Abstract
Introduction
Proximal humerus nails (PHN) are commonly used for the treatment of simple proximal humerus fractures, and have a reported malunion rate of about 10%. The surgeons who used PHN in one medical institution have noticed a high rate of fracture re-displacement in the early post-operative period. This study's aim is to evaluate the rate of secondary displacement and malunion of patients treated for two part proximal humerus fractures with an angle-stable PHN (MultiLoc), and to assess possible risk factors for this secondary displacement.
Methods
A retrospective study comprised of 25 consecutive patients with 2 part surgical neck or metaphysis displaced proximal humerus fracture, treated with PHN between the years 2014–2017. Results assessed included radiographic measures (neck-shaft angle) and clinical data: range of motion (ROM) and functional scores (Constant, DASH, SSV). A univariate regression analysis was used to assess possible risk factors for secondary displacement.
Results
Mean age was 66.6 (range 17–93), and mean follow up was 20 months (range 6–40). Mean neck shaft angle (NSA) changed from 139.1° post operatively to 122.6° at last follow up, with 6 patients (24%) having a NSA change larger than 20°. Two patients (8%) ended up with NSA less than 90°, defined as malunion. The deltoid tuberosity index was found to correlate with the degree of displacement (−0.41, p = 0.04).
Conclusions
PHN for simple displaced proximal humerus fractures was associated with fair clinical results but an unacceptable rate secondary displacement. The deltoid tuberosity index was found to correlate with the degree of this secondary displacement.
Keywords: Proximal humerus fracture, Proximal humerus nail, Fracture displacement, Malunion, Deltoid tuberosity index
1. Introduction
Proximal humerus fractures (PHF) are the third most common fractures in the adult population and account for 6% of all fractures.1 The incidence of PHF increases with age, with more than 70% occurring in patients over 60 years of age,2 and they are 3–4 times more common in elderly women than men.3,4 Approximately 80% of PHF are non-displaced or minimally displaced, for which non-operative treatment is usually indicated.4,5
In cases of displaced PHF, surgical treatment is usually indicated in active patients. Many operative techniques have been implemented, with no single technique demonstrating evidence-based superiority.6 For displaced 2 part fractures, the common practice is open reduction and internal fixation with a locking plate or closed reduction and internal fixation with intra medullary nail (IMN).7 The purported advantages of IMN include decreased soft tissue disruption, preservation of blood supply to the humerus, and shorter operative times.8 Historically, proximal humerus nails suffered from inadequate security of the proximal screws, which led to screw back out and loss of proximal fixation.9 “Third generation” nails evolved to solve this issue by implementing a more secure locking mechanism that allows for a fixed angular stable contract.9
In our Medical institution, an angle-stable proximal humerus nail (MultiLoc by Synthes, West Chester, PA USA) was introduced in 2014 and was utilized mostly for displaced 2 part surgical neck or metaphysis proximal humerus fracture. The senior surgeons who performed the operations have noticed a high rate of fracture re-displacement in the early post-operative period. This study's main aim is to evaluate the rate of secondary displacement and malunion in this cohort, and to present their functional and radiological outcomes. A second aim is to evaluate possible risk factors for this secondary displacement. Since the literature about proximal humerus fracture treatment usually suffers from high heterogeneity of fracture types, we have decided to examine 2 part surgical neck or metaphysis fractures only.
2. Methods
After institutional review board approval, a retrospective study was preformed examining all patients who were surgically treated for a displaced 2 part surgical neck or metaphysis proximal humerus fracture within one medical center between 2014 and 2017. Surgeries were performed by 2 senior fellowship trained shoulder surgeons (Y.G. and O.C.). Patients were included after a minimum follow up of 6 months.
Collected data included age, gender, type of fracture, diameter of nail, number of proximal screws used. Outcome measures included range of motion, subjective shoulder value (SSV),10 modified constant score,11 disabilities of the arm shoulder and hand score (QuickDASH),12,13 and complications. Radiographic measures included the deltoid tuberosity index (DTI)14 in the pre-operative AP radiograph, and the neck-shaft angle (NSA) on post-operative AP radiographs taken on the first post-operative day and in the last follow up. The NSA was evaluated by 2 different senior residents who were not involved in the surgical treatment, and the average between the measures was used. Malunion was defined as a varus\valgus angular deformity of more than 45° (Type III malunion according to Beredjiklian).15 Possible risk factors for secondary displacement assessed included age, sex, number of proximal screws, nail diameter, DTI, early post-operative NSA.
