Abstract
Background
An unintended consequence of medical technologies is loss of personal interactions and humanism between patients and their healthcare providers, leading to depersonalisation of medicine. As humanism is not integrated as part of formal postgraduate anaesthesiology education curricula, our goal was to design, introduce, and evaluate a comprehensive humanism curriculum into anaesthesiology training.
Methods
Subject-matter experts developed and delivered the humanism curriculum, which included interactive workshops, simulation sessions, formal feedback, and patient immersion experience. The effectiveness of the programme was evaluated using pre- and post-curriculum assessments in first-year postgraduate trainee doctors (residents).
Results
The anaesthesiology residents reported high satisfaction scores. Pre-/post-Jefferson Scale of Patient Perceptions of Physician Empathy showed an increase in empathy ratings with a median improvement of 12 points (range; P=0.013). After training, patients rated the residents as more empathetic (31 [4] vs 22 [5]; P<0.001; 95% confidence interval [CI]: 7–12) and professional (47 [3] vs 35 [8]; P<0.001; 95% CI: 9–16). Patient overall satisfaction with their anaesthesia provider improved after training (51 [6] vs 37 [10]; P<0.001; 95% CI: 10–18). Patients rated their anxiety lower in the post-training period compared with pretraining (1.8 [2.3] vs 3.6 [1.6]; P=0.001; 95% CI: 0.8–2.9). Patient-reported pain scores decreased after training (2.3 [2.5] vs 3.8 [2.1]; P=0.010; 95% CI: 0.4–2.8).
Conclusions
Implementation of a humanism curriculum during postgraduate anaesthesiology training was well accepted, and can result in increased physician empathy and professionalism. This may improve patient pain, anxiety, and overall satisfaction with perioperative care.
Keywords: anaesthesia curriculum, burnout, humanism, patient outcomes, postgraduate medical education, simulation
Editor's key points.
-
•
Increased reliance on technology in medicine has the unintended consequence of loss of personal interactions and humanism between patients and doctors.
-
•
A humanism curriculum was developed and evaluated using pre- and post-curriculum assessments in first-year postgraduate anaesthesia trainee doctors.
-
•
Implementation of a humanism curriculum was well accepted, and increased physician empathy and professionalism as well as patient satisfaction.
-
•
Although resource intensive, such a curriculum can improve patient pain, anxiety, and overall satisfaction with perioperative care whilst potentially reducing physician burnout.
The Arnold P. Gold Foundation, which has dedicated itself to addressing humanism in healthcare, describes humanism as a ‘respectful and compassionate relationship between physicians, members of the health care team and their patients’ focused on integrity, excellence, collaboration, compassion, respect, and empathy.1 However, whilst humanism is a cornerstone of patient-centred care, there are surprisingly few residency-training programmes that integrate humanism and compassion into a formal curriculum.2 Those that do tend to be non-surgical programmes, such as family medicine, internal medicine, and paediatrics, and physicians in these specialties score significantly higher on empathy assessments than their counterparts in anaesthesiology and other surgical specialties.3, 4
The need for a formal humanism curriculum may be even more critical with the increased production pressures in healthcare5, 6 and the rise of the electronic health record (EHR). If the EHR has provided an opportunity for healthcare to transform into a data-driven science,7 allowing for data to be centralised and available for individual care and for advances in digital health,8 then one of its unintended consequences is a loss of personal interactions between patients and their healthcare providers, and between healthcare teams, often credited with contributing to physician burnout and to the de-humanisation of medicine.9, 10 De-humanisation, along with feelings of emotional exhaustion and low personal accomplishment, exacerbates physician burnout.11
Anaesthesiologists and anaesthesiology trainees are not immune from the aforementioned adverse events, with as many as 50% of anaesthesiologists across training reporting burnout, with depersonalisation of healthcare as a common cited contributor.5, 12, 13, 14 With so much of the anaesthesiology workforce reporting burnout, creating a formal humanism curriculum to counter the effects of a hidden curriculum,15, 16 where educators teach by example, may model unprofessional behaviour, unwittingly transmitting a culture devoid of empathetic medical care.
With the support of a Challenge Grant award from the Picker Institute and the Arnold P. Gold Foundation, we developed and implemented the ‘humanism in perioperative medicine curriculum’ with the aim of training first-year anaesthesiology residents in compassion, communication, and empathetic care to supplement their technical anaesthesia training. We describe the development and implementation of a humanism curriculum for anaesthesiology residents, and evaluate whether it improved physician perceived empathy translating into improved patient pain, anxiety, and overall satisfaction using the Kirkpatrick model of training and assessment.17, 18
Methods
The humanism in the perioperative medicine curriculum was developed and implemented at the Department of Anesthesiology and Perioperative Care, University of California, Irvine, CA, USA. After an institutional review board approval from the University of California, Irvine (HS#2010-7868), the impact of the implementation of this curriculum was studied using a before/after methodology focusing on 10 residents enrolled in clinical anaesthesia Year 1 (CA-1), and 60 patients (30 before implementation and 30 after implementation) undergoing elective surgery. Both residents and patients gave written informed consent to participate in the programme evaluation.
Curriculum development
We developed the curriculum centred around the creation of perioperative always events.19 Always events were initially conceived by the Picker Institute20 and are now championed by the Institute for Healthcare Improvement; they were developed as a term in opposition to never events, which were adopted by the Centers for Medicare & Medicaid Services as events that should never happen during healthcare delivery. Always events are ‘aspects of the patient experience that are so important to patients and families that healthcare providers should always get them right’.
The humanism in the perioperative medicine curriculum was developed to address patients' values regarding what is considered compassionate and empathetic care, with close attention to the patients' fears, pain, and anxiety during the perioperative experience. Specifically, a diverse group of course instructors, with experience in their respective fields, contributed to the curriculum by addressing patient-centred always events.19 The 15 course instructors comprised a group of anaesthesiologists (general, paediatric, chronic, and regional pain), a physiatrist (physician specialist in physical medicine and rehabilitation), palliative medicine experts, a clinical psychologist with expertise in perioperative medicine and behaviour change, a certified medical acupuncture specialist, certified simulation instructors, a guided mindfulness meditation and imagery facilitator, and a marketing consultant/author. The course director (DP) created working groups and met each instructor to discuss the aims of the curriculum, and worked with them to develop the comprehensive curriculum focusing on always events, which formed the basis of the humanism training.
