Abstract
Background:
Urgency urinary incontinence afflicts many adults, and most commonly affects women. Medications, a standard treatment, may be poorly tolerated with poor adherence. This warrants investigation of alternative interventions. Mind-body therapies such as hypnotherapy may offer additional treatment options for those with urgency urinary incontinence.
Objective:
To evaluate hypnotherapy’s efficacy compared to medications in treating women with urgency urinary incontinence.
Study Design:
This investigator-masked, non-inferiority trial compared hypnotherapy to medications at a Southwestern U.S. academic center and randomized women with non-neurogenic urgency urinary incontinence to weekly hypnotherapy sessions for two months (and continued self-hypnosis thereafter) or to medication and weekly counseling for two months (and medication alone thereafter). The primary outcome was the between group comparison of percent change in urgency incontinence on 3-day bladder diary at two months. Important secondary outcomes were between group comparisons of percent change in urgency incontinence at six and 12 months. Outcomes were analyzed based on non-inferiority margins of 5% for between group differences, P<0.025 (i.e. for between group difference in percentage change in urgency incontinence, if the lower bound of the 95% CI was >−5%, non-inferiority would be proven).
Results:
One hundred fifty-two women were randomized to treatment between April 2013-October 2016. One-hundred forty-two women (70 hypnotherapy, 72 medications) had 3-day diary information at two months and were included in the primary outcome analysis. Secondary outcomes were analyzed for women with diary data at six then 12 months’ time-points; 138 women (67 hypnotherapy, 71 medications) at six months, 140 women (69 hypnotherapy, 71 medications) at 12 months. There were no differences between group’s urgency incontinence episodes at baseline: median (Q1, Q3) for hypnotherapy was 8 (4, 14) and medication 7 (4, 11), P=0.165. For the primary outcome, while both interventions showed improvement, hypnotherapy did not prove non-inferior to medication at 2 months. Hypnotherapy’s median percent improvement was 73.0% (95% CI 60.0%−88˖9%), medication’s improvement was 88.6% (95% CI 78.6%−100.0%). The median difference in percent change between groups was 0% (95% CI −16.7–0.0%); because the lower margin of the CI did not meet the predetermined non-inferiority margin of > −5%, hypnotherapy did not prove non-inferior to medication. In contrast, hypnotherapy was non-inferior to medication for the secondary outcomes at six months (hypnotherapy 85.7% improvement, 95% CI 75.0–100%; medications 83.3% improvement, 95% CI 64.7%−100%; median difference in percent change between groups of 0%, 95% CI 0.0%−6.7%) and 12 months (hypnotherapy 85.7% improvement, 95% CI 66.7–94.4%; medications 80% improvement, 95% CI 54.5100%; median difference in percent change between groups of 0%, 95% CI −4.2%−9.5%).
Conclusions:
Both hypnotherapy and medications were associated with substantially improved urgency urinary incontinence at all follow-up. The study did not prove the non-inferiority of hypnotherapy compared to medications at 2 months, the study’s primary outcome. Hypnotherapy proved non-inferior to medications at longer-term follow-up, 6 and 12 months. Hypnotherapy is a promising, alternative treatment for women with UUI.
Keywords: urgency urinary incontinence, hypnotherapy, mind-body therapy, pharmacotherapy, randomized trial in women
Introduction
Urinary urgency incontinence (UUI), involuntary urine loss associated with a sudden, compelling desire to urinate,1 is common and costly. Twice as prevalent in women, UUI increases with age, afflicting 24% of women ≥ 40 years old.2 Those affected by UUI may also experience depression, loss of work productivity and independence.2,3 Pharmacotherapy, an accepted 2nd line UUI treatment, may have side effects limiting patient adherence and medication’s effectiveness. UUI medication continuation is as low as 45% at one month and 13% at one year.
Increased awareness of UUI as a functional disorder suggests that therapy directed towards the brain rather than the bladder alone could serve as alternative treatment. Functional disorders, including irritable bowel syndrome (IBS) and UUI, exhibit increased visceral sensitivity to physiologic stimulation. Brain imaging studies have reported differences in brain activity in patients with functional disorders, including those with IBS6 and UUI.7,8,9 Women with UUI manifest abnormal activation of portions of the brain that govern interoception, the perception and interpretation of physiologic stimuli arising within the body. These abnormalities, and the effect they have on other regions in the brain, likely influence bladder storage abnormalities.5 Brain regions governing interoception can in turn be modulated by areas of the brain responsible for executive control. Mind-body therapies such as hypnotherapy likely affect these executive control networks.
Despite the U.S. population’s increasing reliance on mind-body therapies for chronic conditions,10 few studies have focused on the use of alternative therapies, including hypnosis, for treatment of UUI. Freeman’s case series and a pilot study from our institution are two of the few reports supporting hypnotherapy’s use in Overactive Bladder/UUI.12,13 The American Psychologic Association describes hypnosis as, “…a therapeutic technique in which clinicians make suggestions to individuals who have undergone a procedure to relax… and focus their minds…for a wide range of conditions....”14 Although hypnotherapy has been used to treat other visceral conditions such as irritable bowel syndrome (IBS),15,16 reports of its use in UUI are scarce.
The aim of the current randomized trial was to compare hypnotherapy to medications in UUI treatment. This non-inferiority design, comparing a novel to standard intervention, tested whether bladder-directed hypnotherapy was non-inferior to medications. Our hypothesis was that bladder-directed hypnotherapy would be non-inferior to medications for the primary outcome, change in UUI episodes, at 2 months. Secondary outcomes included evaluation of the non-inferiority of hypnotherapy based on other time-points (6 and 12 months) as well as other exploratory measures.
Materials & Methods
Study Design.
Methodology for the Hypnotherapy Or Pharmacotherapy Trial has been described previously.17 Briefly, this randomized, parallel group, single institution, non-inferiority trial recruited women with UUI from a Southwestern U.S. academic center. The study used a non-inferiority design based on the rationale that, although medications are a standard UUI treatment, medication side effects limit effectiveness. The study was approved by the University of New Mexico Institutional Review Board (HRRC #09–314) and registered with ClinicalTrials.gov. #NCT01829425. All participants gave written consent.
Participants.
Study eligibility required women to have non-neurogenic UUI for at least three months, Overactive Bladder-Awareness Tool scores ≥ eight,18 and ≥ three UUI episodes (UUIEs) per week. 17 The inclusion criteria regarding UUI frequency were similar to those used in other medication trials.19,20,21 Exclusions included untreated urinary tract infection, pelvic prolapse beyond the hymen, contraindications to study interventions, anti-muscarinic medication use within three weeks of enrollment, or history of intravesical botulinum-toxin or UUI neuromodulator treatment.
Randomization and masking.
A computer-generated randomization sequence determined treatment group allocation in a 1:1 ratio. A research coordinator otherwise unaffiliated with the study placed group assignments in opaque, sequentially numbered, sealed envelopes. Randomization was stratified by UUI severity (≤ three or ≥four UUIEs on three-day diary) in varying permuted block sizes of four to eight. Randomization envelopes were securely stored and, upon completion of baseline information, opened by study coordinators. Hypnotic susceptibility testing was performed prior to randomization. Hypnotherapists performing susceptibility testing, investigators performing data analysis/interpretation and personnel performing data entry were masked to treatment assignment. Hypnotherapists providing treatment, medication counselors and participants were not masked. The mask was broken when the final participant completed 12-month follow-up.
Procedures:
Hypnotherapy & Medication.
At the baseline visit and prior to randomization, study coordinators educated all participants regarding first-line UUI behavioral interventions in a standard fashion. Education included urge suppression, bladder training and pelvic floor exercise verbal instruction, supplemented with written handouts. All participants received instruction regarding voiding diaries; these were returned at baseline, 8 weeks, 6 and 12 months.
Hypnotherapy.
