Abstract
The technique of high tibial osteotomy (HTO) was traditionally documented for symptomatic medial tibiofemoral arthrosis associated with coronal plane malalignment in a stable knee., recently, more attention has been given to the treatment of coronal malalignment in lax knees with HTO with or without ligament reconstruction.
Patients with overwhelming pain, chronic ligament deficiency and coronal or sagittal deformity are generally easier to treat with HTO as compared to those who have mild pain and a proximal tibial deformity. The instability at the knee joint can be either in the coronal or sagittal plane or in both planes. Younger patients with chronic ACL deficiency, varus malalignment and advanced medial compartment arthritis, who present with pain and slight instability show satisfactory results with HTO.
Double-limb weight bearing anteroposterior view radiographs are used to plot mechanical leg axis (from the centre of the femoral head to the centre of the knee), anatomical axis (a line from the centre of the piriformis fossa to the centre of the knee joint and a line through the long axis of tibia) and weight bearing axis (line drawn from the centre of the femoral head to the centre of the ankle joint) and are used to plan HTO. A 3-dimensional pre-operative plan using CT and MRI is recently studied.
The decision to perform HTO alone or in combination with ligament reconstruction involves consideration of patient demographics, symptoms and ligaments involved. The most commonly used surgical techniques for high tibial osteotomy include lateral close wedge osteotomy, medial open wedge osteotomy and dome osteotomy. The post-operative rehabilitation depends on the rigidity of fixation.
Keywords: High tibial osteotomy, Instability, Medial open wedge osteotomy, Lateral closed wedge osteotomy
1. Introduction
The technique of high tibial osteotomy (HTO) was traditionally documented for symptomatic medial tibiofemoral arthrosis associated with coronal plane malalignment in a stable knee.1 Recently, medial open wedge osteotomies have become more popular as compared to lateral closed wedge osteotomies.2 Both these techniques aim to divert the load from the medial to the lateral compartment.
Initially, it was believed that varus thrust and instability were contraindications to the use of HTO.3,4 However, recently, more attention has been given to the treatment of coronal malalignment in lax knees with HTO with or without ligament reconstruction.5, 6, 7 More attention is placed on the correction of posterior tibial slope and correction of the sagittal balance of the knee.
Patients with overwhelming pain, chronic ligament deficiency and coronal or sagittal deformity are generally easier to treat with HTO as compared to those who have mild pain and a proximal tibial deformity.8
2. Instability of the knee joint
The knee is stabilized in the coronal and sagittal plane by primary and secondary mechanisms. Instability of the knee in the sagittal plane increases the load distribution over posteromedial part of the tibial plateau. This may eventually lead to injury to injury to the medial meniscus, especially the posterior horn. Medial meniscus injury increases the mechanical posterior tibial slope and increases anterior tibial translation. The vicious cycle thus formed culminates into advanced secondary osteoarthritis of the medial compartment.
2.1. Coronal instability
The instability in the coronal plane is assessed on full length scannogram from pelvis to ankle performed in a standing position. Medial joint space narrowing, lateral joint space opening or both are identified to assess coronal plane imbalance. The four major contributors to coronal instability are:
-
1.
Acl rupture-it causes internal rotation of the tibia and hence, medialisation of the weight bearing axis of the body.
-
2.
Medial meniscal injury-when partial meniscectomy is done with ACL reconstruction, the risk of osteoarthritis (OA) reaches 30%. With total meniscectomy, the risk increases to 60%.9
-
3.
Posterolateral corner injury- These structures prevent tibiofemoral external rotation and varus opening. The lateral collateral ligament is the most important of these structures.
-
4.
Constitutional varus deformity-increases medial compartment forces.
2.1. Sagittal instability
The instability in the sagittal plane is assessed on comparative lateral radiographs of both knees taken in 30° of flexion. The major contributors to sagittal instability are:
-
1.
ACL rupture-it causes more anterior tibial translation.
-
2.
Medial meniscal injury- The medial meniscus, posterior horn specifically, acts as a brake to decrease anterior tibial translation. With anterior tibial translation of 6 mm, 70% knees will show a meniscal or posteromedial corner injury. With translation of 10 mm or more, the incidence of meniscal or posteromedial corner injury reaches 90%.
