Abstract
Rationale
Ineffective peak inspiratory flow rate (PIFR) generation in patients using inhalers results in insufficient drug delivery to the lungs and poor clinical outcomes. Low inspiratory muscle strength is associated with suboptimal PIFR.
Objective
To examine in a prospective study the relationship between PIFR and skeletal muscle strength using hand grip strength (HGS) as a surrogate.
Methods
Adult patients admitted with acute exacerbation of chronic obstructive pulmonary disease (COPD) were enrolled. PIFR was measured within 48 hours before discharge. PIFR below 60L/min was considered suboptimal. HGS was measured using a handheld dynamometer. Any readmissions and emergency department visit data were collected. The associations between PIFR, HGS, 30 and 90-day COPD and all-cause readmissions were examined, without and with adjustment for age, race and gender.
Results
Of the 75 enrolled patients, 56% had suboptimal PIFR; they were older (63.9±9.7 vs. 58.2±7.7 years) and had significantly lower HGS (24.2±11.1 vs. 30.9±10.9 Kg) compared to those with optimal PIFR. There were no significant differences between the two PIFR groups by gender, race, history of coronary artery disease, congestive heart failure, hypertension or functional scores. Each kilogram increase in HGS was associated with 0.50 (95%CI 0.18–0.89, p = 0.003) L/min increase in PIFR. We did not observe an association between PIFR and 30 or 90-day readmission rates.
Conclusion
We found a significant association between HGS and PIFR in hospitalized patients with acute exacerbations of COPD. Whether interventions aimed at increasing skeletal muscle strength also result in improvement in PIFR remains unclear and need further study.
Introduction
Patients with chronic obstructive pulmonary disease (COPD) are high users of healthcare. The estimated annual cost of COPD management in the US has been estimated at up to 50 billion dollars, a third of which is directly related to inpatient hospitalization for COPD exacerbations[1]. About one in five patients admitted with an acute exacerbation of COPD (AECOPD) is re-hospitalized within 30 days of hospital discharge.[2,3] Inhaled drugs are the cornerstone for prevention of COPD exacerbation and hospitalization[4], and provide better pulmonary bioavailability, lower dose requirement and less systemic toxicities than the oral or injectable drugs. Current recommendations advise that all patients hospitalized with AECOPD should be discharged on a controller inhaler to reduce risk of exacerbation and to improve control of COPD.[5,6]
Effective peak inspiratory flow rate (PIFR) generation is associated with optimal drug delivery to distal airways and lung parenchyma, and better clinical outcomes in those on inhaler therapy, especially dry powder inhaler (DPI) users.[7,8,9] Several studies have investigated the effect of suboptimal PIFR on the efficacy of different DPIs in preventing COPD exacerbations, however, most trials have been done in outpatient settings and in patients with controlled COPD.[10,11,12] In one study, subjects with suboptimal PIFR were found to have fewer days to next COPD exacerbation compared to patients with optimal PIFR.[13]
One determinant of PIFR is the strength of inspiratory muscles.[14] COPD is associated with skeletal respiratory muscle dysfunction and reduced muscle endurance.[15–17]. Limb muscle dysfunction has been well described in COPD. For example, the collaborative guidelines issued in 2014 by American Thoracic Society and European Respiratory Society discuss limb atrophy and weakness in stable COPD, as well as significant skeletal muscle dysfunction from the baseline during acute exacerbation of COPD.[18] However, the relationship between PIFR and skeletal muscle strength in hospitalized patients has not been examined. It is important to know whether patients with sub-optimal PIFR have impaired skeletal muscle strength as well, which may correlate with a higher risk of frailty. Our objective was to prospectively examine the relationship between PIFR and hand muscle strength in hospitalized patients with AECOPD.