The curriculum centred around five always events developed by a patient representative who is also a communications author (CL), members of the educational steering committee, and the course director (DP), with the five always events adopted by a general consensus by the committee, to address the Picker Institute's patient-centred principles of respect for patients' values, preferences, and expressed needs: communication, education, physical comfort, emotional support and alleviation of fear and anxiety, and involvement of family and friends.21 Additionally, the programme addresses all of the Arnold P. Gold Foundation criteria (integrity, excellence, compassion and collaboration, altruism, respect and resilience, empathy, and service) to advance humanistic patient care,1 and is directly applicable to the US Accreditation Council for Graduate Medical Education (ACGME) core competencies of patient care, interpersonal and communication skills, and professionalism.22 These five always events are described in detail as follows:
Always event 1: determine the patient's view of the perioperative experience, and his/her preferences, needs, and wishes, and use this to develop a personalised plan for care of that patient
Residents undergo intense technical training during their residency to prepare them to manage routine and complex clinical cases. They receive an intensive didactic programme to develop analytical and critical-thinking skills. The number and breadth of cases to which they are exposed are closely monitored. In-training examinations help measure their medical knowledge progress throughout their training. Their patients are screened for co-morbidities, and the procedure and underlying disease are targeted to improve patient outcomes. However, the humanism and empathic portion of anaesthesia are rarely formally addressed in anaesthesiology. Residents are not often trained or encouraged to incorporate the patient's wishes or weigh the patient's point of view when developing a treatment plan. In fact, many residents have never undergone surgery, and it may be difficult for them to empathise with the loss of control experienced whilst a patient is undergoing surgery. To address this, residents participated in two distinct trainings:
-
(i)
The patient as a customer: working towards a shared decision-making model23 (Table 1)
-
(ii)
Immersion session
Table 1.
Humanism in the perioperative medicine curriculum.
| Curriculum session | Format | Description |
|---|---|---|
| Empathy without borders: how to be empathetic without falling apart yourself | 1 h workshop | Residents identify challenging situations that require empathy. Residents discuss maintaining empathy by identifying stressful situations that affect them emotionally and physically (signs of stress are also identified). This is followed by a discussion of strategies to maintain empathy in the moment, followed by practice with verbal and non-verbal strategies via role play with feedback. |
| Perioperative anxiety | 1 h workshop | Residents learn about and explore the use of guided imagery as an anxiolytic through a formal interactive presentation. Residents are taught various relaxation techniques, including guided imagery, which allows one to have a measure of control over his/her surgical experience, thereby eliminating some of his/her fears. |
| Perioperative pain | 1 h workshop | Residents are asked to write down the key elements involved in pain history taking at the start of the session. A didactics session on the necessary elements to consider in the evaluation of pain is given, and residents are asked to write down the necessary elements again after the presentation. The didactic presentation covers the consequences of uncontrolled pain, the key elements of obtaining a pain history, validated pain intensity scales (in the general population, the paediatric population, the neonatal population, and the elderly and demented populations), the definition of patient-controlled analgesia, and special questions to ask in postoperative patients. |
| The patient as a customer: working towards a shared decision-making model | 1 h workshop | The residents are asked to introduce themselves and enlighten the group on the most important elements of introducing oneself to another person. The speaker then discusses her perceptions of what patients want from their physicians; a New York Times article on patient-centred care is also reviewed14 (https://www.nytimes.com/2009/06/04/health/04chen.html). |
| Breaking bad news: mistakes in anaesthesiology | 1 h workshop plus simulation | A didactic session on the key elements of breaking bad news is given, and residents watch two videos: a video of a cardiac arrest that ends in death and a video of the discussion that follows with a family member (standardised patient). Residents debrief the scenario and critique the physicians' behaviour when giving the family bad news. |
| Non-verbal communication skills | 1 h workshop | This session highlights the definition of non-verbal communication, and recalls the elements of sending and receiving messages (gestures, body language, posture, facial expression, eye contact, metaphors, meaning, symbolism, and imagery). Residents discern paralanguage non-verbal cues of voice (volume, tempo, qualifiers, speaking style, rhythm, intention, articulation, and pitch) and identify the characteristics of non-verbal communication. |
| Intraoperative awareness | 1 h workshop plus simulation | This session includes a simulated scenario with a standardised patient who refuses general anaesthesia for a procedure because he reports ‘waking up during anaesthesia’ previously; the faculty member and residents debrief the scenario, and critique the physicians' behaviour when discussing intraoperative awareness with the patient. This simulation experience is followed by a didactic session on the key elements of intraoperative awareness (including data about the incidence of intraoperative awareness and instruction of a standardised approach to discussing intraoperative awareness). |
| The angry patient | 1 h workshop | Anger is discussed as a secondary emotion with a purpose; the emotions behind anger are recognised (fear, sadness, frustration, a feeling that ‘it is not fair’, resentment towards others not suffering, and blame on others for lack of support) and residents discuss how anger makes them feel. The residents are instructed on emotional aikido as a method of self-instruction or control of oneself. Principles are taught (principle of oneness, principle of circular motion, range of effectiveness, principle of Ki, and principles to unify the mind and the body) and explained. |
| The paediatric patient | 1 h workshop | Residents write down the key elements involved in history taking at the start of the session. A didactics session on the necessary elements to consider in the evaluation of a paediatric patient is given; a variety of videos of patient/physician interactions are played and critiqued. |
| Professionalism | 1 h workshop | Residents define professionalism and what actions would exhibit professionalism as an anaesthesiologist; role play involves two scenarios followed by debriefing. The ASA standards of professionalism are discussed. |
