Abstract
Background
Arthroscopic suprascapular nerve release has yielded good results previously. However, comprehensive literature is still lacking.
Purpose
This study assessed results of suprascapular nerve release in patients with intractable shoulder pain with confirmed suprascapular neuropathy.
Methods
Retrospectively reviewed patients undergoing suprascapular nerve release. Patients were evaluated with VAS scores and supraspinatus/infraspinatus strength.
Results
112 patients were included showing reduction in VAS pain scores from the initial visit to final follow up. Additionally, improvement in both supra/infraspinatus strength occurred. There were no major complications.
Conclusion
This series demonstrates improvement in pain and strength following suprascapular nerve release with limited risk.
Level of evidence
IV.
Keywords: Suprascapular nerve decompression, Suprascapular neuropathy, Transverse scapular ligament, Outcomes, Chronic shoulder pain
1. Introduction
Once viewed as a diagnosis of exclusion, suprascapular neuropathy is becoming a progressively accepted cause of chronic shoulder pain. The diagnosis is generally made clinically with the presence of persistent posterior shoulder pain in addition to weakness of the supraspinatus and infraspinatus muscles. Electromyography and nerve conduction studies, in the setting of positive exam findings, can be helpful in confirming the diagnosis. The true incidence and prevalence is unknown but estimated to be around 4% of all comers to a shoulder referral practice and 43% in patients suspected of having the diagnosis, including overhead athletes and patients with massive rotator cuff tears.6,19,22
Originally, decompression was performed with an open approach with acceptable results.2 Recently, Lafosse et al. pioneered arthroscopic suprascapular release, and has shown excellent results in 10 patients with improved constant scores and normalization of nerve conduction latency.18 In a similar series, Shah et al. again reported a decrease in VAS scores and improvement in ASES scores in 27 patients.26 Outside of these two studies there have been no larger reports analyzing arthroscopic decompression of the nerve at the suprascapular notch.
The goal of this study was to present the results of a larger single surgeon series of arthroscopic suprascapular nerve decompressions at the suprascapular notch in patients with and without reparable rotator cuff tears. Our goal was to analyze the outcomes and complications of this treatment method in a fairly heterogeneous patient population with shoulder pain thereby laying the ground work for future prospective studies.
2. Materials and methods
Institutional review board approval was granted in February 2018. Following this, a retrospective review of prospectively collected data was performed from the electronic medical record of patients who underwent arthroscopic suprascapular nerve release between November 2013 to November 2014 (184 patients). Patients were identified according to current procedural terminology (CPT) code. Patients were included if they had a preoperative history and follow-up notes to document comorbidities as well as visual analog spectrum (VAS) pain scores. Patients were asked to quantify their VAS pain scores as 0 (no pain) to 10 (excruciating pain) according to their level of shoulder pain. Supraspinatus and infraspinatus strength was documented by the senior author at pre and post-operative visits on the manual muscle test scale of 0–5 (5: antigravity + maximal resistance, 4: antigravity + moderate resistance, 3: antigravity alone, 2: movement with gravity eliminated, 1: trace movement, 0: no movement). All patients also underwent preoperative electromyography and nerve conduction studies (EMG/NCS) to document the presence of a suprascapular neuropathy as well as a magnetic resonance imaging (MRI) to document any concomitant pathology. Patients were excluded if they were <18 yrs age, lacked a diagnosis of SSN on EMG/NCS, had an incomplete medical record, or had a concomitant diagnosis of brachial plexopathy, thoracic outlet syndrome or long thoracic nerve dysfunction (72 patients).
2.1. Non-operative management
All patients underwent initial non-operative management consisting of non-steroidal anti-inflammatory medications, physical therapy and diagnostic/therapeutic suprascapular notch injections in the office setting. Patients were scheduled for surgery on the basis of a positive EMG/NCS study and relief of shoulder pain and improved supraspinatus/infraspinatus muscle function with a suprascapular nerve block having failed at least 6 weeks of conservative therapy as defined by unmanageable pain.