Methods
Hospitalized adult patients who were admitted with AECOPD at Virginia Commonwealth University Hospital (VCU) from January 2018 to June 2018 were eligible for enrollment in this prospective study. We excluded patients with tracheostomy and those with physical or cognitive limitations. Patients were approached for written consent if their treating clinician expected them to be discharged within the next 48 hours. Demographic and clinical information data were obtained from medical records. The study was approved under Virginia Commonwealth University School of Medicine (VCU) Institutional Review Board and ethics committee under expedited review (IRB HM20012033)
PIFR was measured by using In-Check® DIAL device (Alliance Tech Medical) at bedside. In-Check® DIAL device is a small simple dial, that has been used in previous studies to measure PIFR.[10,12,19]
The device is well validated,[20,21] capable of measuring inspiratory flow rates between 15 and 120 L/min. The accuracy is within ±10% or within 10 L/min, whichever is greater.[22] This device has the option to be set for a specific level of resistance to airflow. We set the resistance to simulate the Discus® DPI; Discus® DPI is a commonly prescribed DPI, with low to medium resistance.[23] Patients were instructed to inhale as fast as possible after a complete exhalation in a sitting position. Patients were allowed to attempt up to 3 times, with 1–3 minutes breaks between attempts; the breaks were allowed so that patients can return to their baseline respiration ability. We used the mean of the three attempts in our analysis. In accordance with prior literature, a PIFR of >60 L/min was considered optimal force for drug delivery of a DPI, while a PIFR below 60L/min was considered suboptimal.[24–26]
Muscle strength was measured with hand grip strength (HGS) using a handheld dynamometer, Jama®, in kilograms.[27] The test was performed at bedside with the subject also in sitting position, shoulder adducted, and elbow on the side of the dominant hand flexed to 90 degrees. Subject was asked to squeeze the dynamometer handle as hard as possible for 3–5 seconds. The test was performed with two attempts, with one-minute breaks in-between trials, and the mean of the two was used in data analyses.
The level of functional limitation due to dyspnea and COPD related symptoms were assessed via modified Medical Research Council (mMRC) dyspnea scale and COPD Assessment Test (CAT) for enrolled patients. The mMRC is a 5-point (0–4) scale based on the severity of dyspnea, “0” being minimal dyspnea with activity and “4” being dyspnea at rest. The CAT includes eight items related to the severity of cough, sputum, dyspnea, chest tightness, capacity for exercise and activities, confidence, sleep quality and energy levels, the score ranging from 0 to 40.[28]
Subjects were also asked about the contact phone number where they could be reached at 30 and 90 days after discharge. Rehospitalization data after index hospital admission were collected via chart review at 30 and 90 days. Those with no readmission on chart review at day 30, were contacted via phone and inquired about any emergency department visit or hospitalization at any other facilities; same process was done at 90 days after index admission. Those with 30-day readmission due to any cause were excluded from the 90-day follow-up.
Data were summarized using mean ± standard deviation for continuous variables and with frequencies for categorical variables. Difference between the groups were measured using independent t-test, rank sum test, or chi-square test as appropriate. Linear regression models were used to assess the relationship between PIFR and HGS, and logistic regression models were used to assess the relationship between dichotomized PIFR and HGS, without and with adjustment for age, gender, and race. To examine the relationship between readmissions at 30 or 90 days and PIFR, we used logistic regression models, without and with adjustment for age, gender, race, and mMRC score. All regression models were performed using bootstrap with 1000 replications using Stata 14.1 for Windows (College Station, Texas, USA).
Results
Of 75 patients enrolled in the study, 56% (n = 42) had sub-optimal PIFR (S-PIFR). The mean S-PIFR was 46.1±10 vs 74.2±11 L/min,(p = 0.76) in optimal PIFR (O-PIFR) group. Patients with S-PIFR were older (63.9±9.7 years vs 58.2±7.7 years, p = 0.008), as compared to those with O-PIFR. Sixty percent of patients with S-PIFR were current smokers. The mean CAT score was 25±8.3 for S-PIFR cohort and 26.3±6.8 for O-PIFR (p = 0.4). Mean mMRC was 2.9±0.8 in S-PIFR group vs 2.6±1.0 for O-PIFR (p = 0.13). There was no statistically significant difference in CAT and mMRC between the two cohorts. There were also no significant differences by gender, race, history of coronary artery disease, congestive heart failure, or hypertension between the two PIFR groups (Table 1). The numbers of patients with concomitant asthma was higher in the O-PIFR than in S-PIFR group (12/18 (66.6%) vs 6/18 subjects (33.3%), p = 0.03).
Table 1. Patient demographics and clinical characteristics for all participants and by peak inspiratory flow rate (PIFR) categories suboptimal PIFR (S-PIFR) and optimal PIFR (O-PIFR).
