Abstract
Background and Objective
Patient portal use has increased over the last two decades in response to consumer demand and government regulation. Despite growing adoption, few guidelines exist to direct successful implementation and governance. We describe the policies and procedures that have governed over a decade of continuous My Health at Vanderbilt (MHAV) patient portal use.
Methods
We examined MHAV usage data between May 2007 and November 2017. We classified patient portal activity into eight functional categories: Appointment, Billing, Document Access, Genetics, Health Result, Immunization, Medication, and Messaging. We describe our operating policies and measure portal uptake, patient account activity, and function use over time.
Results
By the end of the study period, there were 375 517 registered accounts. Policies made MHAV available to competent adults and adolescents 13 and over. Patients signed up for a limited access account online, which could be upgraded to a full-access account after identity verification. Patients could assign proxy accounts to family and caregivers, which permitted nonpatient access to select MHAV functions. Laboratory and radiology results were accessible via MHAV. Results were classified into three groups based on sensitivity, which govern the length of delay before results appeared in MHAV.
Discussion and Conclusion
Patient portals offer significant opportunity to engage patients in their healthcare. However, there remains a need to understand how policies can promote uptake and use. We anticipate that other institutions can apply concepts from our policies to support meaningful patient portal engagement.
Keywords: patient portals, patient engagement, consumer health informatics, policy
BACKGROUND AND SIGNIFICANCE
Patient portals are web- and mobile-based programs that allow patients and their proxies remotely to interact with healthcare systems and their care providers.1–3 These portals commonly allow users to view selected information from the electronic health record (EHR), review test results, message providers, schedule appointments, and pay medical bills.4 A report by the Institute of Medicine specifies online access to personal health records, such as patient portals, as a promising technology to support patient engagement.5 Functionality delivered through patient portals has been shown to improve chronic disease management, increase adherence to preventive care such as immunizations and screening, improve patient satisfaction, and better outcomes for some patients with chronic disease.6–14
Patient portals have been in use for nearly two decades, but adoption has increased recently in response to consumer demand and government regulations, such as the Health Information Technology for Economic and Clinical Health Act (HITECH Act).15 They have been implemented in diverse settings, including large academic medical centers, primary and specialty care practices, and community hospitals.16 Implementing and maintaining patient portals may require significant capital and resource investments17 Understanding how patients and health systems use the portal to support patient engagement and self-management is important to evolving functionality and improving patient engagement.18–20 Studies have been conducted to understand ways in which the patient portal meets the needs of patients and their caregivers.20–25
Despite widespread adoption, there are few published guidelines to support meaningful patient portal adoption and use.26 Only several studies have provided frameworks for successful implementation and maintenance.26–28 In our previous work, we published a paper detailing the policies directing the functionality of a home-grown patient portal implemented at our institution in its first 5 years of use.29 The My Health at Vanderbilt (MHAV) patient portal was one of the earliest implemented and has been in continuous since 2003.30,31 In this manuscript, we provide an update on MHAV usage patterns and present its current policies.
METHODS
Study site
Vanderbilt University Medical Center (VUMC) is a private, nonprofit, and academic healthcare center located in Middle Tennessee. VUMC includes the 758-bed Vanderbilt University Hospital (VUH) and the 267-bed Monroe Carrell Jr. Children’s Hospital at Vanderbilt (MCJCHV). VUH receives over 70 000 emergency department visits and 1.6 million ambulatory visits yearly; MCJCHV receives over 53 000 emergency department visit and 303 000 ambulatory visits yearly.
My Health at Vanderbilt
My Health at Vanderbilt (MHAV) is an institutionally developed patient portal which launched in a limited fashion in 2003 before being more widely deployed throughout all clinical specialties starting in 2007 (Figure 1). The VUMC informatics, legal and operational teams internally established policies and procedures to govern MHAV use by patients, proxies, and healthcare providers. The initial policies are described by Osborn et al.29 MHAV and its associated EHR were certified for Meaningful Use stages 1 and 2. MHAV supports core functionality similar to those of other patient portals, including secure messaging, appointment scheduling, bill management, access to select laboratory results, and access to select EHR data.29,32 There were incremental changes to usage logging and functionality throughout the duration of continuous use.
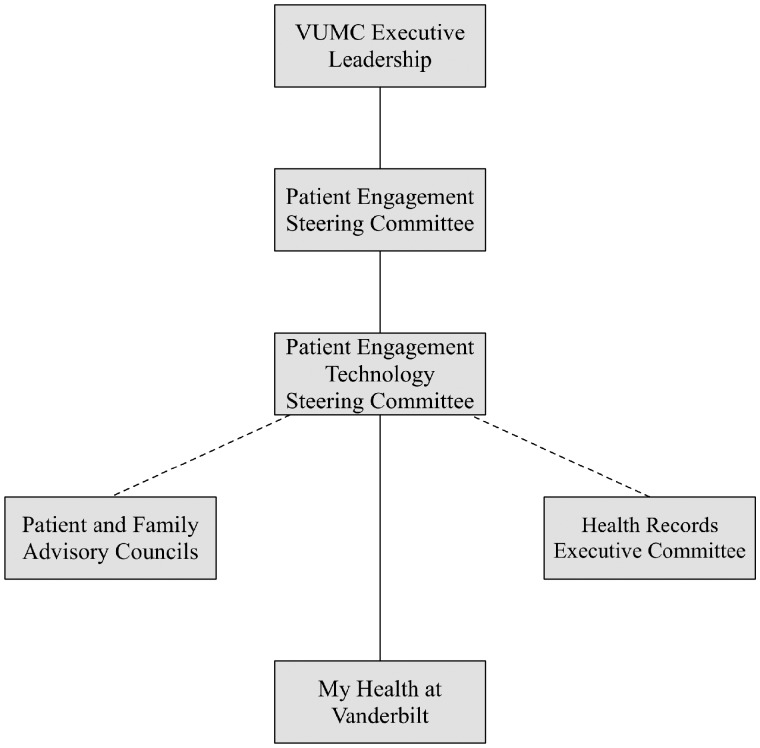
Figure 1.
