Abstract
Arthroscopic techniques for anterior talofibular ligament (ATFL) repair and reconstruction have been developed in recent years. We simultaneously performed anatomical arthroscopic ATFL repair and reconstruction using a free tendon graft. The ATFL remnant is carefully dissected only at the footprint of the superior limb of the ATFL, and a bone tunnel is created on each side of the fibula and talus. A soft suture anchor with 2 sets of threads is inserted into the fibular tunnel. One set of threads is used to grab the ATFL remnant via a lasso-loop technique, whereas the other set of threads is used to introduce the ATFL graft. The graft is first fixed with a screw in the talar tunnel. Subsequently, the ATFL remnant and the graft are tightened simultaneously by pulling the 2 sets of suture anchor threads at the fibular tunnel and are fixed with a screw. This technique provides the possible advantages of remnant preservation and promotion of load sharing by the repaired ATFL remnant and the reconstructed ATFL graft.
The anterior talofibular ligament (ATFL) is the most frequently injured ligament in ankle sprains.1 The Broström technique is the most popular procedure for repairing the ruptured ATFL.2 However, because the repair's strength depends on ATFL remnant quality, postoperative results may be poor when much time has passed after an ankle sprain, a patient is obese, and/or a high-demand athlete sustains repeated ankle sprains. A ligament reconstruction method using a free tendon is indicated in such cases.3, 4 A few technical reports5, 6, 7, 8, 9 and short-term clinical results10, 11, 12, 13 of arthroscopic lateral ankle ligament reconstruction have been published. Recently, remnant-preserved anterior cruciate ligament (ACL) reconstruction has gained popularity because the remnant-preservation effect may be advantageous for graft remodeling, proprioceptive recovery, and clinical outcomes.14, 15, 16
We describe the technique of anatomical arthroscopic ATFL repair and reconstruction (AAARR) using a free tendon graft, which has the possible advantages of not only remnant preservation but also sharing of the ligament load by the repaired ATFL remnant and the reconstructed ATFL graft. A summary of the key steps is provided in Table 1, and a summary of the technique is shown in Video 1.
Table 1.
Pearls and Pitfalls of Key Surgical Steps
| Key Surgical Step | Pearls | Pitfalls |
|---|---|---|
| Creation of AM portal | The ankle is positioned neutrally. The AM portal is created medial and slightly proximal to the joint line. | If the AM portal is created too medially or too distally, visualization of the ATFL remnant will be difficult. |
| Creation of AAL portal | The ankle is dorsiflexed to view the ATFL remnant. Before the AAL portal is created, a needle is inserted into the portal site to confirm accessibility to the talar footprint of the ATFL superior limb. | If the AAL portal is created without confirmation by the needle, the AAL portal position will not be suitable for talar tunnel creation. |
| Creation of talar tunnel | A microfracture awl is used to mark the center of the ATFL talar footprint, and a guidewire is inserted through the AAL portal to drill the talus toward the distal end of the medial malleolus. | A guidewire may slip at the ATFL talar footprint without marking. If the guidewire is directed too posteriorly, the neurovascular bundle is at risk of damage. If the tunnel is deeper than 20 mm, the risk of talar penetration may be higher. |
| Creation of ST portal | The ST portal is created just below the distal end of the fibula after confirmation of accessibility to the fibular footprint by a needle. | If the ST portal is created too anteriorly, the fibular tunnel direction will be distal and the risk of tunnel fracture will be higher. |
| Creation of fibular tunnel | Intraoperative fluoroscopy is used to confirm the guidewire insertion position and direction. The insertion point should be proximal to the articular tip and the FOT. | If the fibular tunnel is created without fluoroscopic assistance, the risks of tunnel fracture and malposition may be higher. If the fibular tunnel is created below the FOT, the CFL footprint may be damaged. |
| Suture anchor placement | A soft suture anchor, which has 2 sets of threads, is placed at the fibular cortex behind the fibular tunnel. | If the suture anchor is placed inside the fibular bone, the fixation strength will be weak and the suture anchor may drop out during surgery. |
| ATFL remnant repair | An 18-gauge hollow needle or a suture passer penetrates the ATFL inferior limb remnant to grab the ATFL remnant using the lasso-loop technique. | If a smaller amount of the ATFL remnant is grasped, the mechanical strength of the remnant repair via a lasso loop will weaken. |
| Graft fixation | The graft is fixed with a screw in the talar tunnel first. Subsequently, the ATFL remnant and the ATFL graft are tightened simultaneously by pulling the 2 sets of suture anchor threads at the fibular tunnel. | If the graft is fixed in the fibular tunnel first, the remnant and the graft cannot be tightened simultaneously because neither shares the load. |
AAL, accessory anterolateral; AM, anteromedial; ATFL, anterior talofibular ligament; CFL, calcaneofibular ligament; FOT, fibular obscure tubercle; ST, subtalar.
Surgical Technique
Step 1: Patient Positioning
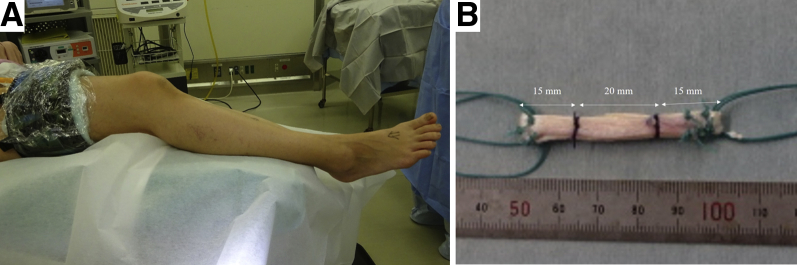
This surgical procedure is performed with the patient in the supine position under general anesthesia. A tourniquet is placed on the proximal thigh. The foot is suspended from the distal edge of the bed, and the contralateral leg is slightly lowered to provide a wide working space (Fig 1A).8
Fig 1.