2.2. Surgical management
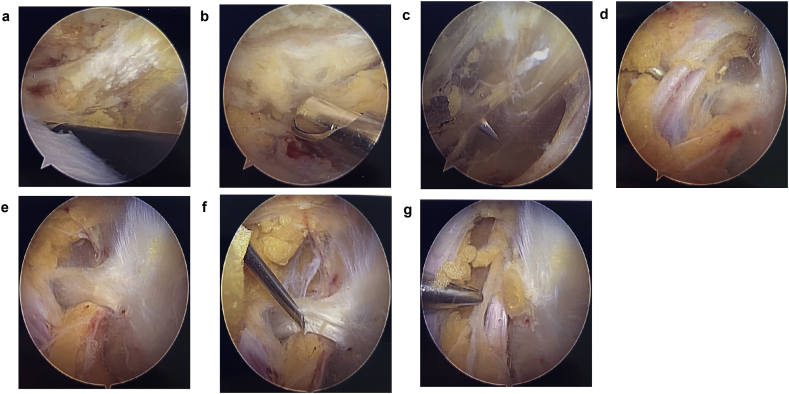
All patients were positioned in the lateral decubitus position. A posterior portal was established, and standard diagnostic arthroscopy performed. The arthroscope was then placed in the subacromial space and a subacromial decompression (if abnormal acromial morphology present) in addition to a bursectomy were performed using the radiofrequency ablator. The AC ligament is identified and followed down to identify the coracoclavicular ligaments. The coracoclavicular ligaments were then identified and dissection carried out posterior and medial towards the base of the coracoid. The suprascapular artery was identified, and a separate Neviaser portal was established. A smooth switching stick was inserted and utilized to dissect and retract the supraspinatus bluntly. The 30° arthroscope was then switched to a 70° arthroscope, allowing easy visualization of the suprascapular ligament with the nerve lying beneath. The ligament was then resected using an 18-gauge spinal needle. The nerve was then carefully mobilized using the smooth switching stick (see Fig. 1).
Fig. 1.
A: View from the posterior portal. The CA Ligament is identified following subacromial decompression. B: Dissection carried medially as the coracoclavicular ligaments are identified from the posterior portal. The shaver is coming in from an anterior-lateral portal created in-line with the supraspinatus muscle. C: A smooth switching stick is placed just behind the base of the coracoclavicular ligaments and used to retract the supraspinatus in a posterior direction as viewed from a posterior lateral viewing portal. Neviaser portal for additional retraction is then established using a spinal needle. D: A blunt switching stick from the Nevasier portal is used for gentle soft tissue retraction and to expose the transverse scapular ligament with the nerve beneath. E: A 70° arthroscope is utilized to maximize visibility of the suprascapular ligament and nerve relationship. F: A Spinal needle is introduced adjacent to the Neviaser portal and used to sharply dissect the ligament, with care to protect the nerve. G: Final viewing of the suprascapular nerve following ligament release and debridement.
2.3. Statistics
Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) software (IBM, Version 24.0, Chicago, USA). The dependent t-test was used to compare means between scalar variables within the same group (i.e initial and final VAS scores). The independent t-test was used to compare means between scalar variables of different groups (i.e. those with and without rotator cuff repairs). Binary logistic regression was used to assess for risk factors for the development of complications.
3. Results
3.1. Demographics
One hundred eighty-four patients were identified as potential candidates from which 112 (female = 60) patients were selected based on the inclusion and exclusion criteria. The average age of this group was 50 years and they had an average duration of symptoms of 19 months prior to presentation. The average follow-up period for the group was 8.74 months (range 1–52 months) post op. Twenty-seven patients underwent concomitant rotator cuff repair, 5 underwent concomitant labral repair, and 23 had concomitant biceps tenodesis.
