Abstract
Objective
To retrospectively compare the efficacy of suprascapular nerve block (SSNB) versus interscalene block (ISB) for analgesia after arthroscopic rotator cuff repair (ARCR).
Methods
Ninety-seven patients who underwent ARCR were retrospectively divided into three groups. Group S comprised 33 patients who received SSNB, group I comprised 52 patients who received ISB, and group C comprised 12 patients who received a glenohumeral injection as a control. SSNB and ISB were performed with 20 ml of 0.375% ropivacaine before surgery, while glenohumeral injection was performed after surgery. The Visual analog scale (VAS) pain scores were recorded at 1,3, and 6 h and 1, 3, and 6 days postoperatively. The total number of additional analgesic administrations was also counted for 6 days postoperatively.
Results
Compared with group C, the VAS pain score was significantly lower in group S at 1 h and 6 days postoperatively, and in group I at 1 and 3 h postoperatively. There were no significant differences between groups S and I in the VAS pain scores, or the administration of additional analgesia. There were no major complications associated with SSNB or ISB.
Conclusion
There were no significant differences between SSNB and ISB in the duration of analgesia and the VAS pain scores after ARCR.
Keywords: Rotator cuff tear, Arthroscopic repair, Suprascapular nerve block, Interscalene block, Glenohumeral injection, Visual analog scale
1. Introduction
Arthroscopic rotator cuff repair (ARCR) can result in severe postoperative pain. Postoperative pain management is an important component of perioperative care, and inadequate analgesia may lead to stress and chronic pain syndromes. Postoperative analgesia is one of the keys to successful early rehabilitation and recovery. The approaches used to reduce pain after ARCR include opioid analgesia, nonopioid analgesia, cryotherapy, intralesional analgesia, suprascapular nerve block (SSNB), and interscalene block (ISB). ISB is one of the most effective regional blocks for shoulder surgery, but it can sometimes cause phrenic nerve palsy, resulting in hemidiaphragmatic paresis and other neurologic complications.1,2 Moreover, ISB is difficult to perform and is associated with higher complication rates when performed by less experienced anesthetists compared with experienced anesthetists.3 SSNB is effective in providing analgesia after arthroscopic shoulder surgery, and has been described as an alternative to ISB.4,5 Furthermore, SSNB is a simple, easily reproducible technique that can be performed by the surgeon, and complications are rare. The present study aimed to compare the efficacy of SSNB versus ISB in providing analgesia after ARCR.
2. Materials and methods
All procedures described in this study were approved by the institutional review board of our hospital. Ninety-seven patients who underwent ARCR were included. The average patient age was 66.6 years (range 41–83 years). Informed consent was obtained from all included patients. Rotator cuff tears were diagnosed using preoperative magnetic resonance imaging, and the size of the rotator cuff tear was confirmed at the time of arthroscopic surgery. The rotator cuff tear was small-sized in 43 patients, medium-sized in 37, and large or massive in 17. Intraoperatively, tears of the supraspinatus and/or infraspinatus and subscapularis tendon were repaired, with or without associated procedures on the biceps tendon and acromion. The indication for ARCR was a symptomatic full-thickness rotator cuff tear or a partial-thickness rotator cuff tear that had failed to respond to conservative therapy for a minimum of 3 months. All patients were divided into three groups; group S comprised 33 patients who received SSNB, group I comprised 52 patients who received ISB, and group C comprised 12 patients who received a glenohumeral injection as a control.
2.1. Anesthetic procedure
SSNB and ISB with 20 ml of 0.375% ropivacaine were performed preoperatively after general anesthesia, while glenohumeral injection was performed postoperatively. ISB was performed under ultrasound guidance by an anesthesiologist (Fig. 1), while SSNB was performed by the surgeon (T.F). In SSNB, the needle was placed medial to the convergence of the spine and clavicle (Neviaser portal) and advanced toward the coracoid process to a depth of about 3–4 cm in accordance with a previously reported method (Fig. 2).6
Fig. 1.
Ultrasound-guided interscalene block performed in a left shoulder by senior anesthesiologists.
Fig. 2.
Suprascapular nerve block performed based on specific anatomic landmarks in a left shoulder by a surgeon.
