Abstract
Recently a visually pleasing smile has become a major concern for the patients; therefore, dental bleaching has gained importance due to its safety and great aesthetic results. The aim of this paper is to report a case of a non-vital, discolored, maxillary central incisor bleached by Sodium Perborate with the use of glass ionomer cement as a mechanical barrier. The patient was a 35-year-old female complaining of a discolored and unaesthetic appearance of her upper front tooth. After endodontic retreatment, the bleaching treatment was applied to the maxillary left central incisor. Following the treatment, a satisfactory aesthetic result was achieved.
Keywords: bleaching, discoloration, walking bleaching method, non-vital bleaching, endo bleach, mechanical barrier
Introduction
Aesthetic dentistry has evolved, gained popularity and became one of the highly important factors in the dentistry field. Recently a visually pleasing smile has become a major concern for the patients, and a noticeable improvement in the perception of beauty concept was observed in the media [1].
There are several important dental aesthetic concerns such as, tooth discoloration, hypo-calcification and surface irregularities [2].
The etiology, appearance, localization and severity of discolored teeth vary, and the discoloration is classified as intrinsic, extrinsic, or both according to its location and etiology [3].
Extrinsic discoloration is caused by the habitual intake of chromogenic dietary sources such as, wine, coffee, tea, carrots, oranges, chocolate, tobacco, mouth rinses, or plaque on the tooth surface [4].
As for intrinsic discoloration, it can either be caused by systemic or local factors. Systemic causes include drug-related (tetracycline), metabolic, fluorosis, and genetic (hyperbilirubinemia, amelogenesis imperfecta, and dentinogenesis imperfecta) [5].
Local causes include pulp necrosis, intrapulpal hemorrhage, pulp tissue remnants after endodontic therapy, endodontic materials, coronal filling materials, root resorption, and aging [5].
Bleaching of discolored teeth, either vital or non-vital, has become one of the highly popular approaches to resolve this problem. Therefore, it is considered as one of the least invasive economical procedure for discoloration treatment [6,7,8].
Multiple dental bleaching materials have been used for example, oxalic acid, calcium hypochlorite, hydrogen peroxide, carbamide peroxide, and sodium perborate [8].
30%-35% hydrogen peroxide and sodium perborate either in combination or separately are the most commonly used agents for non-vital bleaching of endodontically treated teeth, in which oxidation reaction and degradation of pigment molecules are resulted [9,10].
Case Report
A 35 years old female patient, who complained of discolored and unaesthetic appearance of her upper front tooth without any pain or symptoms, attended to the dental clinic in King Saud bin Abdulaziz university for health sciences in Riyadh, Saudi Arabia on 26.12.2018.
The patient was free from systemic disorders and was not under any medications that cause staining of the teeth.
A written informed consent form was obtained from the patient prior to any examination or treatment.
In addition, a second written consent was taken for the case documentation and presentation.
Then, clinical and radiographic examinations were carried out.
Upon examination of #21, defective palatal amalgam with recurrent caries was found.
