Abstract
Introduction
Autologous bone grafts are used to treat scaphoid non-union with shortening and humpback deformity. The superiority of internally fixed bone graft to embedded bone graft has not been clearly proven.
Methods
Retrospectively analyzed 42 cases of scaphoid waist non-union treated using the “butterfly bone graft” (modified Matti-Russe technique).
Results
Complete healing was reached by all patients, with an average time of 4.4 (SD ± 0.7) months. Mayo Wrist Score improved from and QuickDASH score significantly improved in all patients after treatment.
Conclusions
Butterfly bone graft is effective and reliable in treating scaphoid non-union with shortening and humpback deformity.
Keywords: Humpback deformity, Scaphoid non-union, Bone graft, Scaphoid, Fracture healing, Nonunion
1. Introduction
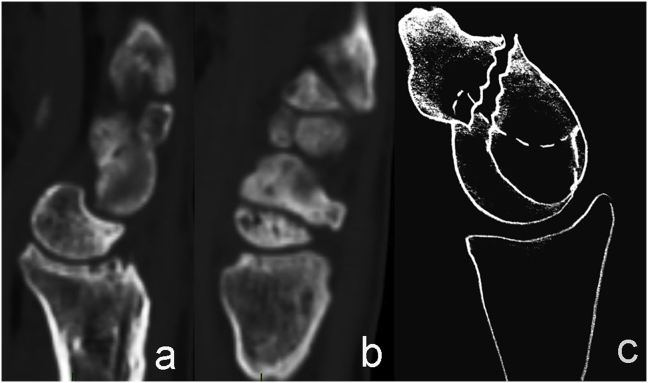
Scaphoid non-union (SNU) could be an unfortunate complication of a scaphoid fracture. The scaphoid bone had not a good healing capacity, it depends on a poor vascular support from the intraosseus vascularization.1,2 The major blood vessel derives from the radial artery and enters dorsally through small foramina.1 Scaphoid is a bone without periosteum, therefore it could heal only by primary bone healing. Furthermore, a scaphoid fracture could displace, depending on the kind and the plane of fracture, and, as a result, the healing capacity is impaired.2 In case of displaced and/or unstable fracture (type B according to Herbert classification), healing is impaired and bone resorption may occurs, causing bone loss at the scaphoid waist. Therefore, the bone shortens and the distal pole bends towards the wrist (flexion deformity) (Fig. 1).2 Finally, fibrous scar tissue at the fracture site fixes the deformity, thus carpal kinematics and function are impaired. SNU of the waist can be treated with open surgical debridement and bone grafting, to allow a natural healing process. Autologous bone is considered the best choice in term of osteoconduction, osteoinduction and osteogenesis.3,4
Fig. 1.
Carpal disarrangement caused by scaphoid humpback deformity.
The aims of surgical treatment are to give primary stability and avoid rotation of fragments in order to allow sufficient time for bone graft incorporation. Furthermore bone graft should restore length and shape of the scaphoid bone, restoring the correct scapholunate angle. Considering the state of art of fixation systems available, kind and design of graft and the combination of them, to date there is no sufficient evidence in favor of a best treatment for SNU.5,6 Furthermore, contrary to a frequent assumption, internally fixed bone grafts are not significantly superior to embedded bone grafts (without internal fixation).5,7
Scaphoid bone grafting was firstly described by Matti in 1937, Russe and Green have been amongst the first who tried to improve it.2 In 1997, Fanfani et al. described a modified Matti-Russe technique called “butterfly bone graft” (BBG), due to its special shape.8 BBG is currently widely used in our institution. This kind of bone graft is expected to embed perfectly fixing the fracture, correcting any shortening and deformity and filling the bone loss. We report our experience with this particular kind of bone graft.
2. Materials and methods
2.1. Study design and setting
We conducted a retrospective analysis on patients with waist SNU operated using BBG in our institution (Fondazione Policlinico Universitario A. Gemelli IRCCS, Rome) from January 2012 to February 2016. All surgical procedures were performed by two expert hand surgeons (G.T. and R.D.V.). The study was in accordance with the principles of the Declaration of Helsinki. Considering that our method was a modification of a widely used technique, an ethical approval was not requested. Written informed consents were obtained in all patient before the surgery.