P values: S-PIFR vs O-PIFR.
| All | S-PIFR | O-PIFR | p value | |
|---|---|---|---|---|
| Patients, n (%) | 75 (100) | 42 (56) | 33 (44) | |
| Age, mean (SD) | 61.4 ±9.2 | 63.9 ±9.7 | 58.2 ±7.7 | 0.008 |
| Female, n (%) | 42 (56) | 26 (61.2) | 16 (48.4) | 0.34 |
| Race | ||||
| White, n (%) | 21 (28) | 11 (26.1) | 10 (30.3) | 0.79 |
| Other, n (%) | 54 (72) | 31 (73.8) | 23 (69.7) | |
| Current smoker, n (%) | 46 (61.3) | 25 (59.5) | 21 (63.6) | 0.81 |
| CAT score, mean (SD) | 25.6 ±7.6 | 25.0 ±8.3 | 26.3 ±6.8 | 0.44 |
| mMRC, mean (SD) | 2.7 ±0.9 | 2.9 ±0.8 | 2.6 ±1.0 | 0.13 |
| Coronary artery disease, n (%) | 16 (31.3) | 9 (21.4) | 7 (21.2) | 0.99 |
| Hypertension, n (%) | 51 (68) | 32 (76.1) | 19 (57.5) | 0.13 |
| Diabetes mellitus, n (%) | 26 (34.6) | 14 (33.3) | 12 (36.3) | 0.81 |
| Congestive heart failure, n (%) | 20 (26.6) | 13 (30.9) | 7 (21.2) | 0.43 |
| Asthma, n (%) | 18 (24) | 6 (33.3) | 12 (66.6) | 0.03 |
| Hand Grip Strength (kg), mean (SD) | 27.2 ±11.4 | 24.2 ±11.1 | 30.9 ±10.9 | 0.003 |
| PIFR (L/min), mean (SD) | 58.6 ±17.6 | 46.1 ±10.4 | 74.2 ±11.4 | 0.76 |
Association between Hand Grip (HGS) and PIFR
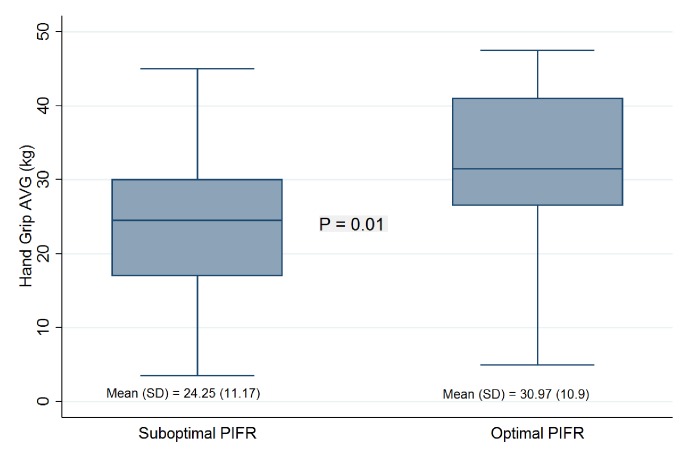
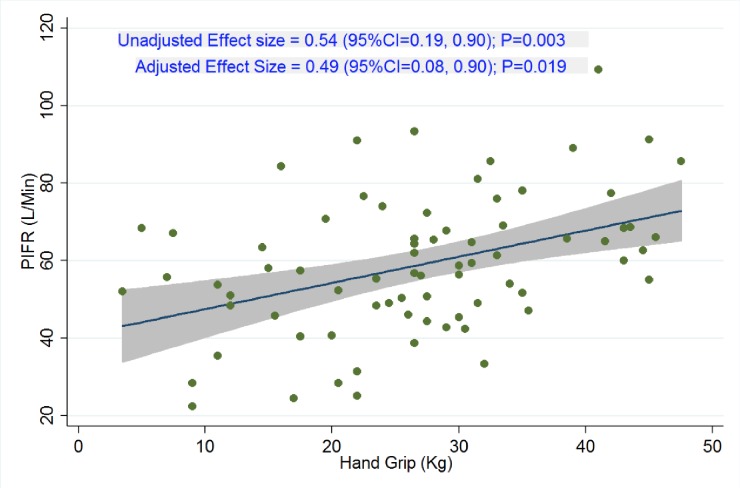
The mean hand grip strength (HGS) was 27.2±11.4 kg in the study cohort. Patients in the S-PIFR group had significantly lower HGS than those in the O-PIFR group (24.2±11.1 vs 30.9±10.9 kg, p = 0.01, Figs 1 & 2). Each kilogram increase in HGS was associated with 0.54 L/min (95% confidence interval [CI], 0.18–0.89; P = 0.003) increase in PIFR in unadjusted model. The association remained significant when adjusted for age, sex, and race (effect size = 0.49; 95%CI = 0.08 to 0.90; P = 0.02).
Fig 1. Association between peak inspiratory flow rate (PIFR) and Hand grip strength (HGS).