| The art of observation | 1 h workshop | Observation through art metaphorically allows one to study humanism and compassion in medicine. An artist and a painting are present, and residents discuss the mood, values, and points of interest regarding the canvas. The artist teaches the group to analyse the canvas in terms of composition, temperature, objects vs masses, areas of interest vs areas of restraint/passivity, artist personality, linearity vs painterly nature, essence of the subject, and balance between calm and energy. Utilisation of this approach in patient observation and assessment is discussed. |
| How to obtain informed consent | Proctored plus formal feedback session | Each resident participated in a proctored informed consent for general anesthsia. Every resident was proctored by the same faculty member, and was given formal feedback and the end of the case. |
| Immersion sessions | 4–6 h | Each resident is scheduled for an individual half-day immersion session where he/she is treated as a surgical patient. Residents are treated as close to real patients as possible (described in text). |
| University of California, Irvine's Preparing for Surgery – Mind, Body and Spirit Program | 2 h workshop | Each resident participated in a 2 h workshop as both a ‘patient’ and a resident to help guide patients through guided imagery, meditation, and deep-breathing techniques to improve healing (described in text and handbook available at http://www.anesthesiology.uci.edu/downloads/mind-body-surgery-handbook.pdf). |
Previous reports of role playing and immersion sessions indicate they can be an effective adjunct tool for cultivating empathy,24, 25 but require active supervision and reflection. Emphasis must be placed during the development and before implementation to ensure participants are both physically, emotionally, and psychologically safe during and after the immersive learning experience.24 To that end, we implemented a fully immersive session, where each resident was scheduled for surgery and treated as close to a real patient as possible. Like all elective surgery patients, after being scheduled for surgery, each resident received a preoperative call and evaluation, and was given instructions for the day of surgery, including instructions of nil per os after midnight. The resident was asked to arrive at the preoperative check-in desk where he/she received a patient identification band, asked to change into a patient gown, wheeled into the operating room (OR), placed on the OR bed with standard ASA monitors, received preoxygenation, and a surgical time out was performed. After the time out, the resident was placed back onto the gurney and taken from the OR to the PACU until ‘discharged’.
Always event 2: use empathetic communication in all patient interactions
Empathetic communication was the overlying focus of the curriculum, and several training sessions (Table 1) highlight communication challenges in the perioperative setting, including.
-
(i)
how to obtain informed consent
-
(ii)
breaking bad news: mistakes in anaesthesiology
-
(iii)
empathy with borders: how to be empathetic without falling apart yourself
-
(iv)
non-verbal communication skills
-
(v)
how to deal with intraoperative awareness
-
(vi)
communication when patients are angry
These workshops incorporated opportunities for residents to practice new communication skills that will directly translate into their work in the perioperative environment.
Always event 3: identify and mitigate each patient's level of anxiety using empirically based techniques that specifically target the individual
Major life stressors, such as surgery and associated anxiety, can adversely affect the ability to heal. The training session incorporated techniques to reduce anxiety, including guided imagery and deep breathing methods. The residents then participated in the University of California, Irvine's Preparing for Surgery – Mind, Body and Spirit Program26 (Table 1) as both ‘patients’ and instructors, learning the patients' perspective on perioperative anxiety. This 2 h patient workshop focused on alleviating perioperative anxiety by providing knowledge about the imminent surgery and established relaxation techniques27, 28 (i.e. guided imagery, deep breathing, relaxing the mind by managing anxious thoughts, and empowering attitudes [Table 1]), giving patients a measure of control over their surgical experience.
Always event 4: pay close attention to pain and anxiety, before and after surgery, and develop a specific plan to address physical discomfort keeping emotional factors in mind
Anxiety before surgery can amplify pain after surgery. Therefore, the curriculum included targeted training on the assessment of perioperative pain and anxiety. A didactics session on the elements and need for pain assessment was taught by pain medicine specialists. This was followed by a workshop with actual patients where the residents practiced assessment of pain. Additionally, each resident participated in the University of California, Irvine's Preparing for Surgery – Mind, Body and Spirit Program with patients to learn the impact of pain on the fear of surgery and on the perioperative experience.
Always event 5: communicate empathically and clearly with family and friends
The role of family and friends is extremely important in the perioperative setting. Anaesthesiologists rarely receive formal training on addressing family and friends, although family and friends are often in the perioperative environment with the patient. Indeed, in the recovery room, it may be that important information must be shared with family and friends rather than with the patient directly. With this in mind, the humanism in the perioperative medicine curriculum targeted this important area with sessions including the (Table 1):
-
(i)
paediatric patient
-
(ii)
patient and the family
Curriculum implementation
The curriculum was integrated into the weekly resident education days. Working together with the Chair of Anaesthesiology (ZNK), Vice Chair of Education (CTA), Program Director (SS), residency coordinator, and clinical schedulers, the curricular programme was delivered over a 6 month training period. During resident education days, the residents were relieved of all clinical and pager duties with required attendance regardless of rotation. Physician instructors were relieved of clinical duties during scheduled sessions. Non-clinical instructors, standardised patients, simulation centre, and instructors were also scheduled during this time period. As the programme was adopted by the education committee as standard training, all CA-1 residents were required to attend and participate in the humanism curriculum. Only those residents that consented to participate were included in the study. CA-1 residents were selected for the curriculum implementation, as they were new to anaesthesiology training and had the least exposure to the hidden curriculum.
The curriculum consisted of a proctored informed consent session with formative feedback, plus 11 sessions (1 h each) and one half-day immersion session and 2 h workshop for each resident (Table 1). The multimodal sessions centred around always events; addressed the ACGME core competencies of patient care, interpersonal and communication skills, and professionalism; and included several teaching/learning modalities: a brief didactic component, group discussion, and use of an interactive teaching method, such as role play, patient videos, or formal simulation (standardised patient/manikin simulator). During the course, instructors guided discussions on methods to enhance the physician–patient relationship in the perioperative setting. During the immersion session, the residents became the patients and experienced each aspect of being scheduled for elective surgery.
