Abstract
Background.
This study assessed the independent associations between participation in self-reported sport and exercise activities and incident cardiovascular disease.
Methods.
Data were from 13,204 participants in the Atherosclerosis Risk in Communities (ARIC) Study cohort (1987–2015). Baseline sport and exercise activities were assessed via the modified Baecke questionnaire. Incident cardiovascular disease included coronary heart disease, heart failure, or stroke. Multivariable-adjusted Cox proportional hazard models assessed the association of participation in specific sport and exercise activities at enrollment with risk of cardiovascular disease.
Results.
During a median follow-up time of 25.2 years, 30% of the analytic sample (n=3,966) were diagnosed with incident cardiovascular disease. In fully adjusted models, participation in racquet sports (hazard ratio [HR] 0.75; 95% confidence interval [CI] 0.61, 0.93), aerobics (HR 0.75; 95% CI 0.63, 0.88), running (HR 0.68; 95% CI 0.54, 0.85), and walking (HR 0.89; 95% CI 0.83, 0.95) were significantly associated with a lower cardiovascular disease risk. There were no significant associations for bicycling, softball/baseball, gymnastics, swimming, basketball, calisthenics exercises, golfing with cart, golfing with walking, bowling, or weight training.
Conclusions.
Participation in specific sports and exercises may substantially reduce risk for cardiovascular disease.
INTRODUCTION
There is substantial evidence of an inverse dose-response relationship between physical activity and cardiovascular disease (CVD) risk.1,2 Physical activity is also important for the prevention and management of risk factors for CVD such as obesity, hypertension, dyslipidemia, and insulin resistance.3,4 However, research on the association of specific sport and exercise participation on health outcomes such as CVD is limited.5 The majority of studies that have examined the association between various sport and exercise types and health outcomes have been cross-sectional.5 Furthermore, the few intervention studies of the association of sports participation have had limited scope, mainly examining running and soccer/football.5 Prospective cohort studies have examined walking, running, bicycling, and swimming, but the results have been mixed.6–11 There is evidence of a dose-response relation between walking and bicycling and all-cause mortality.6 For cardiovascular health specifically, there is evidence of a dose-response relationship between walking and coronary heart disease (CHD).7 Running has been shown to be inversely associated with CVD incidence and mortality in some, but not all studies, with no clear indication of a dose-response relationship.8–11 Swimming and bicycling historically have shown no association with CVD incidence;11 however, a recent study reported an inverse dose-response relationship between activities such as swimming, racquet sports, and aerobics with CVD mortality.10
It is important to recognize that physical activity occurs through participation in a specific sport or exercise activity, rather than as a general level of intensity (light, moderate, vigorous) or metabolic equivalent of task (MET) value. Data from the 2011 Behavioral Risk Factor Surveillance System (BRFSS) and the 1999–2006 National Health and Nutrition Examination Survey (NHANES) indicate that for sport and exercise participation within the past month, United States’ adults most commonly report walking.12,13 In addition to walking, sport and exercise activities including running, conditioning exercises, bicycling, and dancing/aerobics are also regularly reported.12,13 These various sport and exercise activities require use of different muscle groups and movements and have distinct energy costs and requirements.14 When comparing two or more sport and exercise activities, while they may have similar MET values, they may also require the use of different muscle groups, different consistency in movement, or different types of movement that vary in intensity. In addition, some sports and exercise activities may be more conducive to longer bouts of activity at a given time, and regular participation over a lifetime. These differences may lead to differential effects on cardiovascular health, above and beyond the effect of total energy expenditure alone.
A systematic review by Oja and colleagues called on the research community to examine the association of different sports on health outcomes.5 Sports and exercise are a feasible way to address the current state of inactivity in the population.15 Further, it is essential to consider what types of sport and exercise activities can provide the largest impact on population health, given that only a small proportion of a person’s day may be committed to leisure-time physical activity. The aim of this study was to examine the independent associations between participation in the most frequently reported types of sport and exercise and incident CVD.
METHODS
Study Population
Data for this analysis are from the Atherosclerosis Risk in Communities (ARIC) Study, a multicenter prospective cohort study that began in 1987. The ARIC methodology and study population have been previously described.16 Briefly, male and female participants were aged 45–64 years at baseline, and resided in one of the four study communities: Forsyth County, North Carolina; Jackson, Mississippi; suburban Minneapolis, Minnesota; and Washington County, Maryland. Baseline data collection was conducted between 1987 and 1989. Data were collected via home interview, clinic examinations, annual telephone follow-up, and diagnosis of clinical events. Events were investigated by review of hospital records and by query of physicians and family members and were given standardized diagnoses. The Institutional Review Boards at all participating institutions (University of North Carolina at Chapel Hill, Wake Forest Baptist Medical Center, University of Mississippi Medical Center, University of Minnesota, and Johns Hopkins University) approved study protocols, and all participants provided written informed consent at each study visit.
