Abstract
3-methylglutaric (3MG) acid is a conspicuous C6 dicarboxylic organic acid classically associated with two distinct leucine pathway enzyme deficiencies. 3MG acid is excreted in urine of individuals harboring deficiencies in 3-hydroxy-3-methylglutaryl (HMG) CoA lyase (HMGCL) or 3-methylglutaconyl CoA hydratase (AUH). Whereas 3MG CoA is not part of the leucine catabolic pathway, it is likely formed via a side reaction involving reduction of the α-ß trans double bond in the leucine pathway intermediate, 3-methylglutaconyl CoA. While the metabolic basis for the accumulation of 3MG acid in subjects with deficiencies in HMGCL or AUH is apparent, the occurrence of 3MG aciduria in a host of unrelated inborn errors of metabolism associated with compromised mitochondrial energy metabolism is less clear. Herein, a novel mitochondrial biosynthetic pathway termed “the acetyl CoA diversion pathway”, provides an explanation. The pathway is initiated by defective electron transport chain function which, ultimately, inhibits acetyl CoA entry into the TCA cycle. When this occurs, 3MG acid is synthesized in five steps from acetyl CoA via a novel reaction sequence, providing a metabolic rationale for the connection between 3MG aciduria and compromised mitochondrial energy metabolism.
Keywords: Organic aciduria, 3-methylglutaconic acid, mitochondria, inborn error of metabolism, leucine, acetyl CoA diversion pathway
Introduction
1.1. Primary 3MG aciduria.
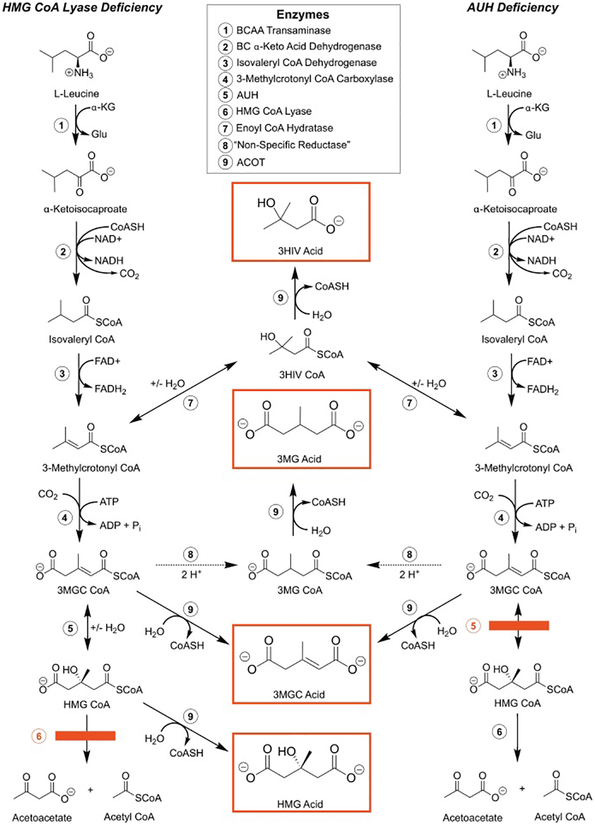
3-methylglutaric (3MG) acid was originally identified as an organic acid present in urine of individuals harboring one of two distinct leucine catabolic pathway enzyme deficiencies. 3MG aciduria is known to occur in individuals with mutations in either 3-hydroxy-3-methylglutaryl CoA (HMG CoA) lyase (HMGCL) [1] or 3-methylglutaconyl CoA hydratase (AUH) [2]. In these disorders, leucine catabolism is effectively blocked (Figure 1) resulting in “primary” 3MG aciduria. When the leucine metabolic pathway is blocked in this manner, the resulting accumulation of upstream pathway intermediates leads to the formation of characteristic organic acids that are excreted in urine. For example, in HMGCL deficiency, abundant organic acids include HMG acid, 3-methylglutaconic (3MGC) acid, 3-hydroxyisovaleric (3HIV) acid and 3MG acid. Likewise, in the case of AUH deficiency (see Figure 1), 3 major organic acids are produced including 3MGC acid, 3HIV acid and 3MG acid. As expected, HMG acid accumulation is not observed in AUH deficiency. Moreover, consistent with a block in the leucine catabolic pathway, administration of leucine to subjects with primary 3MG aciduria leads to increased excretion of these organic acids [3].
Figure 1. Biosynthesis of organic acids associated with two leucine pathway enzyme deficiencies.
The leucine catabolism pathway is depicted on the left and right with the position of enzyme deficiencies for HMG CoA lyase (left) and AUH (right) depicted by red filled rectangular boxes. Molecules in the center depict side reactions caused by the buildup of pathway intermediates that ultimately lead to the organic acid products (red boxes) that appear in urine. Numbers refer to specific enzymes (see list). BCAA, branched chain amino acid.
