Abstract
Purpose
To compare complications following arthroscopy and arthrotomy for treatment of septic knee arthritis.
Methods
Patients undergoing arthroscopy and arthrotomy for a diagnosis of septic knee arthritis were identified in National Surgical Quality Improvement Program and placed in a multivariate analysis to determine if type of surgery contributed to postoperative complications.
Results
Knee arthrotomy was associated with an increased risk for increased operative time [Parameter estimate 4.555 (95% CI:3.023–6.085); p < 0.0001], minor morbid events [OR 2.064 (95% CI: 1.447–2.943); p < 0.0001], and any morbidity [OR 2.285 (95% CI:1.527–3.419); p < 0.0001].
Conclusions
Knee arthrotomy was associated with a higher risk of complications.
Keywords: Septic knee, Arthroscopy, Arthrotomy
1. Introduction
Acute septic arthritis is rare, but can cause significant morbidity and mortality without prompt diagnosis and treatment with increased risk to those with underlying joint conditions, those with joint prostheses, and in elderly populations.1,2 Complications include irreversible joint damage due to the ensuing inflammatory process and sepsis.3,4 While any joint can be infected, acute septic arthritis most commonly occurs in the knee and hip, followed by the shoulder and ankle.3 The mainstay of treatment is surgical irrigation and debridement followed by intravenous antibiotics.2,3,5 Most common for irrigation and debridement are arthroscopy, a less invasive procedure, or arthrotomy, an open procedure, although the majority of orthopedic surgeons and rheumatologist recommend arthroscopy as their preferred treatment.6
In acute septic arthritis of the knee, several small retrospective studies and one small randomized control trial have investigated whether treatment by arthroscopy or arthrotomy results in better post-operative outcomes.7, 8, 9, 10, 11 The largest of these studies included 70 patients. In each study, arthroscopy was preferred over arthrotomy due to better functional results, lower reinfection rate and less need for multiple procedures. However, multiple studies indicated that the primary determinant of outcome is time to treatment.7,9,11
Most recently, a study examined 30-day complications for septic knee arthritis treated with arthrotomy versus arthroscopy using the American College of Surgeons National Surgical Quality Improvement Program (NSQIP).12 This study noted higher trends of minor adverse events in the open arthrotomy treatment, while the rates of serious adverse events were higher in the arthroscopic surgery treatment group. Ultimately, multivariate analysis concluded a lack of superiority in either treatment. However, the study was only powered to detect a difference of approximately 15%, indicating that the study may have been underpowered.12 The purpose of this study was to evaluate 30-day complications following arthrotomy versus arthroscopy for the treatment of septic knee arthritis using a larger national database cohort.
2. Patients and methods
2.1. Data source and patient selection
This research has been approved by the authors’ affiliated institutions.
The ACS-NSQIP database is a nationally validated, outcomes-based program that collects data on patients from over 600 hospitals across the United States undergoing inpatient or outpatient surgery.13 Trained clinical reviewers at each location prospectively collect data from patient interviews and chart reviews related to patient demographics, potential preoperative risk factors, intraoperative variables, and complications through 30 days postoperatively.
The NSQIP database was queried from 2006 to 2016 to identify CPT codes of patients’ undergoing knee arthroscopy (29850, 29851, 29855, 29856, 29866, 29867, 29868, 29870, 29871, 29873, 29874, 29875, 29876, 29877, 29879, 29880, 29881, 29882, 29883, 29884, 29885, 29886, 29887) and knee arthrotomy (27310, 27330, 27331, 27334, 27335). This subset of surgeries was further queried to only include patients with a diagnosis of knee septic arthritis utilizing the ICD-9 (711.08, 711.09, 711.46, 711.48, 711.49, 711.96, 711.98, 711.99) or the ICD-10 codes (M00.0, M00.060, M00.061, M00.62, M00.069, M00.09, M00.10, M00.160, M00.161, M00.169, M00.20, M00.260, M00.261, M00.262, M00.269, M00.80, M00.860, M00.861, M00.862, M00.869, M00.890, M00.90).
Furthermore, postoperative morbid events were classified as minor (transfusion of a blood product, pneumonia, wound dehiscence, urinary tract infection and renal insufficiency) and serious (wound infection, thromboembolic event, renal failure, myocardial infarction, prolonged ventilation, unplanned intubation, sepsis/septic shock, and death). Outcomes collected were operative time, reoperation, hospital length of stay, readmission and morbid events.
