Abstract
Meniscal allograft transplantation has been introduced as a treatment for symptomatic meniscus-deficient patients to improve clinical outcomes. We describe an arthroscopic technique for meniscal allograft with soft-tissue fixation including the anterior intermeniscal ligament (AIML): arthroscopic double soft-tissue fixation technique. The AIML and anterior and posterior roots are detached and sutured using running locked Krackow stitches. After preparation of the meniscal bed, the meniscus is passed into the knee and the posterior meniscal horn is fixed with sutures through bone tunnels. The body of the meniscus is fixed with all-inside sutures. Then, the anterior meniscal suture is fixed on the anatomic point of the anterior root with an anchor. The AIML suture is fixed with an anchor to the bare area of the proximal tibia, anterior to the anterior cruciate ligament insertion. This reliable and reproducible technique is less complex than bone plug methods; it is less invasive but still provides stable and secure graft fixation. It will help surgeons to improve clinical results and to limit early secondary extrusion of the graft.
Meniscal tears are the most common knee injury, and their management has changed in recent decades.1, 2, 3 Smaller meniscal tears are treated by direct repair or partial resection, depending on the location and type of tear.3 However, large, complex meniscal tears that are unsuitable for repair are usually treated by total meniscectomy, which affects their primary functions of load sharing and shock absorption, as well as their secondary function of knee stabilization, and induces premature arthritic changes.3, 4, 5
Meniscal allograft transplantation (MAT) has been introduced as a treatment for symptomatic patients after subtotal or total meniscectomy to reduce knee pain and improve clinical outcomes.1,2,5, 6, 7, 8, 9, 10 Successful allograft fixation has been reported using bone block fixation or soft-tissue fixation, although it remains unclear which technique is better.1,2,11, 12, 13, 14, 15, 16, 17, 18 However, graft extrusion after MAT can remain a factor in postoperative failure, and various surgical techniques are still being introduced to reduce extrusion.19, 20, 21, 22, 23
The anterior intermeniscal ligament (AIML) stabilizes the meniscus mechanically as part of the “meniscal belt.”24, 25, 26 When the AIML was resected in a biomechanical study, mechanical meniscal extrusion was also observed.24 Therefore, the AIML might help to prevent extrusion after MAT. In this report, we introduce an arthroscopic MAT method with soft-tissue fixation including the AIML—the arthroscopic double soft-tissue fixation technique—that is a simpler, less invasive procedure than bone plug techniques, and it secures the allograft.
Surgical Technique
Video 1 shows the arthroscopic lateral MAT technique in a right knee with double soft-tissue fixation. Medial MAT can be performed using the same philosophy as lateral MAT.
Step 1: Patient Positioning, Diagnostic Arthroscopy, and Meniscal Remnant Preparation
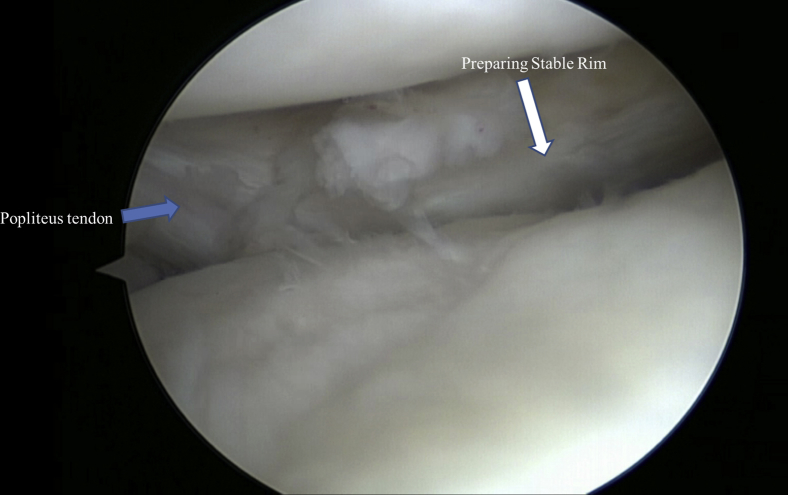
The surgical procedure is performed with the patient under general or regional anesthesia positioned supine with a tourniquet and a single leg holder. Standard anterolateral and anteromedial portals are made at 90° of knee flexion. For lateral MAT, the knee is positioned in the figure-of-4 position. For medial MAT, the knee is positioned in valgus by the operating or assistant surgeon. Diagnostic arthroscopy is performed systematically, with careful evaluation of concomitant pathology in the MAT compartment. After probing to assess the remaining meniscal tissue, the meniscal rim is prepared using arthroscopic biters and shavers to debride the remaining meniscal tissue, resulting in a stable 1- to 2-mm rim (Fig 1).
