Abstract
Background:
The purpose of this cross-sectional study was to examine if Healthy Eating Index (HEI-2015) scores are associated with coronal caries experience and odds of untreated coronal caries in adults age 20 years and older.
Methods:
Data on decayed, missing and filled teeth (DMFT), untreated coronal caries and HEI-2015 scores were obtained from 7,751 adults who completed a dental examination and two 24-hour dietary recalls in NHANES cycles 2011–12 and 2013–14. HEI-2015 scores were categorized into quintiles, with HEI quintile I being least compliant with 2015–2020 US Dietary Guidelines. The authors used multivariable linear regression to assess associations of HEI-2015 with DMFT, and logistic regression for associations with untreated coronal caries. All regression models were controlled for age, gender, race/ethnicity, current cigarette use, family income-to-poverty threshold ratio, last dental visit, education, and ever told had a heart attack.
Results:
Relative to HEI quintile I, the adjusted odds of any untreated coronal caries were: quintile V (OR=0.61, 95% CI= 0.46–0.80), IV (OR=0.66, 95% CI= 0.53–0.84), III (OR=0.76. 95% CI= 0.56–1.04) and II (OR=0.93, 95% CI= 0.66–1.31). Participants who met the recommendations for the total fruits, whole fruits, greens and beans, and added sugars components of the HEI-2015 score were less likely to have untreated coronal caries than those who failed to meet the recommendations. Overall, mean coronal DMFT also decreased as HEI-2015 scores increased but trends were not consistent in all racial/ethnic groups.
Conclusions:
Greater compliance with US Dietary Guidelines is associated with lower prevalence and odds of untreated caries in adults.
Practical Implications:
Dietary counseling for caries prevention by dental professionals should incorporate comprehensive dietary guidelines that are consistent with those intended for enhancing overall health and reducing risk of common systemic diseases.
INTRODUCTION
Dental caries is almost universal among U.S. adults. In 2011–2012, 90% of adults age 20 to 64 had caries experience, and approximately 1 in 4 had untreated caries (1). Caries risk factors include a susceptible tooth, presence of cariogenic bacteria, and available substrate – particularly in the form of simple sugars – for the bacteria to metabolize into acid.
Humans consume a complex, varied diet comprised of foods and nutrients that possess cariostatic as well as cariogenic properties. Although sugar is acknowledged as a major dietary risk factor for caries development, the effect of sugar on caries risk may be attenuated by the presence and amounts of proteins, fats, minerals, and antioxidants that confer protective effects by stimulating saliva, buffering plaque pH or inhibiting bacterial activity (2). Thus, it is reasonable to examine the relationship between total diet and caries prevalence.
The Healthy Eating Index (HEI) is a widely used measure of total dietary quality that was developed by the US Department of Agriculture to monitor the intakes of the US population (3). The reference base for the HEI-2015 scoring algorithm is the 2015–2020 Dietary Guidelines for Americans (4), which sets recommended intake levels of food groups and nutrients that are associated with common health outcomes. Higher HEI-2015 total scores and component scores for each of 13 food groups or nutrients reflect greater compliance with the dietary guidelines.
Studies using previous versions of the HEI have shown that children with early childhood caries (ECC) or severe ECC had lower HEI scores than caries-free children (5–7). In addition to having poorer overall diet quality, children with ECC were more likely to fail to meet the recommendations for grain, meat, fruit, dairy, and sodium components (5,6).
Less is known about diet quality and its association with prevalence of caries among adults. The purpose of this study was to examine if a healthy eating pattern, as measured by the HEI-2015, is associated with coronal caries experience and odds of untreated coronal caries among U.S. adults.
SUBJECTS AND METHODS
Participants
We used existing de-identified data from adults age 20 years and older who participated in both the dental examination and dietary interview in the 2011–12 and 2013–14 cycles of NHANES for this study. NHANES is a cross-sectional survey of the non-institutionalized U.S. civilian population that yields nationally representative estimates of disease prevalence and risk factors. Signed, informed consent was obtained from each participant on forms approved by the National Center for Health Statistics Research Ethics Review Board.
Coronal caries
The dental examinations were performed by licensed, calibrated examiners in the mobile examination center. Each quadrant was air-dried after which 4 surfaces (lingual, buccal, mesial, distal) of anterior teeth, and 5 surfaces (occlusal, lingual, buccal, mesial, distal) of first and second molars were examined using a mirror and explorer. Each coronal surface present was scored as sound, decayed, or restored. If a surface had both a caries lesion and a restoration, or was a retained root fragment, it was considered decayed (8). For missing teeth, surfaces were scored as missing due to dental disease (caries/periodontal disease) or due to other causes (8). Number of teeth with coronal decay (untreated coronal caries) was computed. DMFT was computed as the sum of number of teeth with coronal decay, missing due to dental disease, or restored. Third molars were excluded from the tooth count, DMFT and untreated caries. Throughout this paper, the terms DMFT and caries refer to coronal surfaces only.