Exposure – Sport and Exercise Activities
Participation in sport and exercise activities was assessed via an interviewer administered modified Baecke Questionnaire at baseline.17 As part of the Baecke Questionnaire, participants were asked to report up to four sport or exercise activities that they most often performed in the past year. For each sport or exercise activity reported, participants were asked to report how many hours per week and how many months per year they do this sport/exercise. Information provided was converted to minutes/week for each activity. The Baecke Questionnaire also asked about television watching during leisure time (a proxy for sedentary behavior) and walking and/or bicycling to and from work or shopping (a proxy for active transportation).
Activities chosen for this analysis were based on sample size and assumed purpose; any activity that had at least 100 participants and was not potentially performed to acquire food (i.e., hunting, fishing, gardening) was included. Some activities were combined if they were considered to be conceptually similar as well as having comparable MET values (e.g., softball and baseball).14 The following activities were examined: aerobics, basketball, bicycling, bowling, calisthenics, golfing with cart, golfing with walking, gymnastics, racquet sports, running, softball/baseball, swimming, walking, and weight training (Supplemental Table 1). For the purposes of this analysis, a binary (yes/no) variable for each sport/exercise was created; participants were categorized as participating in a specific sport/exercise if they reported performing said sport in the past year; participants were otherwise categorized as a non-participant for that sport/exercise.
Outcome – Incident CVD
The primary outcome for this study was incident CVD. As part of the ARIC Study, CVD events were identified via annual interviews, study visits, and community-wide surveillance of hospitalization discharge listings and vaflidated via physician review. For this analysis, incident CVD was defined as the first identified incident CHD, heart failure, or stroke.18 CHD was defined as definite or probable myocardial infarction, fatal CHD, or coronary revascularization. Definite or probable heart failure was defined as first occurrence of hospitalization of heart failure via hospital discharge code.19 Definite or probable stroke was identified via a computer algorithm based on criteria adapted from the National Survey of Stroke,20 which utilized classification, signs, symptoms, neuroimaging, and other diagnostic reports.21
Covariates
Socio-demographic factors identified as potential confounders via previous literature, but not theorized to be on the causal pathway, were tested for their association with the outcomes of interest and two exposures (bicycling and swimming) using chi-squared tests and t-tests. Final covariates, assessed at baseline, included age (calculated from self-reported date of birth), sex, smoking status (current, former, never), alcohol consumption (current, former, never), race by study site (due to differential distribution of race by study site; Black – Jackson, Black – Forsyth County, White – Forsyth County, White – Minneapolis, White – Washington County), education (basic [highest grade completed in school < 11 and not missing], intermediate [highest grade completed in school 12–16], advanced [highest grade completed in school 17–21]), annual household income (<$25,000, $25,000-$34,999, $35,000-$49,999, $50,000+, not reported), marital status (married, not married), active transportation (minutes per day: <5, 5 to <15, 15 to <30, 30 to <45, 45+), and television watching (never, seldom, sometimes, often, very often) . Body mass index (BMI) was also included as a covariate, calculated from measured height and weight and categorized as underweight/normal weight if less than 25 kg/m2, overweight if between 25 kg/m2 and 30 kg/m2, and obese if greater than or equal to 30 kg/m2. Total sport/exercise minutes/week minus the minutes/week spent in the specific activity under study was further included as a covariate.
Statistical analyses
Participants from the Minneapolis, Minnesota and Washington County, Maryland sites were primarily white, while all Jackson participants were black. This differential distribution of race by study site resulted in small sample sizes for black participants from Minneapolis and Washington County (n=44), as well as non-white/non-black participants from all sites (n=45); these participants were therefore excluded. Participants with prevalent CVD, defined as CHD (n=766), heart failure (n=752), or stroke (n=284) at cohort enrollment, were excluded from this analysis (total n=1,802). Prevalent CHD was identified via self‐reported prior physician diagnosis of myocardial infarction or coronary revascularization, or prevalent myocardial infarction by 12‐lead electrocardiogram. Prevalent heart failure was identified via participant reported medication use for heart failure or the Gothenburg Criteria.22 Prevalent stroke was identified via self-reported physician diagnosed stroke. Participants with missing data for relevant covariates were also excluded from this analysis (n=881). Finally, participants with less than 1 year of follow-up were excluded (n=49).
Cox proportional hazard models [Hazard Ratios (HR) and 95% Confidence Intervals (CI)] were used to assess the association between any participation (yes/no) in a sport/exercise activity and risk of CVD; the reference group was participants who did not report participation in that activity. Unadjusted models were first examined for each of the sport/exercise activities and outcomes. Sport/exercise activities that showed a significant association with an outcome (p<0.05) were then examined in a multivariable model, adjusted for covariates. Multivariable models were also adjusted for total minutes of sport/exercise participation minus the time spent in the sport/exercise activity being examined, such that the association of that specific activity with CVD above and beyond all other sport/exercises that could be examined. Proportional hazard assumptions were checked by examining Schoenfeld residuals and log-minus-log plots in the fully adjusted single-activity models. The hazards were not proportional; age and sex were identified as problematic. An interaction between age and sex was added to all models; the proportional hazard assumption was checked again and found to be proportional. Final models controlled for the following covariates: baseline age, sex, age*sex, smoking status, alcohol consumption, race by study site, education, income, marital status, television watching, active transportation, BMI, and total sport/exercise minutes/week minus the minutes/week spent in the specific activity under study.