Fig 1.
Arthroscopic meniscal rim preparation is performed using biters and shavers to make a stable 1- to 2-mm rim. The lateral meniscus is shown in a right knee.
Step 2: Preparation of Meniscal Allograft
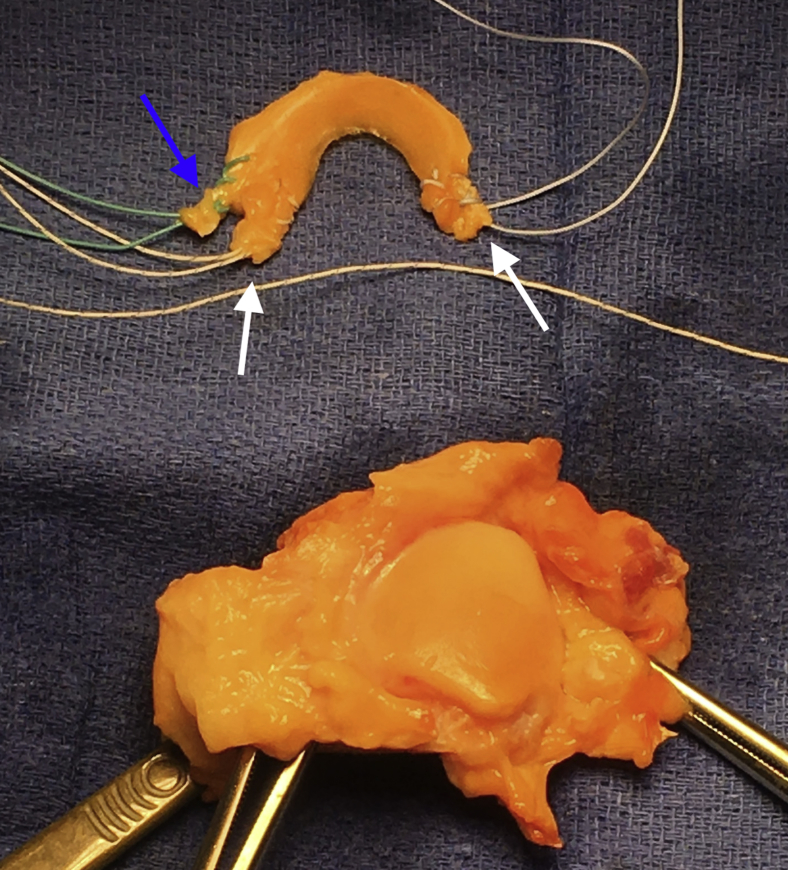
The meniscal allograft, which is ordered from a national tissue bank and includes the tibial plateau bone block with all soft tissues, is thawed in normal saline solution. For our technique, the AIML is identified first. Because the AIML is present in 54% to 94% of knees25 and usually connects the anterior horns of the medial and lateral menisci,27 it is easily found regardless of type.24,27 If the AIML does not clearly connect the menisci, such as in a type 2 AIML,27 the AIML is sharply excised with the associated soft tissues, including the anterior capsular structure (Table 1). On the basis of a biomechanical study, we believe that additional fixation of the AIML increases the stability of the transplanted allograft and prevents its early extrusion (Video 1).24 After the AIML is prepared, the anterior and posterior roots of the meniscal allograft are detached from the bone block, and a running locked Krackow stitch is performed using Ethibond (Ethicon, Somerville, NJ) and FiberWire (Arthrex, Naples, FL) on the AIML and anterior and posterior roots (Fig 2). The allograft is trimmed to remove unusable edges that could interrupt reduction of the allograft to the stable remaining meniscal tissue, which was prepared in the previous step.
