Abstract
A large to massive rotator cuff tear is a common issue that lacks reliable options to return a patient's range of motion and function when conservative treatment has failed. With up to 96% of massive rotator cuff repairs failing within the first 6 months of repair, surgeons have been searching for a reliable treatment option for this difficult subset of patients. Surgical options for massive, retracted rotator cuff tears include re-establishing the counterforce coupling of the rotator cuff with techniques such as a partial repair or superior capsular reconstruction, preventing superior humeral migration as seen with balloon spacer implantation, and eliminating pain generators with techniques such as biceps tenotomy; however, these do not reconstitute dynamic cuff control. More recently, an acellular dermal allograft, as seen in superior capsular reconstruction, has been used to reconstruct the remaining rotator cuff. We describe a technique using a fascia lata autograft to reconstruct the rotator cuff in the setting of a massive cuff tear. This is of particular importance in centers that lack the funding or institutional approval to use acellular dermal allografts that have been popularized to date.
Rotator cuff disease is a highly prevalent pathology that follows an age-wise distribution and is a significant cause of morbidity and decreased quality of life. The natural history of rotator cuff tears involves progression over time, particularly in those that have become symptomatic. The correlation between tear size and symptomatology has been investigated, with an increased tear size resulting in increased symptoms and an increase in symptoms relating to increasing tear size, leading to increased disability in these patients.1 Massive rotator cuff tears have been reported to have a prevalence as high as 40% among all rotator cuff tears2 and increase the risk of irreparable tears. Risk factors for irreparability include tears that are greater than 4 cm in width and length,3 those with static humeral migration on plain radiographs (reduced acromiohumeral index), and those with fatty degeneration of the supraspinatus and infraspinatus, as well as tears that are greater than 5 years old.4
Rotator cuff repair is an effective treatment option for most acute tears; however, in patients with massive rotator cuff tears, the failure rate of repair has been reported to be up to 40% to 94%.5, 6, 7 Non-arthroplasty treatment options for irreparable tears range from simple debridement with or without biceps tenotomy or tenodesis,8,9 partial repair,10 and latissimus dorsi tendon transfer11 to salvage options such as superior capsular reconstruction12 and balloon or biodegradable spacer implantation.13, 14, 15 When there is considerable glenohumeral joint arthropathy, treatment options shift to osseous procedures including glenohumeral joint arthrodesis and, recently, reverse shoulder arthroplasty (RSA).16
Bridging techniques have been described that improve the biomechanical environment of the repair, with many bridging grafts being used, including long head of the biceps tendon autograft,17 fascia lata autograft or allograft,18 and dermal patch allograft,19 as well as synthetic materials such as poly-L-lactic acid.20 The purpose of this article was to describe our preferred surgical approach for the reconstruction of a massive irreparable rotator cuff tear using a fascia lata patch autograft.
Surgical Technique
The complete surgical technique can be seen in Video 1. The pitfalls and pearls are summarized in Table 1, and the advantages and disadvantages are summarized in Table 2.
Table 1.
Pearls and Pitfalls of Technique
| Pearls |
| Neviaser portal for suture management and passage through medialized rotator cuff |
| Creation of tension-free partial repair |
| Use of goalpost sutures for partial repair and fixation of graft prior to fixation to remaining rotator cuff tendon |
| Lateral marking on graft to aid in proper orientation of graft intra-articularly |
| Suture management |
| Use of road map and color-coded sutures to aid in organization and intra-articular suture retrieval |
| Passage of graft sutures through their respective portals to aid in graft tensioning and orientation |
| Fixation of graft to remaining cuff in sequential order (lateral, followed anterior, medial, and posterior) |
| Pitfalls |
| Suture tangling |
| Suture management and retrieval |
| Graft orientation and twisting |
| Anterior and posterior releases to aid in partial repair mobility because this devitalizes remaining cuff |
Table 2.
Advantages and Disadvantages of Technique
| Advantages |
| Restoration of counterforce couple |
| Dynamic cuff control |
| Does not rely on access to costly allograft materials |
| Does not require extensive cuff release |
| Reconstruction performed without excessive tension on repair |
| Incorporates partial repair that is reinforced by reconstruction |
| Disadvantages |
| Graft donor-site morbidity |
| Requires adequate quality of medial cuff tissue |
| Suture tangling |
| Graft orientation |
Preoperative Assessment
A focused and thorough history and physical examination are undertaken prior to operative intervention. Included in the history is the timing of the initial injury, functional limitations, aggravating and alleviating activities, and a detailed pain history. On physical examination, particular note should be paid to differences between active and passive range of motion because the reconstruction is meant to restore functional motion and cannot achieve more range than the patient has passively. Testing of the rotator cuff musculature is performed to help identify the tendons involved in the tear, which include the Jobe test for supraspinatus deficiency, resisted external rotation for infraspinatus deficiency, horn-blower sign for a combination of infraspinatus and teres minor deficiency, and bear-hug test for subscapularis deficiency. In addition, one must look for any signs of axillary nerve or other neurologic injury affecting the extremity in question. On range-of-motion testing, abduction, forward elevation, external rotation, and internal rotation behind the back, as well as signs of a pseudoparalytic shoulder (abduction <90°), should be noted. Plain radiographs of the shoulder are taken to look for any signs of glenohumeral arthritis or superior migration of the humeral head, and a magnetic resonance imaging study of the shoulder is reviewed to determine tear size and retraction, as well as any other signs of irreparability including fatty infiltration and atrophy. Prior to undergoing an operation, the patient should undergo physiotherapy that focuses on strengthening of the deltoid and periscapular musculature.