Follow-up was to event, loss to follow-up, death, or end of follow-up (December 31, 2015). Sensitivity analyses were conducted. First, to assess the potential for reverse causality, individuals who were diagnosed with CVD (n=182) within the first 24 months of follow-up were excluded from the dataset and the models were then re-analyzed. Second, to assess the influence of a purposeful amount of time spent in a specific sport/exercise activity greater than “any” (which could theoretically be one minute of activity) versus “none”, minutes/week of participation in each sport/exercise activity was categorized as ≥ 30 minutes/week (yes, no) and examined as the exposure. Third, to assess the influence of more than two categories of an exposure, minutes/week of participation in each sport/exercise activity was categorized into tertiles and included as the exposure. For these tertiles, all individuals who did not participate in the activity under consideration were categorized into the lowest tertile (and set as the referent), and those individuals who did participate in the activity were dichotomized based on the distribution of the time spent for that specific activity. All statistical tests were at 5% significance level. Analyses were conducted in 2018 using STATA, version 15.0 (College Station, TX).
RESULTS
A total of 15,792 participants were enrolled in the ARIC Study. After excluding participants with prevalent CVD at baseline, non-white/non-black participants from all sites, black participants from Minneapolis and Washington County, and missing data for relevant covariates, the final analytic sample included 13,204 participants. Over a median follow-up time of 25.2 years (ranging from 3 days to 29.1 years), 30% of the analytic sample (n=3,966) were diagnosed with incident CVD; 1365 were diagnosed with heart failure only, 740 with CHD only, 590 with stroke only, and 1,271 with multiple CVD diagnoses during follow-up. Among 13,204 participants, the crude incidence rate for CVD was 14.3 per 1,000 person-years (95% CI 13.9, 14.8). In general, participants with incident CVD were older at baseline and more likely to be a male, current smoker, never alcohol user, Black from the Jackson site, have a basic education, and have a household income <$25,000 per year (Table 1). Overall, participants with incident CVD acquired less physical activity minutes in a typical week and were less likely to have reported participation in any specific sport. In this sample, 63.8% of participants reported participating in at least one sport/exercise activity; the five most commonly reported sport/exercise activities were walking, bicycling, calisthenics, aerobics, and swimming.
Table 1.
Descriptive characteristics of the study sample at baseline by incident CVD status; The ARIC Study, 1987–2015
| Variable | Total n=13,204 |
Incident CVD n=3,966 |
No Incident CVD n=9,238 |
|---|---|---|---|
| Age; mean (SD) | 54.0 (5.7) | 55.7 (5.6) | 53.2 (5.6) |
| Sex; n (%) | |||
| Male | 5,812 (44.0) | 1,995 (50.3) | 3,817 (41.3) |
| Female | 7,392 (56.0) | 1,971 (49.7) | 5,421 (58.7) |
| Smoking status; n (%) | |||
| Never | 5,662 (42.9) | 1,412 (35.6) | 4,250 (46.0) |
| Former | 4,178 (31.6) | 1,293 (32.6) | 2,885 (31.2) |
| Current | 3,364 (25.5) | 1,261 (31.8) | 2,103 (22.8) |
| Alcohol consumption; n (%) | |||
| Never | 3,273 (24.8) | 1,050 (26.5) | 2,223 (24.1) |
| Former | 2,327 (17.6) | 855 (21.6) | 1,472 (15.9) |
| Current | 7,604 (57.6) | 2,061 (52.0) | 5,543 (60.0) |
| Race by study site; n (%) | |||
| Black (Jackson) | 2,906 (22.0) | 1,067 (26.9) | 1,839 (19.9) |
| Black (Forsyth) | 388 (2.9) | 124 (3.1) | 264 (2.9) |
| White (Forsyth) | 3,122 (23.6) | 855 (21.6) | 2,267 (24.5) |
| White (Minneapolis) | 3,555 (26.9) | 864 (21.8) | 2,691 (29.1) |
