Abstract
We cannot deny that technology has become an important part of our daily life, not only in automobiles, houses or cellphones but also in hospitals. In the OR, in particular for knee arthroplasty, image free navigation has proven to reduce the number of outliers and by that the revision rate in younger patients. Over the last years robotics has again been introduced into the operation theatres. However, in their present version they add time and costs, but only minimal benefits to the procedure. Therefore, future robots should be faster and instrumentation free. Beside those more economical aspects, the goal of this digital technology must be an improvement in clinical outcome. To achieve that, additional steps for analyzing the pre-, and intra-OP quantitative data is key. With the use of artificial intelligence and/or machine learning a data based algorithm will probably be developed, which helps the surgeon to integrate all parameters into his individual cutting and releasing plan for each patient. Digital data therefore, might become the key to enable the surgeon to treat patients more individual and by that hopefully deliver better outcome.
1. Introduction
In all parts of our daily life digital solutions have already changed or will change our lives dramatically. Just remember a world without worldwide web, mobile phones, robots in production streets of automobiles, and so on. In the world of medicine this change has also started, but has not reached all hospitals and all fields of patient treatment. While imaging in radiology departments has become digital more than a decade back and fusion of different imaging modalities became available and standard of care for example in tumor surgery of the brain, orthopaedics is still in a starting phase.
While some steps like navigation had been made a while ago, others just started (e.g. 2nd generation robotics) and for others we need to wait for some more years to come (e.g. AI for TKA). Not only inside the OR, but also outside, in OPD or on the ward we will see more and more digital technologies to come within the next years.
In this Editorial, different aspects of digitalisation inside the OR are demonstrated; of course the editor does not know today which of all the promising options definitely will become the new gold standard in patient treatment. In the next Editorial, the options and aspects for digitalisation outside the OR will be demonstrated.
2. Digital solutions in the OR
2.1. Navigation/robotics/AI
More than 10 years back, the first navigation machines had been introduced in orthopaedics. In the beginning 2 modalities ran parallel, nowadays in extremity surgery image free navigation has become the method of choice. In the first years, navigation could show that it is able to improve coronal alignment from 61% to 75% up to 91%–96% within the 3° corridor.1, 2, 3 Even in Indian population with severe deformities those results could be confirmed.4 Over the following years alternative techniques, like patient specific instrumentation had been introduced however never reached this high accuracy.5,6 This made navigation the method of choice regarding alignment. However, this improvement in accuracy of alignment was not automatically leading to an improvement in patient results. This factor and the additional problems of costs and learning curve restricted the expansion of navigation in the following years in most parts of the world.7 By introducing more modern navigation software, it became possible to perform an advanced soft tissue balancing in real time.8,9 For the first time, it became possible to perform quantitative TKA surgery, meaning that all cutting steps and their effects on soft tissue balance can be visualized, planned and controlled. However, also this modern navigation technology still has to prove whether it really will help to improve patient outcome. Some studies have shown a reduced revision rate and improved knee scores at least if a gap balanced technique was used.10,11 This is accordance to the results of the Australian Arthroplasty Register. From 2015 on, the register could show that the survival rate of navigated TKA in younger patients (<65 years) is higher compared to other techniques'.12 This is leading to an increased acceptance of the method in Australia so that nowadays around 40% of all knees are navigated.
Navigation technology is the basis for all modern technologies, such as robotics. While some companies favour an image-based, others again use an image free approach. Image-based technologies are advantageous in complex anatomical scenarios like spine- or brain-surgery. In total hip or knee arthroplasty, however, this extra information seems not be necessary to achieve good results. An additional CT or MRI for referencing just adds costs and is time consuming. That's why this Editor believes that image free robotics will finally succeed in total hip and knee arthroplasty. Until now, the quality of the robotic procedure is based on the quality of the navigation data and by that finally on the experience of the surgeon with that technology. The robot is just preforming the bone cuts. So, an improved knowledge of the algorithm behind the navigation and prevention of typical navigation mistakes (e.g. imprecise anatomical referencing) is important. The robot itself, at least in its present form, will not improve quality. It will just make very precise cuts, but the planning of the specific cutting plane and angle depends still on the surgeon's experience and knowledge.
This is leading to the following important question: What are the potential benefits that can convince me as a surgeon to use a robot instead of my current technology? Of course, it is a marketing tool, however this effect will not last for long and if it is not accompanied by further more fundamental advantages, such as improvement of clinical outcome, reduction of process time and process costs it will not become the new Golden Standard. Currently, this is not guaranteed because all robots on the market are expensive and time consuming. So it is very important to develop a next generation of robots that will really help the surgeon to reach their goals.
