Abstract
Background
From a clinical perspective, it is important to understand the outcomes that occur after total hip arthroplasty (THA) and do these vary with surgical approach. The objective of the study was to compare physical performance-based and patient-report outcomes between the Direct Anterior (DA) and Direct Lateral (DL) surgical approach at one-year after THA surgery.
Methods
We evaluated patients attending their one-year follow-up assessment after primary elective unilateral THA surgery for osteoarthritis of the hip. The Activities-specific Balance Confidence Scale, Falls Risk in Older People in a Community Setting, Timed Up and Go Test, 30-Second Chair Stand Test, Step Test, 6-Meter Walk Test, Harris Hip Score (HHS), Short-form 12 and the Western Ontario and McMaster Osteoarthritis Index (WOMAC) were assessed. The standardized mean difference (SMD) and 95% confidence intervals (CI) was calculated to evaluate the statistical difference between groups and the magnitude of the effects.
Results
In total, 135 individuals met the inclusion criteria and participated in the study. A statistically significant and clinically important difference in favor of the DA was found for the WOMAC (0.60, 95% CI (0.25, 0.95), p = .004), SF-12 Physical component (0.42, 95% CI (0.07, 0.76), p = .01) and 6-Meter Walk Test (0.52, 95% CI (−0.86, −0.17), p = .009). Small effect sizes, though not statistically significant differences, were found in favor of the DA approach for the other patient-report and physical performance-based measures.
Conclusion
The WOMAC, gait speed and SF-12 Physical component scores were significantly different in favor of the DA procedure at one-year after THA. However, only the WOMAC scores exceeded a clinically important threshold in favor of DA approach. The other self-report and physical performance measures were not significantly different between the two procedures at one-year postoperatively.
Keywords: Total hip arthroplasty, Outcomes, Surgery, Functional tests
1. Introduction
Total hip arthroplasty (THA) can be regarded as one of the most successful orthopaedic surgical procedures for the treatment of end-stage hip osteoarthrits.1,2 A recent meta-analysis indicated that the lateral and anterior surgical approaches produced the best post-operative pain reduction outcomes and self-reported function scores after 4–6 weeks when compared with other approaches.3 The most recent systematic review that compared direct anterior (DA) and lateral (DL) approach found the Harris Hip Score (HHS) was similar between the groups at one-year following surgery.4
Functional activity after THA with DA versus other approaches has been analyzed in many studies during the early postoperative period and the results are variable. Several studies have reported advantages in functional activity after DA.5, 6, 7, 8 On the other hand, other studies found no differences between the DA and other surgical approaches regarding functional activity.9, 10, 11, 12 According to Barry et al.13 no studies have demonstrated activity advantages that extend beyond the initial 3 months after surgery. For patient-reported outcomes, significant advantages of the DA over the DL approach have been found at one-year follow-up after THA.2,14 More specifically, Ilchmann et al.14 demonstrated a significant improvement in SF-36 scores and the Western Ontario and McMaster Osteoarthritis Index (WOMAC) one-year after the THA, but the differences were not maintained at 2-years. Restrepo et al.2 found better HHS and patient satisfaction for the DA compared to the DL approach after one-year, but no difference after 2-years. In contrast, Amlie et al.15 found the WOMAC, quality of life and visual analog scale scores for pain and satisfaction were statistically significantly lower for the direct lateral approach up to 3 years after the surgery.
The Harris Hip Score, Western Ontario McMaster Osteoarthritis Index and health-related quality of life are the most commonly used outcomes. However, from a rehabilitation perspective it is important to understand both the functional and patient-reported outcomes between the DA and DL approach as this will provide a fuller understanding of recovery after THA. Therefore, the objective of this study was to compare physical performance-based and patient-reported outcomes between the DA and DL approach at one year after THA in a Canadian population. We hypothesized there would be no difference in functional and patient-reported outcomes one year after the operation between the DA and DL approach.
2. Methods
2.1. Study design
We conducted a cross-sectional study of patients attending their one-year follow-up appointment after THA. This study was conducted at a single centre with the patients of three high volume fellowship-trained arthroplasty surgeons. This study was approved by the Health Sciences Research Ethics Boards at the XXXX and by the Clinical Resources Impact Committee of XXX Research Institute.