Baseline evaluation
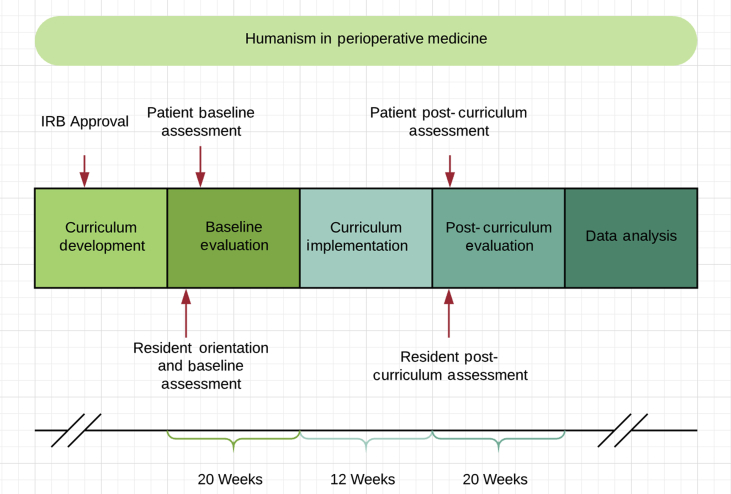
The curriculum was evaluated using a pre-/post-curriculum implementation design, where we assessed residents who participated in the curriculum and patients being treated by the resident cohort (Fig. 1). Before curriculum implementation, patients being treated by the resident cohort scheduled for outpatient elective surgery were identified and consented before surgery. Patients were informed of which physician was being evaluated, but the residents did not know which patients were included in the study. After their procedure, the patients were asked to complete a Jefferson Scale of Patient Perceptions of Physician Empathy form,29 perceived resident professionalism questionnaire, patient satisfaction questionnaire, visual analogue scale for anxiety (VAS-A),30 and pain numeric rating scale (PNRS).31 During an orientation and introduction session, residents completed a pre-curriculum self-assessment of empathy: the Jefferson Scale of Physician Empathy, Health Professions version (JSE-HP).32
Fig 1.
Humanism in perioperative medicine. IRB, institutional review board.
Post-curriculum evaluation
Three months after the immersion sessions and curriculum, all residents were asked to complete a reflection diary, evaluate the curriculum, and once again asked to self-evaluate their empathy skills using the JSE-HP form. The patients were again asked to complete a Jefferson Scale of Patient Perceptions of Physician Empathy form, perceived resident professionalism questionnaire, patient satisfaction questionnaire, VAS-A, and PNRS.
Data acquisition
The primary aim of the programme was to develop and implement a comprehensive humanism curriculum for anaesthesiology residents to improve physician perceived empathy, thereby improving postoperative pain and anxiety. We assessed the effectiveness of the educational programme using the Kirkpatrick model for evaluating training courses. The Kirkpatrick model evaluates training and educational programmes on four levels:17
-
(i)
Kirkpatrick model, Level 1 reaction (participant's level of satisfaction with the training programme): Level 1 of the Kirkpatrick model looks at the degree to which participants find the training favourable, engaging, and relevant to their jobs. We measured resident satisfaction using a 5-point Likert-type-scale questionnaire (Table 2). The residents were also asked to complete a reflection diary that was used for formative evaluation and for a feedback session at the end of the course with the course director.
-
(ii)
Kirkpatrick model, Level 2 learning (impact of the training on knowledge acquisition or attitude change): Level 2 looks at the degree to which participants acquire the intended knowledge, skills, attitude, confidence, and commitment based on their participation in the training. Kirkpatrick Level 2 was measured using pre- and post-curricular resident assessments using the validated JSE-HP.32 The JSE-HP is a 20-item instrument developed to measure empathy in physicians and practicing health professionals. The 20 items are answered on a 7-point Likert-type scale (1=strongly disagree; 7=strongly agree) with a possible raw score of 20–140. The instrument was developed for assessment of professional development of health professionals in training and in practice, and for evaluation of educational outcomes. Higher scores correlate to higher empathy scores.33
-
(iii)
Kirkpatrick model, Level 3 behaviour (transfer of knowledge or attitude by looking at the application of new information): Level 3 of the Kirkpatrick model looks at the degree to which participants apply what they learned during training when they are back on the job. Traditionally, Levels 3 and 4 of the Kirkpatrick model are harder to achieve, given the complexity of measuring transferability of skills.18 We assessed behaviour (Kirkpatrick Level 3), specifically, how the residents applied what they learned, using the Jefferson Scale of Patient Perceptions of Physician Empathy,29 a resident professionalism questionnaire, and an overall patient satisfaction questionnaire (pre- and post-curriculum). The Jefferson Scale of Patient Perceptions of Physician Empathy questionnaire consists of five items, answered on a 7-point Likert-type scale (1=strongly disagree; 7=strongly agree) with a possible raw score of 5–35. The resident professionalism questionnaire consists of seven items, answered on a 7-point Likert-type scale (1=strongly disagree; 7=strongly agree) with a possible raw score of 7–49. The overall patient satisfaction questionnaire consists of eight items, answered on a 7-point Likert-type scale (1=strongly disagree; 7=strongly agree) with a possible raw score of 8–56.
-
(iv)
Kirkpatrick model, Level 4 results (outcomes that occurred because of the training programme): Kirkpatrick Level 4 is the hardest level to achieve,18 and looks at the degree to which targeted outcomes occur as a result of the training. To assess this, we looked at clinical outcomes of the comprehensive humanism curriculum by comparing pre- and post-curricular VAS-A and PNRS in patients.
Table 2.