There were 15 cases of failed previous arthroscopic shoulder surgery performed at outside facilities (13% of all cases), where patients either failed to improve from the index procedure, or only improved for a short time with persistence of shoulder pain or weakness of the rotator cuff. Of these cases, 6 were subacromial decompression with bursectomy, 4 were rotator cuff repair, 4 were SLAP or labral repairs, and 1 was a capsular plication.
3.2. Outcomes
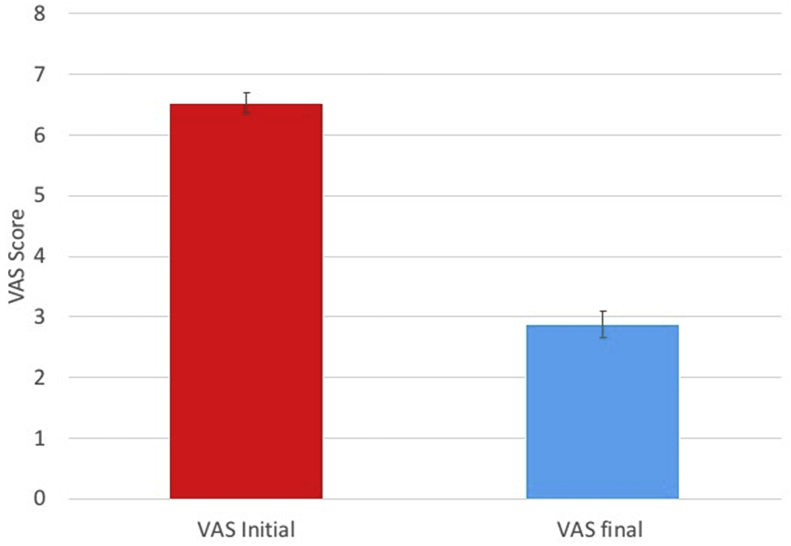
Overall, there was a statistically significant difference in initial VAS score (m = 6.53, std = 1.93) and the VAS score at final follow up (m = 2.88, std = 2.40), t(111) = 13.79, p < 0.0001 (see Fig. 2) Patients with prior failed arthroscopic shoulder surgery also experienced a significant improvement in their VAS score from initial (m = 6.14, std = 1.65) to final (m = 2.29, std = 1.97), t(13) = 5.62, p < 0.0001.
Fig. 2.
Initial and final VAS pain scores displayed with error bars showing one standard error. t(222) = 12.49, p < 0.0001.
There was no statistically significant difference between final VAS scores of patients with a concomitant RTCR performed concomitant to the suprascapular nerve release (m = 3.93, std = 2.70) and those who underwent isolated SSN release (m = 3.55, std = 2.83). t(110) = -0.6, p = 0.54.
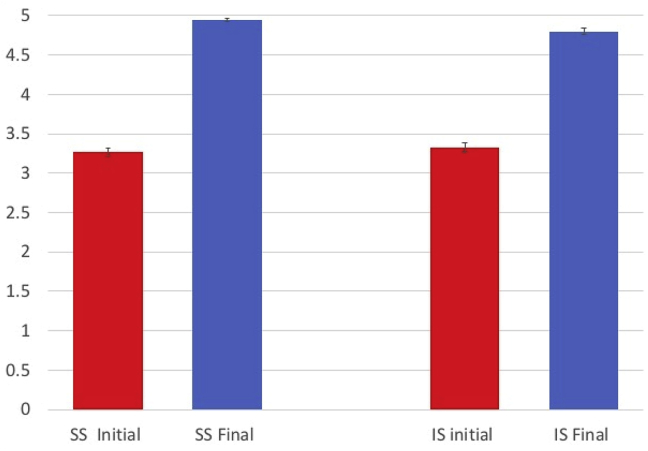
Overall, there was a statistically significant difference in initial supraspinatus strength (m = 3.26, std = 0.58) and supraspinatus strength at final follow up (m = 4.93, std = 0.22), t(111) = -29.51, p < 0.0001. Finally, there was also a statistically significant difference in initial infraspinatus strength (m = 3.33, std = 0.62) and infraspinatus strength at final follow up (m = 4.80, std = 0.43), t(111) = -21.03, p < 0.0001 (see Fig. 3). Patients with prior failed arthroscopic shoulder surgery also experienced a significant improvement in their supraspinatus and infraspinatus strength from initial (SS: m = 3.21, std = 0.57, IS: m = 3.28, std = 0.61) to final (SS: m = 4.89, std = 0.28, IS: m = 4.89, std = 0.3), SS: t(13) = -10.32, p < 0.0001, IS: t(13) = -9.61, p < 0.0001.