| White (Washington) | 3,233 (24.5) | 1,056 (26.6) | 2,177 (23.6) |
| Education; n (%) | |||
| Basic | 2,878 (21.8) | 1,215 (30.6) | 1,663 (18.0) |
| Intermediate | 5,459 (41.3) | 1,541 (38.9) | 3,918 (42.4) |
| Advanced | 4,867 (36.9) | 1,210 (30.5) | 3,657 (39.6) |
| Annual household income; n (%) | |||
| <$25,000 | 4,423 (33.5) | 1,679 (42.3) | 2,744 (29.7) |
| $25,000–$34,999 | 2,244 (17.0) | 678 (17.1) | 1,566 (17.0) |
| $35,000–$49,999 | 2,513 (19.0) | 656 (16.5) | 1,857 (20.1) |
| $50,000+ | 3,261 (24.7) | 712 (18.0) | 2,549 (27.6) |
| Not reported | 763 (5.8) | 241 (6.1) | 522 (5.7) |
| Marital status; n (%) | |||
| Not married | 2,484 (18.8) | 849 (21.4) | 1,635 (17.7) |
| Married | 10,720 (81.2) | 3,117 (78.6) | 7,603 (82.3) |
| Television watching; n (%) | |||
| Never/seldom | 2,557 (19.4) | 671 (16.9) | 1,886 (20.4) |
| Sometimes | 6,224 (47.1) | 1,786 (45.0) | 4,438 (48.0) |
| Often | 3,457 (26.2) | 1,103 (27.8) | 2,354 (25.5) |
| Very Often | 966 (7.3) | 406 (10.2) | 560 (6.1) |
| BMI; n (%) | |||
| Underweight/normal weight | 4,559 (34.5) | 1,061 (26.8) | 3,498 (37.9) |
| Overweight | 5,214 (39.5) | 1,584 (40.0) | 3,630 (39.3) |
| Obese | 3,431 (26.0) | 1,321 (33.3) | 2,110 (22.8) |
| Active transportation min/day; n (%) | |||
| <5 | 4,791 (36.3) | 1,472 (37.1) | 3,319 (35.9) |
| 5 to <15 | 3,648 (27.6) | 1,072 (27.0) | 2,576 (27.9) |
| 15 to <30 | 2,723 (20.6) | 801 (20.2) | 1,922 (20.8) |
| 30 to <45 | 1,249 (9.5) | 362 (9.1) | 887 (9.6) |
| 45 + | 793 (6.0) | 259 (6.5) | 534 (5.8) |
| Total physical activity minutes/week; median (IQR) | 91.8 (248.5) | 63.0 (220.9) | 100.8 (248.5) |
| Sport activity participation; n (%) | |||
| Aerobics | 762 (5.8) | 149 (3.8) | 613 (6.6) |
| Basketball | 209 (1.6) | 52 (1.3) | 157 (1.7) |
| Bicycling | 1,581 (12.0) | 393 (9.9) | 1,188 (12.9) |
| Bowling | 540 (4.1) | 160 (4.0) | 380 (4.1) |
| Calisthenics | 1,054 (8.0) | 253 (6.4) | 801 (8.7) |
| Golf using a cart | 623 (4.7) | 195 (4.9) | 428 (4.6) |
| Golf with walking | 648 (4.9) | 159 (4.0) | 489 (5.3) |
| Gymnastics | 244 (1.9) | 67 (1.7) | 177 (1.9) |
| Racquet sports | 506 (3.8) | 89 (2.2) | 417 (4.5) |
| Running | 447 (3.4) | 76 (1.9) | 371 (4.0) |
| Softball/baseball | 267 (2.0) | 80 (2.0) | 187 (2.0) |
| Swimming | 709 (5.4) | 177(4.5) | 532 (5.8) |
| Walking | 5,313 (40.2) | 1,379 (34.8) | 3,934 (42.6) |
| Weight training | 364 (2.8) | 74 (1.9) | 290 (3.1) |
Note: CVD = cardiovascular disease; ARIC = the Atherosclerosis Risk in Communities Study; SD = standard deviation; IQR = interquartile range
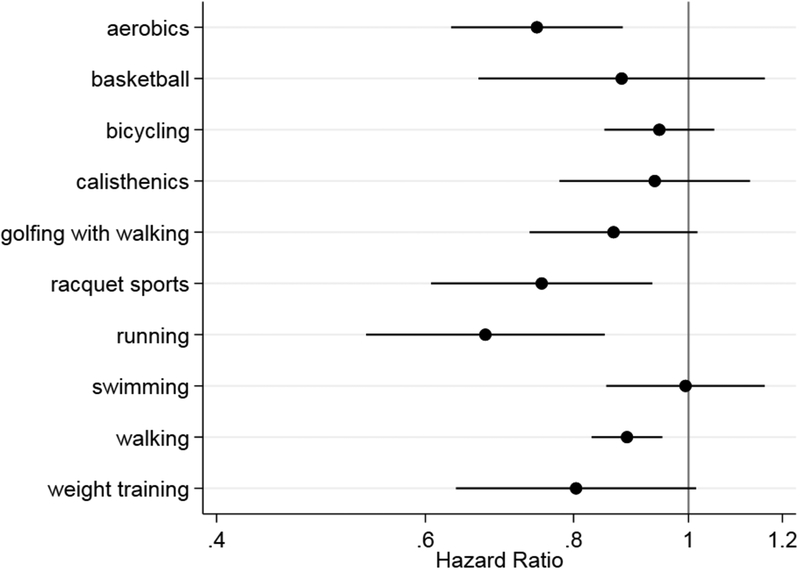
Unadjusted Cox models (Supplemental Table 2) indicated that participation in softball/baseball, gymnastics, golfing with cart, and bowling were not significantly associated with risk of incident CVD; therefore, these sports were dropped from further analysis in the multivariable models. In multivariable Cox models, racquet sports (HR 0.75; 95% CI 0.61, 0.93), aerobics (HR 0.75; 95% CI 0.63, 0.88), running (HR 0.68; 95% CI 0.54, 0.85), and walking (HR 0.89; 95% CI 0.83, 0.95) were significantly associated with incident CVD (Figure 1, Supplemental Table 2). In sensitivity analyses, excluding participants who were diagnosed with CVD within the first 24 months of follow-up (n=182) did not notably change the strength of the associations (Table 2). Further, categorizing activities as ≥30 minutes/week (yes, no) did not produce notably different findings in terms of point estimates or significance (Table 3). Categorizing the activities into distribution based tertiles did not notably change the hazard ratio point estimates, but in some instances the significance level was attenuated (likely due to a reduction in sample size for any one category) (Supplemental Table 3).
