Abstract
Background
Lack of conceptual clarity and measurement methods have led to underdeveloped efforts to measure experience of participation in care by next of kin to older people in nursing homes.
Objective
We sought to assess the measurement properties of items aimed at operationalizing participation in care by next of kin, applied in nursing homes.
Methods
A total of 37 items operationalizing participation were administered via a questionnaire to 364 next of kin of older people in nursing homes. Measurement properties were tested with factor analysis and Rasch model analysis.
Results
The response rate to the questionnaire was 81% (n = 260). Missing responses per item varied between <0.5% and 10%. The 37 items were found to be two-dimensional, and 19 were deleted based on conceptual reasoning and Rasch model analysis. One dimension measured communication and trust (nine items, reliability 0.87) while the other measured collaboration in care (nine items, reliability 0.91). Items successfully operationalized a quantitative continuum from lower to higher degrees of participation, and were found to generally fit well with the Rasch model requirements, without disordered thresholds or differential item functioning. Total scores could be calculated based on the bifactor subscale structure (reliability 0.92). Older people (≥ 65 years) reported a higher degree of communication and trust and bifactor total scores than younger people (p < 0.05 in both cases). People with a specific contact person experienced a higher degree of participation in the two subscales and the bifactor total score (p < 0.05 in all three instances).
Conclusion
Psychometric properties revealed satisfactory support for use, in nursing home settings, of the self-reported Next of Kin Participation in Care questionnaire, with a bifactor structure. Additional research is needed to evaluate the effectiveness of the scales’ abilities to identify changes after intervention.
Trial registration
The KUPA project has Clinical Trials number NCT02708498.
Introduction
Many next of kin wish to participate in the care of frail older relatives at the end of their relatives’ lives [1, 2]. Such participation can benefit both parties [3, 4]. This represents one component of palliative care, and has been shown to increase the quality of care in nursing homes [5–8]. However, studies indicate that next of kin seldom actually participate in care in nursing homes, and nursing home staff describe this as problematic [9–14]. The topic is therefore a pressing target for interventions. The present study reports the development and testing of an instrument measuring the outcomes of such participation (i.e., the next of kin’s experience of participation in care).
Many older people live in nursing homes at the end of their life [15], often involving a loss of independence [16, 17]. Moreover, next of kin commonly describe nursing homes as bleak places, even labeling them “death’s waiting room” [18]. However, a Norwegian study reported that an older person’s move to a nursing home can prompt feelings of safety for next of kin, even though they still feel responsible for the care [19]. Many next of kin want to continue to participate in the care of their relatives [19], while others experience a pressure to take on more tasks than they would like to [19, 20]. The motivations for people wanting to participate in care vary, including love, a guilty conscience [21], or a desire to maintain the older person’s identity [22]. In an interview-based study of 17 next of kin of older people who had recently died, Andersson et al. [23] found that participation in care could induce feelings of satisfaction and a sense of importance. The implication was that such participation could be a strategy for next of kin to maintain a sense of control and cope with anxiousness and the passage of time. Another study [24] concluded that next of kin not taking part in end-of-life care could negatively affect their grieving process and the quality of care.
All people have the right to receive palliative care at the end of life, regardless of age or location [25]. The palliative care approach aims to improve quality of life for individuals facing the end of life, and their families. It aims to relieve suffering, taking physical, psychosocial, and spiritual needs into account in addition to the inclusion and support of next of kin [25]. Palliative care has been developed within care for terminal cancer patients, but is lacking in other contexts, such as nursing homes [26], and for other diagnoses, such as dementia [27]. This imbalance has led to a call from the World Health Organization [25] for interventions to improve palliative care for older people. A project called Implementation of Knowledge-Based Palliative Care in Nursing Homes (Swedish acronym KUPA) was established in response to this situation [28]. Although evaluation of the project included several outcome measurements from various perspectives, the need to develop a new instrument for measuring next of kin’s participation in care remains, as no measures have previously been adapted for use in nursing homes.
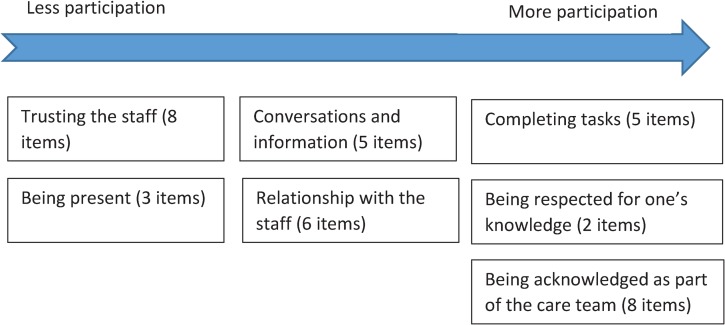
In this context, there is no consensus definition of “participation.” However, in the empirical literature, a recent study from the KUPA project [29] describing how next of kin participate in care at nursing homes concluded that participation was a balancing act between maintaining one’s own responsibility while also acceding responsibility to the nursing home staff. Another study within the project, exploring the meaning of participation in the care of older people in nursing homes [30], reported that participation had multiple perceived meanings and a prerequisite for participation was being present in different ways, whether physically, mentally, or both. Other ways of perceiving participation include conceiving information about the older person and performing practical tasks at the nursing home. Being present [31–33], conceiving information [31, 33–37], and doing practical tasks [31, 33–36] have been reported to represent participation among family caregivers in previous studies. Participation has also been expressed by next of kin as being respected for their knowledge [35–39], having a strong relationship with health care staff [35, 36, 39], and being admitted as part of the care team [31, 32, 39]. Based on these previous findings, we expected participation, from a next of kin perspective, to include: trusting staff, staff being present, conversations and information, having a good relationship with the staff, being invited by staff to complete tasks, being respected for one’s knowledge, and being acknowledged as part of the care team. Based on these areas, participation was operationalized in a novel questionnaire aimed at assessing participation in end-of-life care at nursing homes.
Aim
The present study aimed to assess the measurement properties of items intended to operationalize next of kin’s experience of participation in the care of older people in nursing homes.
Materials and methods
Design
This cross-sectional study was a psychometric evaluation of a newly developed questionnaire.
Setting
The study took place within the context of the Swedish welfare system. This system is based on the individual’s need for support and provides equal access for everyone in need of health care, care for older people, and social services. Responsibilities for health care in Sweden fall under the purview of two main authorities: county councils and municipalities. The former provide primary and specialist health care, and are responsible for investigations leading to diagnosis, medical treatment, and follow-up examinations. The latter are responsible for providing care and necessary assistance for older people living at home or in nursing homes, as well as social services [40].
In Sweden, next of kin do not have an obligation to provide care for older family members, although provision of substantial informal support and care is common. Hence, the Social Service Act [41] obligates municipalities to establish special housing, such as nursing homes for people aged ≥ 65 years, and to comprehensively satisfy their needs for daily life. Nursing homes typically consist of small apartments that residents lease and that provide all-hours service and care. Municipal social workers must assess prospective residents’ needs for support and care in daily life to determine their lease eligibility. This normally occurs when an older person becomes too sick and/or frail to continue independent living in his or her own home [41, 42].
Research setting
The KUPA project consists of an educational intervention about knowledge-based palliative care for nursing home staff and managers, as detailed in previous studies [28, 29]. The intervention consists of five seminars given over a period of 6 months, including, among other topics, the communication and participation of next of kin in palliative care.
Questionnaire development
In planning the KUPA project, no instrument was found in the literature for outcome assessment of next of kin’s participation in care within nursing homes. The most closely related instrument was the Family Collaboration Scale (FCS), [43, 44], which measures collaboration between relatives of frail older patients and nurses in acute hospital wards from the perspective of the relatives. The development of the 62-item FCS was based on relatives’ “lived experience” of collaboration, as explored in a phenomenological study, including testing of face and content validity [43–45].
Development of the new instrument started with a literature review using the keywords: next of kin, participation, palliative care, and nursing home in together with relevant synonyms. The databases used were PubMed and CINAHL. One of the researchers (LB) read the relevant articles identified in the search, and listed the concepts of “participation” or the synonym “involvement”. The definition and operationalization of the concepts were guided by the FCS questions, earlier qualitative studies [31–39], a theoretical framework [46], and a systematic review in the area [1]. Even if there was no direct involvement of next of kin in the item generation or concept elicitation stages, next of kin were indirectly involved by having contributed to the findings in earlier studies, inspiring the development of the novel instrument in the present study.
The relevance of the results for nursing home settings were scrutinized and discussed in three meetings with two experienced researchers in palliative care and instrument development (BR and GA). The content of the concepts was then operationalized into items (by LB) with four labeled response categories. The items were reviewed during three meetings and final response categories were increased from four to five to handle greater variation in the analysis. Face validity of this version was tested among five next of kin of older persons living in nursing homes recruited through convenience selection. This helped in refining the questions.