Anesthesia and Patient Positioning
The patient is positioned on a Jackson table with a beanbag positioner placed underneath. A general anesthetic is then administered along with perioperative antibiotic prophylaxis. Once anesthetized, the patient is moved into the lateral decubitus position with approximately 30° of posterior angulation to align the glenoid parallel to the floor, with optimal support proximally ensured via the bag to resist any posteriorly directed forces. The operative shoulder is then prepared and draped in sterile fashion prior to being placed in a Spider arm limb positioner (Smith & Nephew, London, England). Once secured, the arm is placed in 60° of abduction and slight traction is applied.
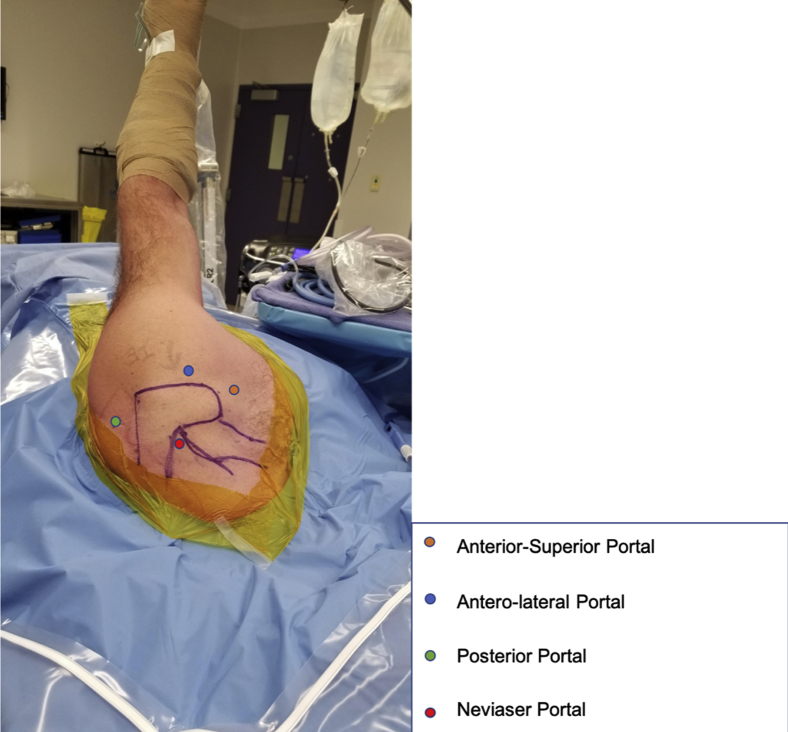
After the operative time-out, operative landmarks are identified and drawn, including the borders of the acromion, coracoid process, clavicle, scapular spine, and acromioclavicular (AC) joint, to guide portal placement (Fig 1). The posterior portal is then identified prior to performing a diagnostic arthroscopy.
Fig 1.
Patient placed in lateral decubitus position with light traction with use of hydraulic Spider arm positioner. The approximate positions of the portal sites are marked on the left shoulder.
Diagnostic Arthroscopy and Debridement
A diagnostic arthroscopy is performed from the posterior portal, which is made 1 cm inferior and lateral to the posterolateral corner of the acromion. First, the biceps tendon is examined as it attaches onto the superior labrum, followed by examination of the capsulolabral complex. After this, the articular surfaces of the glenoid and humerus are examined for signs of chondral damage and bone loss. Attention is then shifted to the rotator cuff footprint, looking for tear involvement and size. Next, the anterior and lateral portals are created using an inside-out technique to ensure the proper position and trajectory for anchor placement into the greater tuberosity. A Neviaser portal is created just medial to the AC joint to aid in graft passage as well as eventual fixation to the retracted portion of the cuff. Through the anterior portal, the posterior glenoid is briefly examined for any obvious signs of labral pathology. The camera is then switched to the lateral portal to examine the subacromial space and to assess and measure the dimensions of the tear (Fig 2). Here, we look for any signs of impingement, including acromial morphology, and perform an examination of the coracoacromial ligament. If signs of impingement are found, a release of the coracoacromial ligament is performed, followed by an acromioplasty of the anterior half of the acromion to the AC joint. Once the subacromial space is decompressed, the rotator cuff is examined for tear morphology and the degree of mobility. In this case, anterior and posterior releases of the rotator cuff are not performed to maintain as much vascular supply to the remaining tissue as possible. A grasper is used to determine the proper placement of the partial repair for a tension-free repair. The greater tuberosity is then examined for bone spurs or bone loss, followed by preparation of the rotator cuff footprint using either a burr or shaver to provide a fresh bleeding bone bed for the repair and eventual reconstruction.
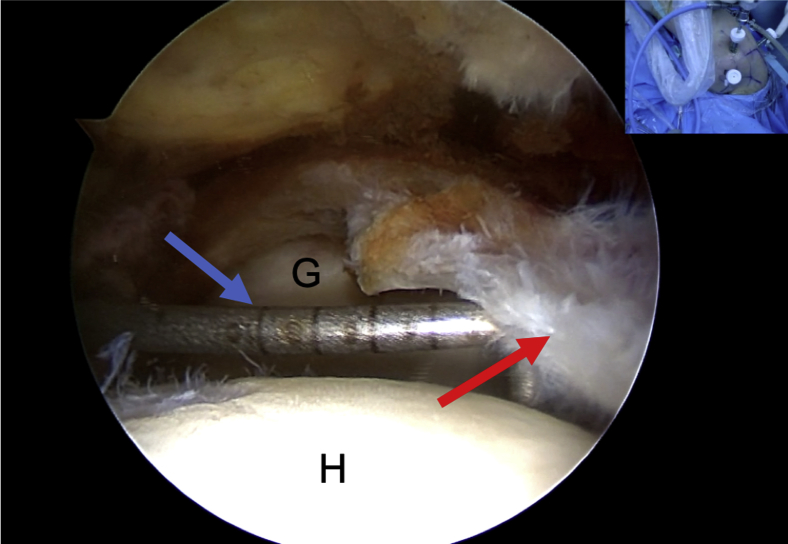
Fig 2.
