Abstract
Background
Visceral Fat (VF) is the underlying culprit for cardiovascular diseases, type 2 diabetes, breast cancer, etc. VF can be estimated at present only by using expensive instruments as Bio Impedance Analyzer (BIA), DEXA scanner, etc. Measurement of Waist-Hip Ratio (WHR) can be used as a proxy for VF. Hence, the present study was done to assess the role of WHR as appropriate technology for assessment of VF. The aim of this study was to find correlation of Visceral Fat Area (VFA) with (WHR), Waist Circumference (WC) and Body Mass Index (BMI) in young healthy adults.
Methods
It was a descriptive cross-sectional study conducted on 215 healthy adults over one year in Western Maharashtra. Biospace 720 was used to assess VF. Data was analyzed by using software SPSS version 20.0. In body 720 was used to assess VF of subjects.
Results
Majority 155 (73%) were males and 57 (27%) were females. Nearly half (42% of males, 49% of females) had VFA above cut off value (i.e. 100 cm2) and 42% of males had WHR >0.9 and 56% of females had WHR >0.8. We found a very strong correlation between VFA and WHR (r = 0.936, p < 0.05) among males and females (r = 0.920, p < 0.05) and correlation between WC and BMI with VFA (r = 0.739, r = 0.758) for males, (r = 0.774, r = 0.605) for females was modest.
Conclusion
There is a strong correlation between VF and WHR. Measurement of WHR is simple, handy, and inexpensive tool which can be used as a surrogate to measure VF.
Keywords: Visceral fat area, Waist–hip ratio, Correlation, Appropriate technology
Introduction
Urbanization, unhealthy dietary practices and sedentary life style has lead to an increase in prevalence of lifestyle diseases in South East Asia Region (SEAR).1 The epidemic of obesity is spreading from urban to peri-urban and to rural population.2 Obesity represents excessive subcutaneous and intra-abdominal fat and is a known risk factor for many Non Communicable Diseases (NCDs).3, 4
Human body is composed of (a) active mass (muscle, liver, heart, etc.), (b) Fatty mass (fat), (c) extracellular fluid (blood, lymph, etc.), (d) connective tissue (skin, bones, connective tissue). Out of this total body fatty mass consist of subcutaneous fat and intra-abdominal fat. Abdominal fat can be divided into intraperitoneal and retroperitoneal fat. Intraperitoneal fat is also called as visceral fat (VF) which surrounds the mesenteries and omental fat masses.5 Metabolic obesity (visceral obesity with normal weight) represents fat levels that are higher than normal limits, even if a person's weight is within or below the standard for their height.6 Such people are thin outside but fat inside.
Increased VF is associated with the increased release of free fatty acids (FFA) into portal circulation which results in insulin resistance and other metabolic syndromes.5, 7 VF is also one of the main culprits for development of cardiovascular diseases, Type 2 diabetes, breast cancer, colorectal cancer, Alzheimer's disease, etc.4, 8, 9, 10, 11, 12, 13 These diseases account for 38 million (68%) worldwide.14
Measurement of VF is not easy. It can only be measured using expensive instruments like bio impedance analyzer (BIA), magnetic resonance analyzer and dual energy X-ray absorptiometry (DEXA) scanner, etc. BIA is a common method used to assess body composition in healthy adults. It offers the advantages of being non-invasive and relatively easy to perform.11, 15 However, its high cost and design restricts its use in field conditions and at community level.16, 17
Indians are known to have high central adiposity despite having lean body mass.18 Review of literature suggests that waist circumference (WC) and waist to height ratio (WHtR) are better measure for central and visceral adiposity over WHR and BMI. However, these findings have not yet been confirmed among Indians and in Asians.10, 19, 20
BMI though recommended as index of obesity and disease risks has its limitations as it doesn’t represent the correct measure of subcutaneous and visceral fat and hence obesity. Hence, it cannot predict the risks associated with high VF.21 The Y-Y paradox or the thin-fat Indian phenotype states that not all adults who have a BMI within the acceptable range of being healthy have healthy weight; rather they may have lots of fat but very little muscle and hence are at cardiovascular risk.22
There is an immense need to have simple, easy, cheap and handy to use tool in community settings which can be used as surrogate for VF measurement. This study was conducted to assess correlation of visceral fat area (VFA) with waist–hip ratio (WHR), waist circumference (WC), and BMI, to find out the best surrogate of VF.