Next of Kin Participation in Care questionnaire
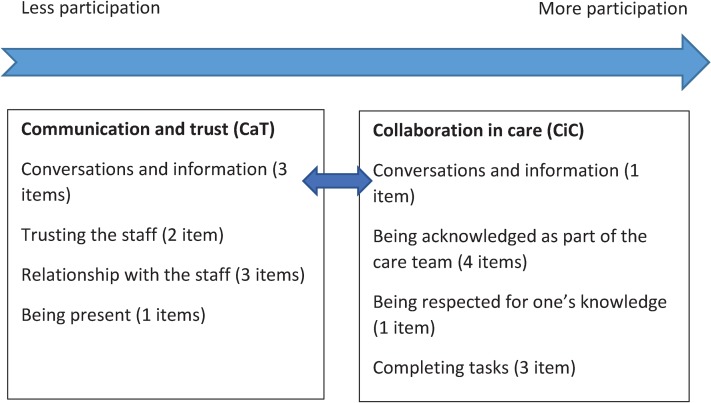
The subsequently developed self-reported questionnaire was named Next of Kin Participation in Care (NoK-PiC). It consists of a background section with 12 items about next of kin’s demographic data (e.g., age, sex, relationship to the older person, contact person in the nursing home) and 37 items about the next of kin’s perception of participation in care. The 37 items were divided into seven subject areas based on the content: trusting the staff (eight items), being present (three items), conversations and information (five items), relationship with the staff (six items), completing a task (five items), being respected for one’s knowledge (two items), and being acknowledged as part of the care team (eight items) (Fig 1). The five possible responses were: disagree (0), somewhat disagree (1), neither agree nor disagree (2), somewhat agree (3), and strongly agree (4). Items were expected to capture aspects from less to more participation. Besides the theoretical framework of 37 items that could be grouped into seven subject areas, the dimensionality of the items was uncertain, including whether items could be used in a single scale with a total score, or only in subscales with their own separate scores, or if a combination of subscale and total scale scores could be used.
Fig 1. Conceptualization and operationalization (37 items) of the Next of Kin Participation in Care questionnaire.
Sampling and study group
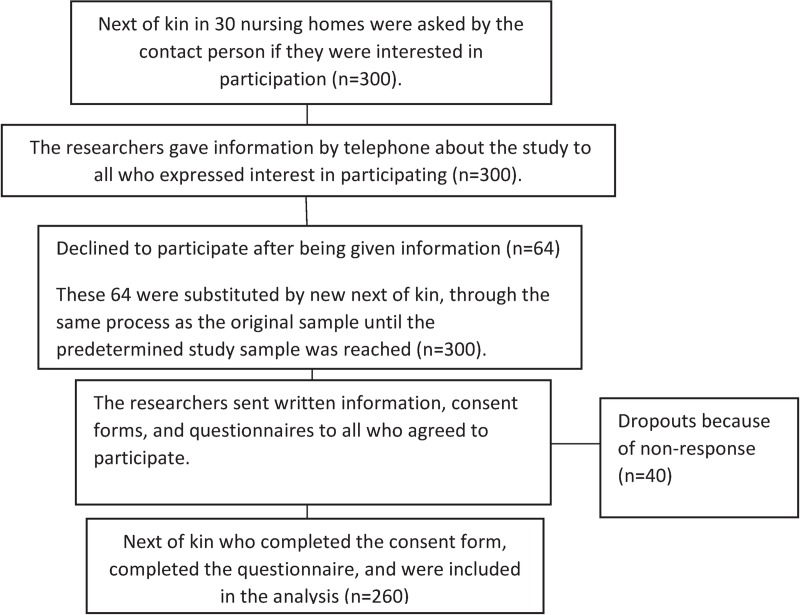
The inclusion criterion for questionnaire respondents was having a close relationship with an older person living in one of the 30 participating nursing homes in the KUPA project [28]. The respondents were recruited from these nursing homes before the educational intervention began. At each included nursing home, one nurse or manager was designated as contact person and informed the next of kin about the KUPA project and asked them about their interest in participating in the study (Fig 2). If interest was expressed, the contact person gave the candidate participant’s contact information to the research team. One researcher then contacted the candidate participants by telephone and provided further information. Candidates were consecutively included until the predetermined goal of 300 was reached (Fig 2). Those who agreed to participate then received written information, a consent form, and the questionnaires by postal mail. Candidates then returned the consent form and completed questionnaires to the project administrator by mail, and these were stored separately from each other. Of the 300 people who expressed interest in participating, 260 completed the questionnaire. The reasons for the 40 non-respondents are unknown (Fig 2).
Fig 2. Flowchart illustrating the inclusion procedure of next of kin in this study.
For Rasch model analysis (RMA) in general, and in the absence of major targeting problems, sample sizes of approximately 10–15 times the number of estimated item parameters are considered adequate (see the FAQ section at www.rummlab.com.au). Recently, a simulation study with 25 dichotomous items suggested that a sample size of around 250–500 provided a good balance for interpretation of the statistical RUMM2030 fit statistics [47].
Data analysis
Data are available from the Swedish National Data Service (DOI: 10.5878/8mj1-3y24), and upon request from the first author.
Step 1. Dimensionality
Because of uncertainties about the dimensionality of the 37 items, dimensionality was explored via explorative factor analysis (EFA). EFA requires complete data with no missing responses in any items. EFA was conducted based on recommendations, including parallel analysis to decide how many factors to retain for rotation, minimum rank factor analysis (MRFA), which is able to estimate the percentage of common variance explained by the EFA model, and on promin rotation that allowed factors to correlate (oblique) [48]. Additionally, as the items are polytomous and MRFA assumes only minor departures from normality, we based the analysis on a polychoric correlation matrix [49–50]. The appropriateness of performing EFA was checked based on quality criteria, using the Kaiser-Meyer-Olkin measure of sampling adequacy (ideally ≥ 0.50) and Bartlett’s test (ideally p < 0.05) [51]. FACTOR 10.5.03 (Lorenzo-Seva and Ferrando, Rovira i Virgili University, Tarragona, Spain) was used to conduct EFA.
Step 2. Item reduction
Data were then entered to the RUMM2030 Professional Edition 5.4 (RUMM Laboratory Pty Ltd, Duncraig, Australia) [52]. Item reduction was conducted based on conceptual reasoning among the researchers, and on polytomous RMA, i.e. partial credit model parameterisation was used. Decisions about item deletion were made through an iterative process, moving back and forth between the total scale and the two factors. During the iterative process, the following considerations for item deletion were kept in mind: items with a conceptual relationship with each other, with the factors and the seven theoretical subject areas; high residual correlations (indicating local dependency); high positive fit residuals (> 2.5, indicating multidimensionality); and an attempt to maintain items located at the end of the scale continuum, as much as possible. As mentioned above, one statistical reason for item deletion concerned item fit. In general, individual item fit residuals should range between −2.5 and 2.5, with 0 as the ideal value [53]. Signs of multidimensionality/under-discriminating items (fit residuals > 2.5) and response dependency/trait dependency/over-discriminating items (fit residuals < −2.5) [54] led to further exploration of the possible reasons for a lack of fit. This examination included inspection of the residual correlations between item pairs, and the item characteristic curves, to acquire a visual understanding of the deviations from Rasch model expectations.
After having a set of conceptually important items, which fitted the Rasch model expectations relatively well, local dependency was assessed within each factor separately. Residual correlations were now considered relative to the average observed residual correlation. Residual correlations that are high, relative to the overall set of correlations, indicate violation of the local independence assumption [55]. The critical value for relative residual correlations was identified following the procedures described by Christensen et al. [56].
Step 3. RMA of separate factors
RMA dictates that a set of items (which are supposed to be unidimensional) are rated using dichotomous or polytomous scoring in a sample, and compared with the Rasch model, which is based on fundamental measurement principles from the physical sciences [57]. The model separately locates people and items on a common interval level logit metric, ranging from minus to plus infinity, with mean item location set at zero. The extent to which successful measurement has been achieved is determined by examining the fit between observed data and model expectations. Linear measurement and invariant comparisons are possible if data are sufficiently in accord with the model [58]. However, almost no scale is perfect; thus, “almost perfect” may be an appropriate goal. Here, the RMA addresses targeting, reliability, model fit, differential item functioning (DIF; by sex and age), and hierarchical item ordering.
Step 4. Subtest analysis
A subtest is simply a single large item, created by adding together all of the items within it. These are also known as ‘super-items’, or ‘testlets’. A bifactor/subscale structure can be taken into account when conducting RMA in RUMM2030 and the feasibility of constructing a total score from the subscales can be evaluated [59]. Thus, by combining items within each domain into a subtest, each subtest is treated as a single item in the analysis. A subtest analysis takes account of multidimensionality in the data and indices (A, C2, and r) are estimated, specific to the subtest structure. The value A describes the non-error variance common to all subscales, the value C2 characterizes the variance that is unique to the subscales (relative to the common variance = 1), and the variable r is the latent correlation between the subscales. A subtest analysis performed on an approximate unidimensional scale will return high values for both A and r, and a low value for C2 [60, 61].
Step 5. Error of measurement and detectable difference
The standard error of measurement (SEM = ), representing the amount of variability in the scale that is caused by measurement error [62], and the minimal detectable change (95% confidence; MDC95 = ), representing the smallest change on an outcome measure that would be considered important [63], were calculated for the total ordinal sum scale as well as for the interval-level scale. To get an interval-level scale, the raw scores were transformed, using the metric (in logits) derived from the RMA, to an interval-level scale of the same range as the original raw scores [64].