The middle line in the box is the median HGS, the upper and lower boundaries of the box represent 75th and 25th percentiles of HGS distribution, the whiskers are 1.5*IQR from 75th and 25th percentiles from HGS.
Fig 2. Association between peak Inspiratory flow rate (PIER, L/min) and Hand Grip Strength(HGS, kg) as continuous variables.
Association of PIFR with readmission rate
The 30-day all-cause readmission rate was 21% (16/75), while the 90-day all-cause readmission rate was 37% (28/75). While our data did not show a statistically association between PIFR and 30 or 90-day readmission rates, patients in the S-PIRF group had a trend towards higher rate of 30-day (11/42 vs 5/33 patients, RR 0.36 (0.06–2.3), p = 0.2) and 90-day all-cause readmission rate (17/42 vs 11//33, RR 0.71 (0.20–2.5, p = 0.6) as compared to the O-PIFR group (Table 2).
Table 2. Readmission rates for all patients, suboptimal PIFR (S-PIFR) and optimal PIFR (O-PIFR).
CI: confidence interval; COPD: chronic obstructive pulmonary disease; OR: Odds Ratio, P values: S-PIFR vs O-PIFR.
| Total (n = 75) | S-PIFR (n = 42; 56%) | O-PIFR (n = 33; 44%) | OR (95%CI) | p value | |
|---|---|---|---|---|---|
| COPD readmission within 30 days, n (%) | 12 (16) | 7 (16.6) | 5 (15.1) | 0.65 (0.07, 5.6) | 0.70 |
| COPD readmission within 90 days, n (%) | 20 (26.6) | 12 (28.5) | 8 (24.2) | 0.82 (0.18, 3.6) | 0.79 |
| Emergency department visit for COPD within 30 days, n (%) | 14 (18.6) | 8 (19.0) | 6 (18.1) | 0.67 (0.13, 3.5) | 0.64 |
| Emergency department visit for COPD within 90 days, n (%) | 22 (40.8) | 11 (26.1) | 11 (33.3) | 1.01 (0.30, 3.4) | 0.98 |
| All cause readmission within 30 days, n (%) | 16 (21.3) | 11 (26.1) | 5 (15.1) | 0.36 (0.06, 2.3) | 0.28 |
| All cause readmission within 90 days, n (%) | 28 (37.3) | 17 (40.4) | 11 (33.3) | 0.71 (0.20, 2.5) | 0.60 |
Discussion
In this prospective study, we found that suboptimal PIFR is highly prevalent among hospitalized patients with AECOPD (i.e., more than half). Further, we found a linear relationship between HGS and PIFR. This relationship was robust and remained statistically significant after adjusting for potential confounders. We did not find a statistically significant association between PIFR and 30 or 90-day readmission.
Respiratory and non-respiratory skeletal muscle dysfunction has been previously described in COPD, which suggests biological plausibility for a relationship between PIFR and HGS.[29] The mechanisms of skeletal muscle dysfunction in COPD are still poorly understood, however it has been hypothesized that a net loss of muscle mass and myodysfunction due to intrinsic alterations such as mitochondrial abnormalities and loss of contractile proteins may occur, but also due to external factors such as hypoxia, hypercapnia and acidosis.[18,30] Chronic hypoxia interferes with protein synthesis in muscle cells, leading to muscle dysfunction.[31,32] Further, proinflammatory cytokines such as tumor necrosis factor- α levels are increased in COPD patients,[33,34] which can cause increased apoptosis of the skeletal muscle cells through a variety of mechanisms.[35,36]
In recent years, HGS use has been of great interest in different areas, including in the geriatric population, as a predictor of frailty and as a surrogate marker of cognitive function.[37] In a large metanalysis of 23,400 patients with cardiovascular disease, HGS emerged as an independent predictor of cardiac death, all-cause mortality and hospital admission.[38] Further, the clinical importance of HGS test in patients with COPD has also been reported in numerous studies.[39,40] HGS was found to be lower in patients with COPD as compared to healthy subjects.[15] Reduced HGS is associated with increased risk of hospital readmission due to acute exacerbation of COPD.[41] In one study, patients with COPD had a 15% decrease in maximum strength as compared to the control group.[42] In addition to muscle strength, in COPD patients HGS has been correlated well with overall exercise capacity, as measured by 6 minute walk test,[42–44] which has been found to be a good determinant of global quality of life and general mortality in these patients.[45–47] However, in spite of its importance, exercise capacity is not routinely measured in clinical practice because it entails time and space, and sometimes cannot be performed due to comorbid conditions such as arthritis, heart or cerebrovascular disease. As such, HGS has been recommended as a marker of muscle strength, especially when 6-minute walk test cannot be performed.[42,43]. Moreover, an association between HGS and forced expiratory volume in 1 second have been described in patients with COPD.[15,16]
The direct relationship between HGS and PIFR indicates that HGS may serve as an indirect tool to predict inspiratory muscle strength, as it can be performed at the bedside and is easily repeatable in hospitalized patients.[48] A formal measurement of inspiratory muscle strength requires special devices that are often only available in research settings, and hence not feasible for routine clinical purposes. Whether interventions aimed at increasing skeletal muscle strength also result in improvement of PIFR remains unknown, but such interventions are worth investigating.