Material and methods
This was a descriptive cross-sectional study, conducted on adults age > 18 years and apparently healthy individuals working in medical college of western Maharashtra during period from 01 Sept 2015 to 31 Aug 2016. Sample size was calculated as per mean and standard deviation for various parameters under study viz. body fat % and visceral fat area (VFA) (cm2) from previous studies. Sample size was also calculated as per correlation coefficient through review of literature between VFA and WHR. Sample size for the highest parameter was taken (i.e. 212). A Sampling frame of approx 800 was prepared after obtaining details from the administrative office of the college. Subjects were selected by simple random sampling using random number table. Subjects having any chronic illness such as metabolic disorders, hypertension and on any medication were excluded from study. Ethical clearance was taken from Institute Ethical Committee and informed consent from all participants.
Anthropometric measurements
Anthropometric parameters of subjects were measured by trained staff, maintaining the privacy. Weight (kg) was measured using electronic weighing machine, height (cm) measured near to 0.1 cm using stadiometer, waist circumference (WC) (cm) was measured at midpoint between lower rib and iliac crest using measuring tape near to 0.1 cm, hip circumference (HC) (cm) was measured at widest part around hip near to 0.1 cm using non-stretchable measuring tape at end of expiration. Visceral fat area (VFA) (cm2), skeletal muscle mass (SMM) (kg), body fat %, and fitness score (out of 100) were recorded from database of bio impedance analyzer (BIA) (Biospace In Body 720 made in South Korea), in which parameters get recorded automatically.23 Body composition parameters of apparently healthy subjects were measured and using BIA after 20 min of rest prior to study and current of 50 Hz was used. Subjects were required to adhere to certain prerequisites before undergoing actual measurements of various parameters like; subjects should be empty stomach for 2 h, to empty bladder, remove all metallic ornamentals, should not have any active or chronic illness, etc. so that results were accurate. Subjects were explained about instructions to follow during measurements as per manual of BIA. The study participants were asked to stand bare footed. Minimal clothing was kept on. The participant was asked to stand on the machine such that both heel and the ball of feet would touch the foot electrode. The participant was instructed to take the hand electrode in their hand and stand still for 2–3 min. Once the test was underway, the patient was asked to keep the same posture until the end of the test.
The modified classification of BMI for Asian populations was used in this study to define overweight (23–24.99 kg/m2) and obesity (>25 kg/m2) (based on the World Health Organization Asia Pacific Guidelines). Cutoff points used to define central obesity were WC ≥ 90 cm for men and ≥80 cm for women. WHR > 0.90 in men and >0.80 in women was taken as high.21, 24 Cut off for VFA in males and females was taken as 100 cm2 (based on manual of BIA).
Awareness about the prevention and control of Non-Communicable Diseases (NCDs) was provided to all participants and those with abnormal parameters were advised to keep check of same at regular intervals through diet and exercise.
Data was analyzed by SPSS version 20.0. Mean, SD and percentages were calculated. Correlation coefficient (Pearson product-moment correlation coefficient, a measure of the strength and direction of the linear relationship between two variables) was used. A value of correlation coefficient r = 0 signifies no linear relationship, +0.30 weak, +0.50 moderate and +0.70 strong positive linear relationship. Receiver Operating Characteristic curve (ROC curve) was drawn by plotting sensitivity, and 1 − specificity on X and Y axis respectively. Area under the curve (AUC) was calculated. An area of 1 represents a perfect test; .90–1 excellent, .80–.90 good, .70–.80 fair, .60–.70 poor, .50–.60 = fail (F). AUC for different variables was used to compare and find the best surrogate for VFA.
Results
Data was analyzed for 212 subjects. Majority 155 (73%) were males and 57 (23%) were females. Mean and SD for age was 29.4 ± 7.82 years and 30.63 ± 7.82 years for males and females respectively. Mean values for various anthropological parameters are given in Table 1.
