Highlights
-
•
Attendance to cervical cancer screening is related to gender identity development.
-
•
Provider attitudes are critical to improving cancer screening for transgender men.
-
•
Healthcare public physical spaces can promote cancer screening for transgender men.
Keywords: Cervical neoplasm, Cancer screening, Transgender persons, Gender identity, Qualitative research
Abstract
Lack of attendance to cervical cancer screening (CCS) services is the most attributable factor to the development of cervical cancer. Transgender men, individuals whose gender identity does match with their natal female sex, use CCS less often than the general female population. The underlying reasons for deficient CCS among transgender men relate mostly to their stigmatized identity, such as discrimination and unwelcoming healthcare environments. However, additional research is needed to expand our understanding of this complex issue. This exploratory qualitative research study aimed to identify the determinants of CCS from the perspective of transgender men. Twenty transgender men ages 21–65 were conveniently sampled to participate in a semi-structured interview in 2018. The data were analyzed using a deductive-inductive content analysis approach and the results were sorted into a socioecological framework (SEM). The participants were mostly non-Hispanic and white. The mean age was 33, and 55% of the sample had attended CCS in the last three years. Eight overarching factors were identified in the data. Each factor included descriptive sub-factors. At the institutional and interpersonal SEM levels, factors related to healthcare providers and healthcare organizations. At the individual level, factors related to past negative experiences, gender identity development, and socioeconomic status. To the investigators’ knowledge, this is the first study to report the relationship between gender identity development and CCS behaviors. Gender identity development refers to the transition or coming-out process and gender dysphoria. This suggests that attendance to CCS services change as a transgender person’s identity evolves.
1. Introduction
Although cervical cancer (CC) is one of the most understood and preventable cancers, over 13,000 people will be diagnosed and 4000 people will die from this cancer in the United States this year (American Cancer Society, 2019). Most of these cases will occur among people who do not attend regular cervical cancer screening (CCS), which is recommended once every 3 years in people with a cervix between the age of 21 and 65 (U.S. Preventive Services Task Force, 2019). Because lack of screening is the most common attribution to the development of CC (Leyden et al., 2005), studying sub-populations known to underuse CCS is important to reducing CC rates.
Transgender men (TM) are one such sub-population that has low rates of CCS. TM are individuals whose gender identity does not match with their natal female sex. For the purposes of this paper, TM is an umbrella term that refers to any natal female sex person who identifies with a different gender. TM use CCS less often than the general female population as well as cisgender sexual minority women, non-transgender women who identify with a sexual orientation other than heterosexual (Johnson et al., 2016a, Kiran et al., 2019, Peitzmeier et al., 2014). Factors found to influence receipt of healthcare services and CCS among TM include misperceptions of CC risks (Potter et al., 2015), stigma (Poteat et al., 2013, Reisner et al., 2013), lack of health insurance (Grant et al., 2011, Johnson et al., 2016a), embarrassment (Potter et al., 2015), disclosure of gender identity (Poteat et al., 2013), and gender dysphoria (Johnson et al., 2016b). Most of those studies examined healthcare services and did not focus solely on CCS. Additionally, most CCS research sampled both sexual minority women and TM. Given those gaps, this study aimed to identify the determinants of CCS of TM.
1.1. Theoretical framework
The socioecological model (SEM) (McLeroy et al., 1988) posits that individual health is influenced by factors at different levels. The SEM is useful in shifting from the traditional viewpoint of individuals and their immediate environment to acknowledging the broader multiple levels of influence (Fleury and Lee, 2006). Health disparities among lesbian, gay, bisexual, and transgender (LGBT) individuals are rooted in stigma, which permeates every level. Thus, the SEM model is salient to LGBT health disparities research and has been used extensively (Institute of Medicine, 2011). It is important to note that although the term LGBT is used throughout this paper, sexual orientation should not be conflated with gender identity. They are separate and unrelated identities but are commonly grouped together. The SEMs emphasis on the spheres of influences among families, communities, and society is especially useful for studying complex issues (Institute of Medicine, 2011), such as CCS among TM. For this study, the SEM was used to partly guide the development of interview questions and data analysis and to contextualize the themes.
2. Design and methods
This qualitative study used an exploratory design and a deductive-inductive content analysis approach. The Consolidated Criteria for Reporting Qualitative Research (Tong et al., 2007) guided this article. The University of Nevada, Las Vegas approved this study.
