The worldwide burden of pneumonia is high—the disease caused 1·2 million deaths in 2010, mostly in children younger than 2 years.1 In the same year, at least 76·7 million disability-adjusted life-years (DALYs) were attributed to pneumonia and pneumococcal disease,2 although DALYs are inevitably increased in diseases that mostly affect young children. Infections of the lower respiratory tract (many of which are probably pneumonia-related) were the single largest cause of worldwide DALYs in children younger than 1 year.2 Streptococcus pneumoniae is the most common cause of pneumonia, although other bacteria, viruses, and fungi are also important sources of infection.
The Research Investments in Global Health study3 analysed public and philanthropic infectious disease research funding awarded to UK institutions, and reported data about funding for respiratory infectious diseases.4 The total research investment in pneumonia (£27·2 million) relative to the 2010 burden was £0·58 per DALY, which is substantially lower than that for tuberculosis (£3·14) and influenza (£4·16), and also lower than investments for all other respiratory infectious diseases (where data were available) for which effective vaccinations are available and widely used, except for measles and pertussis.
A threat report on antimicrobial resistance released by the US Centers for Disease Control and Prevention (CDC) in 2013 rated the threat level for S pneumoniae as severe.5 In the UK, during the period 1997–2010, investments for antimicrobial resistance seem historically inadequate,6 despite the concerns and urgency of the problem; however, focus seems to be increasing in this important area.5,7
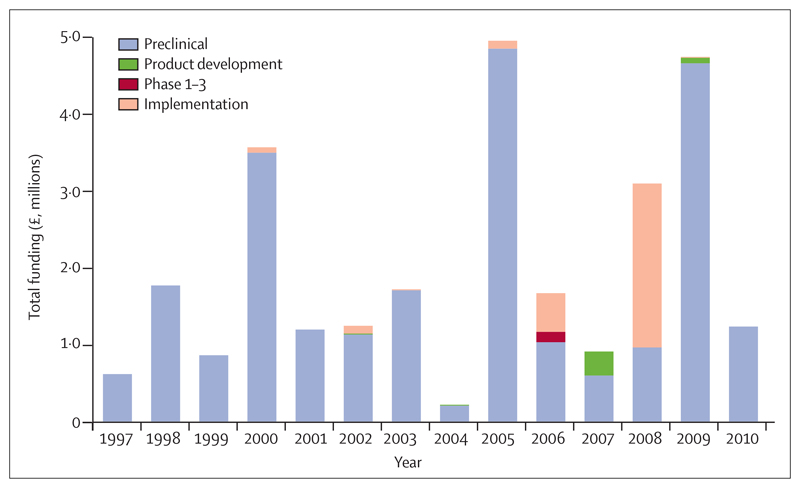
An important factor in the assessment of investments in research is the stage of research and its position along the research and development pipeline. Our analysis shows that in the UK, pneumonia research is almost entirely preclinical (figure), accounting for 87·5% of the total funding for pneumonia-related research. Conversely, funding for phase 1–3 trials, product development studies, or implementation research by public and philanthropic funders is low. Publicly available information about private sector investments by pharmaceutical companies, who typically invest in phase 1–4 studies or product development research, is scarce. The apparent low levels of investment in phase 1–3 research by public and philanthropic organisations suggests a real need to accurately document the contributions of the private sector in this area of research.
Figure. Total public and philanthropic funding in pneumonia-related research in 1997–2010, including breakdown of stage of research.
No published systematic analyses of the worldwide portfolio of research for pneumonia exist. One study8 lists some awards (including some from the private sector) relating to diagnostics and vaccines for pneumonia. Further research is needed to ascertain the amount and nature of funding for infectious disease research across several countries (eg, the G20 and other leading world economies)—especially for pneumonia-related research—to identify research gaps, reduce duplication of research investments, and help with the development of collaborations across centres or countries. Although several small research groups in the UK do pneumococcal-related research, few large research centres of excellence exist. This fragmented approach to pneumonia research and its funding might well hinder crucial large-scale research that can lead to breakthroughs. With the economic burden being difficult to measure, and the disease burden being concentrated in resource-poor settings, little incentive exists for the private sector to concentrate further investments in this particular area. In 2015, the Millennium Development Goals will give way to the Sustainable Development Goals, and not only have few countries indicated they are likely to meet their existing targets in relation to child mortality, but also, these new targets contain little reference to health.9
Investment in pneumonia research is low relative to its burden, in the UK and worldwide, and a call for increased funding has merit—although factors other than disease burden clearly affect resource allocation for research. However, what is clear, is that sustained political leadership worldwide, as occurred with HIV and AIDS,10 can promote research investment from preclinical to translational studies, and that attention on those pathogens that cause widespread mortality of young children in the poorest regions of the world should be increased and sustained. The efficiency of these investments can benefit from worldwide tracking of research funding that informs decision-making processes of policy makers and funders.