-
3.
Posterior tibial slope (PTS) - it is calculated on lateral radiographs as the angle subtended by the line parallel to the mid-diaphysis of the tibia and the line parallel to the posterior inclination of the tibial plateau. The range of normal values is wide. Medially, 9–11° and laterally 6–8° is considered normal. Any value more than 13° is considered abnormal.10 The posterior tibial slope also depends on integrity of the medial meniscus and chondral surfaces. The anterior tibial translation increases with abnormal posterior tibial slope in both ACL intact and ACL injured knees.11
In a PCL deficient knee, an anterior opening tibial wedge osteotomy, which increases PTS, the posterior tibial sag reduces significantly. Medial opening wedge osteotomy has a tendency to increase PTS. A small change in the gap height of 1 mm has the ability to change the posterior slope by 2°.12
3. Clinical assessment of instability
Patients present with symptoms of acute or chronic instability like pain, swelling and giving way. There is difficulty in climbing up stairs up and down and difficulty in squatting. The Lysholm knee scoring scale can be used to score the severity of symptoms on initial visit and on follow up. The age of the patient, occupation, degree of physical activity and type of instability all play an important role in the decision making process. It is important to identify on history if the pain of the patient relates to arthritis.
Younger patients with chronic ACL deficiency, varus malalignment and advanced medial compartment arthritis, who present with pain and slight instability show satisfactory results with HTO.13 In patients with instability as the primary complaint with or without pain with medial unicompartmental osteoarthritis, the indication of ACL reconstruction can be extended by performing a valgus HTO.14,15
A thorough inspection of both knees in the standing posture will reveal effusion and coronal imbalance if any. Gait examination is to be done for signs of varus/valgus or recurvate thrusts. Tenderness over the medial joint line will indicate meniscal tear or arthritis. The presence of crepitations is an early sign of chondral damage. A precise assessment of the range of movement will reveal genu recurvatum or any fixed deformities. Tests for instability are to be performed, especially to identify lateral collateral and posterolateral corner injuries. Tibiofemoral subluxation if any, should be should be categorized as reducible or non-reducible.
4. Pre-operative planning
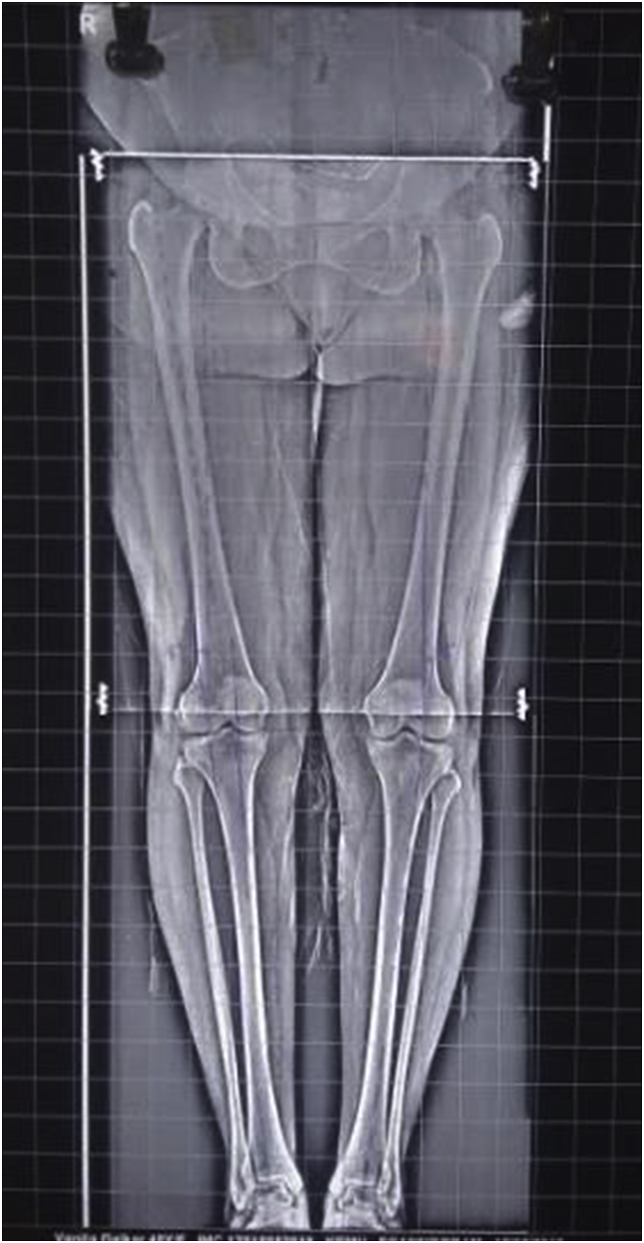
Double-limb weight bearing anteroposterior view radiographs (Fig. 1) are used to plot mechanical leg axis (from the centre of the femoral head to the centre of the knee), anatomical axis (a line from the centre of the piriformis fossa to the centre of the knee joint and a line through the long axis of tibia) and weight bearing axis (line drawn from the centre of the femoral head to the centre of the ankle joint) and are used to plan HTO.16 Normal values include a mechanical axis of up to 3° of varus, anatomical axis of 5–7° valgus, 6° of valgus between the mechanical and anatomical axes. The goal of valgus HTO is to reach 8–10° of valgus in the anatomical axis and 3–5° of valgus in the mechanical axis.