It is generally considered that the final step in organic acid production is thioester hydrolysis of the corresponding acyl CoA. In the case of HMG acid and 3MGC acid, for example, as the leucine pathway intermediates HMG CoA and / or 3MGC CoA accumulate, acyl CoA thioesterase (ACOT)-mediated thioester hydrolysis is the only reaction involved. In the case of 3HIV acid, however, this organic acid is thought to arise from alternate metabolism of the leucine catabolism pathway intermediate, 3-methylcrotonyl CoA. As the concentration of 3-methylcrotonyl CoA increases as a result of a downstream enzyme deficiency, it undergoes a side reaction, presumably catalyzed by crotonase, a member of the enoyl CoA hydratase superfamily [4, 5]. In this reaction, the α-ß trans double bond in 3-methylcrotonyl CoA is hydrated, forming 3HIV CoA. As 3HIV CoA levels increase, it serves as a substrate for ACOT-mediated thioester hydrolysis, generating 3HIV acid and free CoASH. The final organic acid that accumulates in these disorders is 3MG acid. As with 3HIV CoA, 3MG CoA is not part of any known biochemical pathway and is presumed to arise directly from a side reaction involving reduction of the α-ß trans double bond in the leucine pathway intermediate, 3MGC CoA. As 3MG CoA levels increase in mitochondria, it becomes a substrate for ACOT-mediated thioester hydrolysis, generating 3MG acid and free CoASH. Insofar as mitochondrial CoASH is involved in fatty acid and intermediary metabolism, ACOT-mediated thioester hydrolysis of these acyl CoAs effectively serves a protective role by replenishing the free CoASH / acyl CoA ratio. Moreover, release of CoASH reduces toxicity associated with increased concentrations of acyl CoAs [6].
Among the reactions involved in production of these four organic acids, all but three are well characterized. Of the three less well studied reactions, the enzyme involved in the conversion of 3-methylcrotonyl CoA to 3HIV CoA is likely to be crotonase [7, 8]. Crotonase normally catalyzes hydration of crotonyl CoA to ß-hydroxybutyryl CoA. In the present case, however, crotonase is postulated to accept 3-methylcrotonyl CoA as an alternate substrate, yielding 3HIV CoA (Figure 1). Although there are many members of the enoyl CoA hydratase enzyme family [4], including AUH, given the structural similarity between crotonyl CoA and 3-methylcrotonyl CoA, crotonase is the most likely member of the enoyl CoA hydratase enzyme family to catalyze this reaction. Given that 3HIV acid does accumulate under normal physiological circumstances, it may be inferred that 3-methylcrotonyl CoA is not a preferred substrate for crotonase and, therefore, this enzyme is unlikely to compete with 3-methylcrotonyl CoA carboxylase for this substrate. On the other hand, when there is a downstream block in the leucine catabolism pathway, causing 3-methylcrotonyl CoA levels to rise dramatically, this side reaction does proceed. Whereas conversion of short chain (i.e C5 or C6) acyl CoAs to the corresponding organic acid undoubtedly involves an ACOT, as many as 15 unique ACOT enzymes exist in the cell and several of these localize to mitochondria [9]. Based on studies of their subcellular localization and substrate specificity, it may be inferred that ACOT 9 plays a role in production of one or more of the four organic acids under discussion here [10].
Conversion of 3MGC CoA to 3MG CoA is also likely to occur via a side reaction. However, since few, if any, mitochondrial enzymes catalyze the reduction of trans α-ß double bonds in acyl CoA substrates, the identity of the responsible enzyme has eluded investigators. Considering the chemistry required for conversion of 3MGC CoA to 3MG CoA, Faull et al [11] proposed two possible enzyme-mediated routes. First, they surmised that isovaleryl CoA serves as an alternate substrate for 3-methylcrotonyl CoA carboxylase, an enzyme which normally carboxylates 3-methylcrotonyl CoA to form 3MGC CoA (see Figure 1). If this mechanism were operative, however, one would expect 3MG acid to appear in urine of patients with isovaleric aciduria caused by a deficiency in isovaleryl CoA dehydrogenase, yet this is not observed [12]. A second possibility is that 3MGC CoA serves as an alternate substrate in a reversal of the reaction normally catalyzed by isovaleryl CoA dehydrogenase, an enzyme that converts isovaleryl-CoA to 3-methylcrotonyl CoA in the leucine metabolism pathway. This scenario is also unlikely since 3MGC CoA is a dicarboxylic compound while 3-methylcrotonyl-CoA is monocarboxylic. Other investigators have simply described the formation of 3MG CoA from 3MGC CoA as catalyzed by a “non-specific reductase” [13,14]. At this point more work is necessary to identify the enzyme involved in this reaction.
1.2. Secondary 3MG aciduria.
Understanding the biochemical origin of 3MG acid has taken on additional importance given its occurrence in numerous, seemingly disparate, inherited mitochondrial disorders collectively referred to as “secondary” 3MG acidurias. Importantly, in every instance of secondary 3MG aciduria, 3MG acid is present together with 3MGC acid, further supporting a precursor / product relationship between 3MGC CoA and 3MG CoA. In contrast to primary 3MG acidurias, however, neither 3HIV acid nor HMG acid (specific to HMGCL deficiency) are present in secondary 3MG aciduria. Moreover, no leucine pathway enzyme deficiencies have been reported in cases of secondary 3MG aciduria and, unlike primary 3MG aciduria, no further accumulation of 3MGC acid or 3MG acid occurs upon leucine loading [3]. Thus, it may be concluded that, in secondary 3MG aciduria, characteristic organic acids arise via a biosynthetic route that is independent of leucine catabolism. Clues as to the nature of the biosynthetic pathway involved may be obtained through an understanding of various inborn errors of metabolism that manifest 3MG aciduria as a phenotypic feature (Table 1). An example of such a disorder is Barth Syndrome. The genetic defect in Barth Syndrome is a mutation in the tafazzin (TAZ) gene, which encodes a cardiolipin transacylase. Ikon and Ryan [15] described how altered cardiolipin content and composition in this disorder causes organic aciduria and, ultimately, cardiomyopathy. Briefly, TAZ mutation-induced defects in the content and composition of cardiolipin damage inner mitochondrial membrane integrity which, in turn, impairs electron transport chain (ETC) function. Two consequences of this are 1) reduced aerobic ATP production and 2) increased reliance on anaerobic glycolysis, resulting in hypoglycemia and lactic acidemia. The observation that, in at least 8 distinct mitochondrial disorders (Table 1), 3MGC acid and 3MG acid accumulate, despite the absence of defects in the leucine catabolism pathway, supports the existence of an alternate biosynthetic pathway in these disorders. Directly or indirectly, each of the gene mutations listed in Table 1 impair mitochondrial function in a way that perturbs oxidative metabolism. As described below, when this occurs, 3MGC acid and 3MG acid are produced via a novel biosynthetic pathway.