Regarding process costs, the robot in its present form needs reflectors, Steinman pins and fixation tools. This causes extra costs. This extra money can be compensated if other instrument trays may become redundant. Therefore, the robot should be able to perform bone cuts “free hand”. However, at the moment all robots available still need conventional cutting blocks. The newer generation of robots hopefully will be able to get rid of the cutting blocks and by that the number of trays can be significantly reduced. Due to that development the daily costs per case will be reduced. The investment for the robot itself is still enormous, although the newer generations seem to get cheaper. However, only with a number of more than 250 TKA per year or even more, the investment for a robot is making sense. The current robots do not help to speed up surgery. Like in navigation, extra time for pin placement and registration of the anatomical landmarks is needed. After a learning curve on handling of cutting block placement, a surgeon can save time during surgery as no opening of the intramedullary canal of mounting of cutting jigs is required. One actual robot system uses drill burrs, which need a lot more time for cartilage and bone removal, so that saws finally will be the power tool of choice. However, only without cutting blocks the use of a robot can be faster than a conventional procedure. Simulations at that point described a save of time of around 10–15 minutes. This will indirectly help to reduce complications like infection and to reduce daily costs even further.
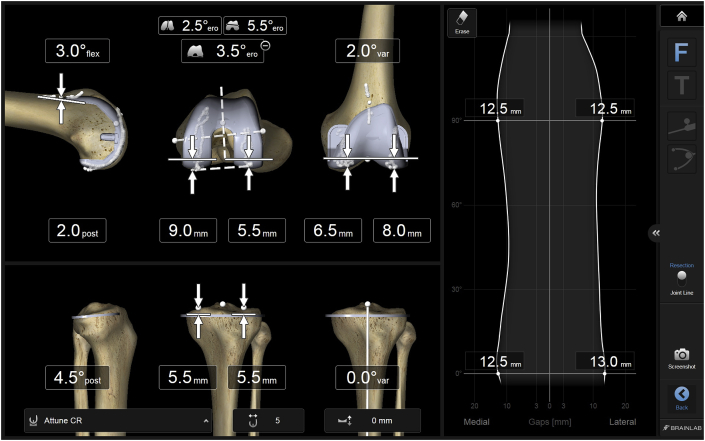
The most important argument for using a robot would still be an improved precision of the surgical process and an increased clinical outcome. Those 2 success parameters are not automatically coming along together. This fact has also been shown for navigation is the past. Navigation has shown to reduce the number of outliers regarding alignment and gap balancing compared to conventional techniques.1,2,9 On a planning screen the relationship between the different cuts and the gap widths (medial/lateral and extension/flexion) is quantitatively visualized (Fig. 1). This enables the surgeon to plan an optimized alignment, implant position and balanced joint in the same approach. Although this is demonstrating an optimized surgical process quality until now it is still not fully proven whether this is automatically leading to an improved quality in patient outcome. To achieve this most important objective, a huge amount of data sets might be necessary. Knees are showing a huge variability regarding the amount of deformity, bony morphology, ligament imbalance, ligament laxity. Beside the individuality of the knee all patients show specific factors (e.g. BMI, activity level, …) that also influence the final outcome. Performing the same work flow in all those variations in the same way might not be the solution to achieve increased patient satisfaction.13, 14, 15
Fig. 1.
Planning screen for femoral component placement. All parameters are visualized and can be altered according to the individual plan. A change in cutting will automatically affect the gaps (right side of the screen). In that way a balanced knee as one important goal can be achieved. This planning is performed before any femoral cut is made.
Only with quantitative intra-OP data on bone cuts and gap sizes and their correlation, we will understand how good we are as a surgeon to achieve our goals in patient treatment. By additionally analysing pre-OP and post-OP knee scores we will finally understand in which knees we are able to achieve our goals and which are the ones in which we fail. This will help to answer the question whether our goals should be the same for all knees equally or maybe different for specific subgroups. Only with that kind of data, we will be able to answer the questions of preferred alignment. While mechanical alignment within a 3° corridor was defined as the goal for coronal alignment, we have nowadays the concept of anatomical as well as that of kinematic alignment.16, 17, 18 Again, only with the help of larger data sets we will be able to understand which knees are favourable for which approach. The same discussion is whether really all knees should have equal medial and lateral gaps as well as equal extension and flexion gaps. As by nature this is not the case in most of the knees, some surgeons argue that it should not be the goal after TKA.19, 20, 21, 22 Maybe there are some knees that need larger flexion gaps than extension gaps, while some others might need lateral gaps to be a bit larger than medial gaps. How does alignment and stability correlate? All those questions can only be answered with the help of huge quantitative data sets.