Fig. 3.
Initial and final strength (graded 0–5) for supraspinatus and infraspinatus displated with error bars showing one standard error. t(222) = -28.27, p < 0.0001.
There was no statistically significant difference in supraspinatus strength improvement between patients with a concomitant RTCR (m = 1.5, std = 0.63) and those who underwent isolated SSN release (m = 1.74, std = 0.58). t(110) = 1.7, p = 0.09. There was no statistically significant difference in infraspinatus strength improvement between patients with a concomitant RTCR (m = 1.24, std = 0.8) and those who underwent isolated SSN release (m = 1.54, std = 0.71). t(110) = 1.9, p = 0.07.
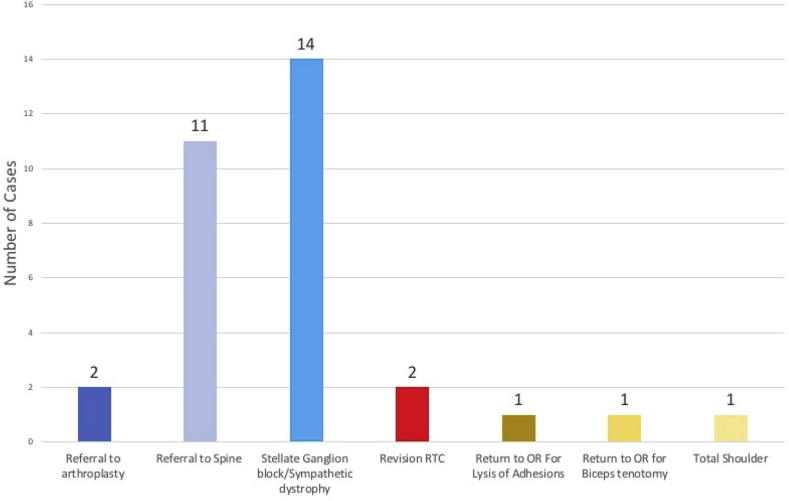
3.3. Complications
There were zero instances of infection, neurovascular injury, deep venous thrombosis or fracture (see Fig. 4 for complete outline of complications) in this series. The most common complication was post-operative development of a type of sympathetic mediated pain (sympathetic dystrophy) characterized by varying degrees of diffuse burning, muscle spasm, hyperesthesia and tingling in the shoulder area in 14 patients (12%). The authors believe this was most likely attributed to type 2 sympathetic dystrophy. Of the 14 patients who developed this problem 12 were treated with a series of stellate ganglion blocks and had reduction in their pain over 3 months. Particular success was noted in patients who were caught early. 1 patient improved without the use of a stellate ganglion block and 2 patients were referred to spine surgery and eventually diagnosed with cervical radiculopathy. Logistic regression analysis failed to find a significant association with any risk factor (smoking status, diabetes, work comp status, concomitant rotator cuff repair, cervical spine disease) and the development of this complication.
Fig. 4.
Bar chart depicting rate of complications.
The next most common complication was enhancement of spine mediated radicular pain following surgery which occurred in 11 patients (10%). These patients noted improvement in their shoulder pain but had increasing radicular pain and were referred to spine specialists for evaluation. Two patients required eventual referral to arthroplasty for concomitant pre-existing glenohumeral arthritis.