MHAV governance structure.
At the time covered by this review, two policies and standard operating procedures collectively drive how MHAV user access is granted, tests are released, messages routed, and how other features are intended to be used. The policy, “MHAV Eligibility and Levels of Access” directed practice around who was eligible for MHAV use, what was required to receive access, and what access classes were available. A second policy, “MHAV Accessing Radiology and Lab Results” directed practice around test result availability in MHAV. These policies are described in detail, below.
Data sources and analysis
We examined MHAV usage event logs from May 5, 2007 to November 2, 2017. This study period allows us to evaluate usage patterns from early implementation up to the transition to a commercially developed patient portal and EHR system. We collected data on all MHAV usage events, including user name, user role (self or proxy), event timestamp, event type, and unique patient identifier. We similarly extracted demographic characteristics from the EHR for each MHAV user.
We assigned all usage events to eight categories (Box 1). Summary statistics were calculated to evaluate account activity and portal usage. Account activity was determined as any instance of portal use. We define portal usage as any successful login or use of any MHAV function. We focused our analysis on the four functions that have been in use since the initial portal release: account management, view selected health results, create or view upcoming appointments, and secure messaging. We assessed patient portal use by session. We define a session as any sequence of patient portal events by a single user for a single patient that occurred within 30 minutes of previous use without any login or logout events. We calculated the duration of each session as the time between a user’s first and last patient portal event within the respective session. We similarly calculated the duration of patient portal use, in months, as the time between a user’s first and last session. All analyses were conducted in R version 3.2.2.33 The Vanderbilt University institutional review board approved this study.
Box 1. My Health at Vanderbilt Function Groups. Function groups marked with an asterisk (*) were available to limited access accounts
| Appointment* |
| Modify scheduled appointment |
| Schedule appointment |
| View summary of past appointments |
| View summary of upcoming appointments |
| Billing |
| Enter payment information |
| View bills |
| View insurance information |
| Document Access |
| Download document |
| Transmit document |
| View document |
| Genetics |
| View genetic information |
| Health Result |
| View labs |
| View past reports |
| View vitals |
| Immunization |
| View immunizations |
| Medication |
| View medications |
| Messaging* |
| Delete message |
| Forward message |
| Reply to message |
| Send message |
| View message |
RESULTS
Policy on patient access and registration
During the period covered by this review, My Health at Vanderbilt was made available to all competent adults age 18 and older, regardless of whether they had an established relationship with a Vanderbilt site (ie, whether they had a medical record number). With permission from a parent or guardian and enrollment as a surrogate user, adolescent patients age 13 and older were eligible for a MHAV account. The full set of eligibility criteria are listed in Table 1. MHAV policy allowed two access levels: limited access and full access. Users could create limited access accounts by logging into MHAV from anywhere with an internet connection, and providing a user name, password, and basic identifying information. Once created, a limited access account gave users access to the basic portal features, including access to medical center information, generic educational materials, and secure messaging and request appointments. Limited access users could not see their own protected health information. Limited access users were also able to serve as proxies for other users and use portal functions on their behalf.
Table 1.
MHAV eligibility criteria
| Individuals eligible to enroll in MHAV | |
|---|---|
| 1) | Adult individuals (aged 18 years or older) requesting access to an account for themselves |
| 2) | Adult individuals requesting access to an account for a minor child (under the age of 13 years) for whom they are the parent or guardian |
| 3) | Adult individuals who are the parent or Guardian of a minor child aged 13–17 years together with the minor child aged 13–17 years who mutually agree and request joint access; to the minor child's aged 13–17 years MHAV account |
| 4) | Adult individuals who are the parent or Guardian of a minor child age 13–17 years whose teen has a medical condition, determined by the teen's provider, that prevents the teen from participating in making MHAV access decisions |
| 5) | Adult individuals who are requesting access to an account for an individual for whom they are the Conservator |
| 6) | Adult individuals with Full Access to their own MHAV account may grant another adult individual Delegate Access to their MHAV account. |
| 7) | Emancipated minors are required to present legal documentation of the emancipation to be reviewed by the Office of Legal Affairs before granting access as an adult individual. |
| Eligibility limitations | |
| a) | Minors (under the age of 18 years) are not eligible for self-enrollment |
| b) | Individuals who are incapable or lack the capacity to give consent for access are not eligible for an account |
| c) | Participation in MHAV may be withheld, denied, or terminated, and a MHAV account may be deactivated, with respect to any patient's information at any time at the sole discretion of VUMC |
| d) | Upon notification that a MHAV user is deceased, the MHAV account is suspended automatically. |
To access the entire suite of MHAV functions and personal protected health information, policy required users to upgrade to a full access account. Upgrading to full access required that a medical center employee verify the user's identity via a government-issued identification, such as a driver's license or passport. Verification took place in person during clinic visits, or through video conferencing with MHAV support staff team members. With verification, MHAV accounts get linked to the institutional EHR and the user’s electronic medical records. As a result, full access users could log into MHAV to view protected health information from their medical record, targeted educational materials and lab interpretations, and past and upcoming appointments. Full access users could also pay bills and self-manage proxy accounts.
