Abstract
Objectives:
Elevated blood cholesterol (hypercholesterolemia) is a significant cause of cardiovascular disease. We aimed to estimate national and zonal prevalence of hypercholesterolemia in Nigeria to help guide targeted public health programs.
Design:
This is a systematic review and synthesis of publicly available epidemiologic data on hypercholesterolemia in Nigeria.
Methods:
We systematically searched MEDLINE, EMBASE, Global Health, and Africa Journals Online for studies on the prevalence of hypercholesterolemia in Nigeria published between 1990 and 2018. We used a random-effects meta-analysis (Freeman-Tukey double arscine transformation) and meta-regression model to estimate the prevalence of hypercholesterolemia in Nigeria in 1995 and 2015.
Results:
13 studies (n=16981) were retrieved. The pooled crude prevalence of hypercholesterolemia in Nigeria was 38% (95% CI: 26–51), with prevalence in women slightly higher (42%, 23–63) compared to men at (38%, 20–58). The prevalence was highest in the South-south (53%, 38–68) and lowest in the South-west (3%, 2–4) and North-east (4%, 2–7). Urban dwellers had a significantly higher rate (52%, 24–79) compared to rural dwellers (10%, 6–15). We estimated over 8.2 million persons (age-adjusted prevalence 16.5%) aged 20 years or more had hypercholesterolemia in Nigeria in 1995, increasing to 21.9 million persons (age-adjusted prevalence 25.9%) in 2015.
Conclusions:
Our findings suggest a high prevalence of hypercholesterolemia in Nigeria. Urbanization, lifestyles, diets, and culture appear to be driving an increasing prevalence, especially among women. Population-wide awareness and education on reducing elevated cholesterol levels and associated risks should be prioritised.
Keywords: hypercholesterolemia, dyslipidaemia, prevalence, ischemic heart disease, Nigeria
INTRODUCTION
Elevated blood cholesterol (hypercholesterolemia) is a leading cause of disease burden, accounting for one-third of ischemic heart disease and one fifth of stroke1, 2. In 2015, hypercholesterolemia resulted in 4.5% and 2% of global deaths and disability-adjusted life years (DALYs), respectively3. Recent reports reveal a rising prevalence across many low- and middle-income countries, including Nigeria, with a quarter of adults affected3.
The rising burden of hypercholesterolemia in Nigeria corresponds with increasing rates of unhealthy diets and lifestyles in the population. A key driver of this is urbanization, and the corresponding expansion of processed food outlets in the country4, 5. Further, reports suggest that major cooking oils in the country are high in saturated fats, and these are often unbranded or content not displayed6. Though, even if this information was better reported, many people do not check fats or cholesterol content of cooking oils, due to limited population-wide information and awareness on associated risks6. There is also evidence of a growing number of Nigerians with sub-optimal levels of physical activity3, 7, another driver of poor cholesterol management.
Yet public health responses are largely absent across many settings8. Epidemiologic studies are few, thus limiting a precise understanding of the burden8, 9. Thus, we systematically searched and synthesized available data to estimate the national and zonal prevalence of hypercholesterolemia in Nigeria. Our primary goal is to raise awareness regarding this burden and to prompt relevant policy response and measures across the country.
METHODS
Search strategy
We searched MEDLINE, EMBASE, Global Health, and Africa Journals Online (AJOL), for studies on hypercholesterolemia or dyslipidemia in Nigeria using the search terms shown in Table 1. Searches were conducted on 01 August 2018 and limited to studies published after 1 January 1990. Unpublished documents were sourced from Google Scholar and Google searches. Titles and abstracts of studies were reviewed, and the full-text of relevant studies accessed. The reference lists of accessed full-texts were further hand-searched for additional studies. We contacted authors of selected papers for any missing information.
TABLE 1.
Search terms on hypercholesterolemia in Nigeria
| # | Searches |
|---|---|
| 1 | africa/ or africa, sub-sahara/ or africa, western/ or nigeria/ |
| 2 | exp vital statistics/ |
| 3 | (incidence* or prevalence* or morbidity or mortality).tw. |
| 4 | (disease adj3 burden).tw. |
| 5 | exp “cost of illness”/ |
| 6 | case fatality rate.tw |
| 7 | hospital admissions.tw |
| 8 | Disability adjusted life years.mp. |
| 9 | (initial adj2 burden).tw. |
| 10 | exp risk factors/ |
| 11 | 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 |
| 12 | exp dyslipidemia / or abnormal lipids / or abnormal cholesterol / or hypercholesterolemia /or elevated cholesterol |
| 13 | 1 and 11 and 12 |
| 14 | Limit 13 to “1990-current” |
Selection criteria
We selected population- or hospital-based studies reporting on the prevalence of hypercholesterolemia in a Nigerian setting. However, due to the high number of studies on cardio-metabolic risks identified from an initial scoping exercise reporting on cholesterol levels or any form of dyslipidemia, we also carefully reviewed several studies on NCDs risks in Nigeria and extracted data on hypercholesterolemia or population lipid levels from such studies when reported. We excluded studies on Nigerians in diaspora, reviews, case reports, viewpoints, and commentaries.
Case definitions
We checked for studies that defined hypercholesterolemia as elevated blood levels of total cholesterol, high low-density lipoprotein (LDL)-cholesterol, or high non-high-density lipoprotein (HDL)-cholesterol (which is the subtraction of HDL-cholesterol from total cholesterol)3. Some studies were based on dyslipidemia (i.e., abnormal lipid levels), as elevated cholesterol levels may be accompanied by a decrease in HDL-cholesterol or an increase in triglycerides. Hence, we also checked for studies that provided numerical estimates on elevated plasma cholesterol, triglycerides, or a low HDL cholesterol level, which satisfies a working definition of dyslipidemia3. However, to limit heterogeneity resulting from different case definitions in our analysis, we applied the United States National Heart, Lung, and Blood Institute recommended diagnostic criteria for hypercholesterolemia or dyslipidemia10 in our quality checks as follows: i) total cholesterol ≥200 mg/dl (5.2 mmol/l); ii) LDL-cholesterol ≥130 mg/dl (3.4 mmol/l); iv) HDL-cholesterol ≤40mg/dl (1.0 mmol/l); or v) triglyceride ≥150 mg/dl (1.7 mmol/l). We included any studies that reported estimates based on these diagnostic criteria.