2.1. Participants and recruitment
The inclusion criteria were female natal sex individuals ages 21–65 who self-identified as TM and spoke the English language. The age criteria of 21–65 represents the clinical guidelines for CCS (American Cancer Society, 2013). A convenience sample was recruited using internet, community, and snowball approaches. The principal investigator (PI) distributed recruitment materials to social networking groups, listservs, and internet forums. The PI asked LGBT community centers to distribute recruitment flyers to their members. People who were interested in participating contacted the PI directly. Participants received a $25 electronic gift card.
2.2. Data collection
Data were collected through one-time semi-structured telephone interviews. The PI, who has extensive experience with qualitative research, conducted all interviews. After potential participants were screened for inclusion criteria, they were scheduled for an interview. Eligible participants read a research statement and consented to the study.
The interview consisted of demographic and CCS questions and a semi-structured guided interview. The interview included 13 questions and focused on different areas of the SEM. For example, participants were asked about (un)welcoming healthcare environments, communication style of their providers, and gender dysphoria. The intent of the interview was to elicit participants’ perspectives on CCS. The telephone interviews were audio recorded, professionally transcribed, and verified by the PI. The PI also recorded field notes.
2.3. Data analysis
Data analysis was conducted by the PI and two doctoral students. The PI prepared the transcripts for data analysis in Microsoft Word format. The data were coded using a deductive-inductive content analysis approach (Elo and Kyngas, 2008). The PI trained both assistants on the coding procedure and created a video demonstrating the data analysis procedure to provide additional guidance. Because of the deductive-inductive approach, some of the code names were identified in advance, whereas others were derived from the data. All team members coded each transcript separately. The PI reviewed all codes and collapsed them into broader themes and then sought feedback from the assistants. This process occurred until data was saturated.
3. Results
Twenty people participated in the telephone interviews. The interviews ranged from 20 to 45 min. The participants were mostly non-Hispanic (75%) and white (50%) and the mean age was 33 years. In addition, 55% of the sample had received routine CCS (screened in the last 3 years). See Table 1 for the complete sample description.
Table 1.
Descriptive characteristics of study participants, sampled in year 2018.
| Characteristics (N = 20) | n | % |
|---|---|---|
| Ethnicity | ||
| Non-Hispanic | 15 | 75 |
| Hispanic | 5 | 25 |
| Race | ||
| White | 10 | 50 |
| Black or African American | 4 | 20 |
| Asian | 3 | 15 |
| Multiracial | 3 | 15 |
| Gender Identitya | ||
| Transgender | 9 | 45 |
| Genderqueer | 8 | 40 |
| Gender non-conforming | 3 | 15 |
| Sexual Orientation | ||
| Queer | 12 | 60 |
| Gay/Lesbian | 6 | 30 |
| Bisexual | 2 | 10 |
| Screener Type | ||
| Routine (Screened in last 3 years) | 11 | 55 |
| Non-routine (Screened more than 3 years ago) | 5 | 25 |
| Never Screened | 4 |
20 |
| Mean |
SD (Range) |
|
| Age, y | 33 | 9 (23–60) |
Genderqueer and gender non-conforming are terms that fall under the transgender umbrella in this study. They were included on this table to respect the identities of the participants.
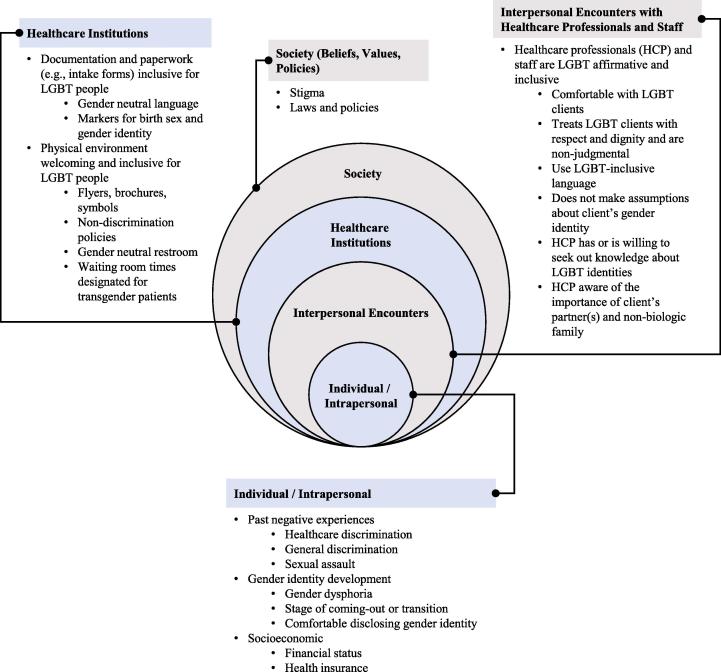
Data analysis resulted in 8 overarching factors that were contextualized within the SEM levels. Most overarching factors included descriptive sub-factors. See Fig. 1 for the final model. Due to the complexity of behaviors in attending CCS services, the factors are not discrete, and some are multidimensional.