Surgical method: Surgery was performed under general anesthesia, with the patient in a beach-chair position. Following standard preparation and draping, a trans deltoid approach was performed: skin incision, exposing of the deltoid muscle and splitting the anterior and middle sections, bursectomy, and longitudinal split of the supraspinatus tendon. The nail insertion point was determined under fluoroscopy at the top of the humeral head approximately 1 cm medial and 1 cm posterior to the bicipital groove. A Multilock PHN (length 160 mm) was inserted until reaching 1–2 mm deep to the cortical bone. Proximal fixation of the humeral head was done usually using 2–3 screws. Post-operative protocol involved 6 weeks of sling use, with pendulum exercises for the first 2 weeks and gentle passive range-of-motion exercises in the remaining 4 weeks, followed by full range of motion exercises.
Statistical methods: All statistical analyses were performed with IBM SPSS 19. Descriptive statistics included means, standard deviations, ranges, and proportions. Comparative statistics included the t-test for numerical data, Mann-whitney test for ordinal data and χ2 test for categorical data. Univariate logistic regression was conducted to assess for possible risk factors for displacement of the fracture, represented by the variable “NSA difference”. The significance level was set at α = 0.05.
3. Results
A total of 27 patients met the inclusion criteria, of whom 2 were lost to follow-up, leaving 25 patients in the cohort. The patients were followed for an average of 20 ± 11 months (range 6–40 months). The average age at the time of surgery was 67 ± 21 years (range 17–93 years). 21 were female (84%) and 4 were male (16%). In 22 cases (88%) the fracture was a surgical neck fracture, and in the remaining 3 cases (12%) a more distal metaphyseal fracture. In all cases nail length was 160 mm, and the diameter was 8 mm in 17 cases (68%) and 9.5 mm in 8 cases (32%). The number of proximal screws used was 1 in 1 case (4%), 2 in 14 cases (56%), 3 in 8 cases (32%), and 4 in 2 cases (8%).
The range of motion and functional outcomes are summarized in Table 1.
Table 1.
Range of motion and functional outcomes.
| All (N = 25) | |
|---|---|
| Forward flexion, deg ± SD | 121 ± 37 |
| Abduction, deg ± SD | 108 ± 46 |
| External rotaion, deg ± SD | 44 ± 27 |
| Internal rotation (a) | 6 ± 3 |
| SSV | 78 ± 18 |
| Constant score | 54 ± 21 |
| DASH score | 31 ± 22 |
DASH - disabilities of the arm shoulder and hand, SSV – subjective shoulder value.
Score is rated according to the constant score internal rotation criteria: lateral thigh-0, buttock-2, lumbosacral junction-4, L3 (waist)-6, T12–8, T7 (intrascapular)-10.
Radiographic measures: DTI had an average of 1.45 ± 0.17 (range 1.20–1.90). Average immediate post-operative NSA was 139° ± 11° (range 120°–169°), and NSA at last follow up was 123° ± 17° (range 83°–168°). Overall 6 patients had NSA difference of over 20°, representing severe loss of reduction. Their range of motion and functional outcomes did not differ significantly from patients without reduction loss (Table 2). Two patients had a final NSA of less than 90°, representing malunion (Fig. 1).
Table 2.
Range of motion and functional outcomes of patients with and without loss of reduction.
| Loss of reduction (N = 6) | No Loss of reduction (N = 19) | P value | |
|---|---|---|---|
| Forward flexion, deg ± SD | 115 ± 29 | 123 ± 40 | 0.67 |
| Abduction, deg ± SD | 106 ± 32 | 108 ± 50 | 0.94 |
| External rotaion, deg ± SD | 59 ± 22 | 39 ± 27 | 0.12 |
| Internal rotation (a) | 6 ± 4 | 6 ± 2 | 0.72 |
| SSV | 70 ± 20 | 81 ± 17 | 0.24 |
| Constant score | 47 ± 18 | 55 ± 22 | 0.45 |
| DASH score | 30 ± 21 | 32 ± 22 | 0.91 |
DASH - disabilities of the arm shoulder and hand, NSA – neck-shaft angle, SSV – subjective shoulder value.
Score is rated according to the constant score internal rotation criteria: lateral thigh-0, buttock-2, lumbosacral junction-4, L3 (waist)-6, T12–8, T7 (intrascapular)-10.
