restricted to China. However, if the virus is transmitted to other countries, it is likely that there will be a similar expansion in antigenic diversity of the virus population as previously seen in the case of H5N1 and H5Nx viruses, leading to new requirements for additional pre-pandemic vaccine candidates.
H9 viruses
H9N2 viruses are endemic in poultry across large parts of Eurasia and Africa, with sporadic H9N2 outbreaks and human infections reported since the 1990s.83 Compared to HPAI viruses, the clinical manifestation on H9 viruses in infected chicken is mild and typical for LPAI viruses.84 In China, the first outbreak of H9N2 virus was reported in Guangdong in 1994. Similar to H5N1 viruses, H9N2 was consistently isolated from multiple poultry hosts, and formed a high proportion of influenza A viruses detected and isolated from quail, partridge and pheasant.85 These birds are commonly referred to as ‘minor poultry’ in the context of LBMs in China. While H9N2 viruses were isolated globally, viruses in North America were mostly isolated from wild birds and no sustained circulation in poultry has been observed.86 Currently, there are two major H9N2 virus lineages circulating in Eurasia, referred to as the G1 and Y-280-like viruses.84,87
The first human H9N2 case was recorded in Guangdong, China in 1998, with another case detected in Hong Kong in 1999.88 The viruses isolated from these cases were found to be related to a virus isolated from quail in Hong Kong, A/quail/Hong Kong/G1/1997, the prototype virus of the H9N2 G1-lineage. A total of 5 cases of human infection with H9N2 virus were reported in Guangdong province in 1998,84 and there have since been more than 30 confirmed cases reported from China, Egypt and Bangladesh from 1998 to 2016, and a single fatal patient with other underlying disorders.25,89 Although the majority of cases were very mild and could have been easily mistaken for seasonal influenza infections, sequencing of virus genetic material identified them as H9N2. The main reason for their detection was the contemporaneous occurrence of H5N1 infections in Hong Kong in 1997 that lead to the in-depth analysis of any human infection not identified as seasonal influenza and irrespective of clinical severity. Due to its large geographical distribution, high prevalence in poultry and ability to infect humans, H9N2 viruses are considered to have pandemic potential83,85,90 and the WHO recommends pre-pandemic vaccine strains against the subtype.62 Although infection with human viruses may generate antibodies that cross-react with H9N2 virus, complicating serological surveys for this subtype, a recent meta-analysis determined the prevalence of H9N2 human infections at 1.3%.91
Another intriguing characteristic of H9N2 viruses is their role as source for genes present in the majority of emerging AIV that infect humans. Genetic analyses have shown that H9N2 viruses circulating in LBMs in China played a central role in the genesis of HPAI H5N1 and H5Nx viruses.59,68 Furthermore, the internal genes of H7N9 and H10N8 zoonotic AIV are derived from H9N2 viruses found in chicken in China.80,92 These events not only reflect high prevalence of H9N2 in land-based poultry (e.g. chicken, quail, etc.) in southern China, but also suggest that the internal genes of H9N2 viruses confer increased virus replication in mammalian cells.59,92 Some of the previously isolated H9N2 viruses exhibit human-like receptor binding preference93; however, their receptor binding profile is not yet fully determined and warrants further study.