Fig. 1.
Qualitative factors that influence cervical cancer screening among transgender men sorted by socioecological level.
3.1. Society
This level includes those broad societal factors that create a climate that (do not) support the equality of transgender individuals. Two broad factors emerged at this level, including stigma and policies. Most participants voiced concerns about attacks on the transgender community at the hands of U.S. government officials. One participant stated, “I feel like the government doesn’t support us. They villainize transgender people, which spreads fear and hatred. If I were discriminated against at my doctor’s office, I feel like my government wouldn’t even protect me.” This feeling was common among the participants.
3.2. Healthcare institutions
These factors relate to healthcare organizational characteristics. Two factors were sorted into this level: 1) documentation and paperwork (e.g., intake forms) inclusive for LGBT people, and 2) physical environment welcoming and inclusive for LGBT people. Each factor includes descriptive sub-factors that identify specific recommendations. Fig. 1 delineates each sub-factor.
Nearly every participant expressed the importance of LGBT-inclusive documentation and physical environments. A participant stated, “Hospitals need to think about the entrance and lobby areas. I want to know if the hospital is a safe space for me and my partner. If I see pride or equality stickers, LGBT posters, or questions on the admission form about my sexual orientation and gender identity, I know it is a safe space.” If intake forms included gender neutral language and markers for birth sex and gender identity, the participants were more likely to use that healthcare professional (HCP). Likewise, if a healthcare organization had gender neutral bathrooms and included LGBT-friendly pamphlets and signs in the waiting and exam rooms, participants felt safer. Additionally, participants were more likely to attend CCS if the healthcare facility had blocks of appointment times for TM.
3.3. Interpersonal encounters with healthcare professionals and staff
The influence of interpersonal relationships on health behaviors is widely recognized. These processes relate to (in)formal interpersonal relationships and encounters (McLeroy et al., 1988). The participants in this study exclusively talked about interpersonal encounters with HCP and staff. One distinct overarching factor emerged in this level: HCPs and staff are LGBT affirmative and inclusive. The sub-factors describe the elements of affirmative and inclusive interpersonal interactions and relate to knowledge, skills, attitudes, and communication of HCPs and staff (see Fig. 1).
TM were more likely to use HCPs who were comfortable with, respectful toward, non-judgmental of, and knowledgeable about LGBT people. Participants spoke about the importance of HCPs and staff being comfortable with LGBT clients, treating LGBT people with respect and dignity, and using LGBT-inclusive language. A participant stated, “I just want the doctors, nurses, and staff to treat me like a human being and not get so awkward around me when they discover I am a queer transman.” Participants were more likely to visit an HCP for CCS who was willing to seek out knowledge about LGBT identities, include partners and non-biologic family in the care, and not make assumptions about someone’s gender identity. Another participant stated, “I understand that a lot of doctors are not familiar with queer people and that is okay. But, they are trained medical professionals, so they should know to educate themselves about diverse people.”
3.4. Intrapersonal
The intrapersonal level consists of characteristics of the individual and developmental history (McLeroy et al., 1988). Three overarching factors were sorted into this socioecological level: 1) past negative experiences, 2) gender identity development, and 3) socioeconomic status. The sub-factors under past negative experiences include healthcare discrimination, general discrimination, and sexual assault. The sub-factors under gender identity development include gender dysphoria, stage of coming-out or transition, and comfortable disclosing gender identity.
Most of the participants spoke about the impact that past negative experiences have on CCS behaviors, specifically related to healthcare and general encounters and sexual assault. People who experienced discrimination during a past healthcare encounter anticipated repeat discrimination, and avoided using CCS services. Similarly, participants who were the target of past discrimination in general settings, such as in public or at work or school, were also less likely to use healthcare services. A participant stated, “I have experienced so much discrimination in my life from family, friends, and strangers on the street. It has affected me to the point where I fear being in certain situations. I really don’t see a doctor because I fear how they will treat me.” Numerous participants also discussed past sexual assault as a barrier to CCS. Past experiences with sexual assault caused the person to avoid CCS because of the intimate nature and loss of control. One participant who was sexually assaulted as a young adult described their experience with CCS, “Although hard to talk about, being raped has had a long-lasting effect on me. It is hard for me to think about being penetrated with a tool during a Pap test. I will try to build myself up days leading up to the exam, but I usually end up canceling the appointment.”