Fig. 1.
Double limb weight bearing anteroposterior radiograph.
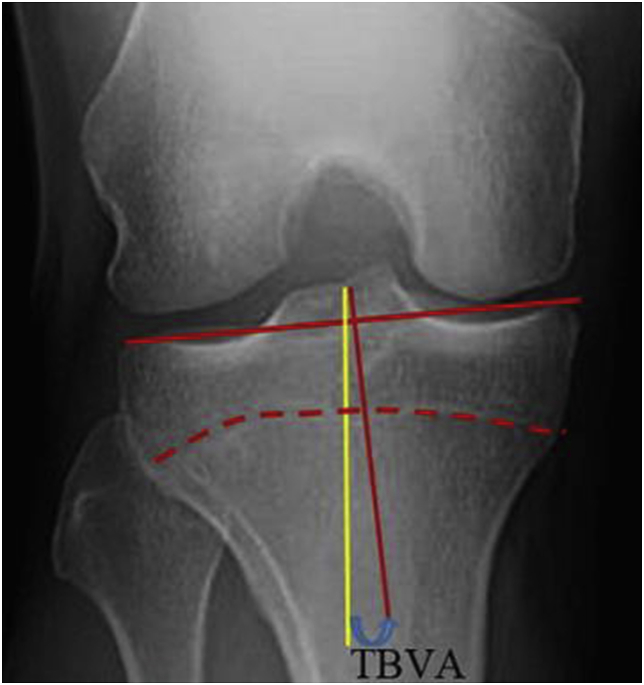
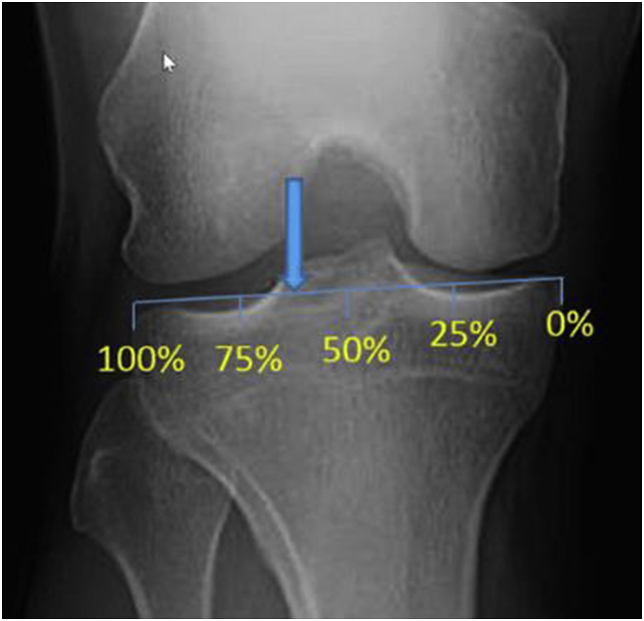
Stress views are mandatory when the clinical examination reveals ligamentous laxity. The tibia bone varus angle (TBVA) is measured on AP radiograph (Fig. 2). TBVA more than 5° is considered to be a good prognostic factor for HTO. Patella height and Insall-Salvati index are calculated on the lateral radiograph. It is essential to plot the Fujisawa point (Fig. 3) to determine the angle of correction required to restore the alignment.