Dietary data
The first day dietary recall interview was conducted in person by trained interviewers using a computer-assisted system and collected detailed information about all foods and beverages consumed during the previous 24 hours (9). Measuring guides and food models were available to help estimate portion sizes. The second recall was collected by telephone 3 to 10 days later; 89% of respondents interviewed in 2011–12 and 87% of those interviewed in 2013–14 provided reliable dietary data for both days.
We used the simple HEI scoring algorithm method after summing intakes for the two days of recording to compute an HEI-2015 score for each individual (10). The HEI-2015 total score has a maximum value of 100 and is the sum of 13 individual component scores. Maximum scores on the components are either 5 or 10 points. Higher scores on the 9 adequacy components (total vegetables, greens and beans, total fruits, whole fruits, dairy, total protein foods, seafood and plant proteins, whole grains and fatty acid ratio) reflect higher intakes. The other 4 are moderation components (refined grains, sodium, saturated fats and added sugars) and are computed so that higher scores indicate lower intakes. The maximum score for each component is assigned when the individual is compliant with the intake level recommended by the Dietary Guidelines (4). Except for the fatty acid ratio, the component scores are standardized to number of servings per 1,000 calories. We categorized total HEI-2015 scores into quintiles, with HEI quintile I having the lowest scores and quintile V the highest. We also classified participants as being compliant or not for each of the 13 HEI-2015 components.
Other data
Data on potential covariates were obtained from in-person interviews and included age, gender, race/ethnicity (Mexican-American, Other Hispanic, non-Hispanic White, non-Hispanic Black, non-Hispanic Asian, Other-including Multiracial), family income-to-poverty threshold ratio, current cigarette use in the previous 30 days, highest education level achieved, ever been told by a physician or health professional they had a medical condition (diabetes, heart attack, heart disease, congestive heart failure, stroke, or cancer), length of time since last dental visit and medication use within the past 30 days. Cigarette use was classified as current smoker or nonsmoker. Three categories of last dental visit (within the past year, >1 year but ≤3 years, or >3 years), and 3 categories of education (11th grade or less, high school graduate/GED, or some college/AA degree /college graduate) were formed. The number of medications with moderate to strong associations with xerostomia (11) was tallied for each person.
Of the 11,329 participants age 20 and older who participated in the 2 examination cycles, 10,113 had a complete oral examination. Untreated caries and DMFT were not determined for 19 participants whose teeth were all missing due to causes other than disease or for whom the condition of all teeth could not be assessed. Of those with valid caries data, 8,389 completed 2 reliable 24-hour dietary interviews. Further exclusions were made due to missing data on cigarette use (n=27), income (n=597), education (n=3), medical conditions (n=5) and last dental visit (n=6), leaving 7,751 participants for analysis of DMFT and HEI. For analysis of untreated caries and HEI, only dentate individuals (n=7,219) were included.
Statistical Analysis
Multivariable logistic regression was used for models in which odds of having untreated caries was the outcome of interest and linear regression was used to assess the association of total HEI-2015 with DMFT. We constructed the regression models by initially including age, gender, ethnicity, current cigarette use, family income-to-poverty threshold ratio, education, last dental visit, each medical condition, and number of xerostomic medications used. Age, gender and ethnicity were kept in all models whereas the other covariates were sequentially removed, beginning with the largest P value, until all those remaining had a P value<0.05. The final linear and logistic regression models included age, gender, race/ethnicity, current cigarette use, family income-to-poverty threshold ratio, education, last dental visit, and ever told had a heart attack.
To further explore how different components of the diet may influence the probability of caries, we used multivariable logistic regression to estimate the odds of untreated caries for participants who were compliant for each of the 13 HEI-2015 components relative to those who were non-compliant. These models were controlled for the same covariates as in the total HEI-2015 model as well as the added sugar component score.
We also examined interactive effects of HEI-2015, gender, race/ethnicity, income, cigarette use, last dental visit, education, and ever told had heart attack on untreated caries and on DMFT. We saw no significant interactions of HEI-2015 and any covariates with regard to untreated caries. For DMFT, we observed a significant interaction (p<0.01) between HEI-2015 and race/ethnicity.
All means, prevalence estimates and odds ratios were weighted to account for the NHANES complex survey design by using survey procedures in SAS 9.4 (SAS Institute, Cary, NC).