Aspects of a person’s gender identity development surfaced in nearly all the interviews, especially around gender dysphoria and the stage of coming-out or transition. Gender dysphoria, which is the distress associated with the dissonance between a person’s birth sex and gender identity, can be a barrier to CCS. The cervical exam can remind TM about the mismatch between their birth sex and gender identity, which can be distressing enough for some people to avoid screening. A participant stated, “…it is hard to undergo a procedure that reminds me of the body part I hate the most.”
Numerous participants also spoke at length about their stage of transition or coming-out process as a TM and how that impacted their CCS behavior. Although transition phase and coming-out process are separate concepts, the participants interweaved them during the interviews. Transition refers to the process of changing one’s gender presentation and sex characteristics to match with one’s internal sense of gender identity. The coming-out process refers to the development of a transgender identity (Bockting and Coleman, 2016). These processes are different for every person and is often fluid. Further, the stage of coming-out or transition is closely related to gender dysphoria because participants described how dysphoric feelings fluctuate with the stage of transition. One participant changed his gender presentation back to female when getting screened for CC to avoid uncomfortable interactions with the HCP. “My gender presentation is pretty fluid right now, and so I will present as a woman when I know that a situation will be uncomfortable.” Another participant couldn’t bring themselves to seek CCS services until the tail-end of their transition process. “I had a really hard time going to see a gynecologist which transitioning. I really can’t explain why I felt that way, but was just uncomfortable, awkward, and not very confident in myself. Now that I have almost fully transitioned, I am much more confident in myself and have found a great doctor who understands me.”
The remaining intrapersonal factors relate to disclosing gender identity and socioeconomic characteristics. Numerous participants stated that their comfort level in disclosing their gender identity to HCP was sometimes a determining factor when seeking CCS services. Participants who were comfortable disclosing their gender identity were more likely to use CCS services. Finally, every participant spoke about the importance of financial status and health insurance in being able to access CCS services.
4. Discussion
The rate of routine CCS in this study was 55%. Although the sample size in this study was small due to the qualitative nature, the CCS rate is like other recent research that sampled TM (Greene et al., 2019, Kiran et al., 2019). However, this rate is lower than the general population, which has recently been between 65 and 70% (Centers for Disease Control and Prevention, 2017, MacLaughlin et al., 2019). Although there is a stark disparity in CCS rates between TM and the general population, it is challenging to make comparisons because the United States cancer registry does not collect gender identity. Despite the lack of population-level data for transgender people, the lower CCS rates are concerning. The constellation of factors that emerged in this study are meaningful to understanding CCS behaviors among TM.
This study revealed the importance of healthcare organizations feeling safe to TM. Other studies (Johnson et al., 2016a, Johnson et al., 2016b) have established the importance of safe and welcoming healthcare environments for TM seeking CCS services; however, this study identified some specific elements of a safe and welcoming environment. Public entrance areas and waiting rooms in healthcare organizations should be inclusive to LGBT people, such as adding LGBT flyers, brochures, and symbols to public areas. Additionally, scholars have long advocated for the inclusion of sexual orientation and gender identity questions on healthcare forms (Cahill and Makadon, 2013), which emerged as a finding in this study. The gender binary system (female/male) that dominates healthcare establishments is a significant barrier for transgender people. Simply including questions about gender identity that goes beyond female/male and sexual orientation on intake forms conveys inclusivity to LGBT people. LGBT people perceive gender identity and sexual orientation routine questions as important (Bjarnadottir et al., 2017).
Participants in this study recognized the need for healthcare organizations to develop and display LGBT non-discrimination policies to ensure patients feel included and safe. These policies should be extended to ensure equal visitation and employment non-discrimination (Human Rights Campaign, n.d.). Given the reports (Grant et al., 2011, Shires and Jaffee, 2015) of discrimination experienced by transgender people in healthcare settings, it is imperative for healthcare organizations to ensure all LGBT people are protected while receiving services. However, healthcare organizations need to do more than just develop and publicly display these policies. A recent study (Jabson et al., 2016) found no differences in physicians’ attitudes and knowledge about LGBT patients between hospitals with and without a non-discrimination policy. Although laws and policies to protect LGBT from discrimination are important and effective (Barron, 2009, Sellers, 2014), LGBT non-discrimination policies need to be enacted beyond being visible to patients in public areas. Healthcare organizations should operationalize the policies and measure satisfaction of LGBT patients.