Patient position and graft preparation (patient 1). (A) The right ankle is the operative side. The surgical procedure is performed with the patient under general anesthesia in the supine position. A tourniquet is placed on the proximal thigh. The foot is suspended from the distal edge of the bed. The contralateral leg (left ankle) is slightly lowered to provide a wide working space. (B) The gracilis tendon is harvested from the pes anserinus, and a 2- or 3-strand graft is prepared. Tendon allograft is an alternative. The harvested tendon usually needs to be longer than 100 mm and contains an approximately 20-mm-long 2-strand bundle for the anterior talofibular ligament (ATFL). The length is determined on preoperative magnetic resonance imaging. The 2 ends form a 15-mm-long loop to facilitate attachment of the thread for graft delivery. The recommended graft diameter is 4.5 to 6.0 mm. Because the harvested tendon is thin and longer than 150 mm in this case, the graft is folded into a 3-strand bundle for the ATFL.
Step 2: Graft Preparation
The autogenous gracilis tendon is harvested from the pes anserinus, and a 2- or 3-strand graft is prepared. Use of the endoscopic harvest technique is recommended to ensure a smaller scar.17 Tendon allograft is an alternative. The harvested tendon usually needs to be longer than 100 mm to contain a 2-strand bundle for the ATFL that is at least 20 mm long. The length is determined on preoperative magnetic resonance imaging. The 2 ends form a 15-mm-long loop to facilitate attachment of the thread for graft delivery (Fig 1B). The recommended graft diameter is 4.5 to 6.0 mm. If the harvested tendon is thin and longer than 150 mm, the graft can be folded into a 3-strand bundle for the ATFL.
Step 3: Portal Placement of Ankle Arthroscopy
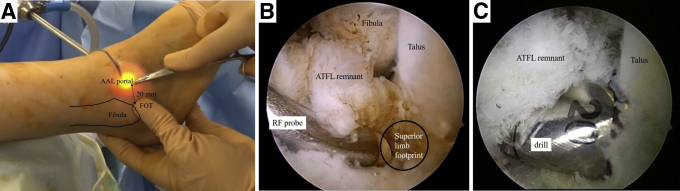
Three portals are created in a step-by-step manner: anteromedial (AM), accessory anterolateral (AAL), and subtalar (ST). The ankle is positioned neutrally. The AM portal is created medial to the anterior tibial tendon8 and slightly proximal to the joint line. A 30° 2.7- or 4.0-mm-diameter arthroscope is introduced through the AM portal. The ATFL remnant is viewed with the ankle in a dorsiflexed position. After a needle is inserted into the portal site to confirm accessibility to the talar attachment site of the ATFL superior limb, the AAL portal is created. The portal is usually created at approximately 20 mm anterior to the anteroinferior tubercle of the distal fibula, called the fibular obscure tubercle (FOT)18, 19 (Fig 2A). The conventional anterolateral portal is created only if necessary for the treatment of other lesions (e.g. osteochondral lesions).
Fig 2.
Creation of accessory anterolateral (AAL) portal and talar tunnel (right ankle). (A) An arthroscope is introduced through the anteromedial portal. The ankle is dorsiflexed to view the anterior talofibular ligament (ATFL) remnant. Before the AAL portal is created, a needle is inserted into the portal site to confirm accessibility of the ATFL talar footprint. The portal is usually created at a point approximately 20 mm anterior to the fibular obscure tubercle (FOT).19 (B) The ATFL remnant is carefully dissected to only the minimum necessary area for tunnel creation at the talar and fibular footprint of the superior limb of the ATFL using a radiofrequency (RF) probe. (C) A microfracture awl is used to mark the center of the ATFL talar footprint, and a 2.4-mm guidewire is inserted through the AAL portal to drill the talus from the ATFL footprint toward the distal end of the medial malleolus. The guidewire is then over-drilled using a drill bit with the same diameter as the graft end to create a 20-mm-deep talar tunnel. (Fig 2A is from patient 1 whereas Figs 2B and 2C are from patient 2 because of image quality.)
Step 4: Tunnel Creation
The ATFL remnant is carefully dissected to only the minimum necessary area for tunnel creation at the talar and fibular footprint of the superior limb of the ATFL using a radiofrequency probe (Fig 2B). A microfracture awl is used to mark the center of the dissected footprint, and a 2.4-mm guidewire is inserted through the AAL portal to drill the talus toward the distal end of the medial malleolus.20 The guidewire is then over-drilled using a drill bit with the same diameter as the graft end to create a 20-mm-deep talar tunnel (Fig 2C).