Other subtypes
With the advance in clinical diagnostics and increased awareness of zoonotic pathogens, sporadic human LPAI infections are more frequently identified. The first documented human infection with H10 subtype virus was in 2004 in two Egyptian infants94 and subtyped H10N7. The same virus was also isolated in wild ducks from a market frequented by the parents of the patients, where they travelled as a poultry merchant.94 In 2010, slaughterhouse workers in Australia were found infected with H10N7 from chickens.95 However, the HA gene from those viruses were similar to viruses found in North American wild birds and not related to the viruses isolated in Egypt.95 During 2013–2014, China reported three human H10N8 infections in Jiangxi province that resulted in two deaths. All patients had visited LBMs before falling ill and being hospitalized.92,96 Comparison of the genes from human isolates with those of viruses isolated from chickens revealed a scenario resembling the genesis of H7N9 viruses. The HA and NA of H10N8 could be traced back to viruses in wild birds, while all internal genes were derived from H9N2 viruses.92 In 2013, Taiwan reported the first H6N1 human infections with severe respiratory symptoms.97 While the source of virus could not be directly identified, it was genetically similar to viruses endemic H6N1 in chickens in Taiwan.97,98
Pandemic mitigation strategies
Given the tremendous public health importance of circulating AIV, the World Health Organization, through coordinating reference laboratories, closely examines viral antigenicity in order to select strains for the development of candidate vaccine viruses for pandemic preparedness.62 To date, candidate vaccines are available for H5, H7 and H9 viruses.62 In order to reduce poultry losses and also to reduce human infections by reducing the viral load of birds in farms and markets, vaccination programmes in poultry have been implemented in several countries.99 However, varying reactivity in different host species, the short production cycle of these birds and generally low immunogenicity prevent broad usage due to the moderate effectiveness of these vaccines.45 Thus, vaccination alone is not an optimal strategy for eliminating AIV.45,100 Recent progress on the development of a ‘universal’ influenza vaccine has shed light on possible strategies to prevent infection with any subtype of influenza viruses in the future. These vaccines aim to elicit antibodies targeting conserved regions across all known influenza strains,101 and a number of clinical trials are ongoing.102,103
A number of drugs, such as oseltamivir, peramivir and zanamivir, have been developed that inhibit virus NA function.104,105 However, resistance can emerge very quickly due to several mutations in the NA gene that lower drug efficacy by varying degrees.104,106 In 2018, a new drug, Baloxavir marboxil (Xofluza™), was approved for the treatment of influenza patients.107 By inhibiting virus polymerase activity, this antiviral provides a therapeutic option to combat viruses that are resistant to the other currently approved drugs targeting the influenza NA and M proteins.107
Conclusions
The phenotypic properties of influenza A viruses, such as receptor preference, shape the natural history and emergence of novel subtypes. Large populations of domestic birds and pigs provide a link between human activities and the natural reservoir of influenza viruses. Past human infections with either H5 or H7 viruses have provided the opportunity to study and understand viral factors involved in human transmissibility and virulence. Whereas multiple molecular markers in influenza genes have been linked to enhanced infection and replication in humans, determinants of zoonotic events are still not fully understood, largely due to a lack of systematic longitudinal surveillance across multiple hosts. Understanding the ecological and evolutionary context that drives the emergence of novel viruses in poultry and pig populations is also crucial to understanding zoonotic events and to possibly prevent, or at least prepare for future pandemics.
Funding
The authors are supported by the Duke-National University Singapore Signature Research Programme funded by the Ministry of Health, Singapore, and by contract HHSN272201400006C from the National Institute of Allergy and Infectious Disease, National Institutes of Health, US Department of Health and Human Services.
Conflict of interest statement
The authors have no potential conflicts of interest.
References
- 1. Webster RG, Bean WJ, Gorman OT, et al. Evolution and ecology of influenza A viruses. Microbiol Rev 1992;56:152–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Shi Y, Wu Y, Zhang W, et al. Enabling the 'host jump': structural determinants of receptor-binding specificity in influenza A viruses. Nat Rev Microbiol 2014;12:822–31. [DOI] [PubMed] [Google Scholar]
- 3. Shaw M, Palese P. Orthomyxoviridae In: Fields Virology, Vol. 1, 6th edn. Philadelphia: Lippincott, Williams & Wilkins, 2013 [Google Scholar]
- 4. Roberton SI, Bell DJ, Smith GJ, et al. Avian influenza H5N1 in viverrids: implications for wildlife health and conservation. Proc Biol Sci 2006;273:1729–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Vijaykrishna D, Mukerji R, Smith GJ. RNA virus reassortment: an evolutionary mechanism for host jumps and immune evasion. PLoS Pathog 2015;11:e1004902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Joseph U, Su YC, Vijaykrishna D, Smith GJ. The ecology and adaptive evolution of influenza A interspecies transmission. Influenza Other Respir Viruses 2017;11:74–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Medina RA, Garcia-Sastre A. Influenza A viruses: new research developments. Nat Rev Microbiol 2011;9:590–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. FAO Economic and Social Impacts of Avian Influenza. http://www.fao.org/avianflu/documents/Economic-and-social-impacts-of-avian-influenza-Geneva.pdf.