As compared to patients in outpatient setting, we found in our study population a higher prevalence of S-PIFR. Mahler et al. found in 213 patients with stable COPD that 19% had S-PIFR (<60 L/min) against the resistance of Discus; S-PIFR was associated with age, female gender and lower percent predicted forced vital capacity and inspiratory capacity compared to O-PIFR.[10] However, the prevalence rate in our study is consistent with other studies conducted in inpatient setting.[13,19] For example, in a multicenter prospective study of 268 hospitalized patients with AECOPD, Sharma et al observed 81 patients with S-PIFR (32%); interestingly, the S-PIRF group was comprised mostly by older women.[19] In another retrospective study of hospitalized patients with AECOPD the prevalence of S-PIFR was 52% (64/123 subjects), and the majority were older than 65 years. The high prevalence rate may be due to the catabolic nature of the acute illness and coexistent metabolic derangements such as hypoxia, hypercapnia and acidosis, hence AECOPD leading to weaker respiratory muscles.
One may hypothesize that S-PIFR is associated with higher 30 or 90-day readmission in patients discharged on DPIs, however no large prospective study to date has evaluated the effect of S-PIFR on re-hospitalization. In a retrospective study, Loh et al found significantly lower number of days to readmission in discharged subjects with PIFR<60 L/min.[13] While we did not find a relationship between PIFR and 30 or 90-day readmission rates, the study was not powered for these outcomes.
This study has notable strengths and some potential limitations. In this prospective study we managed to follow patients for readmissions, including hospitalizations in other institutions within 90 days from the index admission, with very few dropouts, as opposed to other similar studies [19,13] that evaluated readmissions to the same healthcare facility. A potential limitation is that we measured PIFR against the simulated resistance of one DPI, a Discus® DPI. Discus DPI is commonly used and has lower internal resistance than others such as Turbuhaler® and Handihaler® DPIs. Because we found high prevalence of S-PIFR (~50%) against low resistance DPI, the prevalence of S-PIFR is likely even higher when patients are discharged on DPIs with higher internal resistance. Furthermore, we did not perform routine pulmonary function testing or 6 minute walk tests to determine in a standard fashion the severity of global functional impairment. Moreover, we could not confirm patients’ adherence to DPI usage after discharge, issue that may impact 30 and 90-day readmission rates. Although there was trend toward higher 30 and 90-day all-cause readmission and 30-day COPD readmission in individuals with S-PIFR, this was not statistically significant. A larger sample size may yield more comprehensive results that could support this hypothesis.
This is the first study to investigate the association between PIFR with HGS in hospitalized patients with AECOPD. The HGS can be used as a surrogate measurement to assess inspiratory muscle strength. Whether interventions aimed at increasing skeletal muscle strength also result in improvement in PIFR remains unclear and needs future study. However, both PIFR and HGS measurements are simple and likely beneficial in clinical practice. As such, we recommend PIFR and HGS to be measured routinely in clinical setting in order to assess this dimension of frailty, and potentially to determine the proper DPI type upon discharge. As such, subjects with S-PIFR may benefit from lower internal resistance DPIs or even long-acting controller medications in nebulized form.
Supporting information
(XLSX)
Acknowledgments
All authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript by contributing to design, data process, drafting and critically revising the manuscript; and approving this draft for submission and accepting responsibility for the contents within. Authors wish to thank Chris Dewilde, PhD for her contribution in preparing IRB documentation, submission and correspondence, and for her effort to coordinate study activities. Authors also want to thank Laura Puckette, RNCC and Dena Khorsandi, MD for their work in recruiting patients and data collection.