Step 6. Group comparisons
IBM SPSS Statistics for Windows, Version 23.0 (IBM Corp., Armonk, NY, USA) was used for comparisons between independent groups, using the interval-level scales of the same range as the original raw scores [64]. Data were assessed regarding the underpinning assumptions, described, and analyzed using the t-test. The significance level was set at p < 0.05.
Ethical considerations
This study was part of the KUPA project approved by the governmental authority; the Regional Ethics Review Board in Lund, Sweden (no. 2015/69). The project was guided by the ethical principles for medical research [65]. Information was provided to participants regarding their right to withdraw from the study at any time without incurring any consequences. Each participant gave both oral and written informed consent before the questionnaire was administered. The KUPA project, including this study, is registered in the Clinical Trials database (NCT02708498).
Results
In total, 195 (75%) women and 65 (25%) men were included (mean age 63.9 ± 9.6 years).
Of the total study population (n = 260), 81% (n = 211) answered all the NoK-PiC items. The response pattern for each item is shown in Table 1. Missing responses per item varied between < 0.5% and 10% (Table 1). The sample size was sufficient for conducting RMA.
Table 1. Theoretically grouped Items, item response patterns, and missing items (n = 260).
| Agree, n | ||||||
|---|---|---|---|---|---|---|
| Theoretical categories Item (i) number and label |
Completely | Somewhat agree | Neither agree nor disagree | Somewhat disagree | Not at all | Missing, n (%) |
| Conversations and information | ||||||
| i1. I feel well-informed * | 68 | 104 | 57 | 23 | 6 | 2 (0.7) |
| i2. Staff discuss my older relative’s care with me * | 53 | 81 | 70 | 35 | 20 | 1 (0.3) |
| i3. Information about how I can best help * | 32 | 49 | 89 | 51 | 35 | 4 (1.5) |
| i4. Staff take time to talk with me * | 92 | 87 | 62 | 13 | 5 | 1 (0.3) |
| i5. I can consult with the staff if I have questions or concerns | 145 | 75 | 29 | 9 | 1 | 1 (0.3) |
| Being present | ||||||
| i6. I can be at my older relative’s side when I want | 205 | 40 | 9 | 5 | 0 | 1 (0.3) |
| i7. There are opportunities for privacy | 195 | 52 | 11 | 1 | 0 | 1 (0.3) |
| i8. I am notified when there is a change | 104 | 83 | 46 | 17 | 6 | 4 (1.5) |
| Completing tasks | ||||||
| i9. Asked to participate in the care | 21 | 60 | 62 | 60 | 51 | 6 (2.3) |
| i10. Agree with the staff | 52 | 80 | 55 | 35 | 29 | 9 (3.5) |
| i11. Discuss with the staff what tasks in the care I can be responsible for | 33 | 50 | 49 | 58 | 60 | 10 (3.8) |
| i12. Tasks the staff are responsible for | 94 | 82 | 58 | 15 | 7 | 4 (1.5) |
| i13. Opportunity to participate | 83 | 89 | 55 | 21 | 8 | 4 (1.5) |
| Being respected for one’s knowledge | ||||||
| i14. Ask me about my knowledge * | 34 | 60 | 71 | 42 | 44 | 9 (3.5) |
| i15. My knowledge is used * | 42 | 81 | 68 | 33 | 27 | 9 (3.5) |
| Being acknowledged as part of the care team | ||||||
| i16. I feel that I am respected | 80 | 86 | 50 | 22 | 16 | 6 (2.3) |
| i17. Being asked about my opinion * | 51 | 75 | 67 | 35 | 27 | 5 (1.9) |
| i18. Involved in decisions * | 56 | 91 | 58 | 33 | 19 | 5 (1.9) |
| I19. Agree on what to do * | 69 | 81 | 65 | 23 | 17 | 5 (1.9) |
| i20a. Formulate goals, symptom relief | 39 | 62 | 60 | 47 | 37 | 15 (5.8) |
| i20b. Formulate goals, nursing | 34 | 62 | 68 | 43 | 37 | 16 (6.1) |
| i20c. Formulate goals, termination of treatment | 32 | 50 | 55 | 50 | 46 | 27 (10.4) |
| i21. Happy with the influence I have * | 72 | 68 | 69 | 26 | 15 | 10 (3.8) |
| Relationship with the staff | ||||||
| i22. Staff are accommodating * | 161 | 72 | 23 | 3 | 0 | 1 (0.3) |
| i23. Interest in me as a person | 71 | 62 | 61 | 35 | 29 | 2 (0.7) |
| i24. Feelings can be expressed * | 95 | 93 | 44 | 16 | 5 | 7 (2.6) |
| i25. Criticism can be given * | 69 | 92 | 61 | 19 | 8 | 11 (4.2) |
| i26. Staff understand my situation * | 93 | 97 | 41 | 19 | 4 | 6 (2.3) |
| i27. Pleased with the contact * | 123 | 74 | 45 | 14 | 1 | 3 (1.1) |
| Trusting the staff | ||||||
| i28. Can maintain her/his identity | 86 | 86 | 50 | 22 | 10 | 6 (2.3) |
| i29a. Gets enough to eat * | 158 | 69 | 21 | 8 | 0 | 4 (1.5) |
| i29b. Gets enough to drink * | 147 | 78 | 21 | 7 | 1 | 6 (2.3) |
| i29c. Gets relief * | 104 | 94 | 45 | 8 | 1 | 8 (3.1) |
| i29d. Gets good care * | 131 | 86 | 27 | 7 | 1 | 8 (3.1) |
| i29e. Gets well approached * | 150 | 93 | 11 | 3 | 0 | 3 (1.1) |
| i30. Trust that he/she gets necessary care * | 120 | 84 | 44 | 7 | 1 | 4 (1.5) |
| i31. I do not need to ensure that my older relative receives the care he/she needs * | 116 | 80 | 38 | 12 | 7 | 7 (2.6) |
*Items inspired by the Family Collaboration Scale. Items are rephrased and response categories changed [46].
There were no significant age- or sex-related differences between those who did and did not fully complete the questionnaire.
Step 1. Dimensionality of the 37 items
EFA
EFA revealed that the 37 items could be divided into two factors. One was represented by 20 items covering communication and trust (CaT) and the second was represented by 17 items covering collaboration in care (CiC)(Table 2), in partial agreement with the hypothetical model (Fig 1). It is likely that the first factor (CaT) was a prerequisite for the second factor (CiC), such that the first factor contained items that are easy to affirm, and the second factor contained items that are difficult to attain, providing a so-called “difficulty factor solution”.
Table 2. Minimum rank factor analysis based on polychoric correlations and promin rotation (oblique, allows factors to correlate) to achieve factor simplicity (n = 211).
| Items (i) | Collaboration in care | Communication and trust |
|---|---|---|
| Conversations and information | ||
| i1. I feel well-informed | 0.313 | 0.556 |
| i2. Staff discuss my older relative’s care with me | 0.572 | 0.301 |
| i3. Information about how I can best help | 0.622 | |
| i4. Staff take time to talk with me | 0.608 | |
| i5. I can consult with the staff if I have questions or concerns | 0.712 | |
| i6. I can be at my older relative’s side when I want | 0.493 | |
| i7. There are opportunities for privacy | 0.631 | |
| i8. I am notified when there is a change | 0.569 | |
| Completing tasks | ||
| i9. Asked to participate in the care | 0.819 | |
| i10. Agree with the staff | 0.831 | |
| i11. Discuss with the staff what tasks in the care I can be responsible for | 0.958 | |
| i12. Tasks the staff are responsible for | 0.339 | |
| i13. Opportunity to participate | 0.708 | |
| Being respected for one’s knowledge | ||
| i14. Ask me about my knowledge | 0.848 | |
| i15. My knowledge is used | 0.846 | |
| Being acknowledged as part of the care team | ||
| i16. I feel that I am respected | 0.727 | |
| i17. Being asked about my opinion | 0.811 | |
| i18. Involved in decisions | 0.902 | |
| I19. Agree on what to do | 0.794 | |
| i20a. Formulate goals, symptom relief | 0.905 | |
| i20b. Formulate goals, nursing | 0.881 | |
| i20c. Formulate goals, termination of treatment | 0.909 | |
| i21. Happy with the influence I have | 0.669 | |
| Relationship with the staff | ||
| i22. Staff are accommodating | 0.735 | |
| i23. Interest in me as a person | 0.335 | 0.401 |
| i24. Feelings can be expressed | 0.550 | |
| i25. Criticism can be given | 0.570 | |
| i26. Staff understand my situation | 0.750 | |
| i27. Pleased with the contact | 0.757 | |
| Trusting the staff | ||
| i28. Can maintain her/his identity | 0.761 | |
| i29a. Gets enough to eat | 0.895 | |
| i29b. Gets enough to drink | -0.301 | 0.963 |
| i29c. Gets relief | 0.892 | |
| i29d. Gets good care | 0.989 | |
| i29e. Gets well approached | 0.966 | |
| i30. Trust that he/she gets necessary care | 0.931 | |
| i31. I do not need to ensure that my older relative receives the care he/she needs | 0.882 | |
| Eigenvalue | 19.59 | 3.71 |
| Proportion of common variance | 52.95 | 10.03 |
| Cumulative proportion of common variance | 52.95 | 62.97 |
Bartlett’s statistic = 7319.7 (p = 0.00001, should be p < 0.05]. Kaiser-Meyer-Olkin (KMO) test = 0.95445 (very good performance is represented by values > 0.5).