Acknowledgments
MGH works for the Infectious Disease Research Network, which has supported this work and is funded by the UK Department of Health. JRF has received funds from the Wellcome Trust and is a steering group member for the Infectious Disease Research Network. JAGS has received support from GlaxoSmithKline Biologicals for research on pneumococcal vaccine safety and from Merck for travel to attend a Merck meeting. RA has received research funding from the Medical Research Council, the National Institute for Health Research, and the UK Department for International Development. RA is also a member of the Medical Research Council Global Health Group. SCC currently receives unrestricted research funding from Pfizer (previously Wyeth Vaccines), research funding from GlaxoSmithKline, and has received consulting fees from GlaxoSmithKline, Pfizer, and Novartis, in addition to financial assistance from vaccine manufacturers to attend conferences; all grants and honoraria are paid into accounts within the respective National Health Service Trusts or Universities, or to independent charities. M-LN declares no competing interests. SCC and RA are acknowledged as the joint last author.
Footnotes
For more on research investments in globabl health see http://www.researchinvestments.org
Contributor Information
Michael G Head, Research Department of Infection and Population Health, Royal Free Campus, University College London, London NW3 2PF, UK.
Joseph R Fitchett, King’s College London, London, UK.
Marie-Louise Newell, Faculty of Medicine and Institute for Life Sciences, University of Southampton, Southampton, UK.
J Anthony G Scott, Department of Infectious Disease Epidemiology, London School of Hygiene and Tropical Medicine, London, UK.
Stuart C Clarke, Faculty of Medicine and Institute for Life Sciences, University of Southampton, Southampton, UK; University of Southampton Malaysia Campus, Nusajaya, Malaysia; Southampton NIHR Respiratory Biomedical Research Unit, University Hospital Southampton NHS Foundation Trust, Southampton, UK.
Rifat Atun, Harvard School of Public Health, Harvard University, Boston, MA, USA.
References
- 1.Walker CLF, Rudan I, Liu L, et al. Global burden of childhood pneumonia and diarrhoea. Lancet. 2013;381:1405–16. doi: 10.1016/S0140-6736(13)60222-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Murray CJ, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2197–223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 3.Head MG, Fitchett JR, Cooke MK, Wurie FB, Hayward AC, Atun R. UK investments in global infectious disease research 1997–2010: a case study. Lancet Infect Dis. 2013;13:55–64. doi: 10.1016/S1473-3099(12)70261-X. [DOI] [PubMed] [Google Scholar]
- 4.Head MG, Fitchett JR, Cooke MK, et al. Investments in respiratory infectious disease research 1997–2010: a systematic analysis of UK funding. BMJ Open. 2014;4:e004600. doi: 10.1136/bmjopen-2013-004600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Threat Report 2013. Antibiotic resistance threats. [accessed Oct 14, 2013];2013 http://www.cdc.gov/drugresistance/threat-report-2013/
- 6.Head MG, Fitchett JR, Cooke MK, et al. Systematic analysis of funding awarded for antimicrobial resistance research to institutions in the UK, 1997–2010. J Antimicrob Chemother. 2014;69:548–54. doi: 10.1093/jac/dkt349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Davies SC, Fowler T, Watson J, Livermore DM, Walker D. Annual Report of the Chief Medical O?cer: infection and the rise of antimicrobial resistance. Lancet. 2013;381:1606–09. doi: 10.1016/S0140-6736(13)60604-2. [DOI] [PubMed] [Google Scholar]
- 8.Moran M, Guzman J, Chapman N, et al. Neglected disease research and development: the public divide. Sydney: Policy Cures; 2013. [accessed March 7, 2014]. http://www.policycures.org/downloads/GF_report13_all_web.pdf. [Google Scholar]
- 9.United Nations. Sustainable development goals. [accessed April 5, 2014];2013 http://sustainabledevelopment.un.org/index.php?menu=1300.
- 10.Piot P, Bartos M, Larson H, Zewdie D, Mane P. Coming to terms with complexity: a call to action for HIV prevention. Lancet. 2008;372:845–59. doi: 10.1016/S0140-6736(08)60888-0. [DOI] [PubMed] [Google Scholar]