Viewing from the lateral portal in left shoulder lateral decubitus position, tear morphology and dimensions are measured using a probe (blue arrow) from the posterior portal. Red arrow indicates anterior cuff. (G, glenoid; H, humeral head.)
Anchor Placement for Partial Repair
Once the tuberosity is prepared, 2 triple-loaded Helicoil all-suture anchors (Smith & Nephew) are placed percutaneously into the tuberosity (Fig 3), 1 anteriorly and 1 posteriorly. Full-thickness bites are taken through the leading edge of healthy tissue of the supraspinatus and infraspinatus tendons and secured to the anterior and posterior anchors, respectively, again ensuring a tension-free repair. The remaining sutures are left in their percutaneous portals to be used to aid in graft shuttling and fixation.
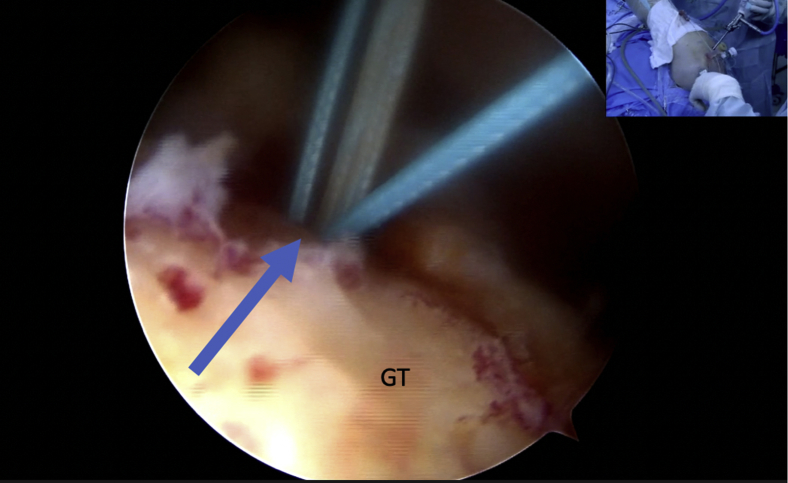
Fig 3.
Humeral anchor insertion (arrow) viewing from posterolateral portal in left shoulder lateral decubitus position. (GT, greater tuberosity.)
Graft Harvest
A 10-cm incision is marked over the lateral aspect of the hip, centered over the greater trochanter (Fig 4). The incision site, which was previously prepared and draped in sterile fashion, is taken down through the skin and subcutaneous tissue. The superficial fat is then bluntly dissected off the fascia lata with a clean sponge exposing the graft site. A rectangular patch measuring 10 cm longitudinally by 3 cm anteriorly to posteriorly is marked because prior measurements on magnetic resonance imaging determined the defect to be approximately 2.5 × 2.5 cm. The fascial defect is then closed using a No. 1 Vicryl suture (Ethicon, Somerville, NJ), followed by subcuticular closure with No. 2-0 Vicryl and staples for the skin.
Fig 4.
Fascia lata harvest site. (ASIS, anterior superior iliac spine; GT, greater tuberosity.)
Graft Preparation
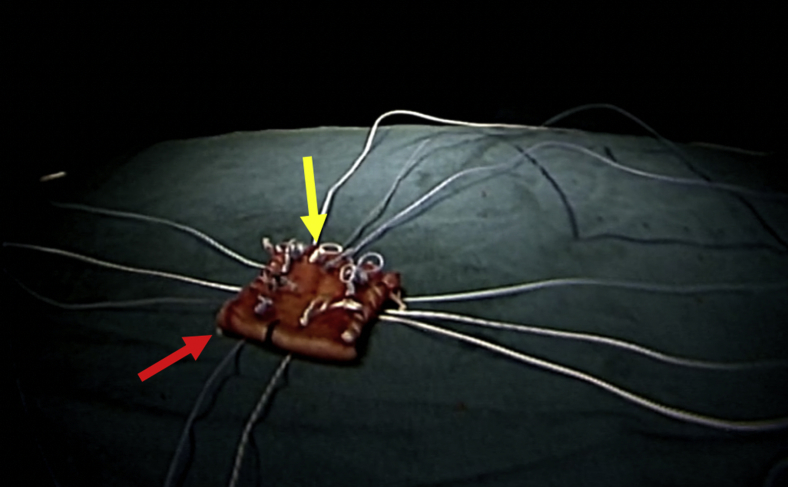
The fascia lata autograft is prepared on the back table. The excised graft is then folded over itself and cut to obtain a graft measuring 3 × 3 cm. The graft's free ends are sutured using a whipstitch technique to secure the graft's final dimensions (Fig 5). Suture placement sites on the graft are marked, with 3 located medially for fixation to the retracted rotator cuff at the glenoid, 3 for fixation to the supraspinatus tendon, 3 for fixation to the teres minor or remaining infraspinatus tendon, and 2 for fixation to the greater tuberosity. A mark is made on the lateral aspect of the graft to help guide orientation (Fig 6). A road map is created on the side table, drawing out the graft and the color-coded sutures (Fig 7). Eleven sutures are then passed through the graft at their respective sites according to the map, and short-tailed interference knots are tied over a switching stick for graft passage and eventual fixation (Fig 8).