Complete data for patients suffering from SNU included:
-
-
pre and post-operative plain radiographs (semi-pronated oblique view, anterior-posterior view, lateral view);
-
-
pre and post-operative functional assessment using QuickDASH score (validated Italian version),9 Mayo wrist score (MWS)
-
-
Pain (measured using VAS) and symptoms registration.
2.2. Aim of the study
The aim of the investigation was to evaluate clinical, radiographic and functional results from patients suffering from SNU of the waist (with shortening and humpback deformity) treated using BBG. Complete healing was defined as radiographic fusion and contemporary absence of clinical findings (spontaneous pain at day and/or night, pain at wrist motion, pain at compression of snuffbox).
2.3. Inclusions and exclusion criteria
Indication to this techniques is SNU of the waist, with shortening and humpback deformity. Patients affected by scaphoid non-union advanced collapse (SNAC) grade 2, 3 and 4,10 associated ligamentous lesions, proximal pole avascular necrosis, previous trauma and/or surgical treatment on the treated hand were excluded. Patients with less than 6 months follow-up and incomplete pre and post-operative data settings were excluded.
2.4. Statistical analysis
Data were statistically analyzed using the t-Student test to compare quantitative variables. The significance was established for a value of p < 0.05. Dedicated SPPS v.19.0 software statistical calculation software (SOSS Inc, Chicago, IL) was employed. Data are presented as mean and standard deviation (SD). Only one decimal place has been reported, rounded up.
2.5. Participants
Fifty patients were operated in the examined period. All patient extracted had complete pre and post-operative data (plain radiographs, functional assessment, clinical assessment). Eight of them were excluded because they met exclusion criteria. Forty-two patients (39 males and 3 females) were included in the study.
The average age was 30.5 (SD ± 6.7) years. Thirty-five patients (83.3%) underwent a conservative treatment for a period of 6–12 weeks with a cast. The remaining seven patients had a neglected scaphoid fracture, and they had been left untreated. The interval between the injury and the time of surgical treatment was an average of 18 months (range: 12–37 months).
2.6. Technique
General anesthesia and supine position are required. Both upper limb and iliac crest (contralateral) operating field are prepared. A pneumatic cuff is applied at arm for transient ischemia.
A volar approach is performed, in agreement with Gelberman,1 to respect dorsal vascularization. A skin incision at volar-lateral region of the wrist is performed on the tendon of flexor carpi radialis (FCR), which is retracted ulnarly. The radial artery does not cross the exposure. The palmar cutaneous branch of the median nerve is identified and protected. The capsule of the wrist joint is incised, exposing the scaphoid from proximal to distal pole. Non-union is exposed. A debridement is performed in a first time without using powered tools, thus the gap is exposed. Then the housing for the bone graft is created using the high-powered burr.
A 5 cm incision to iliac crest, centered on the iliac tubercle, is performed. The deeper tissues are dissected, the fascia over gluteus medius and the fascia over the external oblique are recognized. The origins of the gluteus medius and minimus are removed to expose the bone below. A parallelepiped of tricortical bone graft of about 3.5 cm length is taken with a chisel.
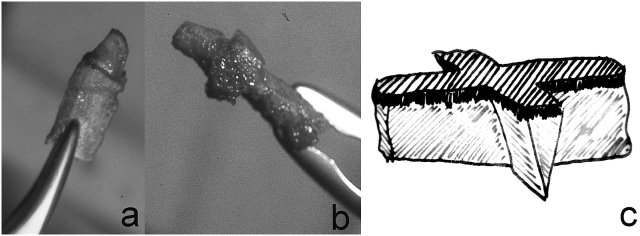
Two lateral masses (“wings”) are sculpted on the rough parallelepiped bone graft. The graft obtained is made of a major axis, which links proximal pole to distal pole of the scaphoid bone, and two “wings” in the middle third, shaped in a wedged way. The apex of the wedged part should be oriented dorsally and the cancellous portion of bone graft should stay inside the scaphoid bone.