Participants randomized to hypnotherapy received eight weekly, one-hour, one-on-one bladder-directed hypnotherapy sessions delivered by a board certified hypnotherapist using a standardized format17 (outlined in Appendix Table 1). The education in the 1st session mirrored that given by medication counselors. Thereafter, hypnotherapy, in contrast to medication counseling, primarily focused on the emotional issues (e.g. anxiety, shame, fear) associated with UUI, including triggers and responses, identified by participants during hypnotherapy sessions. Hypnotherapists helped participants develop therapeutic suggestions to address UUI and its associated emotions. A board certified hypnotherapist (R.E.S.), designed the hypnotherapy procedures manual in collaboration with a local hypnotherapy teaching institution, trained study hypnotherapists on the protocol, and monitored hypnotherapy quality, but did not personally administer the intervention. Procedures were reviewed with the four hypnotherapy interventionists in a four-hour training prior to study initiation. All hypnotherapy sessions were audio-recorded. Study personnel audited the recordings, confirming hypnotherapists’ adherence to study procedures. Participants received two recordings to encourage self-hypnosis with an additional optional hypnotherapy session offered between 6 and 12-month follow-up.
Medications.
Participants randomized to medications received eight weekly, one-on-one medication counseling sessions delivered using a standardized format17 (outlined in Appendix Table 1) Medication counselors were trained on anti-muscarinic use/side-effects during a four-hour session (Y.M.K.) and followed a medication procedures manual. Medication counselors reviewed medications and side effects during scheduled weekly phone or in-person sessions. All sessions were audio-recorded. Study personnel audited the recordings, confirming counselors’ adherence to study procedures. Participants received long-acting UUI medications; extended release oxybutynin 10 mg/day initially or extended release tolterodine 4 mg/day if oxybutynin had been previously ineffective or poorly tolerated. Participants could switch between these medications if one or the other’s side effects or efficacy were unacceptable.
Baseline Assessment and follow-up.
Baseline data obtained prior to randomization included participant characteristics (Table1), three-day bladder diaries, validated questionnaire results, hypnotic susceptibility tests, and pre-treatment expectations. The Stanford Hypnotic Susceptibility Scale22 was administered in individualized sessions prior to randomization by a hypnotherapist other than the hypnotherapist administering the intervention. Participants were categorized into high, medium and low hypnotic susceptibility group’s post-hoc for one of the exploratory secondary analyses.23 Participants rated their pre-treatment expectations following randomization and before treatment. Follow-up occurred following two months of the active intervention (hypnotherapy or medications/medication counseling), and at 6 and 12 months.
Table 1.
Baseline Characteristics of Participants
| Hypnotherapy (70) | Pharmacotherapy (72) | |
|---|---|---|
| Age (years) Mean (SD) | 57.6 (12.77) | 59.5 (10.30) |
| BMI (Kg/m2) Mean (SD) | 32.3 (8.04) | 30.5 (7.87) |
| Ethnicity N (%) Non-Hispanic | 45 (64.29) | 55 (76.39) |
| Hispanic/Latina | 24 (34.29) | 15 (20.83) |
| Unknown/Not reported/Refused | 1 (1.43) | 2 (2.78) |
| Race N (%) American Indian/Alaskan Native | 2 (2.86) | 2 (2.78) |
| Asian | 0 (0) | 0 (0) |
| Hawaiian/Pacific Islander | 1 (1.43) | 0 (0) |
| Black/African-American | 3 (4.29) | 1 (1.39) |
| White | 52 (74.29) | 61 (84.72) |
| Other | 11 (15.71) | 7 (9.72) |
| Unknown/Not reported/refused | 1 (1.43) | 1 (1.39) |
| Education (%) Less than High School | 2 (2.86) | 0 (0) |
| High School or Equivalent | 7 (10.00) | 10 (13.89) |
| Some College | 23 (32.86) | 15 (20.83) |
| Associates Degree | 7 (10.00) | 8 (11.11) |
| Bachelor’s Degree/Graduate Degree | 31 (44.29) | 39 (54.17) |
| Parity Median (Q1, Q3) | 2.00 (1, 3) | 2.00 (1, 3) |
| Prior OAB Treatment (%) None | 34 (48.57) | 28 (38.89) |
| Physical Therapy | 7 (10.00) | 9 (11.11) |
| Medication | 21 (30.0) | 24 (33.33) |
| Bladder (Voiding) Diary | 11 (15.71) | 11 (15.28) |
| Pelvic Floor Exercise/Kegels | 24 (34.29) | 26 (36.11) |
| Bladder Drills/Timed Voids | 3 (4.29) | 6 (8.33) |
| Smokes cigarettes (%) | 7 (10.0) | 6 (8.33) |
| Requires assistance walking (%) | 4 (5.71) | 3 (4.17) |
| Practice any of the following (%) None | 49 (70.00) | 45 (62.50) |
| Meditation | 12 (17.14) | 13 (18.06) |
| Yoga | 8 (11.43) | 16 (22.22) |
| Tai Chi | 0 (0) | 3 (4.17) |
| Acupuncture | 5 (7.14) | 6 (8.33) |
| Pelvic Organ Prolapse Quantitation Stage | ||
| Stage 0 | 17 (24.3) | 8 (11.1) |
| Stage 1 | 22 (31.4) | 23 (31.9) |
| Stage 2 (all points ≤ 0; prolapse does not extend past hymen) | 31 (44.3) | 41 (56.9) |
| Hypnotic Susceptibility (%) Low | 4 (5.7) | 6 (8.3) |
| Medium | 13 (18.6) | 18 (25.0) |
| High | 53 (75.7) | 48 (66.7) |
| Pre-Treatment Expectation: “I expect that my treatment will improve my urinary urgency incontinence.” Range 1–5; 1=strongly disagree, 5=strongly agree (SD) | 4.0 (0.87) | 4.2 (0.87) |
| Overactive Bladder Questionnaire-Short Form (OABq-SF) symptom bother (SD) | 66.88 (21.26) | 66.99 (21.60) |
| Overactive Bladder Questionnaire-Short Form (OABq-SF) quality of life (SD) | 47.11 (27.40) | 50.38 (25.29) |
| Incontinence Severity Index (SD) | 7.14 (3.11) | 7.00 (3.18) |
| Patient Perception of Bladder Condition (SD) | 4.19 (1.20) | 4.25 (0.92) |
| Prolapse Incontinence Sexual Questionnaire-12 (SD) | 85.60 (18.35) | 86.65 (15.10) |
Primary Outcome.
The primary outcome was the difference between treatment group’s percent change in UUIEs on three-day diaries at two months utilizing a modified intention-to-treat analysis.
Secondary Outcomes.
Differences between group’s percent change in UUIEs at six and 12-months were important secondary outcomes. Validated questionnaire and other diary results at 2, 6 and 12 months were other secondary outcomes chosen to support or counter UUIE diary outcome results. Questionnaires included: the Overactive Bladder Short Form questionnaire (OABq-SF),18 Patient Perception of Bladder Condition (PPBC),24 Incontinence Severity Index (ISI),25 and the Prolapse and Incontinence Sexual Questionnaire Short Form (PISQ-12).26 Secondary diary outcomes included >70% change in UUIEs, number of voids and pads, and UUI cure.
Per protocol analysis of change in UUIEs between groups was also performed, comparing differences in UUIEs in those compliant with hypnotherapy or medications. At 2-months, hypnotherapy compliance was defined as ≥60% attendance of hypnotherapy sessions. At six and 12-months, hypnotherapy compliance was defined as answering “yes” to: “Do you perform self-hypnosis or listen to your hypnotherapy recording?” Medication compliance was defined as answering “yes” to: “Are you still taking your medication for urgency urinary incontinence?”
Coordinators reviewed adverse event (AE) occurrence at each study visit and by spontaneous participant report. Medication AEs included constipation, dyspepsia, dry eyes, dry mouth, and voiding difficulties. Hypnotherapy AEs included emotional upset attributable to hypnotherapy interfering with daily activities.
Statistical Analysis.
This study tested whether hypnotherapy was non-inferior to medication. A sample size of 104 women (52/group) provided 80% power with α=0.025 using a one-sided, two-sample t-test, with a non-inferiority margin of 5% to detect a between group difference in percent change in UUIEs of 9%, assuming standard deviations of 25% for each group.21 Assuming 30% loss by 12-month follow-up, 152 participants (approximately 76/group) were required for randomization.
Analyses of differences between group’s percent change in UUIEs for the two-month primary outcome and the 6 and 12-month secondary outcomes were performed based on a modified intention-to-treat. Women with complete diary information at 2, 6 and 12-month time-points were included in the analyses. Analyses were based on participant’s original group assignments. Since missing data were few, imputation was not performed at 6 or 12-months, precluding a strict intention-to-treat analysis.