Data extraction
Assessment of eligible studies was conducted independently by two reviewers (DA and AA), with an eligibility guideline to ensure that consistent selection criteria were applied. Any disagreement in study selection was resolved by consensus. Data on the location, study period, study design, study setting (urban or rural), sample size, diagnostic criteria, and mean age of the population were extracted. These were matched with corresponding data on persons with hypercholesterolemia, sample population, the prevalence of hypercholesterolemia in each study. For studies conducted on the same study site, population or cohort, the first published study was selected, and all additional data from the other studies were extracted and merged with data from the selected paper.
Quality assessment
For each full text selected, we further screened for an explicit description of methodology, case definitions, and generalizability of reported estimates to a larger population within the geopolitical zone. For quality grading, we adapted a previously used quality assessment criteria for studies examining the prevalence of chronic diseases11–14. For each full text selected, we screened for sampling strategy (was it representative of a target subnational population?), statistical methods (was it appropriate for the study outcome?), and case ascertainment (was it based on standard diagnostic criteria, unspecified clinical criteria, informant interviews, or not reported?). Studies were graded as high (4–5), moderate (2–3), or low quality (0–1) (see Tables 2 and 3, for details of all full-text manuscripts accessed and quality grading).
TABLE 2.
Quality assessment of selected studies
| Quality criteria | Assessment | Score | Maximum score |
|---|---|---|---|
| Sampling method (was it representative of a target subnational population?) | Yes | 1 | 1 |
| No | 0 | ||
| Appropriateness of statistical analysis | Yes | 1 | 1 |
| No | 0 | ||
| Case ascertainment (was it based on standard diagnostic criteria, other criteria or case definition, unclear, or not reported?) | Standard diagnostic criteria | 3 | 3 |
| Other criteria | 2 | ||
| unclear | 1 | ||
| Not-reported | 0 | ||
| Total (high (4–5), moderate (2–3), or low quality (0–1)) | 5 | ||
TABLE 3.
Characteristics of studies on prevalence of hypercholesterolemia in Nigeria
| Author | Study Period | Location | Geopolitical zone | Study design | Study Setting | Mean age (years) | Sample | Prevalence (%) | Quality |
|---|---|---|---|---|---|---|---|---|---|
| Agaba et al21 | 2014 | Jos, Plateau State | North-central | Population-based | Urban | 44 | 883 | 51.8 | High |
| Emerole et al22 | 2007 | Owerri, Imo State | South-east | Descriptive cross-sectional study | Urban | 53 | 241 | 91.3 | Moderate |
| Ugwuja et al23 | 2008 | Abakaliki, Ebonyi State | South-east | Descriptive cross-sectional study | Urban | 40.9 | 205 | 37.1 | Moderate |
| Oladapo et al24 | 2005 | Egbeda, Oyo State | South-west | Population-based | Rural | 42.1 | 2000 | 3.2 | Moderate |
| Odenigbo et al25 | 2009 | Asaba, Delta State | South-south | Hospital-based | Urban | 67 | 176 | 69.9 | Moderate |
| Okaka & Eiya26 | 2013 | Ovia, Edo state | South-south | Hospital-based | Rural | 48 | 161 | 31.7 | Moderate |
| Odenigbo et al27 | 2008 | Asaba, Delta State | South-south | Population-based | Mixed | 41.6 | 100 | 23.0 | Moderate |
| Oyeyemi & Adeyemi28 | 2013 | Maiduguri, Borno State | North-east | Population-based cross-sectional study | Mixed | 44.9 | 292 | 6.8 | High |
| *Forrest et al29 | 1992 | Benin, Edo State | South-south | Population-based cross-sectional study | Urban | 41.1 | 799 | High | |
| Oguoma et al30 | 2015 | Kwale, Delta State | South-south | Population-based cross-sectional study | Mixed | 39.9 | 422 | 38.1 | High |
| Ojji et al31 | 2010 | Abuja, FCT | North-central | Hospital-based | Urban | 49 | 913 | 22.5 | High |
| Iloh et al32 | 2009 | Imo State | South-east | Hospital-based | Rural | 40 | 2156 | 7.8 | Moderate |
| Iloh et al33 | 2008 | Imo State | South-east | Hospital-based | Semi-Urban | 37 | 9296 | 8.2 | Moderate |
study reported only blood lipid levels.
Data Analysis
A random-effects meta-analysis was employed to generate national and sub-national estimates of the prevalence of hypercholesterolemia and mean cholesterol levels in Nigeria, using the Freeman-Tukey double arscine transformation15 to normalize data given the wide variation in extracted crude estimates from studies. Standard errors were determined from the reported crude estimates and population denominators, assuming a binomial (or Poisson) distribution. Heterogeneity between studies was assessed using I-squared (I22) statistics. Publication bias was assessed using Egger’s regression test for funnel plot asymmetry16. A meta-regression model based on mean age from each study and adjusted for the study period was developed to determine prevalence distribution of hypercholesterolemia by the age of the Nigerian population over two separate years. As explained in previous studies17, 18, we tested various models (linear, exponential, polynomial, logarithmic, etc.) to determine which was most predictive, representing the greatest proportion of variance(R2) of the prevalence of hypercholesterolemia as explained by the inputted variables. The equation of the model was used to generate age-adjusted prevalence of hypercholesterolemia, at midpoints of 5–year age groups (ie. from 20–24 (22), 25–29 (27), 30–34 (32), to 80 years and over). The age-adjusted prevalence for each year was multiplied by the corresponding United Nation (UN) population for Nigeria (by 5-year age group)19 to estimate the absolute number of persons with hypercholesterolemia in Nigeria for the years 1995 and 2015. All statistical analyses were conducted in Stata (Stata Corp V.14, Texas, USA). The study was guided by the PRISMA checklist20.