Step 2. Item reduction
Based on iterative conceptual considerations and RMA, items were deleted one at a time, for each factor separately. The main reason for considering item deletion was due to local dependency, and this was especially the case between items 20a–20c and 29a–29e. For the 17-item CaT (Q3,* = residual correlation (r) max 0.573 –r mean -0.045 = 0.618) and the 20-item CiC (Q3,* = r max 0.585 –r mean -0.058 = 0.643) there were considerable local dependency since Q3,* values were above Yen´s critical value of 0.24 (95th percentile)[56]. In a stepwise procedure, 11 items within the factor CaT and eight items within the factor CiC were deleted, leaving nine items in each scale.
Step 3. RMA of separate factors
Targeting and reliability
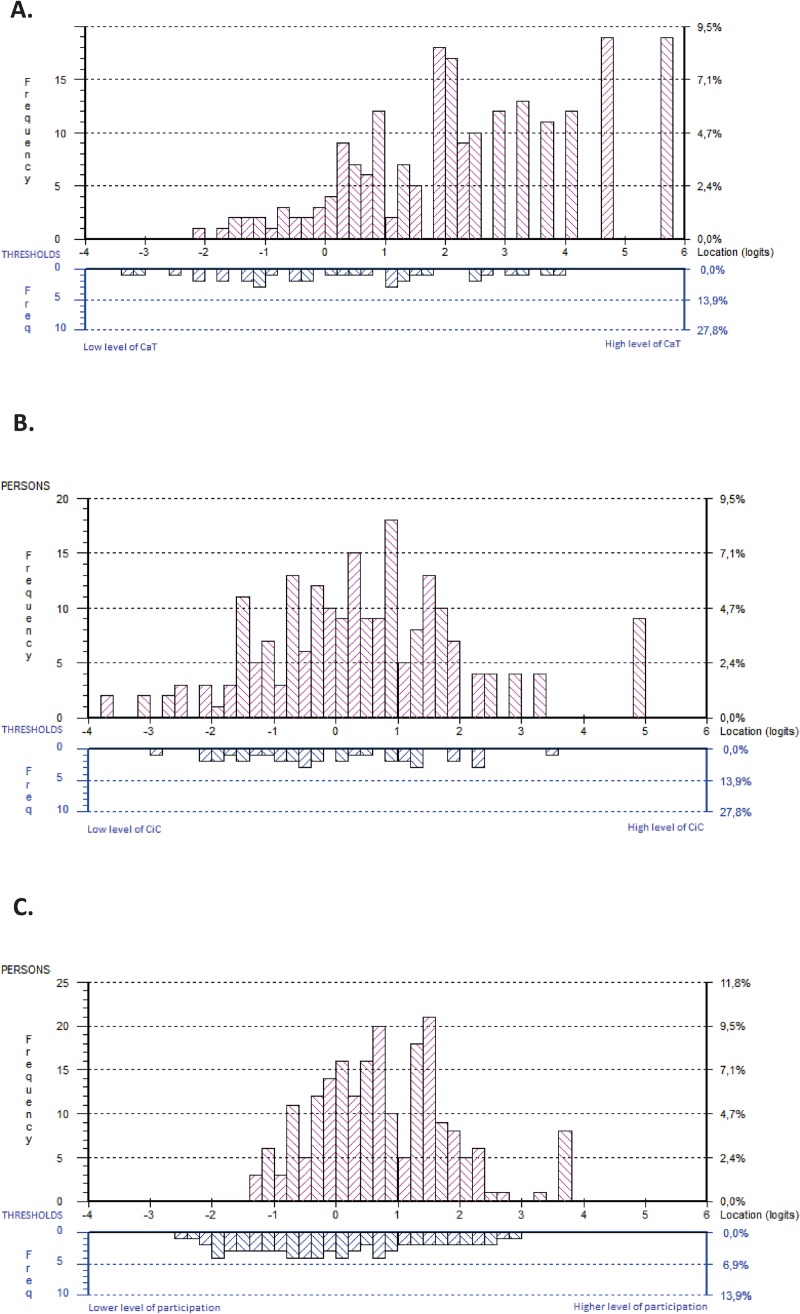
The person-item distribution of the 9-item CaT displayed a relatively even distribution of item thresholds between −3.5 and 4 logits from lower to higher levels, with no major gaps. The CaT was able to separate people along the continuum with a reliability (Person Separation Index, PSI) of 0.87, indicating that there were 3.7 detectable strata [66]. However, the CaT failed somewhat to represent higher levels of CaT (> 4 logits), where a substantial proportion of the sample was located. This means these people experienced a higher degree of CaT than the items captured. This was also illustrated by a mean person location of 2.384 (standard deviation 1.852) logits; that is, the sample reported CaT 2.717 logits, on average, above that represented by the CaT scale (Fig 3, Panel A).
Fig 3.
Distribution of next of kin (upper panel, n = 211) and the item category thresholds (lower panel), for Communication and Trust (CaT, Panel A), Collaboration in Care (CiC, Panel B), and Next of Kin Participation in Care subtests (NoK-PiC, Panel C) on the common logit metric (x-axis; positive values = higher level of CaT/CiC/NoK-PiC). Thresholds are locations at which there is a 50/50 probability of a response in either of two adjacent categories.
The person-item distribution of the 9-item CiC spanned approximately six logits from lower to higher levels of CiC, with no major gaps. The CiC was able to separate people along the continuum with a reliability (PSI) of 0.91, indicating that there were 4.5 detectable strata [66]. However, targeting of people was slightly compromised at the higher (> 3 logits) and lower (<-3 logits) ends of the CiC range of measurement. This finding indicates that the CiC, to a small extent, failed to represent lower and higher levels of CiC. The mean person location was 0.461 (standard deviation 1.663) logits (Fig 3, Panel B).
Model fit
Table 3 shows the fit of CaT item response data to the Rasch measurement model. Data were consistent with expectations, except for one item in the CaT scale that showed signs of multidimensionality (fit residual > 2.5: CaT i25 fit residual 2.736). In addition, one item in the CaT scale indicated local dependency (fit residual < −2.5: CaT i27 fit residual −2.787) (Table 3). Graphical inspection of the ICCs suggested that these misfits were relatively minor. The Q3,* for the CaT was 0.35 (r max 0.23 –r mean −0.11 = 0.35) and for CiC 0.36 (r max 0.24 –r mean −0.12 = 0.36) indicating that some local dependency still existed in the data, since Q3,* was above Yen’s critical value of 0.24 [56].
Table 3. “Communication and trust”, “collaboration in care” and subtests item-level Rasch locations and fit statistics.
| Location | Standard error | Fit residual | Chi-square | Probability | |
|---|---|---|---|---|---|
| Communication and trust, items (i) | |||||
| i22. Staff are accommodating | −2.202 | 0.135 | −1.240 | 7.269 | 0.0638 |
| i5. I can consult with the staff if I have questions or concerns | −0.637 | 0.119 | −0.645 | 2.668 | 0.4456 |
| i30. Trust that he/she gets necessary care | −0.373 | 0.120 | −0.742 | 3.068 | 0.3813 |
| i27. Pleased with the contact | −0.247 | 0.113 | −2.787 | 11.381 | 0.0098* |
| i8. I am notified when there is a change | 0.388 | 0.106 | 0.482 | 1.777 | 0.6199 |
| i4. Staff take time to talk with me | 0.532 | 0.110 | −0.508 | 3.419 | 0.3315 |
| i1. I feel well-informed | 0.807 | 0.110 | −0.470 | 2.855 | 0.4145 |
| i28. Can maintain her/his identity | 0.818 | 0.101 | 1.336 | 7.893 | 0.0483* |
| i25. Criticism can be given | 0.916 | 0.106 | 2.736 | 8.537 | 0.0361* |
| Collaboration in care, items (i) | |||||
| i13. Opportunity to participate | −1.001 | 0.097 | 1.133 | 6.484 | 0.0903 |
| i16. I feel that I am respected | −0.629 | 0.091 | −1.541 | 1.528 | 0.6758 |
| i21. Happy with the influence I have | −0.558 | 0.091 | −1.372 | 2.610 | 0.4557 |
| i18. Involved in decisions | −0.350 | 0.092 | −0.644 | 2.915 | 0.4049 |
| i17. Being asked about my opinion | −0.067 | 0.089 | −2.186 | 9.139 | 0.0275* |
| i3. Information about how I can best help | 0.409 | 0.089 | 2.373 | 2.911 | 0.4055 |
| i14. Ask me about my knowledge | 0.492 | 0.085 | 1.581 | 0.158 | 0.9841 |
| i11. Discuss with the staff what tasks in the care I can be responsible for | 0.788 | 0.083 | 1.041 | 1.082 | 0.7814 |
| i9. Asked to participate in the care | 0.916 | 0.089 | 0.804 | 3.058 | 0.3828 |
| Subtests | |||||
| Communication and trust | −0.163 | 0.028 | 0.670 | 0.707 | 0.8715 |
| Collaboration in care | 0.163 | 0.025 | −0.313 | 1.065 | 0.7856 |
*Not significant after Bonferroni adjustment
The overall item-trait interaction Chi square test-of-fit was significant for the CaT scale (p = 0.006) but not for the CiC scale (p = 0.319).