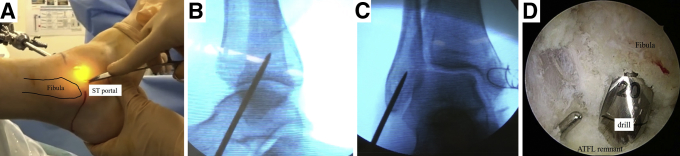
When the fibular footprint of the ATFL superior limb is not adequately viewed through the AM portal, the surgeon can try to dorsiflex the ankle, change the scope to a 70° arthroscope, or place the scope through the AAL portal. The ST portal is created just below the distal end of the fibula after a needle confirms accessibility of the fibular footprint (Fig 3A). A guidewire is inserted through the ST portal to drill the fibula. Intraoperative fluoroscopy is used to confirm the guidewire insertion position and direction. The insertion point should be proximal to the articular tip and the FOT.19 The angle between the guidewire direction and the long axis of the fibula on the lateral view is 10° to 30° (Fig 3B) and almost on the angle bisector of the fibular end on the anteroposterior view (Fig 3C). Viewed from the AM or AAL portal, the guidewire is then over-drilled to create a 20-mm-deep fibular tunnel (Fig 3D). The surgeon must be careful not to dissect the footprint of the inferior limb of the ATFL because it usually connects with calcaneofibular ligament (CFL) footprint.21, 22, 23
Fig 3.
Creation of subtalar (ST) portal and fibular tunnel (right ankle). (A) The ST portal is created just below the distal end of the fibula after confirmation of accessibility of the fibular footprint by a needle. (B) A guidewire is inserted through the ST portal. Intraoperative fluoroscopy is used to confirm the guidewire position. The insertion point should be proximal to the articular tip and the fibular obscure tubercle.19 The angle between the guidewire direction and the long axis of the fibula on the lateral view is 10° to 30°. (C) The guidewire direction is almost on the angle bisector of the fibular end on the anteroposterior view. (D) Viewed from the anteromedial or accessory anterolateral portal, the guidewire is over-drilled to create a 20-mm-deep fibular tunnel. (Figs 3A, 3B, and 3C are from patient 1 whereas Figure 3D is from patient 2 because of image quality.)
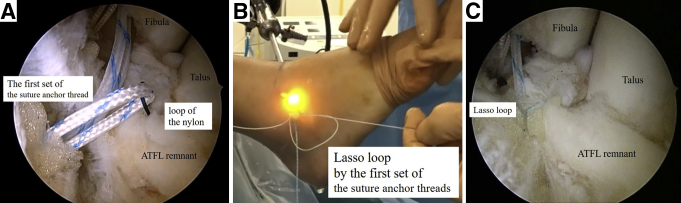
Step 5: Suture Anchor Placement and ATFL Remnant Repair
The surgeon penetrates the fibular tunnel bottom to the opposite cortex using a 2.9-mm drill wire through the ST portal. If it does not reach the opposite cortex, the drill wire is inserted anteriorly from the anterior edge of the tunnel inlet to the posterior and proximal end to penetrate the posterior cortical wall of the fibula.8 A 2.9-mm JuggerKnot Soft Anchor (Zimmer Biomet, Warsaw, IN), which has 2 sets of threads, is placed at the fibular cortex behind the fibular tunnel. The first set of threads is used to grasp the ATFL remnant via a lasso-loop technique.24 An 18-gauge hollow needle with No. 2-0 nylon thread penetrates the ATFL inferior limb remnant25, 26 through the AAL or ST portal depending on the accessibility to the remnant. A suture passer, such as the Micro SutureLasso (Arthrex, Naples, FL) or SpeedSnare (Zimmer Biomet), is also useful for grasping the ATFL remnant. The loop of the nylon is retrieved through the same portal using a grasping instrument, and the needle is withdrawn. One end of the first set of suture anchor threads is passed through the nylon loop. The nylon loop is then used to pull just the mid portion of the suture anchor through the ATFL remnant, creating a suture loop in the ATFL remnant (Fig 4A). The free end of the first thread set is passed through this loop and pulled tight, creating a self-cinching lasso loop (Fig 4B). The other end of the first thread set is then used to draw the lasso loop, tightening the ATFL remnant (Fig 4C).
Fig 4.
Suture anchor placement and anterior talofibular ligament (ATFL) remnant repair (right ankle). (A) The surgeon penetrates from the fibular tunnel bottom to the opposite cortex with a 2.9-mm drill wire through the subtalar portal. A 2.9-mm JuggerKnot Soft Anchor, which has 2 sets of threads, is placed at the fibular cortex behind the fibular tunnel. The first set of suture anchor threads is used to grab the ATFL remnant via a lasso-loop technique. An 18-gauge hollow needle with No. 2-0 nylon thread penetrates the ATFL remnant through the accessory anterolateral or subtalar portal depending on the accessibility of the remnant. The nylon loop is retrieved through the same portal using a grasping instrument, and the needle is withdrawn. One end of the first thread set is then passed through the nylon loop, which is used to pull just the mid portion of the suture anchor through the ATFL remnant such that a suture loop is created in the ATFL remnant. (B) The free end of the first set of suture anchor threads is passed through the loop and pulled tight, creating a self-cinching lasso loop. (C) The other end of the first thread set is used to draw the lasso loop, tightening the ATFL remnant. (Figs 4A and 4C are from patient 2 whereas Fig 4B is from patient 1 because of image quality.)