Exploratory secondary outcomes compared questionnaire results and the other diary parameters using intention-to-treat analysis. Outcomes were evaluated using a linear mixed model with an unstructured covariance pattern. Binary diary parameters, greater than 70% UUIE improvement and restoration of continence, were analyzed with Fisher Exact Test. Per-protocol analyses of group difference in percent change in UUIEs was also performed. The per-protocol analyses included those who complied with treatment and had complete diary information.
The non-inferiority analyses for both the primary UUIE intention-to-treat and the secondary UUIE per-protocol outcomes were based on two-sample t-tests. The data demonstrated skewed distributions with large singularity at 100% change in UUIE. With this distribution, the two sample t-test was not appropriate for analysis; we analyzed these results (between group differences in percent change in UUIEs) using the Exact Mann-Whitney, reporting within group median, first quartile (Q1) and third quartiles (Q3). Because of the skewed distribution of UUIE following treatment, confidence intervals (CI) are reported as medians. The difference in medians between two groups, however, does not correspond to the median difference between individuals in the two groups, which was calculated by the Hodges–Lehmann estimator. The resulting Hodges–Lehman median difference measured the expected benefit associated with membership in the superior group.27 Hypnotherapy was considered non-inferior to medication if the lower bound of the 95% CI for the difference in UUIE percent change compared to medication was > −5%, P<0.025. If the lower bound of the 95% CI was ---−−4.9% or higher (meaning more positive), non-inferiority would be proven; if it was −5.1% or lower (meaning more negative), non-inferiority would not be proven. Hypnotherapy was superior if the confidence limit lower bound was > zero.
Exploratory investigation of covariates identified a priori in the study protocol (pre-treatment expectations and hypnotic susceptibility) was performed. UUIE outcomes were count variables with repeated measures (baseline, 2, 6, 12 months). Count data models using log link were evaluated using Akaike Information Criterion to deal with zero-inflation and over-dispersion. The negative binomial was superior by that criterion. Repeated measures were managed using generalized estimating equations (GEE), with the negative binomial regressions fit using PROC GENMOD in SAS (version 9˖4). This linear mixed model assessed changes from baseline to 2, 6 and 12 months and 95% CIs are reported for the least squares mean (LSM), or adjusted means, and their ratios.
Results
Four hundred seventy women were screened for eligibility, 152 were randomized (74 hypnotherapy, 78 medications) April 2013-October 2016. Of these, 142 (70 hypnotherapy, 72 medications) completed treatment and had UUIE primary outcome information at 2 months; ≥ 90% had UUIE information at 6 and 12-months (Figure 1). Baseline participant characteristics did not differ (Table 1). The average participant was in her 6th decade and obese, had undergone some prior overactive bladder (OAB) therapy, received some college education, and was Non-Hispanic White (Table 1).
Figure 1. Consort Diagram.
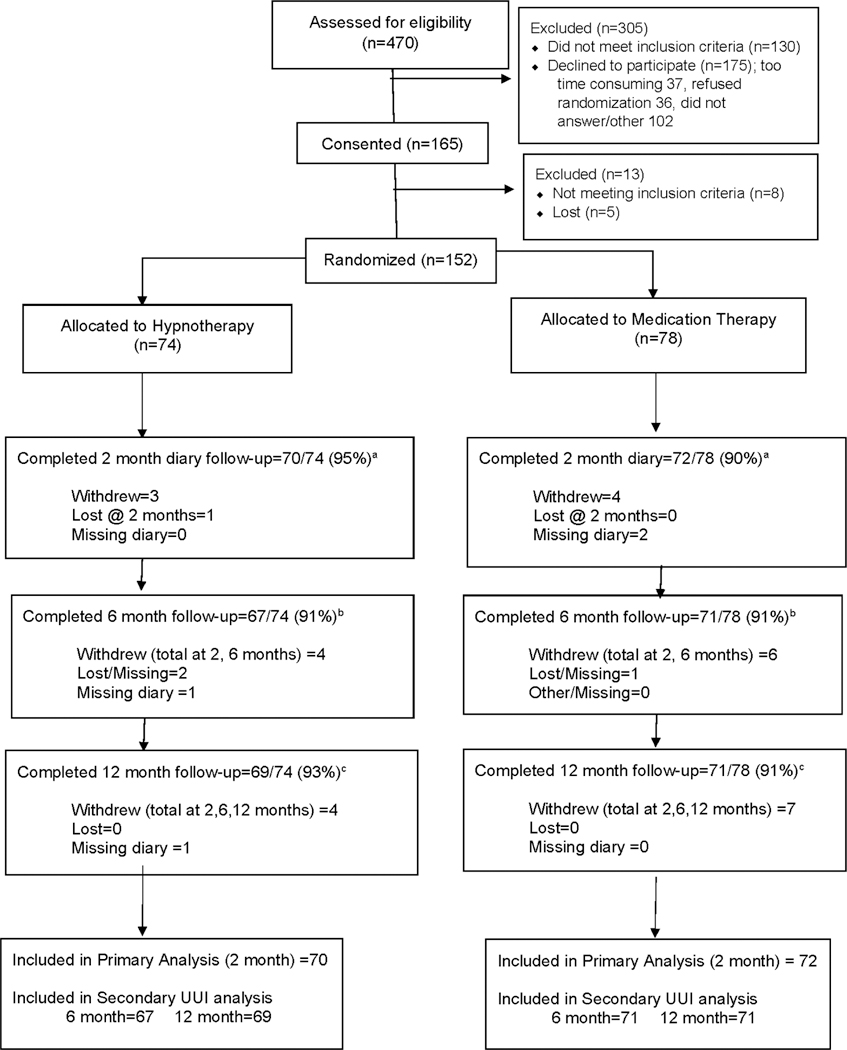
Participant Flow through the Study
The intention-to-treat UUIE outcomes at 2,6 and 12 months are summarized in Table 2 & Appendix Figure 1. Baseline UUIE medians on 3-day diary were similar for hypnotherapy [8 (4,14)] and medications [7 (4,11)]. UUIEs for both groups improved at all time-points. For the 2-month primary outcome, the non-inferiority of hypnotherapy was not proven. Although the median percent change from baseline comparing hypnotherapy and medications was 0% (95% CI −16.7% to 0.0%), the lower bound of the 95% CI was < −5.0%. (Appendix Figure 2 illustrates individual participant’s percent change in UUIEs by treatment group.) The UUIE secondary outcomes at 6 and 12 months, did find hypnotherapy to be non-inferior to medications (Table 2, Appendix Figure 1).
Table 2.
Intention-to-Treat Comparisons UUIa Episodes on 3-day Diary & Percent Change Between Groups
| Hypnotherapy Median UUI Episodes on 3-day diary (Q1,Q3) Median % Change (95% CI)b at follow-up | Pharmacotherapy Median UUI Episodes on 3-day diary (Q1,Q3) Median % Change (95% CI)b at follow-up | Median Difference in % Change between Groupsc,d (95% CI) | Meets Non- Inferiority Criteria e (95% CI Lower Bound > −5%)e | |
|---|---|---|---|---|
| Baseline UUI (N=142) Median UUI Episodes (Q1,Q3) | N=70 8 (4, 14) | N=72 7 (4, 11) | Not Applicable | Not Applicable |
| 2 months UUI (N=142) Median UUI Episodes (Q1,Q3) Median % Change UUI Episodes (95% CI) | N=70 2 (0, 6) 73.0% (60.0%– 88.9%) | N=72 1 (0, 3) 88.6% (78.6% – 100.0%) | 0% (−16.7% – 0.0%) | NO |
| 6 months UUI (N=138) Median UUI Episodes (Q1,Q3) Median % Change UUI Episodes (95% CI) | N=67 1 (0, 4) 85.7% (75.0% – 100.0%) | N=71 1 (0, 4) 83.3% (64.7% – 100.0%) | 0% (0.0% – 6.7%) | YES |
| 12 months UUI (N=140) Median UUI Episodes (Q1,Q3) Median % Change UUI episodes (95% CI) | N=69 1 (0, 3) 85.7% (66.7% – 94.4%) | N=71 1 (0, 6) 80.0% (54.5% – 100.0%) | 0% (−4.7% – 9.5%) | YES |
Urgency Urinary Incontinence
CI=Confidence Interval. Exact Mann-Whitney test used to account for skewed data with many tied values
All within group changes relative to baseline for Exact Test confidence intervals. Hodges-Lehmann estimate of differences between groups can differ from differences between group medians
Median difference in % change= Hypnotherapy % change – Medication % change
The lower bound (i.e. smaller number noted in 95% CI) of the difference in Hypnotherapy % change – Medication % change must be >− 5% in order to meet the non-inferiority criteria. For example, −5.1% for the lower bound would mean that hypnotherapy did not meet the non-inferiority criteria; −4.9% would mean that hypnotherapy did meet the non-inferiority criteria
Exploratory secondary outcomes included the questionnaire (Table 3) and UUIE per-protocol (Appendix Table 1) results. The per-protocol analysis found hypnotherapy to be non-inferior in reduction of UUIEs at 2, 6 and 12 months. There were no differences between groups regarding questionnaire results when adjusted for baseline.