Abbreviations
- AECOPD
acute exacerbation of chronic obstructive pulmonary disease
- PIFR
peak inspiratory flow rate
- DPI
dry powder inhaler
- Mmrc
modified Medical Research Council
- CAT
COPD Assessment Test
- HGS
hand grip strength
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
Research grant from VCU Johnson Center (VJC) for Critical Care and Pulmonary Research- non for profit source of funding provided by the department of pulmonary and critical care at VCU
References
- 1.National Heart Lung and Blood Institude. Morbidity and mortality: 2012 chart book on cardiovascular, lung, and blood diseases. https://www.nhlbi.nih.gov/files/docs/research/2012_ChartBook_508.pdf.
- 2.Xu J, Murphy SL, Kochanek KD, Bastian BA. Deaths: Final Data for 2013. Natl Vital Stat Rep. 2016;64(2):1–119. [PubMed] [Google Scholar]
- 3.Braman SS. Hospital Readmissions for COPD: We Can Meet the Challenge. Chronic Obstr Pulm Dis. 2015;2(1):4–7. 10.15326/jcopdf.2.1.2015.0130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Salpeter SR. Bronchodilators in COPD: impact of beta-agonists and anticholinergics on severe exacerbations and mortality. Int J Chron Obstruct Pulmon Dis. 2007;2(1):11–18. 10.2147/copd.2007.2.1.11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Global Initiative for Chronic Obstructive Lung Disease. Global strategy for diagnosis, management and prevention of chronic obstructive pulmonary disease. 2017; https://goldcopd.org.
- 6.Crompton GK, Barnes PJ, Broeders M, et al. The need to improve inhalation technique in Europe: a report from the Aerosol Drug Management Improvement Team. Respir Med. 2006;100(9):1479–1494. 10.1016/j.rmed.2006.01.008 [DOI] [PubMed] [Google Scholar]
- 7.Al-Showair RA, Tarsin WY, Assi KH, Pearson SB, Chrystyn H. Can all patients with COPD use the correct inhalation flow with all inhalers and does training help? Respir Med. 2007;101(11):2395–2401. 10.1016/j.rmed.2007.06.008 [DOI] [PubMed] [Google Scholar]
- 8.Newman SP. Principles of metered-dose inhaler design. Respir Care. 2005;50(9):1177–1190. [PubMed] [Google Scholar]
- 9.Newman SP. Drug delivery to the lungs from dry powder inhalers. Curr Opin Pulm Med. 2003;9 Suppl 1:S17–20. [DOI] [PubMed] [Google Scholar]
- 10.Mahler DA, Waterman LA, Gifford AH. Prevalence and COPD phenotype for a suboptimal peak inspiratory flow rate against the simulated resistance of the Diskus(R) dry powder inhaler. J Aerosol Med Pulm Drug Deliv. 2013;26(3):174–179. 10.1089/jamp.2012.0987 [DOI] [PubMed] [Google Scholar]
- 11.Malmberg LP, Rytila P, Happonen P, Haahtela T. Inspiratory flows through dry powder inhaler in chronic obstructive pulmonary disease: age and gender rather than severity matters. Int J Chron Obstruct Pulmon Dis. 2010;5:257–262. 10.2147/copd.s11474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kawamatawong T, Khiawwan S, Pornsuriyasak P. Peak inspiratory flow rate measurement by using In-Check DIAL for the different inhaler devices in elderly with obstructive airway diseases. J Asthma Allergy. 2017;10:17–21. 10.2147/JAA.S127580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Loh CH, Peters SP, Lovings TM, Ohar JA. Suboptimal Inspiratory Flow Rates Are Associated with Chronic Obstructive Pulmonary Disease and All-Cause Readmissions. Ann Am Thorac Soc. 2017;14(8):1305–1311. 10.1513/AnnalsATS.201611-903OC [DOI] [PubMed] [Google Scholar]