Step 6: Tendon Graft Introduction and Fixation
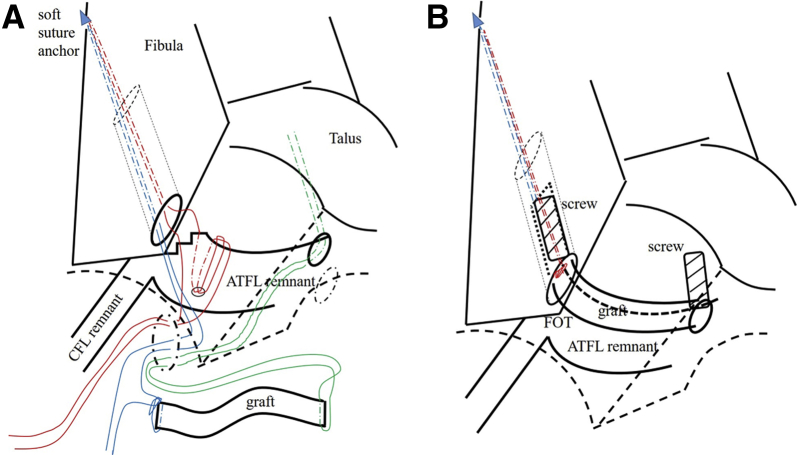
The second set of suture anchor threads, which is not used to repair the ATFL remnant, is used to introduce the ATFL graft. One strand is sutured and connected to the fibular end of the graft. The other strand is pulled for the later graft introduction (Fig 5A). A 1.6-mm passing pin (Meira, Nagoya, Japan) is inserted into the talar tunnel through the AAL portal and penetrates the bone and skin on the opposite side. A looped thread is passed through the eye of the passing pin. The passing pin is pulled out to the opposite side. The looped thread penetrating the talar tunnel is led from the AAL portal to the ST portal. The tendon graft is introduced from the ST portal into the talar tunnel by pulling the looped threads and into the fibular tunnel by pulling the other strand of the second suture anchor thread as mentioned earlier (Fig 6A). The graft is fixed with a 15-mm-long bioabsorbable interference screw in the talar tunnel. Subsequently, the ATFL remnant and graft are tightened simultaneously by pulling the 2 sets of suture anchor threads at the fibular tunnel (Fig 5B). They are fixed together with another screw with the ankle in approximately 30° to 45° of plantar flexion to avoid postoperative plantar flexion restrictions. Both sets of suture anchor threads are tied in situ by conventional tying for security just in case the screw happens to drop out from the fibular bone tunnel postoperatively (Fig 5, Fig 6C and 6B). If the fibular bone is weak because of osteoporosis or a patient's low activity level, a smaller screw is chosen; alternatively, the 2 sets of suture anchor threads are tied without screw fixation while the ATFL remnant and graft are tightened. The insertion of a larger screw into the fibular tunnel may cause wall fracture in these patients. If the screw is not firmly fixed, the screw size is changed to a larger size or the cancellous bone tips are grafted to the space between the tunnel and the tendon graft.8
Fig 5.
Passing pin direction in fibular tunnel (right ankle). (A) The second set of suture anchor threads is used to introduce the anterior talofibular ligament (ATFL) graft. One strand is sutured and connected to the fibular end of the graft, whereas the other strand is pulled for graft introduction. (B) The tendon graft is introduced from the subtalar portal into the talar tunnel by using the passing pin (Meira) and into the fibular tunnel by pulling the other strand of the second suture anchor thread. The graft is fixed with an appropriate-diameter 15-mm-long bioabsorbable interference screw in the talar tunnel first. Subsequently, the ATFL remnant and graft are tightened simultaneously by pulling the 2 sets of suture anchor threads at the fibular tunnel. (C) The ATFL remnant and graft are fixed together with another screw with the ankle in an approximately 30° to 45° plantar flexion position to avoid postoperative plantar flexion restrictions. Both sets of suture anchor threads are tied in situ by conventional tying. The ATFL graft is lying over the ATFL remnant. (Figs 5A and 5B are from patient 1 whereas Fig 5C is from patient 2 because of image quality.)
Fig 6.
Technique in right ankle. (A) The anterior talofibular ligament (ATFL) remnant is sutured by the first set of suture anchor threads using the lasso-loop technique. The graft is prepared for introduction through the subtalar portal. (B) The ATFL remnant is repaired and the graft is fixed with a 15-mm-long bioabsorbable interference screw simultaneously after screw fixation in the talar tunnel. The red lines indicate the first set of soft suture anchor threads; blue lines, the second set of soft suture anchor threads; and green lines, a loop thread penetrating the talar tunnel. (CFL, calcaneofibular ligament; FOT, fibular obscure tubercle.).
Discussion
Ankle sprains are the most common injuries during sports activities.3, 4 Chronic ankle instability has been reported in up to 70% of patients.27 The ATFL is the most frequently injured ligament in ankle sprains.1 Although the Broström technique is the most popular procedure for repairing a ruptured ATFL,2 the repair's strength depends on ATFL remnant quality, which is thought to be weaker than the intact ATFL. Therefore, postoperative results may be poor when a long time has passed after an ankle sprain, a patient is obese, and/or a high-demand athlete sustains repeated ankle sprains. A ligament reconstruction method using a free tendon is indicated in these patients.3, 4 Whether CFL reconstruction is added or not remains controversial,4 however; we consider reconstructing only the ATFL when the plantar flexion and external rotational stress test9, 28 results are negative, indicating a hard endpoint and no apprehension, or when the talar tilt angle is less than 10°.
Remnant-preserved ACL reconstruction is gaining popularity because the remnant-preservation effect may have the advantages of synovial coverage of the graft, graft remodeling, proprioceptive recovery, stability, and better clinical outcomes,14, 15, 16, 29 although controversial reports exist.30, 31 However, most remnant-preserved ACL reconstructions do not repair the remnant. This means that the load does not conduct to the remnant and the remnant does not share the stress. Although one Technical Note has described an ACL remnant-preservation technique that repaired the remnant via the lasso-loop technique,14 the remnant and the graft were not simultaneously fixed. Thus, they may not share the load owing to stress shielding.