RESULTS
Search results
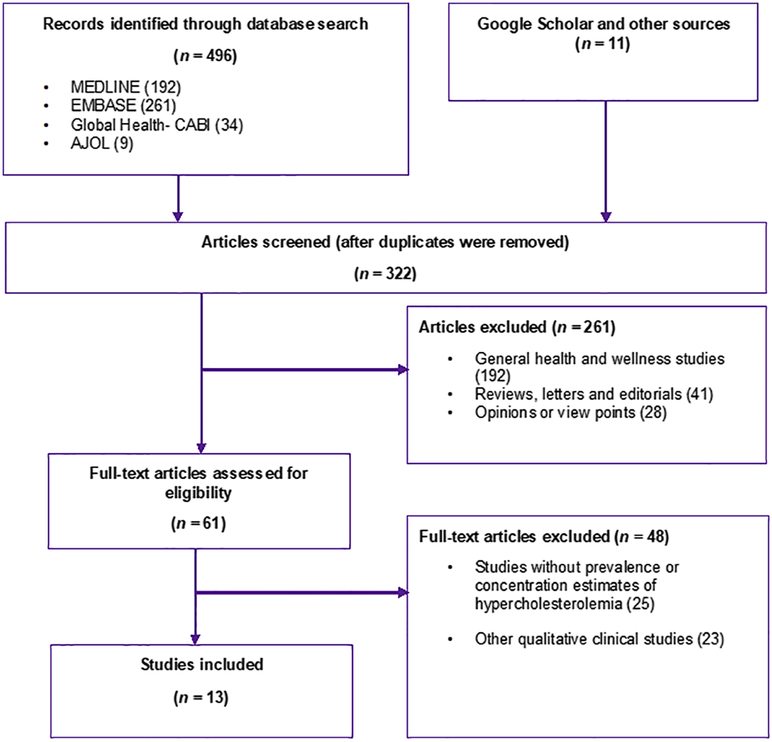
The databases’ searches returned 496 studies (MEDLINE 192, EMBASE 261, Global Health 34, and AJOL 9). An additional 11 studies were identified through Google Scholar, and hand-searching reference lists of relevant studies. After duplicates have been removed, 322 titles were screened for relevance (i.e. any epidemiologic studies on hypercholesterolemia in Nigeria). On applying the selection criteria, 261 studies were excluded. Hence, 61 full-texts were assessed and further screened comprehensively using the pre-designed selection and quality criteria. Forty-eight studies were then excluded at this stage. We finally included 13 studies21–33 for both quantitative and qualitative synthesis (Figure 1).
FIGURE 1.
Flow chart of selection of studies on hypercholesterolemia in Nigeria.
Study Characteristics
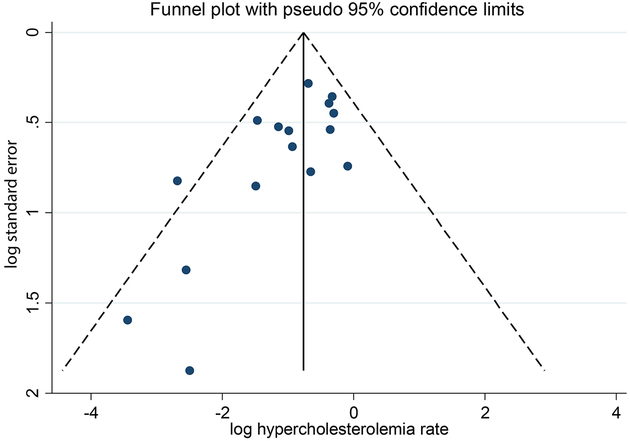
The 13 studies covering a population of 16981 were selected across the southern and northern parts of Nigeria, with only the North-western geopolitical zone not represented (Table 3). There were five studies from the South-south, four from the South-east, two from the North-central, and one study each from the North-east and South-west. Although most studies were conducted outside hospital settings, they may not be entirely referred as population-based, as some studies were limited to specific population groups, including professionals, civil servants, university employees, with a total population of 16,981. Most studies mainly presented prevalence estimates for hypercholesterolemia (expressed as the proportion of the population with total cholesterol ≥200 mg/dl or 5.2 mg/dl). Hence this was the only pooled prevalence rate reported in this study. However, as mean blood cholesterol levels were reported across studies, we pooled nation-wide blood levels of total cholesterol LDL-cholesterol, HDL-cholesterol and triglycerides. Six (6) studies were conducted in urban settings, four (4) in semi-urban settings (i.e. a mix of urban and rural dwellers), and three (3) in rural settings. Study period ranged from 1992 to 2015, with most studies conducted within a one-year period. The aggregated mean age from all studies ranged from 22 to 65 years (Table 3). Although five studies were rated as high quality, heterogeneity was high across studies (I-squared (I22)=99.6%, P≤0.001) and funnel plot was asymmetrical suggesting publication bias (Egger’s test (z)=1.67, P=0.008) (Figure 2).
FIGURE 2.
Funnel plot showing distribution of selected studies
Egger’s test (z) = −1.67, P = 0.008.