Table 1.
Anthropological parameters of study subjects.
| Variables | Males (n = 155) |
Females (n = 57) |
||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| Age (years) | 29.4 | 7.82 | 30.63 | 7.82 |
| Weight (kg) | 73.16 | 8.84 | 60.80 | 6.05 |
| Height (m) | 1.73 | 0.54 | 1.58 | 0.05 |
| BMI (kg/m2) | 24.42 | 2.815 | 24.46 | 2.72 |
| WC (cm) | 83.06 | 7.91 | 78.19 | 8.67 |
| HC (cm) | 95.64 | 16.37 | 93.18 | 6.97 |
| WHR | 0.88 | 0.04 | 0.84 | 0.07 |
| VFA (cm2) | 87.41 | 29.18 | 93.16 | 18.72 |
| SMM (kg) | 33.88 | 26.19 | 21.04 | 2.84 |
| Body fat (%) | 16.91 | 6.57 | 25.91 | 6.63 |
| Fitness score (out of 100) | 72.48 | 6.18 | 68.37 | 6.50 |
We found 65 (42%) of males and 28 (49%) of females had VFA above cut off value (Table 2). Nearly 42% of males had WHR > 0.9 and more than half; 32(56%) of females had WHR > 0.8. Twenty one percent males and 45% females had WC above the cut value, i.e. >90 cm and >80 cm respectively. Fitness score was good for 63% males and 45% females. 42.5% males and 37% females were overweight. We found 27 subjects (14 males and 13 females) fulfilling the Y-Y paradox, i.e. BMI < 25 kg/m2 but VFA > 100 cm2 (Table 3).
Table 2.
Percentage distribution of study subjects for variables.
| Variable | Male (n = 155) | Female (n = 57) |
|---|---|---|
| VFA > 100 cm2 | 65 (42%) | 28 (49%) |
| WHR (> 0.9, > 0.8)a | 66 (42.5%) | 32 (56%) |
| WC (>90, >80)b | 32 (21%) | 26 (45%) |
| BMI > 25c | 66 (42.5%) | 21 (37%) |
| Fitness score (>70)d | 98 (63%) | 26 (45%) |
WHR > 0.9 & >0.8 cut off value for males and females respectively.
WC > 90 cm & >80 cm are cut off values for male and females respectively.
BMI > 25 kg/m2 cut off for both genders for over weight.
Fitness score of > 70(out of 100) was good fitness score for both genders.
Table 3.
Distribution of subjects based on BMI and VFA (YY Paradox).
| Gender | BMI | Visceral fat area |
Total | |
|---|---|---|---|---|
| <100 cm2 | >100 cm2 | |||
| Males | BMI < 25 kg/m2 | 75 | 14 | 89 |
| BMI > 25 kg/m2 | 14 | 52 | 66 | |
| Total | 89 | 66 | 155 | |
| Females | BMI < 25 kg/m2 | 23 | 13 | 36 |
| BMI > 25 kg/m2 | 6 | 15 | 21 | |
| Total | 29 | 28 | 57 | |
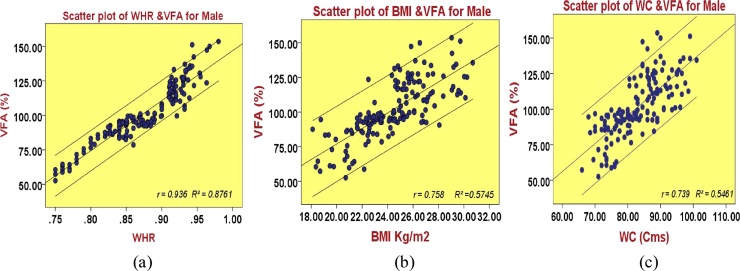
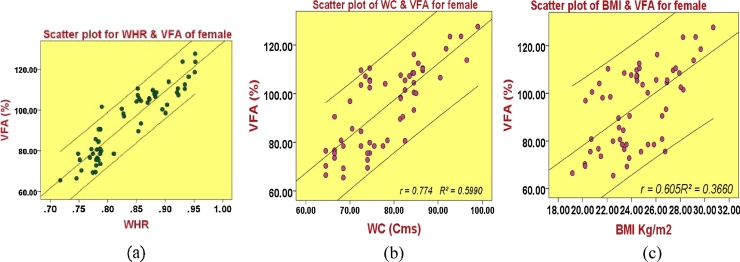
There was a very strong correlation between VFA and WHR (r = 0.936, R2 = 0.8761, CI (0.92, 0.95), p < 0.05) among males and females (r = 0.920, R2 = 0.8464, CI (0.90, 0.94), p < 0.05) Scatter plot drawn to see linear correlation between WHR, WC, BMI and VFA for both males and females (Fig. 1, Fig. 2).