Several technical reports5, 6, 7, 8, 9 and short-term clinical results10, 11, 12, 13 of arthroscopic lateral ankle ligament reconstruction have been published. Although the remnant-preserving technique has already been reported in 2 studies,32, 33 neither study repaired the remnant. On the contrary, the ATFL remnant and graft can share the load in our procedure because they are simultaneously fixed with the screw at the fibular tunnel.
Intraoperative fluoroscopy is used to confirm the guidewire insertion position and guidewire direction to ensure the correct fibular tunnel position and safe creation of the fibular tunnel,8 respectively. Because the center of the ATFL origin on the fibula is located 3.7 mm (range, 0-6.7 mm) proximal to the FOT,19 the fibular tunnel of the ATFL superior limb should be created proximal to the FOT. Tunnel creation distal to the FOT may damage the CFL footprint.8, 19
Drawbacks of our technique include the need to dissect the footprint of the ATFL superior limb to create the anatomic bone tunnels, which may potentially weaken the remnant strength. However, the superior limb remnant can remain in place as much as possible through careful dissection of only the minimum necessary area for tunnel creation to preserve the ATFL inferior limb remnant. Thus, mechanical stabilization of the repair technique can be added to the ATFL reconstruction to some degree. The advantages and disadvantages of the technique are described in Table 2.
Table 2.
Advantages and Disadvantages
| Advantages |
| Possibly better ATFL strength, graft maturation, ankle proprioception, and long-term clinical results |
| Safe and reproducible tunnel creation |
| Anatomic reconstruction and less postoperative risk of ROM restriction |
| Only 3 portals in total, including 2 for viewing |
| Optional technique for graft fixation in fibular tunnel in patients with lower bone quality |
| Disadvantages |
| Footprint dissection of ATFL superior limb remnant may weaken strength of repair technique |
| Possible risk of tunnel fracture |
| Need for basic arthroscopic skills |
| Use of intraoperative fluoroscopy |
ATFL, anterior talofibular ligament; ROM, range of motion.
AAARR has the possible advantage of not only remnant preservation but also sharing of the ligament load by the repaired ATFL remnant and the reconstructed ATFL graft. Thus, ATFL strength, graft maturation, ankle proprioception, and long-term clinical results are expected to improve after AAARR.
Acknowledgment
The authors thank Editage (www.editage.jp) for English-language editing.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Surgical technique for anatomic arthroscopic anterior talofibular ligament (ATFL) repair and reconstruction using a free tendon in the right ankle. This surgical procedure is performed with the patient under general anesthesia in the supine position. A tourniquet is placed on the proximal thigh. The foot is suspended from the distal edge of the bed. The contralateral leg is slightly lowered to provide a wide working space. A 2- or 3-strand graft is prepared using the gracilis tendon or a tendon allograft. It contains an approximately 20-mm-long bundle for the ATFL. The length is determined on preoperative magnetic resonance imaging. The 2 ends form a 15-mm-long loop to facilitate thread attachment for graft delivery. The recommended graft diameter is 4.5 to 6.0 mm. Three portals are created in a step-by-step manner: a conventional anteromedial (AM) portal, an accessory anterolateral (AAL) portal, and a subtalar (ST) portal. The ankle is positioned neutrally. The AM portal is created medial to the anterior tibial tendon and slightly proximal to the joint line. A 30° 2.7- or 4.0-mm-diameter arthroscope is introduced through the AM portal. The ATFL remnant is viewed with the ankle in a dorsiflexed position. After a needle is inserted into the portal site to confirm accessibility to the talar attachment site of the ATFL superior limb, the AAL portal is created. The portal is usually created approximately 20 mm anterior to the anteroinferior tubercle of the distal fibula, which is called the “fibular obscure tubercle” (FOT). The ATFL remnant is carefully dissected to only the minimum necessary area for tunnel creation at the talar and fibular footprint of the superior limb of the ATFL using a radiofrequency (RF) probe. A microfracture awl is used to mark the center of the dissected footprint, and a 2.4-mm guidewire is inserted through the AAL portal to drill the talus toward the distal end of the medial malleolus. The guidewire is then over-drilled to create a 20-mm-deep talar tunnel. The ST portal is created just below the distal end of the fibula after confirmation of accessibility of the fibular footprint by a needle. A guidewire is inserted through the ST portal to drill the fibula. Intraoperative fluoroscopy is used to confirm the guidewire insertion position and direction. The insertion point should be proximal to the articular tip and the FOT. The angle between the guidewire direction and the long axis of the fibula on the lateral view is 10° to 30° and almost on the angle bisector of the fibular end on the anteroposterior view. The guidewire is then over-drilled to create a 20-mm-deep fibular tunnel. The surgeon penetrates from the fibular tunnel bottom to the opposite cortex with a 2.9-mm drill wire through the ST portal. A 2.9-mm JuggerKnot Soft Anchor, which has 2 sets of threads, is placed at the fibular cortex behind the fibular tunnel. The first set of threads is used to grab the ATFL remnant via a lasso-loop technique. An 18-gauge hollow needle with a 2-0 nylon thread is penetrated to the ATFL inferior limb remnant through the AAL portal or ST portal, depending on the accessibility to the remnant. A suture passer (e.g. Micro SutureLasso or SpeedSnare) is also useful to grasp the ATFL remnant. The nylon loop is retrieved through the same portal using a grasping instrument, and the needle is withdrawn. One end of the first set of suture anchor threads is passed through the nylon loop, which is then used to pull just the mid portion of the suture anchor through the ATFL remnant so that a suture loop is created in the ATFL remnant. The free end of the first thread set is passed through this loop and pulled tight, creating a self-cinching lasso loop. The other end of the first thread set is then used to draw the lasso loop, tightening the ATFL remnant. The second set of suture anchor threads, which is not used to repair the ATFL remnant, is used to introduce the ATFL graft. One strand is sutured and connected to the fibular end of the graft. The other strand is pulled for the graft introduction later. A 1.6-mm passing pin (Meira) is inserted into the talar tunnel through the AAL portal. This pin penetrates the bone and skin on the opposite side. A looped thread is passed through the eye of the passing pin, which is pulled out to the opposite side. The looped thread penetrating the talar tunnel needs to be led from the AAL portal to the ST portal. The tendon graft is introduced from the ST portal into the talar tunnel by pulling the looped threads and into the fibular tunnel by pulling the other strand of the second suture anchor thread. The graft is fixed with a 15-mm-long bioabsorbable interference screw in the talar tunnel first. Subsequently, the ATFL remnant and the ATFL graft are tightened simultaneously by pulling the 2 sets of suture anchor threads at the fibular tunnel. They are fixed together with another screw, with the ankle in an approximately 30° to 45° plantar flexion position. Both sets of suture anchor threads are tied in situ using a conventional knot. The video was created using the records of patients 1, 2, and 3 because of image quality and for the purpose of showing several optional techniques.