Table 3.
Questionnaires, Diary & Compliance Results
| Hypnotherapy | Pharmacotherapy | P | Estimated Group Difference (95% CI)a | |
|---|---|---|---|---|
| Overactive Bladder questionnaire-Short Form Symptom Botherb Scores | ||||
| Baseline Mean (CI) | 66.88 (61.81–71.94) | 66.99 (62.92–72.07) | 0.97 | −0.11 (−7.23–7.00) |
| 2 months Meansc (CI) | 38.17 (30.19–46.14) | 35.33 (28.64–42.02) | 0.59 | 2.84 (−7.58–13.25) |
| 6 months Meansc (CI) | 34.61 (26.26–42.96) | 27.93 (20.66–35.20) | 0.24 | 6.68 (−4.39–17.76) |
| 12 months Meansc (CI) | 32.27 (22.89–41.66) | 30.74 (22.53–38.95) | 0.81 | 1.53 (−10.94–14.00) |
| Overactive Bladder questionnaire-Short Form Quality of Lifed Scores | ||||
| Baseline Mean (CI) | 47.11 (40.58–53.65) | 50.38 (44.39–56.36) | 0.46 | −3.26 (−12.04–5.52) |
| 2 months Meansc (CI) | 73.96 (66.93–81.00) | 74.86 (68.96–80.76) | 0.85 | −0.90 (−10.08–8.28) |
| 6 months Meansc (CI) | 75.85 (68.24–83.46) | 80.19 (73.63–86.75) | 0.40 | −4.34 (−14.39–5.72) |
| 12 months Meansc (CI) | 75.71 (68.07–83.35) | 81.57 (74.91–88.23) | 0.26 | −5.86 (−16.00–4.28) |
| Incontinence Severity Indexe Scores | ||||
| Baseline Mean (CI) | 7.14 (6.40–7.88) | 7.00 (6.25–7.75) | 0.79 | 0.14 (2.82–3.56) |
| 2 months Meansc (CI) | 4.74 (3.54–5.94) | 5.18 (4.17–6.19) | 0.58 | −0.44 (−2.01–1.12) |
| 6 months Meansc (CI) | 4.87 (3.60–6.13) | 4.69 (3.58–5.79) | 0.83 | 0.18 (−1.50–1.86) |
| 12 months Meansc (CI) | 3.64 (2.52–4.76) | 3.33 (2.34–4.31) | 0.67 | 0.32 (−1.17–1.81) |
| Patient Perception Bladder Conditionsf Scores | ||||
| Baseline Mean (CI) | 4.19 (3.90–4.47) | 4.25 (4.03–4.47) | 0.72 | −0.06 (−0.42–0.29) |
| 2 months Meansc (CI) | 3.19 (2.75–3.64) | 3.35 (2.98–3.72) | 0.59 | −0.16 (−0.74–0.42) |
| 6 months Meansc (CI) | 3.12 (2.67–3.58) | 2.71 (2.31–3.10) | 0.17 | 0.42 (−0.19–1.02) |
| 12 months Meansc (CI) | 2.93 (2.46–3.40) | 2.65 (2.24–3.06) | 0.37 | 0.29 (−0.34–0.91) |
| Prolapse & Incontinence Sexual Questionnaire-12g Scores | ||||
| Baseline Mean (CI) | 85.60 (79.57–91.62) | 86.65 (81.69–91.62) | 0.99 | 0.065 (−7.71–7.84) |
| 2 months Meansc (CI) | 93.08 (85.29–100.86) | 91.58 (84.58–98.59) | 0.77 | 1.50 (−6.48–14.64) |
| 6 months Meansc (CI) | 92.73 (84.33–101.13) | 89.00 (81.92–96.08) | 0.50 | 3.73 (−7.29–14.75) |
| 12 months Meansc (CI) | 93.74 (86.45–101.05) | 92.36 (85.84–98.89) | 0.78 | 1.39 (−8.43–11.22) |
| # Pads on 3-day diary | ||||
| Baseline Mean (CI) | 5.52 (4.06–6.98) | 4.63 (3.57–5.70) | 0.33 | 0.89 (−0.89–2.67) |
| 2 months Meansc (CI) | 3.57 (2.37–4.77) | 2.74 (1.82–3.66) | 0.28 | 0.83 (−0.67–2.33) |
| 6 months Meansc (CI) | 3.01 (1.87–4.16) | 2.63 (1.85–3.40) | 0.58 | 0.38 (−0.99–1.76) |
| 12 months Meansc (CI) | 3.46 (2.07–4.84) | 3.07 (2.13–4.01) | 0.65 | 0.39 (−1.28–2.05) |
| # Voids on 3-day diary | ||||
| Baseline Mean (CI) | 29.07 (27.06–31.08) | 29.19 (27.14–31.24) | 0.94 | −0.12 (−2.97–2.73) |
| 2 months Meansc (CI) | 26.4 (24.29–28.59) | 25.35 (23.59–27.12) | 0.44 | 1.08 (−1.67–3.85) |
| 6 months Meansc (CI) | 25.58 (23.48–27.68) | 24.28 (22.69–25.87) | 0.32 | 1.30 (−1.31–3.91) |
| 12 months Meansc (CI) | 25.74 (23.69–27.79) | 25.37 (23.71–27.02) | 0.78 | 0.37 (−2.24–2.99) |
| > 70% improvement of Urgency Urinary Incontinence | ||||
| 2 months N (%)(CI) | 60 (86%)(CI 75–93%) | 59 (82%; CI 71%–90%) | 0.65 | OR 0.76 (0.27–2.04)h |
| 6 months N (%)(CI) | 55 (82%)(CI 71–90%) | 58 (82%; CI 71%–90%) | 1.00 | OR 1.05 (0.40–2.81)h |
| 12 months N (%)(CI) | 54 (78%)(CI 67–87%) | 53 (75%; CI 63%–84% | 0.69 | OR 0.81 (0.33–1.94)h |
| Continent (No UUI on diary) | ||||
| At 2 months N (%)(CI) | 24 (34%)(CI 23–47%) | 30 (42%; CI 30–54%) | 0.39 | OR 1.4 (0.66–2.86)h |
| At 6 months N (%)(CI) | 29 (43%)(CI 31–56%) | 28 (39%; CI 28–52%) | 0.73 | OR 0.85 (0.41–1.78)h |
| At 12 months N (%)(CI) | 25 (36%)(CI 25–49%) | 30 (42%; CI 31–55%) | 0.49 | OR 1.3 (0.62–2.69)h |
| No UUI at all follow-up N (%;CI) | 11 (16%)(CI 8.–27%) | 16 (23%; CI 14–34%) | 0.39 | OR 1.5 (0.60–4.00)h |
| Treatment Compliance | ||||
| At 2 months N (%)(CI) | 67/70 (96%) | 61/72 (85%) | 0.63 | OR 1.13 (0.68–1.87)h |
| At 6 months N (%)(CI) | 54/67 (81%) | 55/71 (77%) | 0.90 | OR 1.04 (0.61–1.77)h |
| At 12 months N (%)(CI) | 53/69 (77%) | 47/71 (66%) | 0.60 | OR 1.16 (0.67–2.00)h |
Estimated group differences & 95% Confidence Intervals (CI) were derived using linear mixed models. .