Figure 1.
Single activity model estimates for the adjusted association between participation in each sport/exercise activity and risk for incident CVD; The ARIC Study, 1987–2015 (n=13,204) Note: CVD = cardiovascular disease; ARIC = the Atherosclerosis Risk in Communities Study. All models adjusted for marital status, income, race by study site, smoking, alcohol, education, age*sex, tv watching, body mass index (BMI), active transportation, and total physical activity minutes/week minus minutes/week for specific activity. Values for estimates and 95% confidence intervals are reported in Supplemental Table 2.
Table 2.
Adjusted association between participation in each sport/exercise and risk for incident CVD after excluding participants with CVD diagnosis within the first 24 months of follow-up; The ARIC Study, 1987–2015 (n=13,022)
| Sport/exercise | HR (95% CI)a.b |
|---|---|
| Bicycling | 0.93 (0.84, 1.04) |
| Racquet Sports | 0.76 (0.59, 0.98)* |
| Aerobics | 0.76 (0.64, 0.90)** |
| Running | 0.68 (0.54, 0.86)** |
| Swimming | 1.00 (0.85, 1.17) |
| Basketball | 0.90 (0.68, 1.20) |
| Calisthenics | 0.87 (0.76, 0.99)* |
| Walking | 0.88 (0.82, 0.95)** |
| Golf walking | 0.88 (0.75, 1.04) |
| Weight training | 0.81 (0.64, 1.03) |
p<0.05,
p<0.01
Note: CVD = Cardiovascular Disease; ARIC = Atherosclerosis Risk in Communities Study; HR = Hazard Ratio; CI = Confidence Interval
231 participants were excluded due to a CVD diagnosis within the first 24 months of follow-up
All models adjusted for marital status, income, race by study site, smoking, alcohol, education, age*sex, tv watching, BMI, active transportation, and total sport/exercise minutes/week minus minutes/week for specific activity
Table 3.
Adjusted association between participation in each sport/exercise categorized as ≥30 minutes per week and risk for incident CVD; The ARIC Study, 1987–2015 (n=13,204)
| Sport/exercisea | HR (95% CI)b |
|---|---|
| Aerobics | 0.74 (0.60, 0.90)** |
| Basketball | 0.92 (0.65, 1.29) |
| Bicycling | 1.03 (0.92, 1.16) |
| Calisthenics | 0.87 (0.75, 1.02) |
| Golf walking | 0.87 (0.73, 1.04) |
| Racquet Sports | 0.74 (0.57, 0.95)* |
| Running | 0.68 (0.53, 0.88)** |
| Swimming | 1.11 (0.92, 1.34) |
| Walking | 0.91 (0.85, 0.98)* |
| Weight training | 0.81 (0.62, 1.05) |
p<0.05,
p<0.01,
p<0.001
Note: CVD = Cardiovascular Disease; ARIC = Atherosclerosis Risk in Communities Study; HR = Hazard Ratio; CI = Confidence Interval
Categorized as ≥30 minutes per week, yes vs. no (referent)
All models adjusted for marital status, income, race by study site, smoking, alcohol, education, age*sex, tv watching, BMI, active transportation, and total sport/exercise minutes/week minus minutes/week for specific activity
DISCUSSION
In this large prospective cohort of men and women residing in the United States, the most commonly reported sport and exercise activities were examined for their association with risk of CVD. These sport and exercise activities included bicycling, softball/baseball, racquet sports, aerobics, gymnastics, running, swimming, basketball, calisthenics, walking, golfing with cart, golfing with walking, bowling, and weight training. It is evident that engaging in certain specific sport and exercise activities was significantly associated with reduced risk for CVD, even after controlling for time spent being physically active in other activities. The findings reported here suggest that, in this sample, self-reported participation in racquet sports (tennis, racquetball, and squash), aerobics, running, and walking provided greater cardiovascular benefit than participation in any of the other activities examined. When considering physical activity guidelines23 to reduce incident CVD, it may be of value to advise individuals to engage in activities associated with the largest cardiovascular benefit, while also being safe and enjoyable.