2.2. Assessment criteria
The primary outcome measure was the mean postoperative shoulder pain score assessed by the patient using the visual analog scale (VAS; 0 to 10). The VAS pain scores were recorded at 1, 3, and 6 h and 1, 3, and 6 days postoperatively. The number of additional analgesic administrations were also recorded for 6 days postoperatively. The total volume of intravenous patient-controlled analgesia (PCA) and total number of diclofenac suppositories (suppo) administered were recorded. Analgesic complications were also evaluated.
2.3. Statistical methods
The Shapiro Wilk test and Mann-Whitney U test were used in the statistical analysis. The Mann-Whitney U test was adopted to evaluate the inter-rater reliability for every group. P < .05 was considered statistically significant.
3. Results
Data from 97 patients who underwent ARCR from July 2017 to March 2018 were retrospectively analyzed. There were no patients whose SSNB or ISB was considered a failure (VAS pain score of 10), and so no patient was excluded from the analysis. The three groups significantly differed regarding patient characteristics such as height, weight, and operative time (Table 1).
Table 1.
Demographic characteristics of the suprascapular nerve block (SSNB), interscalene block (ISB), and glenohumeral injection (GHI) groups.
| SSNB | ISB | GHI | P value | |
|---|---|---|---|---|
| Age, yr | 66.6 ± 7.9 | 61.7 ± 11.6 | 67.6 ± 8.4 | 0.055 |
| Height, cm | 157.1 ± 8.1 | 163.2 ± 9.5 | 167.2 ± 5.9 | 0.008 |
| Weight, kg | 58.7 ± 10.8 | 66.2 ± 15.1 | 62.0 ± 8.5 | 0.049 |
| BMI | 23.7 ± 3.1 | 24.6 ± 4.0 | 23.3 ± 2.5 | 0.37 |
| Operative time, min | 151.2 ± 49.6 | 118.9 ± 42.1 | 106.3 ± 42.9 | 0.001 |
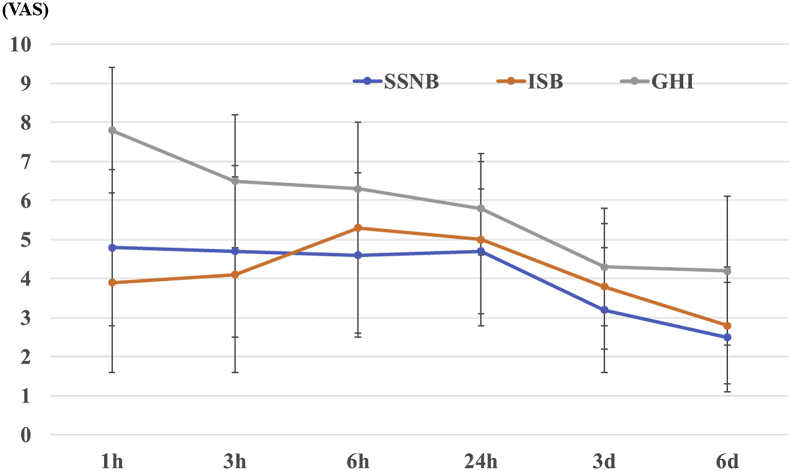
Compared with group C, the VAS pain score was significantly lower in group S at 1 h and 6 days postoperatively, and in group I at 1 and 3 h postoperatively. The VAS pain scores did not significantly differ between groups S and I (Fig. 3). Groups S and I also had a similar incidence of additional analgesic administration (Table 2). There were no complications associated with SSNB and glenohumeral injection. However, there were two complications (3.8%) in group I; one patient experienced transient phrenic nerve paralysis that lasted for a few hours and did not require treatment, while the other experienced ring and little finger numbness for more than 6 months.
Fig. 3.
Mean postoperative visual analog scale pain scores in the three groups. The pain scores did not significantly differ between the suprascapular nerve block (SSNB) and the interscalene block (ISB) group.
Table 2.