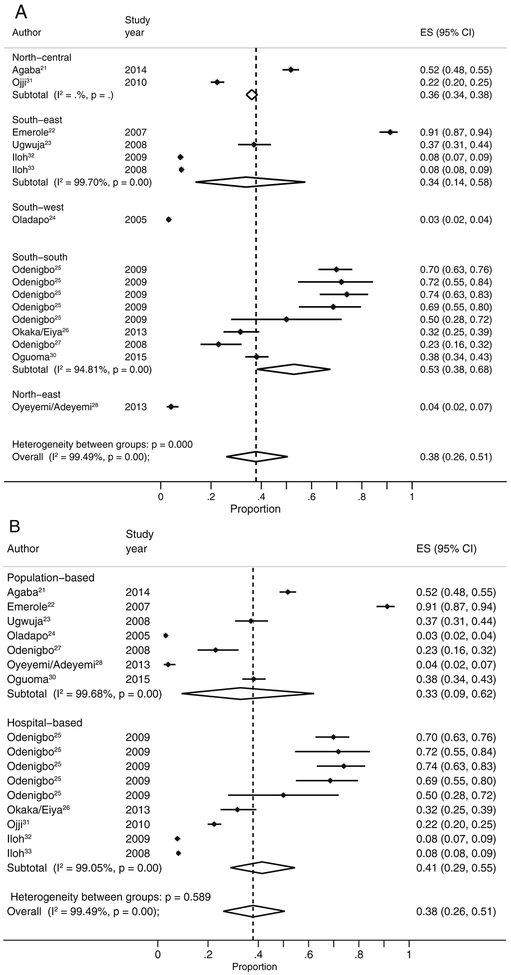
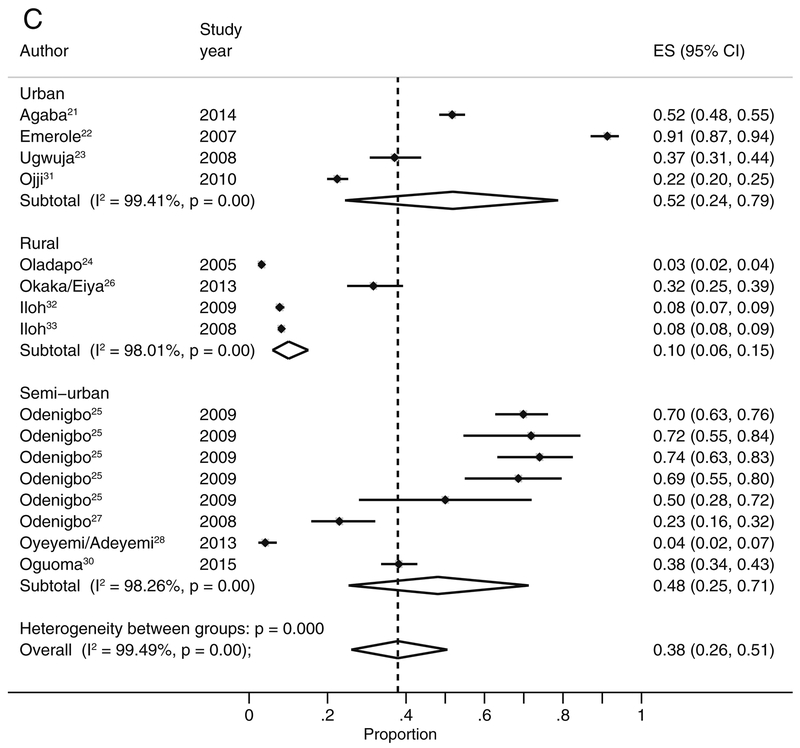
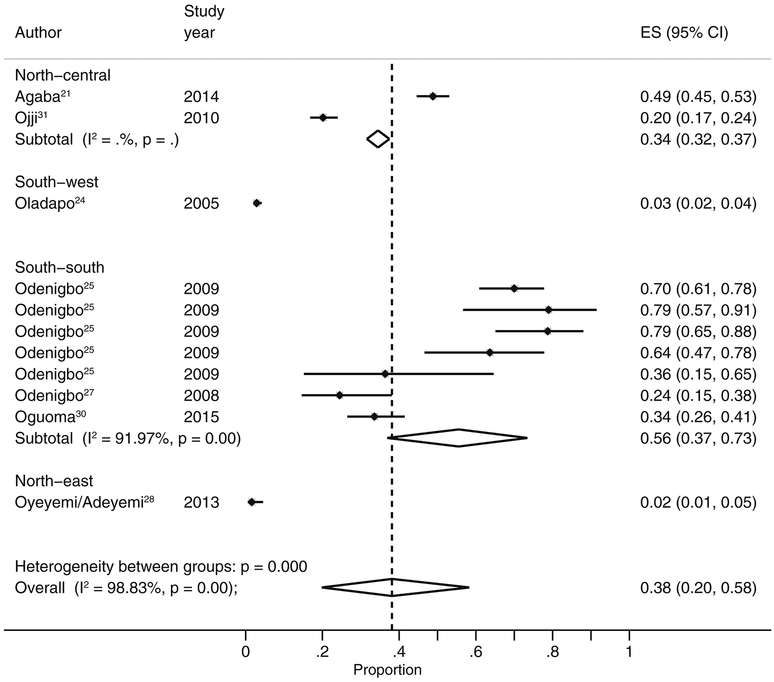
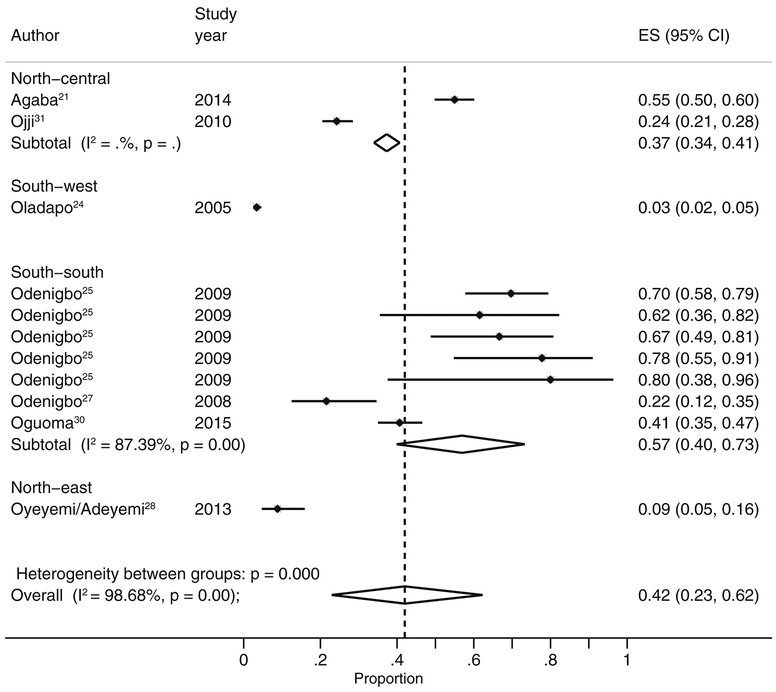
Prevalence of hypercholesterolemia in Nigeria
The highest prevalence of hypercholesterolemia was reported among staffs of a higher education institution in Owerri, Imo State, South-east Nigeria at 91.3%22. Other high estimates of hypercholesterolemia were reported among elderly urban residents in Asaba, Delta State, South-south Nigeria (70.0%)25, and in another higher education community in Jos, Plateau State, North-central Nigeria (51.8%)21. The lowest prevalence of hypercholesterolemia was reported in Egbeda, a rural town in Oyo State, South-west Nigeria, at 3.2%24. There were also some low prevalence rates of hypercholesterolemia estimated in two separate sites in Imo State, South-east Nigeria, at 7.8% and 8.2%32, 33 (Table 3). Across all data-points, the pooled crude prevalence of hypercholesterolemia in Nigeria was 38% (95% CI: 26–51). (Figure 3). When estimates from population-based studies were considered, the pooled prevalence was 33% lower, though the confidence interval were wide (95% CI: 9–62). The prevalence in women was higher at 42% (95% CI: 23–63) than estimated among men at 38% (95% CI: 20–58) (Figures 4 & 5, Table 4). Across the geo\political zones, the prevalence of hypercholesterolemia was highest in the South-south at 53% (95% CI: 38–68), followed by North-central (36%, 95% CI: 34–38) and South-east (34%, 95% CI: 14–58). The South-west (3.2%, 95% CI: 2–4) and the North-east (4%, 95% CI: 2–7) had the lowest estimated prevalence rates. The distribution of the prevalence of hypercholesterolemia across study settings suggest a significantly higher rate in urban settings at 52% (95% CI: 24–79), compared to rural settings at 10% (95% CI: 6–15) (Table 4). See supplementary material for detailed sex variation across study design, setting and geopolitical zone.