- 14.Barnes N, Agyapong-Badu S, Walsh B, Stokes M, Samuel D. Reliability and acceptability of measuring sniff nasal inspiratory pressure (SNIP) and peak inspiratory flow (PIF) to assess respiratory muscle strength in older adults: a preliminary study. Aging Clin Exp Res. 2014;26(2):171–176. 10.1007/s40520-013-0146-2 [DOI] [PubMed] [Google Scholar]
- 15.Shah S, Nahar P, Vaidya S, Salvi S. Upper limb muscle strength & endurance in chronic obstructive pulmonary disease. Indian J Med Res. 2013;138(4):492–496. [PMC free article] [PubMed] [Google Scholar]
- 16.Strandkvist VJ, Backman H, Roding J, Stridsman C, Lindberg A. Hand grip strength is associated with forced expiratory volume in 1 second among subjects with COPD: report from a population-based cohort study. Int J Chron Obstruct Pulmon Dis. 2016;11:2527–2534. 10.2147/COPD.S114154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gosselink R, Troosters T, Decramer M. Peripheral muscle weakness contributes to exercise limitation in COPD. Am J Respir Crit Care Med. 1996;153(3):976–980. 10.1164/ajrccm.153.3.8630582 [DOI] [PubMed] [Google Scholar]
- 18.Maltais F, Decramer M, Casaburi R, et al. An official American Thoracic Society/European Respiratory Society statement: update on limb muscle dysfunction in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2014;189(9):e15–62. 10.1164/rccm.201402-0373ST [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sharma G, Mahler DA, Mayorga VM, Deering KL, Harshaw O, Ganapathy V. Prevalence of Low Peak Inspiratory Flow Rate at Discharge in Patients Hospitalized for COPD Exacerbation. Chronic Obstr Pulm Dis. 2017;4(3):217–224. 10.15326/jcopdf.4.3.2017.0183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chrystyn H. Is inhalation rate important for a dry powder inhaler? Using the In-Check Dial to identify these rates. Respir Med. 2003;97(2):181–187. 10.1053/rmed.2003.1351 [DOI] [PubMed] [Google Scholar]
- 21.Broeders ME, Molema J, Vermue NA, Folgering HT. In Check Dial: accuracy for Diskus and Turbuhaler. Int J Pharm. 2003;252(1–2):275–280. 10.1016/s0378-5173(02)00650-6 [DOI] [PubMed] [Google Scholar]
- 22.Alliance Tech Medical I. In-Check DIAL Inhaler Technique Training and Assessment Tool. http://www.alliancetechmedical.com/products/check-dial-training-device/, 2018.
- 23.Dal Negro RW. Dry powder inhalers and the right things to remember: a concept review. Multidiscip Respir Med. 2015;10(1):13 10.1186/s40248-015-0012-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Prime D, Grant AC, Slater AL, Woodhouse RN. A critical comparison of the dose delivery characteristics of four alternative inhalation devices delivering salbutamol: pressurized metered dose inhaler, Diskus inhaler, Diskhaler inhaler, and Turbuhaler inhaler. J Aerosol Med. 1999;12(2):75–84. 10.1089/jam.1999.12.75 [DOI] [PubMed] [Google Scholar]
- 25.Janssens W, VandenBrande P, Hardeman E, et al. Inspiratory flow rates at different levels of resistance in elderly COPD patients. Eur Respir J. 2008;31(1):78–83. 10.1183/09031936.00024807 [DOI] [PubMed] [Google Scholar]
- 26.Mahler DA, Waterman LA, Ward J, Gifford AH. Comparison of dry powder versus nebulized beta-agonist in patients with COPD who have suboptimal peak inspiratory flow rate. J Aerosol Med Pulm Drug Deliv. 2014;27(2):103–109. 10.1089/jamp.2013.1038 [DOI] [PubMed] [Google Scholar]
- 27.products P. User manual for the JAMAR Hydraulic Hand Dynamometer 2018; https://www.prohealthcareproducts.com/blog/user-manual-for-the-jamar-hydraulic-hand-dynamometer/.