Proxy and nonpatient access
The access policy also allowed a number of proxy access classes to account for diverse ways that family members or other caregivers support individuals receiving health care. Proxy access is defined as an access class in which one individual receives access to another individual’s protected health information, communication tools, and functions in MHAV. In all cases, the proxy had to meet the eligibility criteria outlined in the table, even if the patient did not. Individuals could serve as proxies for competent adult patients, patients who were children or adolescents, and adult patients who met legal criteria for lacking the capacity to make medical decisions. VUMC policy distinguished two general categories of proxies: delegates and surrogates. The policy defined delegates as “an adult individual invited by a MHAV account holder to have access to that account holder’s MHAV account,” and stipulated that the account holder be a competent adult. For example, a competent adult may invite her spouse, adult friend, and adult child aged 18 or older to have delegate access to her account.
Surrogate accounts were proxy accounts held by competent adults that give access to MHAV as a stand in for individuals who did not meet eligibility criteria for having their own independent account. This included children, adolescents, and adults lacking the capacity for medical decision making. For children age 0–12, a parent or guardian could serve as a surrogate proxy and have full access to the child's account unless prohibited by a formal legal ruling provided by a judge (such as what might occur in the case of domestic abuse). For children age 13–17, a parent or guardian could have surrogate access to the child's account only if both the parent and teenager mutually agree to establish a MHAV account for the teenager with the parent or guardian serving as a proxy. In the case of a teenage account, certain clinical information was unavailable in MHAV to respect state laws around the teenager's privacy, such as health records containing information about sexually transmitted infections, pregnancy or testing for drug use. Last, surrogate proxy accounts were available to those supporting the healthcare of adults who lack the capacity to make medical decisions, such as for the adult children of an individual who has developed advanced dementia, or for the parents of an adult with severe autism. All categories of surrogate access had set expiration dates and had to be reviewed and renewed periodically, including when a child turned 13 and when a teenager turned 18. These expiration dates forced patients and their proxies periodically to reconsider whether they wanted the proxy access to continue, especially as patients moved from one access category to another.
Tethered electronic health record data
A key patient portal function is to share health data contained in a tethered electronic medical record system with patients and their proxies. During the study period, a subset of all health records were made available to MHAV users. The “MHAV Accessing Radiology and Lab Results” policy defined the content of and timing for which patients or their proxies could access laboratory testing and radiology results via MHAV. The policy stated that, “laboratory and radiology information is organized functionally into three groups, defined by their information sensitivity. Table 2 presents the evolution health result access permissions by classification groups for adult and pediatric patients. Groups were classified as Group A, Group B, and Group C. These groupings determined whether and when patients would have access to various lab and radiology results through the MHAV web portal.” Group A tests were those with results deemed to have high value for immediate patient viewing with low risk of untoward reaction to the information, and were made available to MHAV immediately upon appearing in the EHR. Examples included cholesterol testing, hemoglobin A1C, and serum pregnancy testing in adults. Group B tests comprised the bulk of laboratory and radiology testing. They were made available through MHAV after a delay of 3 business days from the time test results appeared in the EHR to permit time for the healthcare team to review the results prior to release. Examples included chest radiographs, serum amylase testing, and sweat chloride testing. Group C tests were those that generally warrant healthcare provider review to confirm the validity of the result or report and communicate context and education to the patient. These results were made available through MHAV after a delay of 7 business days from the time they appear in the EHR. Examples included tumor markers, human immunodeficiency virus (HIV) polymerase chain reaction (PCR) and genetic testing.
Table 2.
Evolution of health result release policies
| Policy date | Category A | Category B | Category C adult | Category C peds | Radiology |
|---|---|---|---|---|---|
| 2/2006 | Immediate | 7 calendar days | Never | Never | 14 days |
| 6/2011 | Immediate | 3 business days | Never | Never | 3 business days |
| 4/2015 | Immediate | 3 business days | 7 business days | Never | 3 business days |
A results committee assigned each individual laboratory test and radiology test in the EHR to one of these three groups, and for each patient access age category (ie, age 0–12, 13–17, and 18+). Assignments strived to balance timeliness of the results' availability for patients with appropriate safeguards to ensure accurate information, high quality patient care and results counseling. Further, the policy noted that, “result availability in MHAV is not intended to replace provider notification of laboratory results, but rather to support patient access and participation in their care, and to improve quality of care.” Result group assignments respected age categories such that a given laboratory or radiology result may be assigned to different release groups for different patient ages. Further, for patients under age 18, group C results did not ever display in MHAV given added complexity of the data sensitivity, patient privacy, and laws around adolescent medical independence for certain conditions. Examples of tests categorized as group C for those under age 18 included urine or serum pregnancy testing, abdominal ultrasounds, and urine chlamydia PCR.
Governance
My Health at Vanderbilt was managed by a robust institutional governance that connected oversight with executive leadership and key stakeholders. A physician faculty member served as the application's director, responsible for overall direction setting, policy recommendations, and community outreach. A co-director managed the day to day operation, software development prioritization, and resourcing. The software development team was further managed by a dedicated analyst, and was made up of a team of software developers. Working alongside the MHAV software development team, a team from Vanderbilt's Strategic Marketing group guided user experience interface design. The user interface team provided relevant software code, style sheets, and graphics to ensure that MHAV's user experience aligned with that of other medical center websites.