Table 1.
Gene defects associated with secondary 3MG aciduria
| Affected Gene | Gene Function | Location | 3MGc acid1 (mmol/mol creatinine) | 3MG acid1 (mmol/mol creatinine) | Reference |
|---|---|---|---|---|---|
| TAZ | Cardiolipin transacylase | Inner mitochondrial membrane | 58.4 | 7.5 | [32,33] |
| DNAJC19 | Chaperone protein; mitochondrial protein import | Inner mitochondrial membrane | 130 | 14 | [34] |
| 120–130 | 95 | [35] | |||
| SERAC1 | Phosphatidyl-glycerol remodeling | Localized to interface between ER and mitochondria | 182–420 | 42–360 | [36] |
| 119 | 38 | [37] | |||
| TMEM70 | Complex V (ATPase) assembly | Inner mitochondrial membrane | 32–167 | 8–54 | [38] |
| 60–122 | 15–41 | [38] | |||
| 121 | 33 | [39] | |||
| 91–284 | 20–83 | [40] | |||
| CLPB | AAA+ protease and chaperone involved in disaggregation of misfolded proteins | Mitochondria | + | + | [41] |
| Mitochondrial DNA deletions | - | Mitochondria | + | + | [42] |
| QIL/MIC13 | Component of the mitochondrial cristae organizing system | Inner mitochondrial membrane | + | + | [43] |
| TIMM50 | Subunit of mitochondrial import machinery | Intermembrane space | 53–508 | 20–220 | [44] |
Where indicated “+” signs indicate the organic acid was present but not quantified.
1.3. The acetyl CoA diversion pathway.
In each of the gene mutations listed in Table 1, it is proposed that 3MG CoA is synthesized de novo from acetyl CoA in five steps. Key to this reaction scheme is an accumulation of acetyl CoA in the mitochondrial matrix due to a functional defect in the ETC. Such defects affect one or more of the following: mitochondrial membrane lipid content and composition, inner membrane protein/enzyme function or assembly of ATP synthase. Directly or indirectly, these mutations have an impact on a) electron flux via the ETC, b) establishment of a proton gradient or c) productive coupling of an established proton motive force to ADP phosphorylation. When any of these functions is impaired, ATP production and energy metabolism are compromised. Under these circumstances, NADH and FADH2 generated during oxidative metabolism of fuel molecules are not able to efficiently donate electrons to the ETC. As levels of NADH rise in the mitochondrial matrix, enzymes that generate NADH are subject to end product inhibition, thereby impeding key metabolic pathways, including the TCA cycle. Given the tight coupling of FADH2 oxidation to the ETC via electron transferring flavoprotein activity, when ETC activity slows, decreased flavoenzyme FADH2 oxidation interferes with the activity of acyl CoA dehydrogenase enzymes (e.g. succinyl CoA dehydrogenase).
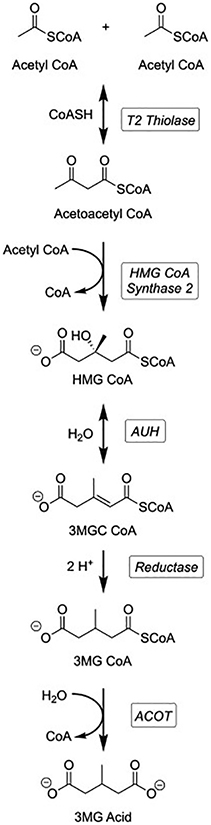
As ETC activity slows in cardiac / skeletal muscle mitochondria as a result of these inborn errors of metabolism, matrix levels of acetyl CoA rise, initiating the acetyl CoA diversion pathway (Figure 2). Above a threshold level of matrix acetyl CoA, acetoacetyl CoA thiolase (T2) functions in the reverse direction, catalyzing condensation of two acetyl CoA to generate acetoacetyl CoA. In the second reaction, HMG CoA synthase 2 catalyzes the condensation of acetoacetyl CoA and acetyl CoA, generating HMG CoA and CoASH. Subsequently, this leucine pathway intermediate is dehydrated to 3MGC CoA by AUH in a reversal of its usual direction in leucine metabolism [16]. Note that under normal physiological circumstances, HMG CoA is a substrate for HMG CoA lyase, generating acetoacetate and acetyl CoA. This reaction does not occur in this case because a) HMG CoA lyase levels in heart / skeletal muscle tissue mitochondria are only a fraction of that in liver, where it functions in ketone body production and b) accumulating acetyl CoA serves as an end product inhibitor of the enzyme. Once formed, 3MGC CoA is unable to proceed further upstream in the leucine catabolic pathway because the next reaction, catalyzed by 3-methylcrotonyl CoA carboxylase, is irreversible. Thus, 3MGC CoA levels continue to rise, driven by the accumulation of acetyl CoA in an environment where it is unable to undergo oxidative metabolism. At this point 3MGC CoA has three possible fates: 1) if acetyl CoA levels normalize it can be hydrated to form HMG CoA (via AUH activity) followed by HMG CoA lyase-mediated conversion to acetoacetate and acetyl CoA (Figure 1). A second possible fate of 3MGC CoA generated via the acetyl CoA diversion pathway is ACOT-mediated thioester hydrolysis, generating 3MGC acid. Finally, a third fate of 3MGC CoA is enzymatic reduction to form 3MG CoA. The enzyme responsible for this conversion is not known and has been referred to as a “non-specific reductase” [13,14]. As described in section 1.1, the reaction involves reduction of the α-ß trans double bond in 3MGC CoA to the corresponding saturated acyl CoA (i.e. 3MG CoA). In all likelihood, 3MGC CoA is not the natural substrate for the enzyme in question but, instead, as its concentration increases in the mitochondrial matrix, it serves as an alternate substrate. Once 3MG CoA is formed, 3MG acid is generated by ACOT-mediated thioester hydrolysis. As described below, however, 3MG CoA can undergo other reactions as well.