Many of the sport and exercise activities examined were inversely associated with incident CVD in unadjusted models (bicycling, racquet sports, running, swimming, basketball, calisthenics, walking, golfing with walking, and weight training); however, once sociodemographic factors were controlled for, fewer activities were associated with significant risk reduction for CVD. Interestingly, categorization of the explored sport/exercise activity time as ≥30 minutes/week, or as distribution based tertiles showed no substantial difference in risk reduction when compared to any participation in the sport/exercise activities. This builds upon previous evidence indicating that participation in any activity can be important for health.24
Walking was the most commonly reported leisure-time physical activity in this sample, a finding comparable to nationally representative samples.12,13 Although walking provides light or moderate intensity activity for most adults,14 it has generally been found to be associated with reduced CVD risk, including lower blood pressure and more favorable measures of adiposity.25 Previous research on walking has generally shown it to be associated with CVD, specifically in post-menopausal women26 and older adults.27 Walking has also been shown to have an inverse dose-response relationship with CVD such as stroke28 and CHD.7 The results presented here build upon this previous evidence through the inclusion of multiple types of CVD diagnosis in both men and women with a substantial follow-up time. Further, these findings support the United States Surgeon General’s call to action to promote walking and walkable communities.29 Walking is one of the most approachable types of sport or exercise activities examined here, in that it requires no special equipment or training. Walking as a type of physical activity should continue to be explored for cardiovascular health, with further consideration for specific aspects of the activity such as intensity.
Running inherently involves a baseline level of absolute vigorous intensity activity,14 in that if a person must perform a certain speed and stride of movement to be considered running rather than walking, which may be particularly beneficial for cardiovascular health. Conversely, aerobics generally uses the whole body and can provide both muscle strengthening as well as cardiovascular conditioning. Racquet sports, including squash, racquetball, and tennis also use muscles in both the upper and lower body, as well as providing cardiovascular conditioning at moderate to vigorous intensity level. Activities that reach a threshold level of intensity and engage the whole body may burn more calories per bout and strengthen more muscles, and therefore be particularly important for cardiovascular health in a manner over and above the other activities explored here.
To date, few other studies to date have examined as wide a breadth of sport activity in relation to CVD risk, with existing studies mainly focusing on all-cause mortality. Oja and colleagues (2017)10 examined different sport participation and risk for all-cause and CVD mortality in a British cohort. They found that in adjusted models, swimming, racquet sports, and aerobics were significantly associated with lower CVD mortality, while bicycling, running, and football (soccer) were not.10 More generally, most prospective cohort studies examining this topic have shown that activities such as tennis and running are associated with lower CVD mortality,8,11,30 although this association is primarily evident in men.11,30 Only one other study has examined risk for incident CVD in relation to different physical activities. They found that bicycling was associated with reduced risk, while walking was not.31 However, their operationalization of walking was at greater than or equal to 3.5 hours per week, which was substantially higher than the analysis reported here, which may in part explain the differential findings.
All of the activities explored here theoretically provide moderate-to-vigorous physical activity (>3 METs).14 Clearly not all result in reduced risk for CVD, after controlling for other physical activity, indicating that using METs alone may not fully account for or describe reported types of activity. One possibility for these disparate findings is that they are influenced by the amount of time spent in a specific sport or exercise activity at any one time. Some activities may typically be performed for a longer bout of time than others, for example, a session of tennis might be longer than a session of swimming. Although it is not possible to examine time spent in a single session for a sport or exercise activity with these data, when examining the mean minutes/week spent in each activity among those who participated, no clear pattern emerges to link time spent in the activity with reduced CVD risk. The highest mean minutes/week were reported for walking, followed by running, weight training, golfing with cart, bowling, and gymnastics (Supplemental Table 1). It is possible, however, that the sport and exercise activities found to be significantly associated with incident CVD have a combination of intensity, time spent in motion, and muscle group engagement that is particularly important for cardiovascular health.
Strengths and Limitations
This study is one of the few that have used a large prospective cohort of men and women to examine the association between specific sport and exercise activities and CVD. There are a few limitations to note. Firstly, as this is an observational study, causality cannot be determined. Further, this observational study cannot account for self-selection of the types of activities, such that people chose to do the activities for reasons that were not documented. Although a wide-ranging number of covariates were controlled for in multivariable models, residual confounding cannot be ruled out. In particular, while models controlled for other minutes/week spent in sport/exercise physical activity and minutes per day in active transportation, time spent in other physical activity domains, such as workplace physical activity, were not accounted for. This may have resulted in residual confounding, in that individuals who participate in physical activity in other domains may be less likely to participate in leisure-time physical activity.
Although the sample size was large and the length of follow-up was substantial, the number of individuals exposed to some examined sport and exercise activities may have limited the statistical power for these analyses. For example, in adjusted models the point estimate for walking was comparable to basketball and golf with walking, but potentially due to differing sample sizes walking indicated a significant association while the others did not. Although prevalent cases at baseline were excluded, and a sensitivity analysis was conducted excluding participants that were diagnosed within the first 24 months of follow-up, reverse causality is still a possibility. Sport and exercise participation examined in this study was measured at baseline only, so change in physical activity over time was not accounted for. Individuals may be likely to engage in certain types of sport and exercise activities into late life more than others, which may have influenced these findings. This is an important consideration for future research, however, in that some sport/exercise activities may have greater longevity of participation as compared to others, leading to greater reductions in CVD morbidity and mortality.