Figure 1 visualizes the MHAV governance structure. The MHAV team—through its Directors—reported to a medical center Patient Engagement Technology Steering Committee. This steering committee was charged “to bring strategic oversight and operational direction to all existing and newly developed patient engagement technologies such as patient facing online tools, applications, and interactive programs aimed at engaging VUMC patients either about their health and wellness, clinical care, research opportunities, health education, and overall experience with VUMC services.” The committee also recommended changes to policy, resourcing, and strategy around all institutional patient engaging technologies. The committee is chaired by the medical center's Chief Medical Officer and Chief Patient Experience & Service Officer. Membership included representation from the offices of Legal Affairs, Compliance, and Privacy; operational leadership representing the Adult and Pediatric hospitals; leaders from Strategic Marketing, the Health Information Technology department, and the Office of Patient Engagement; representation of the research enterprise; and, the MHAV Directors. The Patient Engagement Technology Steering Committee reported directly upward to the Medical Center's executive leadership through an intermediary Patient Engagement Steering Committee, and had an advisory reporting to the Health Records Executive Committee. The Health Records Executive Committee produced and revised any policy governing the use of MHAV, such as those presented in this manuscript. The Patient Engagement Technology Steering Committee also had a bidirectional advisorial relationship with the medical center's Patient and Family Advisory Councils (PFAC). The PFACs partner with health care team members, medical center leadership, and medical center initiatives to ensure that the patient voice is represented. There exist PFACs representing patients and families from the adult general medical and surgical practices, from pediatric practices, and from behavioral health.
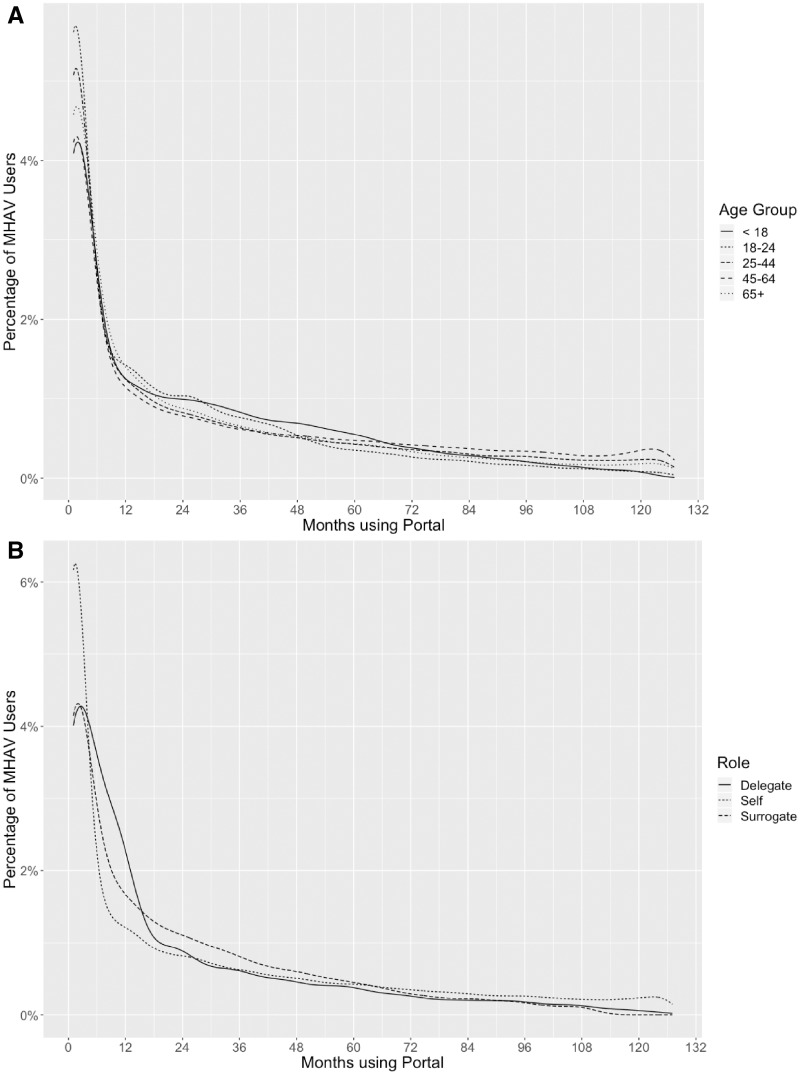
MHAV usage
As of November 2, 2017, MHAV had accumulated 375 517 registered accounts that were associated with 402 744 patients. This represented 20.4% of all unique VUMC patients seen over the entire studied period, and 40.5% of VUMC patients seen in 2017. There was a 625% growth in active accounts between 2007 and 2017. Among users, 61% are female and 77.7% are Caucasian. Table 3 provides demographic data for MHAV users. The average user was 41.1 years of age at registration. There were 172 425 patients aged 25–44 and 59 519 patients aged 18–25 during portal use, the most and least among all age groups, respectively. Each user accessed MHAV in a median of 12 sessions over 8 unique days. Among all patients, 7636 (2.0%) users assigned a delegate access to their account. There were 24 008 (6.4%) patients who assigned a surrogate access to their account. Figure 2 shows length of time using MHAV by age and account type. Most patients (51.3%) used MHAV for at least 1 year. The duration of use for 40% of patients was at least 2 years and for 18.8% of patients at least 5 years.
Table 3.