Table 1.
Types of Insertion Patterns of Anterior Intermeniscal Ligament
| Type 1: attachments to the anterior horn of the medial meniscus and anterior margin of the lateral meniscus |
| Type 2: medial attachment to the anterior margin of the medial meniscus and lateral attachment to the joint capsule anterior to the lateral meniscus |
| Type 3: medial and lateral capsular anterior attachments only, with no direct attachments to the anterior horn of the medial meniscus or to the lateral meniscus |
Fig 2.
Graft preparation for lateral meniscal allograft transplantation in a right knee. A locked Krackow stitch is located on the anterior intermeniscal ligament (blue arrow) and anterior and posterior roots (white arrows). Green Ethibond is passed through the anterior intermeniscal ligament, and white FiberWire is passed through the anterior and posterior horns.
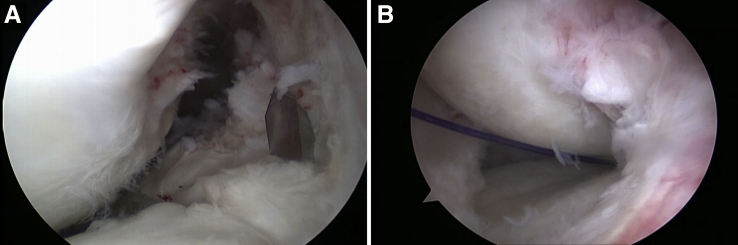
Step 3: Preparation of Posterior Root Tunnel
The tibial tunnel for the posterior root is located in the anatomic position just posterior to the anterior cruciate ligament (ACL) for lateral MAT and just posterior to the medial tibial spine for medial MAT (Fig 3). The insertion site for the posterior horn is prepared using a shaver until the subchondral bone is exposed. After a 1-cm skin incision is made on the medial tibia, the ACL tibial guide is inserted through the working portal and placed on the posterior-horn insertion site. The tibial tunnel for the posterior root is initially drilled with a Beath pin to confirm the appropriate tunnel location, and it is then overdrilled with a 4.5-mm cannulated drill, with the tip left safely positioned (Fig 3). A loop of PDS (Ethicon) is passed through the cannulated drill bit and retrieved through the working portal using an arthroscopic grasper (Fig 3).
Fig 3.
The insertion site of the posterior horn is prepared in a right knee. (A) The Beath pin is located just posterior to the anterior cruciate ligament for lateral meniscal allograft transplantation. (B) A loop of PDS is retrieved through the working portal.
Step 4: Graft Passage and Placement
By use of a loop of PDS suture, a running locked suture in the posterior root of the allograft is passed through the tibial tunnel at the insertion site of the posterior horn. Then, the meniscal allograft is passed through the working portal while pulling the locked sutures and is placed in the knee joint in the correct orientation using a blunt trocar. The posterior-root sutures are secured temporarily over the tibial bone bridge using a Kelly clamp.