RESULTS
Characteristics of the population are shown in Tables 1 and 2. Persons in the highest HEI quintile were older, more likely to be female, have higher levels of income and education, more likely to have had a dental visit in the past year, and less likely to smoke cigarettes compared to those in lower quintiles (Table 1). There were also significant race/ethnicity differences among the HEI quintiles. Persons who identified as other Hispanic, non-Hispanic white, or non-Hispanic Asian tended to be over-represented in HEI quintile V, while Mexican-Americans and non-Hispanic blacks were over-represented in HEI quintile I (Table 1).
Table 1.
Demographic characteristics of US adults ≥ 20 years by quintile of Healthy Eating Index (HEI-2015) score, NHANES 2011–2012 and 2013–2014. Frequencies and means (± standard errors) are weighted to account for the complex survey design and yield estimates generalizable to the US population.
| HEI 2015 Quintile | I | II | III | IV | V | Total |
|---|---|---|---|---|---|---|
| HEI 2015 Range | 16.93 – 42.62 | 42.63– 50.44 | 50.45 – 57.89 | 57.90 – 66.74 | 66.75 – 95.80 | 16.93 – 95.80 |
| Number of participants | 1550 | 1551 | 1550 | 1550 | 1550 | 7751 |
| Age (y)* | 41.9±0.7 | 45.5±0.9 | 48.5±0.7 | 48.8±0.8 | 52.4±0.9 | 47.4±0.5 |
| Gender (%)† | ||||||
| Men | 55.5 | 52.3 | 50.5 | 45.1 | 40.4 | 48.8 |
| Women | 44.5 | 47.7 | 49.5 | 54.9 | 59.6 | 51.2 |
| Race/Ethnicity (%)† | ||||||
| Mexican-American | 10.1 | 8.6 | 7.8 | 8.5 | 5.7 | 8.2 |
| Other Hispanic | 4.1 | 5.3 | 5.8 | 6.2 | 6.2 | 5.5 |
| Non-Hispanic White | 66.8 | 67.1 | 67.9 | 66.7 | 70.2 | 67.7 |
| Non-Hispanic Black | 13.1 | 12.7 | 11.3 | 10.4 | 7.3 | 11.0 |
| Non-Hispanic Asian | 2.7 | 3.8 | 4.5 | 6.0 | 8.6 | 5.1 |
| Other, including Multi-racial | 3.3 | 2.5 | 2.6 | 2.2 | 2.1 | 2.6 |
| Family income-to-poverty threshold ratio * | 2.49±0.09 | 2.76±0.12 | 2.95±0.12 | 3.18±0.09 | 3.41±0.12 | 2.95±0.08 |
| Highest education (%)† | ||||||
| 11th grade or less | 17.4 | 16.1 | 13.6 | 12.5 | 8.7 | 13.7 |
| High school graduate/GED | 27.9 | 23.2 | 21.8 | 17.0 | 13.2 | 20.7 |
| Some college, AA degree, or college graduate | 54.7 | 60.7 | 64.6 | 70.5 | 78.1 | 65.6 |
| Last dental visit (%)† | ||||||
| Within past 1 year | 48.5 | 56.5 | 60.6 | 65.7 | 76.9 | 61.5 |
| >1 year but <= 3 years | 22.6 | 19.9 | 19.5 | 19.6 | 12.3 | 18.8 |
| > 3years | 28.9 | 23.6 | 20.0 | 14.8 | 10.8 | 19.7 |
| Current cigarette use (%)† | 32.9 | 21.3 | 19.5 | 11.3 | 8.8 | 18.8 |
| Ever told by a doctor had heart attack (%) | 3.0 | 3.0 | 4.4 | 2.6 | 3.3 | 3.3 |
Linear trend across quintiles, p<0.001.
Significantly different distribution among quintiles, p<0.001.
Table 2.
Dental health characteristics of US adults ≥ 20 years by quintile of Healthy Eating Index (HEI-2015) score, NHANES 2011–2012 and 2013–2014.