- 9. Chan PK. Outbreak of avian influenza A (H5N1) virus infection in Hong Kong in 1997. Clin Infect Dis 2002;34:S58–64. [DOI] [PubMed] [Google Scholar]
- 10. FAO EMPRES-i Global Animal Disease Information System. http://empres-i.fao.org/eipws3g/ (July 2019, data last assessed).
- 11. WHO Cumulative Number of Confirmed Human Cases of Avian Influenza A (H5N1) Reported to WHO. 2019. https://www.who.int/influenza/human_animal_interface/2019_05_10_tableH5N1.pdf?ua=1 (10 May 2019, date last accessed).
- 12. Gao R, Cao B, Hu Y, et al. Human infection with a novel avian-origin influenza A (H7N9) virus. N Engl J Med 2013;368:1888–97. [DOI] [PubMed] [Google Scholar]
- 13. FAO H7N9 Situation Update. http://www.fao.org/ag/againfo/programmes/en/empres/h7n9/situation_update.html (July 2019, data last assessed)
- 14. Kile JC, Ren R, Liu L, et al. Update: increase in human infections with novel Asian lineage avian Influenza A (H7N9) viruses during the fifth epidemic—China, October 1, 2016-August 7, 2017. MMWR Morb Mortal Wkly Rep 2017;66:928–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Widdowson MA, Bresee JS, Jernigan DB. The global threat of animal Influenza viruses of zoonotic concern: then and now. J Infect Dis 2017;216:S493–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Tong XC, Weng SS, Xue F, et al. First human infection by a novel avian influenza A (H7N4) virus. J Infect 2018;77:249–57. [DOI] [PubMed] [Google Scholar]
- 17. Beigel JH, Farrar J, Han AM, et al. Avian influenza A (H5N1) infection in humans. N Engl J Med 2005;353:1374–85. [DOI] [PubMed] [Google Scholar]
- 18. Gao HN, Lu HZ, Cao B, et al. Clinical findings in 111 cases of influenza A (H7N9) virus infection. N Engl J Med 2013;368:2277–85. [DOI] [PubMed] [Google Scholar]
- 19. Chen Y, Liang W, Yang S, et al. Human infections with the emerging avian influenza A H7N9 virus from wet market poultry: clinical analysis and characterisation of viral genome. Lancet 2013;381:1916–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Cheung CY, Poon LL, Lau AS, et al. Induction of proinflammatory cytokines in human macrophages by influenza A (H5N1) viruses: a mechanism for the unusual severity of human disease? Lancet 2002;360:1831–7. [DOI] [PubMed] [Google Scholar]
- 21. Liu J, Xiao H, Wu Y, et al. H7N9: a low pathogenic avian influenza A virus infecting humans. Curr Opin Virol 2014;5:91–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lai S, Qin Y, Cowling BJ, et al. Global epidemiology of avian influenza A H5N1 virus infection in humans, 1997-2015: a systematic review of individual case data. Lancet Infect Dis 2016;16:e108–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wang X, Jiang H, Wu P, et al. Epidemiology of avian influenza A H7N9 virus in human beings across five epidemics in mainland China, 2013–17: an epidemiological study of laboratory-confirmed case series. Lancet Infect Dis 2017;17:822–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cowling BJ, Jin L, Lau EH, et al. Comparative epidemiology of human infections with avian influenza A H7N9 and H5N1 viruses in China: a population-based study of laboratory-confirmed cases. Lancet 2013;382:129–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Freidl GS, Meijer A, de Bruin E, et al. Influenza at the animal-human interface: a review of the literature for virological evidence of human infection with swine or avian influenza viruses other than A (H5N1). Euro Surveill 2014;19:8–26. [DOI] [PubMed] [Google Scholar]
- 26. Watanabe Y, Ibrahim MS, Suzuki Y, Ikuta K. The changing nature of avian influenza A virus (H5N1). Trends Microbiol 2012;20:11–20. [DOI] [PubMed] [Google Scholar]
- 27. de Graaf M, Fouchier RA. Role of receptor binding specificity in influenza A virus transmission and pathogenesis. EMBO J 2014;33:823–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Yamada S, Suzuki Y, Suzuki T, et al. Haemagglutinin mutations responsible for the binding of H5N1 influenza A viruses to human-type receptors. Nature 2006;444:378–82. [DOI] [PubMed] [Google Scholar]