All participants in this study discussed the impact that interpersonal encounters with HCPs had on their CCS behaviors. Patient-HCP interactions can be a barrier to quality healthcare (Boehmer, 2018). Extant research has identified some of the quality care attributes for transgender individuals, such as having trust between the HCP and the patient, having affirmative and open HCP-patient communication, having knowledgeable HCPs, and having sensitive and caring HCPs (Johnson et al., 2016a, Johnson et al., 2016b, Kosenko et al., 2013, Poteat et al., 2013, Tabaac et al., 2019). This study revealed similar quality care attributes; HCPs should: 1) feel comfortable treating LGBT patients, 2) treat LGBT patients with respect and dignity, 3) not be judgmental, 4) search for knowledge about LGBT identities and identity-specific care, and 5) use inclusive language. Further, because past discrimination in healthcare settings also emerged as an intrapersonal factor, negative encounters between TM and HCPs likely have a lasting effect on CCS behaviors.
At the intrapersonal level, past sexual assault emerged as a barrier. Transgender individuals have a higher prevalence of sexual assaults compared to the general population. Among the general population, 20% of women and 1.5% of men have been sexually assaulted at some point in their life (National Sexual Violence Resource Center, 2015). In comparison, 47% of transgender people have been sexually assaulted at some point in their life (James et al., 2016). To the investigators’ knowledge, the relationship between sexual assault among TM and CCS behaviors has never been studied. However, sexual assault is a barrier to CCS among the general female population (Cadman et al., 2012, Pedersen and Cohen, 2010, Weitlauf et al., 2010). Women with a history of sexual assault may find the pelvic exam as distressing, embarrassing, and frightening (Weitlauf et al., 2010), are more likely to express hesitation about the safety and necessity of the screening (Pedersen and Cohen, 2010), and report more physical pain during the exam (Cadman et al., 2012). TM with a sexual assault history likely share similar experiences and may have additional barriers and needs with the intersection of the trauma with their gender minority status.
Gender dysphoria, which is the distress transgender people experience as a result of the dissonance between their natal sex and gender identity, has been identified as a barrier to CCS in previous research (Johnson et al., 2016b). Although gender dysphoria was not a unique result in this study, the stage of coming-out or transition is a novel factor. Collectively, coming-out and transition refer to the development of a transgender identity and the process of changing gender presentation and characteristics to match with one’s sense of gender identity. Numerous stages have been applied to the transgender coming out process (Devor, 2004, Gagne et al., 1997, Lev, 2004). One of the latest models (Bockting and Coleman, 2016) posits that coming-out is a multi-staged process; each stage encompasses various developmental tasks, emotions, and physical changes. Individuals do not move through these stages neatly. They often cycle through different stages, depending on external psychosocial factors.
Although researchers have yet to study the association between stage of coming-out or transition among TM and their CCS behaviors, there is likely a relationship. Research has established that gender medical transition using hormones or surgical procedures is effective at ameliorating gender dysphoria and improving the well-being of transgender people. After medically transitioning, transgender people reported improved quality of life (Ainsworth and Spiegel, 2010, Castellano et al., 2015, Manieri et al., 2014), lower levels of anxiety, stress, and depression (Bouman et al., 2016, Boza and Perry, 2014, Collizzi et al., 2013, Gomez-Gil et al., 2012), and higher levels of self-esteem (Bouman et al., 2016). Although these studies did not directly examine the different stages of coming-out, they suggest that transgender individuals experience improved health outcomes as they progress through the stages of transition and coming-out, which likely includes CCS behaviors. Future research needs to tease out differences between coming-out and transition in relation to CCS behaviors. Studying the link between CCS behaviors and stage of coming-out or transition would arguably be a critical contribution to the science of cancer prevention for transgender people.
4.1. Limitations
This study has several limitations. First, the sample was mostly non-Hispanic white individuals who were recruited through convenience sampling approaches. Second, this study only included TM and thus were not compared to non-transgender individuals. Third, the findings in this study are from the perception of the participants; additional research is needed to confirm the factors.