Figure 2. The acetyl CoA diversion pathway.
A sequence of five enzyme-mediated reactions that lead to 3MG acid from acetyl CoA is depicted. Initially, T2 thiolase catalyzes a Claisen condensation of 2 acetyl CoA. Acetoacetyl CoA generated by this reaction reacts with acetyl CoA in a second Claisen condensation, catalyzed by HMG CoA synthase 2. Subsequently AUH hydratase dehydrates HMG CoA to 3MGC CoA in a reversal of the leucine catabolic pathway reaction. 3MGC CoA is then reduced to 3MG CoA by an unknown “non-specific reductase”. Finally 3MG CoA is hydrolyzed to 3MG acid by a mitochondrial ACOT.
1.4. Detection, differentiation and frequency of 3MG acidurias.
Detection of 3MG aciduria (primary and secondary) can be achieved by gas chromatography – mass spectrometry analysis of patient urine samples [17]. This method is routine for many organic acids and is generally correlated to mmol/mol creatinine. Alternatively, NMR spectroscopy can be used as a method to detect 3MG acid [18].
Once the presence of 3MG acid has been verified, distinguishing between primary and secondary 3MG aciduria can be achieved by one or more of the following analyses. In cases of primary 3MG aciduria, a leucine loading test will result in increased levels of 3MGC acid and 3MG acid as a direct result of mutations in leucine pathway enzymes. On the other hand, no such increase occurs in secondary 3MG aciduria [3]. Likewise, in primary 3MG aciduria increased levels of 3HIV acid will be present while this acid is not produced in secondary 3MG aciduria [19]. A third distinguishing feature is the ratio of 3MGC acid to 3MG acid (see section 1.6 below). It should be noted, however, that a definitive diagnosis requires identification of the specific gene defect underlying the symptoms presented.
In terms of the frequency of these disorders, primary 3MG aciduria, caused by mutations in HMG CoA lyase or 3-methylglutaconyl CoA hydratase (AUH), are considered rare [20], and extremely rare [21], respectively. Likewise, the frequency of secondary 3MG acidurias is rare to extremely rare. For example, the frequency of Barth syndrome (see Table 1) is between 1 in 300,000 and 1 in 400,000 [22]. Because the responsible gene in Barth Syndrome is X-linked, it is considered that this disorder may be more prevalent than other inborn errors of metabolism listed in Table 1. In the case of mutations in DNAJC19, however, the frequency of this disorder is more frequent in Canadian Dariusleut Hutterite families, as a result of consanguineous relationships [23]. The remaining gene mutations that give rise to this phenotype are considered very rare to extremely rare.
1.5. Alternate metabolic fates of 3MG CoA.
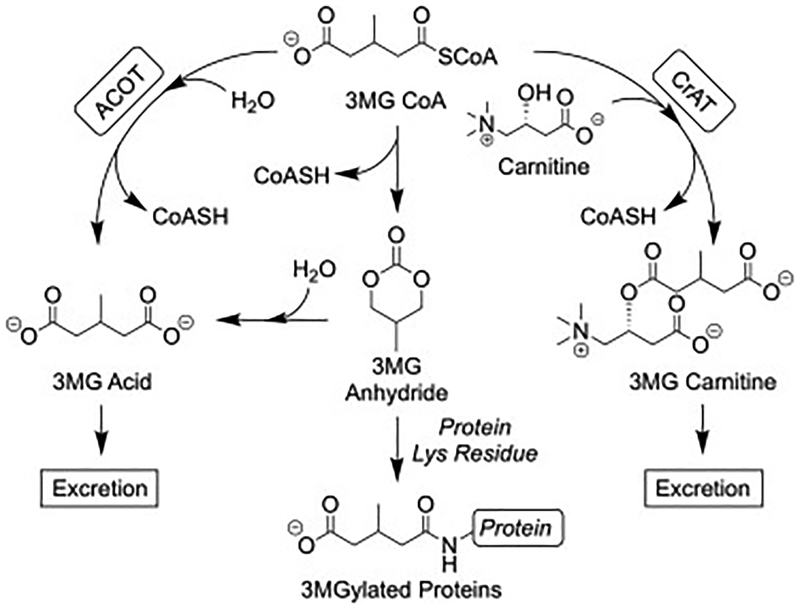
Once 3MG CoA is formed, because it is not part of a metabolic pathway, it is not able to undergo energy yielding metabolism. Rather, its fate is restricted to three possible outcomes (Figure 3). As mentioned above, 3MG CoA can undergo ACOT-mediated thioester hydrolysis, forming 3MG acid. This organic acid product is destined for excretion in urine, resulting in 3MG aciduria. A second potential fate involves a nonenzymatic intramolecular rearrangement, forming a symmetric cyclic anhydride and free CoASH [14]. Once formed, 3MG anhydride is a reactive intermediate, capable of acylating lysine side chain amino groups of mitochondrial proteins [24]. Studies of this phenomenon in HMG CoA lyase deficient mice have revealed that the NAD+ dependent deacylase, sirtuin 4, enzymatically removes 3MG from proteins. Consistent with this, sirtuin 4 knockout mice manifest increased protein 3MGylation. Interestingly, proteins subject to this post translational modification include leucine pathway enzymes, suggesting a potential regulatory function [24]. Third, when sufficient amounts of free carnitine are available, 3MG CoA serves as a substrate for carnitine acyltransferase-mediated formation of 3MG carnitine [13]. Carnitine derivatization of small organic molecules is a widely known mechanism for exporting “dead end” metabolites that would otherwise accumulate in the mitochondrial matrix. Indeed, in newborn blood spot analysis, 3MG carnitine, detected by mass spectrometry, is used to diagnose HMG CoA lyase deficiency. 3MG carnitine has also been reported in AUH deficiency [25] and is likely to occur in secondary 3MG acidurias as well. To our knowledge, however, the presence of 3MG carnitine in secondary 3MG aciduria has yet to be reported.