Fig. 1.
Scatter plot showing correlation between VFA and WHR, WC, BMI in males.
Fig. 2.
Scatter plot showing correlation between VFA and WHR, WC, BMI in females.
There was moderate linear Correction between VFA and WC for males (r = 0.739), but strong for females (r = 0.774). There was modest linear correlation for BMI and VFA in males (r = 0.758) and weak correlation in females (r = 0.605).
For all variables, coefficient of determination (R2) was calculated using correlation coefficient values (Table 4). R2 for WHR (independent variable) can explains variation in VFA values (dependent variable) by 93.60% for males and around 92.00% for females. R2 for other variables (WC, BMI and fitness score) explains variation of VFA.
Table 4.
Statistical values for VFA and various parameters.
| Variables |
Male (n = 155) |
Female (n = 57) |
||||||
|---|---|---|---|---|---|---|---|---|
| ra | R2b | p value | CI | ra | R2b | p value | CI | |
| WHR | 0.936 | 0.8761 | 0.000 | (0.92,0.95) | 0.920 | 0.8464 | 0.000 | (0.90,0.94) |
| WC | 0.739 | 0.5461 | 0.000 | (0.67,0.79) | 0.774 | 0.5990 | 0.000 | (0.71,0.82) |
| BMI | 0.758 | 0.5745 | 0.000 | (0.69,0.81) | 0.605 | 0.3660 | 0.000 | (0.51,0.68) |
r = Pearson correlation coefficient value.
R2 = Coefficient of determination is square of correlation coefficient (r).
Regression equation (Y = a + bX) £ was calculated to predict values of dependent variable (VFA) from Independent variable (WHR) using regression analysis.
Regression equation was calculated for VFA and WHR as there was strong correlation
£ = a is known as a Y-intercept, b is known as slope of the regression line, it measures the amount of increase or change in y (dependent variable) for each unit change in x (independent variable). Y is the predicted value of y for a given value of x.
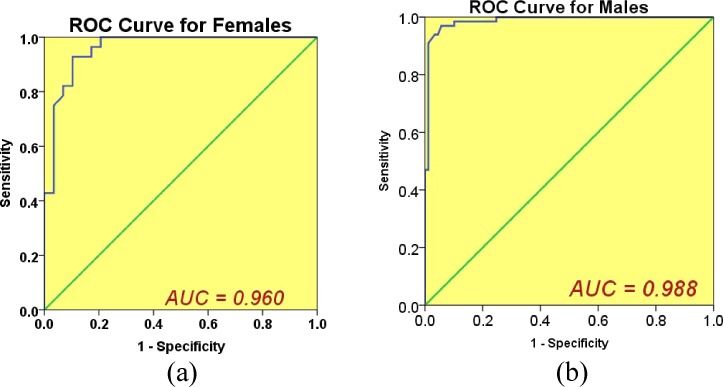
When Cohen kappa coefficient was calculated for VFA and WHR, WC and BMI, there was almost prefect agreement between VFA and WHR as k value was 0.858 and significant as p-value was 0.000. However, k value for VFA with WC (k = 0.483) & BMI (k = 0.473), showed moderate agreement with significant p. ROC curve between WHR and VF for males and females is given in Fig. 3(a) and (b) respectively. Area under curves along with 95% CI for various parameters is given in Table 5. Sensitivity and Specificity of WHR, WC and BMI with respect to VFA are given in Table 6.