Learning from complex data is bringing another field of digital technologies into the focus: machine learning and artificial intelligence. In this future field, the data sets will be analysed taken all different parameters into account. Based on the individual parameters the computer will recommend an individual surgical plan for cuts and soft tissue balancing. In this TKA 4.0 the surgeon is still deciding whether the plan is adequate or whether another modification should be applied. However, his decision will be based more on data than on experience only.
To summarize that part of navigation, robotics and artificial intelligence: We have started a long journey, which will not be stopped until the new technologies offer us benefits in all parts of surgery (time, costs, process quality and outcome). Only with an increased, data-based knowledge of knees and the TKA procedure itself, we will be able to develop the next steps of digital surgery successfully. The time of magic hands being the reason for success will be replaced by standardised and quantitative surgery. Understanding the data will become more important and makes the difference in the future. Finally, it has to be pointed out, that the technique is made to support us as a surgeon allowing us to achieve best surgical outcome in every single case.
3. Standardised patient workflows
Another field in which digital technology can support the surgical team is that of workflow standardisation. This technology can be applied in 2 different areas of arthroplasty: 1. In primary THA/TKA as optimisation tool and 2. in complex revision arthroplasty as a tool for reducing the learning curve.
3.1. Primary THA/TKA
In this area, the great advantage of this digital technology is that a team is performing the same workflow in all of their routine cases. This is helping to reduce a) process time, b) instrument sets, c) complications and d) to increase employee's satisfaction.
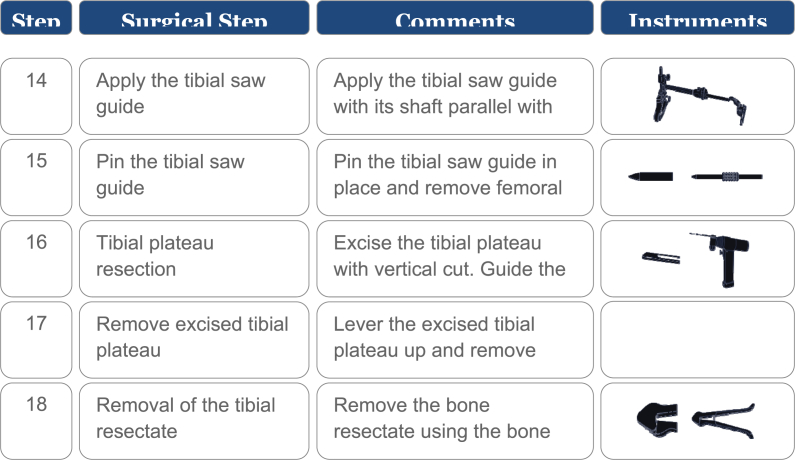
Before a workflow can be implemented in a Hospital, it is very important to sit together as a Team. This Team should include all senior surgeons as well as the experienced scrub nurses and doctors from Anaesthology. Each step from team time out until final wound closure and draping is described in the work flow, and all instruments used for each step are defined. At that point the surgeons need to agree on one standard (Fig. 2).
Fig. 2.
All steps of the surgery are defined, including the instruments needed. This work flow will then be visualized on a monitor.
After this individual digital standard has been defined, it can be implemented in the OR. Each step is announced by a voice and shown on the monitor (Fig. 3). The instruments needed for that step are also shown. To improve interaction between the nurse and the surgeon and within the surgeon team, the following step is also shown on the monitor (Fig. 3). With a foot pedal, the next step of the standard is selected. In case of an exception, for example based on a specific pathology, the surgeon can leave the standard workflow, shortly describe the reason for leaving it and later can return to it.
Fig. 3.
Intra-OP monitor showing the actual and the next step including the instruments that are required. On the lower part of the screen, the time planning is shown. So a difference between planning and actual time is visualized.