2.2. Participants
Participants were eligible to participate if they were older than 50 years of age, had undergone a primary elective unilateral THA surgery for a diagnosis of OA of the hip in the previous 12 months, and were ambulatory for a minimum of 10 m without the assistance of another person (but with the allowance of a gait aid). Patients were excluded if they had surgery for a diagnosis other than OA and they were not ambulatory at the one-year follow-up appointment following THA.
2.3. Data collection
A research assistant who was trained to administer the patient-reported and performance-based tests collected all outcome measures. The following information was obtained by subjective interview: age, sex, height, surgical approach, current physical activity level, gait aid use and type of aid, number of prescription medications and comorbidities. The following tests were administered to the participants: Montreal Cognitive Assessment (MoCA), Activities-specific Balance Confidence Scale (ABC), Falls Risk in Older People in a Community Setting (FROP-com), Timed Up and Go Test (TUG), 30-Second Chair Stand Test, Step Test, 6-m Walk Test, Harris Hip Score (HHS), Short-Form 12 (SF-12) and the Western Ontario and McMaster Osteoarthritis Index (WOMAC).
2.4. Patient-reported outcomes
2.4.1. Harris Hip Score
The Harris Hip Score (HHS) is a clinician-based outcome that covers the 4 domains of pain, function, range of motion and absence of deformity.16 The overall score is a maximum of 100 points, which represents the best possible outcome. The grading of HHS can be reported as poor (<70), fair (70–79), good (80–89) or excellent (90–100).16
2.4.2. Western Ontario and McMaster Osteoarthritis Index
The Western Ontario and McMaster Osteoarthritic Index (WOMAC) assesses pain, joint function and stiffness.17 The tool is comprised of 24 questions divided into three domains: pain, stiffness and physical function. Our institution uses a weighted and inverted conversion such that there is a score out of 100 on each domain and higher scores indicate better overall health status.
2.4.3. Short Form-12
The Short Form-12 Survey (SF-12) is a 12-question self-report questionnaire used to assess a person's overall health-status. The assessment generates an individual score for each of mental and physical health subdomains, higher scores indicate better health.18
2.4.4. Activities-specific Balance Confidence Scale
Balance confidence was measured with the Activities-specific Balance Confidence Scale (ABC).19 The ABC is a 16-item self-report measure of a person's confidence in performing various activities of daily living without falling or experiencing a sense of unsteadiness. Each item is rated on a scale of 0–100%, with a score of 0 representing no confidence, while a score of 100 represents complete confidence. A summary score is calculated by adding responses on each item and dividing by the total number of items.
2.4.5. Falls Risk for Older People in a Community Setting
Future falls risk was assessed using the Falls Risk for Older People in a Community Setting (FROP-Com) questionnaire20; a multifactorial falls risk assessment consisting of 28 questions assessing 13 known falls risk factors. Individual responses to each question were summed to generate a total score used to determine falls risk. Scores of 0–10 indicate mild falls risk, whereas scores of 11–18 depict moderate risk and scores greater than 19 are designated high falls risk, warranting further action.
2.5. Performance-based tests
2.5.1. Timed Up and Go Test
The Timed Up-and-Go Test was used to assess functional mobility.21 Participants began seated in a standard chair (seat height of 45 cm from the floor) with arm rests. The participant was instructed to stand up, using the armrests as required, walk 3 m, walk around a pylon positioned on the floor and return to the chair in a seated position. Participants were timed to the nearest 100th of a second with a stopwatch from the examiner's command of “go” until the moment they returned to the seated position.
2.5.2. 30-Second Chair Stand Test
The 30-Second Chair Stand Test is a valid and reliable test of leg strength in older adults with lower limb OA.22 Participants began seated in a chair (seat height of 45 cm from the floor) with arms folded across the chest and feet planted firmly on the floor. Upon the examiner's instruction of “go” participants stood fully upright and then returned to the seated position as many times as possible in 30 s while keeping their arms folded.