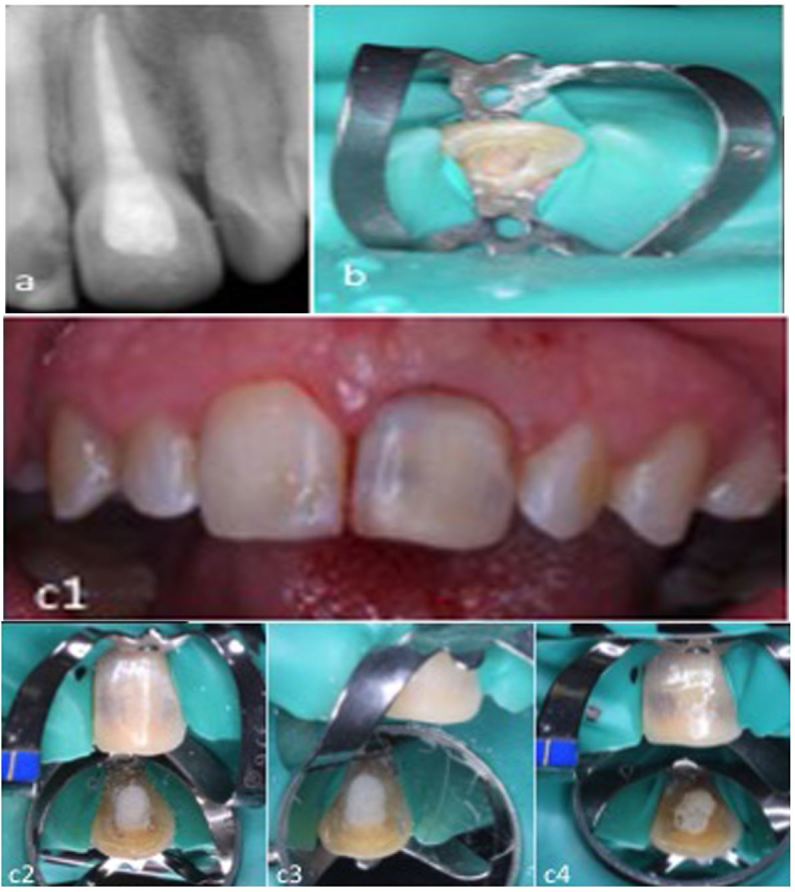
The pulpal diagnosis was previously treated with asymptomatic apical periodontitis, based on the supplementary endodontic tests (Fig.1).
Figure 1.
Pre bleaching, a. extra oral, b. intra oral photographs, c. periapical radiograph
The shade guide of the discolored tooth was assessed under normal daylight with a Vita porcelain shade guide (Vita Zahnfabrik, Bad Sackingen, Germany).
Also, pre-and post-bleaching photographs were taken for the patient.
A conventional endodontic treatment was done for the patient.
The bleaching process was undertaken using Sodium perborate powder.
The gingiva was protected by water-soluble cream (Vaseline) applied to soft tissues, and rubber dam isolation was achieved. 2mm of the gutta-percha was removed in an apical direction beyond the cemento-enamel junction (CEJ).
The tooth was rinsed and dried; then, 1mm of glass ionomer cement (GIC) base was placed over the gutta percha to form a barrier between the sealed root canal and the bleaching material (mechanical seal).
Sodium perborate powder was mixed with saline and then placed into the opened pulp chamber over the dentinal walls, cotton pellet was placed and a calcium sulphate based temporary filling material (Cavit™ Temporary Filling Material, 3M, United States) for temporization.
Sequence of the Treatment
During the first visit, the palatal amalgam was removed and recurrent caries was excavated.
The access cavity was refined; then, removal of the obturating material, gutta percha, was done using Chloroform.
Hand files were used for cleaning and shaping, calcium hydroxide application and then the access was closed with cotton pellet, Cavit and GIC.
Second visit, after 1 week, calcium hydroxide was removed; obturation with gutta percha was done.
The cavity was closed with Cavit and GIC (Fig.2a).
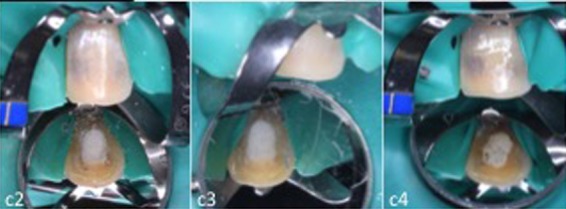
Figure 2.
a. Periapical radiograph after retreatment#21, b.GIC barrier at the CEJ, c1. #21 after one week of Sodium perborate application, c2.Re-application of Sodium perborate, c3. Placement of cotton pallet above the bleaching material, c4. Placement of Cavit
Third visit, after 3 weeks, no signs or symptoms were present.
GIC and Cavit were removed; gutta percha was reduced 2mm below CEJ. 1mm layer of GIC was placed as a barrier (Fig.2b).
Sodium perborate was mixed with saline and placed over the dentinal walls, cotton pellet and Cavit for temporization.
Fourth visit, after one week, an obvious color change was noticeable with light spots facially. Cavit and Sodium perborate were removed.
Sodium perborate re-application was done and closed with cotton pellet and Cavit (Fig.2c).