Validated questionnaire reflecting symptoms. Higher scores indicate more symptoms; higher scores are worse. Score range 0–100. < 2% missing data
Adjusted Means
Validated questionnaire reflecting quality of life. Higher scores indicate better quality of life: higher scores are better. Score range 0–100. <1% missing data
Validated index. Higher scores indicate greater incontinence severity. Score range 1–12. 2% missing data
Validated global scale regarding patient’s perception of the severity of their bladder condition. Lower scores are better, Higher scores are worse. Score range=1–6. No missing data
Validated sexual function questionnaire in women with prolapse or incontinence. Higher scores are better. Range=0–123. Only administered to women having heterosexual relations in the last 6 months (33 women in each group: met criteria and answered these questions).
Odds ratios (OR) & 95% Confidence Intervals (CI) based on Fisher’s Exact test
We also explored the impact of baseline UUIEs and hypnotic susceptibility on outcomes. Repeated measures regression analysis indicated that follow-up UUIEs were associated with number of UUIEs at baseline (P < 0.0001), and that a group X time X hypnotic susceptibility 3-way interaction existed (P < 0.0001). UUIE counts at all time-points were integrated into the regression model. UUIE adjusted means, controlling for baseline UUIE, were calculated for the nine levels representing time (2, 6, 12 months) X hypnotic susceptibility (low, medium, high). Adjusted results suggested that change in UUIE between groups differed at various time-points and depended on participant’s hypnotic susceptibility (Appendix Table 2, Appendix Figure 3). In this model at 6 months, among medium hypnotic susceptibility participants, hypnotherapy was superior to medication. At 12 months, among high hypnotic susceptibility participants, hypnotherapy was superior to medication. In these participants, UUIE improved between 2–12 months in the hypnotherapy group (LSM decreased from 2.35 to 2.10) but worsened in the medication group (LSM increased from 1.61 to 3.74). The difference in these trends was significant (P = 0.0002, point estimate 2.60, 95% CI 1.56–4.34).
Of 152 randomized women, 62 (40.8%) reported at least one AE: 25 hypnotherapy, 34 medications. Medication participants reported anticipated AEs 12 times. No hypnotherapy participant reported the anticipated AE of severe emotional upset. Both groups reported the following AEs: urinary tract infection (six medications, five hypnotherapy), falls (five medications, three hypnotherapy), headache (three medications, three hypnotherapy), and back pain (four medications, three hypnotherapy). Four Serious AEs (three medications, one hypnotherapy) occurred, likely unrelated to treatment: hospitalizations for pre-existing disease (three), a fall horseback-riding (one).
Comment
Main Findings
This study found that hypnotherapy and medications were both associated with markedly reduced UUIEs, although when comparing hypnotherapy to medications, hypnotherapy was not found non-inferior to medications at the two-month, primary endpoint. Hypnotherapy did attain non-inferiority at the secondary 6 and 12-month endpoints. Thus, hypnotherapy and medications were both associated with substantially decreased UUIEs and these decreases were sustained over time.
Clinical Implications
Hypnotherapy and medications were both associated with decreased UUIEs. Notably, both groups were associated with a > 70% decrease in UUIEs, a previously identified point at which women report enhanced quality of life and treatment satisfaction.10 Over three-quarters of women maintained this meaningful change for 12months. Secondary outcomes (questionnaires, other diary data and the per-protocol analysis) further supported the comparative effectiveness of the treatments; participants in both groups experienced similar improvement at all time-points.
Exploratory repeated measures regression analysis suggested that hypnotic susceptibility affected the results for both interventions. Both treatments were associated with improved UUIEs in medium and high hypnotic susceptibility participants (>90% of participants). Among low hypnotic susceptibility participants (7% of participants), trends in UUI improvement favored medications, suggesting hypnotherapy may be less efficacious in this sub-group.
Both groups’ high treatment continuation rates were unexpected. Individualized UUI education and 2-months of weekly contact may have improved continuation. Although for UUI, patient education and individualized follow-up are routinely recommended,28 the attention provided to study participants may have exceeded that provided in clinical practice, enhancing treatment continuation. Approximately 75% of hypnotherapy and 66% of medication participants continued treatment at one year. In contrast, database studies have reported 1-year medication continuation rates of 10%25%.29,30 Implications for routine UUI care with medications seem clear; augmenting medications with education and individualized follow-up likely improves medication continuation and efficacy.29,31 Hypnotherapy continuation was also high. Audio-recordings encouraging self-hypnosis practice may have improved this behavioral intervention’s continuation. The importance of personal contact and follow-up in UUI, though difficult to measure, conceivably contributed to the success of both treatments.
Scant literature exists regarding hypnotherapy’s efficacy in OAB and/or UUI. A pilot study compared hypnotherapy to behavioral therapy in women with OAB (with or without incontinence); hypnotherapy had greater global improvement in OAB symptoms.13 The lone report describing hypnotherapy in women with UUI (i.e. OAB with incontinence), to our knowledge, has been that of Freeman.12 That case series of 50 women found that following UUI-directed hypnotherapy, 60% were cured, 28% improved and 14% unchanged.12 At 6-months, 86% continued to be cured/improved. The current trial further strengthens existing evidence that hypnotherapy is associated with UUI improvement, and that these associations are durable. Similar to Freeman’s study, this trial found that hypnotherapy was associated with a 73% median improvement in UUIEs at 2-months. However, its non-inferiority to medications was not proven as medications were associated with 88.3% improvement. At 6 and 12-months, hypnotherapy was non-inferior to medications and both treatments maintained ≥ 80% improvement. Hypnotherapy’s UUIE improvement, compared to medication, occurred later and remained stable at 1 year.
This study indicates that UUI-directed hypnotherapy is associated with improved UUI despite its uncertain mechanism of action. Emotional distress frequently accompanies UUI,2 potentially manifesting as enhanced sensory sensitivity.32,33 Whether hypnotherapy affects UUI’s emotional distress, tempers UUI’s enhanced sensory sensitivity or acts by other means, remains unknown. Functional Magnetic Resonance Imaging (fMRI) during hypnotic induction has suggested increased interaction between the attentional component of the executive network and the salience, or interoceptive network 34,35,36 Interestingly, fMRI of UUI patients suggests that interaction between the executive and interoceptive areas of the brain (responsible for interpretation of physiologic stimuli within the body) may underlie the response of UUI to physical therapy.37,38 Although little is known about hypnotherapy’s brain-related effects outside the hypnotic state, we postulate that hypnotherapy modulates output received from afferents via central brain mechanisms.
This study did not prove the non-inferiority of hypnotherapy to medications at 2 months, but did prove non-inferiority at 6 and 12 months. This may reflect an association between hypnotherapy and UUI improvement that increases over time. Other mind-body studies have also shown a similar trend. A randomized trial of patients with chronic back pain compared two mind-body therapies, Mindfulness Based Stress Reduction (MBSR) and Cognitive Behavioral Therapy (CBT), to usual care.39 Groups did not differ in pain reduction at 2 months, but both mind-body treatment groups demonstrated greater improvement at 6 and 12 months compared to controls. An IBS trial randomized women to 8 weeks of mindfulness training or to a control group with follow-up at 2 and 3 months.15 Not only were mindfulness group findings superior to controls, improvement within the mindfulness group increased between 2 and 3 months. Repeated measures regression analysis performed in the current hypnotherapy study also demonstrated a group × time difference in UUIEs. In patients with moderate-high hypnotic susceptibility (94% of the cohort), UUI improvement increased between two and 6–12 months, a pattern not demonstrated by medications. This supports the supposition that symptom improvement associated with hypnotherapy increases over time. Perhaps brain remodeling potentially associated with mind-body therapies requires additional time in order to exert its effect. In aggregate, both prior work and our data suggest these therapies may be associated with continued symptom improvement over longer duration. This may have resulted in hypnotherapy’s comparative non-inferiority at longer-term, but not initial, follow-up.
Study Strengths & Weaknesses
This study is one of few evaluating hypnotherapy in UUI, and its results support its use as an alternative UUI treatment. This study’s novelty notwithstanding, its limitations warrant acknowledgement. First, participants were not masked to treatment, potentially biasing treatment results. However, since both groups had high pre-treatment expectations, this potential bias did not favor one treatment over another. Additionally, participants willing to engage in a one-year trial may be more committed to treatment success than typical patients. Study strengths include its innovative use of a mind-body therapy compared to accepted therapy in treating UUI, treatment standardization, treatment fidelity monitoring, and its high participant retention at 1-year.