References
- 1.Ferran N.A., Maffulli N. Epidemiology of sprains of the lateral ankle ligament complex. Foot Ankle Clin. 2006;11:659–662. doi: 10.1016/j.fcl.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 2.Broström L., Sprained ankles VI. Surgical treatment of “chronic” ligament ruptures. Acta Chir Scand. 1966;132:551–565. [PubMed] [Google Scholar]
- 3.Guillo S., Bauer T., Lee J.W. Consensus in chronic ankle instability: Aetiology, assessment, surgical indications and place for arthroscopy. Orthop Traumatol Surg Res. 2013;99:S411–S419. doi: 10.1016/j.otsr.2013.10.009. [DOI] [PubMed] [Google Scholar]
- 4.Michels F., Pereira H., Calder J. Searching for consensus in the approach to patients with chronic lateral ankle instability: Ask the expert. Knee Surg Sports Traumatol Arthrosc. 2018;26:2095–2102. doi: 10.1007/s00167-017-4556-0. [DOI] [PubMed] [Google Scholar]
- 5.Lui T.H. Arthroscopic-assisted lateral ligamentous reconstruction in combined ankle and subtalar instability. Arthroscopy. 2007;23:554.e1–554.e5. doi: 10.1016/j.arthro.2006.07.038. [DOI] [PubMed] [Google Scholar]
- 6.Guillo S., Archbold P., Perera A., Bauer T., Sonnery-Cottet B. Arthroscopic anatomic reconstruction of the lateral ligaments of the ankle with gracilis autograft. Arthrosc Tech. 2014;3:e593–e598. doi: 10.1016/j.eats.2014.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Takao M., Glazebrook M., Stone J., Guillo S. Ankle arthroscopic reconstruction of lateral ligaments (ankle anti-ROLL) Arthrosc Tech. 2015;4:e595–e600. doi: 10.1016/j.eats.2015.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Higashiyama R., Aikawa J., Iwase D., Takamori Y., Watanabe E., Takaso M. Anatomical arthroscopic anterior talofibular ligament and calcaneofibular ligament reconstruction using an autogenic hamstring tendon: Safe creation of anatomical fibular tunnel. Arthrosc Tech. 2019;8:e215–e222. doi: 10.1016/j.eats.2018.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Higashiyama R. Arthroscopic reconstruction of the posterior talofibular, anterior talofibular, and calcaneofibular ligaments: Scopic PAC. In: Lui T.H., editor. Arthroscopy and endoscopy of the foot and ankle: Principle & practice. Springer Singapore; Singapore: 2019. pp. 159–169. [Google Scholar]
- 10.Song B., Li C., Chen N. All-arthroscopic anatomical reconstruction of anterior talofibular ligament using semitendinosus autografts. Int Orthop. 2017;41:975–982. doi: 10.1007/s00264-017-3410-9. [DOI] [PubMed] [Google Scholar]
- 11.Higashiyama R., Aikawa J., Iwase D. Arthroscopic anterior talofibular ligament reconstruction using a gracilis tendon. Knee Surg Sports Traumatol Arthrosc. 2014;22(suppl 1):S324–S325. [Google Scholar]
- 12.Vila-Rico J., Cabestany-Castella J.M., Cabestany-Perich B., Nunez-Samper C., Ojeda-Thies C. All-inside arthroscopic allograft reconstruction of the anterior talo-fibular ligament using an accessory transfibular portal. Foot Ankle Surg. 2019;25:24–30. doi: 10.1016/j.fas.2017.12.008. [DOI] [PubMed] [Google Scholar]
- 13.Lopes R., Andrieu M., Cordier G. Arthroscopic treatment of chronic ankle instability: Prospective study of outcomes in 286 patients. Orthop Traumatol Surg Res. 2018;104:S199–S205. doi: 10.1016/j.otsr.2018.09.005. [DOI] [PubMed] [Google Scholar]
- 14.Boutsiadis A., Karampalis C., Tzavelas A., Vraggalas V., Christodoulou P., Bisbinas I. Anterior cruciate ligament remnant-preserving reconstruction using a “lasso-loop” knot configuration. Arthrosc Tech. 2015;4:e741–e746. doi: 10.1016/j.eats.2015.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Takahashi T., Kondo E., Yasuda K. Effects of remnant tissue preservation on the tendon graft in anterior cruciate ligament reconstruction: A biomechanical and histological study. Am J Sports Med. 2016;44:1708–1716. doi: 10.1177/0363546516643809. [DOI] [PubMed] [Google Scholar]
- 16.Kim S.J., Choi C.H., Chun Y.M. Anterior cruciate ligament reconstruction using bone-patellar tendon-bone autograft with remnant preservation: Comparison of outcomes according to the amount of remnant tissue. J Knee Surg. 2019;32:847–859. doi: 10.1055/s-0038-1669902. [DOI] [PubMed] [Google Scholar]
- 17.Yeh W.L., Chen J.M., Liu C.H., Tsai P.J., Higashiyama R., Takaso M. Endoscopic harvest of autogenous gracilis and semitendinosus tendons. Arthrosc Tech. 2018;7:e1019–e1024. doi: 10.1016/j.eats.2018.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Buzzi R., Todescan G., Brenner E., Segoni F., Inderster A., Aglietti P. Reconstruction of the lateral ligaments of the ankle: An anatomic study with evaluation of isometry. J Sports Traumatol Relat Res. 1993;15:55–74. [Google Scholar]