Figure 3. Alternate fates of 3MG CoA.
When 3MG CoA is formed in mitochondria, it has three potential fates. ACOT-mediated thioester hydrolysis (left) gives rise to 3MG acid and CoASH. 3MG CoA can also undergo a nonenzymatic intramolecular cyclization, with loss of CoASH, generating 3MG anhydride (center). Once formed, 3MG anhydride can react with H2O to form 3MG acid or with protein lysine side chain amino groups, forming a covalent protein adduct. In a third possible fate, 3MG CoA can be converted to 3MG carnitine, with loss of CoASH, via the action of carnitine acyltransferase (CrAT). Once formed, 3MG acid and 3MG carnitine are targeted for export from mitochondria and excretion in urine.
Curiously, despite the fact that levels of 3MGC acid (in AUH deficiency) or HMG acid (in HMGCL deficiency) vastly exceed those of 3MG acid in primary 3MG acidurias, little, if any, 3MGC carnitine or HMG carnitine are formed [13]. This makes physiological sense because 3MGC CoA and HMG CoA are key metabolic intermediates in an important biochemical pathway (i.e. leucine degradation). Since carnitine derivatization of small organic molecules amounts to an export signal, this would result in waste of their carbon skeletons. On the other hand, 3MG CoA (or 3HIV CoA) is not a metabolic pathway intermediate and, once formed, its carbon skeleton cannot be used for energy production. In this case it makes sense that, as small amounts of 3MG CoA are generated, carnitine esterification provides a means to export it. However, given the relative amounts of 3MG acid excreted in urine versus 3MG carnitine, it is evident that, in primary and secondary 3MG aciduria, ACOT-mediated formation of 3MG acid is a quantitatively important reaction. It may be that, when the cell is replete with free carnitine, the relative proportion of 3MG carnitine versus 3MG acid formed, will increase. Likewise, when small amounts of 3MG CoA are generated, the preferred means to recover its CoASH moiety and excrete the carbon skeleton is carnitine ester formation. When aberrant physiological processes result in increased 3MG CoA production, however, ACOT-mediated thioester hydrolysis becomes active. In this case, free carnitine will be preserved for essential functions while, at the same time, the pool of free CoASH will be retained for vital metabolic processes. As they are produced, both 3MG acid and 3MG carnitine are destined for export from mitochondria and excretion in urine.
1.6. On the ratio of 3MGC acid to 3MG acid.
In secondary 3MG aciduria, where no leucine pathway enzyme deficiencies exist, levels of 3MGC acid and 3MG acid in urine are far lower than values observed in cases of primary 3MG aciduria. At the same time, in general, the amount of 3MG acid relative to 3MGC acid is higher in secondary 3MG aciduria. For example, in a case of HMGCL deficiency (primary 3MG aciduria), Santarelli et al [26] reported urinary 3MGC acid levels = 4100 μmol/mmol creatinine (control value, 6 μmol/mmol creatinine). In this individual, 3MG acid levels were 348 μmol/mmol creatinine (control value, 7 μmol/mmol creatinine). While this 3MGC acid value is extremely high, the 3MG acid value is only modestly higher that values reported in Table 1 for secondary 3MG acidurias. Moreover, as mentioned above, leucine loading has little or no effect on organic acid accumulation in secondary 3MG acidurias. In these disorders, neither 3MGC acid or 3MG acid is produced from leucine catabolism but, rather, they are synthesized de novo via the acetyl CoA diversion pathway. Differences observed in the ratio of 3MGC acid to 3MG acid correlate with the nature of the metabolic defect underlying their production. When 3MG aciduria is caused by a leucine metabolic enzyme deficiency massive quantities of 3MGC acid and relatively lower amounts of 3MG acid are observed. On the other hand, when 3MG aciduria results from an inborn error of metabolism associated with compromised mitochondrial energy metabolism, far lower amounts of 3MGC acid are present and the relative proportion of 3MG acid to 3MGC acid increases. For example, the ratio of 3MGC acid to 3MG acid is in the range of 10 to 12 in primary 3MG acidurias [26,11,27,28] while it is closer to 4 in secondary 3MG aciduria (Table 1).
1.7. 3MG acid toxicity.