Conclusion
In summary, although both hypnotherapy and medications were associated with markedly improved symptoms in women with non-neurogenic UUI, at two-months, the non-inferiority of hypnotherapy compared to medications was unproven. Hypnotherapy did compare favorably to medications at longer term follow-up. This study, which we believe is the first randomized trial evaluating bladder-directed hypnotherapy versus standard pharmacotherapy, provides evidence that hypnotherapy offers an alternative, underutilized treatment for UUI. The findings also suggest that hypnotherapy’s comparative efficacy in treating UUI may improve over time.
Condensation:
This study found that medications and hypnotherapy were both associated with substantial decreases in urgency incontinence, supporting hypnotherapy’s use as an effective, alternative treatment for this condition.
AJOG at a Glance:
Urgency urinary incontinence is common and emotionally distressing. Side effects and non-adherence may limit efficacy of medications, a standard treatment. Our study’s objective was to study the use of hypnotherapy, an alternative mind-body intervention, in treating women with urgency urinary incontinence.
This non-inferiority trial compared the efficacy of hypnotherapy to medications in women with urgency urinary incontinence. Although both treatments improved urgency incontinence, the study did not prove hypnotherapy’s non-inferiority to medications at 2 months (study’s primary outcome). Study findings did prove hypnotherapy’s non-inferiority to medications at 6 and 12 months.
Findings from this randomized trial, one of the first comparing hypnotherapy to pharmacotherapy, supports the use of hypnotherapy in women with urgency urinary incontinence. Hypnotherapy offers a potential alternative treatment for this condition.
Acknowledgements:
Thank-you to the research coordinators, clinicians & patients who made this work possible, including Kathy Hopkins, Cassandra Castaneda-Darley BA, Karen Taylor BA, Elizabeth Medrano RN, Julia Middendorf BSN, Cynthia Wenzel BA, Gena Dunivan MD, Peter Jeppson MD, Sara Cichowski MD, Cara Ninivaggio MD, Gregg Kanter MD & Kate Meriwether MD
Financial Support/Funding Source & Sponsor’s Role:
National Center for Complementary & Integrative Health, National Institutes of Health, Award Number R01AT007171
The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
The authors report the following potential conflicts of interest:
Drs. Komesu, Ketai, Rogers, Sapien, Schrader & Mayer received support from above NIH grant. The authors below have the additional disclosures:
Yuko Komesu MD: Other NIH grants. Site PI for CookMyosite® CELLEBRATE trial Rebecca Rogers MD: Other NIH grants, UpToDate royalties, ABOG & ACOG travel & stipend, International Urogynecologic Association travel and stipend and editorship. Robert Sapien MD: International Board of Hypnotherapy President, Global Hypnotherapy Advancement Foundation, Sapien Wellness LLC, It’s Mental LLC.
Andrew Mayer PhD: Other NIH grants
Appendix Figure 1. Differences in Hypnotherapy versus Pharmacotherapy at 2, 6 & 12 months.
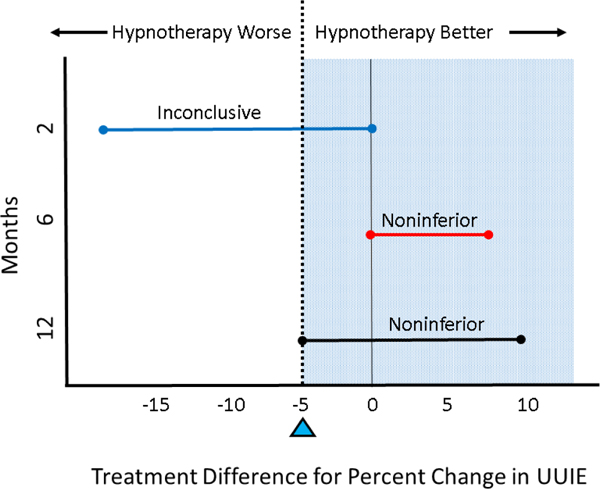
Error bars indicate 95% Confidence Intervals. Dashed line indicates the non-inferiority margin. Treatments whose error bars lie wholly to the right of the dashed line, within the blue tinted area, are non-inferior. Only treatments whose error bars are wholly to the right of the dashed line and do not include zero can be considered superior. Difference between treatments is nonsignificant if error bars include both the non-inferiority margin and zero, but result is inconclusive regarding non-inferiority. At 2 months, hypnotherapy was not non-inferior to Pharmacotherapy and findings were in the inconclusive range. At 6 & 12 months, hypnotherapy was found non-inferior to pharmacotherapy.
Appendix Figure 2. Percent change in UUIEs for Individual Participants.
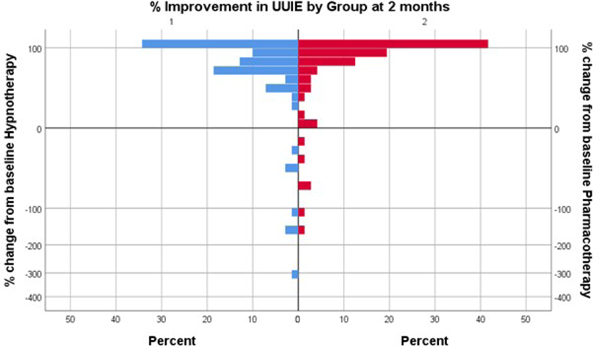
Histogram of % UUIE change on 3-day diary from baseline to 2 months using an exponent transformed (square root) scale. Hypnotherapy results represented in blue and Medications in red. Top bar represents those patients with UUI cure, 100% reduction in UUIE from baseline. Histogram bars below zero represent patients whose UUIE worsened. (One patient in each group had less than −500% improvement, and are not displayed on this graph.)
Appendix Figure 3. Regression analysis 2,6 & 12 months.
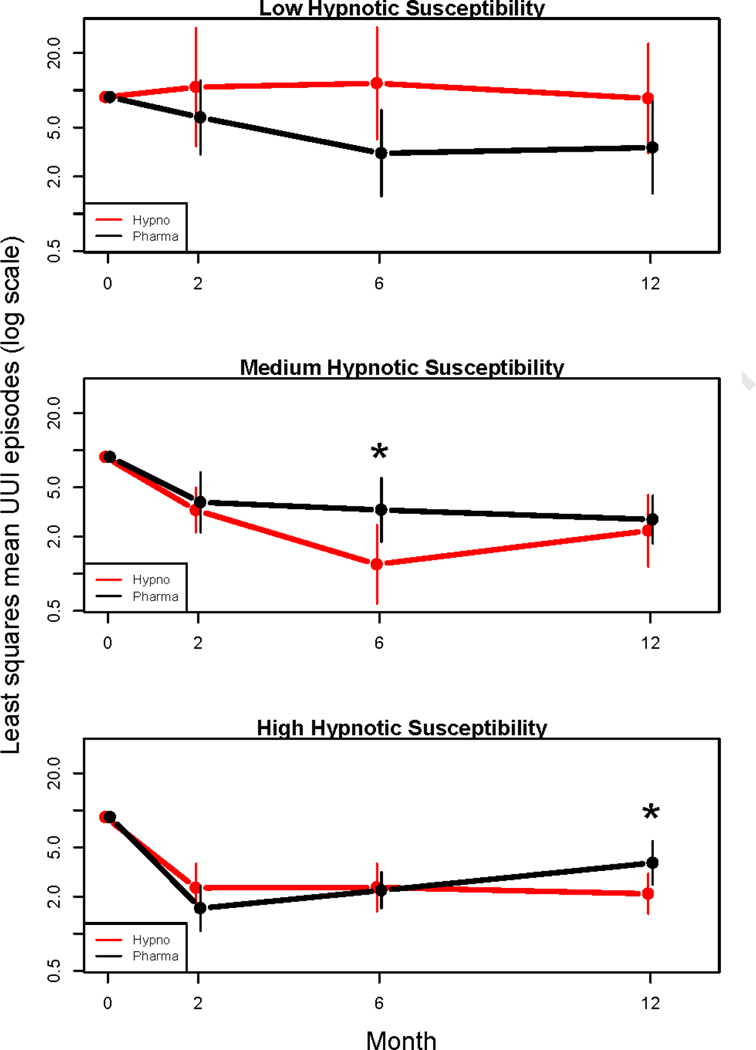
Adjusted means results for months 2, 6 & 12, stratified by hypnotic susceptibility. Least squares means calculated by negative binomial regression adjusting for baseline UUI episodes and hypnotic susceptibility. Vertical lines represent 95% CIs. Each least squares mean is calculated using an overall average baseline value of 8.8 UUI episodes on three-day voiding diary. Asterisk (*) indicates significant group difference (p < 0.05); because of correlation structure the individual confidence intervals may overlap slightly while the test for difference is significant.