2.2. Statistical analysis
Continuous variables are reported as mean ± standard deviation. Categorical variables are reported as counts and percentage of whole. Continuous variables were compared with a student t-test. Categorical variables were compared with Pearson chi-square tests. Knee arthroscopy versus knee arthrotomy was looked at as a risk factor for prolonged operative time, re-operation, prolonged length of stay, and morbid events. The outcomes identified as significant were placed in a multivariate analysis controlling for age, sex, BMI and ASA score. Alpha level was set at p < 0.05 with a Bonferroni correction adjusting for multiple comparisons. All data and statistical analyses were performed using JMP Pro (version 13.0, SAS, Cary, NC).
3. Results
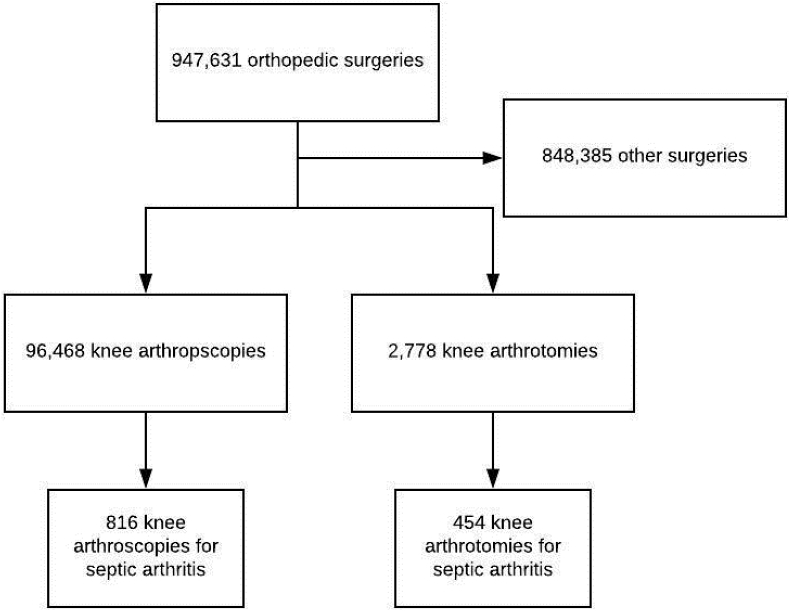
A total of 947,631 orthopedic surgeries were included in the NSQIP database from 2006 to 2016.
Of these cases 2,778 cases included CPT codes for knee arthrotomy and 96,468 cases included CPT codes for knee arthroscopy. Furthermore, when querying for an ICD-9/10 code of septic arthritis, there were 454 patients who underwent knee arthrotomy and 816 patients who underwent knee arthroscopy for septic arthritis (Fig. 1).
Fig. 1.
Patient selection flowchart.
The average age in the knee arthrotomy group was 57.3 ± 16 compared to 57.4 ± 17.9 in the knee arthroscopy group (p = 0.87). There were similar proportions of males (68%) undergoing arthrotomy as arthroscopy (66%). A higher proportion of patients undergoing arthrotomy trended towards having a BMI>30 compared to patients undergoing arthroscopy (44% vs 37.5%; p = 0.022) as well as trended towards a greater proportion of smokers (29.1% vs 23.3%; p = 0.023). Lastly, higher ASA scores were seen in the knee arthrotomy cohort (2.8 ± 0.7) compared to the knee arthroscopy cohort (2.6 ± 0.75; p = 0.0003) (Table 1).
Table 1.
Patient characteristics.
| Characteristic% | All patients (n = 1270) | Knee arthrotomy (n = 454) | Knee arthroscopy (n = 816) | p value* |
|---|---|---|---|---|
| Age | 57.4 ± 17.2 | 57.3 ± 16 | 57.4 ± 17.9 | 0.87 |
| Male | 849 (67) | 310 (68) | 539 (66) | 0.45 |
| BMI >30 | 506 (39.8) | 200 (44) | 306 (37.5) | 0.022 |
| Smoker |
322 (25) |
132 (29.1) |
190 (23.3) |
0.023 |
| ASA score |
2.7 ± 0.7 |
2.8 ± 0.7 |
2.6 ± 0.75 |
0.0003+ |
| 1 | 57 (4.5) | 10 (2.2) | 47 (5.8) | 0.0023+ |
| 2 | 415 (32.9) | 135 (29.7) | 280 (34.7) | |
| 3 | 639 (50.6) | 246 (54.2) | 393 (48.6) | |
| 4 | 15112 | 63 (13.9) | 88 (10.9) |
% Categorical variable reported as number (percent); continuous variables reported as mean ± standard deviation.
