Abstract
We describe a 66-year old patient with a recurrent ulcer on her right ankle. Biopsy revealed medium-vessel vasculitis consistent with cutaneous polyarteritis nodosa. There were no signs or symptoms suggestive of systemic vasculitis, but a 18FDG-PET scan showed areas of increased uptake around the large arteries and the pelvic and shoulder girdles. These findings suggested polymyalgia rheumatica in the setting of large-vessel vasculitis. This case thus supports the statement from the Chapel-Hill consensus conference that classification of systemic vasculitis by vessel size is based on the vessels predominantly involved, but vessels of other sizes may also be affected.
LEARNING POINTS
The classification of vasculitis needs further refinement as some patients may not easily fit into just one category.
Conditions that include aspects of different vasculitis also exist and cannot be classified using the Chapel Hill nomenclature.
The role of PET scan in the assessment of PAN needs further evaluation.
Keywords: Polyarteritis nodosa, polymyalgia rheumatica, giant cell arteritis (GCA), PET scan
CASE DESCRIPTION
A 66-year old patient presented to her dermatologist in May 2018 with a recurrent ulcer on the right ankle (Fig. 1). In September 2016, the patient had first noticed swelling of the right ankle; a few months later a purplish colouration had appeared and, in October 2017, the lesion began to ulcerate and become painful. The patient complained of pain over the right malleolus and also slight dyspnoea. Clinical examination showed no abnormality other than the ulcer.
Figure 1.
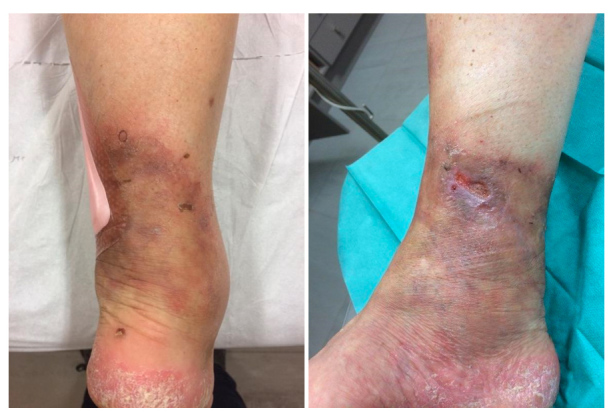
The patient’s right ankle, showing the recurrent ulcer.
The patient’s past medical history consisted of psoriasis of the feet and hands, arterial hypertension, gastro-oesophageal reflux and pneumonia. She had had four pregnancies and no miscarriages. She had been taking oral methotrexate (MTX) at a dose of 12.5 mg/week for the psoriasis, but it had been discontinued in 2017 because of impaired liver function tests. Her psoriasis was currently in remission. Current medication included nebivolol 5 mg/day and pantoprazole 20 mg/day.
Laboratory tests showed that inflammatory and coagulation parameters, blood cell count, creatinine and liver enzymes were within normal ranges, except for an unexplained slightly raised lactate dehydrogenase (LDH). Autoimmune and viral serologies were all negative, including antineutrophil cytoplasmic antibodies (ANCA).
A cutaneous biopsy of the ulcer on the right ankle showed that the deep dermal vessels were surrounded by a dense infiltrate consisting of mononuclear cells mixed with many neutrophils and eosinophils. The vessel walls showed the presence of fibrinoid necrosis. The dermis had a sclerotic appearance with thick collagen bundles. The more superficial vessels had slightly thickened walls. A diagnosis of polyarteritis nodosa (PAN) was made.
Following this diagnosis, a complementary work-up was performed to exclude systemic involvement. Angio-magnetic resonance imaging of the mesenteric and renal vessels was normal. A 18fluorodeoxyglucose-positron emission tomography (18FDG-PET) scan revealed symmetrical increased uptake of large vessels, including the axillary, humeral, iliac, femoral and tibial arteries, but not the aorta (Fig. 2).
Figure 2.

The patient’s 18fluorodeoxyglucose-positron emission tomography (18FDG-PET) scan
The scan also revealed capsulitis and synovitis of the shoulders and hips and bilateral trochanteric bursitis. There was also increased uptake around the right ankle, corresponding to the ulcerated lesion.
A final diagnosis of cutaneous PAN associated with PET scan features of polymyalgia rheumatica (PMR) and large-vessel vasculitis, namely giant-cell arteritis (GCA), but without overt clinical manifestations of PMR or GCA, was made. Low-dose MTX (10 mg/week) was initiated but, because the leg ulcer did not heal, methylprednisolone was added at an initial dose of 32 mg/day, tapering by 8 mg each week so that steroids were withdrawn after one month; this regimen resulted in healing of the ulcer.
When the patient first attended our internal medicine department, we increased the weekly dose of MTX to 17.5 mg, given with folic acid. A second PET scan performed 6 months later showed a clear decrease in uptake of the large arteries but no change around the shoulder and pelvic girdles.
At the patient’s most recent visit in July 2019, she was in clinical remission and tolerating a dose of 15 mg/week MTX.
DISCUSSION
Classical PAN is a systemic necrotizing vasculitis that typically affects medium-sized muscular arteries but which can also involve small muscular arteries. In the definition from the Chapel Hill consensus conference on nomenclature of vasculitis, PAN is also characterized by the absence of glomerulonephritis or involvement of arterioles, capillaries, or venules[1].