FIGURE 3.
Plate A. Pooled rate of hypercholesterolemia in Nigeria, by geopolitical zone. Plate B. Pooled rate of hypercholesterolemia in Nigeria, by study design. Plate C. Pooled rate of hypercholesterolemia in Nigeria, by study setting.
FIGURE 4.
Pooled rate of hypercholesterolemia in Nigeria, men.
FIGURE 5.
Pooled rate of hypercholesterolemia in Nigeria, Women.
Table 4.
Pooled estimates of hypercholesterolemia and blood lipid levels in Nigeria
| Region | Both sexes | Men | Women | ||||
|---|---|---|---|---|---|---|---|
| Prevalence % (95% CI) | I2, P-value | Prevalence % (95% CI) | I2, P-value | Prevalence % (95% CI) | I2, P-value | ||
| Nation-wide | 38 (26–51) | 99.5, <0.001 | 38 (20–58) | 98.8, <0.001 | 42 (23–63) | 98.7, <0.001 | |
| Study design | Population-based | 33 (9–62) | 99.7, <0.001 | 18 (2–46) | 99.3, <0.001 | 23 (3–54) | 99.3, <0.001 |
| Hospital-based | 41 (29–55) | 99.1, <0.001 | 58 (29–85) | 97.1, <0.001 | 62 (34–86) | 94.5, <0.001 | |
| Settings | Urban | 52 (24–79) | 99.4, <0.001 | 34 (32–37) | 0.0 | 37 (34–41) | 0.0 |
| Rural | 10 (6–15) | 98.0, <0.001 | 3 (2–4) | - | 3 (2–4) | - | |
| Semi-urban | 48 (25–71) | 98.3, <0.001 | 46 (19–74) | 97.7, <0.001 | 50 (30–70) | 93.9, <0.001 | |
| Geopolitical zone | North-central | 36 (34–38) | 0.0 | 34 (32–37) | 0.0 | 37 (34–41) | 0.0 |
| North-east | 4 (2–7) | - | 2 (1–5) | - | 9 (5–16_ | - | |
| South-east | 34 (14–58) | 94.6, <0.001 | - | - | - | - | |
| South-south | 53 (38–68) | - | 56 (37–73) | 91.8, <0.001 | 57 (40–73) | 86.6, <0.001 | |
| South-west | 3 (2–4) | - | 3 (2–4) | - | 3 (2–4) | - | |
| Pooled blood lipid levels | |||||||
| Lipid type | Concentration (mg/dl; mmol/l) | I2, P-value | - | - | - | - | |
| Total cholesterol | 189.1 (177.6200.7); 4.9 (4.6–5.2) | 0.0, 0.808 | - | - | - | - | |
| LDL-cholesterol | 100.4 (65.6131.2); 2.6 (1.7–3.4) | 77.7, <0.001 | - | - | - | - | |
| HDL-cholesterol | 61.8 (50.273.3); 1.6 (1.3–1.9) | 24.0, 0.254 | - | - | - | - | |
| Triglycerides | 132.8 (97.4–159.3); 1.5 (1.1–1.8) | 0.0, 0.743 | - | - | - | - | |
Pooled blood lipid levels in Nigeria
The pooled mean total cholesterol concentration in Nigeria is approaching the borderline high levels, with an upper limit reaching the borderline (189.1m mg/dl, 95% CI: 177.6–200.7). The pooled mean concentration of LDL-cholesterol was 100.4 mg/dl (95% CI: 65.6–131.2), which can be regarded as good, but also with an upper limit above the borderline high levels. We estimated a nation-wide mean HDL-cholesterol concentration at 61.8 mg/dl (95% CI: 50.2–73.3) which is in the range of the accepted levels needed to lower cardiovascular disease risk. The estimated pooled triglycerides concentration may also be regarded as acceptable at 132.8 mg/dl (95% CI: 97.4–159.3), although as observed with total cholesterol and LDL-cholesterol, the upper limit is above normal.
Estimated number of persons with hypercholesterolemia in Nigeria
Age-adjusted prevalence of hypercholesterolemia increased as the population ages, P=0.012 (see supplementary material for meta-regression model). Using the United Nations demographic projections for Nigeria, and based on an assumption that our extracted dataset was collected between 1992 and 2015 (see study period in Table 3), we estimated over 8.2 million persons (17%) aged 20 years or more with hypercholesterolemia in Nigeria in 1995. By 2015, cases of hypercholesterolemia have increased by about 166% to 21.9 million persons (26%) in the same age group. Although, it appears the rapid population and demographic changes in Nigeria over this 20-year period were partly responsible for this increase (Table 5).
TABLE 5.