Fig. 3.
ROC curve for WHR and VF% in males and females.
Table 5.
Area under ROC curve for WHR, WC and BMI and VF%.
| Variable | Area under curve (AUC) | 95%CI of AUC | Sensitivity at respective cut off value | 1-Specificity at respective cut off value |
|---|---|---|---|---|
| WHR (males) | 0.988 | 0.973–1.0 | 0.909 | 0.011 |
| WHR (females) | 0.960 | 0.913–1.0 | 0.964 | 0.207 |
| WC (males) | 0.940 | 0.905–0.975 | 0.409 | 0.022 |
| WC (females) | 0.874 | 0.787–0.961 | 0.714 | 0.207 |
| BMI (males) | 0.924 | 0.883–0.964 | 0.788 | 0.155 |
| BMI (females) | 0.812 | 0.700–0.925 | 0.571 | 0.207 |
Table 6.
Sensitivity and specificity for WHR, WC and BMI at respective cut offs in assessing body fat as compared to VFA.
| Variable | Sensitivity% | Specificity% |
|---|---|---|
| WHR (males) | 90.9 | 98.9 |
| WHR (females) | 96.4 | 79.3 |
| WC (males) | 40.9 | 97.8 |
| WC (females) | 71.4 | 79.3 |
| BMI (males) | 78.8 | 85.4 |
| BMI (females) | 57.1 | 79.3 |
Discussion
World Health Organisation (WHO) and UN (United Nations) have been targeting a reduction in overall mortality from NCDs (cardiovascular disease, cancer, diabetes or chronic respiratory disease, etc.) of 25% by 2025.1 To achieve this, there is need to screen people at risk for developing NCDs. There are various screening tools and anthropometric measurements available at community level, but there are limitations in its application across the world, because of difference in geographic regions and ethnicity of people.9, 17 In present study also we tried to assess the VFA and its correlation with WHR, WC and BMI using BIA, so that we can have a screening tool in community to identify individuals at risk because of high VFA using correct anthropometric measurement.8, 25 The anthropological profile/measurements of our subjects was quite similar to study conducted by Verma et al. in Kurushetra.21
We found strong correlation between the WHR and VFA for male and female (r = 0.936, r = 0.920) respectively, modest linear correlation between the WC and VFA for male and females (r = 0.739, r = 0.774) respectively, which is better than BMI for both genders. It suggests that WHR can be used as surrogate marker to predict risk associated for NCDs. Similar results found in a study conducted by Kumar et al. which documented that WHR can be taken as measure of central obesity.18 Hip measurements provide an additional valuable information about gluteofemoral muscle mass and bone structure. WHR hence can be a useful measure, as it also includes the accumulation of fat on the hips which may be beneficial for health.15 Different studies4, 12 have documented that there is an association between WHR and cardiovascular diseases. Our study has focused to establish its correlation with VF.
Vissers et al. in a systematic review and meta-analysis concluded that WC is superior to WHR because of its simplicity of measurement in the field area and WHR is a more robust measure of abdominal obesity and visceral adiposity.26
A case control study conducted by Anand et al. showed that high WHR is associated with cardiovascular diseases (CVDs) and it is better measure for central obesity.27 In a similar attempt as ours Rajput et al. found that WHtR is superior to WC and WHR.28 Many other studies have also focused on finding correlation of WHtR and VFA.29
We found negative linear correlation between the VFA and the fitness score; suggesting that individuals having lesser VFA are more fit. Mean body fat percentage was higher among females (25.91%).
We also found that WC for males at the given cut off has Sensitivity of 40% (False Negativity rate 60%), and for females 71% (False Negativity rate 30%) and the chance of missing out a large number of obese/overweight people if WC is used as a surrogate for VFA. Similarly BMI also has a false negativity of 22% and 47% in males and females. However, sensitivity in respect of WHR is 90.9% and 96.4% for males and females respectively which implies that WHR has much less percentage of false negatives and a better surrogate of VFA as compared to WC.