2.5.3. Step Test
The Step Test was used to measure dynamic balance, requiring participants to weight shift into single leg stance.23 Participants were instructed to stand with feet parallel, approximately 10 cm apart, with a step measuring 15 cm in height placed 5 cm in front of them. Participants placed their entire foot on the step and then back to the floor as rapidly as possible over 15 s. Each leg was tested separately and the total number of times the foot was placed on the step for each leg was recorded.
2.5.4. 6-M Walk Test
The 6-m Walk Test was used to assess walking speed. Start and end points were marked 1-m before and after the test distance to avoid recording acceleration and deceleration. The participants were timed from the moment they moved forward from the 1-m line and the time was stopped when they crossed the 6-m line. Time was recorded to the nearest 100th of a second with a stopwatch.
2.6. Statistical analysis
Baseline characteristics and scores of patient-reported outcomes and performance-based tests were summarized per group (surgical approach) by using means, standard deviations (SD) or frequencies and percentages where it was appropriate. A 2-tailed independent t-test was used to compare the demographic and clinical characteristics between the 2 surgical groups (DA vs DL) to determine if the group differences were statistically significant, p-value was adjusted for multiple comparison using p < 0.005. For all outcomes, we calculated the standardized mean difference (SMD) and 95% confidence intervals (CI) to indicate the magnitude of the effects and we illustrated them into a forest plot. Benchmark values of effects sizes were used to indicate the magnitude of the effects (small<0.5, moderate = 0.5–0.79, large>0.8).24 A standard deviation of 0.5 units was deemed a clinically important difference.25 A post-hoc power analysis determined that a sample size of 135 had a statistical power of 0.81 (two-tailed hypothesis) to detect an effect size at the moderate level (d = 0.5). All analyses were performed with SPPS Statistics version 23 (IBM, Armonk, NJ).
3. Results
3.1. Demographics
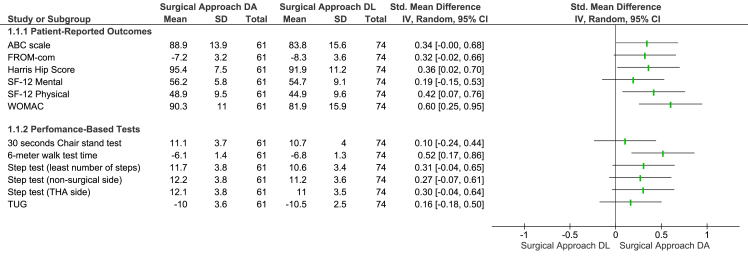
There were 305 individuals screened for the study and 135 met the inclusion criteria and participated in the study. Baseline demographic and clinical characteristics stratified by surgical approach are presented in Table 1. The average age for the DA and DL group was 68.4 ± 9.0 and 69.4 ± 9.2 years, respectively. In the DA group, 41% reported their physical activity as vigorous, 30% as moderate and 10% as seldom; while in the DL group, 43% reported their physical activity as vigorous, 35% as moderate and 22% as seldom. A mobility aid was used by 11% and 24% for the DA and DL group, respectively. The differences in patient-reported outcomes and physical performance-based tests are summarized in Table 2 and the effect sizes between the two surgical groups are illustrated in Fig. 1.
Table 1.
Demographic and clinical characteristics for a sample of adults one year after a unilateral total hip arthroplasty for osteoarthritis. (n = 135).