There were 5 cases of return to the operating room. One patient who had significant preexisting glenohumeral arthritis underwent hemiarthroplasty 7 months after the index procedure by the arthroplasty service. One patient had continued pain over her biceps which failed to resolve and eventually required a biceps tenotomy. Two patients required revision rotator cuff repair approximately 1 year after the index procedure, one of whom also required lysis of adhesions for post-operative adhesive capsulitis. The first patient had a partial repair of her supraspinatus but failed to improve after surgery. Repeat MRI showed re-tear of the repair. The strength of the rotator cuff had returned 1 year after the revision surgery but the patient continued to have radicular pain and was referred to spine surgery. The second patient did not heal their initial repair and underwent revision surgery 6 months after the index procedure, eventually regaining full strength.
In this study there were 10 patients with <2 months of follow up either because they were discharged or lost to follow up. However, 5 of these patients had complete resolution of their pain (VAS changes 8 → 0, 7 → 0, 6 → 0, 9 → 0 and 7 → 0) at their last visit. There were 4 patients who did not have complete resolution of their pain at last visit and were lost to follow up: one had VAS improvement from 8 → 2, another had VAS improvement from 7 → 6 however stated she had 75% improvement in her shoulder overall. Another had a VAS improvement only from 6 → 5 but stated to have 95% improvement in her shoulder overall. The last had VAS improvement from 3 → 2 but reported 80% improvement in her shoulder overall. One patient had worsening in her VAS score from 3 → 4 as a result of sympathetic pain despite stellate ganglion blocks but still reported 50% improvement in her shoulder. She struggled to improve and was lost to follow up. A graphic summary of the complications experienced are summarized in Fig. 4.
4. Discussion
Until recently, suprascapular neuropathy was considered a diagnosis of exclusion. However, improved understanding has led practitioners focus their diagnostic means to elevate it on the differential. The suprascapular nerve contributes to the motor control of the supraspinatus/infraspinatus muscles. However, this nerve also provides the predominant sensory innervation to the glenohumeral and AC joints.7,13,27,28 As a result, compression and irritation of the nerve, specifically at the suprascapular notch, may play a role in the patient's pain response to peri-scapular as well as intra-articular pathology. Multiple etiologies for nerve compression have been described including hypertrophy of the transverse scapular ligament, mass effect from a cyst, varicose veins, tumor, traction from overhead athletics, or retracted rotator cuff tears.1,10,14,20,22
Suprascapular neuropathy typically presents with posterior shoulder pain and difficulty with overhead activities. On examination patients may have weakness of the infraspinatus and supraspinatus muscles with atrophy occurring in extreme cases.5 MRI is useful to identify anatomic causes of mass effect in the suprascapular or spinoglenoid notch as well as signal changes in the muscle.21 Recently a objective spinoglenoid notch distension measurement has been shown to help identify patients with suprascapular neuropathy.16 Furthermore, EMG/NCS remain the gold standard for diagnosis. Despite this, the sensitivity and specificity of these studies are unknown.6,8,11 In the setting of an unclear diagnosis, suprascapular notch injections may be a helpful adjunct to confirm cases with negative EMG/NCS studies for which shoulder pain cannot be explained.5,9
The true incidence and prevalence of SSN is unknown, which is likely due to the lack of a reliable diagnostic test. In this series, 13% of patients were referred to our practice after having failed to improve after an initial arthroscopic surgery performed at another facility. These patients were eventually diagnosed with suprascapular neuropathy on EMG/NCS and had good outcomes after release. Moreover, SSN is commonly associated with other pathological processes in the shoulder such as rotator cuff tear and thus may be masked by other conditions.22 In this series 27 patients had concomitant rotator cuff repair (24%) and had similar outcomes to those with isolated SSN release.