Appendix Table 1.
Overview of Interventions
| Weeks 1–8 | Hypnotherapy | Pharmacotherapy |
|---|---|---|
| Week #1 | Give study overview, explain bladder physiology, UUI pathophysiology, hypnotherapy principles. Participants discuss any fears/concerns regarding interventions. Patients set goals for this session. Perform hypnosis; induction & progressive relaxation/deepening/ therapeutic suggestions/terminate hypnosis. Debrief. | Give study overview, explain bladder physiology, UUI pathophysiology, discuss medications & mechanism of action. Participants discuss any fears/concerns regarding interventions. Medication instructions given and medication dispensed. |
| Week #2 | Review change/persistence in UUI symptoms & prior week’s experiences, address UUI associated emotions/life impact, introduce self-hypnosis.Proceed with hypnosis/debrief (See Week #1). | Review change/persistence in UUI symptoms & prior week’s experiences, tolerability of meds discussed. Coping mechanisms re: side effects discussed. If needed, arrangements made for medication change. |
| Week #3 | Identify emotional triggers or responses associated based on self-discovery of emotional/physical connection with UUI & develop positive actions to deal with these emotions. Proceed with hypnosis/debrief (See Week #1). | Review change/persistence in UUI symptoms& prior week’s experiences, discuss tolerability of medications. Coping mechanisms re: side effects discussed. If needed, arrangements made for medication change. |
| Week #4 | Assist participant develop therapeutic suggestions & imagery to cope with UUI. Proceed with hypnosis/debrief (See Week #1). | Same as above.Medication instructions given and medication dispensed. |
| Week #5 | Provide digital recording for participant; specifically prepared for patient & for hypnotherapy home practice (based on work from week #4, emphasizes ego strengthening). Patients develop own therapeutic suggestions to reverse UUI after identifying beliefs that limit their bladder health. Proceed with hypnosis/debrief (See Week #1). | Same as Week #3. |
| Week #6 | Have participant reflect on their past (including responses resulting in current UUI associated behavior; consider how to alter this behavior). Proceed with hypnosis/debrief (See Week #1). | Discuss urgency incontinence triggers & participant encouraged to develop coping mechanisms. Same as above. |
| Week #7 | Focus on integration of resources developed through hypnotherapy to improve UUI & overall health, countering negative emotions/responses related to emotional & physical connections.Proceed with hypnosis/debrief (See Week #1). | Same as above. |
| Week #8 | Focus on healing imagery & continuation of self-hypnosis. Proceed with hypnosis/debrief (See Week #1). | Same as above. Interventionist discusses potential setbacks & emphasizes these are temporary. Medication side effects & copingmechanisms reviewed. Medications dispensed. |
Table 2 Appendix.
Per-Protocol Between Group Comparisons: Median UUIa Episodes on 3 day diary & Percent
| Hypnotherapy Median UUI Episodes on 3 day diary (Q1,Q3) Median % Change (95% CI)b | Pharmacotherapy Median UUI Episodes on 3 day diary (Q1,Q3) Median % Change (95% CI)b | Median Difference in % Change Between Groupsc,d(95% CI) | Meets Non-Inferiority Criteriae(95% CI Lower Bound > − 5%)e | |
|---|---|---|---|---|
| Change Between Groups | ||||
| Baseline UUI (N=142) Median UUI Episodes (Q1,Q3) | N=67 8 (4, 12.5) | N=61 7 (4, 11) | Not Applicable | Not Applicable |
| 2 months UUI (N=128) Median UUI Episodes (Q1,Q3) Median % Change UUI episodes (95% CI) | N=67 1 (0, 5) 75.0% (62.5% to 88.9%) | N=61 1 (0, 3) 88.9% (83.3% to 100.0%) | 0% (−2.0% to 1.0%) | YES |
| 6 months UUI (N=109) Median UUI Episodes (Q1,Q3) Median % Change UUI episodes (95% CI) | N=54 1 (0, 3) 93.7% (81.8% to 100.0%) | N=55 1 (0, 4) 83.3% (64.7% to 100.0%) | −2.0% (−4.0% to 0.0%) | YES |
| 12 months UUI (N=100) Median UUI Episodes (Q1,Q3) Median % Change UUI episodes (95% CI) | N=53 1 (0, 3) 85.7% (66.7% to 93.8%) | N=47 1 (0, 5.5) 87.5% (54.5% to 100.0%) | −2.0% (−4.0% to 1.0%) | YES |
Urgency Urinary Incontinence
CI=Confidence Interval. Exact Mann-Whitney test used to account for skewed data with many tied values
All within group changes relative to baseline for Exact Test confidence intervals. Hodges-Lehmann estimate of differences between groups can differ from differences between group medians.
Median difference in % change= Hypnotherapy % change – Medication % change
Lower bound (i.e. smaller number of 95% CI) of difference in Hypnotherapy % change – Medication % change must be >− 5% to meet the non-inferiority criteria. For example, −6% for the lower bound would mean that hypnotherapy did not meet the non-inferiority criteria; −4.9% would mean that hypnotherapy did meet the non-inferiority criteria
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Study registered with ClinicalTrials.gov; https://clinicaltrials.gov ID#: NCT01829425
References
- 1.Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodynam. 2010;29:4–20. PMID: 19941278. [DOI] [PubMed] [Google Scholar]
- 2.Coyne KS, Wein AJ, Tubaro A, et al. The burden of lower urinary tract symptoms: evaluating the effect of LUTS on health-related quality of life, anxiety and depression: EpiLUTS. BJUI. 2009;103(3):411. PMID: 19302497. [DOI] [PubMed] [Google Scholar]
- 3.Sexton CC, Coyne KS, Vats V, et al. Impact of overactive bladder on work productivity in the United States: Results from EpiLUTS. Am J Manag Care. 2009;15(4 Suppl):S98–107. PMID: 19355804. [PubMed] [Google Scholar]
- 4.D’Souza AO, Smith MJ, Miller LA, Doyle J, Ariely R. Persistence, adherence, and switch rates among extended-release and immediate-release overactive bladder medications in regional managed care plan. J Manag Care Pharm. 2008;14(3):291301. PMID: 18439051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hubbard CS, Hong J, Jiang Z, Ebrat B, Suyenobu B, Smith S. et al. Increased attentional network functioning related to symptom severity measures in females with irritable bowel syndrome. Neurogastroenterol Motil. 2015;27(9):1282–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Larsson MB, Tillisch K, Craig AD, Engström M, Labus J, Naliboff B, et al. Brain responses to visceral stimuli reflect visceral sensitivity thresholds in patients with irritable bowel syndrome. Gastroenterology 2012;142(3):463–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Griffiths D, Derbyshire S, Stenger A, Resnik N. Brain control of normal and overactive bladder. J Urol. 2005;174(5):1862–7. [DOI] [PubMed] [Google Scholar]
- 8.Nardos R, Karstens L, Carpenter S, Aykes K, Krisky C, Stevens C, et al. Abnormal functional connectivity in women with urgency urinary incontinence: Can we predict disease presence and severity in individual women using Rs-fcMRI. Neurourol Urodyn. 2015. May 1.doi: 10.1002/nau.22767. [DOI] [PubMed] [Google Scholar]
- 9.Komesu YM, Ketai LH, Mayer AR, Teshiba TM, Rogers RG. Functional MRI of the Brain in Women with Overactive Bladder: Brain Activation During Urinary Urgency. Female Pelvic Med Reconstr Surg. 2011;17(1):50–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shamliyan T, Wyman J, Kane RL. Nonsurgical Treatments for Urinary Incontinence in Adult Women: Diagnosis and Comparative Effectiveness Comparative Effectiveness Review No. 35. (Prepared byt the University of Minnesota Evidence-based Practice Center under Contract No. HHSA 290–2007-10064-I). AHRQ Publication No. 11 (12)EHC074-EF. Rockville, MD: Agency for Healthcare Research and Quality; April 2012. Available at:www.effetivehealthcare.ahrq.gov/reports/final.cfm. [PubMed] [Google Scholar]
- 11.Falci L, Shi Z, Greenlee H. Multiple Chronic Conditions and Use of Complementary and Alternative Medicine Among US Adults: Results From the 2012 National Health Interview Survey. Prev Chronic Dis 2016;13:150501. DOI: 10.5888/pcd13.150501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Freeman RM, Baxby K. Hypnotherapy for incontinence caused by the unstable detrusor. Br Med J. 1982;284(6332):1831–4. PMID: 6805716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Komesu YM, Sapien RE, Rogers RG, Ketai LH. Hypnotherapy for treatment of overactive bladder: a randomized controlled trial pilot study. Female Pelvic Med Reconstr Surg 2011;17(6):308–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.https://www.apa.org/topics/hypnosis/ American Psychological Association website accessed July 1, 2019.