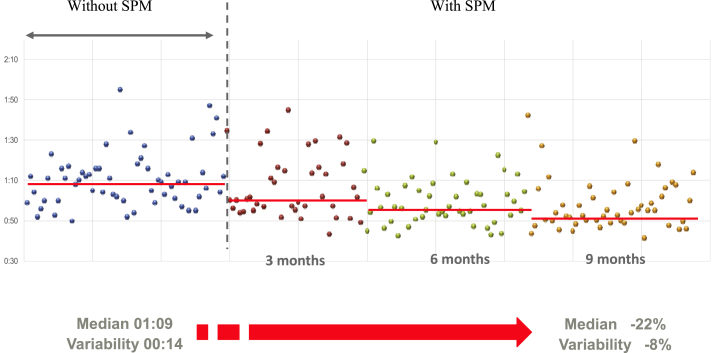
By using a standard workflow, mean surgical time for primary THA or TKA can be reduced by around 10–20%, even in experienced arthroplasty teams23 (Fig. 4). Time reduction is automatically reducing the potential of complications such as infection. After finishing the work flow, the report can be stored in the patient file. This again safes time and extra work. Additional images or videos can be attached to the file. This makes the documentation easier, faster and more individual.
Fig. 4.
Analysis of surgical time before and after introduction of standardisation (SPM). It is shown that directly after implementation a positive effect can be measured. Over time this effect is even more pronounced.
The same digital technology has been introduced for complex Revision TKA. In this scenario not every surgical step is defined, but all implant related steps. As a revision can be performed in a lot of different ways, all of them are defined and can be selected by the surgeon. While in some cases a cemented stem is favourable, in others the stem should be cementless, with or without offset. Or even sleeves might be necessary to achieve good fixation. As all those different options need different instruments and handlings and as revisions are not as frequently performed as primary TKA, this concept of standard process manager (SPM) is very appealing. Even smaller videos for example for implant assembling can be integrated. All that helps to reduce the learning curve of the Team, when a new revision system is introduced. Additionally, it minimizes the potential of making mistakes.
4. Conclusion
Digital technology is part of our daily lives and will also become more and more a part of orthopaedics. We already have collected some experience with digital technology in the OR over the past years. The current robots are a next step on the long way to quantitative TKA and THA. Future developments in robotics should help to speed up surgery and get rid of cutting blocks. By that the costs per procedure can be reduced, however the investment for a robot will still be high.
Improving outcome and minimizing the number of outliers are the final goals for this field of digital technology. The great chance of this technology will be the fact that a huge number of data will be collected case by case. With this kind of data we will be able to find out the relevant parameters of the process; and by that we will learn to develop a more individualised arthroplasty surgery.
As all health care systems over the world are short on money (except a few), it is not sure whether this technologic progress will continue everywhere in the same speed. And in huge arthroplasty centres the introduction of modern and expensive technology will be easier than in smaller ones. However, if the technology can finally prove an improvement for patient outcome, it has the potential to become the new Golden Standard.
References
- 1.Huang N.F.R., Dowsey M.M., Ee E., Stoney J.D., Babazadeh S., Choong P.F. Coronal alignment correlates with outcome after total knee arthroplasty. Five-year follow-up of a randomized controlled trial. J Arthroplast. 2012;27(9):1737–1741. doi: 10.1016/j.arth.2012.03.058. [DOI] [PubMed] [Google Scholar]
- 2.Cheng T.1, Zhao S., Peng X., Zhang X. Does computer-assisted surgery improve postoperative leg alignment and implant positioning following total knee arthroplasty? A meta-analysis of randomized controlled trials? Knee Surg Sport Traumatol Arthrosc. 2012 Jul;20(7):1307–1322. doi: 10.1007/s00167-011-1588-8. [DOI] [PubMed] [Google Scholar]
- 3.Roßkopf J., Singh P.K., Wolf P., Strauch M., Graichen H. Influence of intentional femoral component flexion in navigated TKA on gap balance and sagittal anatomy. Knee Surgery, Sport Traumatol Arthrosc. 2014;22(3):687–693. doi: 10.1007/s00167-013-2731-5. [DOI] [PubMed] [Google Scholar]