| Characteristic | Mean ± SD or Frequency (%) |
p value | |
|---|---|---|---|
| Direct Anterior Surgical Approach (n = 61) | Direct Lateral Surgical Approach (n = 74) | ||
| Age (years) | 68.4 ± 8.99 | 69.4 ± 9.18 | .51 |
| Sex (females) | 31 (50%) | 44 (59%) | .22 |
| Body Mass Index (kg/m2) | 27.4 ± 3.6 | 30.6 ± 5.7 | <.001* |
| Surgical side (Left) | 27 (44%) | 37 (50%) | .60 |
| Montreal Cognitive Assessment | 26.5 ± 2.67 | 26.3 ± 2.7 | .29* |
| Activities-specific Balance Confidence Scale | 88.9 ± 13.99 | 83.8 ± 15.62 | .052 |
| Number of Prescribed medications | 2.7 ± 2.9 | 3.4 ± 3.4 | .24 |
| Number of Comorbidities | 3.3 ± 2 | 4 ± 1.9 | .46* |
| Physical Activity: | |||
| Vigorous | 25 (41%) | 32 (43%) | |
| Moderate | 30 (49%) | 26 (35%) | |
| Seldom | 6 (10%) | 16 (22%) | .001* |
| Mobility Aid (Yes) | 7 (11%) | 18 (24%) | .001* |
| Type of Mobility: | |||
| Cane | 4 (7%) | 16 (22%) | .001* |
| Walker | 3 (5%) | 2 (3%) | |
| Mobility Aid Use: | |||
| Intermittent | 5 (8%) | 12 (16%) | .001* |
| All the time | 2 (3%) | 6 (8%) | .001* |
Table 2.
Patient-reported outcomes and physical performance-based tests compared between the direct anterior and direct lateral surgical approach for people one year after THA surgery. (n = 135).
| Outcome | Direct Anterior Procedure Mean (SD) | Direct Lateral Procedure Mean (SD) | p value | Effect Size SMD (95% CI) |
|---|---|---|---|---|
| Patient-Reported Outcomes | ||||
| Activities-specific Balance Confidence scale | 88.9 (13.9) | 83.8 (15.6) | .052 | 0.34 (−0.00, 0.68) |
| FROP-com | 7.2 (3.2) | 8.3 (3.6) | .055 | 0.32 (−0.02, 0.66) |
| Harris Hip Score | 95.4 (7.5) | 91.9 (11.2) | .05* | 0.36 (0.02, 0.70) |
| SF-12 Mental | 56.2 (5.8) | 54.7 (9.1) | .29 | 0.19 (−0.15, 0.53) |
| SF-12 Physical | 48.9 (9.5) | 44.9 (9.6) | .01* | 0.42 (0.07, 0.76) |
| WOMAC | 90.3 (11) | 81.9 (15.9) | .001* | 0.60 (0.25, 0.95) ** |
| Performance-Based Tests | ||||
| 30-s Chair Stand Test (repetitions) | 11.1 (3.7) | 10.7 (4) | .49 | 0.10 (−0.24, 0.44) |
| 6-m Walk Test (seconds) | 6.1 (1.4) | 6.8 (1.3) | .009* | 0.52 (0.17, 0.86)** |
| Step test (side with the least number of steps) | 11.7 (3.8) | 10.6 (3.4) | .09 | 0.31 (−0.04, 0.65) |
| Step test (non-surgical side) | 12.2 (3.8) | 11.2 (3.6) | .15 | 0.27 (−0.07, 0.61) |
| Step test (THA side) | 12.1 (3.8) | 11 (3.5) | .11 | 0.30 (−0.04, 0.64) |
| Timed Up and Go Test (seconds) | 10 (3.6) | 10.5 (2.5) | .38 | 0.16 (−0.18, 0.50) |
Note: SD, standard deviation; SMD, standardized mean difference; FROP-Com, Falls Risk for Older People in a Community Setting; WOMAC, Western Ontario McMaster Osteoarthritis Index; THA, total hip arthroplasty; Benchmark values of effects sizes were used to indicate the magnitude of the effects (small<0.5, moderate = 0.5–0.79, large>0.8)24; *, statistical significant difference; **, effect size is set as clinically important if the SMD>0.5; positive values for the SMD indicate the difference between the direct anterior and direct lateral procedures is in favor of the direct anterior.
Fig. 1.
Forest plot comparing functional and performance-based tests between the 2 surgical approaches of direct lateral (DL) and direct anterior (DA).