The initial treatment of suprascapular neuropathy in the absence of a space occupying lesion consists of activity modification, nonsteroidal anti-inflammatories and physical therapy. There have been several small studies documenting success with this approach.4,12 However, poor outcomes have also been reported with nonoperative management.9,24 While the open approach has been shown to be effective,2,3,17 arthroscopic release provides minimally invasive alternative to decompress the nerve at the suprascapular notch. We could only identify three other series of arthroscopic suprascapular nerve decompression.15,18,25The first by Lafosse was a series of 10 patients who showed normalization of postoperative EMG/NCS exam and significant improvement in their constant scores after arthroscopic decompression. All patients graded their outcome as excellent and had resolution of their shoulder pain.18 Shah et al. published the second study on 27 patients who underwent arthroscopic release and showed improvement in pain, ASES and SSV scores by 10 weeks post op. Garcia et al. published a series of 10 patients with EMG confirmed suprascapular neuropathy and demonstrated improved UCLA shoulder scores.15 Furthermore, Momaya recently published a systematic review including 275 shoulders with a variety of pathology at the spinoglenoid notch and the suprascapular notch treated with open or arthroscopic techniques. They reported improvement in VAS scores and Constant-Murley scores as well as suitable return to sport.23
In this series there were 112 patients who had EMG/NCS confirmed SSN all who underwent arthroscopic release. There was significant improvement in VAS pain scores from the first office visit to final follow up. Moreover, there was significant improvement in strength of the infraspinatus and supraspinatus muscle testing. There was no significant difference in outcome with regards to strength or pain in patients with isolated suprascapular neuropathy versus those who also underwent concomitant rotator cuff reconstruction. The complication rate was low with the primary complication being sympathetic dystrophy treated with stellate ganglion blocks.
There are several weaknesses to this study. The first is the lack of patient evaluation with a shoulder outcome score. As we do not routinely administer a score to our patients, this information was impossible to collect retrospectively. The second weakness was a lack of longer follow up with some patients. In this study there were 10 patients who had less than 2 months of follow-up. However, the majority had complete resolution of their pain or improvement on their initial VAS scores, were doing excellent at their last visit and were discharged by the senior author. We hope this study will help lay the ground work for the evaluation of the arthroscopic suprascapular release by a prospective, randomized control study with long term follow up.
In conclusion, this is the largest series of arthroscopic suprascapular nerve decompressions to date. We show a significant improvement in VAS pain scores as well as supraspinatus and infraspinatus function following arthroscopic release of the suprascapular ligament. The procedure proved safe with a very low complication rate. Practitioners should consider the diagnosis of suprascapular neuropathy in appropriate patients who fail to improve with conservative management or previous operative intervention.
Declaration of competing interest
The authors report no conflict of interest.