Absolute number of persons with hypercholesterolemia in Nigeria, aged 20 years or more, 1995 and 2015
| Age (years) | 1995 | 2015 | ||||
|---|---|---|---|---|---|---|
| Prevalence (%) | Population (000) | Cases (000) | Prevalence (%) | Population (000) | Cases (000) | |
| 20–24 | 0.1 | 9732.1 | 4.4 | 3.9 | 15981.8 | 636.5 |
| 25–29 | 0.8 | 7814.7 | 61.1 | 10.7 | 14051.0 | 1497.6 |
| 30–34 | 5.9 | 6586.9 | 388.2 | 17.3 | 12102.3 | 2097.7 |
| 35–39 | 12.6 | 5534.3 | 695.6 | 24.0 | 9982.6 | 2396.6 |
| 40–44 | 19.2 | 4611.6 | 887.4 | 30.7 | 7767.7 | 2383.4 |
| 45–49 | 25.9 | 3894.2 | 1009.3 | 37.4 | 6008.7 | 2244.7 |
| 50–54 | 32.6 | 3330.8 | 1085.6 | 44.0 | 4993.8 | 2198.9 |
| 55–59 | 39.3 | 2690.9 | 1056.7 | 50.7 | 4146.1 | 2102.4 |
| 60–64 | 45.9 | 2090.9 | 960.6 | 57.4 | 3325.7 | 1908.4 |
| 65–69 | 52.6 | 1544.5 | 812.7 | 64.1 | 2554.2 | 1636.2 |
| 70–74 | 59.3 | 1031.8 | 611.8 | 70.7 | 1821.5 | 1288.4 |
| 75–79 | 66.0 | 581.5 | 383.6 | 77.4 | 1077.6 | 834.2 |
| 80+ | 76.6 | 353.3 | 270.8 | 88.1 | 721.8 | 635.8 |
| All | 16.5 | 49797.6 | 8227.7 | 25.9 | 84534.9 | 21860.8 |
Note: Estimates based on the epidemiologic model (y=1.335x+0.573t-1178.246). Where y=prevalence of hypercholesterolemia, x=age, and t=year. Coefficients of ‘x’ and ‘t’ are ‘1.335’ and ‘0.573’ for the meta-regressed line, with an intercept of ‘−1178.246’
DISCUSSION
In this study, we sought to estimate the number of individuals living with elevated blood cholesterol levels in Nigeria. We estimate that the age-adjusted prevalence of hypercholesterolemia increased from 17% to 26% among persons aged 20 years or more between 1995 and 2015. In 1992, Akinkugbe and Akinkanju34 estimated a nation-wide prevalence of hypercholesterolemia at 4%. Though there is not yet another national estimate, a number of community-based studies conducted across the country independently suggest an increasing prevalence, with estimates ranging from 27–52% across different population groups4, 8, 9, 35. When compared with the WHO African region, our 2015 estimate is slightly higher (26% versus 23%), although still lower than the global prevalence at 39%3. Moreover, we reported a near-borderline population mean total cholesterol at 189 mg/dl. While mean total cholesterols may not be key indicators of the distribution of hypercholesterolemia in a population36, a coexisting high and rising prevalence imply a need for more comprehensive population-wide measures to prevent health consequences.
In this study, we found a slightly higher hypercholesterolemia prevalence among women compared to men in Nigeria. This difference has also been documented in previous studies1, 36, however the higher rate among women in Nigeria is largely connected to less physical activity and an increasing patronage of processed food outlets34, 37. Reports suggest some women adopt this lifestyle to add weight, as this indicates higher social class and better living standards38, 39. Other factors thought to be influencing the higher prevalence of hypercholesterolemia in females include gender roles and religious expectations. In many Nigerian settings, women are required to primarily stay indoors and complete domestic chores, with this predisposing women to higher caloric intake and sedentary lifestyles38.
Our study sought to provide the first zonal estimates of hypercholesterolemia across Nigeria. Though these are marked by wide uncertainties, the highest prevalence was reported in the South-south at 53%. Some authors have noted that dyslipidemia was highly prevalent across all geopolitical zones in Nigeria, although Southern ethnic groups whose typical diet contained higher fat contents had significantly higher total blood cholesterol levels8, 40. It is likely that the relatively higher socio-economic status in these settings could partly drive elevated blood cholesterol levels, as a positive correlation between hypercholesterolemia and wealth index is well-documented35, 36, 41. As the southern parts of Nigeria are experiencing faster rates of urbanization, the higher rates of hypercholesterolemia in these settings could be explained. Venkichatalam and colleagues1 reported that observed elevated cholesterol levels across world regions vary with national and sub-national economic developments.
Although urbanization, lifestyles, and diets are believed to be leading causes of raised cholesterol levels in Nigeria, culture, ethnic diversities, literacy levels and lack of information also play important roles, and should be considered in preventive measures35, 42. In three studies conducted across southern and northern Nigeria, several participants reported being unaware of the risks of abnormal lipid patterns and a need for lipid profile and screening35, 42, 43. In many parts of the country, the quantity and type of food consumed, and where they are purchased, can contribute to social status44.
Though there is robust evidence linking early identification and treatment of hypercholesterolemia with reduced cardiovascular morbidity and mortality45, 46, interventions targeting hypercholesterolemia in Nigeria are limited. Although the management of elevated blood cholesterol and other cardiovascular risks may be complex at the country level1, the challenges are worsened in Nigeria due to poor understanding of the burden, limited research, varying guidelines, complex prescriptions, and several health system challenges1. Across many health centres, hypercholesterolemia is an incidental clinical finding, and patients appear to be unwilling to incur high out-of-pocket expenses on lipid-lowering therapy as part of the management of other ailments5, 6, 47. Clinicians have advocated for more awareness and government response to complement treatment efforts5, 47
Our study has some limitations. First, there was a limited number of epidemiologic reports on high blood lipids in Nigeria, and studies appear to be poorly conducted, with only five studies rated as high quality. In addition, we could only retrieve studies from five of the six geopolitical zones in Nigeria, with no studies providing information regarding populations from the Northwest. This covers seven states, accounting for about 25% of Nigeria’s population. Second, heterogeneity was high across studies, reflecting varying study designs, case ascertainment, and the population covered—limited to specific groups including university employees, professionals and civil servants in some studies. Third, although we ensured hospital-based studies were from outpatient settings with a well-defined catchment population, our denominators could have been under-reported, thus presenting with higher estimates from hospital-based studies (41%) compared to population-based studies (33%), possibly affecting our overall estimates (38%). Moreover, the different contexts under which these studies were designed are important sources of heterogeneity and indeed affect overall representativeness of our estimates. These are important considerations in the interpretation of our findings. Albeit, we have provided important datasets and estimates relevant that can support and motivate further research and necessary policy interventions.