- 19.Matsui K., Oliva X.M., Takao M. Bony landmarks available for minimally invasive lateral ankle stabilization surgery: A cadaveric anatomical study. Knee Surg Sports Traumatol Arthrosc. 2017;25:1916–1924. doi: 10.1007/s00167-016-4218-7. [DOI] [PubMed] [Google Scholar]
- 20.Michels F., Guillo S., Vanrietvelde F., Brugman E., Stockmans F. How to drill the talar tunnel in ATFL reconstruction? Knee Surg Sports Traumatol Arthrosc. 2016;24:991–997. doi: 10.1007/s00167-016-4018-0. [DOI] [PubMed] [Google Scholar]
- 21.Golano P., Vega J., Perez-Carro L., Gotzens V. Ankle anatomy for the arthroscopist. Part II: Role of the ankle ligaments in soft tissue impingement. Foot Ankle Clin. 2006;11:275–296. doi: 10.1016/j.fcl.2006.03.003. v-vi. [DOI] [PubMed] [Google Scholar]
- 22.Matsui K., Takao M., Tochigi Y., Ozeki S., Glazebrook M. Anatomy of anterior talofibular ligament and calcaneofibular ligament for minimally invasive surgery: A systematic review. Knee Surg Sports Traumatol Arthrosc. 2017;25:1892–1902. doi: 10.1007/s00167-016-4194-y. [DOI] [PubMed] [Google Scholar]
- 23.Edama M., Kageyama I., Kikumoto T. Morphological features of the anterior talofibular ligament by the number of fiber bundles. Ann Anat. 2018;216:69–74. doi: 10.1016/j.aanat.2017.11.001. [DOI] [PubMed] [Google Scholar]
- 24.Lafosse L., Van Raebroeckx A., Brzoska R. A new technique to improve tissue grip: “The lasso-loop stitch. Arthroscopy. 2006;22 doi: 10.1016/j.arthro.2006.05.021. 1246.e1-1246.e3. [DOI] [PubMed] [Google Scholar]
- 25.Takao M., Matsui K., Stone J.W. Arthroscopic anterior talofibular ligament repair for lateral instability of the ankle. Knee Surg Sports Traumatol Arthrosc. 2016;24:1003–1006. doi: 10.1007/s00167-015-3638-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Higashiyama R., Aikawa J., Iwase D. Arthroscopic anatomical anterior talofibular ligament repair and reconstruction using an allogenic iliotibial tract graft: A case report. J Jpn Orthop Soc Knee Arthrosc Sports Med. 2018;43:859–865. [Google Scholar]
- 27.Yeung M.S., Chan K.M., So C.H., Yuan W.Y. An epidemiological survey on ankle sprain. Br J Sports Med. 1994;28:112–116. doi: 10.1136/bjsm.28.2.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ozeki S., Kitaoka H., Uchiyama E., Luo Z.P., Kaufman K., An K.N. Ankle ligament tensile forces at the end points of passive circumferential rotating motion of the ankle and subtalar joint complex. Foot Ankle Int. 2006;27:965–969. doi: 10.1177/107110070602701117. [DOI] [PubMed] [Google Scholar]
- 29.Kim B.H., Kim J.I., Lee O., Lee K.W., Lee M.C., Han H.S. Preservation of remnant with poor synovial coverage has no beneficial effect over remnant sacrifice in anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2018;26:2345–2352. doi: 10.1007/s00167-017-4683-7. [DOI] [PubMed] [Google Scholar]
- 30.Naraoka T., Kimura Y., Tsuda E., Yamamoto Y., Ishibashi Y. Is remnant preservation truly beneficial to anterior cruciate ligament reconstruction healing? Clinical and magnetic resonance imaging evaluations of remnant-preserved reconstruction. Am J Sports Med. 2017;45:1049–1058. doi: 10.1177/0363546516682241. [DOI] [PubMed] [Google Scholar]
- 31.Naraoka T., Kimura Y., Tsuda E., Yamamoto Y., Ishibashi Y. Does remnant preservation influence tibial tunnel enlargement or graft-to-bone integration after double-bundle anterior cruciate ligament reconstruction using hamstring autografts and suspensory fixation? A computed tomography and magnetic resonance imaging evaluation. Orthop J Sports Med. 2018;6 doi: 10.1177/2325967118790238. 2325967118790238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gui J., Jiang Y., Li Y. All arthroscopic remnant-preserving technique to reconstruct the lateral ankle ligament complex. Arthrosc Tech. 2017;6:e549–e557. doi: 10.1016/j.eats.2016.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dong P., Gu S., Jiang Y. All arthroscopic remnant-preserving reconstruction of the lateral ligaments of the ankle: A biomechanical study and clinical application. Biochem Biophys Res Commun. 2018;505:985–990. doi: 10.1016/j.bbrc.2018.10.041. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Surgical technique for anatomic arthroscopic anterior talofibular ligament (ATFL) repair and reconstruction using a free tendon in the right ankle. This surgical procedure is performed with the patient under general anesthesia in the supine position. A tourniquet is placed on the proximal thigh. The foot is suspended from the distal edge of the bed. The contralateral leg is slightly lowered to provide a wide working space. A 2- or 3-strand graft is prepared using the gracilis tendon or a tendon allograft. It contains an approximately 20-mm-long bundle for the ATFL. The length is determined on preoperative magnetic resonance imaging. The 2 ends form a 15-mm-long loop to facilitate thread attachment for graft delivery. The recommended graft diameter is 4.5 to 6.0 mm. Three portals are created in a step-by-step manner: a conventional anteromedial (AM) portal, an accessory anterolateral (AAL) portal, and a subtalar (ST) portal. The ankle is positioned neutrally. The AM portal is created medial to the anterior tibial tendon and slightly proximal to the joint line. A 30° 2.7- or 4.0-mm-diameter arthroscope is introduced through the AM portal. The ATFL remnant is viewed with the ankle in a dorsiflexed position. After a needle is inserted into the portal site to confirm accessibility to the talar attachment site of the ATFL superior limb, the AAL portal is created. The portal is usually created approximately 20 mm anterior to the anteroinferior tubercle of the distal fibula, which is called the “fibular obscure tubercle” (FOT). The ATFL remnant is carefully dissected to only the minimum necessary area for tunnel creation at the talar and fibular footprint of the superior limb of the ATFL using a radiofrequency (RF) probe. A microfracture awl is used to mark the center of the dissected footprint, and a 2.4-mm guidewire is inserted through the AAL portal to drill the talus toward the distal end of the medial malleolus. The guidewire is then over-drilled to create a 20-mm-deep talar tunnel. The ST portal is created just below the distal end of the fibula after confirmation of accessibility of the fibular footprint by a needle. A guidewire is inserted through the ST portal to drill the fibula. Intraoperative fluoroscopy is used to confirm the guidewire insertion position and direction. The insertion point should be proximal to the articular tip and the FOT. The angle between the guidewire direction and the long axis of the fibula on the lateral view is 10° to 30° and almost on the angle bisector of the fibular end on the anteroposterior view. The guidewire is then over-drilled to create a 20-mm-deep fibular tunnel. The surgeon penetrates from the fibular tunnel bottom to the opposite cortex with a 2.9-mm drill wire through the ST portal. A 2.9-mm JuggerKnot Soft Anchor, which has 2 sets of threads, is placed at the fibular cortex behind the fibular tunnel. The first set of threads is used to grab the ATFL remnant via a lasso-loop technique. An 18-gauge hollow needle with a 2-0 nylon thread is penetrated to the ATFL inferior limb remnant through the AAL portal or ST portal, depending on the accessibility to the remnant. A suture passer (e.g. Micro SutureLasso or SpeedSnare) is also useful to grasp the ATFL remnant. The nylon loop is retrieved through the same portal using a grasping instrument, and the needle is withdrawn. One end of the first set of suture anchor threads is passed through the nylon loop, which is then used to pull just the mid portion of the suture anchor through the ATFL remnant so that a suture loop is created in the ATFL remnant. The free end of the first thread set is passed through this loop and pulled tight, creating a self-cinching lasso loop. The other end of the first thread set is then used to draw the lasso loop, tightening the ATFL remnant. The second set of suture anchor threads, which is not used to repair the ATFL remnant, is used to introduce the ATFL graft. One strand is sutured and connected to the fibular end of the graft. The other strand is pulled for the graft introduction later. A 1.6-mm passing pin (Meira) is inserted into the talar tunnel through the AAL portal. This pin penetrates the bone and skin on the opposite side. A looped thread is passed through the eye of the passing pin, which is pulled out to the opposite side. The looped thread penetrating the talar tunnel needs to be led from the AAL portal to the ST portal. The tendon graft is introduced from the ST portal into the talar tunnel by pulling the looped threads and into the fibular tunnel by pulling the other strand of the second suture anchor thread. The graft is fixed with a 15-mm-long bioabsorbable interference screw in the talar tunnel first. Subsequently, the ATFL remnant and the ATFL graft are tightened simultaneously by pulling the 2 sets of suture anchor threads at the fibular tunnel. They are fixed together with another screw, with the ankle in an approximately 30° to 45° plantar flexion position. Both sets of suture anchor threads are tied in situ using a conventional knot. The video was created using the records of patients 1, 2, and 3 because of image quality and for the purpose of showing several optional techniques.