Individuals found to have high WHR in community can be counseled and encouraged for behavioral change, regular aerobic exercises and healthy dietary habits. Various studies have also documented decreased visceral fat after such interventions.29
Findings of present study suggest that WHR is better anthropometric measurement compared to WC and BMI, which can predict visceral fat. WHR is simple, easy to handle, cheap and appropriate, hence may be used by health workers (MPW, FHW or ASHA workers) at community setting for screening of individuals having greater risk for developing NCDs. WHR can be component, as screening tool under the NPCDCS (National programme for prevention and control of cancer, diabetes, cardiovascular disease and stroke). However, the limitation of the present study is that our subjects were from a single institution only.
Conclusion
There is a high correlation between WHR and VF. WHR can be labeled as appropriate technology to be used as a surrogate in community setting for identifying people having higher VF and hence high risk of diseases.
Conflicts of interest
The authors have none to declare.
References
- 1.World Health Organization Fact sheet on statistics of overweight obesity. Available from: http://www.who.int/mediacentre/factsheets/fs311/en Accessed 28.10.16.
- 2.Pradeepa R., Anjana R.M., Joshi S.R., Bhansali A., Deepa M., Joshi P.P. Prevalence of generalized & abdominal obesity in urban & rural. Indian J Med Res. 2015;142:139–150. doi: 10.4103/0971-5916.164234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ali A.T., Crowther N.J. Body fat distribution and insulin resistance. JEMDSA. 2005;10(3):6–9. [PubMed] [Google Scholar]
- 4.Sandeep S., Gokulakrishnan K., Velmurugan K., Deepa M., Mohan V. Visceral & subcutaneous abdominal fat in relation to insulin resistance & metabolic syndrome in non-diabetic south Indians. Indian J Med Res. 2010;131:629–635. [PubMed] [Google Scholar]
- 5.Klein S. The case of visceral fat: argument for the defense. J Clin Invest. 2004;113(11):1530–1531. doi: 10.1172/JCI22028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dudeja V., Misra A., Pandey R.M., Devina G., Kumar G., Vikram N.K. BMI does not accurately predict overweight in Asian Indians in northern India. Br J Nutr. 2001;86:105–112. doi: 10.1079/bjn2001382. [DOI] [PubMed] [Google Scholar]
- 7.Misra A., Chowbey P. Consensus statement for diagnosis of obesity, abdominal obesity and the metabolic syndrome for asian indians and recommendations for physical activity, medical and surgical management. JAPI. 2009;57:163–170. [PubMed] [Google Scholar]
- 8.Barreira T.V., Staiano A.E., Harrington D.M., Heymsfield S.B., Smith S.R., Bouchard C. Mayo Clin Proc. 2012;87(5):452–460. doi: 10.1016/j.mayocp.2011.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wells J.C.K. The evolution of human adiposity and obesity: where did it all go wrong? Dis Model Mech. 2012;5:595–607. doi: 10.1242/dmm.009613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thomas E.L., Parkinson J.R., Frost G.S. The missing risk: MRI and MRS phenotyping of abdominal adiposity and ectopic fat. Nat Publ Group. 2012;20(1):76–87. doi: 10.1038/oby.2011.142. [DOI] [PubMed] [Google Scholar]
- 11.Snijder M.B., Van Dam R.M., Visser M., Seidell J.C. What aspects of body fat are particularly hazardous and how do we measure them? Int J Epidemiol. 2006;35:83–92. doi: 10.1093/ije/dyi253. [DOI] [PubMed] [Google Scholar]
- 12.Singh R., Prakash M., Dubey R., Roy K., Kotwal A., Mahen A. Body composition parameters as correlates of coronary artery disease. Indian J Med Res. 2013;138:1016–1019. [PMC free article] [PubMed] [Google Scholar]
- 13.Rao S., Parab-waingankar P. Performance of waist circumference relative to BMI in predicting risk of obesity and hypertension among affluent Indian adults. Health. 2013;5(8A3):16–22. [Google Scholar]