*Chi-square, t-test.
+statistically significant, alpha<0.01 after Bonferroni correction.
On average, operative time for knee arthrotomy was 10 min longer (53 ± 33) compared to knee arthroscopy (43.7 ± 22; p < 0.0001). No significant difference for re-operation or re-admission rates were identified between the 2 groups. Knee arthrotomy patients had longer length of stays (10.1 ± 10.3 days) compared to the knee arthroscopy patients (8.7 ± 10.9 days; p = 0.0.19) (Table 2). Arthrotomy patients had a higher proportion of patients sustaining an adverse event (17.6%) compared to knee arthroscopy patients (8.8%; p < 0.0001). When the morbid events were further sub-categorized into minor and serious events, there was a higher frequency of minor morbid events in the knee arthrotomy patients (13.9%) vs. the knee arthroscopy patients (6%, p < 0.0001) (Table 2). In a sub-analysis of minor morbid events, transfusion of a blood product (p < 0.0001) and wound dehiscence (p < 0.016) were greater in the knee arthrotomy group.
Table 2.
Outcomes after Knee arthroscopy vs Knee arthrotomy.
| Outcome | Knee arthrotomy | Knee arthroscopy | p value* |
|---|---|---|---|
| Operative time (mean ± SD) | 53 ± 33 | 43.7 ± 22 | <0.0001+ |
| Re-operation | 26 (7.6) | 38 (6.3) | 0.42 |
| Hospital length of stay | 10.1 (10.3) | 8.7 (10.9) | 0.021 |
| Readmission | 22 (10.7) | 36 (9.7) | 0.71 |
| Any morbidity | 80 (17.6) | 72 (8.8) | <0.0001+ |
| Minor morbid event | 63 (13.9) | 49 (6) | <0.0001+ |
| Serious morbid event | 38 (8.4) | 74 (9.1) | 0.67 |
% Categorical variable reported as number (percent); continuous variables reported as mean ± standard deviation.
*Chi-square, t-test.
+statistically significant, alpha<0.007 after Bonferroni correction.
A multivariate analysis adjusting for age, sex, BMI and ASA score was shown to be significantly different from the univariate analysis. After adjustment, operative time Parameter estimate 4.6 (95% CI: 3.02–6.09; p < 0.0001) remained significantly higher in the knee arthrotomy group. On the other hand, prolonged hospital length of stay Parameter estimate 0.48 (95% CI: −0.13-1.086; p = 0.12) trended towards being associated with knee arthrotomy but not to the level of significance. Both any morbid events OR 2.06 (95% CI: 1.45–2.94; p < 0.0001) and minor morbid events OR 2.29 (95% CI: 1.53–3.42; p < 0.0001) were more closely associated with knee arthrotomy in comparison to knee arthroscopy (Table 3).
Table 3.
Multivariate analysis of knee arthrotomy versus knee arthroscopy.
| Knee Arthrotomy as Risk Factor for Following Outcomes | Parameter Estimate (95% CI)% | p value* |
|---|---|---|
| Operative Time | 4.555 (3.023, 6.085) | <0.0001+ |
| Hospital Length of Stay |
0.477 (−0.131, 1.086) |
0.12 |
|
Knee Arthrotomy as Risk Factor for Following Outcomes |
Odds Ratio (95% CI)% |
p value* |
| Any Morbidity | 2.064 (1.447, 2.943) | <0.0001+ |
| Minor Morbid Event | 2.285 (1.527, 3.419) | <0.0001+ |
%- 95% Confidence Intervals.
*multivariate logistic regression analysis adjusting for age, sex, BMI, ASA score.
+statistically significant, alpha<0.01 after Bonferroni correction.
4. Discussion
Septic arthritis is a potentially devastating condition if not treated appropriately in a timely manner.1,2 The treatment for septic arthritis is an emergent irrigation and debridement to prevent irreversible joint damage.3,4 In the knee joint, irrigation of the joint can be accomplished through an arthroscopic or open procedure.