5. Conclusions
The findings in this study demonstrate that intersecting factors at individual, interpersonal, and structural levels impact CCS among TM. Most of the factors relate to HCP and healthcare organizations. Despite the insurgence to promote health equity for transgender people, there needs to be stronger efforts from policymakers, hospital administrators and leaders, and educators to ensure healthcare organizations amend their practices to be more inclusive. Additionally, to the investigators’ knowledge, this is the first study to report the potential relationship between gender identity development and CCS. The transition and coming-out processes are fluid and complex and intersects with physical, mental, and psychosocial aspects of a person’s life. Thus, it is likely that CCS behaviors change as a TM’s identity evolves. Understanding this relationship through further research will be important to improving CCS rates among TM.
Funding
This study was supported by the Clinical and Translational Research Infrastructure Network of the National Institutes of Health under award number 5U54GM104944-05.
CRediT authorship contribution statement
Michael Johnson: Conceptualization, Methodology, Investigation, Data curation, Formal analysis, Visualization, Supervision, Project administration, Funding acquisition. Chris Wakefield: Methodology, Data curation, Formal analysis. KellyAnn Garthe: Data curation, Formal analysis.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Contributor Information
Michael Johnson, Email: michael.johnson@nsc.edu.
Chris Wakefield, Email: wakefc1@unlv.nevada.edu.
KellyAnn Garthe, Email: garthe@unlv.nevada.edu.
References
- Ainsworth T., Spiegel J. Quality of life of individuals with and without facial feminization surgery or gender reassignment surgery. Qual. Life Res. 2010;19(7):1019–1024. doi: 10.1007/s11136-010-9668-7. [DOI] [PubMed] [Google Scholar]
- American Cancer Society. (2013). American Cancer Society guidelines for the early detection of cancer. Retrieved from http://www.cancer.org/healthy/findcancerearly/cancerscreeningguidelines/american-cancer-society-guidelines-for-the-early-detection-of-cancer.
- American Cancer Society. (2019). Key statistics for cervical cancer. Retrieved from https://www.cancer.org/cancer/cervical-cancer/about/key-statistics.html.
- Barron L.G. Promoting the underlying principle of acceptance: the effectiveness of sexual orientation employment antidiscrimination legislation. J. Workplace Rights. 2009;14(2):251–268. [Google Scholar]
- Bjarnadottir R.I., Bockting W., Dowding D.W. Patient perspectives on answering questions about sexual orientation and gender identity: an integrative review. J. Clin. Nurs. 2017;26(13–14):1814–1833. doi: 10.1111/jocn.13612. [DOI] [PubMed] [Google Scholar]
- Bockting W., Coleman E. Developmental stages of the transgender coming-out process. In: Ettner R., Monstrey S., Coleman E., editors. Principles of transgender medicine and surgery. Routledge; New York, NY: 2016. [Google Scholar]
- Boehmer U. LGBT populations’ barriers to cancer care. Semin. Oncol. Nurs. 2018;34(1):21–29. doi: 10.1016/j.soncn.2017.11.002. [DOI] [PubMed] [Google Scholar]
- Bouman W.P., Claes L., Marshall E., Pinner G.T., Longworth J., Maddox V. Socio-demographic variables, clinical features and the role of pre-assessment cross-sex hormones in older trans people. J. Sex. Med. 2016;13(4):711–719. doi: 10.1016/j.jsxm.2016.01.009. [DOI] [PubMed] [Google Scholar]
- Boza C., Perry K.N. Gender-related victimization, perceived social support, and predictors of depression among transgender Australians. Int. J. Transgend. 2014;15(1):35–52. [Google Scholar]
- Cadman L., Waller J., Ashdown-Barr L., Szarewski A. Barriers to cervical screening in women who have experienced sexual abuse: an exploratory study. J. Fam. Plann. Reprod. Health Care. 2012;38(4):214–220. doi: 10.1136/jfprhc-2012-100378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cahill S., Makadon H. Sexual orientation and gender identity data collection in clinical settings and in electronic health records: a key to ending LGBT health disparities. LGBT Health. 2013;1(1):1–8. doi: 10.1089/lgbt.2013.0001. [DOI] [PubMed] [Google Scholar]
- Castellano C., Crespi C., Dell'Aquila C., Rosato R., Catalono C., Mineccia V., Manieri C. Quality of life and hormones after sex reassignment surgery. J. Endocrinol. Invest. 2015;38(12):1373–1381. doi: 10.1007/s40618-015-0398-0. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2017). Use of Pap smears among women aged 18 and over, by selected characteristics: United States, selected years 1987–2015. Retrieved from https://www.cdc.gov/nchs/data/hus/2017/071.pdf.