A few cases of PAN restricted to the lower legs, thus corresponding to cutaneous PAN, have been reported. Cutaneous PAN can be differentiated from classical PAN by the predominant skin involvement and lack of progression to visceral involvement. Characteristic manifestations of cutaneous PAN include subcutaneous nodules, livedo reticularis and ulceration, mostly localised on the lower extremity. The ulcerative form of disease has a more prolonged course and is frequently associated with peripheral neuropathy, resulting from inflammation of the vasa nervorum. In addition to the skin and peripheral nerves, muscles can be affected in cutaneous PAN, in particular the gastrocnemius muscle. The most common features are calf pain, swelling around the lesions and fever; the muscles were not involved in our patient. Cutaneous PAN is also distinguished from classical PAN by the infrequent occurrence of chronic disease and a better prognosis.
The originality of our case lies in the finding of ‘occult’ areas of increased uptake, indicating increased metabolic activity, on the 18FDG-PET scan, the term occult referring to clinically unsuspected lesions. This concept of occult areas of increased metabolism is consistent with findings reported in ANCA-associated vasculitis (AAV). In a retrospective review of 18FDG-PET scans performed in patients with active AAV, we reported that areas of increased metabolism were seen in clinically unsuspected and difficult to assess sites[2]. Our results confirmed those observed in a French multicenter cohort[3]. Unexpected increased metabolism of large-size arteries, as in our patient, is important because increased aortic uptake was observed in 8 of the 33 patients in our series and in 2 of the 14 patients in the French series. In all the cases in our series, this finding was associated with no obvious clinical impact. Notably, in one case, the presence of a subclavian murmur suggested a possible overlap of granulomatosis with polyangiitis (GPA) and Takayasu arteritis. None of the patients in these two series displayed the increased metabolism of the shoulder or pelvic girdles (either capsulitis or bursitis) that is evocative of PMR.
Unexpected arterial uptake of 18FDG has only exceptionally been reported in association with PAN. Puigrenier et al. reported on a patient with biopsy-proven PAN considered clinically as being limited to the right leg with involvement of muscles and the popliteal nerve[4]. Similar to our patient, the 18FDG-PET scan showed clinically unsuspected increased uptake around the humeral, femoral and popliteal arteries. Again, the aorta was not involved, in contrast to what is observed in AAV and GCA, where the aorta is the most frequently involved large vessel. Schollhammer et al. also reported popliteal vasculitis in a patient with PAN[5].
In addition to the difficulty classifying such patients, the main issue raised by the PET scan in our case was whether the presence of increased uptake around the large arteries should lead to treatment of the patient as recommended for systemic large and medium vasculitis or for cutaneous PAN? As the patient had already improved under MTX when she first presented to our Department, we decided not to restart steroids, although they remain the cornerstone of treatment for GCA/large vessel vasculitis (LVV), in PMR and in systemic PAN. MTX has been shown to have a steroid-sparing effect in GCA, and is accepted as a therapeutic option in PAN, although azathioprine is considered a more classical choice.
In conclusion, we report an interesting case of medium vessel-vasculitis consistent, in terms of clinical and pathological findings, with cutaneous PAN, in which the 18FDG-PET scan revealed unexpected increased large artery metabolism. This case thus shows that PET scans can reveal findings that support the statement from the Chapel-Hill consensus conference that classification of systemic vasculitis based on vessel size refers to the vessels that are predominantly involved, but that vessels of other sizes may also be affected. Further studies addressing increased 18FDG uptake by large vessels are needed in PAN.
Footnotes
Conflicts of Interests: The Authors declare that there are no competing interest
REFERENCES
- 1.Jennette JC, Falk RJ, Bacon PA, Basu N, Cid MC, Ferrario F, et al. 2012, Revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum. 2013;65:1–11. doi: 10.1002/art.37715. [DOI] [PubMed] [Google Scholar]
- 2.Kemna M, Vandergheynst F, Vöö S, Blocklet D, Nguyen T, Timmermans SA, et al. Positron emission tomography scanning in anti-neutrophil cytoplasmic antibodies-associated vasculitis. Medicine (Baltimore) 2015;94:e747. doi: 10.1097/MD.0000000000000747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Soussan M, Abisror N, Abad S, Nunes H, Terrier B, Pop G, et al. FDG-PET/CT in patients with ANCA-associated vasculitis: case-series and literature review. Autoimmunity Rev. 2013;13:125–131. doi: 10.1016/j.autrev.2013.09.009. [DOI] [PubMed] [Google Scholar]
- 4.Puigrenier S, Dognon N, Collet G, Duez JP, Quéméneur T. Utilisation du TEP-TDM dans la périartérite noueuse limitée aux membres inférieurs : à propos d’un cas. La Revue de Médecine Interne. 2017;38(Suppl 2):A119–A120. (abstract). [Google Scholar]
- 5.Schollhammer R, Schwartz P, Jullie ML, Pham-Ledard A, Mercie P, Fernandez P, et al. 18F-FDG PET/CT imaging of popliteal vasculitis associated with polyarteritis nodosa. Clin Nucl Med. 2017;42:e385–e387. doi: 10.1097/RLU.0000000000001711. [DOI] [PubMed] [Google Scholar]