Resident evaluation of humanism curriculum. CA-1, clinical anaesthesia Year 1 resident. Data are presented as n (%).
| Strongly disagree | Disagree | Neutral | Agree | Strongly agree | |
|---|---|---|---|---|---|
| The topics covered as part of the humanism curriculum were relevant to my clinical practice. | 0 (0) | 0 (0) | 0 (0) | 4 (40) | 6 (60) |
| The humanism curriculum improved my understanding of patient-centred care. | 0 (0) | 0 (0) | 0 (0) | 5 (50) | 5 (50) |
| The humanism curriculum gave me a better understanding of empathy as a physician. | 0 (0) | 0 (0) | 0 (0) | 7 (70) | 3 (30) |
| The topics discussed allowed me to explore patient care in a new way. | 0 (0) | 0 (0) | 0 (0) | 2 (20) | 8 (80) |
| I recommend this course to be included in next year's CA-1 curriculum. | 0 (0) | 0 (0) | 0 (0) | 6 (60) | 4 (40) |
Statistical analysis
The sample size of the resident cohort was pragmatic in that 10 of the 11 residents in the CA-1 class consented to have their data used as part of this study. We recruited 30 patients before and 30 patients after the humanism curriculum intervention on our residents. A sample size of 30 patients per group allows us to adequately detect (>80% power) standardised effect sizes as small as 0.75 between groups (α=0.05; two-sample t-test) for each item (e.g. satisfaction). Previous literature on this topic2 shows similar/larger magnitudes of effect sizes, so we felt our sample size was justified.
Descriptive statistics for the Jefferson Scale of Patient Perceptions of Physician Empathy were performed by the Center for Research in Medical Education & Health Care at Jefferson Medical College. The completed pre- and post-training forms were returned to the centre, which analysed the data; summary results were subsequently returned to the researchers.
All other data were summarised and analysed locally. Testing for normality was performed using the Shapiro–Wilk test. Data are reported as medians and quartiles if found to be non-normally distributed. For normally distributed data, results are reported as mean (standard deviation). Groups were compared with Mann–Whitney U-test for non-parametric data and with Student's t-test for parametric data. When appropriate, paired sample testing was used (for before–after comparisons of the same residents) using Wilcoxon signed-rank test or paired sample t-test, respectively. The analysis was performed using IBM SPSS Statistics for Windows, version 19.0, released 2010 (IBM Corp., Armonk, NY, USA).
Results
Eleven CA-1 residents completed the curriculum and 10 consented to participate in the study. For each resident (n=10), three patients per resident were recruited and consented before curriculum implementation, and another three after curriculum implementation (n=60; 30 patients before curriculum implementation and 30 patients post-curriculum implementation). Information about resident and patient participants is in Table 3.
Table 3.
Resident and patient characteristics.
|
Residents' data |
n |
| Gender | |
| Male | 7 |
| Female | 3 |
| Age (yr) | |
| 21–30 | 9 |
| 31–40 |
1 |
|
Patients' data |
% |
| Gender | |
| Male | 57.1 |
| Female | 42.9 |
| Age (yr) | |
| 18–39 | 12.5 |
| 40–59 | 32.1 |
| 60–79 | 51.8 |
| 80–99 | 3.6 |
| Type of surgery | |
| General | 17.9 |
| Burn/plastics | 5.4 |
| Vascular | 3.6 |
| Gynaecology/gynaecologic oncology | 16.1 |
| Neurology | 5.4 |
| Orthopaedics | 17.9 |
| Otolaryngology | 12.5 |
| Pulmonary | 3.6 |
| Urology/oncology | 17.9 |
| ASA physical status | |
| 1 | 7.1 |
| 2 | 58.9 |
| 3 | 33.9 |
Kirkpatrick model, Level 1 reaction: level of satisfaction with the training programme
The resident satisfaction data are summarised in Table 2. The residents rated the training programme highly, with 100% agreeing or strongly agreeing (60% and 40%, respectively) the course should be continued in subsequent years. The residents agreed or strongly agreed that the topics were relevant to their practice, allowed them to explore patient care in new ways, and gave them a better understanding of empathy as physician and better understanding of patient-centred care.
During the formative evaluation and feedback sessions, the residents were able to discuss one on one with the course director the highlights of the course, or which sessions could be improved. The immersive sessions were the most controversial in that, at the same time, the residents liked the experience, but felt that they could not disconnect with other tasks they needed to do for the day. The residents noted that, whilst waiting to be ‘discharged’, they wanted to leave so that they could go on with their workday, which made the experience less pleasurable. The residents commented on feeling dis-equilibrated whilst being wheeled on the gurney to the OR; the lights and sounds at times make them feel nauseated. Many commented on how cold and uncomfortable they felt. On a couple of occasions, the residents reported that, during preoxygenation in the OR, the anaesthesia-machine pressure valve was closed, which made it difficult for them to breathe, leaving a memorable experience that they often thought about whilst preoxygenating patients from that point forward.
Kirkpatrick model, Level 2 learning: impact of the training on knowledge acquisition or attitude change
The JSE-HP was administered pre- and post-curriculum. The completed analysis returned by the Center for Research in Medical Education & Health Care is summarised in Table 4. The residents showed increased empathy ratings with a median improvement of 12 points (out of a 140 possible; P=0.013). Statistical testing by Mann–Whitney U-test and confidence intervals were not provided.
Table 4.
Resident self-assessment of empathy pre- and post-curriculum (Jefferson Scale of Patient Perceptions of Physician Empathy). Descriptive statistics for the Jefferson Scale of Patient Perceptions of Physician Empathy performed by the Center for Research in Medical Education & Health Care of the Jefferson Medical College. SD, standard deviation.
| Pre-intervention | Post-intervention | P-value | |
|---|---|---|---|
| No. of observations | 10 | 10 | |
| Empathy scores | |||
| Possible range | 20–140 | 20–140 | |
| Mean (sd) | 107 (6) | 118 (12) | 0.013 |
| Median (quartiles) | 107 (104; 111) | 119 (106; 126) | |
| Sample range | 95–117 | 103–135 | |
Kirkpatrick model, Level 3 behaviour: transfer of knowledge or attitude by looking at the application of new information
Patient assessment of physician empathy was used to evaluate behavioural changes after the intervention. Compared with pretraining, the residents were rated as more empathetic (31 [4] vs 22 [5]; P<0.001; 95% confidence interval [CI]: 7–12) and more professional (47 [3] vs 35 [8]; P<0.001; 95% CI: 9–16). Moreover, patient overall satisfaction with their anaesthesia provider improved after training (51 [6] vs 37 [10]; P<0.001; 95% CI: 10–18).