| HEI 2015 Quintile | I | II | III | IV | V | Total |
|---|---|---|---|---|---|---|
| N | 1550 | 1551 | 1550 | 1550 | 1550 | 7751 |
| Any untreated coronal caries (%)* † | 36.7 (1419) | 35.2 (1446) | 31.7 (1417) | 30.0 (1463) | 28.8 (1474) | 32.7 (7219) |
| Mean number of teeth with decayed, missing or filled coronal surfaces (DMFT)* | 13.2±0.3 | 12.9±0.3 | 12.3±0.3 | 12.2±0.3 | 11.6±0.2 | 12.5±0.2 |
| Mean number of teeth (excluding 3rd molars)* | 21.9±0.2 | 22.0±0.3 | 22.6±0.3 | 22.7±0.3 | 23.7±0.3 | 22.6±0.2 |
Means (± standard errors) and frequencies are weighted) are weighted to account for the complex survey design and yield estimates generalizable to the US population, and adjusted further for age, gender, race/ethnicity (Mexican-American, Other Hispanic, non-Hispanic White, non-Hispanic Black, non-Hispanic Asian, Other-including Multiracial), current cigarette use (yes/no), family income-to-poverty threshold ratio, education (11th grade or less, high school graduate/GED, or some college/AA degree /college graduate), last dental visit (within the past year, >1 year but ≤3 years, or >3 years), and ever told had a heart attack (yes/no).
Linear trend across quintiles, p<0.001.
Dentate persons only. N shown in parentheses.
The adjusted prevalence of untreated caries by HEI quintile is shown in Table 2 and the odds of having any untreated caries in Table 3. Prevalence of untreated caries decreased linearly from HEI quintile I to quintile V, as did mean DMFT after controlling for age, gender, race/ethnicity, current cigarette use, family income-to-poverty threshold ratio, education, last dental visit, and ever told had a heart attack. In contrast, the average number of teeth increased (Table 2). Relative to HEI quintile I, the odds of untreated caries in HEI quintiles V and IV were 39%, 34%lower, respectively. Other variables that were independently related to higher odds of untreated caries included non-Hispanic Black ethnicity, current cigarette use, dental visits more than 1 year ago, high school education or less, and ever been told had a heart attack. Higher income was associated with lower odds of untreated caries.
Table 3.
Adjusted odds ratio (OR) and 95% confidence interval (CI) of any untreated coronal caries among dentate US adults ≥ 20 years, NHANES 2011–2012 and 2013–2014.
| Predictor | OR | 95% CI | |
|---|---|---|---|
| HEI-2015 Quintile | V (highest) | 0.61 | 0.46 – 0.80 |
| IV | 0.66 | 0.53 – 0.83 | |
| III | 0.76 | 0.56 – 1.04 | |
| II | 0.93 | 0.66 – 1.31 | |
| I (lowest) | 1.00* | ||
| Age | Per increment of 10 years | 1.08 | 1.03 – 1.14 |
| Gender | Male | 1.16 | 0.96 – 1.40 |
| Female | 1.00* | ||
| Race/Ethnicity | Mexican-American | 1.18 | 0.87 – 1.61 |
| Other Hispanic | 1.02 | 0.73 – 1.43 | |
| Non-Hispanic Black | 1.97 | 1.60 – 2.62 | |
| Non-Hispanic Asian | 0.91 | 0.65 – 1.26 | |
| Other, including Multi-racial | 1.16 | 0.63 – 2.14 | |
| Non-Hispanic White | 1.00* | ||
| Current cigarette use | Yes | 2.43 | 1.89 – 3.12 |
| No | 1.00* | ||
| Family income-to-poverty threshold ratio | Per increment of 1.0 | 0.76 | 0.71 – 0.82 |
| Last dental visit | > 3years ago | 3.45 | 2.83 – 4.22 |
| > 1 but <= 3 years ago | 2.15 | 1.72 – 2.68 | |
| ≤ 1 year ago | 1.00* | ||
| Ever told by a doctor/ health professional had heart attack | Yes | 1.58 | 1.05 – 2.37 |
| No | 1.00* | ||
| Highest education | 11th grade or less | 1.63 | 1.30 – 2.04 |
| High school graduate/GED | 1.38 | 1.05 – 1.81 | |
| Some college, AA degree, or college graduate | 1.00* |
Reference category
Participants who were compliant with the total fruit, whole fruit, greens and beans, and added sugars components had significantly lower odds of untreated caries (21% to 28% reductions) compared to those who failed to consume the recommended intake levels (Table 4). Odds of untreated caries were also reduced among persons who were compliant with other food groups (total vegetable, whole grains, seafood and plant proteins and refined grains) but the reductions were not statistically significant.
Table 4.