- Collizzi M., Costa R., Pace V., Todarello O. Hormonal tratment reduces psychobiological distress in gender identity disorder, independelty of the attachment style. J. Sex Med. 2013;10(12):3049–3058. doi: 10.1111/jsm.12155. [DOI] [PubMed] [Google Scholar]
- Devor A.H. Witnessing and mirroring: a fourteen-stage model of transsexual identity formation. J. Gay Lesbian Ment. Health. 2004;8(1/2):41–67. [Google Scholar]
- Elo S., Kyngas H. The qualitative content analysis process. J. Adv. Nurs. 2008;62(1):107–115. doi: 10.1111/j.1365-2648.2007.04569.x. [DOI] [PubMed] [Google Scholar]
- Fleury J., Lee S.M. The social ecological model and physical activity in African American women. Am. J. Commun. Psychol. 2006;37(1/2):129–140. doi: 10.1007/s10464-005-9002-7. [DOI] [PubMed] [Google Scholar]
- Gagne P., Tewksbury R., McGaughey D. Coming out and crossing over: Identity formation and proclamation in a transgender community. Gender Soc. 1997;11(4):478–508. [Google Scholar]
- Gomez-Gil E., Zubiaurre-Elorz L., Esteva I., Guillamon A., Godas T., Cruz Almaraz M., Salamero M. Hormone-treated transsexuals report less social distress, anxiety and depression. Psychoneuroendocrinology. 2012;37(5):662–670. doi: 10.1016/j.psyneuen.2011.08.010. [DOI] [PubMed] [Google Scholar]
- Grant J.M., Mottet L.A., Tanis J., Harrison J., Herman J.L., Keisling M. National Center for Transgender Equality and National Gay and Lesbian Task Force; Washington, DC: 2011. Injustice at every turn: A report of the national transgender discrimination survey. [Google Scholar]
- Greene M.Z., Hughes T.L., Hanlon A., Huang L., Sommers M.S., Meghani S.H. Predicting cervical cancer screening among sexual minority women using classification and regression tree analysis. Prev. Med. Rep. 2019;13:153–159. doi: 10.1016/j.pmedr.2018.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Human Rights Campaign. (n.d.). Non-discrimination and staff training. Retrieved from https://www.hrc.org/hei/non-discrimination-and-staff-training-resources.
- Institute of Medicine . The National Academies Press; Washington, DC: 2011. The health of lesbian, gay, bisexual, and transgender people: Building a foundation for better understanding. [PubMed] [Google Scholar]
- Jabson J.M., Mitchell J.W., Doty S.B. Associations between non-discrimination and training policies and physicians' attitudes and knowledge about sexual and gender minority patients: a comparison of physicians from two hospitals. BMC Public Health. 2016;16(256):1–16. doi: 10.1186/s12889-016-2927-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James S.E., Herman J.L., Rankin S., Keisling M., Mottet L., Anafi M. National Center for Transgender Equality; Washington, DC: 2016. The report of the 2015 U.S. transgender survey. [Google Scholar]
- Johnson M.J., Mueller M., Eliason M.J., Stuart G., Nemeth L.S. Quantitative and mixed analyses to identify factors that affect cervical cancer screening uptake among lesbian and bisexual women and transgender men. J. Clin. Nurs. 2016;25:3628–3642. doi: 10.1111/jocn.13414. [DOI] [PubMed] [Google Scholar]
- Johnson M.J., Nemeth L.S., Mueller M., Eliason M.J., Stuart G.W. Qualitative study of cervical cancer screening among lesbian and bisexual women and transgender men. Cancer Nurs. 2016;39(6):455–463. doi: 10.1097/NCC.0000000000000338. [DOI] [PubMed] [Google Scholar]
- Kiran T., Davie S., Singh D., Hranilovic S., Pinto A.D., Abramovich A., Lofters A. Cancer screening rates among transgender adults. Can. Fam. Physician. 2019;65(January):e30–e37. [PMC free article] [PubMed] [Google Scholar]
- Kosenko K., Rintamaki L., Raney S., Maness K. Transgender patient perceptions of stigma in health care contexts. Med. Care. 2013;51(9):819–822. doi: 10.1097/MLR.0b013e31829fa90d. [DOI] [PubMed] [Google Scholar]
- Lev A.I. The Haworth Clinical Practice Press; Binghamton, NY: 2004. Transgender emergence: therapeutic guidelines for working with gender-variant people and their families. [Google Scholar]