The total amount of intravenous patient-controlled analgesia (PCA) and total number of times that a diclofenac suppository (suppo) was administered in the suprascapular nerve block (SSNB), interscalene block (ISB), and glenohumeral injection (GHI) groups.
| SSNB | ISB | GHI | P value | |
|---|---|---|---|---|
| PCA, ml | 13.6 ± 3.1 | 13.2 ± 5.4 | 14.8 ± 4.6 | 0.128 |
| Suppo, times | 0.9 ± 1.0 | 1.5 ± 1.3 | 1.3 ± 1.2 | 0.195 |
4. Discussion
Controlling pain after ARCR is challenging. ARCR is considered one of the most painful arthroscopic shoulder surgeries, and so postoperative analgesia is important for successful early rehabilitation and recovery. Regional blocks such as ISB and SSNB have recently been approved for general use. Previous prospective studies report that SSNB is as effective as ISB for pain control for 6 days postoperatively.4,5 In the present study, there were no significant differences between groups S and I regarding the use of additional analgesia, the total amount of intravenous PCA, and the total number of diclofenac suppositories administered. ISB is an effective method,2,7 but it sometimes causes complications such as phrenic nerve palsy and pneumothorax.3 SSNB is widely used to achieve analgesia in arthroscopic shoulder surgery. The suprascapular nerve originates from the C5 and C6 nerve roots of the superior trunk of the brachial plexus, usually with a contribution from C4 as well.6 The suprascapular nerve supplies 70% of the sensory fibers to the glenohumeral joint, including the superior and posterior regions of the shoulder, capsule, acromioclavicular joint, subacromial bursa, and coracoacromial ligament, and directly innervates the supraspinatus and infraspinatus muscles.8 Compared with ISB, SSNB may be better for older adult patients with lung problems, and it may also be used by surgeons in cases when an ISB is not performed by the anesthesiologist. SSNB is easy to apply, takes very little time, and is a safe method with low complication rates. In fact, there were no complications in group S, while two complications occurred in group I.
A rebound effect in groups S and I resulted in increased pain at about 10 h postoperatively, similarly to a previous report.9 One study reported that ISB provided immediate effective analgesia until 6 h postoperatively, with significant rebound pain at 12 h postoperatively10; however, another study reported that the rebound effect was decreased by adding an ultrasonographically guided axillary nerve block to the SSNB.11 It is unclear whether this short duration of significant pain relief achieved by the ISB justifies the extra procedural time and additional skill required. However, ISB decreases pain for 20 h,12 and an axillary nerve block combined with SSNB is more effective than SSNB alone.8,11 Furthermore, combining an ISB with corticosteroid administration results in a longer duration of block analgesia.13,14 Continuous infusion through an indwelling brachial plexus catheter is reportedly useful; however, almost 30% of patients experience catheter failure, and the risk of phrenic nerve palsy and permanent neuropathy is higher than that after a single injection.15 Furthermore, it is unclear whether these subtle differences in pain control affect the long-term outcome. At our institution, corticosteroids are currently being administered in combination with the nerve block, which seems to result in a longer duration of analgesia; however, this needs to be confirmed in a further study. Comparing SSNB with ISB, there were no significant differences between groups S and I in the duration of analgesia and VAS pain score. However, SSNB had fewer adverse effects and an easier technique than ISB; thus, SSNB might be an effective and safe analgesic alternative to ISB for shoulder surgery, as previously reported.5
5. Limitations
The present study had some limitations. First, the mean operative time significantly differed between groups S and I. Second, PCA and diclofenac suppositories were used simultaneously a baseline in groups S and I, which probably introduced bias due to the effects of the PCA and suppositories on the nerve block. Third, the present study did not evaluate the long-term differences in functional outcome between groups. Fourth, the sample size was small.
6. Conclusion
The present retrospective clinical study found that SSNB is as effective as ISB in providing analgesia after ARCR.
Disclaimer
The authors, their immediate families, and any research foundations with which they are affiliated did not receive any financial payments or other benefits from any commercial entity related to the subject of this article.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
None.