Adjusted odds ratio (OR) and 95% confidence interval (CI) of any untreated coronal caries among participants who met the recommendation for HEI-2015 component scores, dentate US adults ≥ 20 years, NHANES 2011–2012 and 2013–2014.
| HEI-2015 component | Recommendation | OR* | 95% CI |
|---|---|---|---|
| Adequacy components | |||
| Greens & Beans | ≥0.2 cups per 1000 Kcal | 0.72 | 0.59 – 0.88 |
| Total Fruits | ≥ 0.8 cups per 1000 Kcal | 0.75 | 0.60 – 0.94 |
| Whole Fruits | ≥ 0.4 cups per 1000 Kcal | 0.79 | 0.62 – 0.99 |
| Total Vegetables | ≥ 1.1 cups per 1000 Kcal | 0.81 | 0.64 – 1.03 |
| Whole Grains | ≥ 1.5 ounces per 1000 Kcal | 0.85 | 0.59 – 1.23 |
| Seafood & Plant Proteins | ≥0.8 ounces per 1000 Kcal | 0.88 | 0.70 – 1.09 |
| Fatty Acids | Ratio of PUFA+MUFA to SFA ≥2.5† | 1.00 | 0.82 – 1.21 |
| Total Protein Foods | ≥2.5 ounces per 1000 Kcal | 1.05 | 0.83 – 1.32 |
| Dairy | ≥ 1.3 cups per 1000 Kcal | 1.19 | 0.94 – 1.51 |
| Moderation components | |||
| Added sugars | ≤6.5% of energy | 0.74 | 0.58 – 0.93 |
| Refined Grains | ≤1.8 ounces per 1000 Kcal | 0.97 | 0.81 – 1.17 |
| Saturated Fats | ≤8% of energy | 1.09 | 0.91 – 1.31 |
| Sodium | ≤1.1 grams per 1000 Kcal | 1.09 | 0.79 – 1.50 |
Odds of untreated caries compared to those who did not meet recommendation for component. Odds ratios are adjusted for age, gender, race/ethnicity (Mexican-American, Other Hispanic, non-Hispanic White, non-Hispanic Black, non-Hispanic Asian, Other-including Multiracial), current cigarette use (yes/no), family income-to-poverty threshold ratio, education (11th grade or less, high school graduate/GED, or some college/AA degree /college graduate), last dental visit (within the past year, >1 year but ≤3 years, or >3 years), and ever told had a heart attack (yes/no). Odds ratios for components (except for added sugars component) were additionally adjusted for the added sugars score.
PUFA=polyunsaturated fatty acids. MUFA=monounsaturated fatty acids. SFA=saturated fatty acids.
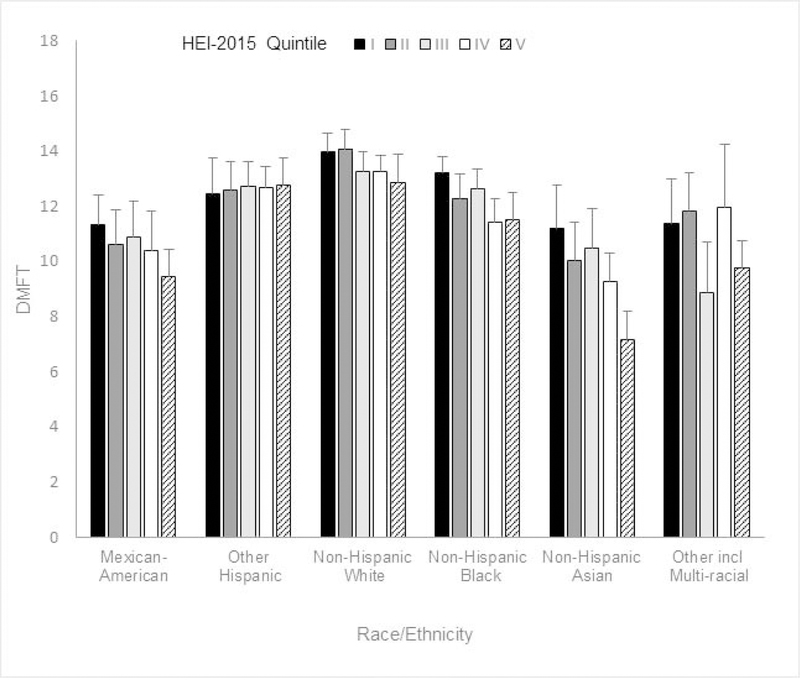
Although mean DMFT was inversely associated with HEI quintiles in the total study population, the interaction between HEI and race/ethnicity indicated this trend was not consistent among all ethnic groups. After adjustment for age, gender, current cigarette use, family income-to-poverty threshold ratio, education, last dental visit, and ever told had a heart attack, the association remained statistically significant only among non-Hispanic whites, non-Hispanic blacks, and non-Hispanic Asians (Figure 1).
Figure 1.