My Health at Vanderbilt patient demographics
| Male | Female | Total | |
|---|---|---|---|
| (n = 156 631) | (n = 245 815) | (N = 402 744) | |
| Age at registration | |||
| Mean (range) | 42.7 (0–96) | 40.3 (0–97) | 41.1 (0–97) |
| Median | 44 | 38 | 40 |
| Race | |||
| African–American | 11 439 (6.5%) | 23 424 (8.6%) | 34 866 (7.7%) |
| American Indian | 336 (0.2%) | 445 (0.2%) | 781 (0.2%) |
| Asian | 4552 (2.6%) | 6541 (2.4%) | 11 095 (2.5%) |
| Caucasian | 139 677 (79.0%) | 210 274 (77.1%) | 349 960 (77.7%) |
| Pacific Islander | 147 (0.1%) | 209 (0.1%) | 356 (0.1%) |
| Other | 5007 (2.8%) | 8372 (3.1%) | 13 532 (3.0%) |
| Unknown | 15 585 (8.8%) | 23 634 (8.7%) | 39 570 (8.8%) |
| Days using portal | |||
| Mean (range) | 36.7 (1–2391) | 37.8 (1–1967) | 37.4 (1–2391) |
| Median | 7 | 9 | 8 |
Figure 2.
Length of time using MHAV by (A) age and (B).
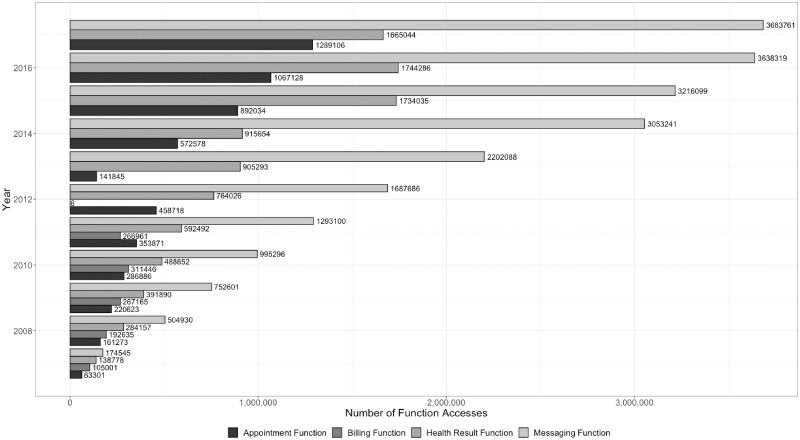
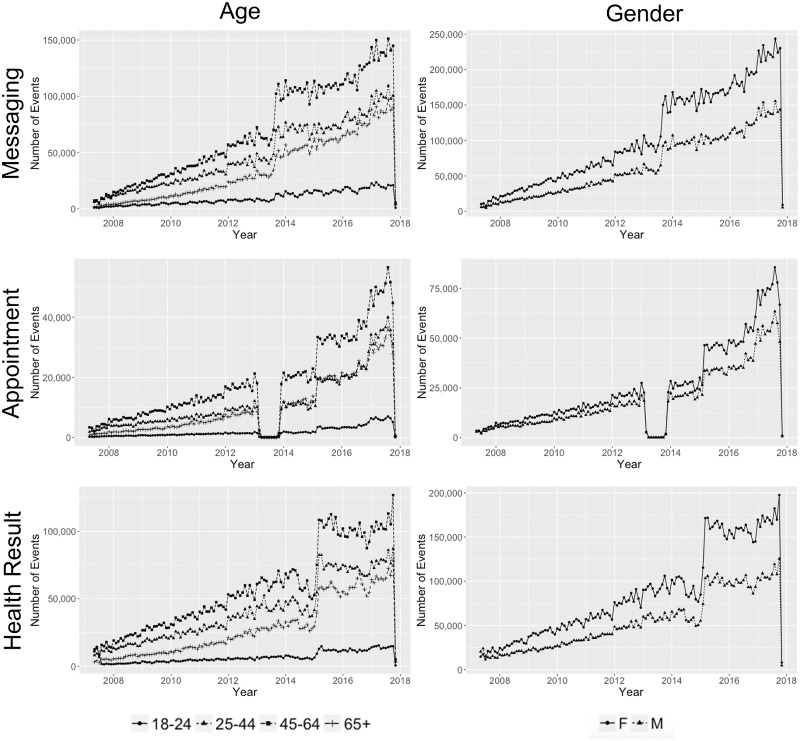
Users initiated 25 096 144 MHAV sessions, with a median of 2 415 478 sessions per year, over our studied period. Patients initiated 96% of these sessions; surrogates and delegates initiated 3.2% and 0.8% of the sessions, respectively. On average, users accessed three portal functions per session, regardless of role or age. The number of function accesses increased yearly an average of 33.8%. Figure 3 presents MHAV function use by year. Secure messaging was the most commonly used MHAV function (Table 4). Seventy-one percent of users had sent or received a secure message through MHAV. Messaging functions were accessed in over half (51%) of the sessions. Health result and appointment-related functions were the second and third most popular functions, respectively accessed by 60.5% and 54% of users. Users accessed health result functions in 24% of sessions while 17% of sessions contained an appointment function. Health result and messaging access increased yearly. We show MHAV function usage by age and gender in Figure 4. Female patients and patients between 45 and 64 years of age accessed the most messaging, appointment, and health result functions each year. All three functions received the least use from patients between 18 and 24 years of age.
Figure 3.
MHAV function access by year.
Table 4.