References
- 1.Faryniarz D., Morelli C., Coleman S. Interscalene block anesthesia at an ambulatory surgery center performing predominantly regional anesthesia: a prospective study of one hundred thirty-three patients undergoing shoulder surgery. J Shoulder Elb Surg. 2006;15:686–690. doi: 10.1016/j.jse.2006.02.001. [DOI] [PubMed] [Google Scholar]
- 2.Singh A., Kelly C., O'Brien T. Ultrasound-guided interscalene block anesthesia for shoulder arthroscopy. J. Bone Joint Surg. Am. 2012;94:2040–2046. doi: 10.2106/JBJS.K.01418. [DOI] [PubMed] [Google Scholar]
- 3.Lenters T.R., Davies J., Matsen F.A. The types and severity of complications associated with interscalene brachial plexus block anesthesia: local and national evidence. J Shoulder Elb Surg. 2007;16:379–387. doi: 10.1016/j.jse.2006.10.007. [DOI] [PubMed] [Google Scholar]
- 4.Desroches A., Klouche S., Schlur C. Suprascapular nerve block versus interscalene block as analgesia after arthroscopic rotator cuff repair: a randomized controlled noninferiority trial. Arthroscopy. 2016;32:2203–2209. doi: 10.1016/j.arthro.2016.03.013. [DOI] [PubMed] [Google Scholar]
- 5.Hussain N., Goldar G., Ragina N. Suprascapular and interscalene nerve block for shoulder surgery. Anesthesiology. 2017;127:998–1013. doi: 10.1097/ALN.0000000000001894. [DOI] [PubMed] [Google Scholar]
- 6.Barber F.A. Suprascapular nerve block for shoulder arthroscopy. Arthroscopy. 2005;21:1015.e1–1015.e4. doi: 10.1016/j.arthro.2005.05.033. [DOI] [PubMed] [Google Scholar]
- 7.Bishop J.Y., Sprague M., Gelber J. Interscalene regional anesthesia for arthroscopic shoulder surgery: a safe and effective technique. J Shoulder Elb Surg. 2006;15:567–570. doi: 10.1016/j.jse.2006.01.009. [DOI] [PubMed] [Google Scholar]
- 8.Checcucci G., Allegra A., Bigazzi P. A new technique for regional anesthesia for arthroscopic shoulder surgery based on a suprascapular nerve block and an axillary nerve block: an evaluation of the first results. Arthroscopy. 2008;24:689–696. doi: 10.1016/j.arthro.2008.01.019. [DOI] [PubMed] [Google Scholar]
- 9.Oh J.H., Kim W.S., Kim J.Y. Continuous intralesional infusion combined with interscalene block was effective for postoperative analgesia after arthroscopic shoulder surgery. J Shoulder Elb Surg. 2007;16:295–299. doi: 10.1016/j.jse.2006.04.015. [DOI] [PubMed] [Google Scholar]
- 10.Kim J.H., Koh H.J., Kim D.K. Interscalene brachial plexus block versus patient-controlled interscalene indwelling catheter analgesia for the first 48 hours after arthroscopic rotator cuff repair. J Shoulder Elb Surg. 2018;27:1243–1250. doi: 10.1016/j.jse.2018.02.048. [DOI] [PubMed] [Google Scholar]
- 11.Lee J.J., Kim D.Y., Hwang J.T. Effect of ultrasonographically guided axillary nerve block combined with suprascapular nerve block in arthroscopic rotator cuff repair: a randomized controlled trial. Arthroscopy. 2014;30:906–914. doi: 10.1016/j.arthro.2014.03.014. [DOI] [PubMed] [Google Scholar]
- 12.Demarco J.R., Componovo R., Barfield W.R. Efficacy of augmenting a subacromial continuous-infusion pump with a preoperative interscalene block in outpatient arthroscopic shoulder surgery: a prospective, randomized, blinded, and placebo-controlled study. Arthroscopy. 2011;27:603–610. doi: 10.1016/j.arthro.2011.01.003. [DOI] [PubMed] [Google Scholar]
- 13.Watanabe K., Tokumine J., Yozozu T. Particulate-steroid betamethasone added to ropivacaine in interscalene brachial plexus block for arthroscopic rotator cuff repair improves postoperative analgesia. BMC Anesthesiol. 2016;16:84. doi: 10.1186/s12871-016-0251-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tandoc M.N., Fan L., Kolesnikov S. Adjuvant dexamethasone with bupivacaine prolongs the duration of interscalene block: a prospective randomized trial. J Anesth. 2011;25:704–709. doi: 10.1007/s00540-011-1180-x. [DOI] [PubMed] [Google Scholar]
- 15.Malik T., Mass D., Cohn S. Postoperative analgesia in a prolonged continuous interscalene block versus single-shot block in outpatient arthroscopic rotator cuff repair: a prospective randomized study. Arthroscopy. 2016;8:1544–1550. doi: 10.1016/j.arthro.2016.01.044. [DOI] [PubMed] [Google Scholar]