3.2. Patient-reported outcomes
The WOMAC demonstrated a statistically significant difference (p = .004) and a clinically important difference in favor of DA approach with a moderate SMD 0.60, 95%CI (0.25, 0.95) (Fig. 1). The SF-12 Physical component score also demonstrated a statistically significant difference (p = .01), though not a clinically important difference, in favor of DA approach with a small effect size of 0.42, (0.07, 0.76). Additionally, the Harris Hip Score (HHS) had a statistically significant difference (p = .05), but not a clinically important difference, in favor of the DA approach and a small effect size of 0.36, 95% CI (0.02, 0.70).
We found no statistically significant (p = .052) or clinically important difference for the ABC scale scores, though there was a small effect size of 0.34, 95% CI (−0.00, 0.68) in favor of DA approach. Additionally, we found no statistically significant (p = .055) or clinically important differences for the FROP-com while again there was a small effect size of 0.32, 95% CI (−0.66, 0.02) in favor of the DA approach. The SF-12 Mental scores were not statistically significantly different (p = .29) or had a clinically important difference, though a small effect size of 0.19, 95% CI (−0.15, 0.53) was found in favor of DA approach.
3.3. Performance-based tests
The 6-m Walk Test demonstrated a statistically significant (p = .009) and a clinically important difference with a moderate effect size (0.52, 95% CI (−0.86, −0.17)) in favor of DA approach (Fig. 1). There was no statistically significant or clinically important difference for 30-Seconds Chair Stand Test (p = .49), Step Test for least number of steps (p = .09), Step Test for non-surgical side (p = .15), Step Test for the THA side (p = .11), or the Timed Up & Go Test (p = .38). There were small effect sizes for these non-significant outcome measures in favor of the DA approach.
4. Discussion
This study found that the DA approach resulted in statistically significant better patient-reported outcomes for the Harris Hip Score, Western Ontario McMaster Osteoarthritis Index and the SF-12 quality of life physical component. However, only the WOMAC scores were found to exceed the clinically important threshold in favor of the DA approach. The DA approach also resulted in statistically significant better gait speed. Our analysis indicated that the gait speed differences that were in favor of the DA approach one-year after the THA exceeded the predefined clinically important difference. We did not detect a statistically significant or clinically important difference for the remainder of the performance-based tests and patient-reported outcomes between the two surgical approaches.
For performance-based tests, we detected no statistically significant differences for the majority of the tests. Previous studies2,14 that compared the two surgical approaches (DA vs. DL) at one-year after THA found significantly better patient-reported outcomes (HHS,2,14 WOMAC14 and SF-3614) for the DA approach. Our results are in the same direction with the three previous studies2,14,15 for patient-reported outcomes, however, the previous studies did not clearly indicate the magnitude of the effects. Additionally, there was a lack of clarity in these previous studies for whether the surgeons were more familiar with either of surgical approaches. It has been described in the literature that a surgeon performing a surgical procedure for which they have greater experience may lead to superior outcomes and this factor was not controlled in either study.26
Another source of differences of our study with existing research in patient-reported outcomes could be due to different factors affecting patient characteristics, timing of surgery since onset of OA symptoms, wait times to have the surgery once determined an appropriate treatment intervention, and pre- and post-operative management. The majority of functional gains after THA surgery are usually achieved by 6 months.27 At this point individuals should have regained a higher level of functioning compared to the immediate post-operative phase and potentially more than their pre-operative functional level.28 Despite the advantages of the DA approach at one-year after THA, the differences in functional outcomes between the two surgical approaches in longer term follow-ups may be negligible or of uncertain clinical importance.14 An additional limitation was that we were unable to control for pre-operative functional status.
The strengths of this study are that we evaluated patient-reported outcomes and performance-based tests between the two surgical approaches and we performed a head-to-head comparison by indicating the magnitudes, the directions of the effects and clinically important differences, and is the only paper to do so. We had adequate power to be confident in our clinically important estimates in favor of DA group for the WOMAC scores and we indicated that the DA approach may produce better gait speed one year after surgery. The main limitation of our study is that it was a cross-sectional design therefore, we were unable to minimize potential systematic error. We also evaluated the functional and performance-based tests in a Canadian population and the results may not be presentative of all people receiving a THA and possibly will vary across populations.