Which of these options is superior for infection eradication and patient outcomes is not entirely known, but recent studies have suggested there may be a benefit to arthroscopic treatment for septic arthritis of the knee. Retrospective cohort studies performed by Johns et al. and Bohler et al. and a small randomized controlled trial by Peres et al. independently found that arthroscopy was associated with a lower reoperation rate than arthrotomy.8,10,14 An additional retrospective cohort study by Wirtz et al. found better functional results in patients treated with arthroscopy compared to arthrotomy.11
Our findings add to the growing body of literature supporting the use of arthroscopy over open treatment for septic arthritis of the knee. After adjusting for potential confounding variables, arthroscopic treatment was associated with fewer adverse events postoperatively than open treatment. In contrast to some of the studies mentioned above, we found no difference in reoperation rate.
It should be noted that a previous analysis of NSQIP data by Bovonratwet et al. found equivocal outcomes following arthroscopy versus open arthrotomy for septic arthritis of the knee.12 In their analysis arthroscopy was associated with more minor adverse events while arthrotomy was associated with more major adverse events, however, no significance was noted after adjustment in the multivariate model. Their analysis only included data through 2014, which represents just a fraction of patients included in our analysis.
The main limitation of this study is its reliance on NSQIP data. While the NSQIP database includes many pertinent patient factors, especially regarding comorbid conditions, it does not include many details, which might be relevant to the cases at hand. Historical details, such as prior history, treating surgeon, and duration of antibiotics are unknown, raising the possibility of selection and treatment bias. Additional, prognostically important confounders such as time to surgery, organism, and Gachter grade (a grading system for severity of infection at the time of surgery) are missing. In particular, different microorganisms have different virulence and susceptibility which would influence the results. Each of these factors have been shown to be important determinants of patient outcomes and/or reoperation rate following irrigation and debridement of septic arthritis.9,15, 16, 17, 18, 19, 20 Ultimately, a well-designed, appropriately powered randomized controlled trial will be needed to definitively determine the best treatment for septic arthritis of the knee.
In the largest study of the published literature to date, this study shows preference towards arthroscopic irrigation and debridement for the treatment of septic knees. Arthrotomy was independently associated with an increased risk for longer operative time, minor morbid events and any morbid events. It is possible that previously published studies may have been underpowered to detect difference in complications following surgical treatment of septic knees.
CREDIT author statement
Daniel J. Johnson: conceptualization, software, investigation, writing; Bennet A. Butler: writing -original draft; Matthew H. Hartwell: formal analysis, conceptualization; Claire E. Fernandez: writing – original draft; Richard W. Nicolay: conceptualization; methodology; Ryan S. Selley,: formal analysis, supervision; Michael A. Terry: supervision, writing – review & editing; Vehniah K. Tjong: supervision, writing – review & editing.
Declaration of competing interest
All authors declare no conflicts of interest.
Footnotes
Study design: clinical; retrospective review.
References
- 1.Kaandorp C.J., Van Schaardenburg D., Krijnen P., Habbema J.D., van de Laar M.A. Risk factors for septic arthritis in patients with joint disease. A prospective study. Arthritis Rheum. 1995 Dec;38(12):1819–1825. doi: 10.1002/art.1780381215. [DOI] [PubMed] [Google Scholar]
- 2.Garcia-Arias M., Balsa A., Mola E.M. Septic arthritis. Best Pract Res Clin Rheumatol. 2011 Jun;25(3):407–421. doi: 10.1016/j.berh.2011.02.001. [DOI] [PubMed] [Google Scholar]