- 15.Gaylord SA, Palsson OS, Garland EL, Faurot KR. Coble RS, Mann JD et al. Mindfulness Training Reduces the Severity of Irritable Bowel Syndrome in Women: Results of a Randomized Controlled Trial. Am J Gastroenterol 2011;106:1678–1688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Flik CE, Laan W, Zuithoff NPA, VanRood YR, Smout AJPM, Weusten BLAM et al. Efficacy of individual and group hypnotherapy in irritable bowel syndrome (IMAGINE): a multicentre randomized controlled trial. Lancet Gastroenterol [DOI] [PubMed] [Google Scholar]
- 17.Komesu YM, Rogers RG, Sapien RE, Schrader RM, Simmerman-Sierra T, Ketai LH. Methodology for a Trial of Brain-Centered versus Anti-cholinergic Therapy for Women with Urgency Urinary Incontinence. Int Urogynecol J. 2017;28(6):865–874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Coyne K, Revicki D, Hunt T, et al. Psychometric validation of an overactive bladder symptom and health-related quality of life questionnaire: The OAB-q. Quality of Life Research. 2002;11(6):563–74. PMID: 12206577 [DOI] [PubMed] [Google Scholar]
- 19.Visco AG, Brubaker L, Richter HE, Nygaard I, Paraiso MF, Menefee SA, Schaffer J, Lowder J, Khandwala S, SIrls L, Spino C, Nolen TL, Wallace D, Meikle SF for the Pelvic Floor Disorders Network. Anticholinergic Therapy vs. OnabotulinumtoxinA for Urgency Urinary Incontinence. JAMA 2012;367:1803–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Diokno AC, Appell RA, Sand PK, Dmochowski RR, Gburek BM, Klimberg IW. Kell SH for the OPERA Study Group. Prospective, Randomized, Double-Blind Study of the Efficacy and Tolerability of the Extended-Release Formulations of Oxybutynin and Tolterodine for Overactive Bladder: Results of the OPERA Trial. Mayo Clin Proc 2003;78:687–695. [DOI] [PubMed] [Google Scholar]
- 21.Burgio KL, Locher JL, Good PS, et al. Behavioral vs. drug treatment for urge urinary incontinence in older women. A randomized controlled trial. JAMA. 1998;280:1995–2000. PMID: 9863850 [DOI] [PubMed] [Google Scholar]
- 22.Hilgard ER, Weitzenhoffer AM, Gough P. Individual Differences in Susceptibility to Hypnosis. Proc Natl Acad Sci USA 1958;44(12):1255–9. Scale Available at: http://www.leevonk.com/information/Hypnosis/Stanford%20Hypnotic%20Susceptibility%20Scale.pdf (last accessed 7/31/2018) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Evans FJ, Schmeidler D. Relationship between the Harvard Group Scale of hypnotic susceptibility and the Stanford Hypnotic Susceptibility Scale; form C1. Int J Clin Exp Hypno. 1966;14(4):333–43. [DOI] [PubMed] [Google Scholar]
- 24.Matza LS, Thompson CL, Krasnow J, Brewster-Jordan J, Zyczynski T, Coyne KS. Patient Perception of Bladder Condition (PPBC), Urgency Questionnaire (UQ), and the Primary OAB Symptom Questionnaire (POSQ). Neurourol and Urodyn 2005; 24:215–25. [DOI] [PubMed] [Google Scholar]
- 25.Sandvik H, Espuna M, Hunskar S. Validity of the incontinence severity index: comparison with pad-weighing tests. Int Urogynecol J 2006;17:520–524. [DOI] [PubMed] [Google Scholar]
- 26.Rogers RG, Coates KW, Kammerer-Doak D, Khalsa S, Qualls C. A short form of the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12). Int Urogynecol J 2003;14:164–168. [DOI] [PubMed] [Google Scholar]
- 27.Conroy RM. What hypotheses do “nonparametric” two-group tests actually test? The Stata Journal 2012;12(2):182–90. [Google Scholar]
- 28.Gormley EA, Lightner DJ, Faraday M, Vasavada SP. Diagnosis and Treatment of Overactive Bladder (Non-Neurogenic) in Adults: AUA/SUFU Guideline Amendment. J Urol 2015;193;15721580. [DOI] [PubMed] [Google Scholar]
- 29.Sexton CC, Notte SM, Maroulis C, Dmochowski RR, Cardozo L, Subramanian D, Coyne KS. Persistence and adherence in the treatment of overactive bladder syndrome with anticholinergic therapy: a systematic review of the literature. Int J of Clin Pract 2011; 65(5):567–585. [DOI] [PubMed] [Google Scholar]
- 30.Chapple CR, Nazir J, Hakimi Z, Bowditch S, Fatoye F, Guelfucci F, Khemiri A, Siddiqui E, Wagg A. Persistence and Adherence with Mirabegron versus Antimuscarinic Agents in Patients with Overactive Bladder; A Retrospective Observational Study in UK Clinical Practice. Euro Urol 2017;72:389–399 [DOI] [PubMed] [Google Scholar]
- 31.Dhaliwal P, Wagg A. Overactive bladder: strategies to ensure treatment compliance and adherence. Clinical Interventions in Aging 2015;11:755–760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yamaguchi O, Honda K, Nomiya M, Shishido K, Kakizaki H, Tanka H et al. Defining Overactive Bladder as Hypersensitivity. Neurorul and Urodyn. 2007;27:904–907. [DOI] [PubMed] [Google Scholar]
- 33.Homma Y OAB symptoms: assessment and discriminator for etiopathology. Curr Opin Urol 2014;24(4):345–51. [DOI] [PubMed] [Google Scholar]; Jiang H, White MP, Greicius MD, Waelde LC, Spiegel D. Brain Activity and Functional Connectivity Associated with Hypnosis. Cereb Cortex 2017;27(8):4083–4093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jiang H, White MP, Greicius MD, Waelde LC, Spiegel D. Brain Activity and Functional Connectivity Associated with Hypnosis. Cereb Cortex 2017;27(8):4083–4093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Faymonville M, Laureys S, Degueldre C. Neural mechanisms of antinociceptive effects of hypnosis. Anesthesiology 2000;92:1257–67. [DOI] [PubMed] [Google Scholar]
- 36.Landry M, Lifshitz M, Raz A. Brain correlates of hypnosis: A systematic review and meta-analytic exploration. Neuroscience and Biobehavioral Reviews 2017;81:75–98. [DOI] [PubMed] [Google Scholar]
- 37.Griffiths D, Clarkson B, Tadic SD, Resnick NM. Brain Mechanisms Underlying Urge Incontinence and its Response to Pelvic Floor Muscle Training. J Urol 2015;194:708–715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Griffiths D Imaging bladder sensations. Neurourol Urodyn. 2007;26 Supple 6:899–903. [DOI] [PubMed] [Google Scholar]
- 39.Cherkin DC, Sherman KJ, Balderson BH, Cook AJ, Anderson ML, Hawkes RJ et al. Cognitive Behavioral Therapy or Usual Care on Back Pain and Functional Limitations in Adults With Chronic Low Back Pain A Randomized Clinical Trial. JAMA 2016;315(12):1240–1249. [DOI] [PMC free article] [PubMed] [Google Scholar]