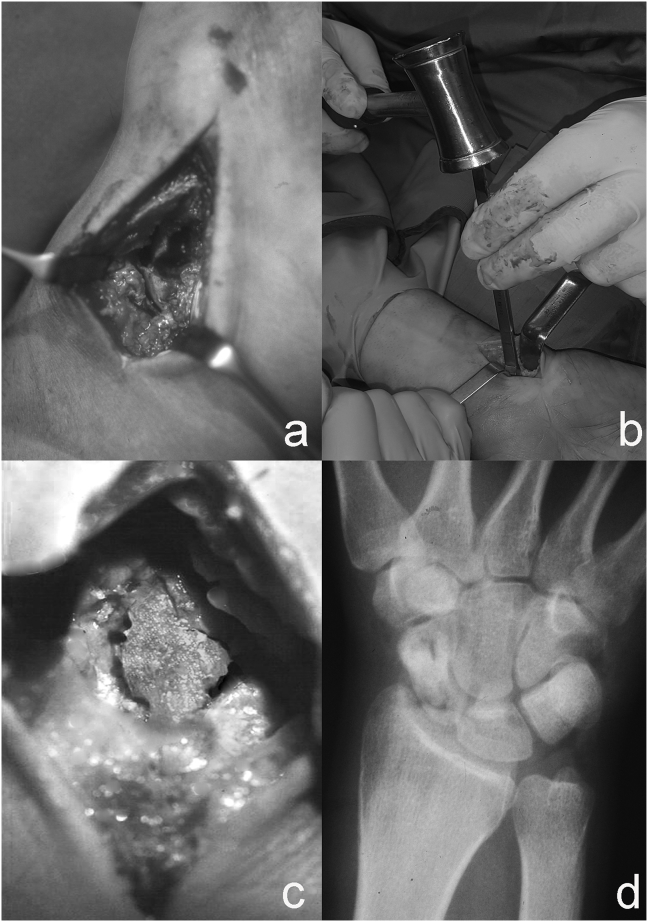
The result is an originally shaped graft that is called “butterfly bone graft” (Fig. 2). The bone graft is embedded into the bone using a hammer. Internal fixation is not required (Fig. 3). The correction of flexion deformity is observed intra-operatively. The central gap is filled and rotation of the poles is fixed.
Fig. 2.
Butterfly bone graft before being inserted.
Fig. 3.
The housing of the bone graft is exposed (a). The bone graft is embedded using hammer (b). Bone graft embedded (c). Butterfly bone graft on X-Ray (d).
An accurate capsular closure using resorbable stitches is performed. Post-operative management includes immobilization in a long arm (above elbow) cast for 4 weeks, then a short forearm cast is recommended for further 8 weeks.
2.7. Follow up and rehabilitation
Early mobilization of the fingers and the shoulder is recommended. Patients are evaluated clinically, to assess the onset of complications (i.e. stiffness, algodistrophy, infections).
Post-operative radiographic assessment was performed through plain radiographs scheduled as follows: post-operative (t0), 1 week, 4 weeks, 8 weeks, 12 weeks, then every month until radiologic union.
Post-operative function was assessed as follow:
-
-
MWS: pre operative, 6 months, 12 months, long term (last visit).
-
-
DASH: pre operative, 12 months, long term (last visit).
-
-
VAS (for pain): pre operative, 6 months, 12 months, long term (last visit).
After the removal of cast, patients were trained to perform passive and active movements of the wrist and forearm. A targeted physiotherapy were always prescribed.
3. Results
The mean follow-up time was 48 months (SD ± 15). All patients (100%) reached complete healing. Complete healing was reached in 4.4 (DS ±0.7) months. All patients improved their hand function. The mean MWS was 42.5 (DS ±6.1) before the surgery, increased to 86.2 (DS ±4.3) at 6 months and 89.1 (DS ±5.8) at last follow up (p = 0.03). The mean QuickDASH was 64.2 (DS ±8.8) before surgery, increased to 10.1 (DS ±3.4) at 12 months (p = 0.002). After a week, measured pain VAS score was 5.7 (DS ±1.9) and decreased to 2.3 (DS ±0.8) at last follow-up (p = 0.002). The overage scapholunate angle value was 46.3° (DS ±8.5°), measured at the last radiographic assessment (normal range 30°–60°). No wound infection has been reported. All patients complained about donor site pain, declining over time. In three patients (7.1%) of our series we had algodystrophy as a complication, recovered within 6 months from surgery with an appropriate treatment. No patient needed to be surgically retreated. All patients needed physiotherapy to reach the complete recovery.