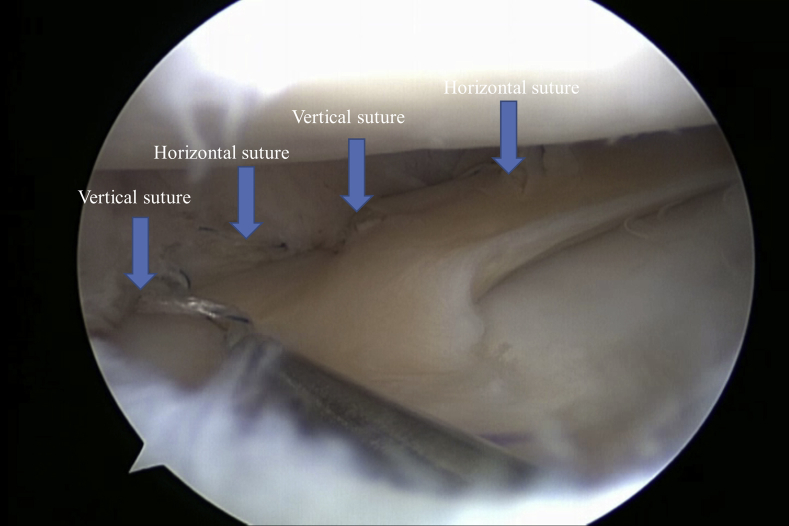
Step 5: Graft Suturing
After the size and position of the meniscal allograft are assessed, all-inside meniscal suturing is completed from the posterior horn to the mid body of the meniscal allograft using the Fast-Fix 360 suture system (Smith & Nephew, Andover, MA). Horizontal and additional vertical sutures are used to achieve stable fixation of the meniscal allograft. The additional vertical sutures are placed alternately between the superior and inferior borders of the meniscocapsular junction (Fig 4). Usually, 6 or 7 stitches are placed.
Fig 4.
Combined horizontal and additional vertical sutures are placed using the Fast-Fix 360 system in a right knee.
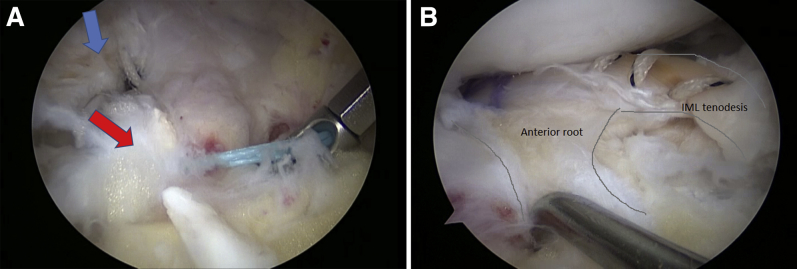
Step 6: Preparation and Fixation of Anterior Root and AIML of Graft
After the meniscal suture, the AIML suture is passed through the viewing portal whereas the anterior-root suture is left in the working portal. The insertion site for the anterior horn is marked using the ArthroCare system (Smith & Nephew) anterior to the lateral tibial spine and lateral to the ACL for lateral MAT and anterior and medial to the ACL for medial MAT (Fig 5). The anterior-root suture is fixed with a 4.75-mm SwiveLock anchor (Arthrex) at the insertion site of the anterior root with proper tension (Fig 5). The insertion site for the anterior root is not debrided using a shaver or burr because of the risk of pulling out the SwiveLock anchor, whereas the posterior-horn insertion site is debrided. After fixation of the anterior root, the AIML suture is fixed with a 4.75-mm SwiveLock anchor to the bare area of the proximal tibia (Fig 5). This bare area is located on the proximal tibial tuberosity, anterior to the ACL insertion and below the infrapatellar fat pad. The fixation point is based on the length of the AIML in the allograft. This allows supplementary anterior transversal fixation of the graft.
Fig 5.
The insertion site for lateral meniscal allograft transplantation is located anterior to the lateral tibial spine and lateral to the anterior cruciate ligament in a right knee. The anterior root is fixed with a SwiveLock anchor. (A) The anterior root of the allograft is fixed on the anatomic point of the lateral meniscus anterior root (blue arrow), and the anterior intermeniscal ligament (red arrow) of the allograft is across from the meniscus at the bare area of the proximal tibia. (B) The anterior intermeniscal ligament (IML) is fixed with a SwiveLock anchor on the bare area: final aspect.
Step 7: Fixation of Posterior Root
After fixation of the anterior root and AIML of the allograft, an EndoButton (Smith & Nephew) is used to fix the posterior-root suture at the entry of the tibial tunnel (Fig 6). After probing to ensure stable fixation, the skin incision and portals are closed. After surgery, a knee brace is applied, flexion is limited to 90°, and weight bearing is not allowed until 4 weeks.
Fig 6.