- 14.World Health Organization . 2014. Global Status Report on Noncommunicable Diseases; pp. 1–128. Available from: http://www.who.int/ncd. [Google Scholar]
- 15.Sun S.S., Chumlea W.C., Heymsfield S.B. Development of bioelectrical impedance analysis prediction equations for body composition with the use of a multicomponent model for use in epidemiologic surveys 1–4. Am J Clin Nutr. 2003;77:331–340. doi: 10.1093/ajcn/77.2.331. [DOI] [PubMed] [Google Scholar]
- 16.Gupta S.R.N. Body composition analysis of staff members of college using bioelectrical impedance analysis method. Int J Chem Eng Appl. 2014;5(3):259–265. [Google Scholar]
- 17.Ellis K.J. Human body composition: in vivo methods CADAVER STUDIES. Physiol Rev. 2000;80(2):649–680. doi: 10.1152/physrev.2000.80.2.649. [DOI] [PubMed] [Google Scholar]
- 18.Kumar M.S., Palanisamy A., Anuradha M.P.N.M., Nagajyothi N., Haribabu N. International research journal of pharmacy. Int Res J Pharm. 2012;3(9):248–252. [Google Scholar]
- 19.Chen C., Chen Y., Chuang C. The study of anthropometric estimates in the visceral fat of healthy individuals. Nutr J. 2014;13(46):1–8. doi: 10.1186/1475-2891-13-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Soni A., Verma V. Anthropometric indicators of obesity and percent body fat – a measure for weight management. Int J Sci Res. 2015;4(4):2229–2233. [Google Scholar]
- 21.Verma M., Rajput M., Sahoo S.S., Kaur N., Rohilla R. Correlation between the percentage of body fat and surrogate indices of obesity among adult population in rural block of Haryana. J Family Med Prim Care. 2016;5:154–159. doi: 10.4103/2249-4863.184642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yagnik C.S., Yudkin J.S. The Y-Y paradox. Lancet. 2004;365:263. doi: 10.1016/S0140-6736(03)15269-5. [DOI] [PubMed] [Google Scholar]
- 23.InBody720 The precision body composition analyzer. User's Manual. 2004:1–46. Available from: http://www.biospace.co.kr. [Google Scholar]
- 24.The IDF consensus worldwide definition of the metabolic syndrome. Int Diabetes Fed. 2006:1–23. Available from: http://www.idf.org. [Google Scholar]
- 25.Kabir Z. Appropriate anthropometric indices to identify cardiometabolic risk in South Asians. WHO South-East Asia J Public Health. 2013;2(3-4):142–148. doi: 10.4103/2224-3151.206760. [DOI] [PubMed] [Google Scholar]
- 26.Vissers D., Hens W., Taeymans J., Baeyens J., Poortmans J., Van Gaal L. The effect of exercise on visceral adipose tissue in overweight adults: a systematic review and meta-analysis. PLoS ONE. 2013;8(2) doi: 10.1371/journal.pone.0056415. e56415(1–10) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Anand S.S., Islam S., Rosengren A. Risk factors for myocardial infarction in women and men: Insights from the INTERHEART study. Eur Heart J. 2008;29(7):932–940. doi: 10.1093/eurheartj/ehn018. [DOI] [PubMed] [Google Scholar]
- 28.Rajput R., Rajput M., Bairwa M., Singh J., Saini O., Shankar V. Waist height ratio: a universal screening tool for prediction of metabolic syndrome in urban and rural population of Haryana. Indian J Endocrinol Metab. 2014;18(3):394–399. doi: 10.4103/2230-8210.131201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lee K., Park H., Yum K. Cut-off values of visceral fat area and waist-to-height ratio: diagnostic criteria for obesity-related disorders in Korean children and adolescents. Yonsei Med J. 2012;53(1):99–105. doi: 10.3349/ymj.2012.53.1.99. [DOI] [PMC free article] [PubMed] [Google Scholar]; Newby P.K., Muller D., Hallfrisch J., Qiao N., Andres R., Tucker K.L. Dietary patterns and changes in body mass index and waist circumference in adults. Am J Clin Nutr. 2003;77:1417–1425. doi: 10.1093/ajcn/77.6.1417. [DOI] [PubMed] [Google Scholar]