MHAV function use by launch date
| Function group | Feature launch date | Feature end date | Number of users |
|---|---|---|---|
| Account Management | May 2, 2007 | November 2, 2017 | 160 350 (39.8%) |
| Health Result Function | May 2, 2007 | November 2, 2017 | 240 219 (59.6%) |
| Appointment Function | May 2, 2007 | November 2, 2017 | 214 522 (53.3%) |
| Messaging Function | May 2, 2007 | November 2, 2017 | 286 406 (71.1%) |
| Medication Function | June 12, 2013 | November 2, 2017 | 101 247 (31.8%) |
| Document Function | February 11, 2011 | November 2, 2017 | 153 339 (41.9%) |
| Immunization Function | September 11, 2008 | November 2, 2017 | 70 478 (17.9%) |
| Genetic Function | March 3, 2015 | November 2, 2017 | 87 670 (32.5%) |
| Billing Function | May 2, 2007 | June 15, 2012 | 51 182 (27.7%) |
Figure 4.
MHAV function usage by age and gender. The drop-off in appointment events in March 2013 corresponds to an interruption to scheduling as new functionality was developed.
DISCUSSION
Patients are increasingly interested in accessing their personal health data through the patient portal.4,24,34 There remains a need to understand how portal policies can enable use and promote engagement.13 Previous studies have found evidence supporting patient portal use and improved chronic disease management, improved patient satisfaction, and improved outcomes6,8,9,23,34–39 However, it is important to recognize best practices and successful frameworks that support meaningful patient portal management and use. In this work, we have described the policies that have regulated the functionality and access to our patient portal, MHAV, for both adult and pediatric patients. The policy changes were put in place to respond to the changing cultural and policy landscape. We also present statistics on patient portal use to highlight the ongoing growth of our portal and compare use of key functions by age and gender. We do not intend to imply that changes in adoption have any direct relationship with changes in policies.
Our portal access and registration policies promote use by allowing portal registration outside of the clinic. Likewise, our three-tiered account structure encourages information sharing between the patient, family, and other caregivers while maintaining patient privacy and protecting secure health information. Nonetheless, our approach to MHAV access has led to several challenges. Among these, the requirement to review an individual's identification before granting full access proved to be a barrier for patients who come to the medical center for healthcare infrequently or from long distances. This requirement also made it difficult for new patients to access full accounts before their first visit with their healthcare provider. Another challenge was that setting up an account was primarily the responsibility of the patient or surrogate, and could not be easily done as part of a clinical encounter. This opt-in model has been shown to limit enrollment in a previous study.40 While there was a way that a medical center staff member could initiate a full-access account in some cases, the primary burden remained on the patient to finalize the account (including confirming the account email and creating a user name and password). Last, creating surrogate accounts required that the surrogate provide the appropriate supporting documentation that would indicate their right of access to the patient's account.
Managing pediatric access to health-related data is inherently challenging, particularly as patients transition from childhood, through adolescence, and into adulthood. This complexity is recognized in four major changes to the eligibility and access policy since initial MHAV implementation in 2003. An initial policy change in 2006 allowed adolescent patients their own MHAV with parental permission. Three superseding policies, in 2014, 2016, and 2017, each adjusted the policy, requiring mutual accounts for both the parent and adolescent patient and further specifying eligibility criteria in response to institutionally determined best practices and governmental regulation. VUMC’s policies are designed to support a family engagement model for adolescent patients, requiring mutual agreement between the patient and parents before MHAV accounts were created.41 This model of adolescent portal access helps adolescents to transition into adulthood by allowing parental oversight, as a surrogate user, of select patient portal functions. Nonetheless, this model limits confidentiality for sensitive health results, such as those related to pregnancy.42 However, the policy requiring that both the adolescent patient and the parent or guardian agree to allow the other access for either to have access made it difficult to enroll adolescent patients. Further, state-by-state laws guiding how children’s and adolescent’s health data can be accessed and by whom inhibit widespread generalizability of approaches to pediatric proxy access to health systems across state lines.42
Our three-tier structure for sharing laboratory and radiology results allow patients to monitor their results online while ensuring providers have adequate time to review sensitive information. Tethered data from the EHR in the patient portal is an important component for users to self-manage their health. The result groups balance the value of viewing each result with the interpretation difficulty, such that providers have sufficient time to discuss each result with the patient when necessary.37 Policy governing health result release has changed twice since initial portal implementation, each time in response to federal requirements. We found that health result functions were highly utilized and usage increased yearly, despite patient privacy and security concerns as have been expressed in other studies.7,23,25,38,39,43 Further, in recent years, initiatives such as OpenNotes have gained traction to encourage sharing of clinical notes with patients. During the studied time period, VUMC did not formally move toward note sharing functionality. The institution has periodically re-evaluated opportunities to implement OpenNotes.
We found that secure messaging was the most commonly used MHAV function, with access by 71% of all users and in 51% of all usage sessions. Other studies have published similar findings, suggesting the importance of patient-provider communication in meaningful patient portal use.18,39,44 Early works on patient portal implementation and use have noted the importance of understanding the effects of patient portal use, namely secure messaging, on provider workload.26,45 However, recent studies have found that engaging patients in their care may reduce provider workload by improving patient-provider communication and reducing appointment no-shows.46,47 Similarly, communications research suggests that asynchronous modalities, such as patient-provider messaging, lead to improved productivity and fewer interruptions compared to synchronous methods of communication.48,49
In analyzing function usage trends over time, we noted abrupt changes in messaging, appointment, and health result access events, due to multiple factors. In March of 2013, there was an interruption to appointment scheduling through MHAV as new functionality was developed. There was a significant increase in 2015 of appointment events and health result events. These corresponded with the addition of new functionality to view and modify existing appointments and to view vital reporting, respectively. There was similarly an increase in August 2013 of messaging events, which was caused by a change in how accesses were recorded. Despite these incremental changes, there remained consistent yearly growth in the number of all function accesses and the number of sessions.