Fifth visit, after one week, the color of #21 was light and matching the color of the adjacent teeth.
Cavit and Sodium perborate were removed.
The pulp chamber was rinsed, dried and obturated with calcium hydroxide for 1 week before the placement of the permanent restoration (light cure composite resin) [11,12]; then, GIC restoration was done.
Sixth visit, one week later, the pulp chamber was rinsed, dried and restored with final palatal composite restoration (Fig.3).
Figure 3.
a. Pre treatment photograph, b. Post bleaching with calcium hydroxide pulp chamber obturation, c. Final result after permanent palatal composite resin restoration
Clinical evaluation was recorded by comparing the tooth shade with its original one before treatment using Vita porcelain shade guide (Vita Zahnfabrik, Bad Sackingen, Germany) and photographs.
Discussion
Restoring the dental aesthetics has been considered one of the chief purposes of modern dental medicine. Novel materials and treatment methods are being developed every day to reach this goal [13].
Dental bleaching is a conservative treatment compared to other treatment methods used for treating discoloration; such as, laminate veneers and full crowns. The bleaching mechanism works on the principle that hydrogen peroxide penetrates the tooth and generates free radicals that oxidize the organic stains [14].
Dental bleaching is reported to be a harmless procedure, with respect to some protection aspects. First, complete soft tissue isolation for the gum, lips, tongue and cheeks is mandatory in order to protect them from eventual burns caused by the peroxide [6].
Second, the risk of cervical resorption has to be considered; thus, a base of 1-2mm glass ionomer cement has to be placed over the root filling material to assure a mechanical barrier between the sealed root canal and the bleaching material, which is in agreement with other studies [15,16].
Moreover, reaching the desired shade guide can be assured by obturating the pulp chamber with calcium hydroxide for seven days before the final filling material. This is necessary to allow for residual oxygen elimination, which interferes with the polymerization of the filling material and to neutralize and render the medium alkaline that reduces the risk of cervical resorption [17].
The result could vary depending on the type of the material that was used and the number of visits it took. According to Amato et al and Feiglin et al, they used a mixture of sodium perborate and hydrogen peroxide along with heat to potentiate the bleaching effect in comparison to our study which only sodium perborate was utilized [16,18].
This can be explained to the drawback effect of having high concentration of bleaching material combined with heat which result in cervical root resorption (internal resorption) in multiple of cases that were reported [17,19,20].
Moreover, in all of the reported studies the number of visits varies depending on the case, the intensity of discoloration, and the satisfaction of the clinician and patient. However, in all of the documented studies, it never extended to more than four visits due to the fear of having internal (cervical root) resorption.
Nowadays, restorative treatment has achieved high aesthetic standards. Among minimally invasive treatments, dental bleaching has gained importance due to its safety and great aesthetic results. Several studies in the literature reported that the office-type whitening was successful [21].
References
- 1.Bahadır HS, Karadağ G, Bayraktar Y. Minimally Invasive Approach for Improving Anterior Dental Aesthetics: Case Report with 1-Year Follow-Up. Case Reports in Dentistry. 2018;2018:1–5. doi: 10.1155/2018/4601795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Muñoz MA, Arana-Gordillo LA, Gomes GM, Gomes OM, Bombarda NH, Reis A, Loguercio AD. Alternative esthetic management of fluorosis and hypoplasia stains: blending effect obtained with resin infiltration techniques. Journal of Esthetic and Restorative Dentistry. 2013;25(1):32–39. doi: 10.1111/j.1708-8240.2012.00527.x. [DOI] [PubMed] [Google Scholar]