Accumulation of 3MG acid has been reported to be toxic to neuronal tissue. Colin-Gonzalez et al [29] found that 3MG acid exerts toxicity through early activation of an oxidative stress response, resulting in mitochondrial dysfunction. It is conceivable that toxic effects elicited by 3MG acid could act as a triggering factor for neurodegeneration during progression of disorders associated with 3MG aciduria. In another study using rat brain tissue, da Rosa et al [30], reaffirmed that oxidative damage is caused by organic acids, specifically HMG acid and 3MG acid. These authors reported that intra-striatal injection of 3MG acid or HMG acid increased the frequency and index of lipid and protein oxidation. In another study Ribeiro et al [31] reported that accumulation of 3MG acid increases the potential for neurodegeneration. Taken together these findings are consistent with the occurrence of cerebral alterations in HMG CoA lyase deficiency and suggest the presence of two independent mechanisms for export and excretion of 3MG acid (i.e. 3MG carnitine and 3MG acid) may serve a protective role by preventing irreparable tissue damage.
2.1. Conclusions.
Two distinct types of 3MG aciduria have been identified, termed primary and secondary. In both types, 3MG acid is always accompanied by 3MGC acid. The observation that, without exception, 3MGC acid is quantitatively more abundant that 3MG acid, the term 3MGC aciduria is often used, with the implication is that 3MG acid will also be present. A key outstanding question in this field relates to the nature of the enzyme responsible for conversion of 3MGC CoA to 3MG CoA. Improved knowledge of this reaction should provide insight into the underlying mechanism whereby mitochondrial defects give rise to its formation and explain the enzymology underlying a rare, if not unheard-of, mitochondrial enoyl CoA reduction reaction. Moreover, characterization of this “non-specific reductase” activity may yield insight into why secondary 3MG aciduria is associated with a higher proportion of 3MG acid versus 3MGC acid, as compared to primary 3MG acidurias.
Acknowledgments
The authors thank Sharon Young and Kathleen Schegg for helpful discussions.
Funding
This work was supported by the National Institutes of Health (R37 HL64159) and a Nevada Undergraduate Research Award to LP.
Abbreviations:
- 3MG
3-methylglutaric
- 3MGC
3-methylglutaconic
- HMG
3-hydroxy-3-methylglutaric
- HMGCL
HMG CoA lyase
- AUH
methylglutaconyl CoA hydratase
- 3HIV
3-hydroxyisovaleric
- ACOT
acyl CoA thioesterase
- ETC
electron transport chain
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of competing interests: None
References
- [1].Pié J, López-Viñas E, Puisac B, Menao S, Pié A, Casale C, Ramos FJ, Hegardt FG, Gómez-Puertas P, Casals N, Molecular genetics of HMG-CoA lyase deficiency, Mol. Genet. Metab 92, (2007) 198–209. [DOI] [PubMed] [Google Scholar]
- [2].IJlst L, Loupatty FJ, Ruiter JP, Duran M, Lehnert W, Wanders RJ, 3-Methylglutaconic aciduria type I is caused by mutations in AUH, Am. J. Hum. Genet 71 (2002) 1463–1466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Wortmann SB, Kluijtmans LA, Sequeira S, Wevers RA, Morava E, Leucine loading test is only discriminative for 3-methylglutaconic aciduria due to AUH Defect, JIMD Rep 16 (2014) 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Hamed RB, Batchelar ET, Clifton IJ, Schofield CJ, Mechanisms and structures of crotonase superfamily enzymes--how nature controls enolate and oxyanion reactivity. Cell Mol. Life Sci 65 (2008) 2507–2527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Holden HM, Benning MM, Haller T, Gerlt JA, The crotonase superfamily: divergently related enzymes that catalyze different reactions involving acyl coenzyme a thioesters. Acc. Chem. Res 34 (2001) 145–157. [DOI] [PubMed] [Google Scholar]
- [6].Röschinger W, Millington DS, Gage DA, Huang ZH, Iwamoto T, Yano S, Packman S, Johnston K, Berry SA, Sweetman L, 3-Hydroxyisovalerylcarnitine in patients with deficiency of 3-methylcrotonyl CoA carboxylase, Clin Chim Acta 240 (1995) 35–51. [DOI] [PubMed] [Google Scholar]
- [7].Maeda Y, Ito T, Ohmi H, Yokoi K, Nakajima Y, Ueta A, Kurono Y, Togari H, Sugiyama N, Determination of 3-hydroxyisovalerylcarnitine and other acylcarnitine levels using liquid chromatography-tandem mass spectrometry in serum and urine of a patient with multiple carboxylase deficiency. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci 870 (2008) 154–159. [DOI] [PubMed] [Google Scholar]
- [8].Sweetman L, Williams JC, Branched chain organic acidurias (Scriver CR, Beaudet AL, Sly WS, Valle D, editors), The metabolic and molecular bases of inherited disease. 7th ed New York: McGraw-Hill Inc; 1995. p. 1387–1422 [Google Scholar]
- [9].Kirkby B, Roman N, Kobe B, Kellie S, Forwood JK, Functional and structural properties of mammalian acyl-coenzyme A thioesterases, Prog. Lipid Res 49 (2010) 366–377. [DOI] [PubMed] [Google Scholar]