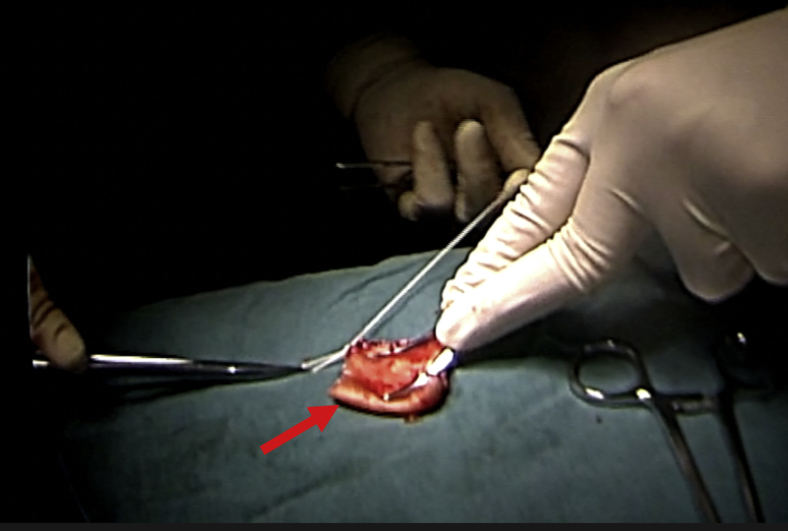
Fig 5.
Iliotibial band autograft (arrow) doubled over and stitched together.
Fig 6.
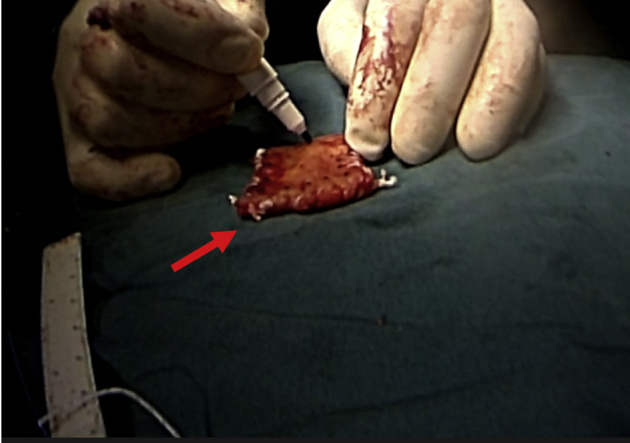
Iliotibial band graft (arrow) with suture markings (dots).
Fig 7.
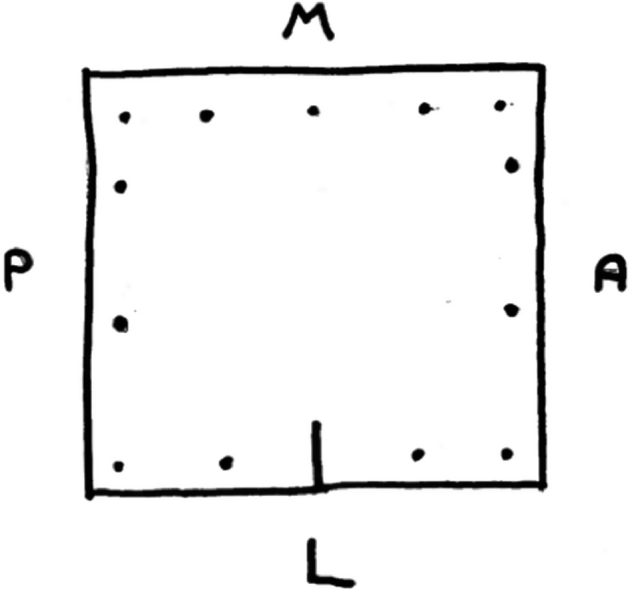
Example of road-map template. (A, anterior; L, lateral [humeral side]; M, medial [glenoid]; P, posterior.)
Fig 8.
Sutures are passed through the predetermined sites on the graft (red arrow) on the back table and are held in place by short-tailed interference knots (yellow arrow).
Securing of Graft
One limb of each goalpost suture from the anterior and posterior repair anchors is passed through the lateral portal and passed through the graft anteriorly and posteriorly; short-tailed interference knots are tied to aid in graft shuttling and tensioning. A suture-shuttling device is then introduced through the anterior portal, brought through the lateral portal for retrieval of the anterior suture limbs of the graft, and passed through the anterior portal. The same is then performed for both the posterior and Neviaser portals for the posterior and medial sutures, respectively. The graft is passed into the shoulder joint by keeping even tension on the anterior, posterior, and medial sutures and goalpost sutures while pushing the graft through the lateral cannula using a suture grasper. The graft is then flattened inside the shoulder by suture tensioning and assessed for correct dimensions. Once deemed appropriate, each of the anterior and posterior goalpost sutures are then tied, securing the graft to the anterior and posterior repair anchors. Next, the free end of each suture is passed through the rotator cuff using a Spectrum device (Linvatec, Largo, FL) sequentially and tied according to the road map, first anteriorly (Fig 9), then medially (Fig 10), and finally posteriorly (Fig 11), ensuring complete coverage and proper tensioning throughout. As part of the anterior repair, the remaining biceps tendon is incorporated into this fixation and undergoes tenodesis to the repair. A double-loaded Q-Fix all-suture anchor (Smith & Nephew) is then passed through the middle of the graft and placed into the greater tuberosity; one should be cognizant of the possibility of poor-quality bone. After this, the anterior tuberosity–sided sutures and 1 limb of the aforementioned suture anchor are passed through a MultiFix suture anchor (Smith & Nephew) and secured anterolaterally into the greater tuberosity (Fig 12). This process is then repeated with the posterior sutures and MultiFix suture anchor posterolaterally (Fig 13). With fixation in place, the tension and fixation of the graft are checked once more for adequate coverage and rippling prior to removal of the scope. With the graft appropriately tensioned, this should re-establish the rotator cuff's anterior-posterior force coupling as well as provide a superior restraint for humeral head depression.