Fig. 2.
Standard anteroposterior view of the knee showing TBVA.
Fig. 3.
Fujisawa point - located at 62% of the tibial plateau width when measured from the medial tibial plateau.
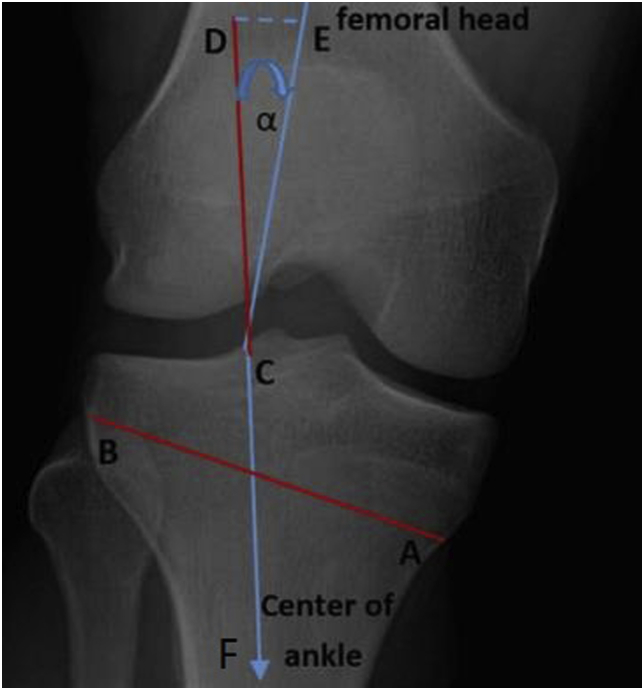
To determine the angle of correction (α), lines are drawn from the Fujisawa point to the centre of the femoral head and the centre of ankle (Fig. 4). The angle formed between these two lines is the amount of correction desired. A line AB is drawn from a point 4 cm below the medial joint line toward the fibular head. The base of the triangle formed as the wedge is equal in millimeters to the correction required in degrees.
Fig. 4.
Determination of the angle of correction (α) on a standard anteroposterior knee radiograph. Line CE is drawn from the Fujisa point to th femoral head. Line CF is drawn from the Fujisawa point to the centre of the ankle joint. Line AB is the the direction of the tibial cut.
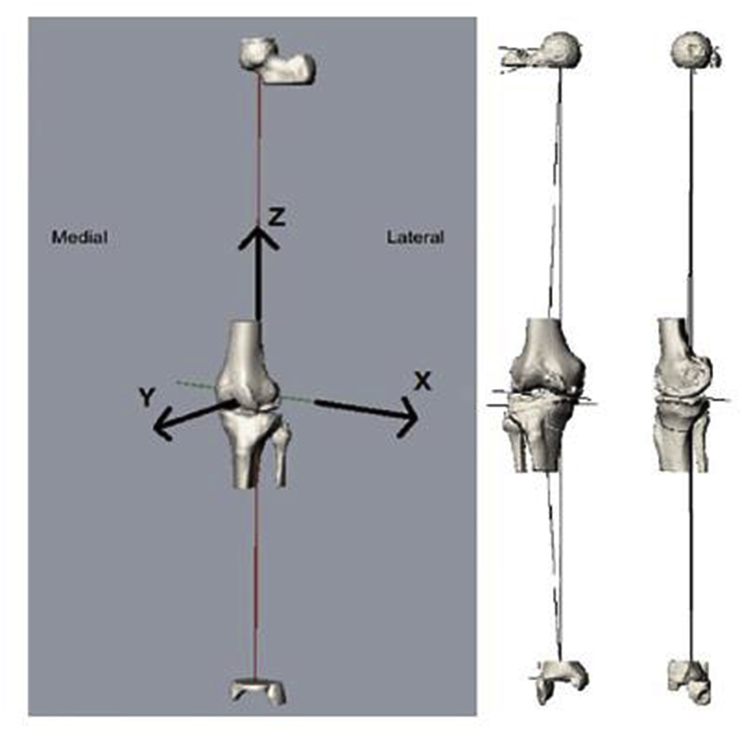
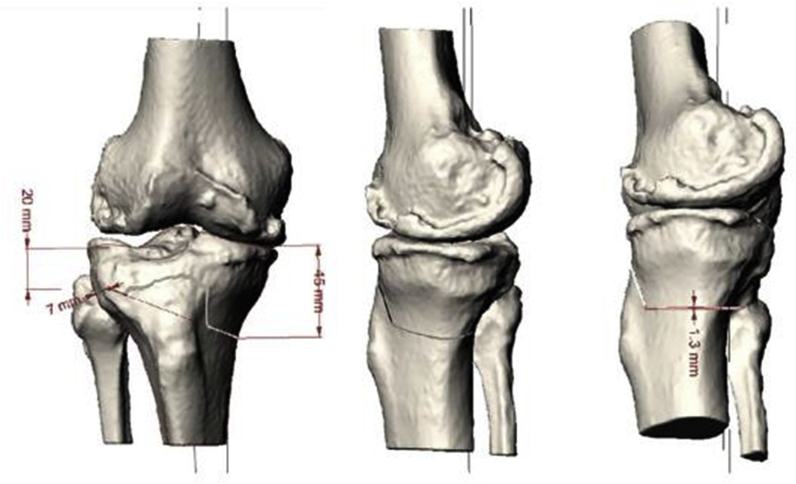
A 3-dimensional pre-operative plan using CT and MRI is recently studied. The pre-operative CT scans are segmented using commercially available software (Mimics; Materialize NV, Leuven, Belgium) to produce a 3D bone model (Fig. 5). The tibial mechanical axis is placed in the Z plane and the anatomical tibial axis in the X and Y planes. A 3D-HTO planning software, like the Grasshopper script for Rhino software (Robert McNeel and associates; Seattle, Washington), a virtual osteotomy cut can be created in the proximal tibia (Fig. 6). The starting point and the direction of the cut can be decided by surgeon preference. The desired correction in the coronal, sagittal and occasionally-axial planes can be achieved.
Fig. 5.
A CT scan derived bone model oriented in space according to established frames of reference
Fig. 6.
A virtual biplanar osteotomy cut made using a known saw blade thickness.
5. Surgical treatment