- 28.Kim S, Oh J, Kim YI, et al. Differences in classification of COPD group using COPD assessment test (CAT) or modified Medical Research Council (mMRC) dyspnea scores: a cross-sectional analyses. BMC Pulm Med. 2013;13:35 10.1186/1471-2466-13-35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bui KL, Nyberg A, Rabinovich R, Saey D, Maltais F. The Relevance of Limb Muscle Dysfunction in Chronic Obstructive Pulmonary Disease: A Review For Clinicians. Clin Chest Med. 2019;40(2):367–383. 10.1016/j.ccm.2019.02.013 [DOI] [PubMed] [Google Scholar]
- 30.Iepsen UW, Pedersen BK. Development of Limb Muscle Dysfunction in COPD—Smoking, Inflammation or Simply Disuse? Am J Respir Cell Mol Biol. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bigard AX, Sanchez H, Birot O, Serrurier B. Myosin heavy chain composition of skeletal muscles in young rats growing under hypobaric hypoxia conditions. J Appl Physiol (1985). 2000;88(2):479–486. [DOI] [PubMed] [Google Scholar]
- 32.Rennie MJ, Edwards RH, Emery PW, Halliday D, Lundholm K, Millward DJ. Depressed protein synthesis is the dominant characteristic of muscle wasting and cachexia. Clin Physiol. 1983;3(5):387–398. 10.1111/j.1475-097x.1983.tb00847.x [DOI] [PubMed] [Google Scholar]
- 33.Di Francia M, Barbier D, Mege JL, Orehek J. Tumor necrosis factor-alpha levels and weight loss in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1994;150(5 Pt 1):1453–1455. [DOI] [PubMed] [Google Scholar]
- 34.Schols AM, Buurman WA, Staal van den Brekel AJ, Dentener MA, Wouters EF. Evidence for a relation between metabolic derangements and increased levels of inflammatory mediators in a subgroup of patients with chronic obstructive pulmonary disease. Thorax. 1996;51(8):819–824. 10.1136/thx.51.8.819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Agusti AG, Noguera A, Sauleda J, Sala E, Pons J, Busquets X. Systemic effects of chronic obstructive pulmonary disease. Eur Respir J. 2003;21(2):347–360. 10.1183/09031936.03.00405703 [DOI] [PubMed] [Google Scholar]
- 36.Adams V, Jiang H, Yu J, et al. Apoptosis in skeletal myocytes of patients with chronic heart failure is associated with exercise intolerance. J Am Coll Cardiol. 1999;33(4):959–965. 10.1016/s0735-1097(98)00626-3 [DOI] [PubMed] [Google Scholar]
- 37.Dudzinska-Griszek J, Szuster K, Szewieczek J. Grip strength as a frailty diagnostic component in geriatric inpatients. Clin Interv Aging. 2017;12:1151–1157. 10.2147/CIA.S140192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pavasini R, Serenelli M, Celis-Morales CA, et al. Grip strength predicts cardiac adverse events in patients with cardiac disorders: an individual patient pooled meta-analysis. Heart. 2019;105(11):834–841. 10.1136/heartjnl-2018-313816 [DOI] [PubMed] [Google Scholar]
- 39.Nyberg A, Saey D, Maltais F. Why and How Limb Muscle Mass and Function Should Be Measured in Patients with Chronic Obstructive Pulmonary Disease. Ann Am Thorac Soc. 2015;12(9):1269–1277. 10.1513/AnnalsATS.201505-278PS [DOI] [PubMed] [Google Scholar]
- 40.Marklund S, Bui KL, Nyberg A. Measuring and monitoring skeletal muscle function in COPD: current perspectives. Int J Chron Obstruct Pulmon Dis. 2019;14:1825–1838. 10.2147/COPD.S178948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vilaro J, Ramirez-Sarmiento A, Martinez-Llorens JM, et al. Global muscle dysfunction as a risk factor of readmission to hospital due to COPD exacerbations. Respir Med. 2010;104(12):1896–1902. 10.1016/j.rmed.2010.05.001 [DOI] [PubMed] [Google Scholar]
- 42.Kovarik M, Joskova V, Patkova A, Koblizek V, Zadak Z, Hronek M. Hand grip endurance test relates to clinical state and prognosis in COPD patients better than 6-minute walk test distance. Int J Chron Obstruct Pulmon Dis. 2017;12:3429–3435. 10.2147/COPD.S144566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.ozyemisci-Taskiran o. Hand grip strength in patients engaged in pulmonary rehabilitation program during COPD exacerbation. Eur Respir J. 2011;38:1247. [Google Scholar]
- 44.Jeong M, Kang HK, Song P, et al. Hand grip strength in patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2017;12:2385–2390. 10.2147/COPD.S140915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Burtin C, Ter Riet G, Puhan MA, et al. Handgrip weakness and mortality risk in COPD: a multicentre analysis. Thorax. 2016;71(1):86–87. 10.1136/thoraxjnl-2015-207451 [DOI] [PubMed] [Google Scholar]
- 46.Pinto-Plata VM, Cote C, Cabral H, Taylor J, Celli BR. The 6-min walk distance: change over time and value as a predictor of survival in severe COPD. Eur Respir J. 2004;23(1):28–33. 10.1183/09031936.03.00034603 [DOI] [PubMed] [Google Scholar]
- 47.Celli BR, Cote CG, Marin JM, et al. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med. 2004;350(10):1005–1012. 10.1056/NEJMoa021322 [DOI] [PubMed] [Google Scholar]
- 48.Frohnhofen H, Hagen O. Handgrip strength measurement as a predictor for successful dry powder inhaler treatment: application in older individuals with COPD. Z Gerontol Geriatr. 2011;44(4):245–249. 10.1007/s00391-011-0222-1 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(XLSX)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.