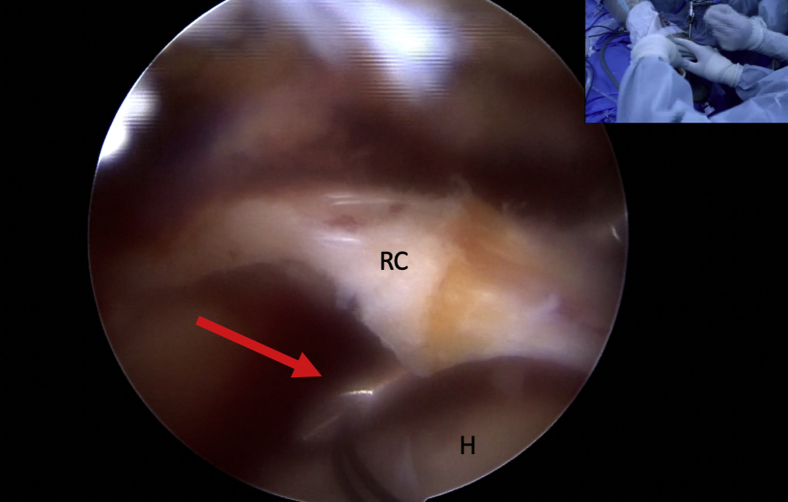
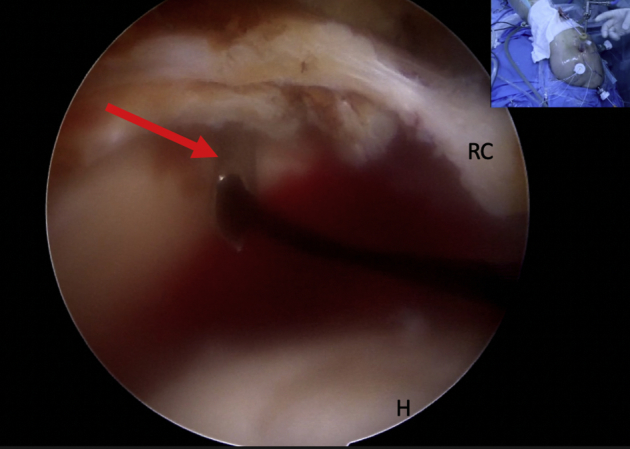
Fig 9.
The Spectrum suture passer (arrow) is passed through the anterior cuff and retrieves the corresponding suture on the graft. Patient position: lateral decubitus; shoulder: left. (H, humeral head; RC, rotator cuff.)
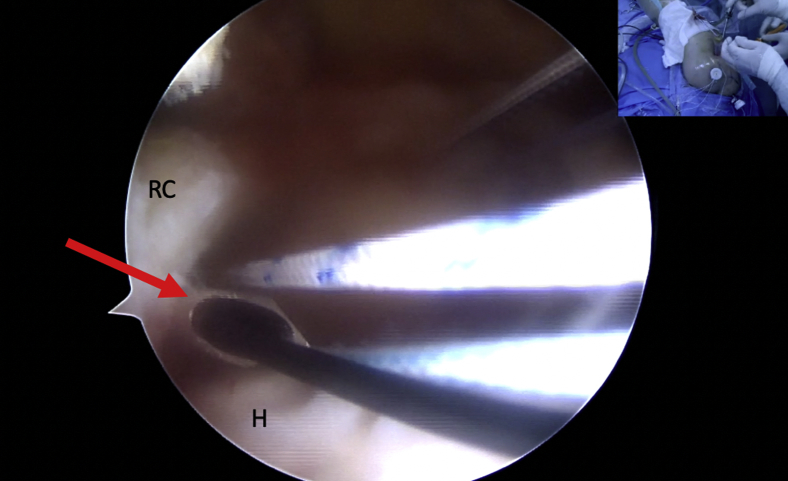
Fig 10.
The Spectrum suture passer (arrow) is passed through the middle cuff and retrieves the corresponding suture on the graft. Patient position: lateral decubitus; shoulder: left. (H, humeral head; RC, rotator cuff.)
Fig 11.
The Spectrum suture passer (arrow) is passed through the posterior cuff and retrieves the corresponding suture on the graft. Patient position: lateral decubitus; shoulder: left. (H, humeral head; RC, rotator cuff.)