- 29. Watanabe Y, Ibrahim MS, Ellakany HF, et al. Acquisition of human-type receptor binding specificity by new H5N1 influenza virus sublineages during their emergence in birds in Egypt. PLoS Pathog 2011;7:e1002068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Glaser L, Stevens J, Zamarin D, et al. A single amino acid substitution in 1918 influenza virus hemagglutinin changes receptor binding specificity. J Virol 2005;79:11533–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Yahav S. Chapter 37—Regulation of body temperature: strategies and mechanisms In: Scanes CG. (ed.). Sturkie’s Avian Physiology, 6th edn. San Diego: Academic Press, 2015,869–905 [Google Scholar]
- 32. Quan C, Shi W, Yang Y, et al. New threats from H7N9 Influenza virus: spread and evolution of high- and low-pathogenicity variants with high genomic diversity in wave five. J Virol 2018;92:e00301-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Imai M, Watanabe T, Hatta M, et al. Experimental adaptation of an influenza H5 HA confers respiratory droplet transmission to a reassortant H5 HA/H1N1 virus in ferrets. Nature 2012;486:420–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Herfst S, Schrauwen EJ, Linster M, et al. Airborne transmission of influenza A/H5N1 virus between ferrets. Science 2012;336:1534–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. WHO Influenza at the Human-Animal Interface. 2018. https://www.who.int/influenza/human_animal_interface/Influenza_Summary_IRA_HA_interface_13_12_2018_FINAL.pdf?ua=1 (13 December 2018, date last accessed).
- 36. WHO H5N1 Highly Pathogenic Avian Influenza: Timeline of Major Events. 2014. http://www.who.int/influenza/human_animal_interface/h5n1_avian_influenza_update20140714.pdf.
- 37. WHO Human Infection with Avian Influenza A (H7N9) Virus—China. 2017. http://www.who.int/csr/don/15-march-2017-ah7n9-china/en/. (15 March 2017, date last accessed).
- 38. Ungchusak K, Auewarakul P, Dowell SF, et al. Probable person-to-person transmission of avian influenza A (H5N1). N Engl J Med 2005;352:333–40. [DOI] [PubMed] [Google Scholar]
- 39. Zhou L, Chen E, Bao C, et al. Clusters of human infection and human-to-human transmission of avian Influenza A (H7N9) virus, 2013-2017. Emerg Infect Dis 2018;24:397–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Munoz O, De Nardi M, van der Meulen K, et al. Genetic adaptation of influenza A viruses in domestic animals and their potential role in interspecies transmission: a literature review. EcoHealth 2016;13:171–98. [DOI] [PubMed] [Google Scholar]
- 41. Lipatov AS, Kwon YK, Sarmento LV, et al. Domestic pigs have low susceptibility to H5N1 highly pathogenic avian influenza viruses. PLoS Pathog 2008;4:e1000102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Isoda N, Sakoda Y, Kishida N, et al. Pathogenicity of a highly pathogenic avian influenza virus, A/chicken/Yamaguchi/7/04 (H5N1) in different species of birds and mammals. Arch Virol 2006;151:1267–79. [DOI] [PubMed] [Google Scholar]
- 43. Bui C, Bethmont A, Chughtai AA, et al. A systematic review of the comparative epidemiology of avian and human influenza A H5N1 and H7N9-lessons and unanswered questions. Transbound Emerg Dis 2015;12327. [DOI] [PubMed] [Google Scholar]
- 44. Kalthoff D, Globig A, Beer M. (Highly pathogenic) avian influenza as a zoonotic agent. Vet Microbiol 2010;140:237–45. [DOI] [PubMed] [Google Scholar]
- 45. Guan Y, Smith GJ. The emergence and diversification of panzootic H5N1 influenza viruses. Virus Res 2013;178:35–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Peiris JS, de Jong MD, Guan Y. Avian influenza virus (H5N1): a threat to human health. Clin Microbiol Rev 2007;20:243–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. FAO FAOSTAT. http://www.fao.org/faostat/en/#compare (June 2019, data last accessed).