4. Discussion
Bone graft is indicated in SNU with bone shortening and bending (humpback deformity). Type B fractures lead to dorsal intercalated segment instability (DISI), thus the full length healing should be reached (Fig. 1).
The restoration of the original shape is not a satisfying result if the fracture does not heal. Hence, the choice of bone graft shape is an important issue, and recent and past literature focuses on several techniques to harvest and sculpt the bone graft, proposed until recent times, to improve bone healing.2,8,11, 12, 13, 14, 15, 16, 17
Cadaveric studies have been performed to investigate for the best fixation method alternative to Matti-Russe, with variable results.18, 19, 20 Unfortunately, cadaveric studies cannot assess the healing process. Matti-Russe and variants technique is today still in use.7,11 The problem of surgical treatment of SNU has not all been completely solved to date.5, 6, 7
The estimated fusion rate using bone graft alone is almost 80%.5,15 However results vary greatly in studies, with a fusion rate up to 100% of fusion rate.5,7,15 Dustmann et al. reported a fusion rate of 84.6% using a modified Matti-Russe technique (ellipsoid graft harvested from iliac crest without fixation). Failure occurred only in previously treated patients (using other techniques) or in sequelae of proximal pole fracture.11 However, in our study where the abovementioned categories were excluded, we succeeded in 100% of cases.
Fixing the bone graft is not exempt from problems and complications, and surgical treatment can fail.5,7,21, 22, 23 The volume of bone graft is reduced by screws or K wires used to fix the bone, thus sintering is impaired and compression is progressively lost.11 This can contribute to lower bone healing capacity. Furthermore polar cartilage is sacrificed.11 Conversely, complications can occur because of instrumentation.24 On the other hand, embedded bone graft without fixation lead to bone stock preservation, and is easier to operate again in case of failure. Internally fixed bone graft does not heal faster, compared with our results.11,15,21,22 Goyal et al. performed a randomized controlled trial comparing non-vascularized bone graft harvested from radius and iliac crest fixed with a screw. They reported a fusion rate of 87% at a medium time of more than four months.21 In our study healing was reached in 4.4 (DS ±0.7) months.
Fixing the bone graft does not avoid further immobilization after surgery, whatever the technique used.13,15,17,21,23,25 Immobilization time vary among the studies. Munk and Larsen systematically reviewed 147 publications including 5246 SNU treated. The average immobilization time after surgery for non vascularized bone graft without fixation was 15 weeks and 7 weeks respectively.15 Dustman recommend an immobilization of 12 weeks after non-vascularized ellipsoid bone graft.11 In our opinion, it might be prudent to avoid protonation and supination of the forearm at least for the first 4 weeks, to avoid stressing the scaphoid. Afterwards cast could be shortened, trusting in the stability of the bone graft. Our results demonstrated that upper limb function is not compromised, MWS and quick dash significantly improved after treatment, compared to pre-treatment assessment.
4.1. From the first bone graft to the present day
Matti-Russe technique allows to restore scaphoid length and gives stability, but further techniques have been proposed to optimize the original technique.2 Green proposed a bone graft as a “matchstick” obtained from the volar aspect of radius. The gap at non-union site was filled with packed cancellous bone derived from the volar aspect of radius.2,12 Fernandez et al. introduced the importance of wedge bone graft in order to correct the humpback deformity. In 1984 Fernandez proposed a wedge shaped bone graft with two K wires to fix it, to correct the bone loss and the bending by a volar approach.13
Dustman et al. have recently described a new kind of sculpting of the bone graft harvested from the iliac crest, an oversized ellipsoid bone graft, in order to compress at the fracture site.11
Previously Fanfani at al. in 1997 described the BBG.8 Using this kind of bone graft, cortical bone remains outside, giving protection to cancellous bone and stability to the scaphoid bone. The wedge shape allows to correct humpback deformity and restore the scapholunate angle, similarly to Fernandez's technique.13 BBG has a two-axis designed bone graft that perfectly embeds into the gap, giving primary stability to the synthesis and not needing further fixation. Bone graft is harvested from iliac crest, avoiding to further compromise the affected wrist. Finally, bone graft has a big area of exposed cancellous bone. In our experience healing was reached in all cases.