Mean (±2 se) coronal DMFT among US adults ≥ 20 years, by quintile of Healthy Eating Index (HEI-2015) score and race/ethnicity, NHANES 2011–2012 and 2013–2014. Means are adjusted for age, gender, current cigarette use (yes/no), family income-to-poverty threshold ratio, education (11th grade or less, high school graduate/GED, or some college/AA degree /college graduate), last dental visit (within the past year, >1 year but ≤3 years, or >3 years), and ever told had a heart attack (yes/no).
P values for linear trend across quintiles were as follows:
Mexican-Americans, P=0.07; Other Hispanic, P=0.64; non-Hispanic White, P<0.01; non-Hispanic Black, P<0.01; non-Hispanic Asian, P<0.001; Other-including Multiracial, P=0.32.
DISCUSSION
The major findings in our study show that that adults whose diets conform more closely to the 2015–2020 Dietary Guidelines for Americans have reduced odds of untreated caries. Between 1999 and 2014, average HEI scores among US adults have risen slightly, but still remain in the range of 56 to 60 (12). Our findings suggest about half of adults may reduce their chance of having untreated caries if their diets were aligned more closely with the 2015–2020 Dietary Guidelines for Americans.. Our results are consistent with those of studies of dietary quality and early childhood caries (5–7) and underscore the recognition that integration of oral health promotion with nutrition education and guidance is crucial to ensure comprehensive care for patients of all ages (13). Despite the ease with which the public can access sound nutritional information, the majority of the US population falls short of meeting many of the dietary guidelines. Consumption of fruits and vegetables in particular has consistently remained below recommended levels (14, 15). If greater advances in diet quality of the population are to be realized, there need to be substantial changes in individual’s dietary intakes. Dentists have the opportunity to play a role in changing behaviors by coordinating and reinforcing nutrition education messages with those given by physicians, dietitians, nurse practitioners and other health professionals.
The results of this analysis do not contradict the well-established association between sugar intake and caries (16); persons who conformed to the recommendation for the added sugars component (≤6.5% of energy) had 24% lower odds of untreated caries than participants who consumed more sugar. It is notable that several other food groups (whole and total fruits green vegetables) were associated with lower odds of decay after controlling for the level of added sugar consumed. These foods are rich sources of other nutrients such as isothionates (17) and polyphenols (18) that are thought to have the potential to restrict the progression of caries. Our findings are consistent with a previous study of dietary quality among children that reported inverse associations between caries and intake of fruits and vegetables (19) and with the lower rate of root caries found in older men who were compliant with the Dietary Approaches to Stop Hypertension eating plan (20), which, like the HEI, stresses increased fruit and vegetable consumption along with limited sweets.
The strengths of this study are the carefully calibrated and systematic collection of coronal caries data and the nationally representative study sample. A possible limitation is the use of self-reported 24-hour dietary recall data to assess intake. The multiple non-consecutive 24-hour recall methodology used by NHANES is a valid tool for assessing usual diet and describing intake percentiles (21, 22), but it is difficult to determine the time frame of exposure that is most relevant for caries progression. Recent diet may be more germane to risk of active caries than to DMFT, which is a reflection of caries experience, access to dental care and oral hygiene practices across the lifespan. Yet we did observe significant inverse associations between HEI and both untreated caries and DMFT. Data from 24-hour recalls may reflect longer-term intakes if eating behaviors are stable over time but the cross-sectional study design precludes examination of changes in behaviors. We speculate that the ethnic disparities we observed in associations between HEI and DMFT could be explained in part by variation in adoption of U.S. dietary patterns among ethnic subgroups of different countries of origin and their length of residence (23–26). Some misclassification of HEI quintile is expected due to under-or over-reporting, but the use of two non-consecutive 24-hour recalls minimizes extreme variations and the effect of misclassification would be to attenuate associations with untreated caries and DMFT. Other limitations include the inability to distinguish between teeth lost due to caries or to periodontal disease, and lack of data on root caries which are prevalent among older adults (27).
These findings suggest an additional dietary strategy for caries prevention, one that promotes overall dietary quality in contrast to a narrow focus on reducing added sugar content of the diet to 5 or 10% of caloric intake (16). Consumers are encouraged to use nutrition fact labels on processed foods to lower their consumption of added sugar. However, many people have difficulty understanding the labels and making calculations such as percent of calories (28). A simpler approach of following dietary guidelines for servings of fruits and vegetables may partially displace sugar-sweetened beverages and sweet bakery products that are the main sources of added sugar in the American diet (29).