For deciding the surgical plan in patients with instability and varus malalignment, the alignment correction is critical and often precedes the soft tissue reconstruction. The broad treatment regimens include either performing HTO alone or in combination with delayed ligament reconstruction.
The decision to perform HTO alone or in combination with ligament reconstruction involves consideration of patient demographics, symptoms and ligaments involved. In case of chronic ACL deficiency, pain due to arthritis and varus malalignment, HTO alone may be sufficient for the management. If instability is the predominant symptom with varus malalignment, ACL reconstruction in combination with HTO may be performed to protect the graft and slow the progression to arthritis. If ACL and PCL both are injured, a correction of the posterior tibial slope may be required in addition to the correction of coronal plane deformity.
The most commonly used surgical techniques for high tibial osteotomy include lateral close wedge osteotomy, medial open wedge osteotomy and dome osteotomy.
5.1. Lateral close wedge osteotomy
The advantages of this technique include no need for bone grafting, less morbidity and faster healing and greater potential for correction.17, 18, 19
The disadvantages are concomitant fibular osteotomy or release of proximal tibiofibular joint, risk of peroneal nerve injury, loss of bone stock, limb shortening, ability to correct the deformity in only coronal plane and more difficult conversion to arthroplasty.20,21
5.2. Medial open wedge osteotomy
The advantages of this technique are the ability to correct the alignment in two planes (coronal and sagittal), no need for fibular osteotomy, little risk of peroneal nerve injury, no limb shortening, use of a single cut with no need of detaching muscles, no bone loss, easier conversion to arthroplasty, ability to adjust the amount of correction during surgery.
Disadvantages include the need for bone graft and the risk of delayed union or non-union. If more than 12.5 mm correction is required, concomitant tibial tuberosity osteotomy should be done to avoid adverse effects of patella baja and increased patellofemoral compartment pressure.