CONCLUSION
Well-designed patient portals, when combined with policies that promote use, offer significant opportunity for patients to engage in their healthcare. Without proper management, portals can suffer from decreased use and poor support from providers. In this work, we discuss the patient portal policies that govern account registration and management, shared access, and test result reporting at VUMC. We anticipate that other organizations can implement concepts from our policies to support the meaningful use of patient portals.
FUNDING
BS was supported by the National Library of Medicine training grant number 4T15LM007450.
CONTRIBUTORSHIP STATEMENT
BS, JW, and TR conceived the study idea and design. BS, JC, BC, GS, and TR retrieved and described relevant policy information. BS and JW conducted quantitative data analysis. All authors participated in writing and reviewed the manuscript. All authors approved the final manuscript.
COMPETING INTERESTS STATEMENT
The authors have no competing interests to declare.
REFERENCES
- 1. Archer N, Fevrier-Thomas U, Lokker C, et al. Personal health records: a scoping review. J Am Med Inform Assoc 2011; 18 (4): 515–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.HealthIT.gov: What is a Patient Portal? 2014. healthit.gov Accessed December 9, 2015.
- 3. Tang PC, Ash JS, Bates DW, et al. Personal health records: definitions, benefits, and strategies for overcoming barriers to adoption. J Am Med Assoc 2006; 13 (2): 121–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Goldzweig CL, Towfigh AA, Paige NM, et al. Systematic review: secure messaging between providers and patients, and patients’ access to their own medical record: evidence on health outcomes, satisfaction, efficiency and attitudes. Washington (DC): Department of Veterans Affairs (US) 2012; 1–63. [PubMed]
- 5.Institute of Medicine (US) Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century 2001; 1–360. [Google Scholar]
- 6. Ross SE, Moore LA, Earnest MA, et al. Providing a web-based online medical record with electronic communication capabilities to patients with congestive heart failure: randomized trial. J Med Internet Res 2004; 6 (2): e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kruse CS, Argueta DA, Lopez L, et al. Patient and provider attitudes toward the use of patient portals for the management of chronic disease: a systematic review. J Med Internet Res 2015; 17 (2): e40–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lin C-T, Wittevrongel L, Moore L, et al. An internet-based patient-provider communication system: randomized controlled trial. J Med Internet Res 2005; 7 (4): e47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Krist AH, Woolf SH, Rothemich SF, et al. Interactive preventive health record to enhance delivery of recommended care: a randomized trial. Ann Fam Med 2012; 10 (4): 312–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Green BB. Effectiveness of home blood pressure monitoring, web communication, and pharmacist care on hypertension control. JAMA 2008; 299 (24): 2857–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Tang PC, Overhage JM, Chan AS, et al. Online disease management of diabetes: engaging and motivating patients online with enhanced resources-diabetes (EMPOWER-D), a randomized controlled trial. J Am Med Inform Assoc 2013; 20 (3): 526–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sarkar U, Lyles CR, Parker MM, et al. Use of the refill function through an online patient portal is associated with improved adherence to statins in an integrated health system. Med Care 2014; 52 (3): 194–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Garrido T, Raymond B, Wheatley B.. Lessons from more than a decade in patient portals. Health Aff 2016; 1–7. doi: 10.1377/hblog20160407.054362. [Google Scholar]
- 14. Ralston JD, Hirsch IB, Hoath J, et al. Web-based collaborative care for type 2 diabetes: a pilot randomized trial. Diabetes Care 2009; 32 (2): 234–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.American Recovery and Reinvestment Act of 2009. H.R. 1 -- 111th Congress: American Recovery and Reinvestment Act of 2009. www.GovTrack.us. 2019.