- [10].Tillander V, Arvidsson Nordström E, Reilly J, Strozyk M, Van Veldhoven PP, Hunt MC, Alexson SE, Acyl-CoA thioesterase 9 (ACOT9) in mouse may provide a novel link between fatty acid and amino acid metabolism in mitochondria, Cell Mol. Life Sci 71 (2014) 933–948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Faull KF, Bolton PD, Halpern B, Hammond J, Danks DM, The urinary organic acid profile associated with 3-hydroxy-3-methylglutaric aciduria, Clin. Chim. Acta 73 (1976) 553–559. [DOI] [PubMed] [Google Scholar]
- [12].Wysocki SJ, French NP, Grauaug A, Organic aciduria associated with isovaleric acidemia, Clin. Chem 29 (1983) 1002–1003. [PubMed] [Google Scholar]
- [13].Roe CR, Millington DS, Maltby DA, Identification of 3-methylglutarylcarnitine. A new diagnostic metabolite of 3-hydroxy-3-methylglutaryl-coenzyme A lyase deficiency, J. Clin. Invest 77 (1986) 1391–1394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Wagner GR, Bhatt DP, O’Connell TM, Thompson JW, Dubois LG, Backos DS, Yang H, Mitchell GA, Ilkayeva OR, Stevens RD, Grimsrud PA, Hirschey MD, A Class of Reactive Acyl-CoA Species Reveals the Non-enzymatic Origins of Protein Acylation, Cell Metab 25 (2017) 823–837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Ikon N, Ryan RO, Barth Syndrome: Connecting Cardiolipin to Cardiomyopathy, Lipids 52 (2017) 99–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Ikon N, Ryan RO, On the origin of 3-methylglutaconic acid in disorders of mitochondrial energy metabolism, J. Inherit. Metab. Dis 39 (2016) 749–756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Suh JW, Lee SH, Chung BC, GC-MS determination of organic acids with solvent extraction after cation-exchange chromatography. Clin. Chem 43 (1997) 2256–2261. [PubMed] [Google Scholar]
- [18].Engelke UF, Kremer B, Kluijtmans LA, van der Graaf M, Morava E, Loupatty FJ, Wanders RJ, Moskau D, Loss S, van den Bergh E, Wevers RA, NMR spectroscopic studies on the late onset form of 3-methylglutaconic aciduria type I and other defects in leucine metabolism. NMR Biomed 19 (2006) 271–278. [DOI] [PubMed] [Google Scholar]
- [19].Wortmann SB, Duran M, Anikster Y, Barth PG, Sperl W, Zschocke J, Morava E, Wevers RA, Inborn errors of metabolism with 3-methylglutaconic aciduria as discriminative feature: proper classification and nomenclature. J. Inherit. Metab. Dis 36 (2013) 923–928. [DOI] [PubMed] [Google Scholar]
- [20].Pié J, López-Viñas E, Puisac B, Menao S, Pié A, Casale C, Ramos FJ, Hegardt FG, Gómez-Puertas P, Casals N, Molecular genetics of HMG-CoA lyase deficiency. Mol. Genet. Metab 92 (2007) 198–209. [DOI] [PubMed] [Google Scholar]
- [21].Spergel CD, Milko M, Edwards C, Steinhoff JP, 3-Methylglutaconyl-Coenzyme-A Hydratase Deficiency and the Development of Dilated Cardiomyopathy. Cardiol. Res 5 (2014) 158–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Finsterer J, Barth syndrome: mechanisms and management. Appl. Clin. Genet 12 (2019) 95–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Davey KM, Parboosingh JS, McLeod DR, Chan A, Casey R, Ferreira P, Snyder FF,Bridge PJ, Bernier FP, Mutation of DNAJC19, a human homologue of yeast inner mitochondrial membrane co-chaperones, causes DCMA syndrome, a novel autosomal recessive Barth syndrome-like condition. J. Med. Genet 43 (2006) 385–393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Anderson KA, Huynh FK, Fisher-Wellman K, Stuart JD, Peterson BS, Douros JD, Wagner GR, Thompson JW, Madsen AS, Green MF, Sivley RM, Ilkayeva OR, Stevens RD, Backos DS, Capra JA, Olsen CA, Campbell JE, Muoio DM, Grimsrud PA, Hirschey MD, SIRT4 Is a lysine deacylase that controls leucine metabolism and insulin secretion, Cell Metab 25 (2017) 838–855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Jooste S, Erasmus E, Mienie LJ, de Wet WJ, Gibson KM, The detection of 3-methylglutarylcarnitine and a new dicarboxylic conjugate, 3-methylglutaconylcarnitine, in 3-methylglutaconic aciduria, Clin. Chim. Acta 230 (1994) 1–8. [DOI] [PubMed] [Google Scholar]
- [26].Santarelli F, Cassanello M, Enea A, Poma F, D’Onofrio V, Guala G, Garrone G, Puccinelli P, Caruso U, Porta F, Spada M, A neonatal case of 3-hydroxy-3-methylglutaric-coenzyme A lyase deficiency, Ital. J. Pediatr 39 (2013) 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Duran M, Ketting D, Wadman SK, Jakobs C, Schutgens RB, Veder HA, Organic acid excretion in a patient with 3-hydroxy-3-methylglutaryl-CoA lyase deficiency: facts and artefacts, Clin. Chim. Acta 90 (1978) 187–193. [DOI] [PubMed] [Google Scholar]
- [28].Stacey TE, de Sousa C, Tracey BM, Whitelaw A, Mistry J, Timbrell P, Chalmers RA, Dizygotic twins with 3-hydroxy-3-methylglutaric aciduria; unusual presentation, family studies and dietary management, Eur. J. Pediatr 144 (1985) 177–81. [DOI] [PubMed] [Google Scholar]