- Leyden W.A., Manos M.M., Geiger A.M., Weinmann S., Mouchawar J., Bischoff K., Taplin S.H. Cervical cancer in women with comprehensive health care access: attributable factors in the screening process. J. Natl. Cancer Inst. 2005;97(9):675–683. doi: 10.1093/jnci/dji115. [DOI] [PubMed] [Google Scholar]
- MacLaughlin K.L., Jacobson R.M., Radecki Breitkopf C., Wilson P.M., Jacobson D.J., Fan C., Rutten L.J.F. Trends over time in Pap and Pap-HPV cotesting for cervical cancer screening. J. Womens Health. 2019;28(2):244–249. doi: 10.1089/jwh.2018.7380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manieri C., Castellano E., Crespi C., Di Bisceglie C., Dell'Aquila C., Gualerzi A., Molo M. Medical treatment of subjects with gender identity disorder: the experience of an Italian public health center. Int. J. Transgend. 2014;15(2):53–65. [Google Scholar]
- McLeroy K.R., Bibeau D., Steckler A., Glanz K. An ecological perspective on health promotion programs. Health Educ. Behav. 1988;15(4):351–377. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- National Sexual Violence Resource Center. (2015). Statistics about sexual violence. Retrieved from https://www.nsvrc.org/sites/default/files/publications_nsvrc_factsheet_media-packet_statistics-about-sexual-violence_0.pdf.
- Pedersen A.H., Cohen B.E. Identifying and overcoming barriers to cervical cancer screening in women with a history of sexual violence and posttraumatic stress disorder. J. Womens Health. 2010;19(7):1239–1241. doi: 10.1089/jwh.2010.2125. [DOI] [PubMed] [Google Scholar]
- Peitzmeier S.M., Khullar K., Reisner S.L., Potter J. Pap test use is lower among female-to-male patients than non-transgender women. Am. J. Prev. Med. 2014;47(6):808–812. doi: 10.1016/j.amepre.2014.07.031. [DOI] [PubMed] [Google Scholar]
- Poteat T., German D., Kerrigan D. Managing uncertainty: a grounded theory of stigma in transgender health care encounters. Soc. Sci. Med. 2013;84:22–29. doi: 10.1016/j.socscimed.2013.02.019. [DOI] [PubMed] [Google Scholar]
- Potter J., Peitzmeier S.M., Bernstein I., Reisner S.L., Alizaga N.M., Agenor M., Pardee D.J. Cervical cancer screening for patients on the female-to-male spectrum: a narrative review and guide for clinicians. J. Gen. Intern. Med. 2015;30(12):1857–1864. doi: 10.1007/s11606-015-3462-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisner S.L., Gamarel K.E., Dunham E., Hopwood R., Hwahng S. Female-to-male transmasculine adult health: a mixed-methods community-based needs assessment. J. Am. Psychiatr. Nurses Assoc. 2013;19(5):293–303. doi: 10.1177/1078390313500693. [DOI] [PubMed] [Google Scholar]
- Sellers M.D. Discrimination and the transgender population: analysis of the functionality of local government policies that protect gender identity. Administration Soc. 2014;46(1):70–86. [Google Scholar]
- Shires D.A., Jaffee K. Experiences among a national sample of female-to-male transgender individuals. Health Soc. Work. 2015;40(2):134–141. doi: 10.1093/hsw/hlv025. [DOI] [PubMed] [Google Scholar]
- Tabaac A.R., Benotsch E.G., Barnes A.J. Mediation models of perceived medical heterosexism, provider-patient relationship quality, and cervical cancer screening in a community sample of sexual minority women and gender nonbinary adults. LGBT Health. 2019;6(2):77–86. doi: 10.1089/lgbt.2018.0203. [DOI] [PubMed] [Google Scholar]
- Tong A., Sainsbury P., Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care. 2007;19(6):349–357. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- U.S. Preventive Services Task Force. (2019). Final recommendation statement: Cervical cancer screening. Retrieved from https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/cervical-cancer-screening2.
- Weitlauf J.C., Frayne S.M., Finney J.W., Moos R.H., Jones S., Hu K., Spiegel D. Sexual violence, posttraumatic stress disorder, and the pelvic examination: how do beliefs about the safety, necessity, and utility of the examination influence patient experiences? J. Womens Health. 2010;19(7):1271–1280. doi: 10.1089/jwh.2009.1673. [DOI] [PubMed] [Google Scholar]