CONCLUSION
Our findings suggest a high prevalence of hypercholesterolemia in Nigeria. Urbanization, lifestyles, diets, and culture appear to be driving an increasing prevalence, especially among women. Population response and clinical management have been sub-optimal. Population-wide awareness and education on elevated cholesterols and associated risks should be prioritized among other interventions.
Supplementary Material
HIGHLIGHTS.
Urbanization, with changing lifestyles, diets and culture, appear to be driving an increasing prevalence of hypercholesterolemia in Nigeria, particularly among women;
In 1995, over 8.2 million persons aged 20 years or more had hypercholesterolemia in Nigeria;
This increased by about 170% to 21.9 million persons in 2015.
Acknowledgements:
The authors acknowledge the support of the Nigeria Federal Ministry of Health and the WHO Nigeria Country Office in the conduct of this study. Special thanks to Victoria Nyawira Nyaga for checking through our statistical analyses.
Funding: MOH is supported by a grant (K99HL141678) from the NIH/National Heart, Lung, and Blood Institute (NHLBI)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure statement: The authors declare no conflicts of interest.
Ethical approval: Not required. This paper was based on publicly available sources and data.
REFERENCES
- 1.Venkitachalam L, Wang K, Porath A, et al. Global variation in the prevalence of elevated cholesterol in outpatients with established vascular disease or 3 cardiovascular risk factors according to national indices of economic development and health system performance. Circulation 2012; 125: 1858–69. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. World health statistics 2016: Cardiovascular diseases Geneva: World Health Organization; 2017. [Google Scholar]
- 3.World Health Organization. Global Health Observatory (GHO) data: Raised cholesterol 2015. [cited 07 January 2019]; Available from: https://www.who.int/gho/ncd/risk_factors/cholesterol_text/en/
- 4.Ukoli FA, Bunker CH, Fabio A, Olomu AB, Egbagbe EE, Kuller LH. Body fat distribution and other anthropometric blood pressure correlates in a Nigerian urban elderly population. The Central African journal of medicine 1995; 41: 154–61. [PubMed] [Google Scholar]
- 5.Amole I, OlaOlorun D. Lipid profile of adult Nigerians attending medical outpatient clinic of Baptist medical center Ogbomoso. Benin Journal of Postgraduate Medicine 2010; 12. [Google Scholar]
- 6.Akpa MR, Agomouh DI, Alasia DD. Lipid profile of healthy adult Nigerians in Port Harcourt, Nigeria. Nigerian journal of medicine : journal of the National Association of Resident Doctors of Nigeria 2006; 15: 137–40. [DOI] [PubMed] [Google Scholar]
- 7.Hallal PC, Andersen LB, Bull FC, Guthold R, Haskell W, Ekelund U. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet (London, England) 2012; 380: 247–57. [DOI] [PubMed] [Google Scholar]
- 8.Oguejiofor OC, Onwukwe CH, Odenigbo CU. Dyslipidemia in Nigeria: prevalence and pattern. Annals of African medicine 2012; 11: 197–202. [DOI] [PubMed] [Google Scholar]
- 9.Ahaneku G, Ahaneku J, Osuji C, Oguejiofor C, Anisiuba B, Opara P. Lipid and some other cardiovascular risk factors assessment in a rural community in Eastern Nigeria. Annals of medical and health sciences research 2015; 5: 284–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.United States National Heart L, and Blood Institute,. ATP III Guidelines At-A-Glance Quick Desk Reference, National Cholesterol Education Program. Bethesda, MD: National Institutes of Health; 2001. [Google Scholar]
- 11.Stanifer JW, Jing B, Tolan S, et al. The epidemiology of chronic kidney disease in sub-Saharan Africa: a systematic review and meta-analysis. The Lancet Global Health 2014; 2: e174–e81. [DOI] [PubMed] [Google Scholar]
- 12.Pai M, McCulloch M, Gorman JD, et al. Systematic reviews and meta-analyses: an illustrated, step-by-step guide. Natl Med J India 2004; 17: 86–95. [PubMed] [Google Scholar]
- 13.Guyatt GH, Rennie D. Users’ guides to the medical literature: a manual for evidence-based clinical practice Chicago: AMA Press; 2002. [Google Scholar]
- 14.Juni P, Altman DG, Egger M. Systematic reviews in health care: assessing the quality of controlled clinical trials. BMJ 2001; 323: 42–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Freeman MF, Tukey JW. Transformations Related to the Angular and the Square Root. Ann Math Statist 1950; 21: 607–11. [Google Scholar]
- 16.Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997; 315: 629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Adeloye D, Olawole-Isaac A, Auta A, et al. Epidemiology of harmful use of alcohol in Nigeria: a systematic review and meta-analysis. The American journal of drug and alcohol abuse 2019; 45: 438–50. [DOI] [PubMed] [Google Scholar]
- 18.George-Carey R, Adeloye D, Chan KY, et al. An estimate of the prevalence of dementia in Africa: A systematic analysis. Journal of global health 2012; 2: 020401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.United Nations. 2017 Revision of World Population Prospects New York, US: United Nations; 2017. [Google Scholar]
- 20.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS medicine 2009; 6: e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Agaba EI, Akanbi MO, Agaba PA, et al. A survey of non-communicable diseases and their risk factors among university employees: a single institutional study. Cardiovascular journal of Africa 2017; 28: 377–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Emerole CO, Aguwa EN, Onwasigwe CN, Nwakoby BA. Cardiac risk indices of staff of Federal University Of Technology Owerri, Imo State, Nigeria. Tanzania health research bulletin 2007; 9: 132–5. [DOI] [PubMed] [Google Scholar]