PUBLIC HEALTH IMPLICATIONS
Greater compliance with the 2015–2020 US Dietary Guidelines may reduce the chance of having untreated caries among adults. Therefore, dietary guidelines for caries prevention can be aligned with those for reducing risk of chronic systemic diseases. Higher HEI scores have been associated with lower risks of health outcomes as diverse as all-cause mortality, cardiovascular and cancer mortality (30), cognitive function (31), and hearing loss (32). An oral health promotion message that integrates the mouth with the rest of the body may be more efficient for improving population health than dietary recommendations that target individual oral conditions (33).
ACKNOWLEDGEMENTS
This study was supported in part by NIDCR, R03 DE18758.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure. None of the authors reported any disclosures.
None of the authors report a conflict of interest related to this study.
Contributor Information
Elizabeth A. Kaye, Department of Health Policy & Health Services Research, Boston University Henry M. Goldman School of Dental Medicine, 560 Harrison Ave., Boston MA 02118.
Woosung Sohn, Department of Population Oral Health, University of Sydney School of Dentistry, Sydney, Australia.
Raul I. Garcia, Department of Health Policy & Health Services Research, Boston University Henry M. Goldman School of Dental Medicine, Boston MA.
REFERENCES
- 1.Dye BA, Thornton-Evans G, Li X, Iafolla TJ. Dental caries and tooth loss in adults in the United States, 2011–2012 NCHS Data Brief, no. 197. Hyattsville, MD: National Center for Health Statistics; 2015. [PubMed] [Google Scholar]
- 2.Giacaman RA. Sugars and beyond. The role of sugars and the other nutrients and their potential impact on caries. Oral Dis. 2018;24:1185–1197. [DOI] [PubMed] [Google Scholar]
- 3.United States Department of Agriculture. Center for Nutrition Policy and Promotion. Healthy Eating Index. Available at: https://www.cnpp.usda.gov/healthyeatingindex (accessed 18 December 2018).
- 4.Office of Disease Prevention and Health Promotion. Dietary Guidelines for Americans 2015–2020, eighth edition. Available at: https://health.gov/dietaryguidelines/2015/guidelines/ (accessed 18 December 2018).
- 5.Nunn ME, Braunstein NS, Kaye EAK, et al. Healthy Eating Index is a predictor of early childhood caries. J Dent Res. 2009;88(4):361–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zaki NAA, Dowidar KML, Abdelaziz WEE. Assessment of the Healthy Eating Index-2005 as a predictor of early childhood caries. Int J Paediatr Dent. 2015;25(6):436–443. [DOI] [PubMed] [Google Scholar]
- 7.AbdelAziz WE, Dowidar KML, El Tantawi MMA. Association of healthy eating, juice consumption, and bacterial counts with early childhood caries. Pediatr Dent. 2015;37(5):462–467. [PubMed] [Google Scholar]
- 8.National Center for Health Statistics. National Health and Nutrition Examination Survey. NHANES 2001–2012: Oral Health Examiners Manual. Available at: https://wwwn.cdc.gov/nchs/data/nhanes/2011-2012/manuals/Oral_Health_Examiners_Manual.pdf (accessed 18 December 2018).
- 9.National Center for Health Statistics. National Health and Nutrition Examination Survey. MEC In-Person Dietary Interviewers Procedures Manual. Available at: https://www.cdc.gov/nchs/data/nhanes/nhanes_03_04/dietary_mec.pdf (accessed 18 December 2018).
- 10.National Cancer Institute. Division of Cancer Control and Population Sciences. Epidemiology and Genomics Research Program. HEI Scoring Algorithm. Available at: https://epi.grants.cancer.gov/hei/hei-scoring-method.html (accessed 18 December 2018).