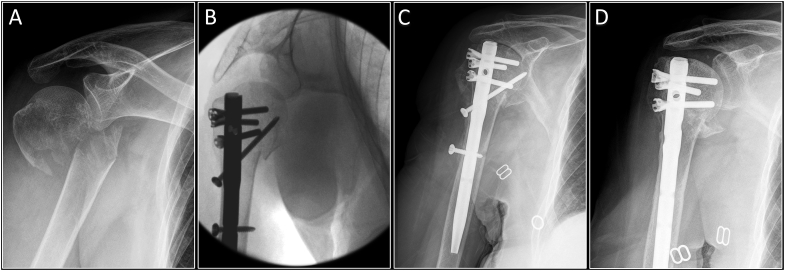
Fig. 1.
AP radiographs of a 64 years old woman who sustained a displaced 2 part surgical neck fracture after a simple mechanical fall. A – Preoperative radiographs showing valgus displacement. Although the patient is relatively young, she had a low deltoid tuberosity index of 1.33. B – Intraoperative radiographs showing adequate reduction. Neck shaft angle on radiograph taken on post-operative day 1 was measured to be 138°. C - 5 months post-operative radiograph showing severe varus collapse of the humeral head, with a neck shaft angle of 82°.
A univariate regression analysis of possible risk factors for secondary displacement (age, sex, DTI, diameter of nail, number of head screws and post-operative NSA), found that only the DTI had a statistically significant correlation with the degree of displacement (−0.41, p = 0.04).
3.1. Complications
There were no cases of nonunion or AVN. A total of 5 patients underwent reoperation: 4 patients (16%) had hardware removal, with one patient having contracture release for poor ROM at the same session of the hardware removal. One patient (4%) had suspected infection and underwent open debridement & lavage.
4. Discussion
The aim of the this study was to evaluate the rate of secondary displacement and malunion of patients treated with a proximal humerus nail for displaced 2 part surgical neck or metaphysis proximal humerus fracture in one medical institution. The main findings are: (1) a high rate of secondary fracture displacement during the early postoperative period; (2) fair clinical results, not associated with the secondary displacement; (3) a correlation between this displacement and the deltoid tuberosity index.
Secondary loss of proximal fixation is the most common complication after surgical treatment of proximal humerus fractures with locking plates16 or proximal humerus nail.8 The primary reason for this mechanism of failure is loss of impaction of the porous bone in the region of the surgical neck. Since the forces on the head screws are high while the proximal screw-bone-interface is weak after a surgical treatment, a collapse is likely to occur.17 This complication is a possible risk factor for poor clinical outcome16 and is more prevalent in elderly patients. This suggests osteopenia as an important predisposing factor for malunion and poor results after proximal humerus fracture fixation.
Older generations of PHN were notorious for their insufficient proximal fixation, leading to a high rate of malunions. Recent advancements in the design of PHN were made mostly to improve this issue by allowing an angular-stable construct, with varying mechanisms of locking the proximal fixation to the nail.9 Reported secondary loos of reduction rate for PHN is about 10%8 for all fracture types, but when examining 2 part fractures only, the reported rate is usually lower: Hatzidakis et al. reported only 2.6% loss of reduction (1 out of 38 patients, average age 65, using T2 nail by Stryker or EX spiral blade by Synthes) with a negligible change in NSA for the rest of the cohort18; Trepat et al. reported an average change in NSA of only 3° in 15 patients (age 64.5 ± 20.7, using T2 nail by stryker)19; and Zhu reported 0% loss of reduction, although on a younger population (0 out of 25 patients, age 54.8 ± 17.1, using PHN by Synthes).20
On the other hand, Nolan et al. reported the results of 12 patients and showed an average NSA varus collapse of 8° between surgery and last follow-up, with 33% ending up with a radiographic malunion (4 out of 12 patients, average age 71, using Polaris nail by Acumed).21 Our experience, which included an ever higher degree of fracture loss of reduction, suggests that this complication might be common, even when using the new generation of PHNs. However, most studies examining PHNs do not report radiographic outcomes apart for fracture union.22
The deltoid tuberosity index (DTI) was introduced lately as a possible simple and reliable measure of proximal humerus bone mineral density.14 In a subsequent article, Spross et al. have shown that the DTI is a significant pre-operative predictor for an acceptable reduction during surgery; and that age, DTI, and good reduction quality are independent factors predicting screw cutout after fixation with an angular stable proximal humerus plate.23 In this study the DTI was found to be correlated with the degree of displacement, adding evidence to its utility as a measure of bone quality.
It is also worth noting that of the four patients who underwent hardware removal, three were indicated for loose or penetrating screws (Fig. 2). These patients were older than average, and their DTIs were 1.22, 1.35 and 1.39 – all below the average in our series of 1.45. The fourth patient underwent hardware removal and contracture release due to poor range of motion.