Some of the sports analyzed may be more uniform in their intensity (light, moderate, vigorous) than others. For example, the categorization of swimming included general recreational swimming as well as more specific swimming strokes at a speed threshold. These different activities were combined to increase the sample size but may have in turn reduced the independent association between high intensity swimming and CVD risk. Further, activities such as racquet sports and running may have a general threshold of intensity that most individuals meet during participation, whereas others, such as swimming or bicycling, can be performed below a threshold of intensity that may provide cardiovascular benefit. This may in part explain the observed differences compared with other studies that showed benefit for swimming and bicycling, for example, if the way these activities were measured differed in meaningful ways.
Conclusions
Physical activity is important for the primary and secondary prevention of CVD. Sport and exercise activities such as racquet sports, gym exercises, running, and walking showed significant inverse associations with CVD risk. Future research should explore how consistent participation in different sport and exercise activities, as well as change in these activities over time is associated with CVD risk. In practice, recommendations for individuals to engage in physical activity for cardiovascular health should consider what activities may provide the most substantial benefit, while at the same time being both safe and enjoyable for the individual. Physical activity occurs in the context of the built environment,32 and it is important to not only encourage individuals to be active, but to consider where these activities might occur. Therefore, communities seeking to promote physical activity should ensure that public spaces are available with resources that enable individuals to be active in ways that best promote health, such as tennis courts, walking/running tracks, trails/greenways, and outdoor fitness equipment.
Supplementary Material
ACKNOWLEDGEMENTS
The authors thank the staff and participants of the ARIC study for their important contributions.
FUNDING SOURCE
AKP was supported by a National Research Service Award postdoctoral research fellowship (T32-HL007055), funded by the National Institutes of Health National Heart, Lung, and Blood Institute. The Atherosclerosis Risk in Communities study has been funded in whole or in part with federal funds from the National Heart, Lung, and Blood Institute, National Institutes of Health, Department of Health and Human Services, under contract numbers (HHSN268201700001I, HHSN268201700002I, HHSN268201700003I, HHSN268201700004I, HHSN268201700005I).
REFERENCES
- 1.Alves AJ, Viana JL, Cavalcante SL, et al. Physical activity in primary and secondary prevention of cardiovascular disease: Overview updated. World J Cardiol. October 26 2016;8(10):575–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Physical Activity Guidelines Advisory Committee 2018 Physical Activity Guidelines Advisory Committee Scientific Report. Washington, DC: U.S. Department of Heatlh and Human Services; 2018. [Google Scholar]
- 3.Bassuk SS, Manson JE. Physical activity and the prevention of cardiovascular disease. Curr Atheroscler Rep. July 2003;5(4):299–307. [DOI] [PubMed] [Google Scholar]
- 4.Myers J. Cardiology patient pages. Exercise and cardiovascular health. Circulation. January 7 2003;107(1):e2–5. [DOI] [PubMed] [Google Scholar]
- 5.Oja P, Titze S, Kokko S, et al. Health benefits of different sport disciplines for adults: systematic review of observational and intervention studies with meta-analysis. British journal of sports medicine. 2015;49(7):434–440. [DOI] [PubMed] [Google Scholar]
- 6.Kelly P, Kahlmeier S, Götschi T, et al. Systematic review and meta-analysis of reduction in all-cause mortality from walking and cycling and shape of dose response relationship. Int J Behav Nutr Phys Act. 2014;11:132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zheng H, Orsini N, Amin J, Wolk A, Nguyen VT, Ehrlich F. Quantifying the dose-response of walking in reducing coronary heart disease risk: meta-analysis. Eur J Epidemiol. 2009;24(4):181–192. [DOI] [PubMed] [Google Scholar]
- 8.Lee DC, Pate RR, Lavie CJ, Sui X, Church TS, Blair SN. Leisure-time running reduces all-cause and cardiovascular mortality risk. J Am Coll Cardiol. August 5 2014;64(5):472–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chakravarty EF, Hubert HB, Lingala VB, Fries JF. Reduced disability and mortality among aging runners: a 21-year longitudinal study. Arch Intern Med. August 11 2008;168(15):1638–1646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Oja P, Kelly P, Pedisic Z, et al. Associations of specific types of sports and exercise with all-cause and cardiovascular-disease mortality: a cohort study of 80 306 British adults. Br J Sports Med. May 2017;51(10):812–817. [DOI] [PubMed] [Google Scholar]