- 16. Davis SE, Osborn CY, Kripalani S, et al. Health literacy, education levels, and patient portal usage during hospitalizations. AMIA Annu Symp Proc 2015; 2015: 1–10. [PMC free article] [PubMed] [Google Scholar]
- 17. Pearl R. Kaiser Permanente Northern California: current experiences with internet, mobile, and video technologies. Health Aff 2014; 33 (2): 251–7. [DOI] [PubMed] [Google Scholar]
- 18. Steitz BD, Cronin RM, Davis SE, et al. Long-term patterns of patient portal use for pediatric patients at an Academic Medical Center. Appl Clin Inform 2017; 8: 779–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Goldzweig CL, Orshansky G, Paige NM, et al. Electronic patient portals: evidence on health outcomes, satisfaction, efficiency, and attitudes. Ann Intern Med 2013; 159 (10): 677–25. [DOI] [PubMed] [Google Scholar]
- 20. Woods SS, Forsberg CW, Schwartz EC, et al. The association of patient factors, digital access, and online behavior on sustained patient portal use: a prospective cohort of enrolled users. J Med Internet Res 2017; 19 (10): e345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Haun JN, Lind JD, Shimada SL, et al. Evaluating user experiences of the secure messaging tool on the Veterans Affairs’ patient portal system. J Med Internet Res 2014; 16 (3): e75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sarkar U, Karter AJ, Liu JY, et al. The literacy divide: health literacy and the use of an internet-based patient portal in an integrated health system—results from the Diabetes Study of Northern California (DISTANCE). J Health Commun 2010; 15 (Suppl 2): 183–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Irizarry T, Shoemake J, Nilsen ML, et al. Patient portals as a tool for health care engagement: a mixed-method study of older adults with varying levels of health literacy and prior patient portal use. J Med Internet Res 2017; 19 (3): e99–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sarkar U, Karter AJ, Liu JY, et al. Social disparities in internet patient portal use in diabetes: evidence that the digital divide extends beyond access. J Am Med Assoc 2011; 18 (3): 318–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Tieu L, Sarkar U, Schillinger D, et al. Barriers and facilitators to online portal use among patients and caregivers in a safety net health care system: a qualitative study. J Med Internet Res 2015; 17 (12): e275–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wakefield DS, Mehr D, Keplinger L, et al. Issues and questions to consider in implementing secure electronic patient-provider web portal communications systems. Int J MedInform 2010; 79 (7): 469–77. [DOI] [PubMed] [Google Scholar]
- 27. Fullerton C, Aponte P, Hopkins R III, et al. Lessons learned from pilot site implementation of an ambulatory electronic health record. Bayl Univ Med Cent Proc 2006; 19 (4): 303–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ruland CM, Brynhi H, Andersen R, et al. Developing a shared electronic health record for patients and clinicians. Stud Health Technol Inform 2008; 136: 57–62. [PubMed] [Google Scholar]
- 29. Osborn CY, Rosenbloom ST, Stenner SP, et al. MyHealthAtVanderbilt: policies and procedures governing patient portal functionality. J Am Med Assoc 2011; 18 (Suppl 1): i18–i23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Koonce TY, Giuse DA, Beauregard JM, et al. Toward a more informed patient: bridging health care information through an interactive communication portal. J Med Libr Assoc 2007; 95 (1): 77–81. [PMC free article] [PubMed] [Google Scholar]
- 31. Duncavage S, Mathe J, Werner J, et al. A modeling environment for patient portals. AMIA Annu Symp Proc 2007; 2007 : 201–5. [PMC free article] [PubMed] [Google Scholar]
- 32. Cronin RM, Davis SE, Shenson JA, et al. Growth of secure messaging through a patient portal as a form of outpatient interaction across clinical specialties. Appl Clin Inform 2015; 6: 288–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.(null) RCT. R: A Language and Environment for Statistical Computing https://www.R-project.org/. Accessed May 20, 2018.
- 34. Irizarry T, DeVito Dabbs A, Curran CR.. Patient portals and patient engagement: a state of the science review. J Med Internet Res 2015; 17 (6): e148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Simon GE, Ralston JD, Savarino J, et al. Randomized trial of depression follow-up care by online messaging. J Gen Intern Med 2011; 26 (7): 698–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Woolf SH, Krist AH, Lafata JE, et al. Engaging patients in decisions about cancer screening: exploring the decision journey through the use of a patient portal. Am J Prev Med 2018; 54 (2): 237–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Giardina TD, Baldwin J, Nystrom DT, et al. Patient perceptions of receiving test results via online portals: a mixed-methods study. J Am Med Assoc 2018; 25 (4): 440–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Powell KR. Patient-perceived facilitators of and barriers to electronic portal use. Comput Inform Nurs 2017; 35: 565–73. [DOI] [PubMed] [Google Scholar]
- 39. Sakaguchi-Tang DK, Bosold AL, Choi YK, et al. Patient portal use and experience among older adults: systematic review. JMIR Med Inform 2017; 5 (4): e38–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Ancker JS, Nosal S, Hauser D, et al. Access policy and the digital divide in patient access to medical records. Health Policy Technol 2017; 6 (1): 3–11. [Google Scholar]
- 41. Thompson LA, Martinko T, Budd P, et al. Meaningful use of a confidential adolescent patient portal. J Adolesc Health 2016; 58 (2): 134–40. [DOI] [PubMed] [Google Scholar]
- 42. Ancker JS, Sharko M, Hong M, et al. Should parents see their teen’s medical record? Asking about the effect on adolescent–doctor communication changes attitudes. J Am Med Assoc 2018; 25 (12): 1593–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Zhao JY, Song B, Anand E, et al. Barriers, facilitators, and solutions to optimal patient portal and personal health record use: a systematic review of the literature. AMIA Annu Symp Proc 2017; 2017: 1913–22. [PMC free article] [PubMed] [Google Scholar]
- 44. Perzynski AT, Roach MJ, Shick S, et al. Patient portals and broadband internet inequality. J Am Med Assoc 2017; 24 (5): 927–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Cronin RM, Fabbri D, Denny JC, et al. Automated classification of consumer health information needs in patient portal messages. AMIA Annu Symp Proc 2015; 2015: 1861–70. [PMC free article] [PubMed] [Google Scholar]
- 46. Zhong X, Liang M, Sanchez R, et al. On the effect of electronic patient portal on primary care utilization and appointment adherence. BMC Med Inform Decis Mak 2018; 18(1): 1–12. doi: 10.1186/s12911-018-0669-8 [DOI] [PMC free article] [PubMed]
- 47. North F, Crane SJ, Chaudhry R, et al. Impact of patient portal secure messages and electronic visits on adult primary care office visits. Telemed J E Health 2014; 20 (3): 192–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Parker J, Coiera E.. Improving clinical communication: a view from psychology. J Am Med Assoc 2000; 7 (5): 453–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Edwards A, Fitzpatrick L-A, Augustine S, et al. Synchronous communication facilitates interruptive workflow for attending physicians and nurses in clinical settings. Int J Med Inform 2009; 78 (9): 629–37. [DOI] [PubMed] [Google Scholar]