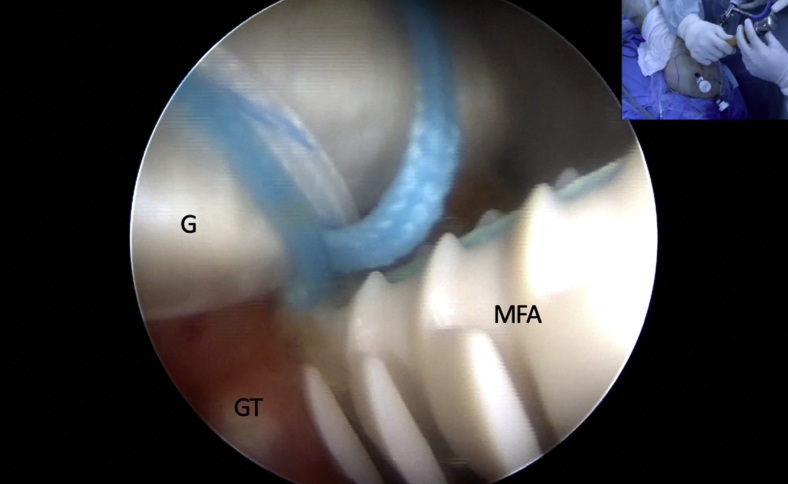
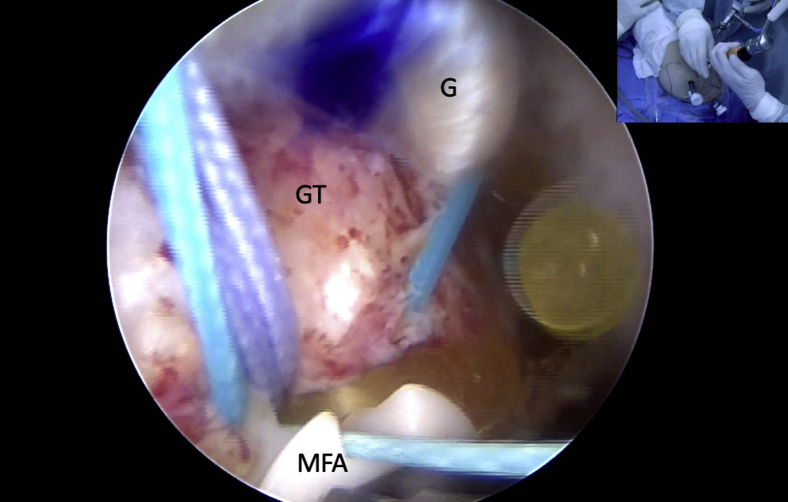
Fig 12.
Anterior lateral-row anchor for repair incorporating anterior partial repair and anterior humeral anchor sutures. Patient position: lateral decubitus; shoulder: left. (G, graft; GT, greater tuberosity; MFA, MultiFix humeral anchor.)
Fig 13.
Posterior lateral-row anchor for repair incorporating posterior partial repair and posterior humeral anchor sutures. Patient position: lateral decubitus; shoulder: left. (G, graft; GT, greater tuberosity; MFA, MultiFix humeral anchor.)
Discussion
Although rotator cuff repair has a high success rate, the treatment of large and massive tears remains an issue because of their high rates of failure. Risk factors for cuff failure have been investigated, and several factors have been found to correlate with increased retear rates. A study by Kim et al.21 showed a retear rate of 42.4%, with fatty degeneration of the infraspinatus muscle belly and rotator cuff retraction being the best predictors of failure. This finding was supported further by a multivariate analysis that showed preoperative fatty degeneration of the infraspinatus to be the greatest independent predictor of retearing.22 Other risk factors include age, tear size, number of tendons involved, acromiohumeral interval, and surgical technique, as well as bone mineral density.23 More recently, Shimokobe et al.24 prospectively followed up 102 patients with large to massive rotator cuff tears and found that preoperative external rotation to less than 25° was also an independent risk factor. In addition to high failure rates, many large to massive tears are deemed irreparable, posing a problem for many orthopaedic surgeons because there remains no clear-cut treatment algorithm for this clinical entity.25 Risk factors for irreparability include tears that result in retraction of the rotator cuff to the level of, or beyond, the glenoid, an increased glenohumeral distance, and a positive tangent sign.26
Treatment options for irreparable tears can be broken down into arthroplasty and soft-tissue procedures. Soft-tissue procedures include techniques involving the removal of significant pain generators, such as debridement and biceps tenotomy, or static humeral head depressors, such as superior capsular reconstruction, as well as subacromial balloon spacer implantation to prevent superior migration of the humeral head, in addition to partial repair and tendon transfer. However, none of these techniques properly re-establish the biomechanics of the glenohumeral joint. To restore normal glenohumeral kinematics, Burkhart27 referenced re-establishment of the force-coupling nature of the anterior and posterior rotator cuff. Limitations to the aforementioned procedures are due to the lack of re-establishment of the proper force vectors provided by an intact cuff. Rotator cuff reconstruction using patch augmentation can help bridge this gap to re-establishing the proper balance. By bridging the anterior and posterior cuff using a patch graft, the force-coupling nature of the rotator cuff is re-established.