Kirkpatrick model, Level 4 results: outcomes that occurred because of the training programme
We used VAS-A and PNRS as measures of clinical outcomes. Patients rated their anxiety lower in the post-training period compared with pretraining (1.8 [2.3] vs 3.6 [1.6]; P=0.001; 95% CI: 0.8–2.9). Likewise, patient-reported pain scores decreased after training compared with pretraining (2.3 [2.5] vs 3.8 [2.1]; P=0.010; 95% CI: 0.4–2.8). Patient-reported perceptions and outcome data are summarised in Table 5.
Table 5.
Patient-reported perceptions and outcomes data. Scores are presented as mean (standard deviation). Patient-reported measures of pain, anxiety, and satisfaction, and patient-perceived levels of empathy and professionalism exhibited by the anaesthesia resident during the perioperative period.
| Parameter | Pre-intervention (n=30) | Post-intervention (n=30) | P-value | 95% Confidence interval |
|---|---|---|---|---|
| Physician empathy | 22 (5) | 31 (4) | <0.001 | 7–12 |
| Physician professionalism | 35 (8) | 47 (3) | <0.001 | 9–16 |
| Overall satisfaction | 37 (10) | 51 (6) | <0.001 | 10–18 |
| Anxiety | 3.6 (1.6) | 1.8 (2.3) | 0.001 | 0.8–2.9 |
| Pain | 3.8 (2.1) | 2.3 (2.5) | 0.010 | 0.4–2.8 |
Discussion
The goal of this comprehensive humanism curriculum was to develop a formal training for anaesthesiology residents to provide empathetic patient-centred care. This is crucial, as surgery can be a uniquely stressful life event and anaesthesiologists play a key role in determining patients' perioperative experience. There is a growing body of literature that shows that empathetic care improves patient outcomes by reducing anxiety,34, 35 improving communication,36 and thereby improving patient care.36, 37, 38 Our work further supports this notion by showing improvement in self-reported humanistic skills, patient-perceived humanistic skills, and patient-reported pain and anxiety scores after the intervention (Kirkpatrick Levels 2–4). Few anaesthesiologists are formally trained in humanism, empathetic communication, or personalising the perioperative environment. The humanism in the perioperative medicine curriculum specifically targets instruction of humanism and empathetic communication in this unique setting, contextualising the perioperative patient care.
Empathy and professionalism are key components to a successful patient-centred care. Our results indicate that a successful humanism curriculum must be aimed at changing both residents' attitudes and behaviours (Kirkpatrick Levels 1–4). The improvements noted in the resident self-assessment of empathy scores (Kirkpatrick Level 2) reflect success in attitude changes secondary to our curriculum, whilst improvements in patient perception of provider empathy and provider professionalism reflect successful implementation of humanistic provider behaviours (Kirkpatrick Level 3). Improvements in patient satisfaction scores, and patient anxiety and pain scores, also reflect the promotion of humanistic values and behaviours by the residents (Kirkpatrick Level 4).
Although the overarching goal was to improve the patient experience by creating a formal curriculum to improve empathy and communication specific to perioperative medicine, one of the unintended themes that emerged was how the training personalised the patient-care experience for the trainee, improving their experience and how they relate to patients. This is important as depersonalisation of healthcare has recently emerged as a strong contributing factor that exacerbates physician burnout.2, 8 Burnout is increasingly becoming a problem not just with trainees, but with practicing healthcare providers as well. In anaesthesiology, burnout for anaesthesiology leadership is particularly high with programme directors reporting up to 52% risk of burnout.39 A survey of anaesthesiology Chairs showed that ∼50% met the criteria for high-to-moderate burnout.13
Traditionally, medicine has been taught in a preceptorship model: the science of medicine is learned in medical school, and the art of medicine is learned in graduate medical education (GME) through modelling, often termed the hidden curriculum.4, 10, 16 The hidden curriculum need not be demonised to represent only the negative role modelling or a culture of care devoid of empathy and professionalism in healthcare.16 However, in recent years, the EHR is helping to shift the art of medicine into data-driven practice.7, 8 Further, practicing anaesthesiologists are suffering from burnout.5, 12, 13, 14, 39 The question then becomes, ‘How are practising anaesthesiologists modelling empathy, humanism, professionalism, and patient-centred care?’ The need for a formal curriculum that focuses not just on resident technical skills, but also on attitude and empathy, is critical. In the early 1990s, the Arnold P. Gold Foundation introduced the first humanism programmes into medical school education in the form of independent practice of medicine. Humanism as a curriculum ought to extend to postgraduate training programmes as well. Most clinical patient–physician interactions in a training institution occur at the GME level; institution of humanism curricula into training programmes would therefore allow the bulk of opportunity for listening, hearing, and understanding the patient's voice, and for provider demonstration and practice with principles, attitudes, and behaviours learned. Medical boards and the ACGME agree with this GME-approach principle, as many of their required competencies are patient centred.
A comprehensive humanism curriculum has the capacity to have a major impact on the way healthcare is delivered, especially in anaesthesiology. This clearly affects not just perioperative patients, but trainees and practising physicians as well. For years now, the need for professionalism and communication have been stressed by the ACGME as core competencies that should be measured in trainees. However, an overarching structured humanism curriculum may be better suited in providing not just patient-centred care, but also in improving the experience of personalisation in medicine for the anaesthesiologist.
Limitations
The development and implementation of this humanism in the perioperative medicine curriculum were resource intensive. We benefited from a close relationship with main campus experts in guided imagery and communication, and the proximity of an author willing to lend her time to the project. Further departmental support was critical in that the curriculum was fully adopted and resources made available for the success of the programme. The hope is that programmes would be able to take the curriculum framework and resources provided. Although not every programme would have the ability to incorporate such a resource intensive programme, the incremental adoption of segments of the programme could yield beneficial results and begin to change culture within any given programme.
Institution of the humanism curriculum resulted in marked improvements in both residents' perception of their own level of empathy and patients' perception of resident empathy and professionalism. One of the limitations and confounding variables is that, throughout training in general, but specifically during the first year of training, anaesthesiology residents experience tremendous growth and maturity, which can, by itself, translate into an improved patient experience. The fact that post-curriculum assessments were performed towards the end of the first year of residency training may have given residents more confidence in their clinical skills as well, which may have come across in their patient interactions.