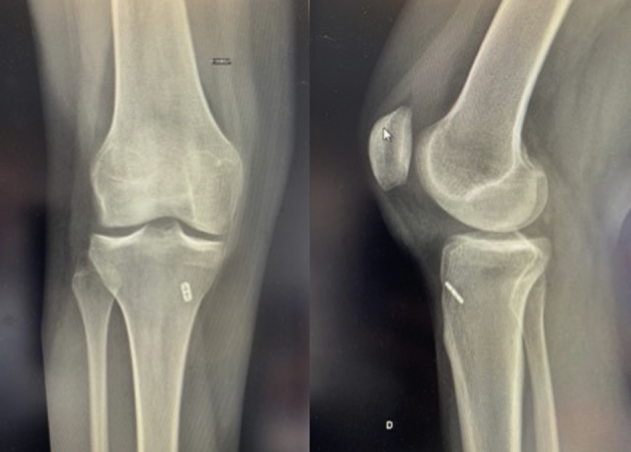
An EndoButton is used to ensure fixation of the posterior-root suture at the entry of the tibial tunnel, as shown on anteroposterior and lateral views of a right knee.
Discussion
For decades, MAT has been performed in young patients before osteoarthritis develops.1,8 However, there are many surgical techniques, especially for root fixation,1 and it is still unclear whether bone fixation or soft-tissue fixation has better clinical and survival outcomes.1,2,8 Biomechanical studies reported potential advantages of bone fixation techniques compared with soft-tissue fixation: lower contact pressure and more secure fixation.28, 29, 30 However, a recent meta-analysis found no difference between the techniques in terms of outcome scores, allograft tear rates, and procedure failure rates, and a high degree of allograft extrusion is found regardless of the technique.1,31 Therefore, we believe that, after combined AIML fixation, our technique can achieve better stability than the previous soft-tissue or bone fixation techniques. Because the AIML seemed to stabilize the meniscus in biomechanical studies,24, 25, 26 our double soft-tissue fixation method can secure the transplanted meniscus and may reduce early extrusion.
Our technique has potential limitations. First, the anatomic variance of the insertion of the AIML, such as type 3, makes the application of this technique difficult. Because there are no connections to the anterior horns of the lateral and medial menisci in type 3 variance, it is hard to use the AIML only as a secondary fixator. To address such situations, we harvest the AIML with the associated soft tissues, including the anterior capsular structure. Second, the length of the AIML depends on the surgeon who harvests the allograft; thus, the fixation point of the AIML might be changed according to the length of the AIML. However, as long as we fix the AIML to the bare area of the proximal tibia, which is relatively broad, we can use this technique with minimum risk even with nominal variance in the length of the AIML. The pearls and pitfalls of our technique are summarized in Table 2, and advantages and disadvantages are shown in Table 3. In our experience, this technique is an easy, reliable, and reproducible method for both lateral and medial MAT and is more flexible in terms of graft size adaptation during surgery.
Table 2.
Pearls and Pitfalls
| Pearls |
| Identify and harvest the AIML first, before detaching the root of the meniscus. |
| Note that careful dissection of the AIML is necessary to avoid a short length or disconnection of the AIML from the meniscus. |
| Adequately prepare the native rim to enhance healing with allograft. |
| Fix the anterior horn and AIML after graft suturing from the posterior horn to the mid body to avoid extensive traction of the allograft. |
| Pitfalls |
| Avoid excessive traction and fixation of the AIML resulting in a large intrusion of the meniscus. |
| Bear in mind that additional vertical sutures to the superior and inferior borders could induce graft eversion. |
AIML, anterior intermeniscal ligament.
Table 3.
Advantages and Disadvantages
| Advantages |
| Additional AIML fixation might make the graft more stable to avoid extrusion. |
| There is more flexibility in determining the fixation point of the anterior horn according to the size of the allograft owing to secondary coverage of the AIML and associated soft tissue. |
| It is easy to apply our technique to both medial and lateral MAT via the same philosophy. |
| Disadvantages |
| Anatomic variance of the AIML insertion makes this technique difficult. |
| Identification and harvesting of the AIML depends on the surgeon's technique. |
| The length and strength might be changed according to the surgeon's harvesting technique. |
AIML, anterior intermeniscal ligament; MAT, meniscal allograft transplantation.