Fig. 2.
AP radiographs of an 83 years old woman who sustained a displaced 2 part surgical neck fracture after a simple mechanical fall. A- Preoperative radiographs showing complete displacement. B - Intraoperative radiographs. C – Radiograph taken 2.5 months post-operative show concentric collapse of the humeral head causing screw penetration to the gleno-humeral joint, and a lateral migration of the distal locking screw. D – The patient underwent removal of the penetrating and distal screws. At the time of the latest follow-up, the patient demonstrated 90° of forward flexion and 45° of external rotation, and a subjective shoulder value of 60%.
In their systematic review of the Outcomes of intramedullary nailing for acute proximal humerus fractures, Wong et al. gave range of motion and functional outcomes subdivided by fracture type.8 Compared to the pooled results of two part fractures, ROM and functional outcomes in our cohort were acceptable, though somewhat inferior: forward flexion 121 (vs. 140), abduction 108 (vs. 154), external rotation 44 (vs. 45), and constant score 54 (vs. 74).
In previous studies, poor bone quality23 and loss of reduction16 was associated with poor results. In this study there was no significant deference in the clinical results of patients suffering from severe reduction loss and patients which did not had reduction loss. This could be the result of a type II error due to the small number of patients in this study.
The strength of this study is the homogeneity of the fracture type and treatment administered in the cohort. The limitations are its retrospective nature, and the cohort size which is insufficient to properly asses the risk factors for secondary displacement.
In conclusion, surgical treatment of displaced 2-part proximal humerus fractures using proximal humerus intramedullary nail was associated with fair clinical results but an unacceptable rate of secondary displacement. The deltoid tuberosity index was found to correlate with the degree of this secondary displacement, adding evidence to its utility as a measure of bone quality. In our department the use of PHNs was abandoned for the use of locked plates.
Funding
This study was not funded.
Declaration of competing interest
All authors declare that they have no conflict of interest.
References
- 1.Court-Brown C.M., Caesar B. Epidemiology of adult fractures: a review. Injury. 2006;37:691–697. doi: 10.1016/j.injury.2006.04.130. [DOI] [PubMed] [Google Scholar]
- 2.Palvanen M., Kannus P., Niemi S., Parkkari J. Update in the epidemiology of proximal humeral fractures. Clin Orthop Relat Res. 2006;442:87–92. doi: 10.1097/01.blo.0000194672.79634.78. [DOI] [PubMed] [Google Scholar]
- 3.Chu S.P., Kelsey J.L., Keegan T.H. Risk factors for proximal humerus fracture. Am J Epidemiol. 2004;160:360–367. doi: 10.1093/aje/kwh224. [DOI] [PubMed] [Google Scholar]
- 4.Court-Brown C.M., Garg A., McQueen M.M. The epidemiology of proximal humeral fractures. Acta Orthop Scand. 2001;72:365–371. doi: 10.1080/000164701753542023. [DOI] [PubMed] [Google Scholar]
- 5.Gaebler C., McQueen M.M., Court-Brown C.M. Minimally displaced proximal humeral fractures: epidemiology and outcome in 507 cases. Acta Orthop Scand. 2003;74:580–585. doi: 10.1080/00016470310017992. [DOI] [PubMed] [Google Scholar]
- 6.Handoll H.H., Ollivere B.J., Rollins K.E. Interventions for treating proximal humeral fractures in adults. Cochrane Database Syst Rev. 2012;12:CD000434. doi: 10.1002/14651858.CD000434.pub3. [DOI] [PubMed] [Google Scholar]
- 7.Bohsali K.I., Bois A.J., Wirth M.A. Fractures of the proximal humerus. In: Rockwood C.A., Matsen F.A., Wirth M.A., Lippitt S.B., Fehringer E.V., Sperling J.W., editors. Rockwood and Matsen's the Shouder. fifth ed. Elsevier; Philadelphia: 2017. pp. 197–200. [Google Scholar]
- 8.Wong J., Newman J.M., Gruson K.I. Outcomes of intramedulary nailing for acute proximal humerus fractures: a systematic review. J Orthop Traumatol. 2016;17:113–122. doi: 10.1007/s10195-015-0384-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dilisio M.F., Nowinski R.J., Hatzidakis A.M., Fehringer E.V. Intramedullary nailing of the proximal humerus: evolution, technique, and results. J Shoulder Elb Surg. 2016;25:e130–e138. doi: 10.1016/j.jse.2015.11.016. [DOI] [PubMed] [Google Scholar]