- 11.Chomistek AK, Cook NR, Flint AJ, Rimm EB. Vigorous-intensity leisure-time physical activity and risk of major chronic disease in men. Med Sci Sports Exerc. October 2012;44(10):1898–1905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Watson KB, Frederick GM, Harris CD, Carlson SA, Fulton JE. U.S. Adults’ Participation in Specific Activities: Behavioral Risk Factor Surveillance System--2011. J Phys Act Health. June 16 2015;12 Suppl 1:S3–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dai S, Carroll DD, Watson KB, Paul P, Carlson SA, Fulton JE. Participation in Types of Physical Activities Among US Adults--National Health and Nutrition Examination Survey 1999–2006. Journal of physical activity & health. 2015;12 Suppl 1:S128–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ainsworth BE, Haskell WL, Herrmann SD, et al. 2011 Compendium of Physical Activities: a second update of codes and MET values. Med Sci Sports Exerc. August 2011;43(8):1575–1581. [DOI] [PubMed] [Google Scholar]
- 15.Khan KM, Thompson AM, Blair SN, et al. Sport and exercise as contributors to the health of nations. Lancet. July 07 2012;380(9836):59–64. [DOI] [PubMed] [Google Scholar]
- 16.The Atherosclerosis Risk in Communities (ARIC) Study: design and objectives. The ARIC investigators. Am J Epidemiol. April 1989;129(4):687–702. [PubMed] [Google Scholar]
- 17.Baecke JA, Burema J, Frijters JE. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am J Clin Nutr. November 1982;36(5):936–942. [DOI] [PubMed] [Google Scholar]
- 18.Kubota Y, Evenson KR, Maclehose RF, Roetker NS, Joshu CE, Folsom AR. Physical Activity and Lifetime Risk of Cardiovascular Disease and Cancer. Med Sci Sports Exerc. August 2017;49(8):1599–1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rosamond WD, Chang PP, Baggett C, et al. Classification of heart failure in the atherosclerosis risk in communities (ARIC) study: a comparison of diagnostic criteria. Circ Heart Fail. March 1 2012;5(2):152–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.The National Survey of Stroke. National Institute of Neurological and Communicative Disorders and Stroke. Stroke. Mar–Apr 1981;12(2 Pt 2 Suppl 1):I1–91. [PubMed] [Google Scholar]
- 21.Rosamond WD, Folsom AR, Chambless LE, et al. Stroke incidence and survival among middle-aged adults: 9-year follow-up of the Atherosclerosis Risk in Communities (ARIC) cohort. Stroke. April 1999;30(4):736–743. [DOI] [PubMed] [Google Scholar]
- 22.Eriksson H, Caidahl K, Larsson B, et al. Cardiac and pulmonary causes of dyspnoea--validation of a scoring test for clinical-epidemiological use: the Study of Men Born in 1913. Eur Heart J. September 1987;8(9):1007–1014. [DOI] [PubMed] [Google Scholar]
- 23.Services UDoHaH. Physical Activity Guidelines for Americans. 2nd ed Washington, DC: US Department of Health and Human Services; 2018. [Google Scholar]
- 24.Arem H, Moore SC, Patel A, et al. Leisure time physical activity and mortality: a detailed pooled analysis of the dose-response relationship. JAMA Intern Med. June 2015;175(6):959–967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Murtagh EM, Nichols L, Mohammed MA, Holder R, Nevill AM, Murphy MH. The effect of walking on risk factors for cardiovascular disease: an updated systematic review and meta-analysis of randomised control trials. Prev Med. March 2015;72:34–43. [DOI] [PubMed] [Google Scholar]
- 26.Manson JE, Greenland P, LaCroix AZ, et al. Walking compared with vigorous exercise for the prevention of cardiovascular events in women. N Engl J Med. September 5 2002;347(10):716–725. [DOI] [PubMed] [Google Scholar]
- 27.Soares-Miranda L, Siscovick DS, Psaty BM, Longstreth WT Jr., Mozaffarian D. Physical Activity and Risk of Coronary Heart Disease and Stroke in Older Adults: The Cardiovascular Health Study. Circulation. January 12 2016;133(2):147–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jefferis BJ, Whincup PH, Papacosta O, Wannamethee SG. Protective effect of time spent walking on risk of stroke in older men. Stroke. Jan 2014;45(1):194–199. [DOI] [PubMed] [Google Scholar]
- 29.Services USDoHaH. Step It Up! The Surgeon General’s Call to Action to Promote Walking and Walkable Communities. Washington, DC: U.S. Dept of Health and Human Services, Office of the Surgeon General; 2015. [Google Scholar]
- 30.Schnohr P, Marott JL, Lange P, Jensen GB. Longevity in male and female joggers: the Copenhagen City Heart Study. Am J Epidemiol. April 1 2013;177(7):683–689. [DOI] [PubMed] [Google Scholar]
- 31.Hoevenaar-Blom MP, Wendel-Vos GCW, Spijkerman AMW, Kromhout D, Verschuren WMM. Cycling and sports, but not walking, are associated with 10-year cardiovascular disease incidence: the MORGEN Study. European Journal of Cardiovascular Prevention & Rehabilitation. February 2011;18(1):41–47. [DOI] [PubMed] [Google Scholar]
- 32.Sallis JF, Floyd MF, Rodriguez DA, Saelens BE. Role of built environments in physical activity, obesity, and cardiovascular disease. Circulation. February 7 2012;125(5):729–737. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.