This article describes a technique of arthroscopic soft-tissue MAT with additional anterior fixation of the intermeniscal ligament. We have performed this technique for more than 5 years, and the short- to mid-term results are encouraging. The arthroscopic double soft-tissue fixation technique is easy and reliable for MAT. Research should examine ways to improve our results and evaluate whether the technique decreases early extrusion and secondary replacement in young patients after meniscectomy.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: N.P. receives payment for development of educational presentations from Zimmer Biomet and Smith & Nephew. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Arthroscopic double soft-tissue fixation technique for lateral meniscal allograft transplantation in a right knee. Traction of the anterior intermeniscal ligament (AIML) shows the movement of the entire meniscus, especially in an intruded direction. Intraoperatively, the AIML is identified first; a running locked Krackow stitch is performed using Ethibond. After detachment of the anterior and posterior roots sharply, a running locked Krackow stitch is performed using FiberWire. For the orientation in an anteroposterior direction with a superoinferior surface, a sign is marked on the meniscal allograft. The tibial tunnel for the posterior root is located in the anatomic position just posterior to the anterior cruciate ligament (ACL). After allograft is located in the knee joint, all-inside meniscal suturing is completed from the posterior horn to the mid body of the meniscal allograft using the Fast-Fix 360 suture system. Then, the anterior-root suture is fixed with a 4.75-mm SwiveLock anchor at the insertion site of the anterior root. After fixation of the anterior root, the AIML suture is fixed with a 4.75-mm SwiveLock anchor to the bare area of the proximal tibia. The fixation point is based on the length of the AIML in the allograft.
References
- 1.Jauregui J.J., Wu Z.D., Meredith S., Griffith C., Packer J.D., Henn R.F., III How should we secure our transplanted meniscus? A meta-analysis. Am J Sports Med. 2018;46:2285–2290. doi: 10.1177/0363546517720183. [DOI] [PubMed] [Google Scholar]
- 2.Elattar M., Dhollander A., Verdonk R., Almqvist K.F., Verdonk P. Twenty-six years of meniscal allograft transplantation: Is it still experimental? A meta-analysis of 44 trials. Knee Surg Sports Traumatol Arthrosc. 2011;19:147–157. doi: 10.1007/s00167-010-1351-6. [DOI] [PubMed] [Google Scholar]
- 3.Woodmass J.M., LaPrade R.F., Sgaglione N.A., Nakamura N., Krych A.J. Meniscal repair: Reconsidering indications, techniques, and biologic augmentation. J Bone Joint Surg Am. 2017;99:1222–1231. doi: 10.2106/JBJS.17.00297. [DOI] [PubMed] [Google Scholar]
- 4.Ryu R.K., Dunbar V.W., Morse G.G. Meniscal allograft replacement: A 1-year to 6-year experience. Arthroscopy. 2002;18:989–994. doi: 10.1053/jars.2002.36104. [DOI] [PubMed] [Google Scholar]
- 5.Pengas I.P., Assiotis A., Nash W., Hatcher J., Banks J., McNicholas M.J. Total meniscectomy in adolescents: A 40-year follow-up. J Bone Joint Surg Br. 2012;94:1649–1654. doi: 10.1302/0301-620X.94B12.30562. [DOI] [PubMed] [Google Scholar]
- 6.Sekiya J.K., Giffin J.R., Irrgang J.J., Fu F.H., Harner C.D. Clinical outcomes after combined meniscal allograft transplantation and anterior cruciate ligament reconstruction. Am J Sports Med. 2003;31:896–906. doi: 10.1177/03635465030310062701. [DOI] [PubMed] [Google Scholar]
- 7.Gonzalez-Lucena G., Gelber P.E., Pelfort X., Tey M., Monllau J.C. Meniscal allograft transplantation without bone blocks: A 5- to 8-year follow-up of 33 patients. Arthroscopy. 2010;26:1633–1640. doi: 10.1016/j.arthro.2010.05.005. [DOI] [PubMed] [Google Scholar]