References
- 1.Albritton M.J., Graham R.D., Richards R.S., Basamania C.J. An anatomic study of the effects on the suprascapular nerve due to retraction of the supraspinatus muscle after a rotator cuff tear. J Shoulder Elb Surg. 2003 Sep;12(5):497–500. doi: 10.1016/s1058-2746(03)00182-4. [DOI] [PubMed] [Google Scholar]
- 2.Antoniadis G., Richter H.-P., Rath S., Braun V., Moese G. Suprascapular nerve entrapment: experience with 28 cases. J Neurosurg. 1996 Dec;85(6):1020–1025. doi: 10.3171/jns.1996.85.6.1020. [DOI] [PubMed] [Google Scholar]
- 3.Antoniou J., Tae S.-K., Williams G.R., Bird S., Ramsey M.L., Iannotti J.P. Suprascapular neuropathy: variability in the diagnosis, treatment, and outcome. Clin Orthop. 2001 May;386:131–138. [PubMed] [Google Scholar]
- 4.Black K.P., Lombardo J.A. Suprascapular nerve injuries with isolated paralysis of the infraspinatus. Am J Sports Med. 1990 Jun;18(3):225–228. doi: 10.1177/036354659001800301. [DOI] [PubMed] [Google Scholar]
- 5.Boykin R.E., Friedman D.J., Higgins L.D., Warner J.J. Suprascapular neuropathy. J Bone Jt Surg Am. 2010 Oct;92(13):2348–2364. doi: 10.2106/JBJS.I.01743. [DOI] [PubMed] [Google Scholar]
- 6.Boykin R.E., Friedman D.J., Zimmer Z.R., Oaklander A.L., Higgins L.D., Warner J.J.P. Suprascapular neuropathy in a shoulder referral practice. J Shoulder Elb Surg. 2011 Sep;20(6):983–988. doi: 10.1016/j.jse.2010.10.039. [DOI] [PubMed] [Google Scholar]
- 7.Brown G.A. Venous thromboembolism prophylaxis After major orthopaedic surgery: a pooled analysis of randomized controlled trials. J Arthroplast. 2009 Sep;24(6):77–83. doi: 10.1016/j.arth.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 8.Buschbacher R.M., Weir S.K., Bentley J.G., Cottrell E. Normal motor nerve conduction studies using surface electrode recording from the supraspinatus, infraspinatus, deltoid, and biceps. PM&R. 2009 Feb;1(2):101–106. doi: 10.1016/j.pmrj.2008.08.002. [DOI] [PubMed] [Google Scholar]
- 9.Callahan J.D., Scully T.B., Shapiro S.A., Worth R.M. Suprascapular nerve entrapment: a series of 27 cases. J Neurosurg. 1991 Jun;74(6):893–896. doi: 10.3171/jns.1991.74.6.0893. [DOI] [PubMed] [Google Scholar]
- 10.Carroll K.W., Helms C.A., Otte M.T., Moellken S., Fritz R. Enlarged spinoglenoid notch veins causing suprascapular nerve compression. Skelet Radiol. 2003 Feb;32(2):72–77. doi: 10.1007/s00256-002-0598-5. [DOI] [PubMed] [Google Scholar]
- 11.Casazza B.A., Young J.L., Press J.P., Heinemann A.W. Suprascapular nerve conduction: a comparative analysis in normal subjects. Electromyogr Clin Neurophysiol. 1998 May;38(3):153–160. [PubMed] [Google Scholar]
- 12.Drez D. Suprascapular neuropathy in the differential diagnosis of rotator cuff injuries. Am J Sports Med. 1976 Apr;4(2):43–45. doi: 10.1177/036354657600400201. [DOI] [PubMed] [Google Scholar]
- 13.Ebraheim N.A., Whitehead J.L., Alla S.R. The suprascapular nerve and its articular branch to the acromioclavicular joint: an anatomic study. J Shoulder Elb Surg. 2011 Mar;20(2):e13–e17. doi: 10.1016/j.jse.2010.09.004. [DOI] [PubMed] [Google Scholar]
- 14.Ferretti A., Cerullo G., Russo G. Suprascapular neuropathy in volleyball players. J Bone Joint Surg Am. 1987 Feb;69(2):260–263. [PubMed] [Google Scholar]