Many different graft types have been used from autogenic and allogeneic sources and include iliotibial band and/or fascia lata graft and biceps tendon graft, as well as dermal allograft patches. In our case, we used the patient's fascia lata because many patients and centers cannot afford the costs attached to a dermal allograft patch. Fascia lata and/or iliotibial band graft has been used with success in many other reconstructive settings and has the ability to gradually remodel to tendinous tissue closely resembling normal tendon.28 In the setting of irreparable rotator cuff tears, the fascia lata provides a large, robust graft that can be cut to any size, with a good ability for suture retention and enhanced healing.29 Graft augmentation can be performed as either a reinforcement or strut for a tenuous repair or as a replacement of otherwise absent or deficient tissue. In our case, with the amount of retracted tendon, we used the graft to bridge the supraspinatus to the teres minor and to span the retracted tendon to the greater tuberosity. To facilitate rotator cuff and graft healing, we started by performing a partial repair under low tension. As shown by Kim et al.,30 there is an inverse relation between tissue tension at the repair site and tendon healing. In addition, Burkhart et al.31 have suggested that a low-tension repair may decrease the amount of postoperative pain owing to a decrease in mechanoreceptor stimulation. It is important to aim to limit the variables that may impede tendon healing and to provide the best environment for repair, which includes limited releases and devitalization of the remaining rotator cuff tendon. In this case, interval slides were not used to aid in mobilizing the tendons for partial repair because studies have shown that there is no improvement in outcomes or healing compared with an in situ partial repair.32
Rotator cuff reconstruction with a fascia lata autograft is an acceptable technique used to re-establish the force-coupling nature of the rotator cuff in tears that are deemed irreparable (Tables 1 and 2). It may be used as an alternative to RSA in a young population or in populations looking to avoid the complications associated with RSA. However, at this time, no long-term follow-up studies have followed patient outcomes of this procedure.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Rotator cuff reconstruction with fascia lata autograft for irreparable rotator cuff tear. The step-by-step technique for reconstructing an irreparable rotator cuff with a fascia lata autograft is outlined, with the patient in the lateral decubitus position.
References
- 1.Tashjian R.Z. Epidemiology, natural history, and indications for treatment of rotator cuff tears. Clin Sports Med. 2012;31:589–604. doi: 10.1016/j.csm.2012.07.001. [DOI] [PubMed] [Google Scholar]
- 2.Bedi A., Dines J., Warren R.F., Dines D.M. Massive tears of the rotator cuff. J Bone Joint Surg Am. 2010;92:1894–1908. doi: 10.2106/JBJS.I.01531. [DOI] [PubMed] [Google Scholar]
- 3.Sugihara T., Nakagawa T., Tsuchiya M., Ishizuki M. Prediction of primary reparability of massive tears of the rotator cuff on preoperative magnetic resonance imaging. J Shoulder Elbow Surg. 2003;12:222–225. doi: 10.1016/s1058-2746(02)86888-4. [DOI] [PubMed] [Google Scholar]
- 4.Nové-Josserand L., Edwards T.B., O’Connor D.P., Walch G. The acromiohumeral and coracohumeral intervals are abnormal in rotator cuff tears with muscular fatty degeneration. Clin Orthop Relat Res. 2005;433:90–96. doi: 10.1097/01.blo.0000151441.05180.0e. [DOI] [PubMed] [Google Scholar]
- 5.Burkhart S.S., Danaceau S.M., Pearce C.E. Arthroscopic rotator cuff repair: Analysis of results by tear size and by repair technique-margin convergence versus direct tendon-to-bone repair. Arthroscopy. 2001;17:905–912. doi: 10.1053/jars.2001.26821. [DOI] [PubMed] [Google Scholar]
- 6.Galatz L.M., Ball C.M., Teefey S.A., Middleton W.D., Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004;86-A:219–224. doi: 10.2106/00004623-200402000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Lo I.K.Y., Burkhart S.S. Arthroscopic revision of failed rotator cuff repairs: Technique and results. Arthroscopy. 2004;20:250–267. doi: 10.1016/j.arthro.2004.01.006. [DOI] [PubMed] [Google Scholar]
- 8.Pill S.G., Walch G., Hawkins R.J., Kissenberth M.J. The role of the biceps tendon in massive rotator cuff tears. Instr Course Lect. 2012;61:113–120. [PubMed] [Google Scholar]
- 9.Boileau P., Baqué F., Valerio L., Ahrens P., Chuinard C., Trojani C. Isolated arthroscopic biceps tenotomy or tenodesis improves symptoms in patients with massive irreparable rotator cuff tears. J Bone Joint Surg Am. 2007;89:747–757. doi: 10.2106/JBJS.E.01097. [DOI] [PubMed] [Google Scholar]
- 10.Burkhart S.S. Partial repair of massive rotator cuff tears: The evolution of a concept. Orthop Clin North Am. 1997;28:125–132. doi: 10.1016/s0030-5898(05)70270-4. [DOI] [PubMed] [Google Scholar]
- 11.Warner J.J. Management of massive irreparable rotator cuff tears: The role of tendon transfer. Instr Course Lect. 2001;50:63–71. [PubMed] [Google Scholar]
- 12.Burkhart S.S., Denard P.J., Adams C.R., Brady P.C., Hartzler R.U. Arthroscopic superior capsular reconstruction for massive irreparable rotator cuff repair. Arthrosc Tech. 2016;5:e1407–e1418. doi: 10.1016/j.eats.2016.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rosa D., Balato G., Ciaramella G., Di Donato S., Auletta N., Andolfi C. Treatment of massive irreparable rotator cuff tears through biodegradable subacromial InSpace Balloon. BMC Surg. 2013;13(suppl 1):A43. [Google Scholar]