6. Methods of fixation
-
1.Plate fixation
-
a.Spacer plates. (e.g. Puddu plate and Aescula plate)
-
i.They require smaller incision but are less rigid.
-
ii.No weight bearing for 6 weeks.
-
i.
-
b.Plate fixators. (e.g. TomoFix)
-
i.Rigid fixation possible.
-
ii.Weight bearing can be started early.
-
i.
-
a.
-
2.Bone healing after HTO without any implant
-
a.Starts from the lateral hinge and gradually proceeds medially.
-
b.Callus formation is visible three months after surgery.
-
a.
-
3.Spacers for Medial Open Wedge HTO
-
a.Locking plate fixation and spacers made of bone graft or bone graft substitutes can be used.
-
a.
-
4.Autograft
-
a.Autogenous iliac crest bone graft can be used as an option in patients who are at risk of non-union such as obese patients and smokers.
-
a.
7. Surgical complications
The commonly recorded complications tend to be those observed from general orthopedic lower limb procedures like deep venous thrombosis, superficial wound infection and hematoma. The complications termed specific to high tibial osteotomy are rare. These include non-union requiring repeat osteotomy and bone grafting, common peroneal nerve palsy, knee stiffness, patella baja and intra-articular fracture. The most commonly reported specific complication of high tibial osteotomy is under-correction requiring revision surgery.
8. Post-operative management
The post-operative rehabilitation depends on the rigidity of fixation. When rigid fixation is achieved with plate fixators, immediate post-operative weight bearing with around 15 kg weight can be started while full weight bearing can be started after 2 weeks. When using spacer plates which are less rigid, weight bearing can be started after 6 weeks. A weight bearing full length lower limb anteroposterior radiogram is done at 2 months to confirm and document the change in the mechanical alignment of the lower limb and to ensure a healthy union (Fig. 7).
Fig. 7.
Weight bearing full length radiogram done 2 months post-surgery after starting weight bearing.
Declaration of competing interest
None of the authors have any financial or other conflicts of interest that may bias the current manuscript.
Contributor Information
Roshan Wade, Email: roshanwade@gmail.com.
Swapneel Shah, Email: shahswapneel@gmail.com.
B.S. Sujith, Email: sujith5791@gmail.com.
Kunal Shah, Email: kunalajitshah@gmail.com.
Aditya Raj, Email: adityagmck@gmail.com.
Nandan Marathe, Email: nandanmarathe88@gmail.com.
References
- 1.Lustig S., Scholes C.J., Costa A.J., Coolican M.J., Parker D.A. Different changes in slope between the medial and lateral tibial plateau after open-wedge high tibial osteotomy. Knee Surg Sport Traumatol Arthrosc. 2013;21:32–38. doi: 10.1007/s00167-012-2229-6. [DOI] [PubMed] [Google Scholar]
- 2.Giffin J.R., Shannon F.J. The role of the high tibial osteotomy in the unstable knee. Sports Med Arthrosc. 2007;15:23–31. doi: 10.1097/JSA.0b013e3180310a89. [DOI] [PubMed] [Google Scholar]
- 3.Coventry M.B. Osteotomy of the upper portion of the tibia for degenerative arthritis of the knee. A preliminary report. J Bone Jt Surg. 1965:984–990. 47-A. [PubMed] [Google Scholar]
- 4.Naudie D.D., Amendola A., Fowler P.J. Opening wedge high tibial osteotomy for symptomatic hyperextension-varus thrust. Am J Sports Med. 2004;32:60–70. doi: 10.1177/0363546503258907. [DOI] [PubMed] [Google Scholar]
- 5.Badhe N.P., Forster I.W. High tibial osteotomy in knee instability: the rationale of treatment and early results. Knee Surg Sport Traumatol Arthrosc. 2002;10:38–43. doi: 10.1007/s001670100244. [DOI] [PubMed] [Google Scholar]