- 15.Garcia Júnior J.C., Paccola A.M.F., Tonoli C., Zabeu J.L.A., Garcia J.P.M. Arthroscopic release OF the suprascapular nerve: surgical technique and evaluation OF clinical cases. Rev Bras Ortop. 2015 Nov 17;46(4):403–407. doi: 10.1016/S2255-4971(15)30252-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Katsuura Y., Hill A.J., Colón L.F., Dorizas J.A. MRI diagnosis of suprascapular neuropathy using spinoglenoid notch distension. Radiol Med. 2019 Mar 5 doi: 10.1007/s11547-019-01005-z. [DOI] [PubMed] [Google Scholar]
- 17.Kim D.H., Murovic J.A., Tiel R.L., Kline D.G. Management and outcomes of 42 surgical suprascapular nerve injuries and entrapments. Neurosurgery. 2005 Jul 1;57(1):120–127. doi: 10.1227/01.neu.0000163406.14384.4f. [DOI] [PubMed] [Google Scholar]
- 18.Lafosse L., Tomasi A., Corbett S., Baier G., Willems K., Gobezie R. Arthroscopic release of suprascapular nerve entrapment at the suprascapular notch: technique and preliminary results. Arthrosc J Arthrosc Relat Surg. 2007 Jan;23(1):34–42. doi: 10.1016/j.arthro.2006.10.003. [DOI] [PubMed] [Google Scholar]
- 19.Lajtai G., Pfirrmann C.W.A., Aitzetmüller G., Pirkl C., Gerber C., Jost B. The shoulders of professional beach volleyball players: high prevalence of infraspinatus muscle atrophy. Am J Sports Med. 2009 Jul;37(7):1375–1383. doi: 10.1177/0363546509333850. [DOI] [PubMed] [Google Scholar]
- 20.Lichtenberg S., Magosch P., Habermeyer P. Compression of the suprascapular nerve by a ganglion cyst of the spinoglenoid notch: the arthroscopic solution. Knee Surg Sports Traumatol Arthrosc Off J ESSKA. 2004 Jan;12(1):72–79. doi: 10.1007/s00167-003-0443-y. [DOI] [PubMed] [Google Scholar]
- 21.Ludig T., Walter F., Chapuis D., Molé D., Roland J., Blum A. MR imaging evaluation of suprascapular nerve entrapment. Eur Radiol. 2001;11(11):2161–2169. doi: 10.1007/s003300100968. [DOI] [PubMed] [Google Scholar]
- 22.Mallon W.J., Wilson R.J., Basamania C.J. The association of suprascapular neuropathy with massive rotator cuff tears: a preliminary report. J Shoulder Elb Surg. 2006 Jul;15(4):395–398. doi: 10.1016/j.jse.2005.10.019. [DOI] [PubMed] [Google Scholar]
- 23.Momaya A.M., Kwapisz A., Choate W.S. Clinical outcomes of suprascapular nerve decompression: a systematic review. J Shoulder Elb Surg. 2018 Jan;27(1):172–180. doi: 10.1016/j.jse.2017.09.025. [DOI] [PubMed] [Google Scholar]
- 24.Post M. Diagnosis and treatment of suprascapular nerve entrapment. Clin Orthop. 1999 Nov;(368):92–100. [PubMed] [Google Scholar]
- 25.Shah A.A., Butler R.B., Sung S.-Y., Wells J.H., Higgins L.D., Warner J.J.P. Clinical outcomes of suprascapular nerve decompression. J Shoulder Elb Surg. 2011 Sep;20(6):975–982. doi: 10.1016/j.jse.2010.10.032. [DOI] [PubMed] [Google Scholar]
- 26.Shah A.S., Waters P.M., Bae D.S. Treatment of the “pink pulseless hand” in pediatric supracondylar humerus fractures. J Hand Surg. 2013 Jul;38(7):1399–1403. doi: 10.1016/j.jhsa.2013.03.047. [DOI] [PubMed] [Google Scholar]
- 27.Vorster W., Lange C.P.E., Briët R.J.P. The sensory branch distribution of the suprascapular nerve: an anatomic study. J Shoulder Elb Surg. 2008 May;17(3):500–502. doi: 10.1016/j.jse.2007.10.008. [DOI] [PubMed] [Google Scholar]
- 28.Warner J.P., Krushell R.J., Masquelet A., Gerber C. Anatomy and relationships of the suprascapular nerve: anatomical constraints to mobilization of the supraspinatus and infraspinatus muscles in the management of massive rotator-cuff tears. J Bone Joint Surg Am. 1992 Jan;74(1):36–45. [PubMed] [Google Scholar]