Further work and research should focus on how vertical integration of formal humanism training can help change the culture of medicine and improve both patient and healthcare provider satisfaction. Humanistic elements introduced as medical students, contextualised during residency and reinforced as fully trained practitioners, are likely to yield the biggest effect to encourage well-rounded empathetic healthcare providers. Formal training is necessary to develop, support, and reinforce humanistic elements of patient care for the benefit of trainee and patients.
Conclusions
Our findings suggest that the introduction of humanism in perioperative medicine curriculum can result in increased physician empathy and professionalism, which translate into improved patient anxiety, pain, and overall patient satisfaction with care in the perioperative setting.
Authors' contributions
Programme development: CC, DP, SS, CTA, ZNK, MAF.
Programme implementation: all authors.
Data collection: CC, DP.
Data analysis: CC, DP.
Data interpretation: CC, DP, SS, CTA, ZNK, MC.
Statistical analysis: MAF, JBR.
Manuscript writing: all authors.
Acknowledgements
The authors thank the Department of Anesthesiology and Perioperative Care, University of California, Irvine Medical Education Simulation Center, and the University of California, Irvine for resources and educational support. The authors would also like to acknowledge Camille Lavington (marketing consultant and author, Newport Beach, CA, USA) for her assistance in curriculum development and for her session on ‘the patient as a customer: working towards a shared decision-making model’, and Debora E. Morrison (Department of Anesthesiology and Perioperative Care, University of California, Irvine) for her proctorship and formal feedback during informed consent training. Additional resources can be made available by contacting the authors.
Handling editor: H.C. Hemmings Jr
Editorial decision: 14 May 2019
Declarations of interest
JBR has funding from Edwards Lifesciences and the National Institutes of Health for other unrelated work. MAF has funding from the National Institutes of Health for other unrelated work. MC has funding from Masimo, Edwards Lifesciences, and the National Institutes of Health for unrelated work. ZNK has funding from Edwards Lifesciences, Studer Group, and the National Institutes of Health for other unrelated work.
Funding
Arnold P. Gold Foundation (2010_1524) Picker Gold Challenge Grant for Residency Training to DP.
References
- 1.Gold A., Gold S. Humanism in medicine from the perspective of the Arnold Gold Foundation: challenges to maintaining the care in health care. J Child Neurol. 2006;21:546–549. doi: 10.1177/08830738060210060401. [DOI] [PubMed] [Google Scholar]
- 2.Dotters-Katz S.K., Chuang A., Weil A., Howell J.O. Developing a pilot curriculum to foster humanism among graduate medical trainees. J Educ Health Promot. 2018;7:2. doi: 10.4103/jehp.jehp_45_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Glass R.M. The patient-physician relationship. JAMA focuses on the center of medicine. JAMA. 1996;275:147–148. [PubMed] [Google Scholar]
- 4.Hojat M., Mangione S., Gonnella J.S., Nasca T., Veloski J.J., Kane G. Empathy in medical education and patient care. Acad Med. 2001;76:669. doi: 10.1097/00001888-200107000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Hyman S.A., Michaels D.R., Berry J.M., Schildcrout J.S., Mercaldo N.D., Weinger M.B. Risk of burnout in perioperative clinicians: a survey study and literature review. Anesthesiology. 2011;114:194–204. doi: 10.1097/ALN.0b013e318201ce9a. [DOI] [PubMed] [Google Scholar]
- 6.Maslach C., Schaufeli W.B., Leiter M.P. Job burnout. Annu Rev Psychol. 2001;52:397–422. doi: 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- 7.Mandl K.D., Bourgeois F.T. The evolution of patient diagnosis: from art to digital data-driven science. JAMA. 2017;318:1859–1860. doi: 10.1001/jama.2017.15028. [DOI] [PubMed] [Google Scholar]
- 8.Verghese A., Shah N.H., Harrington R.A. What this computer needs is a physician: humanism and artificial intelligence. JAMA. 2018;319:19–20. doi: 10.1001/jama.2017.19198. [DOI] [PubMed] [Google Scholar]
- 9.Montgomery L., Loue S., Stange K.C. Linking the heart and the head: humanism and professionalism in medical education and practice. Fam Med. 2017;49:378–383. [PubMed] [Google Scholar]
- 10.Chou C.M., Kellom K., Shea J.A. Attitudes and habits of highly humanistic physicians. Acad Med. 2014;89:1252–1258. doi: 10.1097/ACM.0000000000000405. [DOI] [PubMed] [Google Scholar]
- 11.Patel R.S., Bachu R., Adikey A., Malik M., Shah M. Factors related to physician burnout and its consequences: a review. Behav Sci (Basel) 2018;8:98. doi: 10.3390/bs8110098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sanfilippo F., Noto A., Foresta G. Incidence and factors associated with burnout in anesthesiology: a systematic review. Biomed Res Int. 2017;2017:8648925. doi: 10.1155/2017/8648925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.De Oliveira G.S., Jr., Ahmad S., Stock M.C. High incidence of burnout in academic chairpersons of anesthesiology: should we be taking better care of our leaders? Anesthesiology. 2011;114:181–193. doi: 10.1097/ALN.0b013e318201cf6c. [DOI] [PubMed] [Google Scholar]
- 14.Shanafelt T. Burnout in anesthesiology: a call to action. Anesthesiology. 2011;114:1–2. doi: 10.1097/ALN.0b013e318201cf92. [DOI] [PubMed] [Google Scholar]
- 15.Billings M.E., Lazarus M.E., Wenrich M., Curtis J.R., Engelberg R.A. The effect of the hidden curriculum on resident burnout and cynicism. J Grad Med Educ. 2011;3:503–510. doi: 10.4300/JGME-D-11-00044.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Martimianakis M.A., Michalec B., Lam J., Cartmill C., Taylor J.S., Hafferty F.W. Humanism, the hidden curriculum, and educational reform: a scoping review and thematic analysis. Acad Med. 2015;90:S5–S13. doi: 10.1097/ACM.0000000000000894. [DOI] [PubMed] [Google Scholar]
- 17.Kirkpatrick D.L. Effective supervisory training and development, part 2: in-house approaches and techniques. Personnel. 1985;62:52–56. [PubMed] [Google Scholar]
- 18.Kirkpatrick J.D., Kirkpatrick W.K. ATD Press; Alexandria, VA: 2016. Kirkpatrick’s four levels of training evaluation. [Google Scholar]
- 19.Lembitz A., Clarke T.J. Clarifying “never events” and introducing “always events”. Patient Saf Surg. 2009;3:26. doi: 10.1186/1754-9493-3-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Institute for Healthcare Improvement. Picker Institute always events white paper: creating an optimal patient experience. http://www.ihi.org/Topics/AlwaysEvents/Pages/default.aspx (accessed 5 July 2019).