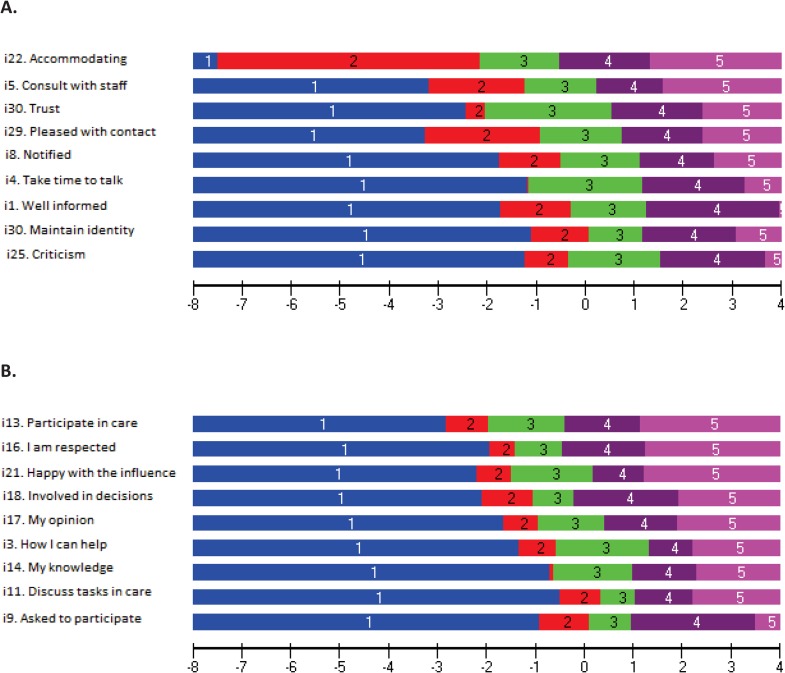
DIF and response category functioning
Regarding DIF, all items in the CaT and CiC scales performed similarly across different groups of individuals (i.e., regarding age and sex). Regarding response category functioning, assessment of the empirical functioning of the five response categories indicated that these worked as intended with all items within CaT (Fig 4, Panel A) and CiC (Fig 4, Panel B).
Fig 4. Response category functioning for each item.
Borders between the respective areas (colors) are logit threshold locations on the Communication and Trust (CaT, Panel A), and Collaboration in Care (CiC, Panel B) continuum (x-axis; positive values = higher level of CaT/CiC) where there is a 50/50 probability of responding in either of the adjacent response categories.
Hierarchical item ordering
Table 3 shows the empirical ordering of item locations from lower to higher levels of CaT, CiC and NoK-PiC. Inspection of the pattern of the hierarchical item ordering generally provided support for a priori expectations. In CaT, the “easiest” (less CaT/easy for care to achieve) was item 22 (staff are accommodating) and the most difficult was item 25 (criticism can be given) (Table 3). In CiC the “easiest” (less CiC/easy for care to achieve) was item 13 (opportunity to participate) and the most difficult was item 9 (asked to participate in the care) (Table 3).
Step 4. Subtest analysis
Since there were some local dependencies in the scales, it was feasible to conduct a subtest analysis in which the dependencies were absorbed by the subtest (i.e., into the response structure of the single ability estimate), and we were able to explore the use of a total score based on the two scales. The mean person location for the two subtests (i.e., the NoK-PiC subscales) was 0.774 (SD, 1.102), indicating that that the sample reported participation of 0.774 logits, on average, above that represented by the NoK-PiC scale (Fig 3, Panel C). The relative locations and fit statistics for the two subscales were acceptable and followed a pattern from the easiest dimension “CaT” to the more difficult to achieve dimension “CiC” (Table 2). There was no DIF by either age or gender.
The alpha, when analyzed as two subscales, was 0.92 (with extremes), and, when analyzed using 18 individual items, it was higher (alpha 0.95) due to local dependency in the item set. In addition, the C2-value (0.12) was low and the latent correlation among the two subscales (r = 0.89) was high. Most of the systematic variance was left as non-error common variance (A = 0.95). Thus, the subtest analysis gave a high value for both A and r, and a low value for C2, supporting an approximate unidimensional scale and thus justifying the use of a total score from the 18 items. The subtest overall test-of-fit (p = 0.939) was better than for the discrete 18 items (p = 0.0002).
Based on the results, a new model for participation was designed, considering the bifactor subscale structure after item reduction (Fig 5). Within each factor, the items from each hypothetical component were intertwined along a hierarchical structure from less participation (easier for care to achieve) to more participation (harder for care to achieve). Communication and trust tended to bridge the two factors, and these were prerequisites for participation in care (Fig 5).
Fig 5. Revised conceptualization and operationalization (20 items) of the next of Kin Participation in Care questionnaire.
Conversations and information are part of both CaT and CiC.
Step 5. Error of measurement and detectable difference
The possible score range was from 0 to 72 in the total scale (0 to 36 in each of the two scales). For the NoK-PiC total score the SEM was ± 3.8 (based on PSI 0.93). The minimal detectable difference (MDC95), that a person was required to show on a scale to ensure that the observed change in NoK-PiC score was real, and not just measurement error, was a score of 10.5. After transformation of the ordinal sum scores to interval scores, of the same range (0–72) as the original raw sum scores [64], the SEM and MDC95 were ± 2.1 and 5.8 respectively.
Step 6. Group comparisons, total scores (n = 211 available for analysis)
It was expected that people generally score higher on CaT than on CiC, since the first was expected to be easier to achieve than the second.
Older people (≥ 65 years) reported a higher degree of CaT and NoK-PiC than younger people (p = 0.001 and p = 0.023, respectively). People with a specific contact person experienced a higher degree of CaT, CiC and NoK-PiC than those without a contact person (p = 0.006; p = <0.001; and p = 0.001, respectively) (Table 4).
Table 4. Scale scores (interval-level scale of the same range as the original raw scores) for respondents (n = 259), comparison between men (n = 65) and women (n = 195); younger (n = 132) and older people (n = 120); and between those who had a contact person (n = 221) and those who did not (n = 32).
| Mean (standard deviation) | Median (q1–q3) | 95% confidence interval of the mean | P-value* | |
|---|---|---|---|---|
| Communication and trust | ||||
| All | 27.7 (4.8) | 27 (14–32) | 27.1–28.3 | – |
| Sex | 0.407 | |||
| Male | 28.0 (3.8) | 27 (26–31) | 27.0–29.0 | |
| Female | 27.6 (5.1) | 27 (24–32) | 26.8–28.3 | |
| Age group | 0.001 | |||
| <65 years | 26.8 (4.7) | 27 (24–30) | 25.9–27.6 | |
| ≥65 years | 28.8 (4.9) | 29 (25–34) | 27.8–29.7 | |
| Has contact person | 0.006 | |||
| Yes | 28.1 (4.6) | 27 (25–32) | 27.4–28.7 | |
| No | 25.5 (5.6) | 24 (22–30) | 23.2–27.2 | |
| Collaboration in care | ||||
| All | 18.9 (6.4) | 19 (15–23) | 18.9–19.8 | - |
| Sex | 0.362 | |||
| Male | 18.2 (5.2) | 18 (15–21) | 17.0–19.7 | |
| Female | 19.1 (6.7) | 19 (15–23) | 18.1–20.2 | |
| Age group | 0.053 | |||
| < 65 years | 18.2 (6.6) | 18 (13–22) | 17.0–19.5 | |
| ≥ 65 years | 19.8 (6.3) | 19 (16–23) | 18.6–21.0 | |
| Has contact person | <0.001 | |||
| Yes | 19.4 (6.3) | 19 (16–23) | 18.6–20.3 | |
| No | 15.2 (6.0) | 14 (11–20) | 13.0–17.5 | |
| NoK-PiC | ||||
| All | 48.9 (8.0) | 48 (44–52) | 47.8–49.9 | – |
| Sex | 0.673 | |||
| Male | 48.5 (5.7) | 48 (44–51) | 47.0–50.0 | |
| Female | 49.0 (8.6) | 48 (44–53) | 47.7–50.3 | |
| Age group | 0.027 | |||
| < 65 years | 47.8 (8.1) | 47 (43–52) | 46.3–49.3 | |
| ≥ 65 years | 50.2 (8.0) | 49 (45–54) | 48.7–51.7 | |
| Has contact person | 0.001 | |||
| Yes | 49.5 (7.8) | 48 (45–53) | 48.4–50.6 | |
| No | 44.1 (7.4) | 43 (38–50) | 41.4–46.9 |
* T-test
Discussion
Participation in care was found to include two constructs: CaT and CiC, where the former was a prerequisite for the latter. Next of kin’s participation in the care of older people has several benefits, and from the next of kin’s perspective, it has been reported to increase the experience of good quality of care [67]. The two subscales, as well as the total scale, developed in the present study can be used to evaluate implementation of an intervention aiming at increasing next of kin’s participation in care. It should be noted that not all older people are comfortable with, or wish for, their next of kin to participate in their care. It is therefore important that nursing home personnel are responsive and respectful toward the older person’s wishes.