5. Conclusion
The WOMAC, gait speed and SF-12 physical component scores were significantly different in favor of the DA procedure at one-year after THA. The other self-report and physical performance measures were not significantly different between the two procedures at one-year after surgery.
Declaration of competing interest
The authors have none to report.
References
- 1.Berger R.A., Jacobs J.J., Meneghini R.M., Della Valle C., Paprosky W., Rosenberg A.G. Rapid rehabilitation and recovery with minimally invasive total hip arthroplasty. Clin Orthop Relat Res. 2004 doi: 10.1097/01.blo.0000150127.80647.80. [DOI] [PubMed] [Google Scholar]
- 2.Restrepo C., Parvizi J., Pour A.E., Hozack W.J. Prospective randomized study of two surgical approaches for total hip arthroplasty. J Arthroplast. 2010 doi: 10.1016/j.arth.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 3.Putananon C., Tuchinda H., Arirachakaran A., Wongsak S., Narinsorasak T., Kongtharvonskul J. Comparison of direct anterior, lateral, posterior and posterior-2 approaches in total hip arthroplasty: network meta-analysis. Eur J Orthop Surg Traumatol. 2018;28(2):255–267. doi: 10.1007/s00590-017-2046-1. [DOI] [PubMed] [Google Scholar]
- 4.Yue C., Kang P., Pei F. Comparison of direct anterior and lateral approaches in total hip arthroplasty. Medicine (Baltim) 2015;94(50):e2126. doi: 10.1097/MD.0000000000002126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Taunton M.J., Trousdale R.T., Sierra R.J., Kaufman K., Pagnano M.W. John charnley award: randomized clinical trial of direct anterior and miniposterior approach THA: which provides better functional recovery? Clin Orthop Relat Res. 2018 doi: 10.1007/s11999.0000000000000112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nakata K., Nishikawa M., Yamamoto K., Hirota S., Yoshikawa H. A clinical comparative study of the direct anterior with mini-posterior approach: two consecutive series. J Arthroplast. 2009 doi: 10.1016/j.arth.2008.04.012. [DOI] [PubMed] [Google Scholar]
- 7.Rodriguez J.A., Deshmukh A.J., Rathod P.A. Does the direct anterior approach in THA offer faster rehabilitation and comparable safety to the posterior approach? Clin Orthop Relat Res. 2014 doi: 10.1007/s11999-013-3231-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barrett W.P., Turner S.E., Leopold J.P. Prospective randomized study of direct anterior vs postero-lateral approach for total hip arthroplasty. J Arthroplast. 2013;28(9):1634–1638. doi: 10.1016/j.arth.2013.01.034. [DOI] [PubMed] [Google Scholar]
- 9.Engdal M., Foss O.A., Taraldsen K., Husby V.S., Winther S.B. Daily physical activity in total hip arthroplasty patients undergoing different surgical approaches: a cohort study. Am J Phys Med Rehabil. 2017 doi: 10.1097/PHM.0000000000000657. [DOI] [PubMed] [Google Scholar]
- 10.Poehling-Monaghan K.L., Kamath A.F., Taunton M.J., Pagnano M.W. Direct anterior versus miniposterior THA with the same advanced perioperative protocols: surprising early clinical results. Clin Orthop Relat Res. 2014 doi: 10.1007/s11999-014-3827-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Taunton M.J., Mason J.B., Odum S.M., Springer B.D. Direct anterior total hip arthroplasty yields more rapid voluntary cessation of all walking aids: a prospective, randomized clinical trial. J Arthroplast. 2014 doi: 10.1016/j.arth.2014.03.051. [DOI] [PubMed] [Google Scholar]
- 12.Christensen C.P., Jacobs C.A. Comparison of patient function during the first six weeks after direct anterior or posterior total hip arthroplasty (THA): a randomized study. J Arthroplast. 2015;30(9):94–97. doi: 10.1016/j.arth.2014.12.038. [DOI] [PubMed] [Google Scholar]