- 10.Gilbart M.K., Gerber C. Comparison of the subjective shoulder value and the Constant score. J Shoulder Elb Surg. 2007;16:717–721. doi: 10.1016/j.jse.2007.02.123. [DOI] [PubMed] [Google Scholar]
- 11.Constant C.R., Gerber C., Emery R.J., Søjbjerg J.O., Gohlke F., Boileau P. A review of the Constant score: modifications and guidelines for its use. J Shoulder Elb Surg. 2008;17:355–361. doi: 10.1016/j.jse.2007.06.022. [DOI] [PubMed] [Google Scholar]
- 12.Hudak P., Amadio P.C., Bombardier C., the Upper Extremity Collaborative Group Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder, and hand) Am J Ind Med. 1996;29:602–608. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 13.Beaton D.E., Wright J.G., Katz J.N., the Upper Extremity Collaborative Group Development of the QuickDASH: comparison of three item-reduction approaches. J Bone Jt Surg. 2005;87A:1038–1046. doi: 10.2106/JBJS.D.02060. [DOI] [PubMed] [Google Scholar]
- 14.Spross C., Kaestle N., Benninger E. Deltoid tuberosity index: a simple radiographic tool to assess local bone quality in proximal humerus fractures. Clin Orthop. 2015;473:3038–3045. doi: 10.1007/s11999-015-4322-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Beredjiklian P.K., Iannotti J.P., Norris T.R., Williams G.R. Operative treatment of malunion of a fracture of the proximal aspect of the humerus. J Bone Joint Surg Am. 1998;80(10):1484–1497. doi: 10.2106/00004623-199810000-00010. [DOI] [PubMed] [Google Scholar]
- 16.Ockert B., Siebenburger G., Kettler M., Braunstein V., Mutschler W. Long-term functional outcomes (median 10 years) after locked plating for displaced fractures of the proximal humerus. J Shoulder Elb Surg. 2014;23:1223–1231. doi: 10.1016/j.jse.2013.11.009. [DOI] [PubMed] [Google Scholar]
- 17.Helfen T., Siebenburger G., Mayer M., Bocker W., Ockert B., Haasters F. Operative treatment of 2-part surgical neck fractures of the proximal humerus (AO 11-A3) in the elderly: cement augmented locking plate PHILOSTM vs. proximal humerus nail MultiLoc. BMC Muscoskelet Disord. 2016;17:1–7. doi: 10.1186/s12891-016-1302-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hatzidakis A.M., Shevlin M.J., Fenton D., Everett D., Nowinski R.J., Fehringer E.V. Angular-stable locked intramedullary nailing of two part surgical neck fractures of the proximal humerus. A multicenter retrospective observational study. J Bone Joint Surg Am. 2011;93:2172–2179. doi: 10.2106/JBJS.J.00754. [DOI] [PubMed] [Google Scholar]
- 19.Trepat A.D., Popescu D., Fernandez-Valencia J.A., Cune J., Rios M., Prat S. Comparative study between locking plates versus proximal humeral nail for the treatment of 2-part proximal humeral fractures. Eur J Orthop Traumatol. 2012;22:373–379. [Google Scholar]
- 20.Zhu Y., Lu Y., Shen J., Zhang J., Jiang C. Locking intramedullary nails and locking plates in the treatment of two-part proximal humeral surgical neck fractures: a prospective randomized trial with a minimum of three years of follow-up. J Bone Joint Surg Am. 2011;93:159–168. doi: 10.2106/JBJS.J.00155. [DOI] [PubMed] [Google Scholar]
- 21.Nolan B.M., Kippe M.A., Wiater J.M., Nowinski G.P. Surgical treatment of displaced proximal humerus fractures with a short intramedullary nail. J Shoulder Elb Surg. 2011;20:1241–1247. doi: 10.1016/j.jse.2010.12.010. [DOI] [PubMed] [Google Scholar]
- 22.Congia S., Palmas A., Marongiu G., Capone A. Is antegrade nailing a proper option in 2- and 3-part proximal humeral fractures? Musculoskelet Surg. 2019 doi: 10.1007/s12306-019-00610-5. [DOI] [PubMed] [Google Scholar]
- 23.Spross C., Zeledon R., Zdravkovic V., Jost B. How bone quality may influence intraoperative and early postoperative problems after angular stable open reduction-internal fixation of proximal humeral fractures. J Shoulder Elb Surg. 2017;26:1566–1572. doi: 10.1016/j.jse.2017.02.026. [DOI] [PubMed] [Google Scholar]