- 3.Shirtliff M.E., Mader J.T. Acute septic arthritis. Clin Microbiol Rev. 2002 Oct;15(4):527–544. doi: 10.1128/CMR.15.4.527-544.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Coakley G., Mathews C., Field M., British Society for Rheumatology Standards G, Audit Working G. BSR & BHPR, BOA RCGP and BSAC guidelines for management of the hot swollen joint in adults. Rheumatology. 2006 Aug;45(8):1039–1041. doi: 10.1093/rheumatology/kel163a. [DOI] [PubMed] [Google Scholar]
- 5.Perry C.R. Septic arthritis. Am J Orthoped. 1999 Mar;28(3):168–178. [PubMed] [Google Scholar]
- 6.Butt U., Amissah-Arthur M., Khattak F., Elsworth C.F. What are we doing about septic arthritis? A survey of UK-based rheumatologists and orthopedic surgeons. Clin Rheumatol. 2011 May;30(5):707–710. doi: 10.1007/s10067-010-1672-3. [DOI] [PubMed] [Google Scholar]
- 7.Balabaud L., Gaudias J., Boeri C., Jenny J.Y., Kehr P. Results of treatment of septic knee arthritis: a retrospective series of 40 cases. Knee Surg Sport Traumatol Arthrosc. 2007 Apr;15(4):387–392. doi: 10.1007/s00167-006-0224-5. [DOI] [PubMed] [Google Scholar]
- 8.Bohler C., Dragana M., Puchner S., Windhager R., Holinka J. Treatment of septic arthritis of the knee: a comparison between arthroscopy and arthrotomy. Knee Surg Sport Traumatol Arthrosc. 2016 Oct;24(10):3147–3154. doi: 10.1007/s00167-015-3659-8. [DOI] [PubMed] [Google Scholar]
- 9.Dave O.H., Patel K.A., Andersen C.R., Carmichael K.D. Surgical procedures needed to eradicate infection in knee septic arthritis. Orthopedics. 2016 Jan-Feb;39(1):50–54. doi: 10.3928/01477447-20151222-05. [DOI] [PubMed] [Google Scholar]
- 10.Peres L.R., Marchitto R.O., Pereira G.S., Yoshino F.S., de Castro Fernandes M., Matsumoto M.H. Arthrotomy versus arthroscopy in the treatment of septic arthritis of the knee in adults: a randomized clinical trial. Knee Surg Sport Traumatol Arthrosc. 2016 Oct;24(10):3155–3162. doi: 10.1007/s00167-015-3918-8. [DOI] [PubMed] [Google Scholar]
- 11.Wirtz D.C., Marth M., Miltner O., Schneider U., Zilkens K.W. Septic arthritis of the knee in adults: treatment by arthroscopy or arthrotomy. Int Orthop. 2001;25(4):239–241. doi: 10.1007/s002640100226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bovonratwet P., Nelson S.J., Bellamkonda K. Similar 30-day complications for septic knee arthritis treated with arthrotomy or arthroscopy: an American College of surgeons national surgical quality improvement program analysis. Arthroscopy. 2018 Jan;34(1):213–219. doi: 10.1016/j.arthro.2017.06.046. [DOI] [PubMed] [Google Scholar]
- 13.ACS NSQIP Hospitals. 2018. https://www.facs.org/search/nsqip-participants?allresults= Available from: [Google Scholar]
- 14.Johns B.P., Loewenthal M.R., Dewar D.C. Open compared with arthroscopic treatment of acute septic arthritis of the native knee. J Bone Joint Surg Am. 2017 Mar 15;99(6):499–505. doi: 10.2106/JBJS.16.00110. [DOI] [PubMed] [Google Scholar]
- 15.Kang T., Lee J.K. Host factors affect the outcome of arthroscopic lavage treatment of septic arthritis of the knee. Orthopedics. 2018 Mar 1;41(2):e184–e188. doi: 10.3928/01477447-20180102-01. [DOI] [PubMed] [Google Scholar]
- 16.Vispo Seara J.L., Barthel T., Schmitz H., Eulert J. Arthroscopic treatment of septic joints: prognostic factors. Arch Orthop Trauma Surg. 2002 May;122(4):204–211. doi: 10.1007/s00402-001-0386-z. [DOI] [PubMed] [Google Scholar]
- 17.Yanmis I., Ozkan H., Koca K., Kilincoglu V., Bek D., Tunay S. The relation between the arthroscopic findings and functional outcomes in patients with septic arthritis of the knee joint, treated with arthroscopic debridement and irrigation. Acta Orthop Traumatol Turcica. 2011;45(2):94–99. doi: 10.3944/AOTT.2011.2258. [DOI] [PubMed] [Google Scholar]
- 18.Hunter J.G., Gross J.M., Dahl J.D., Amsdell S.L., Gorczyca J.T. Risk factors for failure of a single surgical debridement in adults with acute septic arthritis. J Bone Joint Surg Am. 2015 Apr 1;97(7):558–564. doi: 10.2106/JBJS.N.00593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aim F., Delambre J., Bauer T., Hardy P. Efficacy of arthroscopic treatment for resolving infection in septic arthritis of native joints. Orthop Traumatol Surg Res. 2015 Feb;101(1):61–64. doi: 10.1016/j.otsr.2014.11.010. [DOI] [PubMed] [Google Scholar]
- 20.Stutz G., Kuster M.S., Kleinstuck F., Gachter A. Arthroscopic management of septic arthritis: stages of infection and results. Knee Surg Sport Traumatol Arthrosc. 2000;8(5):270–274. doi: 10.1007/s001670000129. [DOI] [PubMed] [Google Scholar]