- 23.Ugwuja E, Ogbonna N, Nwibo A, Onimawo I. Overweight and Obesity, Lipid Profile and Atherogenic Indices among Civil Servants in Abakaliki, South Eastern Nigeria. Annals of medical and health sciences research 2013; 3: 13–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Oladapo OO, Salako L, Sodiq O, Shoyinka K, Adedapo K, Falase AO. A prevalence of cardiometabolic risk factors among a rural Yoruba south-western Nigerian population: a population-based survey. Cardiovascular journal of Africa 2010; 21: 26–31. [PMC free article] [PubMed] [Google Scholar]
- 25.Odenigbo CU, Oguejiofor OC. Pattern of medical admissions at the Federal Medical Centre, Asaba-a two year review. Nigerian journal of clinical practice 2009; 12: 395–7. [PubMed] [Google Scholar]
- 26.Okaka EI, Okwuonu CG. Blood pressure variation and its correlates among patients undergoing hemodialysis for renal failure in Benin City, Nigeria. Annals of African medicine 2017; 16: 65–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Odenigbo CU, Oguejiofor OC, Odenigbo UM, Ibeh CC, Ajaero CN, Odike MA. Prevalence of dyslipidaemia in apparently healthy professionals in Asaba, South South Nigeria. Nigerian journal of clinical practice 2008; 11: 330–5. [PubMed] [Google Scholar]
- 28.Oyeyemi AL, Adeyemi O. Relationship of physical activity to cardiovascular risk factors in an urban population of Nigerian adults. Archives of public health = Archives belges de sante publique 2013; 71: 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Forrest KY, Bunker CH, Kriska AM, Ukoli FA, Huston SL, Markovic N. Physical activity and cardiovascular risk factors in a developing population. Medicine and science in sports and exercise 2001; 33: 1598–604. [DOI] [PubMed] [Google Scholar]
- 30.Oguoma VM, Nwose EU, Skinner TC, Digban KA, Onyia IC, Richards RS. Prevalence of cardiovascular disease risk factors among a Nigerian adult population: relationship with income level and accessibility to CVD risks screening. BMC public health 2015; 15: 397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ojji DB, Ajayi SO, Mamven MH, Atherton J. Prevalence of dyslipidemia in normoglycemic subjects with newly diagnosed high blood pressure in Abuja, Nigeria. Journal of clinical lipidology 2009; 3: 51–6. [DOI] [PubMed] [Google Scholar]
- 32.Iloh GU, Amadi AN, Nwankwo BO. Obesity in adult Nigerians: a study of its prevalence and common primary co-morbidities in a semi-urban Mission General Hospital in South-Eastern Nigeria. Nigerian journal of medicine : journal of the National Association of Resident Doctors of Nigeria 2010; 19: 459–66. [DOI] [PubMed] [Google Scholar]
- 33.Iloh G, Amadi AN, Nwankwo BO, Ugwu VC. Obesity in adult Nigerians: a study of its pattern and common primary co-morbidities in a rural Mission General Hospital in Imo state,South-Eastern Nigeria. Nigerian journal of clinical practice 2011; 14: 212–8. [DOI] [PubMed] [Google Scholar]
- 34.Akinkugbe OO, Akinyanju OO. Non-communicable diseases in Nigeria-final report of a national survey. Lagos: Federal Ministry of Health—National Expert Committee on Non-Communicable Diseases; 1997. [Google Scholar]
- 35.Emma-Okon BO, Onayade AA, Adegoke AO, Soyinka JO, Ademigbuji EA. Lipid profile in an apparently healthy Nigerian population. The Nigerian postgraduate medical journal 2014; 21: 290–3. [PubMed] [Google Scholar]
- 36.Tolonen H, for the WHOMP, Keil U, et al. Prevalence, awareness and treatment of hypercholesterolaemia in 32 populations: results from the WHO MONICA Project. International journal of epidemiology 2005; 34: 181–92. [DOI] [PubMed] [Google Scholar]
- 37.Adeloye D, Ige JO, Aderemi AV, et al. Estimating the prevalence, hospitalisation and mortality from type 2 diabetes mellitus in Nigeria: a systematic review and meta-analysis. BMJ Open 2017; 7: e015424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Afam-Anene OC, Okorie JN, Maduforo AN. Obesity, physical activity pattern and hypercholesterolemia among civil servants in Bida Nigeria State Nigeria. Journal of Dietitians Association of Nigeria 2017; 8: 13–24. [Google Scholar]
- 39.BeLue R, Okoror TA, Iwelunmor J, et al. An overview of cardiovascular risk factor burden in sub-Saharan African countries: a socio-cultural perspective. Globalization and health 2009; 5: 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ighosotu S, Tonukari NJ. The influence of dietary intake on the serum lipid profile, body mass index and risk of cardiovascular diseases in adults on the Niger Delta region. International Journal of Nutrition and Metabolism 2010; 2: 040–4. [Google Scholar]
- 41.Awogbemi OT, Okoromah CA, Roberts AA. Hypercholesterolaemia in schoolchildren in Lagos, Nigeria: an indication of a growing threat of cardiovascular disease? Nigerian quarterly journal of hospital medicine 2013; 23: 110–3. [PubMed] [Google Scholar]
- 42.Awosan K, Ibrahim M, Makusidi M, Essien E, Adeniji A. Impact of intervention on knowledge and risk factors of coronary heart disease among teachers in Sokoto, Nigeria. International Journal of Medicine and Medical Sciences 2013; 5: 456–9. [Google Scholar]
- 43.Ramalan M, Uloko A, Fakhradeen M, Gezawa I. Lipid profile in apparently healthy Nigerian adults. Society for Endocrinology BES 2015; 2015: BioScientifica; 2015. [Google Scholar]
- 44.Adedoyin RA, Ibrahim RA, Awotidebe TO, Ativie RN, Oyeyemi AL. Environmental and socioeconomic factors associated with Nigerian University students’ participation in physical activity. International Journal of Sports Science 2014; 4: 97–102. [Google Scholar]
- 45.Grundy SM, Arai H, Barter P, et al. An International Atherosclerosis Society Position Paper: global recommendations for the management of dyslipidemia-full report. Journal of clinical lipidology 2014; 8: 29–60. [DOI] [PubMed] [Google Scholar]
- 46.Wilson PW. The epidemiology of hypercholesterolemia. A global perspective. The American journal of medicine 1989; 87: 5s–13s. [DOI] [PubMed] [Google Scholar]
- 47.Osuji CU, Omejua EG. Prevalence and characteristics of the metabolic syndrome among newly diagnosed hypertensive patients. Indian journal of endocrinology and metabolism 2012; 16 Suppl 1: S104–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.