In our experience BBG is effective in treatment of even long-standing SNU of the waist, with a very satisfying fusion rate (100%) with an appropriate average healing time (4.4 ± 0.7 months). Hand function improvement was observed in all patients. Hence we consider BBG a reliable, effective and low-cost technique for treatment of SNU.
4.2. Limitations
This is a retrospective study. All patients complained about pain at donor site, but it declined over time. Immobilization time is quite long, but it is necessary in order to reach the complete healing, in agreement with other studies.2,11,15 We reported only three cases of algodystrophy as a complication, that completely recovered after an appropriate treatment.
5. Conclusions
Our experience demonstrates that bone graft without fixation is still a viable option for treatment of SNU with humpback deformity. BBG is effective in restoring carpal anatomical relationships. The success in healing was reached in all cases. We consider important to immobilize the upper limb for 90 days, but that did not prevent to obtain very good functional outcomes. Differently from other studies, we excluded patient who underwent previous surgery, reducing the probability of failure.11 This study demonstrates that research in bone graft design should not be neglected, even if effective instrumentation are available today.
Declaration of competing interest
The authors report no conflicts of interest and no source of funding.
References
- 1.Gelberman R.H., Menon J. The vascularity of the scaphoid bone. J Hand Surg Am. 1980;5(5):508–513. doi: 10.1016/s0363-5023(80)80087-6. [DOI] [PubMed] [Google Scholar]
- 2.Lee S. Fractures of carpal bones. In: Wolfe S., Pederson W., Kozin S.H.C.M., editors. Green's Operative Hand Surgery. seventh ed. Elsevier; Philadelphia: 2016. p. 2091. [Google Scholar]
- 3.Wang W., Yeung K.W.K. Bioactive Materials Bone grafts and biomaterials substitutes for bone defect repair : a review. Bioact Mater. 2017 doi: 10.1016/j.bioactmat.2017.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bauer T.W., Muschler G.F. Bone graft materials. An overview of the basic science. Clin Orthop Relat Res. 2000;371:10–27. [PubMed] [Google Scholar]
- 5.Pinder R.M., Brkljac M., Rix L., Muir L., Brewster M. Treatment of scaphoid nonunion: a systematic review of the existing evidence. J Hand Surg Am. 2015;40(9):1797–1805. doi: 10.1016/j.jhsa.2015.05.003. e3. [DOI] [PubMed] [Google Scholar]
- 6.Ferguson D.O., Shanbhag V., Hedley H., Reichert I., Lipscombe S., Davis T.R.C. Scaphoid fracture non-union: a systematic review of surgical treatment using bone graft. J Hand Surg Eur. 2016;41(5):492–500. doi: 10.1177/1753193415604778. [DOI] [PubMed] [Google Scholar]
- 7.Brewester M., Pinder R., Muir L. Scaphoid non-union. In: Giddins G., Leblebicioğlu G., editors. Evidenced Based Data in Hand Surgery and Therapy. IRIS; Budapest: 2017. pp. 316–335.http://fessh.com/library/2017_icbook.pdf [Google Scholar]
- 8.1997. https://www.sicm.it/it/eventi/15873/La-Monografia-Lo-Scafoide.html VvAa Lo Scafoide. Mattioli.