- 48. Hulse-Post DJ, Sturm-Ramirez KM, Humberd J, et al. Role of domestic ducks in the propagation and biological evolution of highly pathogenic H5N1 influenza viruses in Asia. Proc Natl Acad Sci U S A 2005;102:10682–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Keawcharoen J, Van D, van Amerongen G, et al. Wild ducks as long-distance vectors of highly pathogenic avian influenza virus (H5N1). Emerg Infect Dis 2008;14:600–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Sonnberg S, Webby RJ, Webster RG. Natural history of highly pathogenic avian influenza H5N1. Virus Res 2013;178:63–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Offeddu V, Cowling BJ, Malik Peiris JS. Interventions in live poultry markets for the control of avian influenza: a systematic review. One Health 2016;2:55–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Hill NJ, Runstadler JA. A bird's eye view of Influenza A virus transmission: challenges with characterizing both sides of a co-evolutionary dynamic. Integr Comp Biol 2016;56:304–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Simms L, Jeggo M. Avian influenza from an ecohealth perspective. EcoHealth 2014;11:4–14. [DOI] [PubMed] [Google Scholar]
- 54. Global Consortium for HN, Related Influenza V Role for migratory wild birds in the global spread of avian influenza H5N8. Science 2016;354:213–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. El-Shesheny R, Barman S, Feeroz MM, et al. Genesis of Influenza A (H5N8) viruses. Emerg Infect Dis 2017;23:1368–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Xu X, Subbarao CNJ, Guo Y. Genetic characterization of the pathogenic influenza A/goose/Guangdong/1/96 (H5N1) virus: similarity of its hemagglutinin gene to those of H5N1 viruses from the 1997 outbreaks in Hong Kong. Virology 1999;261:15–9. [DOI] [PubMed] [Google Scholar]
- 57. Smith GJ, Donis RO. World Health Organization/world organisation for animal HF, agriculture organization HEWG. Nomenclature updates resulting from the evolution of avian influenza A(H5) virus clades 2.1.3.2a, 2.2.1, and 2.3.4 during 2013-2014. Influenza Other Respir Viruses 2015;9:271–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Guan Y, Peiris JS, Lipatov AS, et al. Emergence of multiple genotypes of H5N1 avian influenza viruses in Hong Kong SAR. Proc Natl Acad Sci U S A 2002;99:8950–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Guan Y, Shortridge KF, Krauss S, Webster RG. Molecular characterization of H9N2 influenza viruses: were they the donors of the "internal" genes of H5N1 viruses in Hong Kong? Proc Natl Acad Sci U S A 1999;96:9363–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Li KS, Guan Y, Wang J, et al. Genesis of a highly pathogenic and potentially pandemic H5N1 influenza virus in eastern Asia. Nature 2004;430:209–13. [DOI] [PubMed] [Google Scholar]
- 61. Bahl J, Pham TT, Hill NJ, et al. Ecosystem interactions underlie the spread of avian Influenza A viruses with pandemic potential. PLoS Pathog 2016;12:e1005620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. WHO Antigenic and genetic characteristics of zoonotic influenza viruses and development of candidate vaccine viruses for pandemic preparedness. https://www.who.int/influenza/vaccines/virus/201902_zoonotic_vaccinevirusupdate.pdf?ua=1 (February 2019, date last accessed).
- 63. Taubenberger JK, Morens DM. H5Nx panzootic bird flu—Influenza’s newest worldwide evolutionary tour. Emerg Infect Dis 2017;23:340. [Google Scholar]
- 64. Saito T, Tanikawa T, Uchida Y, et al. Intracontinental and intercontinental dissemination of Asian H5 highly pathogenic avian influenza virus (clade 2.3.4.4) in the winter of 2014-2015. Rev Med Virol 2015;25:388–405. [DOI] [PubMed] [Google Scholar]
- 65. Liu L, Zeng X, Chen P, et al. Characterization of clade 7.2 H5 avian Influenza viruses that continue to circulate in chickens in China. J Virol 2016;90:9797–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. WHO Avian Influenza Weekly Update Number 698. 2019. https://www.who.int/docs/default-source/wpro---documents/emergency/surveillance/avian-influenza/ai-20190719.pdf?sfvrsn=30d65594_28.