- 3.Alqahtani MQ. Tooth-bleaching procedures and their controversial effects: a literature review. The Saudi Dental Journal. 2014;26(2):33–46. doi: 10.1016/j.sdentj.2014.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Watts A, Addy M. Tooth discoloration and staining: a review of the literature. British Dental Journal. 2001;190(6):309–316. doi: 10.1038/sj.bdj.4800959. [DOI] [PubMed] [Google Scholar]
- 5.Nathoo SA. The chemistry and mechanism of extrinsic and intrinsic discoloration. Journal of the American Dental Association. 1997;128:6S–10S. doi: 10.14219/jada.archive.1997.0428. [DOI] [PubMed] [Google Scholar]
- 6.Abdelkader NN. Modified Technique for Nonvital Tooth Bleaching: A Case Report. Electronic physician. 2015;7(6):1423–1426. doi: 10.14661/1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.MacIsaac AM, Hoen CM. Intracoronal bleaching: Concerns and considerations. Journal Canadian Dental Association. 1994;60(1):57–64. [PubMed] [Google Scholar]
- 8. Rostein I . Tooth discoloration and bleaching. In: Ingle JI, Bakland LK, editors. Endodontics . 5 . Hamilton, Ontario, Canada : BC Decker Inc ; 2002 . pp. 845– 860. [Google Scholar]
- 9.Attin T, Paque F, Ajam F, Lennon AM. Review of the current status of tooth whitening with the walking bleach technique. International endodontic journal. 2003;36(5):313–329. doi: 10.1046/j.1365-2591.2003.00667.x. [DOI] [PubMed] [Google Scholar]
- 10.Moraru I, Tuculină M, Bătăiosu M, Gheorghiţă L, Diaconu O. Whitening non vital teeth-a case report. Current health sciences journal. 2012;38(3):132–135. [PMC free article] [PubMed] [Google Scholar]
- 11.Rotstein I, Zyskind D, Lewinstein I, Bamberger N. Effect of different protective base materials on hydrogen peroxide leakage during intracoronal bleaching in vitro. Journal of endodontics. 1992;18(3):114–117. doi: 10.1016/S0099-2399(06)81310-5. [DOI] [PubMed] [Google Scholar]
- 12.Steiner DR, West JD. A method to determine the location and shape of an intracoronal bleach barrier. Journal of endodontics. 1994;20(6):304–306. doi: 10.1016/s0099-2399(06)80822-8. [DOI] [PubMed] [Google Scholar]
- 13.Korkut B, Yanıkoğlu F, Günday M. Direct composite laminate veneers: three case reports. Journal of dental research dental clinics dental prospects. 2013;7(2):105–111. doi: 10.5681/joddd.2013.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Polydorou O, Wirsching M, Wokewitz M, Hahn P. Three-month evaluation of vital tooth bleaching using light units-a randomized clinical study. Operative Dentistry. 2013;38(1):21–32. doi: 10.2341/12-041-C. [DOI] [PubMed] [Google Scholar]
- 15.Amengual Lorenzo, Cabanes Gumbau, Cervera Sánchez, Forner Navarro, Llena Puy. Clinical study of a halogen light-activated bleaching agent in non-vital teeth: Case report. Quintessence international. 1996;27(6):383–388. [PubMed] [Google Scholar]
- 16.Amato M, Scaravilli MS, Farella M, Riccitiello F. Bleaching teeth treated endodontically:long-term evaluation of a case series. Journal of endodontics. 2006;32(4):376–378. doi: 10.1016/j.joen.2005.08.018. [DOI] [PubMed] [Google Scholar]
- 17.Titley KC, Tomeck CD, Ruse ND, Knnec D. Adhesion of a composite resin to bleached and unbleached human enamel. Journal of endodontics. 1993;19(3):112–115. doi: 10.1016/S0099-2399(06)80504-2. [DOI] [PubMed] [Google Scholar]
- 18.Feiglin B. A 6-year recall study of clinically chemically bleached teeth. Oral Surgery Oral Medicine Oral Pathology. 1987;63(5):610–613. doi: 10.1016/0030-4220(87)90238-6. [DOI] [PubMed] [Google Scholar]
- 19.Parry R. Bleaching and root resorption. Australian Endodontic Newsletter. 2010;10(2):18–19. [Google Scholar]
- 20.Gheorghiu I, Mitran L, Mitran M, Stoian I. Cervical root resorption. ARS Medica Tomitana. 2013;19(2):99–102. [Google Scholar]
- 21.Al Shethri, Matis BA, Cochran MA, Zekonis R, Stropes M. A clinical evaluation of two in-office bleaching products. Operative Dentistry. 2003;28(5):488–495. [PubMed] [Google Scholar]