- [29].Colín-González AL, Paz-Loyola AL, de Lima ME ME, Galván-Arzate S, Seminotti B, Ribeiro CA, Leipnitz G, Souza DO, Wajner M, Santamaría A, Experimental evidence that 3-methylglutaric acid disturbs mitochondrial function and induced oxidative stress in rat brain synaptosomes: new converging mechanisms, Neurochem. Res 41 (2016) 2619–2626. [DOI] [PubMed] [Google Scholar]
- [30].da Rosa MS, Seminotti B, Amaral AU, Fernandes CG, Gasparotto J, Moreira JC, Gelain DP, Wajner M, Leipnitz G, Redox homeostasis is compromised in vivo by the metabolites accumulating in 3-hydroxy-3-methylglutaryl-CoA lyase deficiency in rat cerebral cortex and liver, Free Radic. Res 47 (2013) 1066–1075. [DOI] [PubMed] [Google Scholar]
- [31].Ribeiro CAJ, Hickmann FH, Wajner M, Neurochemical evidence that 3-methylglutaric acid inhibits synaptic Na+,K+-ATPase activity probably through oxidative damage in brain cortex of young rats, Int. J. Dev. Neurosci 29 (2011) 1–7. [DOI] [PubMed] [Google Scholar]
- [32].Kelley RI, Cheatham JP, Clark BJ, Nigro MA, Powell BR, Sherwood GW, Sladky JT, Swisher WP, X-linked dilated cardiomyopathy with neutropenia, growth retardation, and 3-methylglutaconic aciduria, J. Pediatr 119 (1991) 738–747. [DOI] [PubMed] [Google Scholar]
- [33].Yoo TY, Kim MR, Son JS, Lee R, Bae SH, Chung S, Kim KS, Seong MW, Park SS, Identification of a novel de novo mutation of the TAZ Gene in a Korean patient with Barth Syndrome, J. Cardiovasc. Ultrasound 24 (2016) 153–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Ojala T, Polinati P, Manninen T, Hiippala A, Rajantie J, Karikoski R, Suomalainen A, Tyni T, New mutation of mitochondrial DNAJC19 causing dilated and noncompaction cardiomyopathy, anemia, ataxia, and male genital anomalies, Pediatr. Res 72 (2012) 432–437. [DOI] [PubMed] [Google Scholar]
- [35].Ucar SK, Mayr JA, Feichtinger RG, Canda E, Çoker M, Wortmann SB, Previously Unreported Biallelic Mutation in DNAJC19: Are Sensorineural Hearing Loss and Basal Ganglia Lesions Additional Features of Dilated Cardiomyopathy and Ataxia (DCMA) Syndrome?, JIMD Rep 35 (2017) 39–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Tort FF, García-Silva MT, Ferrer-Cortès X, Navarro-Sastre A, Garcia-Villoria J, Coll MJ, Vidal E, Jiménez-Almazán J, Dopazo J, Briones P, Elpeleg O, Ribes A, Exome sequencing identifies a new mutation in SERAC1 in a patient with 3-methylglutaconic aciduria, Mol. Genet. Metab 110 (2013) 73–77. [DOI] [PubMed] [Google Scholar]
- [37].Lumish HS, Yang Y, Xia F, Wilson A, Chung WK, The Expanding MEGDEL Phenotype: Optic Nerve Atrophy, Microcephaly, and Myoclonic Epilepsy in a Child with SERAC1 Mutations, JIMD Rep 16 (2014) 75–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Tort F, Del Toro M, Lissens W, Montoya J, Fernàndez-Burriel M, Font A, Buján N, Navarro-Sastre A, López-Gallardo E, Arranz JA, Riudor E, Briones P, Ribes A, Screening for nuclear genetic defects in the ATP synthase-associated genes TMEM70, ATP12 and ATP5E in patients with 3-methylglutaconic aciduria, Clin Genet 80 (2011) 297–300. [DOI] [PubMed] [Google Scholar]
- [39].Shchelochkov OA, Li FY, Wang J, Zhan H, Towbin JA, Jefferies JL, Wong LJ LJ, Scaglia F, Milder clinical course of Type IV 3-methylglutaconic aciduria due to novel mutation in TMEM70, Mol. Genet. Metab 101 (2010) 282–285. [DOI] [PubMed] [Google Scholar]
- [40].Holme E, Greter J, Jacobson CE, Larsson NG, Lindstedt S, Nilsson KO, Oldfors A, Tulinius M, Mitochondrial ATP-synthase deficiency in a child with 3-methylglutaconic aciduria. Pediatr. Res 32 (1992) 731–735. [DOI] [PubMed] [Google Scholar]
- [41].Kanabus M, Shahni R, Saldanha JW, Murphy E, Plagnol V, Hoff WV, Heales S, Rahman S, Bi-allelic CLPB mutations cause cataract, renal cysts, nephrocalcinosis and 3-methylglutaconic aciduria, a novel disorder of mitochondrial protein disaggregation, J. Inherit. Metab. Dis 38 (2015) 211–219. [DOI] [PubMed] [Google Scholar]
- [42].Semeraro M, Boenzi S, Carrozzo R, Diodato D, Martinelli D, Olivieri G, Antonetti G, Sacchetti E, Catesini G, Rizzo C, Dionisi-Vici C, The urinary organic acids profile in single large-scale mitochondrial DNA deletion disorders, Clin. Chim. Acta 481 (2018)156–160. [DOI] [PubMed] [Google Scholar]
- [43].Zeharia A, Friedman JR, Tobar A, Saada A, Konen O, Fellig Y, Shaag A, Nunnari J, Elpeleg O, Mitochondrial hepato-encephalopathy due to deficiency of QIL1/MIC13 (C19orf70), a MICOS complex subunit, Eur. J. Hum. Genet 24 (2016) 1778–1782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Tort F, Ugarteburu O, Texidó L, Gea-Sorlí S, García-Villoria J, Ferrer-Cortès X, Arias A, Matalonga L, Gort L, Ferrer I, Guitart-Mampel M, Garrabou G, Vaz FM, Pristoupilova A, Rodríguez MIE, Beltran S, Cardellach F, Wanders RJ, Fillat C, García-Silva MT, Ribes A, Mutations in TIMM50 cause severe mitochondrial dysfunction by targeting key aspects of mitochondrial physiology. Hum. Mutat 40 (2019) 1700–1712. [DOI] [PubMed] [Google Scholar]