- 21.Institute for Healthcare Improvement. Always events toolkit. Available from https://www.england.nhs.uk/wp-content/uploads/2016/12/always-events-toolkit-v6.pdf (accessed 5 January 2019).
- 22.Tetzlaff J.E. Assessment of competency in anesthesiology. Anesthesiology. 2007;106:812–825. doi: 10.1097/01.anes.0000264778.02286.4d. [DOI] [PubMed] [Google Scholar]
- 23.Berwick D.M. What ‘patient-centered’ should mean: confessions of an extremist. Health Aff (Millwood) 2009;28:w555–w565. doi: 10.1377/hlthaff.28.4.w555. [DOI] [PubMed] [Google Scholar]
- 24.Wilkes M., Milgrom E., Hoffman J.R. Towards more empathic medical students: a medical student hospitalization experience. Med Educ. 2002;36:528–533. doi: 10.1046/j.1365-2923.2002.01230.x. [DOI] [PubMed] [Google Scholar]
- 25.Nestel D., Tierney T. Role-play for medical students learning about communication: guidelines for maximising benefits. BMC Med Educ. 2007;7:3. doi: 10.1186/1472-6920-7-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.University of California, Irvine Department of Anesthesiology & Perioperative Care. Preparing for surgery and recovery: a “mind–body” handbook for the pre-surgical patient. Available from http://www.anesthesiology.uci.edu/mindbodyprep.shtml (accessed 6 July 2019).
- 27.Felix M., Ferreira M.B.G., Oliveira L.F., Barichello E., Pires P.D.S., Barbosa M.H. Guided imagery relaxation therapy on preoperative anxiety: a randomized clinical trial. Rev Lat Am Enfermagem. 2018;26 doi: 10.1590/1518-8345.2850.3101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Holden-Lund C. Effects of relaxation with guided imagery on surgical stress and wound healing. Res Nurs Health. 1988;11:235–244. doi: 10.1002/nur.4770110405. [DOI] [PubMed] [Google Scholar]
- 29.Kane G.C., Gotto J.L., Mangione S., West S., Hojat M. Jefferson scale of patient's perceptions of physician empathy: preliminary psychometric data. Croat Med J. 2007;48:81–86. [PMC free article] [PubMed] [Google Scholar]
- 30.Hornblow A.R., Kidson M.A. The visual analogue scale for anxiety: a validation study. Aust N Z J Psychiatry. 1976;10:339–341. doi: 10.3109/00048677609159523. [DOI] [PubMed] [Google Scholar]
- 31.Joos E., Peretz A., Beguin S., Famaey J.P. Reliability and reproducibility of visual analogue scale and numeric rating scale for therapeutic evaluation of pain in rheumatic patients. J Rheumatol. 1991;18:1269–1270. [PubMed] [Google Scholar]
- 32.Glaser K.M., Markham F.W., Adler H.M., McManus P.R., Hojat M. Relationships between scores on the Jefferson Scale of physician empathy, patient perceptions of physician empathy, and humanistic approaches to patient care: a validity study. Med Sci Monit. 2007;13:CR291–CR294. [PubMed] [Google Scholar]
- 33.Hojat M., DeSantis J., Shannon S.C. The Jefferson Scale of Empathy: a nationwide study of measurement properties, underlying components, latent variable structure, and national norms in medical students. Adv Health Sci Educ Theory Pract. 2018;23:899–920. doi: 10.1007/s10459-018-9839-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.van Dulmen S., van den Brink-Muinen A. Patients’ preferences and experiences in handling emotions: a study on communication sequences in primary care medical visits. Patient Educ Couns. 2004;55:149–152. doi: 10.1016/s0738-3991(04)00300-3. [DOI] [PubMed] [Google Scholar]
- 35.Choi S.M., Lee J., Park Y.S., Lee C.H., Lee S.M., Yim J.J. Effect of verbal empathy and touch on anxiety relief in patients undergoing flexible bronchoscopy: can empathy reduce patients’ anxiety? Respiration. 2016;92:380–388. doi: 10.1159/000450960. [DOI] [PubMed] [Google Scholar]
- 36.Derksen F., Bensing J., Lagro-Janssen A. Effectiveness of empathy in general practice: a systematic review. Br J Gen Pract. 2013;63:e76–e84. doi: 10.3399/bjgp13X660814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kain Z.N., Sevarino F., Alexander G.M., Pincus S., Mayes L.C. Preoperative anxiety and postoperative pain in women undergoing hysterectomy. A repeated-measures design. J Psychosom Res. 2000;49:417–422. doi: 10.1016/s0022-3999(00)00189-6. [DOI] [PubMed] [Google Scholar]
- 38.Pereira L., Figueiredo-Braga M., Carvalho I.P. Preoperative anxiety in ambulatory surgery: the impact of an empathic patient-centered approach on psychological and clinical outcomes. Patient Educ Couns. 2016;99:733–738. doi: 10.1016/j.pec.2015.11.016. [DOI] [PubMed] [Google Scholar]
- 39.De Oliveira G.S., Jr., Almeida M.D., Ahmad S., Fitzgerald P.C., McCarthy R.J. Anesthesiology residency program director burnout. J Clin Anesth. 2011;23:176–182. doi: 10.1016/j.jclinane.2011.02.001. [DOI] [PubMed] [Google Scholar]