- 67. Yang ZF, Mok CK, Peiris JS, Zhong NS. Human infection with a novel avian Influenza A (H5N6) virus. N Engl J Med 2015;373:487–9. [DOI] [PubMed] [Google Scholar]
- 68. Bi Y, Chen Q, Wang Q, et al. Genesis, evolution and prevalence of H5N6 avian influenza viruses in China. Cell Host Microbe 2016;20:810–21. [DOI] [PubMed] [Google Scholar]
- 69. Lee DH, Bertran K, Kwon JH, Swayne DE. Evolution, global spread, and pathogenicity of highly pathogenic avian influenza H5Nx clade 2.3.4.4. J Vet Sci 2017;18:269–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Lee DH, Bahl J, Torchetti MK, et al. Highly pathogenic avian Influenza viruses and generation of novel reassortants, United States, 2014–2015. Emerg Infect Dis 2016;22:1283–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Hill NJ, Hussein IT, Davis KR, et al. Reassortment of Influenza A viruses in wild birds in Alaska before H5 clade 2.3.4.4 outbreaks. Emerg Infect Dis 2017;23:654–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Herfst S, Mok CKP, van den JMA, et al. Human clade 2.3.4.4 a/H5N6 Influenza virus lacks mammalian adaptation markers and does not transmit via the airborne route between ferrets. mSphere 2018;3:e00405–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Belser JA, Bridges CB, Katz JM, Tumpey TM. Past, present, and possible future human infection with influenza virus A subtype H7. Emerg Infect Dis 2009;15:859–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Capua I, Alexander DJ. Avian influenza: recent developments. Avian Pathol 2004;33:393–404. [DOI] [PubMed] [Google Scholar]
- 75. Fouchier RA, Schneeberger PM, Rozendaal FW, et al. Avian influenza A virus (H7N7) associated with human conjunctivitis and a fatal case of acute respiratory distress syndrome. Proc Natl Acad Sci U S A 2004;101:1356–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Centers for Disease C and Prevention Update: influenza activity--United States and worldwide, 2002–03 season, and composition of the 2003-04 influenza vaccine. MMWR Morb Mortal Wkly Rep 2003;52:516–21. [PubMed] [Google Scholar]
- 77. Koopmans M, Wilbrink B, Conyn M, et al. Transmission of H7N7 avian influenza A virus to human beings during a large outbreak in commercial poultry farms in the Netherlands. Lancet 2004;363:587–93. [DOI] [PubMed] [Google Scholar]
- 78. Kageyama T, Fujisaki S, Takashita E, et al. Genetic analysis of novel avian a(H7N9) influenza viruses isolated from patients in China, February to April 2013. Euro Surveill 2013;18:20453. [PMC free article] [PubMed] [Google Scholar]
- 79. WHO Human Infection with Avian Influenza A (H7N9) Web Update. 2013. http://www.wpro.who.int/outbreaks_emergencies/H7N9.update.30May2013.pdf?ua=1 (30 May 2013, date last accessed).
- 80. Lam TT, Wang J, Shen Y, et al. The genesis and source of the H7N9 influenza viruses causing human infections in China. Nature 2013;502:241–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Watanabe T, Watanabe S, Maher EA, et al. Pandemic potential of avian influenza A (H7N9) viruses. Trends Microbiol 2014;22:623–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. WHO Human Infection With Avian Influenza A (H7N9) Virus—China. 2017. http://www.who.int/csr/don/27-february-2017-ah7n9-china/en/ (27 February 2017, date last accessed).
- 83. Alexander DJ. An overview of the epidemiology of avian influenza. Vaccine 2007;25:5637–44. [DOI] [PubMed] [Google Scholar]
- 84. Sun Y, Liu J. H9N2 influenza virus in China: a cause of concern. Protein Cell 2015;6:18–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Shen H, Wu B, Li G, et al. H9N2 subtype avian Influenza viruses in China: current advances and future perspectives. Br J Virol 2014;1:54. [Google Scholar]
- 86. Peacock THP, James J, Sealy JE, Iqbal M. A global perspective on H9N2 avian Influenza virus. Viruses 2019;11:620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Shanmuganatham K, Feeroz MM, Jones-Engel L, et al. Antigenic and molecular characterization of avian influenza A (H9N2) viruses, Bangladesh. Emerg Infect Dis 2013;19:1393–1402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Matrosovich MN, Krauss S, Webster RG. H9N2 influenza A viruses from poultry in Asia have human virus-like receptor specificity. Virology 2001;281:156–62. [DOI] [PubMed] [Google Scholar]
- 89. WHO Influenza at the human-animal interface. 2016. http://www.who.int/influenza/human_animal_interface/Influenza_Summary_IRA_HA_interface_10_03_2016.pdf?ua=1 (3 October 2016, date last accessed).