- 8.Hergan D., Thut D., Sherman O., Day M.S. Meniscal allograft transplantation. Arthroscopy. 2011;27:101–112. doi: 10.1016/j.arthro.2010.05.019. [DOI] [PubMed] [Google Scholar]
- 9.Dangelmajer S., Familiari F., Simonetta R., Kaymakoglu M., Huri G. Meniscal transplants and scaffolds: A systematic review of the literature. Knee Surg Relat Res. 2017;29:3–10. doi: 10.5792/ksrr.16.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee B.S., Kim J.M., Sohn D.W., Bin S.I. Review of meniscal allograft transplantation focusing on long-term results and evaluation methods. Knee Surg Relat Res. 2013;25:1–6. doi: 10.5792/ksrr.2013.25.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marcacci M., Marcheggiani Muccioli G.M., Grassi A. Arthroscopic meniscus allograft transplantation in male professional soccer players: A 36-month follow-up study. Am J Sports Med. 2014;42:382–388. doi: 10.1177/0363546513508763. [DOI] [PubMed] [Google Scholar]
- 12.Hommen J.P., Applegate G.R., Del Pizzo W. Meniscus allograft transplantation: Ten-year results of cryopreserved allografts. Arthroscopy. 2007;23:388–393. doi: 10.1016/j.arthro.2006.11.032. [DOI] [PubMed] [Google Scholar]
- 13.Yang B.S., Choi N.H., Kim B.Y. Intraoperative templating in lateral meniscal allograft transplantation. Clin Orthop Surg. 2016;8:481–483. doi: 10.4055/cios.2016.8.4.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ambra L.F., Mestriner A.B., Ackermann J., Phan A.T., Farr J., Gomoll A.H. Bone-plug versus soft tissue fixation of medial meniscal allograft transplants: A biomechanical study. Am J Sports Med. 2019;27 doi: 10.1177/0363546519870179. [DOI] [PubMed] [Google Scholar]
- 15.Masferrer-Pino A., Monllau J.C., Abat F., Gelber P.E. Capsular fixation limits graft extrusion in lateral meniscal allograft transplantation. Int Orthop. 2019;23:019-04398. doi: 10.1007/s00264-019-04398-8. [DOI] [PubMed] [Google Scholar]
- 16.Brial C., McCarthy M., Adebayo O. Lateral meniscal graft transplantation: Effect of fixation method on joint contact mechanics during simulated gait. Am J Sports Med. 2019;47:2437–2443. doi: 10.1177/0363546519860113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Novaretti J.V., Lian J., Sheean A.J. Lateral meniscal allograft transplantation with bone block and suture-only techniques partially restores knee kinematics and forces. Am J Sports Med. 2019;47:2427–2436. doi: 10.1177/0363546519858085. [DOI] [PubMed] [Google Scholar]
- 18.Zaffagnini S., Grassi A., Macchiarola L. Meniscal allograft transplantation is an effective treatment in patients older than 50 years but yields inferior results compared with younger patients: A case-control study. Arthroscopy. 2019;35:2448–2458. doi: 10.1016/j.arthro.2019.03.048. [DOI] [PubMed] [Google Scholar]
- 19.Lee D.H. Incidence and extent of graft extrusion following meniscus allograft transplantation. Biomed Res Int. 2018;2018:5251910. doi: 10.1155/2018/5251910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Noyes F.R., Barber-Westin S.D. A systematic review of the incidence and clinical significance of postoperative meniscus transplant extrusion. Knee Surg Sports Traumatol Arthrosc. 2015;23:290–302. doi: 10.1007/s00167-014-3329-2. [DOI] [PubMed] [Google Scholar]
- 21.Masferrer-Pino A., Monllau J.C., Ibanez M., Erquicia J.I., Pelfort X., Gelber P.E. Capsulodesis versus bone trough technique in lateral meniscal allograft transplantation: Graft extrusion and functional results. Arthroscopy. 2018;34:1879–1888. doi: 10.1016/j.arthro.2018.01.017. [DOI] [PubMed] [Google Scholar]