We identified several prerequisites for participation, as follows: trusting the staff, staff being present, conversations and information, having a good relationship with the staff, being invited to complete tasks, being respected for one’s knowledge, and being acknowledged as part of the care team. These components of participation could be grouped into CaT and CiC. Participation can be understood from the perspective of a study by Andershed and Ternestedt [33] reporting that next of kin’s involvement in palliative care can be classified into three categories: “to know,” “to be”, and “to do.” To know means the next of kin receiving information from staff about the patient, which is not only a way to be involved, but also a prerequisite for involvement. To be means being present in the patient’s life in different ways. To do represents a more task-oriented way of being involved. Thus, “to know” is something that can be captured by the CaT scale while “to do” and “to be” can be captured by the CiC scale.
Our assumption, which was confirmed by the current results, is that a prerequisite for next of kin to participate in care is that the staff mediate good communication and trust. Satisfying this prerequisite should make it easier to achieve high scores on the CaT scale than on the CiC scale, which was also shown in the results (Table 4). This assumption is confirmed by other studies concluding that the highest level of participation arises when the next of kin, older person, and staff are part of a “partnership” [46], similar to the content in the CiC scale. Furthermore, a high level of collaboration between relatives of older patients and nurses is reported to be significantly related to a high level of satisfaction with the care, at least in a hospital context [43]. Relationships between staff and next of kin can be influenced by the needs of the next of kin to receive initial orientation, then ongoing information regarding the nursing home, aging and disease processes, and care issues [68]. Participating in care should be voluntary for next of kin. While the CaT scale measures prerequisites for participation, the CiC scale measures collaboration, involving more action from the next of kin’s perspective. As next of kin’s role in care should be voluntary, it can also be difficult for care to achieve high scores on this scale. Andershed and Ternestedt [46] reported that when the next of kin receive information, they develop insight that can help them decide how they wish to participate in the care. They also mentioned that the possibility of participating in a way that is experienced as meaningful for the next of kin increases if the next of kin have the opportunity to choose. Hence, first, when next of kin are informed about their opportunities, they can decide whether they wish to participate more actively. Similarly to the CiC domain, a previous study [43] reported that it was more difficult to achieve shared decision making, exchange of knowledge, and agreement on definition of the situation according to the FCS than it was to achieve prerequisites for collaboration, similar to the CaT domain (i.e., contact, communication and relationship qualities). One factor that should be taken into consideration when evaluating participation is that collaboration occurs between individuals, rather than organizations [7]. Thus, collaboration is potentially more difficult to improve via interventions. The nursing home can take a supportive approach toward collaboration, but respect and trust, as critical factors for collaboration, can only develop between the next of kin and the staff. The CaT scale can be used to evaluate the prerequisites for participation and the CiC scale to explore participation that is more difficult to achieve.
The developed NoK-PiC scale focused on participation in the nursing home context, while, for instance, the FCS was developed for the hospital context. Even if many aspects of participation are similar between the two contexts, there are others that are not similar, such as the length of stay. Unlike acute care facilities, opportunities for next of kin’s involvement in care in nursing homes occur over a longer time period. In addition, to be perceived as relevant, questions need to be adapted to specific care contexts. The FCS focuses on the process (i.e., before admission, during the stay and after discharge), making several questions irrelevant for the purpose of studying participation in nursing homes. Nevertheless, it appears to be feasible to consider the FCS [44] when developing the NoK-PiC, and, correspondingly, 11 items in the final version of the NoK-PiC were inspired by the FSC. Another instrument, developed for use in psychiatric contexts, is the 28-item Family Involvement and Alienation Questionnaire (FIAQ) [69]. The FIAQ examines family members’ experiences of healthcare professionals’ approach and possible feelings of alienation among family members regarding professional care services [69]. At the time of conducting this study, the FIAQ was only developed for, and tested in the context of psychiatric care, not elderly care. However, more recently, FIAQ was found to be feasible for use not only in psychiatric care, but also in palliative care and diabetes care [70]. In any case, both the FCS and the FIAQ have been developed and tested using classical test theory, not the more robust RMA that was conducted in the current study.
Targeting in the CaT scale was compromised among people experiencing a high level of participation. This is a relatively common problem for this type of measure. For example, in a study of person-centered care (in which participation in care is an underlying concept) in nurse-led outpatient rheumatology clinics, there was also poor targeting of the scale for those experiencing higher levels of person-centered care [71]. If the goal is to examine people experiencing a very high level of participation in greater detail, with less error, it may be necessary to add more items at the end of the scale. However, both scales were able to capture lower levels of participation relatively effectively. On the other hand, mistargeting of the CaT scale is not necessarily a limitation of the scale, as it suggest that this sample had high levels of CaT, which is exactly what would be desired. Due to local dependency among items within the individual CaT and CiC scales users should be cautious of their interpretation of the subscale scores, conclusions may overestimate the validity of the scales. The bifactor model appears to offer a good solution to account for the remaining dependency, but this model is slightly different from the individual scales, as it is based only on what is common between the two individual scales (indicated by high values for r = 0.89 and A = 0.95). In addition, the total 18-item NoK-PiC scale showed better targeting than the separate subscales did, as expected.
One strength of the present study is that the instruments were conceptually based on a literature review (including qualitative research focusing on relatives’ “lived experience” of collaboration) as well as discussion among the researchers, and face validity was tested. Even though, it can be considered a limitation that there was no direct involvement of next of kin in the item generation or concept elicitation stages. It is a strength of the current study that the two instruments were developed based on findings from both FA and RMA. Thus, dimensionality was thoroughly explored in addition to how items and their response categories function. Furthermore, in each of the scales, the hierarchal order of the items from less to more participation by means of both communication and trust, as well as collaboration in care, is now known. The sample size also ensured robust fit interpretations from the RMA.
To the best of our knowledge, this is the first specifically developed instrument for measuring next of kin’s participation in care in nursing homes. This instrument is a promising tool that can contribute to strengthening care as a collaborative process in the triad consisting of an older person, next of kin, and staff members. It is essential that the older person provides consent before the next of kin’s participation in his or her care, and that the older person has an opportunity to participate in a collaborative process. However, a systematic review by Haesler et al. [72] reported that staff expressed an overall interest and support for collaboration with next of kin, but did not apply these beliefs and understanding in clinical practice. Several barriers to implementing involvement of next of kin have been identified, including task-oriented care instead of family-focused care, insufficient communication skills, power and control issues, high workload, and limited staffing, as well as low managerial support [68]. The development of valid instruments for measuring the effectiveness of interventions with the purpose of improving participation is therefore an urgent research issue. In future studies it could be worthwhile to analyze differential item functioning for the older peoples’ length of stay, and the potential difference in subscales and total scores reported.
Conclusions
The present results provide support for use of the NoK-PiC scale and its two subscales, including seven subject areas, for measuring next of kin’s participation in the care of older people in nursing homes. The NoK-PiC consists of two dimensions, exhibiting a bifactorial structure: CaT, expressing preconditions for collaboration in care, and CiC, expressing the meaning and tasks of participation. The scales exhibited satisfactory psychometric properties. Each can be used separately or together, depending on the context for the intervention, aiming to increase the next of kin’s participation. Additional research is needed to evaluate the scales’ ability to effectively detect changes after intervention.
Acknowledgments
We thank the researchers who participated in the data collection; Birgitta Wallerstedt, Ph.D., RN; Helene Åvik Persson, a Ph.D. student and PHN; and research assistant Anne Molina Tall, RN. We would also like to acknowledge the cooperation provided by Professor Birgit Rasmussen, Lund University. Additionally, we thank Adam Goulston, MS, ELS, and Benjamin Knight, MSc, from Edanz Group (www.edanzediting.com/ac) for editing a draft of this manuscript.
Data Availability
Data are available from the Swedish National Data Service (https://snd.gu.se/en/catalogue/study/snd1135), and upon request from the first author.
Funding Statement
This study is part of the KUPA project and is funded by the Swedish Research Council (grant number 2014-2759); Vårdal Foundation (grant number 2014-0071); Medical Faculty, Lund University; The Faculty of Health and Life Sciences, Linnaeus University; The City of Lund. An additional grant from the Foundation of Hedda Andersson, Lund University, made this study possible. The authors declare no conflict of interest and that the grant sponsors had no role in the study design; data collection, analyses, or interpretation; writing of the manuscript; or decision to publish the results.