- 9.Padua R., Padua L., Ceccarelli E. Italian version of the Disability of the Arm, Shoulder and Hand (DASH) questionnaire. Cross-cultural adaptation and validation. J Hand Surg Br. 2003;28(2):179–186. doi: 10.1016/s0266-7681(02)00303-0. [DOI] [PubMed] [Google Scholar]
- 10.Krimmer H., Krapohl B., Sauerbier M., Hahn P. [Post-traumatic carpal collapse (SLAC- and SNAC-wrist)--stage classification and therapeutic possibilities] Handchir Mikrochir Plast Chir. 1997;29(5):228–233. [PubMed] [Google Scholar]
- 11.Dustmann M., Bajinski R., Tripp A., Gulke J., Wachter N. A modified Matti-Russe technique of grafting scaphoid non-unions. Arch Orthop Trauma Surg. 2017;137(6):867–873. doi: 10.1007/s00402-017-2680-4. [DOI] [PubMed] [Google Scholar]
- 12.Green D.P. The effect of avascular necrosis on Russe bone grafting for scaphoid nonunion. J Hand Surg Am. 1985;10(5):597–605. doi: 10.1016/s0363-5023(85)80191-x. [DOI] [PubMed] [Google Scholar]
- 13.Fernandez D.L. A technique for anterior wedge-shaped grafts for scaphoid nonunions with carpal instability. J Hand Surg Am. 1984;9(5):733–737. doi: 10.1016/s0363-5023(84)80025-8. [DOI] [PubMed] [Google Scholar]
- 14.Reed D.N., Fulcher S.M., Harrison S.J. Unstable scaphoid nonunion treatment technique: use of a volar distal radius corticocancellous autograft. Tech Hand Up Extrem Surg. 2012;16(2):91–94. doi: 10.1097/BTH.0b013e31824cc258. [DOI] [PubMed] [Google Scholar]
- 15.Munk B., Larsen C.F. Bone grafting the scaphoid nonunion: a systematic review of 147 publications including 5 246 cases of scaphoid nonunion. Acta Orthop Scand. 2004;75(5):618–629. doi: 10.1080/00016470410001529. [DOI] [PubMed] [Google Scholar]
- 16.Aydin U., Thirkannad S.M. Internal bone grafting for the treatment of scaphoid nonunions. Tech Hand Up Extrem Surg. 2017;21(1):18–21. doi: 10.1097/BTH.0000000000000137. [DOI] [PubMed] [Google Scholar]
- 17.Poggetti A., Rosati M., Castellini I. Treatment of scaphoid waist nonunion using olecranon bone graft and stryker asnis micro cannulated screw: a retrospective study-80 case studies and 6 Years of follow-up. J Wrist Surg. 2015;4(3):194–199. doi: 10.1055/s-0035-1556865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mandaleson A., Tham S.K., Lewis C., Ackland D.C., Ek E.T. Scaphoid fracture fixation in a nonunion model: a biomechanical study comparing 3 types of fixation. J Hand Surg Am. 2018;43(3):221–228. doi: 10.1016/j.jhsa.2017.10.005. [DOI] [PubMed] [Google Scholar]
- 19.Jurkowitsch J., Dall'Ara E., Quadlbauer S. Rotational stability in screw-fixed scaphoid fractures compared to plate-fixed scaphoid fractures. Arch Orthop Trauma Surg. 2016;136(11):1623–1628. doi: 10.1007/s00402-016-2556-z. [DOI] [PubMed] [Google Scholar]
- 20.Goodwin J., Castaneda P., Drace P., Edwards S. A biomechanical comparison of screw and plate fixations for scaphoid fractures. J Wrist Surg. 2018;7(1):77–80. doi: 10.1055/s-0037-1606123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goyal T., Sankineani S.R., Tripathy S.K. Local distal radius bone graft versus iliac crest bone graft for scaphoid nonunion: a comparative study. Musculoskelet Surg. 2013;97(2):109–114. doi: 10.1007/s12306-012-0219-y. [DOI] [PubMed] [Google Scholar]
- 22.Talia A.J., Fraval A., Halliday L., McKie G., Paiva J., Thai D.M. Scaphoid specific volar locking plate and non-vascularised iliac crest bone graft in scaphoid non-union. A comparative cohort study. J Orthop. 2019;16(4):337–341. doi: 10.1016/j.jor.2019.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Quadlbauer S., Pezzei C., Beer T. Treatment of scaphoid waist nonunion by one, two headless compression screws or plate with or without additional extracorporeal shockwave therapy. Arch Orthop Trauma Surg. 2019;139(2):281–293. doi: 10.1007/s00402-018-3087-6. [DOI] [PubMed] [Google Scholar]
- 24.Starnoni M., Colzani G., De Santis G., Leti Acciaro A. 2019. Median Nerve Injury Caused by Screw Malpositioning in Percutaneous Scaphoid Fracture Fixation. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wu F., Ng C.Y., Hayton M. The authors' technique for volar plating of scaphoid nonunion. Hand Clin. 2019;35(3):281–286. doi: 10.1016/j.hcl.2019.03.009. [DOI] [PubMed] [Google Scholar]