- 4.Mullaji A.B.1, Shetty G.M., Lingaraju A.P., Bhayde S. Which factors increase risk of malalignment of the hip-knee-ankle axis in TKA? Clin Orthop Relat Res. 2013 Jan;471(1):134–141. doi: 10.1007/s11999-012-2520-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rodrigues A.S.T., Gutierres M.A.P. Patient-specific instrumentation in total knee arthroplasty. Should we adopt it? Rev Brasileira Ortop (English Ed) 2017;52(3):242–250. doi: 10.1016/j.rboe.2016.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sassoon A., Nam D., Nunley R., Barrack R. Systematic review of patient-specific instrumentation in total knee arthroplasty: new but not improved. Clin Orthop Relat Res. 2015 Jan;473(1):151–158. doi: 10.1007/s11999-014-3804-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Deep K., Shankar S., Mahendra A. Computer assisted navigation in total knee and hip arthroplasty. Sicot-J. 2017;3:50. doi: 10.1051/sicotj/2017034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Roche M., Elson L., Anderson C. Dynamic soft tissue balancing in total knee arthroplasty. Orthop Clin N Am. 2014;45:157–165. doi: 10.1016/j.ocl.2013.11.001. [DOI] [PubMed] [Google Scholar]
- 9.Mehliß V., Strauch Leira M., Serrano Olaizola A., Scior W., Graichen H. Proven accuracy for a new dynamic gap measurement in navigated TKA. Knee Surg Sport Traumatol Arthrosc. 2019 Apr;27(4):1189–1195. doi: 10.1007/s00167-018-4989-0. [DOI] [PubMed] [Google Scholar]
- 10.Lehnen K.1, Giesinger K., Warschkow R., Porter M., Koch E., Kuster M.S. Clinical outcome using a ligament referencing technique in CAS versus conventional technique. Knee Surg Sport Traumatol Arthrosc. 2011 Jun;19(6):887–892. doi: 10.1007/s00167-010-1264-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schnurr C., Güdden I., Eysel P., König D.P. Influence of computer navigation on TKA revision rates. Int Orthop. 2012 Nov;36(11):2255–2256. doi: 10.1007/s00264-012-1606-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.De Steiger R.N., Liu Y.L., Graves S.E. Computer navigation for total knee arthroplasty reduces revision rate for patients less than sixty-five years of age. J Bone Joint Surg Am Vol. 2015;97(8):635–642. doi: 10.2106/JBJS.M.01496. [DOI] [PubMed] [Google Scholar]
- 13.Khuangsirikul S., Lekkreusuwan K., Chotanaphuti T. 10-Year patient satisfaction compared between computer-assisted navigation and conventional techniques in minimally invasive surgery total knee arthroplasty. Comput Assist Surg. 2016;21(1):172–175. doi: 10.1080/24699322.2016.1249959. [DOI] [PubMed] [Google Scholar]
- 14.Hasegawa M., Naito Y., Yamaguchi T., Wakabayashi H., Sudo A. Factors contributing to patient satisfaction and expectations following computer-assisted total knee arthroplasty. J Knee Surg. 2018;31(5):448–452. doi: 10.1055/s-0037-1604144. [DOI] [PubMed] [Google Scholar]
- 15.Neuprez A., Delcour J.P., Fatemi F. Patients' expectations impact their satisfaction following total hip or knee arthroplasty. PLoS One. 2016;11(12) doi: 10.1371/journal.pone.0167911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cherian J.J., Kapadia B.H., Banerjee S., Jauregui J.J., Issa K., Mont M.A. Current Reviews in Musculoskeletal Medicine. 2014. Mechanical, anatomical, and kinematic axis in TKA: concepts and practical applications; pp. 89–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yoon J.R., Han S.B., Jee M.K., Shin Y.S. Comparison of kinematic and mechanical alignment techniques in primary total knee arthroplasty. Medicine (United States) 2017;96(39) doi: 10.1097/MD.0000000000008157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rivière C., Lazic S., Boughton O., Wiart Y., Vïllet L., Cobb J. Current concepts for aligning knee implants: patient-specific or systematic? EFORT Open Rev. 2017;3(1):1–6. doi: 10.1302/2058-5241.3.170021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schindler O. Insall & Scott surgery of the knee. J Bone Joint Surg Br Vol. 2006;88-B(12):1678. [Google Scholar]
- 20.Matsuda S., Ito H. Ligament balancing in total knee arthroplasty - medial stabilizing technique. Asia Pac J Sport Med Arthrosc Rehabil Technol. 2015;2:108–113. doi: 10.1016/j.asmart.2015.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Daines B.K., Dennis D.A. Gap balancing vs. measured resection technique in total knee arthroplasty. Clin Orthop Surg. 2014;6:1–8. doi: 10.4055/cios.2014.6.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chia Z.-Y., Pang H.-N., Tan M.-H., Yeo S.-J. Gap difference in navigated TKA: a measure of the imbalanced flexion-extension gap. Sicot-J. 2018;4:30. doi: 10.1051/sicotj/2018007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lalys F., Jannin P. Surgical process modelling: a review. Int J Comput Assist Radiol Surg. 2014;9:495–511. doi: 10.1007/s11548-013-0940-5. [DOI] [PubMed] [Google Scholar]