- 22.Koh Y.G., Kim Y.S., Kwon O.R., Heo D.B., Tak D.H. Comparative matched-pair analysis of keyhole bone-plug technique versus arthroscopic-assisted pullout suture technique for lateral meniscal allograft transplantation. Arthroscopy. 2018;34:1940–1947. doi: 10.1016/j.arthro.2018.01.053. [DOI] [PubMed] [Google Scholar]
- 23.Novaretti J.V., Patel N.K., Lian J. Long-term survival analysis and outcomes of meniscal allograft transplantation with minimum 10-year follow-up: A systematic review. Arthroscopy. 2019;35:659–667. doi: 10.1016/j.arthro.2018.08.031. [DOI] [PubMed] [Google Scholar]
- 24.Ollivier M., Falguieres J., Pithioux M., Boisrenoult P., Beaufils P., Pujol N. Sectioning of the anterior intermeniscal ligament changes knee loading mechanics. Arthroscopy. 2018;34:2837–2843. doi: 10.1016/j.arthro.2018.03.007. [DOI] [PubMed] [Google Scholar]
- 25.Poh S.Y., Yew K.S., Wong P.L. Role of the anterior intermeniscal ligament in tibiofemoral contact mechanics during axial joint loading. Knee. 2012;19:135–139. doi: 10.1016/j.knee.2010.12.008. [DOI] [PubMed] [Google Scholar]
- 26.Guess T.M., Razu S.S., Kuroki K., Cook J.L. Function of the anterior intermeniscal ligament. J Knee Surg. 2018;31:68–74. doi: 10.1055/s-0037-1600089. [DOI] [PubMed] [Google Scholar]
- 27.Nelson E.W., LaPrade R.F. The anterior intermeniscal ligament of the knee. An anatomic study. Am J Sports Med. 2000;28:74–76. doi: 10.1177/03635465000280012401. [DOI] [PubMed] [Google Scholar]
- 28.Chen M.I., Branch T.P., Hutton W.C. Is it important to secure the horns during lateral meniscal transplantation? A cadaveric study. Arthroscopy. 1996;12:174–181. doi: 10.1016/s0749-8063(96)90007-9. [DOI] [PubMed] [Google Scholar]
- 29.Alhalki M.M., Howell S.M., Hull M.L. How three methods for fixing a medial meniscal autograft affect tibial contact mechanics. Am J Sports Med. 1999;27:320–328. doi: 10.1177/03635465990270030901. [DOI] [PubMed] [Google Scholar]
- 30.McDermott I.D., Lie D.T., Edwards A., Bull A.M., Amis A.A. The effects of lateral meniscal allograft transplantation techniques on tibio-femoral contact pressures. Knee Surg Sports Traumatol Arthrosc. 2008;16:553–560. doi: 10.1007/s00167-008-0503-4. [DOI] [PubMed] [Google Scholar]
- 31.Myers P., Tudor F. Meniscal allograft transplantation: How should we be doing it? A systematic review. Arthroscopy. 2015;31:911–925. doi: 10.1016/j.arthro.2014.11.020. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic double soft-tissue fixation technique for lateral meniscal allograft transplantation in a right knee. Traction of the anterior intermeniscal ligament (AIML) shows the movement of the entire meniscus, especially in an intruded direction. Intraoperatively, the AIML is identified first; a running locked Krackow stitch is performed using Ethibond. After detachment of the anterior and posterior roots sharply, a running locked Krackow stitch is performed using FiberWire. For the orientation in an anteroposterior direction with a superoinferior surface, a sign is marked on the meniscal allograft. The tibial tunnel for the posterior root is located in the anatomic position just posterior to the anterior cruciate ligament (ACL). After allograft is located in the knee joint, all-inside meniscal suturing is completed from the posterior horn to the mid body of the meniscal allograft using the Fast-Fix 360 suture system. Then, the anterior-root suture is fixed with a 4.75-mm SwiveLock anchor at the insertion site of the anterior root. After fixation of the anterior root, the AIML suture is fixed with a 4.75-mm SwiveLock anchor to the bare area of the proximal tibia. The fixation point is based on the length of the AIML in the allograft.