- 90. Rahimi Rad S, Alizadeh A, Alizadeh E, Hosseini SM. The avian influenza H9N2 at avian-human interface: a possible risk for the future pandemics. J Res Med Sci 2016;21:51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Khan SU, Anderson BD, Heil GL, et al. A systematic review and meta-analysis of the seroprevalence of influenza A (H9N2) infection among humans. J Infect Dis 2015;212:562–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Liu M, Li X, Yuan H, et al. Genetic diversity of avian influenza A (H10N8) virus in live poultry markets and its association with human infections in China. Sci Rep 2015;5:7632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Matrosovich MN, Krauss S, Webster RG. H9N2 influenza A viruses from poultry in Asia have human virus-like receptor specificity. Virology 2001;281:156–62. [DOI] [PubMed] [Google Scholar]
- 94. PAHO Avian Influenza Virus A (H10N7) Circulating among Humans in Egypt. 2004. http://www1.paho.org/hq/dmdocuments/2010/Avian_Influenza_Egypt_070503.pdf.
- 95. Arzey GG, Kirkland PD, Arzey KE, et al. Influenza virus A (H10N7) in chickens and poultry abattoir workers, Australia. Emerg Infect Dis 2012;18:814–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Qi W, Zhou X, Shi W, et al. Genesis of the novel human-infecting influenza A(H10N8) virus and potential genetic diversity of the virus in poultry, China. Euro Surveill 2014;19:20841. [DOI] [PubMed] [Google Scholar]
- 97. Wei SH, Yang JR, Wu HS, et al. Human infection with avian influenza A H6N1 virus: an epidemiological analysis. Lancet Respir Med 2013;1:771–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Lee CC, Zhu H, Huang PY, et al. Emergence and evolution of avian H5N2 influenza viruses in chickens in Taiwan. J Virol 2014;88:5677–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Swayne DE. Impact of vaccines and vaccination on global control of avian influenza. Avian Dis 2012;56:818–28. [DOI] [PubMed] [Google Scholar]
- 100. Sims LD. Progress in control of H5N1 highly pathogenic avian influenza and the future for eradication. Avian Dis 2012;56:829–35. [DOI] [PubMed] [Google Scholar]
- 101. Yamayoshi S, Kawaoka Y. Current and future influenza vaccines. Nat Med 2019;25:212–20. [DOI] [PubMed] [Google Scholar]
- 102. Atsmon J, Kate-Ilovitz E, Shaikevich D, et al. Safety and immunogenicity of multimeric-001--a novel universal influenza vaccine. J Clin Immunol 2012;32:595–603. [DOI] [PubMed] [Google Scholar]
- 103. Yassine HM, Boyington JC, McTamney PM, et al. Hemagglutinin-stem nanoparticles generate heterosubtypic influenza protection. Nat Med 2015;21:1065–70. [DOI] [PubMed] [Google Scholar]
- 104. Moscona A. Global transmission of oseltamivir-resistant influenza. N Engl J Med 2009;360:953–6. [DOI] [PubMed] [Google Scholar]
- 105. Alame MM, Massaad E, Zaraket H. Peramivir: a novel intravenous neuraminidase inhibitor for treatment of acute Influenza infections. Front Microbiol 2016;7:450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. CDC H5N1 Genetic Changes Inventory. 2012. https://www.cdc.gov/flu/avianflu/h5n1/inventory.htm.
- 107. Hayden FG, Sugaya N, Hirotsu N, et al. Baloxavir marboxil for uncomplicated Influenza in adults and adolescents. N Engl J Med 2018;379:913–23. [DOI] [PubMed] [Google Scholar]