- 6.Arthur A., LaPrade R.F., Agel J. Proximal tibial opening wedge osteotomy as the initial treatment for chronic posterolateral corner deficiency in the varus knee. A prospective clinical study. Am J Sports Med. 2007;35:1844–1850. doi: 10.1177/0363546507304717. [DOI] [PubMed] [Google Scholar]
- 7.Feucht M.J., Mauro C.S., Brucker P.U., Imhoff A.B., Hinterwimmer S. The role of the tibial slope in sustaining and treating anterior cruciate ligament injuries. Knee Surg Sport Traumatol Arthrosc. 2013;21:134–145. doi: 10.1007/s00167-012-1941-6. [DOI] [PubMed] [Google Scholar]
- 8.Bauer G.C., Insall J., Koshino T. Tibial osteotomy in gonarthrosis (osteoarthritis of the knee) J Bone Jt Surg. 1969:1545–1563. 51-A. [PubMed] [Google Scholar]
- 9.Neyret P., Donell S., Dejour D., DeJour H. Partial meniscectomy and anterior cruciate ligament rupture in soccer players. Am J Sports Med. 1993;21:455–460. doi: 10.1177/036354659302100322. [DOI] [PubMed] [Google Scholar]
- 10.Neyret P., Zuppi G., Ait S.I., Selmi T. Tibial deflexion osteotomy. Oper Tech Sport Med. 2000;8:61–66. [Google Scholar]
- 11.Bonnin M. Les Ruptures du Ligament Croise Anteriieur: Etude Clinique et Biomechanique. Lyon. Universite Claude Bernard; France: 1990. La Subluxation Tibiale Anterieure en Appui Mono- podal. [Google Scholar]
- 12.Noyes F.R., Goebel S.X., West J. Opening wedge tibial osteotomy: the 3-triangle method to correct axial alignment and tibial slope. Am J Sports Med. 2005;33:378–387. doi: 10.1177/0363546504269034. [DOI] [PubMed] [Google Scholar]
- 13.Lattermann C., Jakob R.P. High tibial osteotomy alone or combined with ligament reconstruction in anterior cruciate ligament-deficient knees. Knee Surg Sport Traumatol Arthrosc. 1996;4:32–38. doi: 10.1007/BF01565995. [DOI] [PubMed] [Google Scholar]
- 14.Bonin N., Ait S.I., Selmi T., Donell S.T., Dejour H., Neyret P. Anterior cruciate reconstruction combined with valgus upper tibial osteotomy: 12 years follow-up. The Knee. 2004;11:431–437. doi: 10.1016/j.knee.2004.02.001. [DOI] [PubMed] [Google Scholar]
- 15.Dejour H., Neyret P., Bonnin M. Instability and osteoarthritis. In: Fu F.H., Harner C.D., Vince K.G., editors. Knee Surgery. Lippincott Williams & Wilkins; Baltimore, Maryland: 1994. pp. 859–875. [Google Scholar]
- 16.Brouwer R.W., Raaij Van T.M., Bierma-Zeinstra S.M., Verhagen A.P., Jakma T.S., Verhaar J.A. Osteotomy for treating knee osteoarthritis. Cochrane Database Syst Rev. 2007;3 doi: 10.1002/14651858.CD004019.pub3. CD004019. [DOI] [PubMed] [Google Scholar]
- 17.Coventry M.B., Ilstrup D.M., Wallrichs S.L. Proximal tibial osteotomy. A critical long-term study of eighty-seven cases. J Bone Jt Surg. 1993;75(2):196–201. doi: 10.2106/00004623-199302000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Hernigou P., Medevielle D., Debeyre J., Goutallier D. Proximal tibial osteotomy for osteoarthritis with varus deformity. A ten to thirteen-year follow-up study. J Bone Jt Surg. 1987;69(3):332–354. [PubMed] [Google Scholar]
- 19.Coventry M.B. Upper tibial osteotomy for osteoarthritis. J Bone Jt Surg. 1985;67(7):1136–1140. [PubMed] [Google Scholar]
- 20.Engel G.M., Lippert F.G., 3rd Valgus tibial osteotomy: avoiding the pitfalls. Clin Orthop Relat Res. 1981;160:137–143. [PubMed] [Google Scholar]
- 21.Lobenhoffer P., Agneskirchner J.D. Improvements in surgical technique of valgus high tibial osteotomy. Knee Surg Sport Traumatol Arthrosc. 2003;11(3):132–138. doi: 10.1007/s00167-002-0334-7. [DOI] [PubMed] [Google Scholar]