- 11.Wolff A, Joshi RK, Ekstrom J, Aframian D, Pedersen AML, Proctor G, et al. A guide to medications inducing salivary gland dysfunction, xerostomia, and subjective sialorrhea: A systematic review sponsored by the World Workshop on Oral Medicine VI. Drugs R D. 2017;17(1):1–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wilson MM, Reedy J, Krebs-Smith SM. American Diet Quality: Where it is, where it is heading, and what it could be. J Acad Nutr Diet. 2016; 116(2): 302–310.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Touger-Decker R, Mobley CC, American Dietetic Association. Position of the American Dietetic Association: Oral health and nutrition. J Am Diet Assoc. 2003;103(5):615–625. [DOI] [PubMed] [Google Scholar]
- 14.Blanck HM, Gillespie C, Kimmons JE, Seymour JD, Serdula MK. Trends in fruit and vegetable consumption among U.S. men and women, 1994–2005. Prev Chronic Dis. 2008;5(2):A35 http://www.cdc.gov/pcd/issues/2008/apr/07_0049.htm (accessed 3 May 2019). [PMC free article] [PubMed] [Google Scholar]
- 15.Lee-Kwan SH, Moore LV, Blanck HM, Harris DM, Galuska D. Disparities in state-specific adult fruit and vegetable consumption — United States, 2015. MMWR Morb Mortal Wkly Rep. 2017;66:1241–1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moynihan P. Sugars and dental caries: Evidence for setting a recommended threshold for intake. Adv Nutr. 2016;7(1):149–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ko MO, Kim MB, Lim SB. Relationship between chemical structure and antimicrobial activities of isothiocyanates from cruciferous vegetables against oral pathogens. J Microbiol Biotechnol. 2016;26(12):2036–2042. [DOI] [PubMed] [Google Scholar]
- 18.Ferrazzano GF, Amato I, Ingenito A, et al. Plant polyphenols and their anti-cariogenic properties: a review. Molecules. 2011;16(2):1486–1507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dye BA, Shenkin JD, Ogden CL, et al. The relationship between healthful eating practices and dental caries in children aged 2–5 years in the United States, 1988–1994. J Am Dent Assoc. 2004;135(1):55–66. [DOI] [PubMed] [Google Scholar]
- 20.Kaye EK, Heaton B, Sohn W, et al. The Dietary Approaches to Stop Hypertension Diet and new and recurrent root caries events in men. J Am Geriatr Soc. 2015;63(9):1812–1819. [DOI] [PubMed] [Google Scholar]
- 21.Moshfegh AJ, Rhodes DG, Baer DJ, et al. The US Department of Agriculture Automated Multiple-Pass Method reduces bias in the collection of energy intakes. Am J Clin Nutr. 2008;88(2):324–332. [DOI] [PubMed] [Google Scholar]
- 22.National Cancer Institute. Dietary Assessment Primer. Available at: https://dietassessmentprimer.cancer.gov/approach/table.html#row_1 (accessed 9 May 2019).
- 23.Satia-Abouta J, Patterson RE, Neuhouser ML, Elder J. Dietary acculturation: applications to nutrition research and dietetics. J Am Diet Assoc. 2002;102(8):1105–1118. [DOI] [PubMed] [Google Scholar]
- 24.Lesser IA, Gasevic D, Lear SA. The association between acculturation and dietary patterns of South Asian immigrants. PloS One. 2014;9(2):e88495. doi: 10.1371/journal.pone.0088495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bermudez OI, Falcon LM, Tucker KL. Intake and food sources of macronutrients among older Hispanic adults: association with ethnicity, acculturation, and length of residence in the United States. J Am Diet Assoc. 2000;100(6):665–673. [DOI] [PubMed] [Google Scholar]
- 26.Neuhouser ML, Thompson B, Coronado GD, Solomon CC. Higher fat intake and lower fruit and vegetables intakes are associated with greater acculturation among Mexicans living in Washington State. J Am Diet Assoc. 2004;104(1):51–57. [DOI] [PubMed] [Google Scholar]
- 27.Kim JK, Baker LA, Seirawan H, Crimmins EM. Prevalence of oral health problems in U.S. adults, NHANES 1999–2004: exploring differences by age, education, and race/ethnicity. Spec Care Dentist. 2012;32(6):234–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Campos S, Doxey J, Hammond D. Nutrition labels on pre-packaged foods: a systematic review. Public Health Nutr. 2011;14(8):1496–1506. [DOI] [PubMed] [Google Scholar]
- 29.Bailey RL, Fulgoni VL, Cowan AE, Gaine PC Sources of added sugars in young children, adolescents, and adults with low and high intakes of added sugars. Nutrients. 2018. January 17;10(1).pii: E102. doi: 10.3390/nu10010102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Panizza CE, Shvetsov YB, Harmon BE, et al. Testing the predictive validity of the Healthy Eating Index-2015 in the Multiethnic Cohort: Is the score associated with a reduced risk of all-cause and cause-specific mortality? Nutrients. 2018. April 5;10(4). pii: E452. doi: 10.3390/nu10040452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wright RS, Waldstein SR, Kuczmarski MF, et al. Diet quality and cognitive function in an urban sample: findings from the Healthy Aging in Neighborhoods of Diversity across the Life Span (HANDLS) study. Public Health Nutr. 2017;20(1):92–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Spankovich C, Le Prell CG. Associations between dietary quality, noise, and hearing: data from the National Health and Nutrition Examination Survey, 1999–2002. Int J Audiol. 2014;53(11):796–809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sheiham A, Watt RG. The common risk factor approach: a rational basis for promoting oral health. Community Dent Oral Epidemiol. 2000;28(6):399–406. [DOI] [PubMed] [Google Scholar]