- 13.Barry J.J., Masonis J.L., Mason J.B. Recovery and outcomes of direct anterior approach total hip arthroplasty. Ann Jt. 2018;3 51–51. [Google Scholar]
- 14.Ilchmann T., Gersbach S., Zwicky L., Clauss M. Standard transgluteal versus minimal invasive anterior approach in hip arthroplasty: a prospective, consecutive cohort study. Orthop Rev. 2013;5(4):31. doi: 10.4081/or.2013.e31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Amlie E., Havelin L.I., Furnes O. Worse patient-reported outcome after lateral approach than after anterior and posterolateral approach in primary hip arthroplasty A cross-sectional questionnaire study of 1,476 patients 1-3 years after surgery. Acta Orthop. 2014;85(5):463–469. doi: 10.3109/17453674.2014.934183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harris W.H. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. J Bone Jt Surg Am. 1969;51(4):737–755. [PubMed] [Google Scholar]
- 17.McConnell S., Kolopack P., Davis A.M. The western Ontario and McMaster universities osteoarthritis Index (WOMAC): a review of its utility and measurement properties. Arthritis Rheum. 2001;45(5):453–461. doi: 10.1002/1529-0131(200110)45:5<453::aid-art365>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 18.Cheak-Zamora N.C., Wyrwich K.W., McBride T.D., Wyrich K.W., McBride T.D. Reliability and validity of the SF-12v2 in the medical expenditure panel survey. Qual Life Res. 2009;18(6):727–735. doi: 10.1007/s11136-009-9483-1. [DOI] [PubMed] [Google Scholar]
- 19.Miller W.C., Deathe A.B., Speechley M. Psychometric properties of the activities-specific balance confidence scale among individuals with a lower-limb amputation. Arch Phys Med Rehabil. 2003;84(5) doi: 10.1016/s0003-9993(02)04807-4. as0003999303048074. [DOI] [PubMed] [Google Scholar]
- 20.Russell M.A., Hill K.D., Blackberry I., Day L.M., Dharmage S.C. The reliability and predictive accuracy of the falls risk for older people in the community assessment (FROP-Com) tool. Age Ageing. 2008 doi: 10.1093/ageing/afn129. [DOI] [PubMed] [Google Scholar]
- 21.Podsiadlo D., Richardson S. The Timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142–148. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- 22.Jones C.J., Rikli R.E., Beam W.C. A 30-s chair-stand test as a measure of lower body strength in community-residing older adults. Res Q Exerc Sport. 1999;70(2):113–119. doi: 10.1080/02701367.1999.10608028. [DOI] [PubMed] [Google Scholar]
- 23.Hill K.D., Bernhardt J., McGann A., Maltese D., Berkovits D. A new test of dynamic standing balance for stroke patients: reliability, validity, and comparison with healthy elderly. Physiother Can. 1996;48:257–262. [Google Scholar]
- 24.Cohen J. Statistical power analysis for the behavioral sciences. Stat Power Anal Behav Sci. 1988 [Google Scholar]
- 25.Norman G.R., Sloan J.A., Wyrwich K.W. The truly remarkable universality of half a standard deviation: confirmation through another look. Expert Rev Pharmacoecon Outcomes Res. 2004 doi: 10.1586/14737167.4.5.581. [DOI] [PubMed] [Google Scholar]
- 26.Sadideen H., Alvand A., Saadeddin M., Kneebone R. Surgical experts: born or made? Int J Surg. 2013;11(9):773–778. doi: 10.1016/j.ijsu.2013.07.001. [DOI] [PubMed] [Google Scholar]
- 27.Brander V., Stulberg S. Rehabilitation after hip and knee-joint replacement: an experience- and evidence-based approach to care. Am J Phys Med Rehabil. 2006;85(11):S98–S118. doi: 10.1097/01.phm.0000245569.70723.9d. [DOI] [PubMed] [Google Scholar]
- 28.Sicard-Rosenbaum L., Light K.E., Behrman A.L. Gait, lower extremity strength, and self-assessed mobility after hip arthroplasty. Journals Gerontol - Ser A Biol Sci Med Sci. 2002 doi: 10.1093/gerona/57.1.m47. [DOI] [PubMed] [Google Scholar]