References
- 1.Andershed B. Relatives in end‐of‐life care–part 1: A systematic review of the literature the five last years, January 1999–February 2004. Journal of clinical nursing. 2006;15(9):1158–69. 10.1111/j.1365-2702.2006.01473.x [DOI] [PubMed] [Google Scholar]
- 2.Szebehely M, Meagher G. Nordic eldercare–weak universalism becoming weaker? Journal of European Social Policy. 2018;28(3):294–308. [Google Scholar]
- 3.Geerlings SW, Pot AM, Twisk JW, Deeg DJ. Predicting transitions in the use of informal and professional care by older adults. Ageing & Society. 2005;25(1):111–30. [Google Scholar]
- 4.Norlyk A, Martinsen B. The extended arm of health professionals? Relatives' experiences of patient's recovery in a fast‐track programme. Journal of advanced nursing. 2013;69(8):1737–46. 10.1111/jan.12034 [DOI] [PubMed] [Google Scholar]
- 5.Nolan M, Lundh U, Grant G, Keady J. Partnerships in Family Care: understanding the caregiving career Philadelphia: Open University Press; 2003. [Google Scholar]
- 6.Berglund A. L. Satisfaction with caring and living conditions in nursing homes: Views of elderly persons, next of kin and staff members. International Journal of Nursing Practice. 2007;13(1), 46–51. 10.1111/j.1440-172X.2006.00602.x [DOI] [PubMed] [Google Scholar]
- 7.Henneman EA, Lee JL, Cohen JI. Collaboration: a concept analysis. Journal of advanced nursing. 1995;21(1):103–9. 10.1046/j.1365-2648.1995.21010103.x [DOI] [PubMed] [Google Scholar]
- 8.Gallant MH, Beaulieu MC, Carnevale FA. Partnership: an analysis of the concept within the nurse–client relationship. Journal of advanced nursing. 2002;40(2):149–57. 10.1046/j.1365-2648.2002.02357.x [DOI] [PubMed] [Google Scholar]
- 9.Ward-Griffin C, McKeever P. Relationships between nurses and family caregivers: partners in care? Advances in Nursing Science. 2000;22(3):89–103. 10.1097/00012272-200003000-00008 [DOI] [PubMed] [Google Scholar]
- 10.Walker E, Jane Dewar B. How do we facilitate carers’ involvement in decision making? Journal of advanced nursing. 2001;34(3):329–37. 10.1046/j.1365-2648.2001.01762.x [DOI] [PubMed] [Google Scholar]
- 11.Lindhardt T, Hallberg IR, Poulsen I. Nurses’ experience of collaboration with relatives of frail elderly patients in acute hospital wards: a qualitative study. International journal of nursing studies. 2008;45(5):668–81. 10.1016/j.ijnurstu.2007.01.010 [DOI] [PubMed] [Google Scholar]
- 12.Berthelsen CB, Lindhardt T, Frederiksen K. Inhibiting Interference—a grounded theory of health professionals' pattern of behaviour related to the relatives of older patients in fast-track treatment programmes. Scandinavian journal of caring sciences. 2014;28(3):609–17. 10.1111/scs.12126 [DOI] [PubMed] [Google Scholar]
- 13.Åstedt‐Kurki P, Paavilainen E, Tammentie T, Paunonen‐Ilmonen M. Interaction between adult patients’ family members and nursing staff on a hospital ward. Scandinavian journal of caring sciences. 2001;15(2):142–50. 10.1046/j.1471-6712.2001.00012.x [DOI] [PubMed] [Google Scholar]
- 14.Nyborg I, Danbolt LJ, Kirkevold M. Few opportunities to influence decisions regarding the care and treatment of an older hospitalized family member: a qualitative study among family members. BMC health services research. 2017;17:1–12. 10.1186/s12913-016-1943-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.The National Board of Health and Welfare. Dödsorsaker 2013 –Causes of Death 2013: Socialstyrelsen; 2014 [cited 6 october 2017]. Available from: http://www.socialstyrelsen.se/Lists/Artikelkatalog/Attachments/19736/2015-2-42.pdf.
- 16.Quine S, Morrell S. Fear of loss of independence and nursing home admission in older Australians. Health & social care in the community. 2007;15(3):212–20. [DOI] [PubMed] [Google Scholar]
- 17.Wilson SA. The transition to nursing home life: A comparison of planned and unplanned admissions. Journal of advanced nursing. 1997;26(5):864–71. 10.1046/j.1365-2648.1997.00636.x [DOI] [PubMed] [Google Scholar]
- 18.Ericson-Lidman E, Renström A-S, Åhlin J, Strandberg G. Relatives' perceptions of residents' life in a municipal care facility for older people with a focus on quality of life and care environment. 2015;10(3):160–9. 10.1111/opn.12063 [DOI] [PubMed] [Google Scholar]
- 19.Eika M, Espnes GA, Soderhamn O, Hvalvik S. Experiences faced by next of kin during their older family members' transition into long-term care in a Norwegian nursing home. J Clin Nurs. 2014;23(15–16):2186–95. 10.1111/jocn.12491 [DOI] [PubMed] [Google Scholar]
- 20.Haggstrom E, Kihlgren A, Kihlgren M, Sorlie V. Relatives' struggle for an improved and more just care for older people in community care. J Clin Nurs. 2007;16(9):1749–57. 10.1111/j.1365-2702.2007.01704.x [DOI] [PubMed] [Google Scholar]
- 21.Whitaker A. Family involvement in the institutional eldercare context. Towards a new understanding. Journal of aging studies. 2009;23(3):158–67. [Google Scholar]
- 22.Koplow SM, Gallo AM, Knafl KA, Vincent C, Paun O, Gruss V. Family Caregivers Define and Manage the Nursing Home Placement Process. Journal of Family Nursing. 2015;21(3):469–93. 10.1177/1074840715571365 [DOI] [PubMed] [Google Scholar]
- 23.Andersson M, Ekwall AK, Hallberg IR, Edberg AK. The experience of being next of kin to an older person in the last phase of life. Palliative & supportive care. 2010;8(1):17–26. [DOI] [PubMed] [Google Scholar]
- 24.Andershed B, Ternestedt B-M. Being a close relative of a dying person: development of the concepts “Involvement in the light and in the dark”. Cancer nursing. 2000;23(2):151–9. 10.1097/00002820-200004000-00012 [DOI] [PubMed] [Google Scholar]
- 25.Hall S, Petkova H, Tsouros Agis D, Costantini M, Higginson I. Palliative care for older people: Better practices. World Health Organization Regional Office for Europe. 2011. Available from: https://apps.who.int/iris/bitstream/handle/10665/107290/e95052.pdf Cited 10 January 2019. [Google Scholar]
- 26.Smedbäck J, Öhlén J, Årestedt K, Alvariza A, Fürst C-J, Håkanson C. Palliative care during the final week of life of older people in nursing homes: A register-based study. Palliative and Supportive Care. 2017;15(4):417–24. 10.1017/S1478951516000948 [DOI] [PubMed] [Google Scholar]
- 27.Martinsson L, Lundström S, Sundelöf J. Quality of end-of-life care in patients with dementia compared to patients with cancer: A population-based register study. PloS one. 2018;13(7):e0201051–e. 10.1371/journal.pone.0201051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ahlström G, Nilsen P, Benzein E, Behm L, Wallerstedt B, Persson M, et al. Implementation of knowledge-based palliative care in nursing homes and pre-post post evaluation by cross-over design: a study protocol. BMC palliative care. 2018;17(1):52 10.1186/s12904-018-0308-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wallerstedt B, Behm L, Alftberg Å, Sandgren A, Benzein E, Nilsen P, et al. Striking a Balance: A Qualitative Study of Next of Kin Participation in the Care of Older Persons in Nursing Homes in Sweden. Healthcare. 2018;6(2):46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ekström K, Spelmans S, Ahlström G, Nilsen P, Alftberg Å, Wallerstedt B, et al. Next of kin's perceptions of the meaning of participation in the care of older persons in nursing homes: a phenomenographic study. Scandinavian journal of caring sciences. 2019. January 3 10.1111/scs.12636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lau WY, Shyu YI, Lin LC, Yang PS. Institutionalized elders with dementia: collaboration between family caregivers and nursing home staff in Taiwan. J Clin Nurs. 2008;17(4):482–90. 10.1111/j.1365-2702.2007.01955.x [DOI] [PubMed] [Google Scholar]
- 32.Davies S, Nolan M. 'Making it better': self-perceived roles of family caregivers of older people living in care homes: a qualitative study. International journal of nursing studies. 2006;43(3):281–91. 10.1016/j.ijnurstu.2005.04.009 [DOI] [PubMed] [Google Scholar]
- 33.Andershed B, Ternestedt BM. Involvement of relatives in care of the dying in different care cultures: development of a theoretical understanding. Nursing science quarterly. 1999;12(1):45–51. 10.1177/08943189922106404 [DOI] [PubMed] [Google Scholar]
- 34.Janzen W. Long-term care for older adults. The role of the family. Journal of gerontological nursing. 2001;27(2):36–43. 10.3928/0098-9134-20010201-13 [DOI] [PubMed] [Google Scholar]