- 14.Savarese E., Romeo R. New solution for massive, irreparable rotator cuff tears: The subacromial “biodegradable spacer.”. Arthrosc Tech. 2012;1:e69–e74. doi: 10.1016/j.eats.2012.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Prat D., Tenenbaum S., Pritsch M., Oran A., Vogel G. Sub-acromial balloon spacer for irreparable rotator cuff tears: Is it an appropriate salvage procedure? J Orthop Surg (Hong Kong) 2018;26 doi: 10.1177/2309499018770887. 2309499018770887. [DOI] [PubMed] [Google Scholar]
- 16.Petrillo S., Longo U.G., Papalia R., Denaro V. Reverse shoulder arthroplasty for massive irreparable rotator cuff tears and cuff tear arthropathy: A systematic review. Musculoskelet Surg. 2017;101:105–112. doi: 10.1007/s12306-017-0474-z. [DOI] [PubMed] [Google Scholar]
- 17.Cho N.S., Yi J.W., Rhee Y.G. Arthroscopic biceps augmentation for avoiding undue tension in repair of massive rotator cuff tears. Arthroscopy. 2009;25:183–191. doi: 10.1016/j.arthro.2008.09.012. [DOI] [PubMed] [Google Scholar]
- 18.Mori D., Funakoshi N., Yamashita F. Arthroscopic surgery of irreparable large or massive rotator cuff tears with low-grade fatty degeneration of the infraspinatus: Patch autograft procedure versus partial repair procedure. Arthroscopy. 2013;29:1911–1921. doi: 10.1016/j.arthro.2013.08.032. [DOI] [PubMed] [Google Scholar]
- 19.Gupta A.K., Hug K., Berkoff D.J. Dermal tissue allograft for the repair of massive irreparable rotator cuff tears. Am J Sports Med. 2012;40:141–147. doi: 10.1177/0363546511422795. [DOI] [PubMed] [Google Scholar]
- 20.Lenart B.A., Martens K.A., Kearns K.A., Gillespie R.J., Zoga A.C., Williams G.R. Treatment of massive and recurrent rotator cuff tears augmented with a poly-l-lactide graft, a preliminary study. J Shoulder Elbow Surg. 2015;24:915–921. doi: 10.1016/j.jse.2014.09.044. [DOI] [PubMed] [Google Scholar]
- 21.Kim J.R., Cho Y.S., Ryu K.J., Kim J.H. Clinical and radiographic outcomes after arthroscopic repair of massive rotator cuff tears using a suture bridge technique: Assessment of repair integrity on magnetic resonance imaging. Am J Sports Med. 2012;40:786–793. doi: 10.1177/0363546511434546. [DOI] [PubMed] [Google Scholar]
- 22.Oh J.H., Kim S.H., Ji H.M., Jo K.H., Bin S.W., Gong H.S. Prognostic factors affecting anatomic outcome of rotator cuff repair and correlation with functional outcome. Arthroscopy. 2009;25:30–39. doi: 10.1016/j.arthro.2008.08.010. [DOI] [PubMed] [Google Scholar]
- 23.Saccomanno M.F., Sircana G., Cazzato G., Donati F., Randelli P., Milano G. Prognostic factors influencing the outcome of rotator cuff repair: A systematic review. Knee Surg Sports Traumatol Arthrosc. 2016;24:3809–3819. doi: 10.1007/s00167-015-3700-y. [DOI] [PubMed] [Google Scholar]
- 24.Shimokobe H., Gotoh M., Honda H. Risk factors for retear of large/massive rotator cuff tears after arthroscopic surgery: An analysis of tearing patterns. J Orthop Surg Res. 2017;12:140. doi: 10.1186/s13018-017-0643-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Oh J.H., Park M.S., Rhee S.M. Treatment strategy for irreparable rotator cuff tears. Clin Orthop Relat Res. 2018;10:119–134. doi: 10.4055/cios.2018.10.2.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dwyer T., Razmjou H., Henry P., Gosselin-Fournier S., Holtby R. Association between pre-operative magnetic resonance imaging and reparability of large and massive rotator cuff tears. Knee Surg Sports Traumatol Arthrosc. 2015;23:415–422. doi: 10.1007/s00167-013-2745-z. [DOI] [PubMed] [Google Scholar]
- 27.Burkhart S.S., Fluoroscopic comparison of kinematic patterns in massive rotator cuff tears A suspension bridge model. Clin Orthop Relat Res. 1992;284:144–152. [PubMed] [Google Scholar]
- 28.Sano H., Kumagai J., Sawai T. Experimental fascial autografting for the supraspinatus tendon defect: Remodeling process of the grafted fascia and the insertion into bone. J Shoulder Elbow Surg. 2002;11:166–173. doi: 10.1067/mse.2002.120808. [DOI] [PubMed] [Google Scholar]
- 29.Derwin K.A., Aurora A., Iannotti J.P. Cleveland Clinic; Cleveland, OH: 2008. Allograft fascia lata as an augmentation device for musculoskeletal repairs. [Google Scholar]
- 30.Kim D.H., Jang Y.H., Choi Y.E., Lee H.-R., Kim S.H. Evaluation of repair tension in arthroscopic rotator cuff repair: Does it really matter to the integrity of the rotator cuff? Am J Sports Med. 2016;44:2807–2812. doi: 10.1177/0363546516651831. [DOI] [PubMed] [Google Scholar]
- 31.Burkhart S.S., Johnson T.C., Wirth M.A., Athanasiou K.A. Cyclic loading of transosseous rotator cuff repairs: Tension overload as a possible cause of failure. Arthroscopy. 1997;13:172–176. doi: 10.1016/s0749-8063(97)90151-1. [DOI] [PubMed] [Google Scholar]
- 32.Kim S.-J., Kim S.-H., Lee S.-K., Seo J.-W., Chun Y.-M. Arthroscopic repair of massive contracted rotator cuff tears: Aggressive release with anterior and posterior interval slides do not improve cuff healing and integrity. J Bone Joint Surg Am. 2013;95:1482–1488. doi: 10.2106/JBJS.L.01193. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Rotator cuff reconstruction with fascia lata autograft for irreparable rotator cuff tear. The step-by-step technique for reconstructing an irreparable rotator cuff with a fascia lata autograft is outlined, with the patient in the lateral decubitus position.