- 35.Hertzberg A, Ekman SL. 'We, not them and us?' Views on the relationships and interactions between staff and relatives of older people permanently living in nursing homes. Journal of advanced nursing. 2000;31(3):614–22. 10.1046/j.1365-2648.2000.01317.x [DOI] [PubMed] [Google Scholar]
- 36.Duncan MT, Morgan DL. Sharing the caring: family caregivers' views of their relationships with nursing home staff. The Gerontologist. 1994;34(2):235–44. 10.1093/geront/34.2.235 [DOI] [PubMed] [Google Scholar]
- 37.Wetle T, Shield R, Teno J, Miller SC, Welch L. Family perspectives on end-of-life care experiences in nursing homes. The Gerontologist. 2005;45(5):642–50. 10.1093/geront/45.5.642 [DOI] [PubMed] [Google Scholar]
- 38.Looman WJ, Noelker LS, Schur D, Whitlatch CJ, Ejaz FK. Nursing assistants caring for dementia residents in nursing homes: The family's perspective on the high quality of care. American Journal of Alzheimer's Disease. 1997;12(5):221–6. [Google Scholar]
- 39.Bowers BJ. Family perceptions of care in a nursing home. The Gerontologist. 1988;28(3):361–8. 10.1093/geront/28.3.361 [DOI] [PubMed] [Google Scholar]
- 40.Swedish institute. Elderly care in Sweden. 2013–2019. [cited 2019 6 January]. Available from: https://sweden.se/society/elderly-care-in-sweden/. [Google Scholar]
- 41.The Swedish goverment. Social service act (2001: 453). 2001. June 07 [cited 10 March 2019]. Available from: http://www.riksdagen.se/sv/dokument-lagar/dokument/svensk-forfattningssamling/socialtjanstlag-2001453_sfs-2001-453 [Google Scholar]
- 42.National Board of Health and Welfare. Nursing and elderly care: Status report 2019. (In Swedish: Vård och omsorg om äldre: Lägesrapport 2019). 2019. March 18 [cited 10 May 2019]. Availible from: http://www.socialstyrelsen.se/Lists/Artikelkatalog/Attachments/21265/2019-3-18.pdf [Google Scholar]
- 43.Lindhardt T, Nyberg P, Hallberg IR. Relatives’ view on collaboration with nurses in acute wards: Development and testing of a new measure. International journal of nursing studies. 2008;45(9):1329–43. 10.1016/j.ijnurstu.2007.10.006 [DOI] [PubMed] [Google Scholar]
- 44.Lindhardt T. Collaboration between relatives of frail elderly patients and nurses in acute hospital wards. Dimensions, prerequisites and outcome. P.h.D. Thesis, Lund University. 2007. Availible from: https://lup.lub.lu.se/search/ws/files/4853485/548142.pdf
- 45.Lindhardt T, Hallberg IR, Bolmsjö I. Standing Guard–Being a relative to a hospitalised elderly person. Journal of Aging Studies. 2008;20(2):133–149. [Google Scholar]
- 46.Andershed B, Ternestedt B-M. Development of a theoretical framework describing relatives’ involvement in palliative care. Journal of advanced nursing. 2001;34(4):554–62. 10.1046/j.1365-2648.2001.01785.x [DOI] [PubMed] [Google Scholar]
- 47.Hagell P, Westergren A. Sample Size and Statistical Conclusions from Tests of Fit to the Rasch Model According to the Rasch Unidimensional Measurement Model (Rumm) Program in Health Outcome Measurement. Journal of applied measurement. 2016;17(4):416–31. [PubMed] [Google Scholar]
- 48.Baglin J. Improving your exploratory factor analysis for ordinal data: A demonstration using FACTOR. Practical Assessment, Research & Evaluation. 2014;19(5):2. [Google Scholar]
- 49.Gadermann AM, Guhn M, Zumbo BD. Estimating ordinal reliability for Likert-type and ordinal item response data: A conceptual, empirical, and practical guide. Practical Assessment, Research & Evaluation. 2012;17(3):1–13. [Google Scholar]
- 50.Lorenzo-Seva U, Ferrando PJ. FACTOR: A computer program to fit the exploratory factor analysis model. Behavior research methods. 2006;38(1):88–91. 10.3758/bf03192753 [DOI] [PubMed] [Google Scholar]
- 51.Hair JF, Anderson RE, Tatham RL, Black WC. Multivariate data analysis 5th ed. Upper Saddle River: Prentice Hall; 1998. [Google Scholar]
- 52.Andrich D, Sheridan B, Luo G. RUMM2030: Rasch unidimensional models for measurement Perth, Western Australia: RUMM Laboratory; 2002. [Google Scholar]
- 53.Andrich D, Sheridan B, Luo G. Interpreting Rumm. Perth, RUMM Laboratory Pty; 2004. [Google Scholar]
- 54.Hobart J, Cano S. Improving the evaluation of therapeutic interventions in multiple sclerosis: the role of new psychometric methods. Health Technology Assessment 2009;13(12). 10.3310/hta13120 [DOI] [PubMed] [Google Scholar]
- 55.Marais I. Local Dependence In: Christensen K, Kreiner S, Mesbah M (eds) Rasch Models in Health. John Wiley & Sons, Inc.; 2013. [Google Scholar]
- 56.Christensen KB, Makransky G, Horton M. Critical Values for Yen’s Q3: Identification of Local Dependence in the Rasch Model Using Residual Correlations. Applied Psychological Measurement. 2017;41(3):178–194. 10.1177/0146621616677520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rasch G. Studies in mathematical psychology In: Probabilistic models for some intelligence and attainment tests. Oxford, England: Nielsen & Lydiche; 1960. [Google Scholar]
- 58.Andrich D. Rasch models for measurement California: Sage Publications; 1988. [Google Scholar]
- 59.Andrich D. Components of variance of scales with a bifactor subscale structure from two calculations of alpha. Education Measurement: Issue and Practice 2016; 35:25–30. [Google Scholar]
- 60.Guttersrud O, Naigaga MD, Pettersen KS (2015) Measuring Maternal Health Literacy in Adolescents Attending Antenatal Care in Uganda: Exploring the Dimensionality of the Health Literacy Concept Studying a Composite Scale. Journal of nursing measurement 2015;23(2):50E–66. 10.1891/1061-3749.23.2.E50 [DOI] [PubMed] [Google Scholar]
- 61.Andrich D. Interpreting RUMM2030 Part IV: Multidimensionality and Subtests in RUMM. RUMM Laboratory, Perth, Western Australia; 2013. [Google Scholar]
- 62.Tighe J, McManus IC, Dewhurst NG, Chis L, Mucklow J. The standard error of measurement is a more appropriate measure of quality for postgraduate medical assessments than is reliability: an analysis of MRCP(UK) examinations. BMC Med Educ. 2010; 10:40 10.1186/1472-6920-10-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Donoghue D, Stokes EK. How much change is true change? The minimum detectable change of the Berg Balance Scale in elderly people. J Rehabil Med. 2009;41(5):343–6. 10.2340/16501977-0337 [DOI] [PubMed] [Google Scholar]
- 64.Smith EV. Metric development and score reporting in Rasch measurement. Journal of Applied Measurement. 2000;1(3):303–326. [PubMed] [Google Scholar]
- 65.World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. 1. JAMA. 2013;27;310(20):2191–4. 10.1001/jama.2013.281053 [DOI] [PubMed] [Google Scholar]
- 66.Wright B, Masters G. Rating scale analysis Mesa Press, Chicago; 1982. [Google Scholar]
- 67.Magnusson L, Hansson E, Skoglund AL, Ilett R, Sennemark E, Barbabella F, et al. Kvalitet i äldreomsorg ur ett anhörigperspektiv (in Swedish). Nationellt kompetenscentrum anhöriga. 2016. Avalible from: https://www.anhoriga.se/Global/St%C3%B6d%20och%20kunskap/Publicerat/Rapporter/Dokument/Underlagsrapport%20S201503_web.pdf Cited 10 May 2019. [Google Scholar]
- 68.Haesler E, Bauer M, Nay R. Recent evidence on the development and maintenance of constructive staff–family relationships in the care of older people–a report on a systematic review update. International Journal of Evidence‐Based Healthcare. 2010;8(2):45–74. 10.1111/j.1744-1609.2010.00165.x [DOI] [PubMed] [Google Scholar]
- 69.Ewertzon M, Lutzen K, Svensson E, Andershed B. Developing the concept of family involvement and the alienation questionnaire in the context of psychiatric care. International Journal of Mental Health Nursing. 2008;17(6):439–49. 10.1111/j.1447-0349.2008.00570.x [DOI] [PubMed] [Google Scholar]
- 70.Ewertzon M, Alvariza A, Winnberg E, Leksell J, Andershed B, Goliath I, et al. Adaptation and evaluation of the Family Involvement and Alienation Questionnaire for use in the care of older people, psychiatric care, palliative care and diabetes care. Journal of Advanced Nursing. 2018; 74(8):1839–1850. [DOI] [PubMed] [Google Scholar]
- 71.Bala SV, Forslind K, Fridlund B, Hagell P. Measuring person‐centred care in nurse‐led outpatient rheumatology clinics. Musculoskeletal care. 2018;16(2):296–304. 10.1002/msc.1234 [DOI] [PubMed] [Google Scholar]
- 72.Haesler E, Bauer M, Nay R, Reports I. Constructive staff-family relationships in the care of older adults in the institutional setting: A systematic review. JBI Libr Syst Rev. 2004;2(10):1–76. 10.11124/01938924-200402100-00001 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available from the Swedish National Data Service (https://snd.gu.se/en/catalogue/study/snd1135), and upon request from the first author.